Abstract
Objective
To evaluate whether overweight and obese patients have less trust in their primary care providers (PCPs) if they feel judged about their weight by these PCPs.
Methods
We conducted a national internet-based survey of 600 adults engaged in primary care with a BMI≥25kg/m2 in 2012. Our dependent variable was high patient trust in their PCP (score≥8/10). Our independent variable was “feeling judged about my weight by my PCP” dichotomized as “often/sometimes” versus “never.” We conducted a multivariate logistic regression model adjusted for patient and PCP factors using survey weights.
Results
Overall, 21% felt that their PCP judged them about their weight. Respondents who perceived judgment were significantly less likely to report high trust in their PCP [OR 0.55, 95%CI 0.31-0.98].
Conclusion
While only a fifth of overweight and obese patients perceived weight-related judgment from their PCPs, these patients were significantly less likely to report high trust in these providers. Given patients’ decreased trust in providers who convey weight-related judgment, our results raise concerns about potential effects on the doctor-patient relationship and patient outcomes.
Practice Implications
Addressing provider stigma towards patients with obesity could help build trust in these patient-provider relationships and improve quality of care.
Keywords: Obesity, patient-provider, trust, primary care
1. Introduction
Prior studies have described the influence of physician trust in patient-provider relationships. Patients who trust their primary care provider (PCP) are more likely to be committed to the primary care relationship and more likely to adhere to medical advice (1). A qualitative study of patient-physician dyads found that working together to earn mutual trust helped the pairs navigate challenging primary care relationships (2). Another study found that patients with hypertension who had complete trust in their PCP were more likely to attempt weight loss as compared to patients who had less than complete trust in their provider (3). Conversely, patients with diabetes who reported lower trust in their physician were significantly more likely to be non-adherent to their hypoglycemic medications (4). This evidence suggests that trust within the patient-provider relationship can lead to improved outcomes, which underscores the importance of understanding factors that may decrease patient trust.
Stigmatizing experiences may be a contributing factor in decreased trust and poor health outcomes. A recent study found that African American patients who reported racial discrimination had lower medication adherence, which resulted, in part, from decreased trust in their physicians (5). Weight stigma includes discriminatory attitudes and behaviors against individuals with obesity (6). Weight stigma occurs among patients in relation to their physicians, where they have lower trust in overweight/obese physicians (7). Weight stigma is also pervasive among healthcare providers (6,8-11), and obese individuals commonly report experiencing stigma and insensitive comments from physicians (9,11). Physicians have been shown to have less respect for obese patients (10). These attitudes may lead patients to have less trust in their PCP. However, we are unaware of any studies that have examined this question.
Our objective was to evaluate whether overweight and obese patients have less trust in their PCP if they feel judged about their weight. We hypothesized that patients who feel judged by their PCPs would be less likely to trust these providers.
2. Methods
We conducted a cross-sectional, internet-based survey of a nationally representative sample of 600 overweight and obese U.S. adults about physician factors that influence patient trust (12). The authors designed the survey instrument, which was reviewed for content by obesity and primary care researchers and pilot-tested and revised for comprehensibility and length. We recruited Authentic Response web panel members through invitation to represent a general U.S. population sample. Invited members were eligible for the survey if they had seen their PCP within the last 12 months and their BMI was ≥25 kg/m2. Survey completion rate was 93%, which is similar to other Internet survey research (13). The Johns Hopkins Bloomberg School of Public Health Institutional Review Board approved this study.
Our dependent variable was patient trust in their PCP. We asked participants, “Using any number from 0 to 10, where 0 means that you do not trust this doctor at all and 10 means that you trust this doctor completely, what number would you use to rate how much you trust this doctor?” which has been previously validated and tested (14). This variable demonstrated a skewed distribution favoring higher ratings of trust; therefore, we dichotomized this variable as ‘high trust’ for scores ≥8 and ‘lower trust’ for scores <8 based on a cut point in the data.
Our independent variable was patient perceptions of PCP judgment about their weight. We asked participants, “In the last 12 months, did you ever feel that this doctor judged you because of your weight?” with the options on answering “often,” “sometimes,” or “never.” Participants were asked to keep their current PCP in mind when answering this question. We dichotomized this variable as ‘felt judged’ if participants indicated they were “often” or “sometimes” judged, otherwise they were labeled as ‘not judged.”
Our covariates included several patient- and PCP-level variables. Patient covariates included age, sex, race/ethnicity, BMI, insurance status, education, and duration of relationship with PCP. Patients reported characteristics about their PCP, which included approximate age, sex, perceived race/ethnicity, and approximate BMI evaluated by a body size pictogram.
All analyses were conducted in STATA, version 11 (College Station, TX). We used weighting to address systematic under- or over-representations of subpopulations within the panel, account for systematic non-response along known demographic characteristics, and adjust for sampling biases due to differences in response rates (15). The weighted margin of error was +/−4.9%. We used STATA's SVY function to adjust for the complex survey design in all analyses described below.
We performed descriptive analyses for all variables using chi-square and t-tests as appropriate. We conducted multivariate logistic regression analyses to evaluate the relationship between perceived weight-related judgment and high trust in PCP. All models were adjusted for patient age, patient sex, patient race, patient BMI, PCP relationship duration, PCP race, and perceived PCP BMI. We included these covariates based on their prior associations with the patient-physician relationship (12, 16-18), regardless of statistical significance. Using post-estimation adjust command, we calculated the adjusted predicted probabilities for all outcomes.
3. Results
We screened 1380 panel members who responded to the survey invitation, and excluded 335 participants who had not seen their PCP in the last year, 396 who did not have a BMI≥25kg/m2, 6 who were currently pregnant, and 43 who had incomplete survey responses. Our final sample included 600 participants. Overall, mean age was 47.4 years, 48% were female, mean BMI was 31.5 kg/m2, and 74% reported high trust in their PCP. Table 1 compares patient and PCP characteristics between those participants who perceived judgment by their PCP because of their weight with those who did not feel judged. Patients who perceived judgment were significantly younger, had greater BMI, and had newer relationships with their PCPs (<5 years).
Table 1.
Patient and PCP characteristics between patients who did and did not perceive weight-related judgment
| Not Judged (n=472) | Judged (n=127) | p-value | |
|---|---|---|---|
|
Patient Characteristics
| |||
| Mean age (years) | 49.4 | 40.0 | <0.01 |
| Female | 49% | 41% | 0.18 |
| Race/ethnicity | <0.01 | ||
| Non-Hispanic white | 78% | 66% | |
| Non-Hispanic black | 14% | 14% | |
| Other* | 7% | 20% | |
| Mean BMI (kg/m2) | 31.1 | 33.0 | 0.01 |
| Insurance status | 0.20 | ||
| Private insurance | 53% | 61% | |
| Government insurance** | 38% | 27% | |
| Uninsured | 8% | 12% | |
| Education | 0.49 | ||
| High school or less | 35% | 29% | |
| Vocational or some college | 40% | 41% | |
| College or beyond | 26% | 31% | |
| PCP relationship ≥5 years | 51% | 29% | <0.01 |
|
PCP Characteristics | |||
| Approximate PCP age | 0.30 | ||
| 25-44 years | 32% | 38% | |
| ≥45 years | 68% | 62% | |
| Female PCP | 37% | 34% | 0.59 |
| Perceived PCP race/ethnicity | 0.06 | ||
| Non-Hispanic white | 69% | 61% | |
| Non-Hispanic black | 5% | 7% | |
| Asian | 10% | 19% | |
| Other* | 16% | 13% | |
| Approximate PCP BMI | <0.01 | ||
| Normal | 19% | 11% | |
| Overweight | 56% | 43% | |
| Obese | 26% | 45% | |
PCP primary care provider.
For patients, other race includes Asian, Native American, Pacific Islander, or Hispanic. For PCPs, other race includes Native American, Pacific Islander, or Hispanic.
Government insurance includes Medicare, Medicaid, and military. Estimates generated using survey weights.
For respondents who felt judged by their PCP, 60% reported a high trust score, while 78% of respondents who did not feel judged reported a high score (p<0.01). Respondents who perceived judgment were significantly less likely to report high levels of trust in their PCP [OR 0.55, 95%CI 0.31-0.98, p=0.04] (Table 2). Figure 1 shows the adjusted predicted probabilities for patients reporting high trust in their PCP (score ≥8) by whether or not they perceived weight-related judgment by that PCP.
Table 2.
Association of patient perceived weight-related judgment by their primary care provider (PCP) and other covariates with high trust in PCP
| Variable | Odds Ratio | 95% Confidence Interval | p-value |
|---|---|---|---|
| Perceived PCP weight-related judgment | 0.55 | 0.31-0.97 | 0.04 |
|
Patient Covariates | |||
| Age | 1.02 | 1.01-1.03 | <0.01 |
| Sex | 0.91 | 0.58-1.43 | 0.67 |
| Race/ethnicity | |||
| Non-Hispanic white | Ref | -- | |
| Non-Hispanic black | 1.12 | 0.62-2.04 | 0.70 |
| Other* | 0.98 | 0.40-2.39 | 0.96 |
| BMI | 0.98 | 0.95-1.02 | 0.32 |
| PCP relationship ≥5 years | 1.28 | 0.80-2.05 | 0.30 |
|
Provider Covariates | |||
| Race/ethnicity | |||
| Non-Hispanic white | Ref | -- | -- |
| Non-Hispanic black | 1.09 | 0.43-2.76 | 0.85 |
| Asian | 1.08 | 0.46-2.3 | 0.86 |
| Other* | 0.92 | 0.50-1.68 | 0.78 |
| Approximate BMI | |||
| Normal weight | Ref | -- | -- |
| Overweight | 0.79 | 0.44-1.42 | 0.44 |
| Obese | 0.70 | 0.35-1.39 | 0.31 |
PCP primary care provider.
For patients, other race includes Asian, Native American, Pacific Islander, or Hispanic. For PCPs, other race includes Native American, Pacific Islander, or Hispanic. Estimates generated using survey weights.
Figure 1.
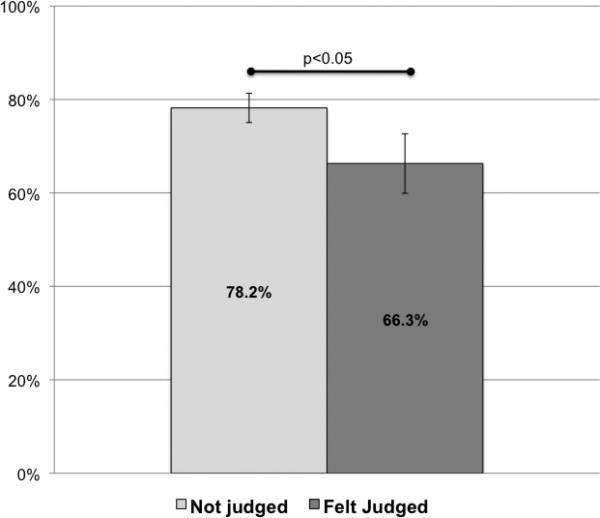
Comparison of predicted probabilities for reporting high trust in primary care provider (PCP) by whether or not patients perceived judgment by their PCP about their weight. High trust level was defined as a score of ≥8 out of 10. Patients who perceived judgment by their PCP were significantly less likely to report high trust in their PCP (p<0.05) as compared to patients who did not perceive their PCP judged them about their weight. Predicted probabilities, 95% confidence intervals, and p-value estimated from logistic regression model adjusted for patient age, patient sex, patient race, patient BMI, PCP relationship duration, PCP race and perceived PCP BMI. Estimates generated using survey weights.
4. Discussion and Conclusion
4.1 Discussion
Our study shows that perceived PCP weight-related judgment is associated with decreased trust in patient-provider relationships. While only 21% of overweight and obese patients perceived judgment from their current PCPs because of their weight, these patients were significantly less likely to report high trust in these providers. Interpersonal competence including caring, concern, listening, and compassion contribute to patients’ trust in physicians, beyond the physicians’ medical knowledge and technical skills (19). A prior study, which used similar high trust scores, found an association between high trust in PCP and patients’ receipt of preventive health screenings (20). Perceived PCP negative regard towards patients with obesity may prevent the development of these interpersonal connections, and could contribute to reduced quality of care and previously documented healthcare disparities for obese patients (21-24).
Many prior studies have documented physicians’ negative regard towards patients with obesity (6,8-11), which seems to negatively influence patient-provider relationships. A recent study found that physicians engage in significantly less emotional rapport building with overweight and obese patients as compared to those of normal weight (25). Our study adds to this literature by demonstrating how overweight and obese patients who feel judged about their weight have lower trust in their PCPs. Given this mounting evidence, investigators need to consider how we can address providers’ weight stigma. A recent pilot study demonstrated that brief anti-stigma films in reducing weight bias significantly improved healthcare trainees’ explicit attitudes and beliefs toward obese people, but did not alter implicit anti-fat bias (26). While the results of this study show promise, additional research is needed to develop and test curricula that address weight stigma and augment healthcare professionals’ skills, especially among providers currently in practice.
Our study has several limitations. As this study was cross-sectional study, we cannot make causal inferences. We caution readers to view our results as exploratory, as we examined the association between two questions that both relied upon the respondent's self-report of experiences with their PCP, which may be less reliable. While we suspect that our findings are related to differences in provider behavior, unmeasured patient confounders may explain the association. We believe that our results need to be replicated and examined with rigorous methods to confirm our findings. We did not evaluate what aspect of patients’ interactions with their PCPs led them to perceive that their PCP judged them because of their weight. Patients are likely to have different interpretations of what signifies ‘judgment.’ We also cannot know whether the PCPs believed that they judged these patients. Future research should consider evaluating both patient and PCP attitudes about judgment, and identify what behaviors may trigger these perceptions. We relied upon self-reported weights to calculate BMI and patient-reported PCP attributes, which may have inaccuracies. We did not have respondents distinguish whether their PCP was a physician or nurse practitioner. We only included patients who were actively engaged in primary care, so our population excludes patients who may not be engaged in care due to dissatisfaction or lack of trust in the healthcare system. A prior study found that overweight and obese patients were more likely to “doctor shop” (27), so our results may underestimate the prevalence of patient-perceived weight-related judgment by providers.
4.2 Conclusion
In this exploratory study, patients who felt that their current PCPs judged them because of their weight were significantly less likely to report high trust in these providers. Given the prior literature documenting the increased risk of non-adherence when patients’ trust in the PCP is low, our results raise concern that the perception of weight-related judgment may contribute to reduced quality of care and health disparities for patients with obesity. Future interventions that address PCP weight bias may help increase obese patients’ trust in these providers, and thereby strengthen patient-provider relationships.
Highlights.
Whether provider weight stigma leads to decreased patient trust in providers in unknown
We found that respondents who perceived weight-related judgment from their primary care provider were significantly less likely to report high levels of trust in that provider
Our exploratory results raise concern that perceived weight-related judgment may contribute to reduced quality of care and health disparities for patients with obesity
Acknowledgements
KAG and SNB were supported by trainee awards from the National Heart, Lung, and Blood Institute's Center for Population Health and Health Disparities (P50HL0105187). The National Heart, Lung, and Blood Institute also provided support through the following grants: KAG by K23HL116601, WLB by K23HL098476, LAC by K24HL083113, and SNB by K01HL096409.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.Berry LL, Parish JT, Janakiraman R, Ogburn-Russell L, Couchman GR, Rayburn WL, et al. Patients’ commitment to their primary physician and why it matters. Ann Fam Med. 2008;6:6–13. doi: 10.1370/afm.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ratanawongsa N, Wright SM, Vargo EM, Carrese JA. Challenges in primary care relationships: seeing it from both sides. Patient Educ Couns. 2011;85:40–5. doi: 10.1016/j.pec.2010.07.042. [DOI] [PubMed] [Google Scholar]
- 3.Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns. 2012;89:57–62. doi: 10.1016/j.pec.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ratanawongsa N, Karter AJ, Parker MM, Lyles CR, Heisler M, Moddwrr HH, et al. Communication and medication refill adherence: the Diabetes Study of Northern California. JAMA Intern Med. 2013;173:210–8. doi: 10.1001/jamainternmed.2013.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuffee YL, Hargraves JL, Rosal M, Briesacher BM, Schoenthaler A, Person S, et al. Reported racial discrimination, trust in physicians, and medication adherence among inner-city African Americans with hypertension. Am J Public Health. 2013;103:e55–62. doi: 10.2105/AJPH.2013.301554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 7.Puhl RM, Gold JA, Luedicke J, DePierre JA. The effect of physicians’ body weight on patient attitudes: implications for physician selection, trust and adherence to medical advice. Int J Obes. 2013;37:1415–21. doi: 10.1038/ijo.2013.33. [DOI] [PubMed] [Google Scholar]
- 8.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring) 2009;17:941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- 9.Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring) 2006;14:1802–15. doi: 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- 10.Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach CM. Physician respect for patients with obesity. J Gen Intern Med. 2009;24:1236–1239. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buxton BK, Snethen J. Obese women's perceptions and experiences of healthcare and primary care providers. Nurs Res. 2013;62:252–9. doi: 10.1097/NNR.0b013e318299a6ba. [DOI] [PubMed] [Google Scholar]
- 12.Bleich SN, Gudzune KA, Bennett WL, Jarlenski M, Cooper LA. How does physician BMI impact patient trust and perceived stigma? Prev Med. 2013;57:120–4. doi: 10.1016/j.ypmed.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Puhl R, Peterson JL, Luedicke J. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. Int J Obes (London) 2013;37:612–9. doi: 10.1038/ijo.2012.110. [DOI] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Quality and Research . About the CAHPS® Cultural Competence Item Set. CAHPS® Clinician & Group Surveys and Instructions; Washington, DC: 2013. [Google Scholar]
- 15.Keeter S, Miller C, Kohut A, Groves RM, Presser S. Consequences of reducing non-response in a national telephone survey. Public Opinion Quarterly. 2000;64:125–48. doi: 10.1086/317759. [DOI] [PubMed] [Google Scholar]
- 16.Roter D, Hall JA. Doctors talking with patients/patients talking with doctors: improving communication in medical visits. second edition Praeger Publishers; Westport, CT: 2006. [Google Scholar]
- 17.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–90. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghods BK, Roter DL, Ford DE, Larson S, Arbelaez JJ, Cooper LA. Patient-physician communication in primary care visits with African-Americans and whites with depression. J Gen Intern Med. 2008;23:600–6. doi: 10.1007/s11606-008-0539-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mechanic D, Meyer S. Concepts of trust among patients with serious illness. Soc Sci Med. 2000;51:657–68. doi: 10.1016/s0277-9536(00)00014-9. [DOI] [PubMed] [Google Scholar]
- 20.O'Malley AS, Sheppard VB, Schwartz M, Mandelblatt J. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004;38:777–85. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 21.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes (Lond) 2006;30:147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 22.Heo M, Allison DB, Fontaine KR. Overweight, obesity, and colorectal cancer screening: disparity beween men and women. BMC Public Health. 2004;4:53. doi: 10.1186/1471-2458-4-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maruthur NM, Bolen S, Brancati FL, Clark JM. Obesity and mammography: a systematic review and meta-analysis. J Gen Intern Med. 2009;24:665–77. doi: 10.1007/s11606-009-0939-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maruthur NM, Bolen SD, Brancati FL, Clark JM. The association of obesity and cervical cancer screening: a systematic review and meta-analysis. Obesity (Silver Spring) 2009;17:375–81. doi: 10.1038/oby.2008.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity (Silver Spring) 2013;21:2146–52. doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swift JA, Tischler V, Markham S, Gunning I, Glazebrook C, Beer C, et al. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized controlled trial. Obes Facts. 2013;6:91–102. doi: 10.1159/000348714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gudzune KA, Bleich SN, Richards TM, Weiner JP, Hodges K, Clark JM. Doctor shopping my overweight and obese patients is associated with increased healthcare utilization. Obesity (Silver Spring) 2013;21:1328–34. doi: 10.1002/oby.20189. [DOI] [PMC free article] [PubMed] [Google Scholar]


