TO THE EDITOR:
There is limited information on the role of fractional excretion of nitric oxide (FeNO) during pediatric acute asthma exacerbations.1, 2 We performed a secondary analysis of data from a prospective cohort ages 5 – 17 years of age. Participants had doctor-diagnosed asthma and presented to our tertiary pediatric emergency department with acute exacerbations defined using NAEPP guidelines that required inhaled bronchodilator and systemic corticosteroid treatment.3 We sought to examine whether there are associations of FeNO with % predicted FEV1 and with relevant patient characteristics during these episodes.4
Pre-bronchodilator pulmonary examination, FeNO testing and spirometry for % predicted FEV1 were performed under an IRB exemption for immediate informed consent. FeNO testing was performed prior to spirometry to avoid alterations of airway tone from forced vital capacity maneuvers that may in turn influence measured airway FeNO.4 Written informed parent consent and participant assent were then obtained and inhaled bronchodilator treatment was administered. The clinical team directed all patient management and was masked to test results.
Demographic information was recorded, and asthma severity variables determined for each participant included expiratory-phase prolongation, air entry, wheezing, accessory muscle use, and SpO2 on room air. These variables were used to electronically calculate the Acute Asthma Intensity Research Score (AAIRS, see Table E1 in the Online Repository), a validated bedside severity score.5
We measured the primary explanatory variable, FeNO, using a Niox MINO (Aerocrine, Solna, Sweden) hand-held analyzer. Visual and auditory feedback from the device assisted the participants in maintaining a steady exhalation. The device provided confirmation of an expiratory maneuver of sufficient quality for valid FeNO output. One validated expiratory measurement was accepted because participants were then asked to perform spirometry prior to receiving expeditious bronchodilator and corticosteroid treatment.
The primary response variable was % predicted FEV1 by spirometry. Spirometry was recorded when a participant was able to perform a minimum of three forced airway maneuvers in accordance with American Thoracic Society quality criteria.6 Secondary outcomes included the AAIRS and participant demographic and asthma characteristics.
To assess for associations of FeNO with % predicted FEV1 and the AAIRS we used separate multivariable regression models adjusted for age, race, sex, body mass index and current use of inhaled albuterol, inhaled CCS and acute oral CCS. FeNO was included as a flexible non87 linear term using restricted cubic spline techniques.7 Statistical analyses were performed using R version 3.0.1 (http://www.r-project.org).
Between April, 2008 and February 2013, 806 unique participants were enrolled, and 436 (54%) were able to perform FeNO measurement, with FeNO 39 ppb [21, 64] (median [IQR]), AAIRS 5 [2, 8] and % predicted FEV1 51 [36, 73]. Demographic and asthma characteristics are displayed in Table E2 in the Online Repository, and univariate associations in Table 1. Higher FeNO levels were associated with most asthma severity variables and with African-American (45 ppb [26, 75]) compared to Caucasian race (32 ppb [16, 54], P=0.001 (Table I).
Table I.
Univariate Associations of FeNO with demographic and asthma characteristics amongst 436 participants ages 5 – 17 years with acute asthma exacerbations
| Patient Characteristic | Median [IQR] FeNO (ppb) |
P value |
|---|---|---|
|
| ||
| Demographic Variables | ||
| Gender | ||
| Female (n=175) | 36 [19, 62] | 0.36 |
| Male (n=261) | 42 [22, 64] | |
| Race | ||
| African-American (n=244) | 45 [26, 75] | <0.001 |
| White (n=191) | 32 [16, 54] | |
| Smoke exposure in primary residence | ||
| Yes (n=173) | 41 [20, 65] | 0.73 |
| No (n=263) | 38 [21, 62] | |
| Upper respiratory symptoms | ||
| Yes (n=156) | 36 [20, 56] | 0.21 |
| No (n=280) | 41 [21, 68] | |
| Season of emergency department visit (n) | ||
| Sept – Nov (n = 138) | 41 [20, 74] | 0.08 |
| Dec – Feb (n = 94) | 32 [16, 52] | |
| Mar – May (n = 113) | 39 [23, 64] | |
| Jun – Aug (n = 91) | 42 [24, 64] | |
| Asthma Severity Variables | ||
| Current Medication Use | ||
| Inhaled corticosteroid | 0.14 | |
| Yes (n=181) | 36 [20, 59] | |
| No (n=255) | 41 [22, 66] | |
| Acute course of systemic CCS | ||
| Yes (n=104) | 32 [16, 62] | 0.071 |
| No (n=332) | 41 [23, 65] | |
| Chronic use of systemic CCS | ||
| Yes (n=17) | 35 [19, 47] | 0.31 |
| No (n=418) | 40 [21, 64] | |
| Leukotriene receptor antagonists | ||
| Yes (n=128) | 36 [19,58] | 0.16 |
| No (n=308) | 40 [22,66] | |
| Expiratory Phase | ||
| Normal (n=235) | 32 [16, 56] | <0.001 |
| Prolonged (n=189) | 47 [28, 69] | |
| Severely prolonged (n=12) | 56 [44, 100] | |
| Air Entry | ||
| Normal (n=202) | 30 [16, 57] | <0.001 |
| Decreased (n=222) | 46 [25, 68] | |
| Severely decreased (n=12) | 51 [46, 83] | |
| Wheeze | <0.001 | |
| None (n=112) | 24 [12, 47] | |
| Expiratory (n=142) | 35 [22, 64] | |
| Inspiratory and expiratory (n=182) | 49 [30, 70] | |
| Sternocleidomastoid Retractions | ||
| Yes (n=192) | 48 [30, 73] | <0.001 |
| No (n=244) | 32 [17, 55] | |
| Intercostal Retractions | ||
| Yes (n=42) | 48 [29, 76] | 0.088 |
| No (n=394) | 39 [20, 63] | |
| Subcostal Retractions | ||
| Yes (n=48) | 50 [34, 79] | 0.008 |
| No (n=388) | 36 [20,62] | |
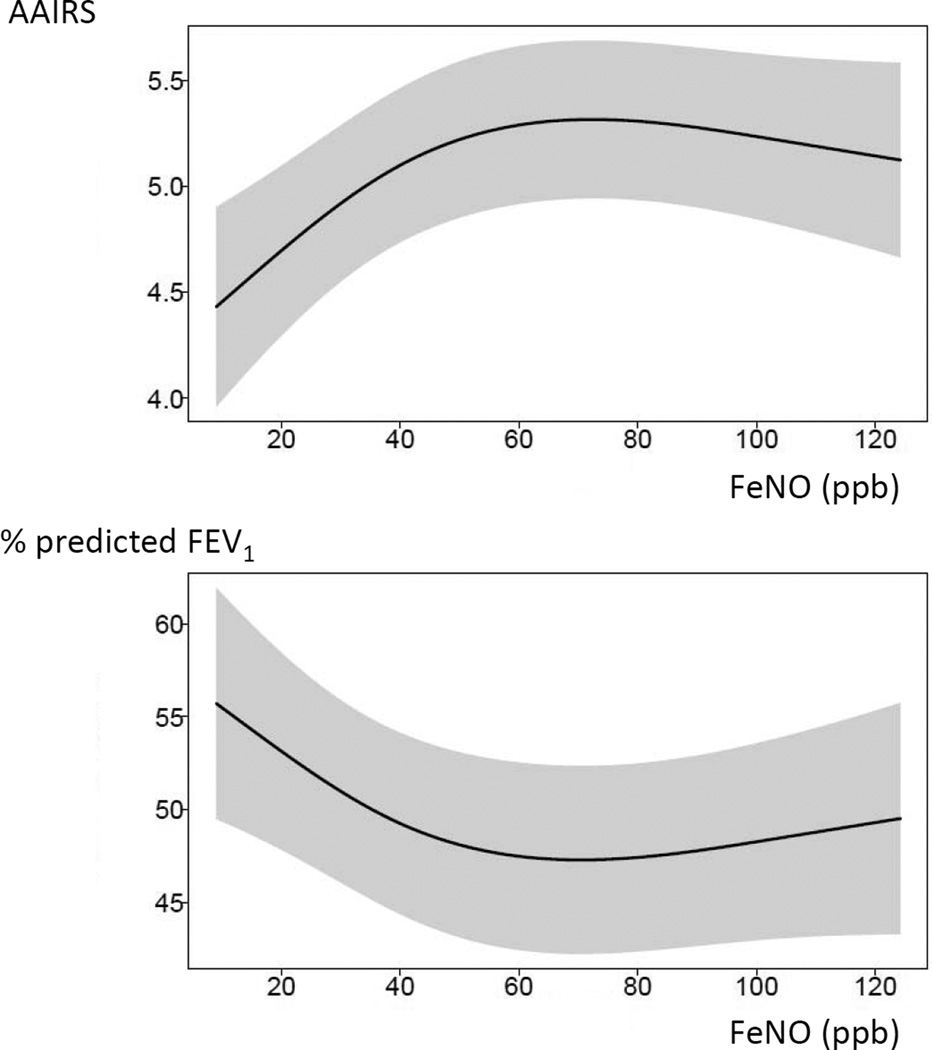
In the primary multivariable regression model FeNO was associated with % predicted FEV1 (P < 0.018), after adjustment for the covariates listed above. The plot derived from this model is presented in Figure 1 and depicts a smooth adjusted association. A 43 ppb increase of FeNO (25th to 75th percentile or 21 to 64 ppb) was associated with increased % predicted FEV1 (β-coefficient −5.5%; 95% CI −1.7, −9.4). This association appeared curvilinear, leveling off at ~65 ppb (the 75%ile) and above. FeNO was also associated with the AAIRS (P < 0.001), although the change of AAIRS was not clinically meaningful (β-coefficient 0.58; 95% CI 0.30., 0.87). In a multivariable model with FeNO as the response variable, there was an association of African-American race with FeNO after adjustment for baseline AAIRS, age, sex, body mass index, second-hand smoke exposure and current use of inhaled albuterol, inhaled CCS, acute or chronic oral CCS and leukotriene antagonist (β-coefficient 13.0; 95% CI 6.1, 19.9).
Figure 1.
Association between fractional excretion of nitric oxide (FeNO, x-axis) with the acute asthma intensity research score (AAIRS, upper panel) and with %-predicted forced expiratory volume in 1-second (% predicted FEV1, lower panel). The plots depict a smooth adjusted association derived from multivariable regression models that included the covariates, age, sex, BMI, asthma severity score, albuterol and inhaled and oral corticosteroid use.
Our results suggest that FeNO measured before treatment in children with acute asthma exacerbations is associated with % predicted FEV1. To our knowledge, a positive correlation between FeNO and % predicted FEV1 during pediatric acute asthma exacerbations has not been previously reported. At levels of FeNO above approximately 65 ppb (75% ile) this association appears to level off. This may indicate that further increases in eosinophilic airway inflammation have a minimal association with lung function measured using % predicted FEV1. Further study is needed to determine whether serial measurement of FeNO predicts an impending acute exacerbation or makes possible interventions to prevent this progression.
We also found that African-American children have significantly higher FeNO levels during acute asthma exacerbations than Caucasian children. Although a racial difference in baseline FeNO levels have been previously reported, to our knowledge this is the first report of a difference during acute exacerbations.8, 9 Further study examining these differences during and after treatment of acute exacerbations according to race may help individualize treatment plans.
Our study has limitations. We obtained a single FeNO measurement for each participant, a decision made due to the short period of time available for study measurements and the need for emergent therapeutic intervention. Although this may limit test reproducibility, the FeNO analyzer provides confirmation of an expiratory maneuver of sufficient quality for valid FeNO output. Second, the study was conducted at a single center, and this may limit external validity. Third, in addition to upper respiratory tract infection and second-hand smoke exposure there are other variables that affect FeNO levels that could confound our results, such as recent food intake, fever, allergic rhinitis, exercise, and other underlying diseases. Lastly, although we did obtain FeNO measurements prior to any treatment administered in the emergency department, many participants were already using albuterol, inhaled corticosteroid, and leukotriene antagonists at baseline or as acute therapy. However, we adjusted for these variables in multivariable analyses.
In summary, we found associations of FeNO with % predicted FEV1 and with African- American race. Knowledge of these associations might inform the use of FeNO before and during acute asthma exacerbations in children, a population in which there are limited objective measures of severity available at the bedside.
Supplementary Material
Clinical Implications.
FeNO is associated with acute pediatric asthma exacerbation severity as measured by % predicted FEV1 and is greater in African-American patients in this population. Knowledge of these associations might inform the use of FeNO before and during acute asthma exacerbations in children.
Acknowledgments
Sources of funding
This research was supported by the National Institutes of Health [Grant K23 HL80005] (Dr. Arnold), NIAID [K24 AI77930] (Dr. Hartert) and NCRR [UL1 RR024975] (Vanderbilt CTSA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nelson KA, Lee P, Trinkaus K, Strunk RC. Exhaled nitric oxide levels during treatment of pediatric acute asthma exacerbations and association with the need for hospitalization. Pediatr Emerg Care. 2011;27:249–255. doi: 10.1097/PEC.0b013e318212a4fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kwok MY, Walsh-Kelly CM, Gorelick MH. The role of exhaled nitric oxide in evaluation of acute asthma in a pediatric emergency department. Acad Emerg Med. 2009;16:21–28. doi: 10.1111/j.1553-2712.2008.00304.x. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel Report 3 (EPR-3): Guidelines for the Diagnosis and Management of Asthma-Summary Report 2007. J Allergy Clin Immunol. 2007;120:S94–S138. doi: 10.1016/j.jaci.2007.09.043. [DOI] [PubMed] [Google Scholar]
- 4.Arnold DH, Gebretsadik T, Abramo TJ, Sheller JR, Resha DJ, Hartert TV. The Acute Asthma Severity Assessment Protocol (AASAP) study: objectives and methods of a study to develop an acute asthma clinical prediction rule. Emerg Med J. 2012;29:444–450. doi: 10.1136/emj.2010.110957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold DH, Saville BR, Wang W, Hartert TV. Performance of the Acute Asthma Intensity Research Score (AAIRS) for acute asthma research protocols. Ann Allergy Asthma Immunol. 2012;109:78–79. doi: 10.1016/j.anai.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am. Rev. Respir. Dis. 1991;144:1202–1218. doi: 10.1164/ajrccm/144.5.1202. [DOI] [PubMed] [Google Scholar]
- 7.Harrell F. Regression modeling strategies : with applications to linear models, logistic regression, and survival analysis. New York: Springer; 2001. [Google Scholar]
- 8.Kovesi T, Kulka R, Dales R. Exhaled nitric oxide concentration is affected by age, height, and race in healthy 9- to 12-year-old children*. CHEST Journal. 2008;133:169–175. doi: 10.1378/chest.07-1177. [DOI] [PubMed] [Google Scholar]
- 9.Linn W, Rappaport E, Berhane K, Bastain T, Avol E, Gilliland F. Exhaled nitric oxide in a population-based study of Southern California Schoolchildren. Respiratory Research. 2009;10:28. doi: 10.1186/1465-9921-10-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.