Abstract
The 5-year risk of death following onset of heart failure (HF) is about 50%. While previous studies have shown beneficial effects of light-to-moderate alcohol consumption and risk of cardiovascular diseases and mortality, it is unclear whether moderate alcohol consumption is associated with a lower risk of death in HF subjects. We investigated whether alcohol consumption and type of alcohol preference are associated with risk of total mortality in 449 US male physicians with prevalent HF. Alcohol consumption was assessed via food frequency questionnaire, and mortality was ascertained via annual follow up questionnaires and adjudicated by an Endpoint Committee. The mean age of subjects was 75.7 ± 8.2 years with an average follow up of 7 years. We found evidence of a J-shaped relation between alcohol consumption and mortality [HR (95% CI): 1.00 (ref), 0.85 (0.61–1.20), 0.60 (0.40–0.88), and 0.71 (0.42–1.21), for alcohol intake of none, <1/day, 1–2/day, and 3+/day respectively (p for quadratic trend: 0.058)]. There was no relation between beverage preference (beer, wine, or liquor) and mortality. In conclusion, our data showed a J-shaped association between alcohol intake and mortality in patients with HF.
Keywords: heart failure, alcohol, mortality, epidemiology
Introduction
The lifetime risk of developing heart failure (HF) at 40 years of age is estimated to be 1 in 5.1 Although survival after HF has improved over time, approximately 50% of individuals with a HF diagnosis will die within 5 years.2,3 A variety of healthy lifestyle factors, including moderate alcohol intake, are related to a lower risk of HF.4–8 In addition, it has been shown that moderate alcohol intake is associated with lower mortality.8,9 Limited data exist on the relation of alcohol intake and mortality among people with HF. In addition, little is known about the relation of alcoholic beverage preference (beer, liquor, or wine) with mortality in HF subjects. A recent European study showed a 29% increase in long-term mortality with moderate alcohol intake in older participants with previously diagnosed HF.10 However, this study only included wine drinkers and only evaluated ≤250 ml/day of alcohol intake.10 Thus, in the current study we examined whether alcohol consumption and type of alcoholic beverage consumed are associated with mortality in US male physicians with prevalent HF.
Methods
The present study used data from the Physicians’ Health Study (PHS) I and II. A detailed description of PHS studies has been previously published.11,12 Briefly, the PHS I was a completed, randomized, double-blind, placebo-controlled trial designed to study low-dose aspirin and beta-carotene for the primary prevention of cardiovascular disease and cancer in US male physicians that began in 1982 and ended in 1995. The PHS II recruited 7000 new physicians and re-enrolled 7641 members of the PHS I between 1997 and 2001. All members of the PHS I who were still alive have been prospectively followed with annual questionnaires, upon trial completion. All physicians who completed the food frequency questionnaire (FFQ) between 1999 and 2001, and had a HF diagnosis prior to the FFQ were eligible to be included in the analysis (n=449). Each participant gave written informed consent, and the institutional review board at Brigham and Women’s hospital approved the study protocol.
Information about alcohol consumption was self-reported using a food frequency questionnaire administered between 1999 and 2001. Participants were asked to provide their average use for each of beer (1 glass, bottle, can), wine (4 oz. glass), and liquor (e.g. whiskey, gin, etc, 1 drink or shot). Possible response categories were “never or less than once per month,” “1–3/month,” “1/week,” “2–4/week,” “5–6/week,” “1/day,” “2–3/day, “4–5/day,” and “6+/day.” Response categories were converted to median number of drinks for beer, wine, and liquor per day and added together. Total alcohol consumption was characterized as none, <1 drink per day, 1–2 drinks per day, and 3+ drinks per day.
Alcoholic preference was classified as consuming no alcohol if a participant indicated “never or less than once per month” for all three alcoholic beverage types. A participant was classified as preferring beer, wine, or liquor if more than 50% of average consumption was from a single source. If a participant consumed less than 50% of total alcohol from either beer, wine, or liquor, then the participant was classified as having no preference.
Incidence of death and morbidities, including HF, was determined with the use of annual follow-up questionnaires. Specifically, a questionnaire was mailed to each participant to obtain information on the occurrence of new medical diagnoses. When participants died, death certificates were obtained for confirmation and review of cause of death. Additional information was obtained from the participants’ next of kin and from medical records. A detailed description of HF validation in the PHS by using a review of medical records in a subsample has been published elsewhere.5,6,13 Demographic and lifestyle information were self-reported at baseline. Diet information was obtained via FFQ.
We used Cox proportional hazards analysis to calculate the multivariable adjusted hazard ratios (HRs) and corresponding 95% confidence intervals (CIs). Proportional hazards assumption was tested by including an interaction with logarithmic person-time in the model. Person time was measured from return of food frequency questionnaire until death or date with last available participant information. We initially assessed confounding by age (<65, 65–<70, 70–<75, 75–<80, 80+), race (white vs. non-white), body mass index (continuous), smoking (never, past, or current), exercise (never, 1–2 days per week, 3–7 days per week), and prevalent atrial fibrillation (yes/no). We then considered coronary heart disease (yes/no), diabetes (yes/no), and hypertension (yes/no) as potential mediators and did not adjust for them in the multivariable model. We obtained p for linear and quadratic trend by creating a new variable that was assigned median alcohol intake in each category and fitted that new variable and its quadratic term in the regression. For beverage preference analyses, we created indicator variables and use non-drinkers as reference group. Analysis was completed using SAS version 9.3 (SAS Institute, Cary, North Carolina). All p values were 2-tailed, and the significance level was set at an alpha of 0.05.
Results
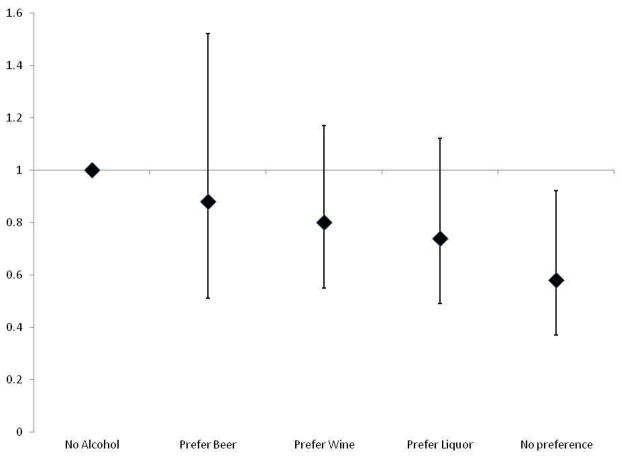
The characteristics at baseline of the 449 HF cases in the PHS are presented in Table 1 according to alcohol consumption. The mean age of participants was 75.7 ± 8.2 years (range, 50.6–97.0). During an average follow-up of 7 years, 206 deaths occurred. The crude incidence rates of mortality were 82.7, 61.1, 55.1, and 61.5 deaths per 1,000 person-years for alcohol consumption of none, <1, 1–2, and 3+ drinks per day, respectively. In a multivariable adjusted Cox regression, there was a J-shaped association between alcohol intake and risk of mortality with HRs (95% CI) of 1.00 (ref), 0.85 (0.61–1.20), 0.60 (0.40–0.88), and 0.71 (0.42–1.21), for alcohol intake of none, <1 drink/day, 1 to 2 drinks/day, and 3+ drinks/day respectively (p for quadratic trend: 0.058), Table 2. Adding potential mediators (prevalent hypertension, coronary heart disease, and diabetes) to the model did not attenuate the associations. In secondary analysis, we did not find evidence for an effect of beverage preference on mortality: compared to non-drinkers in multivariable adjusted models, hazard ratio (95% CI) for mortality was 0.88 (0.51–1.53) for beer preference, 0.82 (0.56–1.20) for wine preference, and 0.73 (0.49–1.11) for liquor preference. Individuals without a beverage preference had a 43% lower risk of mortality compared to non-drinkers (95% CI: 10% to 64%), Figure 1.
Table 1.
Characteristics of the 449 US male physicians according to alcohol consumption
| Characteristics | Frequency of Alcohol Intake | |||
|---|---|---|---|---|
|
| ||||
| Never (n=136) | <1/day (n=159) | 1–2/day (n=103) | >2/day (n=51) | |
| Age (years) | 76.6 ± 8.5 | 74.3 ± 8.5 | 76.8 ± 7.5 | 75.4 ± 7.8 |
| Body Mass Index (kg/m2) | 25.2 ± 4.1 | 26.8 ± 3.9 | 26.0 ± 3.8 | 26.3 ± 3.9 |
| White | 130 (96%) | 147 (92%) | 101 (98%) | 49 (96%) |
| Cigarette Use | ||||
| Never | 72 (53%) | 54 (34%) | 31 (30%) | 9 (18%) |
| Past | 57 (42%) | 98 (62%) | 68 (66%) | 39 (77%) |
| Current | 7 (5%) | 7 (4%) | 4 (4%) | 3 (6%) |
| Exercise Frequency | ||||
| None | 66 (50%) | 80 (50%) | 43 (42%) | 22 (45%) |
| 1–2 days/week | 11 (8%) | 16 (10%) | 15 (15%) | 7 (14%) |
| 3+ days/week | 56 (42%) | 63 (40%) | 44 (43%) | 20 (41%) |
| Atrial Fibrillation | 58 (43%) | 78 (49%) | 50 (49%) | 30 (59%) |
| Hypertension | 93 (68%) | 112 (70%) | 75 (73%) | 34 (67%) |
| Diabetes Mellitus | 39 (29%) | 40 (25%) | 26 (25%) | 11 (22%) |
| Coronary Heart Disease | 78 (57%) | 93 (58%) | 62 (60%) | 26 (51%) |
Data presented as means ± standard deviation or number (percentage).
Table 2.
Incidence rate and hazard ratios (95% CI) of mortality according to frequency of alcohol consumption
| Hazard ratios (95% CI)
|
||||
|---|---|---|---|---|
| Frequency of alcoholic drinks per day | Cases/Person-time | Crude Incidence Rate (per 1000 person-years) | Age Adjusted | Model 11 |
| None | 72/870.7 | 82.69 | 1.00 | 1.00 |
| <1 | 70/1145.2 | 61.13 | 0.84 (0.60–1.17) | 0.85 (0.61–1.20) |
| 1–2 | 43/780.0 | 55.13 | 0.61 (0.42–0.89) | 0.60 (0.40–0.88) |
| >2 | 21/341.5 | 61.50 | 0.77 (0.47–1.26) | 0.71 (0.42–1.21) |
| p for linear trend | 0.110 | 0.069 | ||
| p for quadratic trend | 0.046 | 0.058 | ||
Adjusted for age (<65, 65–<70, 70–<75, 75–<80, 80+), BMI (continuous), smoking (never, past, current), exercise (none, 1–2 days/week, 3+ days/week), race (white/non-white
Figure 1.
Hazard Ratios (95% CI) for mortality according to alcohol preference in 451 male physicians with prevalent heart failure1
1. Adjusted for age (<65, 65–<70, 70–<75, 75–<80, 80+), BMI (continuous), smoking (never, past, current), exercise (none, 1–2 days/week, 3+ days/week), race (white/non-white), and prevalent atrial fibrillation (yes/no)
Discussion
In this prospective study of male physicians with prevalent HF, we found a J-shaped association between alcohol intake and risk of death. Type of alcoholic beverage consumed did not influence such relation.
Few studies have examined total alcohol consumption and alcohol preference in HF subjects and the risk of death.10 Gargiulo and colleagues examined the effects of moderate wine consumption on risk of death in a cohort of elderly individuals from southern Italy. Moderate alcohol consumption was defined as <250 ml/day, which is approximately 2 glasses per day. In the absence of HF, alcohol consumption was associated with a 21% lower risk of death (95% CI: 5%–34%). But, in the presence of HF, there was a 29% (95% CI: 5%–97%) higher risk of death when compared to non-drinkers.10 Although our study was comparable to the Italian study with respect to age of participants and length of follow-up, several differences might explain the inconsistency of the findings. In Gargiulo et al., 62% of participants were women contrasted with 100% men in our cohort; women tend to have diastolic HF (better prognosis) whereas men are prone to systolic HF.14 Additionally, incident mortality was higher in the European study (86.5% for moderate drinkers in Gargiulo et al vs. 43.1% in our study); suggesting that participants may have been sicker at baseline, and long-term alcohol consumption for these individuals may be harmful. Finally, cultural differences and lifestyle habits including diet and smoking rates between Europe and the United States, could partially account for the difference observed between the 2 studies.15
Moderate drinking may confer protection against death via its effect on high-density lipoprotein cholesterol, improving insulin sensitivity and plasma adiponectin, endothelial function, and inhibiting inflammation.16–20 Whether wine, beer, and liquor have differential associations with mortality is not well established. Few studies suggest that resveratrol and other substances in red grape skin may confer additional health benefits over ethanol.21–23 However, our findings do not provide evidence of a differential effect of various types of alcoholic beverages on mortality in subjects with HF.
Our study had several limitations. Due to the observational design of the current study, we cannot exclude residual or unmeasured confounding as partial explanation of observed results. Alcohol consumption could have been misclassified due to self-reports and was only assessed at baseline in most of the study subjects. We did not collect data to distinguish HF with and without preserved left ventricular systolic function. Due to the small sample size, our study has limited statistical power to detect small differences in mortality risk across alcohol groups. Finally, our findings may not be generalizable to other populations and women because we studied male and mostly white physicians who may have had different behaviors than the general population. However, the ability to control for residual confounding through collected covariates, the prospective design of the PHS, and the high confirmation rate of both self-reported HF and deaths are major strengths of this report.
Acknowledgments
Funding: This study was supported by grant R21HL088081 from the NHLBI. The PHS is supported by grants CA-34944, CA-40360, CA-097193, HL-26490, and HL-34595 from the NIH, Bethesda, MD
We are indebted to the participants of the PHS for their outstanding commitment and cooperation and to the entire PHS staff for their expert and unfailing assistance
Footnotes
Financial disclosures: Dr. Djousse is currently serving as PI on an investigator-initiated research funded by GlaxoSmithKline and the California Walnut Commission. He received travel reimbursement from the Wine in Moderation ASBL. No other relations to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lloyd-Jones DM, Larson MG, Leip EP, Beiser A, D’Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJS, Levy D. Lifetime risk for developing congestive heart failure: The Framingham heart study. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 2.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2014 update: A report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, Jacobsen SJ. Trends in heart failure incidence and survival in a community-based population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 4.Walsh CR, Larson MG, Evans JC, Djousse L, Ellison RC, Vasan RS, Levy D. Alcohol consumption and risk for congestive heart failure in the Framingham Heart Study. Ann Intern Med. 2002;136:181–191. doi: 10.7326/0003-4819-136-3-200202050-00005. [DOI] [PubMed] [Google Scholar]
- 5.Djousse L, Gaziano JM. Alcohol consumption and risk of heart failure in the Physicians’ Health Study I. Circulation. 2007;115:34–39. doi: 10.1161/CIRCULATIONAHA.106.661868. [DOI] [PubMed] [Google Scholar]
- 6.Djousse L, Driver JA, Gaziano MJ. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryson CL, Mukamal KJ, Mittleman MA, Fried LP, Hirsch CH, Kitzman DW, Siscovick DS. The association of alcohol consumption and incident heart failure: The Cardiovascular Health Study. J Am Coll Cardiol. 2006;48:305–311. doi: 10.1016/j.jacc.2006.02.066. [DOI] [PubMed] [Google Scholar]
- 8.Kloner RA, Rezkalla SH. To drink or not to drink? that is the question. Circulation. 2007;116:1306–1317. doi: 10.1161/CIRCULATIONAHA.106.678375. [DOI] [PubMed] [Google Scholar]
- 9.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 10.Gargiulo G, Testa G, Cacciatore F, Mazzella F, Galizia G, Della-Morte D, Langellotto A, Pirozzi G, Ferro G, Ferrara N. Moderate alcohol consumption predicts long-term mortality in elderly subjects with chronic heart failure. J Nutr Health Aging. 2012:1–6. doi: 10.1007/s12603-012-0430-4. [DOI] [PubMed] [Google Scholar]
- 11.Final report on the aspirin component of the ongoing physicians’ health study. Steering committee of the physicians’ health study research group. N Engl J Med. 1989;321:129–135. doi: 10.1056/NEJM198907203210301. [DOI] [PubMed] [Google Scholar]
- 12.Christen WG, Gaziano JM, Hennekens CH. Design of Physicians’ Health Study II—a randomized trial of beta-carotene, vitamins E and C, and multivitamins, in prevention of cancer, cardiovascular disease, and eye disease, and review of results of completed trials. Ann Epidemiol. 2000;10:125–134. doi: 10.1016/s1047-2797(99)00042-3. [DOI] [PubMed] [Google Scholar]
- 13.Ho KK, Anderson KM, Kannel WB, Grossman WL, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993;88:107–115. doi: 10.1161/01.cir.88.1.107. [DOI] [PubMed] [Google Scholar]
- 14.Kannel WB. Epidemiology and prevention of cardiac failure: Framingham study insights. Eur Heart J. 1987;8 (Suppl F):23–26. doi: 10.1093/eurheartj/8.suppl_f.23. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. 2012 global progress report on implementation of the WHO Framework Convention on Tobacco Control. World Health Organization; 2012. [Google Scholar]
- 16.Gaziano JM, Buring JE, Breslow JL, Goldhaber SZ, Rosner B, VanDenburgh M, Willett W, Hennekens CH. Moderate alcohol intake, increased levels of high-density lipoprotein and its subfractions, and decreased risk of myocardial infarction. N Engl J Med. 1993;329:1829–1834. doi: 10.1056/NEJM199312163292501. [DOI] [PubMed] [Google Scholar]
- 17.Greenfield JR, Samaras K, Hayward CS, Chisholm DJ, Campbell LV. Beneficial postprandial effect of a small amount of alcohol on diabetes and cardiovascular risk factors: Modification by insulin resistance. J Clin Endocrinol Metab. 2005;90:661–672. doi: 10.1210/jc.2004-1511. [DOI] [PubMed] [Google Scholar]
- 18.Hendriks HF. Moderate alcohol consumption and insulin sensitivity: Observations and possible mechanisms. Ann Epidemiol. 2007;17:S40–S42. [Google Scholar]
- 19.Beulens JW, van Loon LJ, Kok FJ, Pelsers M, Bobbert T, Spranger J, Helander A, Hendriks HF. The effect of moderate alcohol consumption on adiponectin oligomers and muscle oxidative capacity: A human intervention study. Diabetologia. 2007;50:1388–1392. doi: 10.1007/s00125-007-0699-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Imhof A, Woodward M, Doering A, Helbecque N, Loewel H, Amouyel P, Lowe G, Koenig W. Overall alcohol intake, beer, wine, and systemic markers of inflammation in western europe: Results from three MONICA samples (Augsburg, Glasgow, Lille) Eur Heart J. 2004;25:2092–2100. doi: 10.1016/j.ehj.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 21.Wang H, Yang Y, Qian H, Zhang Q, Xu H, Li J. Resveratrol in cardiovascular disease: What is known from current research? Heart Fail Rev. 2012;17:437–448. doi: 10.1007/s10741-011-9260-4. [DOI] [PubMed] [Google Scholar]
- 22.Das M, Das DK. Resveratrol and cardiovascular health. Mol Aspects Med. 2010;31:503–512. doi: 10.1016/j.mam.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Wu JM, Hsieh T. Resveratrol: A cardioprotective substance. Ann N Y Acad Sci. 2011;1215:16–21. doi: 10.1111/j.1749-6632.2010.05854.x. [DOI] [PubMed] [Google Scholar]