To the Editor
Genjiro Kimura,1 an emeritus professor at our university, proposed that impaired renal capacity for sodium excretion is caused by a diminished glomerular ultrafiltration coefficient (KF) and/or enhanced fractional reabsorption of sodium (FRNa), and may result in elevation of the sodium sensitivity of blood pressure (BP). We believe that sodium retention occurs during the day in patients with impaired renal sodium excretion, and that this prevents the nocturnal BP dip, resulting in the promotion of pressure natriuresis (i.e. non-dipper type of circadian BP rhythm).2,3
A recent article4 in the Journal of the Renin Angiotensin Aldosterone System showing attenuation of the transtubular potassium concentration gradient (TTKG) during angiotensin receptor blocker (ARB) treatment supported our thesis that ARBs can increase daytime natriuresis (UNaV).5 In turn, this produces a lower steady state sodium balance6 and can restore the circadian BP rhythm, similarly to diuretics, during the chronic phase (8 weeks) of treatment (Figure 1).
Figure 1.
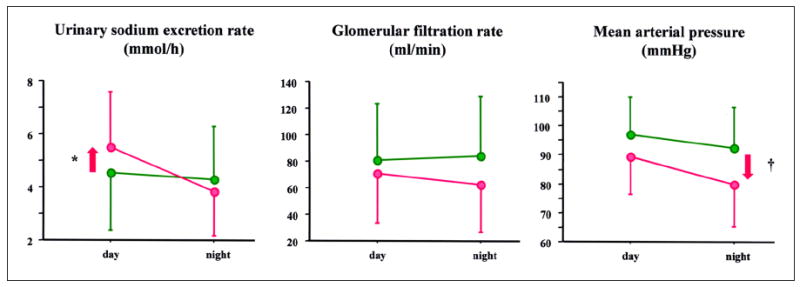
Day–night values of urinary sodium excretion rate, glomerular filtration, and mean arterial pressure at baseline (green) and in the acute phase of treatment with an angiotensin receptor blocker (red). (original source of the figure: Tables 1 and 2 from Fukuda et al.6). If restoration of non-dipper circadian blood pressure rhythm is attributed to the natriuretic effect of ARB, daytime natriuresis proceeded or occurred in the absence of lowering of night-time blood pressure.
The natriuretic effects of ARBs have been shown in experimental models.7-9 Inhibition of FRNa (defined as tubular sodium reabsorption per filtered amount of sodium) in the upper tubules (e.g. proximal tubules or loop of Henle) should lead to a downstream increase in FRNa caused by the tubuloglomerular feedback (TGF) system and epithelial sodium channel (ENaC). However, ARB can resist these sodium-retaining mechanisms. ARBs can alter the TGF responsiveness to promote greater excretion of sodium into urine.10 ARBs can also decrease the ENaC number11 and activity12 independent of circulating aldosterone, although the total reabsorptive capacity of the collecting tubules is limited. Attenuation of the TTKG by ARB treatment indicates decreased ENaC action in patients with chronic kidney disease (CKD).4
A direct correlation between FRNa and proximal tubular angiotensinogen (PT-AGT) expression, which reflects the intrarenal activity of the renin–angiotensin system (RAS), has been shown in patients with IgA nephropathy.13 Concomitant treatment with ARBs largely blocked the increase in PT-AGT in angiotensin II-infused hypertensive rats.14 This supports our hypothesis that ARBs can inhibit FRNa stimulated by inappropriate activation of the intrarenal RAS, and thus restore circadian rhythm.
For these reasons, we believe that ARBs can increase the daytime UNaV to restore non-dipper circadian BP rhythm. The increase in daytime UNaV during treatment with ARBs can be explained by two possible ARB-mediated mechanisms: inhibition of FRNa, similarly to the action of diuretics mentioned above; and lowering of the night-time BP resulting in attenuation of night-time UNaV, and thus leading to a compensatory increase in daytime UNaV. Therefore, we examined whether an increase in daytime UNaV (Figure 1, *) or a decrease in night-time BP (Figure 1, †) occurs first within 2 days after the start (acute phase) of oral administration of olmesartan (20 mg/day) once in the morning in CKD patients with hypertension and proteinuria. The patients were six men and two women with a median (interquartile ranges) of age, office BP, estimated glomerular filtration rate, and proteinuria of 56 (44–68) years old, 147/82 (145–153/75–87) mmHg, 56 (19–76) ml/min/1.73m2, and 1320 (950–2190) mg/gCre, respectively. All patients provided informed consent. The study was approved by the institutional review board of Nagoya City University Hospital and conducted in accordance with the Declaration of Helsinki.
At baseline, three of the eight patients had dipper circadian BP rhythm and five had non-dipper BP rhythm. The three dippers at baseline exhibited an increase in daytime UNaV within 2 days after starting ARB treatment. One of the five non-dippers showed an increase in UNaV on the first day of treatment and the rhythm was restored to a dipper pattern on the same day. The other four non-dippers at baseline had no change in this status in the first 2 days of treatment. However, all four patients had an increase in daytime UNaV within 2 days after starting treatment (1 day for three patients; 2 days for one patient), even though circadian BP rhythm was not restored (Table 1).
Table 1.
Changes in the circadian blood pressure rhythm and daytime natriuresis in an acute phase of the treatment with ARB.
| Age, gender | Baseline
|
ARB
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| eGFR | Office BP | Proteinuria | Circadian BP rhythm | Circadian BP rhythm | Increase in daytime UNaV | ||||
| 1 | 32y, M | 106 | 131/69 | 1001 | Dipper | Remained dipper | Day 1 | ||
| 2 | 53y, M | 70 | 172/100 | 1504 | Dipper | Remained dipper | Day 2 | ||
| 3 | 58y, M | 89 | 143/83 | 1138 | Dipper | Remained dipper | Day 2 | ||
| 4 | 74y, F | 42 | 146/61 | 807 | Non-dipper | Restored into dipper at Day 1 | Day 1 | ||
| 5 | 33y, M | 71 | 148/93 | 712 | Non-dipper | Remained non-dipper | Day 1 | ||
| 6 | 47y, F | 21 | 147/86 | 2680 | Non-dipper | Remained non-dipper | Day 1 | ||
| 7 | 82y, M | 11 | 161/76 | 2022 | Non-dipper | Remained non-dipper | Day 1 | ||
| 8 | 66y, M | 10 | 151/80 | 6565 | Non-dipper | Remained non-dipper | Day 2 | ||
Baseline office BP and proteinuria were measured at the three different visits, and two consecutive seated BP reading were measured after at least 5 minutes rest on each visit. eGFR: estimated glomerular filtration rate (ml/min/1.73m2); UNaV: urinary sodium excretion rate (mmol/h).
The participants were different from our previous study Fukuda et al.6
These findings indicate that the increase in daytime UNaV is not attributable to BP reduction during the previous night. Rather, the increase in daytime UNaV can restore the circadian BP rhythm. We postulate that diuretics suppress most of the FRNa at their action site, whereas ARBs suppress inappropriate enhancement of FRNa stimulated by intrarenal RAS. This suggestion is based on the much larger natriuretic effect exerted by ARBs in patients with a more severe non-dipper BP rhythm before treatment in our clinical study.5 The sympathetic nerve system can also stimulate the tubular sodium reabsorption, whereas ARBs were reported to inhibit the central and peripheral sympathetic nerve activity.15 Therefore, further study is needed to investigate whether ARBs can restore the non-dipper BP rhythm in patients with activated intrarenal RAS or in other patients with particular conditions.
Acknowledgments
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of Interest
None declared.
References
- 1.Kimura G, Brenner BM. The renal basis for salt sensitivity in hypertension. In: Laragh JH, Brenner BM, editors. Hypertension: Pathophysiology, Diagnosis and Management. 2. New York: Raven; 1995. pp. 1569–1588. [Google Scholar]
- 2.Fukuda M, Munemura M, Usami T, et al. Nocturnal blood pressure is elevated with natriuresis and proteinuria as renal function deteriorates in nephropathy. Kidney Int. 2004;65:621–625. doi: 10.1111/j.1523-1755.2004.00419.x. [DOI] [PubMed] [Google Scholar]
- 3.Fukuda M, Mizuno M, Yamanaka T, et al. Patients with renal dysfunction require a longer duration until blood pressure dips during the night. Hypertension. 2008;52:1155–1160. doi: 10.1161/HYPERTENSIONAHA.108.115329. [DOI] [PubMed] [Google Scholar]
- 4.Ogiyama Y, Miura T, Watanabe S, et al. Circadian rhythm of urinary potassium excretion during treatment with an angiotensin receptor blocker. J Renin Angiotensin Aldosterone Syst. 2013 Feb 6; doi: 10.1177/1470320313475909. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 5.Fukuda M, Yamanaka T, Mizuno M, et al. Angiotensin II type 1 receptor blocker, olmesartan, restores nocturnal blood pressure decline by enhancing daytime natriuresis. J Hypertens. 2008;26:583–588. doi: 10.1097/HJH.0b013e3282f2fded. [DOI] [PubMed] [Google Scholar]
- 6.Fukuda M, Wakamatsu-Yamanaka T, Mizuno M, et al. Angiotensin receptor blockers shift the circadian rhythm of blood pressure by suppressing tubular sodium reabsorption. Am J Physiol Renal Physiol. 2011;301:F953–F957. doi: 10.1152/ajprenal.00167.2011. [DOI] [PubMed] [Google Scholar]
- 7.Barreto-Chaves ML, Mello-Aires M. Effect of luminal angiotensin II and ANP on early and late cortical distal tubule HCO3- reabsorption. Am J Physiol. 1996;271:F977–F984. doi: 10.1152/ajprenal.1996.271.5.F977. [DOI] [PubMed] [Google Scholar]
- 8.Lerolle N, Bourgeois S, Leviel F, et al. Angiotensin II inhibits NaCl absorption in the rat medullary thick ascending limb. Am J Physiol Renal Physiol. 2004;287:F404–F410. doi: 10.1152/ajprenal.00265.2003. [DOI] [PubMed] [Google Scholar]
- 9.Quan A, Baum M. Endogenous production of angiotensin II modulates rat proximal tubule transport. J Clin Invest. 1996;97:2878–2882. doi: 10.1172/JCI118745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Braam B, Mitchell KD, Koomans HA, et al. Relevance of the tubuloglomerular feedback mechanism in pathophysiology. J Am Soc Nephrol. 1993;4:1257–1274. doi: 10.1681/ASN.V461257. [DOI] [PubMed] [Google Scholar]
- 11.Beutler KT, Masilamani S, Turban S, et al. Long-term regulation of ENaC expression in kidney by angiotensin II. Hypertension. 2003;41:1143–1150. doi: 10.1161/01.HYP.0000066129.12106.E2. [DOI] [PubMed] [Google Scholar]
- 12.Peti-Peterdi J, Warnock DG, Bell PD. Angiotensin II directly stimulates ENaC activity in the cortical collecting duct via AT(1) receptors. J Am Soc Nephrol. 2002;13:1131–1135. doi: 10.1097/01.asn.0000013292.78621.fd. [DOI] [PubMed] [Google Scholar]
- 13.Fukuda M, Urushihara M, Wakamatsu T, et al. Proximal tubular angiotensinogen in renal biopsy suggests nondipper BP rhythm accompanied by enhanced tubular sodium reabsorption. J Hypertens. 2012;30:1453–1459. doi: 10.1097/HJH.0b013e328353e807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kobori H, Prieto-Carrasquero MC, Ozawa Y, et al. AT1 receptor mediated augmentation of intrarenal angiotensinogen in angiotensin II-dependent hypertension. Hypertension. 2004;43:1126–1132. doi: 10.1161/01.HYP.0000122875.91100.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ye S, Zhong H, Duong VN, et al. Losartan reduces central and peripheral sympathetic nerve activity in a rat model of neurogenic hypertension. Hypertension. 2002;39:1101–1106. doi: 10.1161/01.hyp.0000018590.26853.c7. [DOI] [PubMed] [Google Scholar]


