Synopsis
The Chicago Classification defines esophageal motility disorders in high resolution manometry using Clouse plots. This is based on individual scoring of 10 swallows performed in supine position. The update version of the Chicago Classification, named Chicago Classification v3.0, has many new revisions that will improve and simplify the current version. Disorders of EGJ outflow obstruction are defined by a median integrated relaxation pressure (IRP) above the limit of normal and further divided into 3 achalasia subtypes and EGJ outflow obstruction. In case of 100% failed contractions, achalasia should be considered if there is a borderline IRP or evidence of panesophageal pressurization. Major motility disorders (aperistalsis, distal esophageal spasm, and hypercontractile or jackhammer esophagus) are patterns not encountered in controls in the context of normal EGJ relaxation. Compared to the previous version of the Chicago Classification, failed contraction corresponds to a contraction with a distal contractile integral (DCI) below 100 mmHg-s-cm, as opposed to an isobaric contour plot definition. At least 2 hypercontractile swallows (DCI > 8,000 mmHg-s-cm) are required for the diagnosis of jackhammer esophagus in the Chicago Classification v3.0. Finally with the latest version of the Chicago Classification, only two minor motor disorders are now considered. Ineffective esophageal motility (IEM) is defined as at least 50% of swallows with a DCI below 450 mmHg-s-cm. Fragmented peristalsis is defined as at least 50% of fragmented swallows (that are contractions with DCI>450 mmHg-s-cm and break > 5 cm in the 20-mmHg isobaric contour) not meeting IEM criteria.
Keywords: Esophageal high resolution manometry, achalasia, esophago-gastric junction outflow obstruction, aperistalsis, distal esophageal spasm, hypercontractile esophagus, ineffective esophageal motility
Introduction
High resolution manometry (HRM) is the current gold standard technique to assess esophageal motility. It utilizes closely spaced pressure sensors to create a dynamic representation of pressure change along the entire length of the esophagus. Data acquisition is easier than with conventional manometry and interpretation is facilitated by esophageal pressure topography (Clouse) plots1.
Along with the technological innovation, an international consensus process has evolved over recent years to define esophageal motility disorders using HRM, Clouse plots, and standardized metrics. This classification, titled The Chicago Classification, was firstly published in 20092 and subsequently updated in 20123. It was intended to be applied to HRM studies performed in supine position with 5-ml water swallows and for patients without previous esophagogastric surgery. The 2012 version of the Chicago Classification focused entirely on redefining esophageal motor disorders associated with dysphagia in HRM terms; it did not provide guidance on the assessment of the esophago-gastric junction (EGJ) at rest or upper esophageal sphincter (UES) function. Since that publication, substantial further research has been presented and published aimed at improving the diagnostic accuracy and clinical utility of The Chicago Classification. In recognition of this, the international HRM Working Group met in Chicago in May 2014 in conjunction with Digestive Disease Week to discuss these new data in the context of working toward an update of the Chicago Classification (v3.0). This review will present a brief summary of these discussions and proposals to work toward the Chicago Classification 3.0; a process due to be completed in early 2015.
Metrics and swallow pattern characterization
The Chicago Classification is based on scoring of ten 5-ml water swallows performed in supine position. EGJ relaxation, esophageal contractile activity and esophageal pressurization are evaluated for each swallow. However, a major indication for manometric studies is in the evaluation of patients for potential antireflux surgery and some description of EGJ morphology and quantification of contractility is desirable. Hence, the incorporation of simple metrics relevant to these aspects of motility will be incorporated into Chicago Classification v3.0. Proposed metrics under discussion include mean inspiratory pressure, mean expiratory pressure, the extent and variability of the separation between the lower esophageal sphincter and crural diaphragm (LES-CD separation), and the EGJ contractile integral (EGJ-CI), all of which have been used in publications. However, discrepancies exist in the details of calculation methodology for these metrics, the strength of data supporting their utility, and their normative ranges among HRM devices4–11, all important limitations meriting further consideration.
Esophagogastric junction morphology and deglutitive relaxation
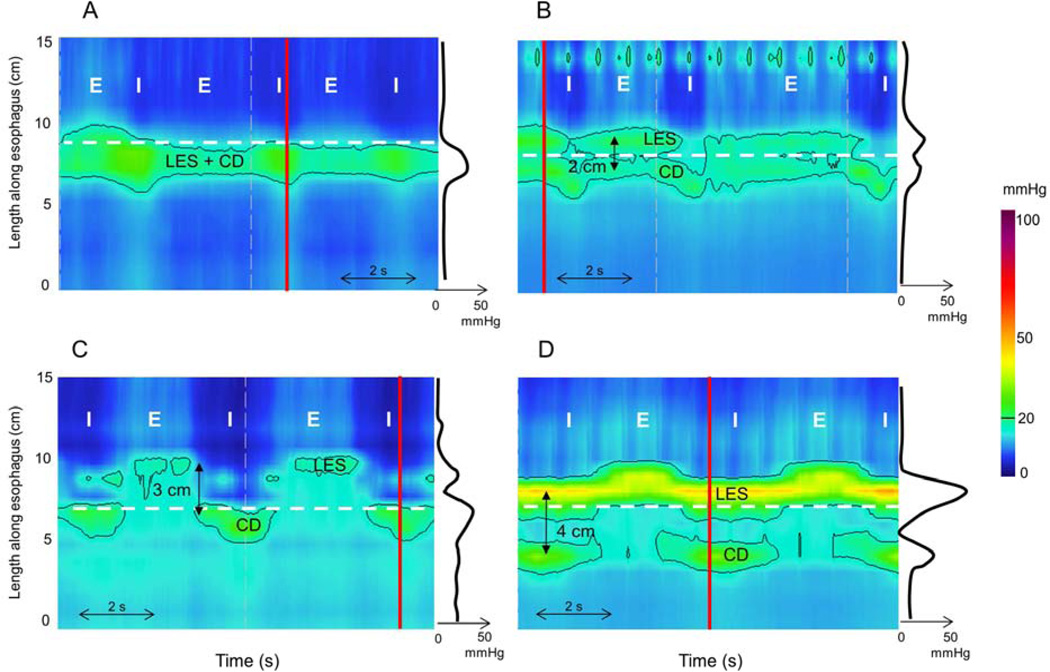
With HRM and Clouse plots, the relative localization of the 2 constituents of the EGJ, the lower esophageal sphincter (LES) and the crural diaphragm (CD), define EGJ morphologic subtypes12. This is a fundamental feature or EGJ morphology, likely pertinent to its functional integrity. With type I EGJ morphology, there is complete overlap of the CD and LES with no spatial separation evident on the Clouse plot (Figure 1) and no double peak on the associated spatial pressure variation plot. With type II EGJ morphology, the LES and CD are separated (double-peaked spatial pressure variation plot), but the nadir pressure between the two peaks does not decline to gastric pressure; the separation between the pressure peaks is less than 3 cm. With type III EGJ morphology, the LES and CD are clearly separated as evidenced by a double peaked spatial pressure variation plot and the nadir pressure between the peaks equal to or less than gastric pressure; with type IIIa the pressure inversion point remains at the CD level, while in type IIIb it is located at the LES level. However, it is important to note that the separation between LES and CD may fluctuate in the course of the study and in those instances this should be reported as a range13. Hence in reporting the LES-CD, the range of observed LES-CD separation observed throughout the study is reported for types II and III EGJ morphology.
Figure 1.
Esophago-gastric junction (EGJ) morphology subtypes. For each panel the instantaneous spatial pressure variation plot corresponding to the red line on the pressure topography plot is illustrated by the red line on the right. The two main EGJ components are the lower esophageal sphincter (LES) and the crural diaphragm (CD), which cannot be independently quantified when they are superimposed as with a type I EGJ (Panel A). The respiratory inversion point (RIP), shown by the horizontal dashed line, lies at the proximal margin of the EGJ. During inspiration (I) EGJ pressure increases whereas it decreases during expiration (E). Type II EGJ pressure morphology is illustrated in Panel B. Note the 2 peaks on the instantaneous spatial pressure variation plot; the nadir pressure between the peaks is greater than the intra gastric pressure. Panels C and D correspond to type III EGJ pressure morphology defined as the presence of 2 peaks of the instantaneous spatial pressure variation plot with a nadir pressure between the peaks equal to or less than intragastric pressure. The RIP is proximal to the CD with type IIIa (Panel C) whereas it is proximal to the LES in IIIb (Panel D).
The simplest measurement of baseline EGJ pressure is an average pressure for 3 normal respiratory cycles, ideally in a quiescent portion of the recording, remote from either spontaneous or test swallows in order to exclude the effect of the post-deglutitive contraction. The inspiratory EGJ pressure is the mean maximal inspiratory EGJ pressure and the expiratory EGJ pressure is the average EGJ pressure midway between inspirations. Normative values are reported in Table 1.
Table 1.
Reported normal ranges of basal EGJ pressures for control subjects in a supine position among studies and among manometric devices.
| Author | Equipment | Number of controls |
End expiratory EGJ pressure (mmHg) |
|---|---|---|---|
| Pandolfino2 | Given | 75 | Mean (±2 SD) =18 (4–33) |
| Sweis9 | Given | 23 | Median (5th–95th percentile) 19 (5–38) |
| Niebisch8 | Given | 68 | Median (5th–95th percentile) 15 (3–31) |
| Weijenborg10 | Given | 50 | Median (5th–95th percentile) 15 (3–31) |
| Bogte4 | MMS -Solid state (Unisensor AG) | 52 | Median (5th–95th percentile) 31 (9–51) |
| Kessing7 | MMS – Water perfused system | 50 | Median (5th–95th percentile) 10 (3–30) |
During swallowing, EGJ relaxation is evaluated using the integrated relaxation pressure (IRP). This has been and will continue to be defined as the mean of the 4s (contiguous or non-contiguous) of maximal deglutitive relaxation in the 10s window beginning at deglutitive UES relaxation. The IRP is referenced to gastric pressure. Normal values are, however, strongly dependent on the specific manometric hardware utilized making this an important diagnostic consideration (Table 2).
Table 2.
Reported normal ranges of integrated relaxation pressure (IRP) for control subjects in a supine position among studies and among manometric devices. Upper limit of normal (UNL).
Deglutitive peristaltic vigor and pattern
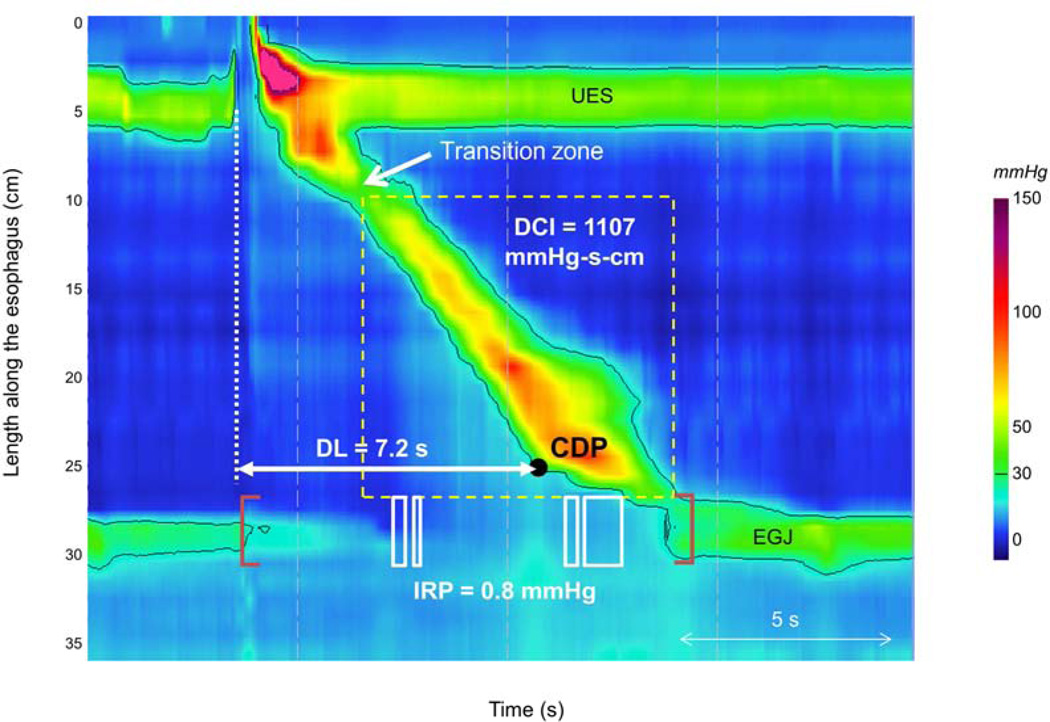
Metrics are used to evaluate esophageal contractile function are the distal esophageal integral (DCI) and the distal latency (DL) (Figure 2 and Table 3). They are used to characterize each of the ten 5-ml test swallows (Table 4). Contractile vigor is summarized using the distal DCI. This metric applies an algorithm to quantify the contractile pressure exceeding 20 mmHg for the region spanning from the transition zone to the proximal aspect of the EGJ. As such, it encompasses the space-time domain of the 2nd and 3rd contractile segments defined by Clouse and provides a single number summarizing contractile vigor in this region. Cut off values between diagnostic categories are somewhat dependent on the manometric hardware and software utilized (Table 3). A DCI between 450 and 8,000 mmHg-s-cm is considered normal. Based on the conclusions of a study on ineffective contractile contraction14, the International HRM Working Group is inclined to define failed and weak contraction based on the DCI value in the Chicago Classification v3.0. The current proposal is that a contraction with a DCI <100 mmHg-s-cm defines a failed contraction and a weak contraction is defined as a DCI >100 but <450 mmHg-s-cm. Both failed and weak contractions are ineffective. Finally, a DCI ≥8,000 mmHg-s-cm defines hypercontractility15.
Figure 2.
Normal esophageal peristaltic contraction. The integrated relaxation pressure (IRP) is measured during the deglutitive window indicated by the brown bracket. The IRP is the lowest pressure for 4 s (contiguous or non-contiguous) identified by the white boxes within the deglutitive window. The distal contractile integral (DCI) is measured from the transition zone to the EGJ, equating to the product of the amplitude × duration × length of the contraction located within the dashed box. The contractile deceleration point (CDP, black dot) represents the inflexion point in the velocity of contractile front propagation. Distal latency (DL) is measured from upper esophageal sphincter (UES) relaxation (dashed vertical line) to the CDP.
Table 3.
Reported normal ranges of distal contractile integral (DCI) and distal latency (DL) for control subjects in a supine position among studies and among manometric devices.
| Author | Equipment | Number of controls |
Median DCI (5–95th percentile) (mmHg-s-cm) |
Median DL (5th percentile) (s) |
|---|---|---|---|---|
| Xiao11 | Given | 75 | 1612 (448–4721) | 5.8 (4.3) |
| Niebisch8 | Given | 68 | 1485 (420–4236) | 6.8 (5.4) |
| Weijenborg10 | Given | 50 | 834 (178–2828) | 6.8 (5.4) |
| Bogte4 | MMS -Solid state (Unisensor AG) | 52 | 1008 (186–3407) | 6.1 (5.0) |
| Kessing7 | MMS – Water perfused system | 50 | 970 (142–3675) | 7.4 (6.2) |
Table 4.
Characteristics of deglutitive peristaltic function proposed for the Chicago Classification v3.0 (note that contraction pattern is not scored with failed or weak vigor)
| Contractile Vigor | |
| Failed | DCI <100 mmHg-s-cm |
| Weak | DCI >100 mmHg-s-cm, but <450 mmHg-s-cm |
| Ineffective | Failed or Weak |
| Normal | DCI >450 mmHg-s-cm but <8,000 mmHg-s-cm |
| Hypercontractile | DCI ≥8,000 mmHg-s-cm |
| Contraction Pattern | |
| Premature | DL <4.5 s |
| Fragmented | Large break (>5 cm) in the 20 mmHg isobaric contour, but not failed and DCI >450 mmHg-s-cm |
| Intact | Not achieving the above diagnostic criteria |
| Intrabolus Pressure Pattern (30 mmHg isobaric contour referenced to atmospheric) | |
| Panesophageal pressurization | Uniform pressurization of >30 mmHg extending from the UES to the EGJ |
| Compartmentalized esophageal pressurization | Pressurization of >30 mmHg extending from the contractile front to the EGJ |
| EGJ Pressurization | Pressurization restricted to zone between the LES and CD in conjunction with LES-CD separation |
| Normal | No bolus pressurization >30 mmHg |
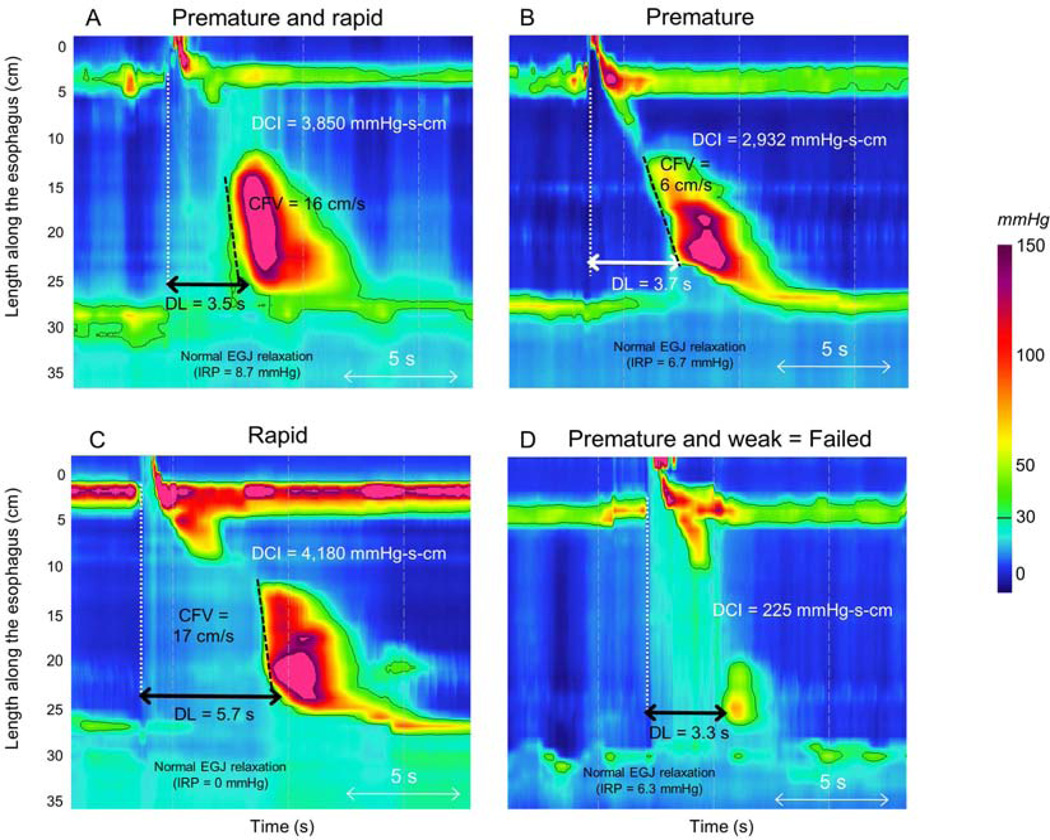
The contractile deceleration point (CDP) is a key landmark in the assessment of the contraction pattern. It represents the inflexion point in the contractile front propagation velocity on the 30-mmHg isobaric contour in the distal esophagus16. After the CDP, propagation velocity slows signifying the termination of peristalsis and the onset of ampullary emptying; this is usually located 2–3 cm proximal to the EGJ17. The distal latency (DL) corresponds to the period of deglutitive inhibition that precedes esophageal contraction at the CDP and it is measured as the interval from UES relaxation to the CDP18. A value less than 4.5 s is considered abnormal and defines a premature contraction. However, if the contraction is weak (DCI < 450 mmHg-s-cm) with a DL <4.5 s, it may be considered a failed contraction as this contraction is most likely ineffective (Figure 4D).
Figure 4.
Premature contraction is defined as a distal latency (DL) <4.5 s (Panels A and B); in conjunction with normal EGJ relaxation they are the defining features of distal esophageal spasm. The contractile front velocity (CFV) of a premature contraction might be elevated (>9 cm/s) (Panel A) or normal (Panel B). The clinical significance of rapid contraction with normal DL (Panel C) remains to be determined. A weak contraction (DCI <450 mmHg-s-cm) with a reduced distal latency is considered failed (Panel D).
The contractile front velocity (CFV) is estimated by determining the slope of the tangent skirting the 30-mmHg isobaric contour from the transition zone to the CDP. Although this metric of velocity has historical relevance, it has been removed from the Chicago Classification v3.0 due to its lack of specificity to define esophageal spasm and the unknown clinical relevance of rapid contraction with normal distal latency.
Peristaltic integrity is defined by gaps in the 20-mmHg isobaric contour of the peristaltic contraction between the UES and EGJ. Although no longer utilized in defining weak peristalsis, peristaltic integrity is still proposed as an important morphologic characteristic of peristalsis in Chicago Classification v3.0 (Figure 3D). While the 2012 classification distinguished small (2–5 cm in length) and large (> 5cm) breaks as subtypes of weak peristalsis, the Working Group proposes that small breaks be considered normal and that only breaks >5 cm in length be scored. Additionally, the nomenclature has changed to distinguish between contractions with breaks and weak contractions as a large break can be encountered in the context of a normal or even high DCI. Thus, a contraction with a normal or elevated DCI and a large break will be classified as a “fragmented” contraction according to the Chicago Classification v3.0.
Figure 3.
Contractile vigor is assessed using the distal contractile integral (DCI). A contraction with a DCI <100 mmHg-s-cm is failed (Panel A). A contraction with a DCI >100 but <450 mmHg-s-cm is weak (Panel B). Both are ineffective swallows. A hypercontractile swallow is defined as a DCI >8,000 mmHg-s-cm (Panel C). Finally a contraction with a normal DCI (450–8,000 mmHg-s-cm) and a break >5 cm is a fragmented contraction (Panel D).
Intrabolus pressure pattern
The pattern of intra-bolus pressure continues to be an important part of the updated classification scheme. Intrabolus pressure is characterized for each swallow using the 30-mmHg isobaric contour and abnormal pressurization corresponds to regions of esophageal pressurization to >30 mmHg. Intrabolus pressure is qualified as panesophageal if it spans from the EGJ to the UES and as compartmentalized if it extends from the deglutitive contractile front to the EGJ. Finally pressurization restricted to zone between the LES and CD in conjunction with hiatal hernia is called EGJ pressurization.
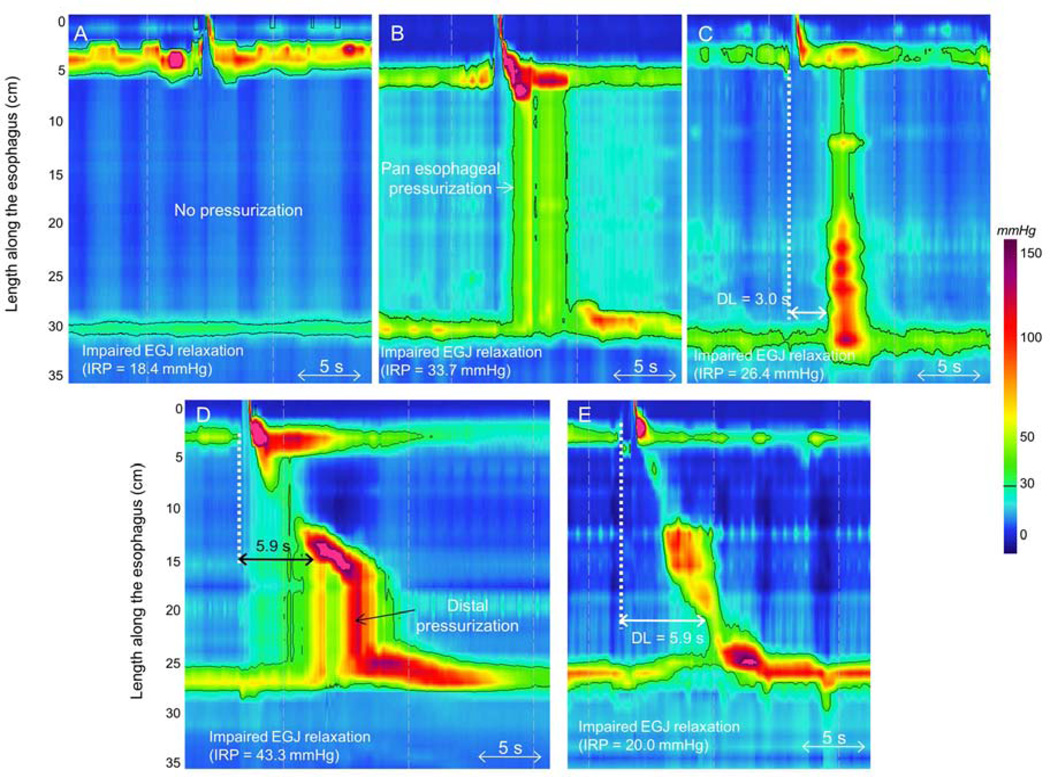
Disorders with EGJ outflow obstruction
The most fundamental assessment of deglutitive contractility in the Chicago Classification is of whether or not an EGJ outflow obstruction is present as defined by the IRP. Disorders of EGJ outflow obstruction are further subdivided into achalasia subtypes and EGJ outflow obstruction based on the contractile and pressurization patterns in the body of the esophagus (Figure 5). Three clinically relevant subtypes of achalasia have been defined in the previous iteration of the Chicago classification19. Type I achalasia was characterized by 100% failed contractions and no esophageal pressurization; type II achalasia was defined as 100% failed contraction and panesophageal pressurization for at least 20% of swallows; and type III achalasia was defined as the presence of preserved fragments of distal peristalsis or premature contractions for at least 20% of the swallows in the 2012 Chicago Classification.
Figure 5.
Disorders associated with EGJ outflow obstruction. Impaired EGJ relaxation is evident by an integrated relaxation pressure (IRP) >15 mmHg. In type I achalasia; there is no esophageal contraction and no esophageal pressurization (Panel A). Type II achalasia is characterized by panesophageal pressurization and absence of a peristaltic contraction (Panel B). In type III achalasia, there are at least 20% premature contraction, defined as DL <4.5 s. (Panel C). EGJ outflow obstruction may represent a variant of achalasia (Panel D). It might also be the consequence of a mechanical obstruction (Panel E) such as a distal esophageal stenosis in a context of esophagitis.
The international HRM working group had several suggestions to improve and clarify these definitions in the Chicago Classification v3.0. First of all, the Working Group proposed that it would be more relevant to base the evaluation of EGJ relaxation on the median rather than the mean IRP of 10 swallows in order to minimize the effect of occasional outliers that occur for a variety of reasons. Secondly, using a regression tree model, it has been recently shown that the critical IRP threshold may vary among achalasia subtypes20. Specifically, in type I achalasia, IRP threshold might be reduced to a cut-off value as low as 10 mmHg to more accurately distinguish is from aperistalsis. Third, the occurrence of panesophageal pressurization for at least 20% of swallows in conjunction with 100% failed contractions would diagnose type II achalasia regardless of the IRP value. Fourth, it was acknowledged that the critical IRP cutoff varied among manometric devices (Table 2). However, in order to simplify the use of the Chicago Classification v3.0 in clinical practice, the current thinking of the HRM Working Group is that it would be better to keep the same IRP threshold for all achalasia subtypes, but leave some flexibility in interpretation when certain combinations of contractility are observed. For instance, due to the relevance of this regression tree model analysis, the HRM Working Group suggested to add a qualifier to the diagnosis of aperistalsis (see below, major peristaltic disorders): in instances of 100% failed contractions, a diagnosis of achalasia should be considered if there is a borderline median IRP value or if there is evidence of esophageal pressurization.
Another pertinent observation made relevant to contractile features defining type III achalasia is that after pneumatic dilation or, more commonly, Heller myotomy, instances of peristalsis can be observed that they were not observed prior to treatment21. This led to the hypothesis that esophageal pressurization might have hidden some instances of peristalsis in the pre-treatment studies. Hence, the Working Group had proposed that in Chicago Classification v3.0, the definition of Type III achalasia should be restricted to premature contractions. Finally, EGJ outflow obstruction is characterized by an elevated median IRP associated with evidence of esophageal contractility that is inconsistent with type I, II, or III achalasia.
Major motility disorders
Major motility disorders are defined as patterns of motor function that are not encountered in controls in the context of normal EGJ relaxation. The Working group strongly supported the continued to use this criterion but, in some case, slightly modified the criteria for defining the major motility disorders. (Table 5)
Table 5.
Esophageal motility diagnoses and criteria proposed for the Chicago Classification v3.0
| DISORDERS with EGJ OUTFLOW OBSTRUCTION | CRITERIA |
|---|---|
| Type I achalasia (classic achalasia) | Elevated median IRP (>15 mmHg†), 100% failed peristalsis (DCI <100 mmHg) Premature contractions with DCI values less than 450 mmHg-s-cm meet criteria for failed peristalsis |
| Type II achalasia (with esophageal compression) | Elevated median IRP (>15 mmHg†), 100% failed peristalsis, panesophageal pressurization with ≥20% of swallows Contractions may be masked by esophageal pressurization and DCI should not be calculated |
| Type III achalasia (spastic achalasia) | Elevated median IRP (>15 mmHg†), no normal peristalsis, premature (spastic) contractions with DCI >450 mmHg-s-cm with ≥20% of swallows May be mixed with panesophageal pressurization |
| EGJ outflow obstruction | Elevated median IRP (>15 mmHg†), sufficient evidence of peristalsis such that criteria for types I-III achalasia not met* |
| MAJOR DISORDERS of PERISTALSIS | (Not encountered in normal subjects) |
| Aperistalsis | Normal median IRP, 100% failed peristalsis Should consider achalasia with borderline IRP values when there is evidence of esophageal pressurization Premature contractions with DCI values less than 450 mmHg-s-cm meet criteria for failed peristalsis |
| Distal esophageal spasm | Normal median IRP, ≥20% premature contractions with DCI >450 mmHg-s-cm†. Some normal peristalsis may be present. |
| Hypercontractile esophagus (jackhammer) | At least two swallows with DCI >8,000 mmHg-s-cm†§ Hypercontractility may be localized to the LES and may be missed using DCI criteria |
| MINOR DISORDERS OF PERISTALSIS | (Characterized by vigor, pattern, and MRS response) |
| Ineffective esophageal motility (IEM) | >50% ineffective swallows Ineffective swallows can be failed or weak Multiple repetitive swallow assessment may be helpful in determining peristaltic reserve |
| Fragmented peristalsis | >50% fragmented contractions not meeting IEM criteria |
| NORMAL ESOPHAGEAL MOTILITY | Not fulfilling any of the above classifications |
Cutoff value dependent on the manometric hardware; this is the cutoff for the Given system
Potential etiologies: early achalasia, mechanical obstruction, esophageal wall stiffness, or manifestation of hiatal hernia in which case it can be subtyped to CD or LES
Hypercontractile esophagus can be a manifestation of outflow obstruction as evident b instances in which it occurs in association with an IRP greater than the upper limit of normal
Aperistalsis
Aperistalsis (previously called absent peristalsis) is defined by the combination of a normal IRP and 100% failed contractions. As mentioned previously, premature contractions with DCI <100 mmHg-s-cm meet the criteria for failed peristalsis. Moreover, based on the CART analysis, type I achalasia should be considered in cases of borderline IRP20 and esophageal pressurization should also alert one to the possibility of achalasia. The definition of “borderline IRP” in this context ranges from 10–15 mmHg with the Given system.
Distal esophageal spasm
Premature contractions, defined as having a DL <4.5s have been shown to be more specific than rapid contractions (defined as a contractile front velocity >9 cm/s) for the diagnosis of distal esophageal spasm18. In fact, the working group concluded that rapid contractions were so nonspecific that they should not be considered a significant abnormality. Consequently it is now proposed that distal esophageal spasm be defined by the occurrence of ≥20% premature contractions in a context of normal EGJ relaxation.
Jackhammer esophagus
The definition of hypercontractile esophagus (nicknamed jackhammer esophagus) was based on the occurrence of at least one swallow with a DCI greater than 8,000 mmHg-s-cm in the 2012 Chicago Classification15. However, it has become apparent that this disorder is heterogeneous and might occur in the context of other esophageal abnormalities, such as EGJ outflow obstruction, gastro-esophageal reflux disease (GERD), or eosinophilic esophagitis. Furthermore, with one Working Group member’s observation of an 8,000 mmHg-s-cm DCI occurring in a control subject, the threshold of one swallow meeting that criterion was deemed insufficient and of uncertain relevance. Hence, the international HRM Working Group proposed to define jackhammer esophagus as the occurrence of ≥20% of swallows with a DCI >8,000 mmHg-s-cm. Another caveat that has come to light is that hypercontractility extended to the LES might be missed using strict DCI criteria. Hence, in some instances, such as that illustrated in Figure 6, expanding the DCI measurement to include the EGJ may be warranted.
Figure 6.
Normal esophageal contraction followed by a prominent contraction of the lower esophageal sphincter. Including the EGJ in the DCI measurement (white dashed box) may result in the diagnosis of hypercontractility.
Minor motility disorders
The clinical significance of minor motility disorders continues to be actively debated. It was the strong feeling of the Working Group that “overly classifying” these was somewhat counter-productive as it distracted attention from the importance of identifying the major disorders. Hence, in order to improve this situation, it has been proposed to define minor motility disorders based on the contractile vigor, contractile pattern and the response to multiple rapid swallows in the Chicago Classification v3.0.
Peristaltic abnormalities as defined in the 2012 Chicago Classification
The 2012 Chicago Classification listed 5 “peristaltic abnormalities.”
Weak peristalsis with large peristaltic defects was defined by a normal IRP and >20% swallows with large breaks in the 20 mmHg isobaric contour (>5 cm in length).
Weak peristalsis with small peristaltic defects corresponded to normal IRP and >30% swallows with small breaks in the 20 mmHg isobaric contour (2–5 cm in length).
Frequent failed peristalsis was defined by >30% but <100% of swallows with failed peristalsis.
Rapid contractions with normal latency corresponded to rapid contractions (CFV>9 cm/s and DL>4.5s) with 20% of swallows.
Hypertensive peristalsis was defined as a mean DCI >5,000 mmHg-s-cm, but not meeting criteria for hypercontractile esophagus.
Limitations of the 2012 Chicago Classification
As alluded to above, the 2012 Chicago Classification for “peristaltic abnormalities” just detailed encountered significant dissatisfaction in the clinical community because of its complexity and because of the unclear relevance of the subtypes. For example, small peristaltic defects are common in healthy controls; Kumar et al. observed that breaks reaching or exceeding 20% of the esophageal length in ≥30% of test swallows was encountered in 27% of control subjects22. The relevance of rapid contractions is also debated and unclear. Among 67 patients with at least 20% of rapid contractions with normal latency, Pandolfino et al. showed that this abnormality was associated with EGJ outflow obstruction (n=7, 11%), weak peristalsis (n=41, 61%), hypertensive peristalsis (n=5, 7%) and even normal peristalsis (n=14, 21%)18. A substantial number of controls might also exhibit rapid contractions. Finally, the relevance of hypertensive peristalsis is not widely accepted. Its definition, based on a mean DCI among 10 swallows being >5,000 mmHg-s-cm, was inconsistent with the general scheme of the Chicago Classification that is otherwise based on the individual scoring of swallows. Furthermore, this value has significant overlap with control subjects.
Minor motility disorders proposed for Chicago Classification v3.0
Given the limitations just described, the Working Group has proposed major simplifications to the definitions of minor motility disorders. Thus, all “peristaltic abnormalities” defined in the 2012 Chicago Classification have been abandoned. In their place, Chicago Classification v3.0 will adopt the terminology “ineffective esophageal motility” popularized in conventional manometric diagnoses and “fragmented peristalsis.”
Ineffective esophageal motility
The unifying feature of swallows contributing to the diagnosis of ineffective esophageal motility (IEM) is poor bolus transit in the distal esophagus. Using conventional manometry, IEM was defined by 50% or more ineffective esophageal swallows which were in turn defined as esophageal contractions exhibiting amplitudes <30 mmHg at pressure sensors positioned 3 or 8 cm above the LES23. Correlating conventional line tracing analysis and Clouse plots analysis, Xiao et al. demonstrated that ineffective swallows (IES) on conventional line tracing potentially corresponded to a mixture of intact contractions (that is a contraction without a break in the 20-mmHg isobaric contour), weak contractions with small or large breaks, and failed contractions on Clouse plots24. However, shifting to the criterion of a DCI <450 mmHg-s-cm was optimal in predicting IES (positive percent agreement 83% and negative percent agreement 90% in a validation sample of 100 patients). Thus, it has been proposed to define ineffective swallows on Clouse plots by having a DCI <450 mmHg-s-cm with more than 50% ineffective swallows constituting IEM. No distinction need be made between failed swallows and weak swallows.
Another recent development relevant to the diagnosis of IEM is that multiple rapid swallowing (MRS) has been proposed as a test to evaluate “peristaltic reserve.” MRS consists of administering five 2-ml water swallows separated by 2–3 s intervals, too brief a period to allow significant peristaltic progression. Multiple rapid swallowing results in profound inhibition of the esophageal body and LES and is normally followed by an esophageal contraction of increased amplitude. Using conventional manometry, half of patients with IEM normalized esophageal contraction amplitude after MRS25 a phenomenon referred to as peristaltic reserve. Applying this concept to HRM, the DCI of the contraction that followed MRS was compared to the average DCI of the ten test 5-ml water swallows in controls and in a cohort of GERD patients prior to fundoplication26. The DCI ratio (DCI after MRS/ average DCI of the 10 swallows) was greater than 1 in 78% of controls, 64% of patients without dysphagia after fundoplication, 44% of patients with early dysphagia after fundoplication and 11% of patients with late dysphagia after fundoplication (p<0.02). Further a DCI ratio >0.85 had a sensitivity of 67% and a specificity of 64% in segregating patients with late postoperative dysphagia from those with no postoperative dysphagia. Thus, the DCI ratio might reflect the peristaltic reserve and help predict the occurrence of postoperative dysphagia after antireflux surgery. The international HRM Working Group acknowledged the utility of MRS in patients with IEM to evaluate the peristaltic reserve, but it is as yet uncertain as to how it will be worked into the classification.
Fragmented peristalsis
Even though breaks in the 20-mmHg isobaric contours are frequently encountered in control subjects and patients, large breaks (>5 cm) might well be clinically relevant. Large breaks are significantly more common in patients with dysphagia than in controls (14 vs 4%, p=0.02)27. Porter et al. showed that the proportion of failed or fragmented contractions was greater in patients with GERD than in controls (61.9% vs 33.3%, p≤0.08). Due to the potential clinical relevance of large breaks, the Working Group has proposed to define fragmented peristalsis as ≥50% fragmented contractions with the added stipulation of not meeting IEM criteria.
Normal esophageal motility
Finally normal esophageal motility is considered if criteria for the above motility disorders are not fulfilled.
What is in the future?
The Chicago Classification is an evolving process. Version 3.0 will take into account interval publications since 2012 and the worldwide clinical experience of the experts in the field. Definitions of esophageal dysmotility will be simplified to facilitate their use in daily clinical practice. As with earlier iterations, these changes aim to segregate clinically relevant disorders from ‘statistically abnormal’ motility. In the future, additional findings will likely be incorporated that further improve accuracy and utility. The use of combined impedance-HRM might be helpful to assess pharyngeal motility and upper esophageal sphincter function28 and may also complement the analysis of esophageal function29,30. Performing HRM in alternative conditions such as upright posture9,11 may also be considered as this may improve diagnostic yield. Similarly, swallow challenges introduced into the clinical study such as free drinking31 or a test meal,32 to trigger motility abnormalities may prove to be clinically relevant.
Key points.
The Chicago Classification of esophageal motility disorders is based on a clinical study comprised of 10 test swallows performed in supine posture
Esophageal motility disorders are divided into disorders with EGJ outflow obstruction, major disorders not encountered in normal subjects and minor motility disorders defined by statistical abnormalities
Three subtypes of achalasia are defined that are clinically distinct in terms of responsiveness to therapeutic intervention
Major esophageal motility disorders are aperistalsis, distal esophageal spasm and hypercontractile (jackhammer) esophagus.
Ineffective esophageal motility will likely replace weak peristalsis and frequent peristalsis in version 3.0 of the Chicago Classification
Acknowledgements
This is a preliminary report of the transactions leading to and during the HRM working Group meeting on HRM that transpired in Chicago on May 6–7, 2014. It represents a summary of the meeting as agreed on by the authors, but is still preliminary in that it has not yet gained approval of the broader group.
This work was supported by Grant No R01 DK079902 (JEP) and R01 DK56033 (PJK) from the National Institutes of Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: SR has served as consultant for Given Imaging
References
- 1.Soudagar AS, Sayuk GS, Gyawali CP. Learners favour high resolution oesophageal manometry with better diagnostic accuracy over conventional line tracings. Gut. 2012;61(6):798–803. doi: 10.1136/gutjnl-2011-301145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pandolfino JE, Fox MR, Bredenoord AJ, et al. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol Motil. 2009;21(8):796–806. doi: 10.1111/j.1365-2982.2009.01311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal esophageal pressure topography (EPT) Neurogastroenterol Motil. 2012;24(Suppl 1):57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bogte A, Bredenoord AJ, Oors J, et al. Normal values for esophageal high-resolution manometry. Neurogastroenterol Motil. 2013;25(9):e762–e579. doi: 10.1111/nmo.12167. [DOI] [PubMed] [Google Scholar]
- 5.Ghosh SK, Pandolfino JE, Rice J, et al. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293(4):G878–G885. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 6.Ghosh SK, Pandolfino JE, Zhang Q, et al. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290(5):G988–G997. doi: 10.1152/ajpgi.00510.2005. [DOI] [PubMed] [Google Scholar]
- 7.Kessing BF, Weijenborg PW, Smout AJ, et al. Water-perfused esophageal high-resolution manometry; normal values and validation. Am J Physiol Gastrointest Liver Physiol. 2014 doi: 10.1152/ajpgi.00447.2013. [DOI] [PubMed] [Google Scholar]
- 8.Niebisch S, Wilshire CL, Peters JH. Systematic analysis of esophageal pressure topography in high-resolution manometry of 68 normal volunteers. Dis Esophagus. 2013 doi: 10.1111/dote.12027. [DOI] [PubMed] [Google Scholar]
- 9.Sweis R, Anggiansah A, Wong T, et al. Normative values and inter-observer agreement for liquid and solid bolus swallows in upright and supine positions as assessed by esophageal high-resolution manometry. Neurogastroenterol Motil. 2011;23(6):e509–e198. doi: 10.1111/j.1365-2982.2011.01682.x. [DOI] [PubMed] [Google Scholar]
- 10.Weijenborg PW, Kessing BF, Smout AJ, et al. Normal values for solid-state esophageal high-resolution manometry in a European population; an overview of all current metrics. Neurogastroenterol Motil. 2014 doi: 10.1111/nmo.12314. [DOI] [PubMed] [Google Scholar]
- 11.Xiao Y, Read A, Nicodeme F, et al. The effect of a sitting vs supine posture on normative esophageal pressure topography metrics and Chicago Classification diagnosis of esophageal motility disorders. Neurogastroenterol Motil. 2012;24(10):e509–e516. doi: 10.1111/j.1365-2982.2012.02001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol. 2007;102(5):1056–1063. doi: 10.1111/j.1572-0241.2007.01138.x. [DOI] [PubMed] [Google Scholar]
- 13.Bredenoord AJ, Weusten BL, Timmer R, et al. Intermittent spatial separation of diaphragm and lower esophageal sphincter favors acidic and weakly acidic reflux. Gastroenterology. 2006;130(2):334–340. doi: 10.1053/j.gastro.2005.10.053. [DOI] [PubMed] [Google Scholar]
- 14.Xiao Y, Kahrilas PJ, Nicodeme F, et al. Lack of Correlation Between HRM Metrics and Symptoms During the Manometric Protocol. Am J Gastroenterol. 2014 doi: 10.1038/ajg.2014.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roman S, Pandolfino JE, Chen J, et al. Phenotypes and clinical context of hypercontractility in high resolution pressure topography (EPT) Am J Gastroenterol. 2012;107(1):37–45. doi: 10.1038/ajg.2011.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pandolfino JE, Leslie E, Luger D, et al. The contractile deceleration point: an important physiologic landmark on oesophageal pressure topography. Neurogastroenterol Motil. 2010;22(4):395–400. doi: 10.1111/j.1365-2982.2009.01443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin Z, Pandolfino JE, Xiao Y, et al. Localizing the contractile deceleration point (CDP) in patients with abnormal esophageal pressure topography. Neurogastroenterol Motil. 2012;24(10):972–975. doi: 10.1111/j.1365-2982.2012.01959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pandolfino JE, Roman S, Carlson D, et al. Distal esophageal spasm in high-resolution esophageal pressure topography: defining clinical phenotypes. Gastroenterology. 2011;141(2):469–475. doi: 10.1053/j.gastro.2011.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: A New Clinically Relevant Classification by High-Resolution Manometry. Gastroenterology. 2008;135(5):1526–1533. doi: 10.1053/j.gastro.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin Z, Kahrilas PJ, Roman S, et al. Refining the criterion for an abnormal Integrated Relaxation Pressure in esophageal pressure topography based on the pattern of esophageal contractility using a classification and regression tree model. Neurogastroenterol Motil. 2012;24(8):e356–e363. doi: 10.1111/j.1365-2982.2012.01952.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roman S, Kahrilas PJ, Mion F, et al. Partial recovery of peristalsis after myotomy for achalasia; more the rule than the exception. JAMA Surg. 2013;148(2):157–164. doi: 10.1001/2013.jamasurg.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar N, Porter RF, Chanin JM, et al. Analysis of Intersegmental Trough and Proximal Latency of Smooth Muscle Contraction Using High-Resolution Esophageal Manometry. J Clin Gastroenterol. 2012;46(5):375–381. doi: 10.1097/MCG.0b013e31823d3403. [DOI] [PubMed] [Google Scholar]
- 23.Blonski W, Vela M, Safder A, et al. Revised criterion for diagnosis of ineffective esophageal motility is associated with more frequent dysphagia and greater bolus transit abnormalities. Am J Gastroenterol. 2008;103(3):699–704. doi: 10.1111/j.1572-0241.2007.01593.x. [DOI] [PubMed] [Google Scholar]
- 24.Xiao Y, Kahrilas PJ, Kwasny MJ, et al. High-Resolution Manometry Correlates of Ineffective Esophageal Motility. Am J Gastroenterol. 2012;107(11):1647–1654. doi: 10.1038/ajg.2012.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fornari F, Bravi I, Penagini R, et al. Multiple rapid swallowing: a complementary test during standard oesophageal manometry. Neurogastroenterol Motil. 2009;21(7):e718–e741. doi: 10.1111/j.1365-2982.2009.01273.x. [DOI] [PubMed] [Google Scholar]
- 26.Shaker A, Stoikes N, Drapekin J, et al. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108(11):1706–1712. doi: 10.1038/ajg.2013.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roman S, Lin Z, Kwiatek MA, et al. Weak peristalsis in esophageal pressure topography: classification and association with dysphagia. Am J Gastroenterol. 2011;106(2):349–356. doi: 10.1038/ajg.2010.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Omari TI, Dejaeger E, van Beckevoort D, et al. A method to objectively assess swallow function in adults with suspected aspiration. Gastroenterology. 2011;140(5):1454–1463. doi: 10.1053/j.gastro.2011.02.051. [DOI] [PubMed] [Google Scholar]
- 29.Lin Z, Imam H, Nicodeme F, et al. Flow time through esophagogastric junction derived during high-resolution impedance-manometry studies: a novel parameter for assessing esophageal bolus transit. Am J Physiol Gastrointest Liver Physiol. 2014 doi: 10.1152/ajpgi.00119.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rommel N, Van Oudenhove L, Tack J, et al. Automated impedance manometry analysis as a method to assess esophageal function. Neurogastroenterol Motil. 2014 doi: 10.1111/nmo.12308. [DOI] [PubMed] [Google Scholar]
- 31.Daum C, Sweis R, Kaufman E, et al. Failure to respond to physiologic challenge characterizes esophageal motility in erosive gastro-esophageal reflux disease. Neurogastroenterol Motil. 2011;23(6):e517–e200. doi: 10.1111/j.1365-2982.2011.01669.x. [DOI] [PubMed] [Google Scholar]
- 32.Sweis R, Anggiansah A, Wong T, et al. Assessment of esophageal dysfunction and symptoms during and after a standardized test meal: development and clinical validation of a new methodology utilizing high-resolution manometry. Neurogastroenterol Motil. 2014;26(2):215–228. doi: 10.1111/nmo.12252. [DOI] [PubMed] [Google Scholar]