Abstract
Anthrax is an infectious fatal disease with epidemic potential. Nowadays, bioterrorism using Bacillus anthracis is a real possibility, and thus society needs an effective weapon to neutralize this threat. The pathogen may be easily transmitted to human populations. It is easy to store, transport, and disseminate and may survive for many decades. Recent data strongly support the effectiveness of bacteriophage in treating bacterial diseases. Moreover, it is clear that bacteriophages should be considered a potential incapacitative agent against bioterrorism using bacteria belonging to B. cereus group, especially B. anthracis. Therefore, we have reviewed the possibility of using bacteriophages active against Bacillus anthracis and other species of the B. cereus group in the face of a bioterrorism threat.
1. Introduction
Shortly after the September 11 terrorist attacks using captured planes, letters containing anthrax spores were posted to news media and the US Senate. Five people died and several others survived the disease. This incident proved that bioterrorism using B. anthracis is a real danger and society needs an efficient weapon to neutralize this threat. Experts believe that if such an attack occurred in a large city, hundreds of thousands of people could be at risk of the deadly disease, while the present systems of defense are insufficient.
Anthrax is an infectious disease with high epidemic potential (characterized by high morbidity and mortality, with real possibility of being used in a bioterrorism attack with spores of B. anthracis). The pathogen (especially spores) that is the cause of anthrax may be transmitted in human populations by way of aerosolization (natural or artificial), resulting in epidemics with high mortality [1]. These bacteria are rare in the USA and highly infective and pose a huge threat to public health [2]. There is no strictly defined infectious dose for humans. Its amount may be influenced by such factors as the route of infection (type of anthrax), state of health of the infected person, and virulence of the infecting strain [3]. The disease caused by B. anthracis is treatable with antibiotics (such as penicillin G, amoxicillin, or ciprofloxacin), but the prognosis depends on the time after which the pathogen is identified and the application of appropriate therapy [4].
Anthrax spores are easy to store, transport, and disseminate and may survive in soil for many decades. Due to this feature, Bacillus anthracis is likely to be used as a bioterrorist weapon [5]. Moreover, the bacteria produce dangerous toxins. Antibiotic resistance in bacteria from environmental samples may cause serious problems in treating anthrax. The capsule that can be present in some strains could be dangerous as it inhibits phagocytosis of these bacteria. Moreover, the B. cereus group—which B. anthracis belongs to—consists of very homogeneous bacteria with close relatedness. This feature may pose problems with identification of and differentiation between bacteria belonging to this taxonomy group.
Bacterial viruses, bacteriophages (phages), are natural enemies of bacteria and recent data strongly suggest their effectiveness in treating bacterial diseases including those caused by antibiotic-resistant microbes [6]. Their biology and current applications have been recently summarized in detail [7]. Therefore, it is clear that phages should also be considered a potential tool against bioterrorism using B. anthracis or other B. cereus group bacteria.
2. B. anthracis as a Bioterrorism Tool
2.1. Pathogenesis of B. anthracis and Other B. cereus Group Bacteria
The etiological agent of anthrax, Bacillus anthracis, is a Gram-positive, aerobic or facultatively anaerobic, spore-forming, and rod-shaped bacterium, which appears in cell chains. B. anthracis, B. anthracis, together with four other species (B. cereus sensu stricto, B. thuringiensis, B. mycoides, and B. weihenstephanensis) constitute the Bacillus cereus group [8]. This zoonotic pathogen is mainly present in soil, water, and animals. It infects animals and, occasionally, humans [5, 9]. There is a risk of passive transfer of anthrax from animals to humans through insects [5]. Spores produced in the presence of oxygen [10] are stable and resistant to harsh external conditions like heat, cold, pH, desiccation, and chemicals. They can germinate when exposed to a nutrient-rich environment, such as the tissues or blood of an animal or human host [11]. The climate may directly or indirectly influence the way in which an animal comes into contact with the spores or affect the general state of a host's health and the level of their resistance to infection [5]. There are data [5] regarding the impact of various factors, such as rainfall, temperature, state of the host, and population density, on the epidemiology of anthrax; however, there is no agreement on the roles played by these factors in the incidence of the disease. Unfortunately, there are no hard scientific data to support these theories.
In humans there are three main forms of this disease, cutaneous, gastrointestinal, and inhalational, according to the route of infection [12]. Each of these forms can be lethal. The most dangerous is the inhalation form (it may be induced by 8 × 103–5 × 104 spores). In people untreated, death occurs in 97 to even 100% of cases within 3–5 days, but in people treated already at the early stage of the disease the mortality rate is reduced to 75%. On the other hand, mortality in untreated cutaneous form of anthrax can range from 10 to 20%, and in treated cases it is below 1% [4, 13].
The virulence of anthrax is associated with the production of poly-D-glutamic acid polysaccharide capsule (PDGA) [14, 15]. The cap gene encoded on the pOX2 plasmid is responsible for the synthesis of the capsule. The mechanism of inhibition is not well established [16]. One of the possibilities may be phagosomal escape. Moreover, it is suggested that the capsule may block bactericidal activities of neutrophil cationic peptides, for example, α- and β-defensins. It has been demonstrated that the capsule is poorly immunogenic and evades recognition as an antigen by the immune system because it protects the surface antigens and protects bacterial cells from the circulating antibodies, therefore enabling the spread of bacilli inside the host body [17]. Moreover, B. anthracis strains produce toxins that consist of three peptides: protective antigen (PA), lethal factor (LF), and edema factor (EF). These peptides are conditioned on the pOX1 plasmid where three genes, pag, lef, and cya, are located. The LF protein in combination with PA creates a lethal toxin, but EF with PA forms an edema toxin. Anthrax toxins are produced by vegetative forms of bacteria. In combination, virulence factors promote the multiplication of bacilli after invading the human organism. The lethal toxin causes the release of tumor necrosis factor (TNF) and interleukin-1 (which are responsible for rapid health deterioration during the inflammatory process) from macrophages, as well as development of symptoms and, possibly, cell damage [18, 19]. The edema toxin causes the formation of edema in tissue as a result of water and Cl− ions loss from cells and may inhibit neutrophil phagocytic activity and oxidative burst [18]. Anthrax can also result in necrosis, septicemia, organ failure, and death. If not treated, patients may die in a few days.
Initially, the symptoms of anthrax are nonspecific (symptoms are difficult to distinguish from those of other diseases); therefore, it is difficult to recognize and quickly apply proper treatment [3]. However, at the initial stage of the disease, people should be treated with antibiotics or vaccinated as early as possible, as progression of the disease (especially in the case of inhalational anthrax) is rapid, and if the treatment is not applied within the first 24 h from first observed symptoms, it may result in death.
In some cases, the consumption of contaminated food (meat and milk) has led to foodborne illnesses associated with B. anthracis [20]. Conversely, the closely related species B. cereus is responsible for the majority of foodborne illnesses attributed to the B. cereus group. There is a broad range of foods associated with B. cereus infection including food of both animal and plant origin. Many of these foods may contain B. cereus since spores of this organism are heat-resistant and can survive cooking [20]. Food poisoning by B. cereus is a result of food-contaminating enterotoxins—emetic (vomiting) and diarrhogenic—that are produced by the bacteria. The first toxin causes intoxication as a result of thermostable toxin (cereulide, cyclic peptide toxin) ingestion, while the second, diarrheal one is an effect of infection by vegetative cells or spores producing heat-labile enterotoxin in the small intestine [21]. The symptoms of emetic poisoning occur within 1–5 h after ingesting contaminated food. This toxin is produced during bacterial growth in food [22]. Strains that are able to cause diarrhea are difficult to identify because of the diverse and complicated mechanisms characterizing this type of infection. The symptoms of diarrheal syndrome occur 8–16 h after food ingestion [23].
2.2. Epidemiology of B. anthracis and Other B. cereus Group Bacteria
Nowadays, the risk of anthrax is extremely small, at least in developed countries, where animal husbandry is carried out in modern conditions and hygiene is respected. Anthrax may constitute a problem especially in countries where the vaccination of animals is not practiced. However, the risk of bioterrorism using the pathogen is also a real threat.
There is no strictly defined infectious dose for humans. Its amount may be influenced by such factors as the route of infection (type of anthrax), state of health of person, and virulence of the infecting strain [3]. The infectious median lethal dose (LD50) is likely within the range of 2500–55000 spores [24]. But there are data indicating that for induction, cutaneous anthrax 10 or fewer spores are required [25]. In the case of gastrointestinal anthrax, however, the defined minimal infectious dose (Mid50) is estimated to be approximately 1011 spores [26]. Epidemiological evidence suggests that the majority of cases of foodborne illness caused by B. cereus have been associated with concentrations in excess of 105 cfu/g in food. Only rare cases of illness involving 103–105 cfu/g of B. cereus in food have been reported [27]. Both B. cereus and B. anthracis bacteria may infect people, but more serious side effects may be observed in immunocompromised, young or old patients in particular [20]. For example, skin injuries may be a convenient way of anthrax spreading; for example, soil contaminations may be dangerous especially for patients predisposed to bacterial infections, such as those suffering from diabetic foot syndrome, because of nonhealing ulcers that may constitute the way for spores or vegetative forms to invade the human organism.
Natural B. anthracis is present in the environment; for example, the highest level of anthrax spores has been detected in Namibia, where in the vicinity of animal carcasses it amounted to 1 000 000 spores per 1 g of soil [28]. Using anthrax bacilli for bioterrorism purposes requires much higher doses [2]. Data show that 100 kilos of powdered spores may be a lethal dose for 1013 people.
A simulation of an expert committee of the World Health Organization [5] showed that the release of 50 kilos of anthrax spores over a city would result in 250 000 infections leading to 95 000 deaths (without treatment). The cost of a bioweapon attack using anthrax was estimated at $26.2 billion per 100 000 people exposed to the biowarfare agent [24]. Turnbull et al. indicated that the highest levels of anthrax spores (20 to 40 colony-forming units of spores per cubic meter were detected) were found in air at dusty anthrax carcass sites in Namibia, 3 to 9 m above those sites [5]. Interestingly, the results of estimation indicated that it would take about 2.5 minutes for a human to inhale 1 spore of B. anthracis. But the authors suggested that the probability of inhaling anthrax spores depends significantly on the size of the particles to which spores are attached [3].
The Convention on the Prohibition of the Development, Production, and Stockpiling of Bacteriological (Biological) and Toxin Weapons of 1971 prohibits conducting research using bacteria (e.g., B. anthracis), their toxins, and viruses, for offensive purposes. It does, however, permit the development of vaccines for defensive purposes. There are speculations yet that somegovernments fund the conduct of research concerning B. anthracis application as a biowarfare agent [29]. The epidemic in the Sverdlovsk military laboratory (1979) was caused by accidentally releasing aerosol containing anthrax spores (probably 1-2 g), which were carried by the wind and which caused the greatest ever documented epidemic of pulmonary anthrax in human history. Moreover, B. anthracis could also be involved in cases of unintentional spread of bacteria, as recently happened when a laboratory mix-up exposed many employees to anthrax [30]. The 2012 report showed that decontamination after the anthrax letters attacks from 2001 in the US, as a result of which 11 cases of anthrax inhalation (five patients died) and 11 cases of cutaneous anthrax were reported, costed $320 million [31].
B. anthracis may be attractive as a biological weapon due to low production costs and ease of transmission [2]. Vegetative B. anthracis forms are not easily transmitted, but spores can be transmitted to humans, and therefore applying spores in the aerosol form is probably the most effective. The anthrax bacillus is easy to obtain in culture and the costs of spore production are low; it is estimated that the production of 1 kilo of spores averages $50 [2, 32]. The source of infection may be anthrax spores contained in aerosol or foods. After release, the anthrax aerosol is odorless and invisible and may be transferred over a long distance (many kilometers). Spores are robust and long-lasting (they are resistant to heat, chemicals, ionizing radiation, and ultraviolet light) [19]; for example, spores that were isolated in Kruger National Park in Africa from animal bones were estimated to survive about 200 years [33]. Boiling spores in water for 10 minutes causes their complete destruction [18]. Bacteria that belong to the B. cereus group are widespread and able to form spores which have the ability to remain resistant despite long-term storage and show thermostability. These are the reasons for the existence of a wide variety of foodborne illnesses.
B. anthracis is usually a drug-sensitive strain, but strains that may be multidrug resistant are deliberately engineered [4]. A potential B. anthracis terrorist attack may be caused by contamination of food and water, spread by letters, or spraying in public transport. It may cause widespread panic and requires special, quickly arranged actions for collective health preparedness. Results of anthrax attack simulation demonstrate that aerosol spores penetratethroughout a building in less than 4.5 min [34]. What is more is that prompt action, such as closing the doors and windows, shutting the ventilation system, and deactivating heating or air conditioning, would effectively reduce spore concentration inside the site in which the aerosol was released [35].
3. B. anthracis Bacteriophages
Bacteriophages (phages) are viruses that infect and multiply only in bacterial cells. It is estimated that their abundance in the biosphere exceeds 1030-31 virions [36, 37], ten times more than bacterial cells [38]. Bacteriophages are present in the environment: soil, marine water [39], and extreme conditions such as the Sahara desert sands or hot springs [37, 38]. We consume them with food and drinking water. Together with bacteria they constitute an integral part of the microbiome [40]. Phages in humans may be successfully used in the treatment of a wide range of infections, both local and systemic [6]. Applying phage therapy is safe for patients. There has been low incidence of phages' adverse effects (e.g., nausea, loss of appetite, superinfection, and body temperature increase) associated with the use of them [6, 41]. The results obtained by Łusiak-Szelachowska et al. (2014) indicated that the induction of antiphage antiserum activity in patients receiving phage therapy does not influence the final outcome of the therapy [42]. Despite these data, phage therapy (regarding the use of different phages or different cocktails consisting of different phages) has not been approved by the FDA so far. Clinical trials that may confirm the safety and effectiveness of the therapy need to be conducted [6].
Interestingly, bacteria's resistance to antibiotics does not contribute to the formation of phage resistance [43]. Therefore, phages may be used to treat infections caused by antibiotic-resistant bacterial strains, for example, methicillin resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus (VRE), and extended-spectrum beta-lactamases producing strains (ESBL) [44–48]. Moreover, phages may be simultaneously active against bacteria resistant to many antibiotics [47, 49].
Anthrax-specific phages were first isolated in the 1950s [50]. In 1951 McCloy isolated the lysogenic W phage from an atypical B. cereus strain [51]. The phage was specific to all 171 isolates from B. anthracis but showed limited activity against B. cereus strains (only 2 of 54 strains) [52]. These data indicate specific activity of the phage, especially against anthrax bacilli. Then, Brown and Cherry isolated a gamma (γ) phage which was the lytic variant of the W phage [53]. They demonstrated that the γ phage is able to lyse both encapsulated and nonencapsulated B. anthracis strains. However Negus et al. suggested that the optimized capsule production in B. anthracis tested by Brown and Cherry might have been carried out incorrectly [54]. Interestingly, the phages tested by Negus et al.—γ, Fah, F7, and F9—were able to lyse B. anthracis Sterne in both capsulated and nonencapsulated form.
Phages active against B. anthracis (both lytic and lysogenic) are widespread in the environment and have been isolated from soil, carcasses, feces, sewage, and the intestinal tract of the earthworm Eisenia fetida [54–58]. B. anthracis specific phages and their characteristics are presented in Table 1. Apart from phages listed in Table 1, there have been many more anthrax phages isolated, for example, Nk, DB, and SP50, belonging to Myoviridae isolated from Iowa topsoil [55]; BA39, BA21, BA28, and BA51 isolated from a sewage treatment plant (Germantown), belonging to Myoviridae [59]; ф20 lysogenic phage induced by exposure to UV light, belonging to Siphoviridae [60]. Interestingly, Lee et al. prepared a review in which they characterized and collected three groups of bacteriophages infecting members of B. cereus group, according to their genomic analysis [61].
Table 1.
Bacillus anthracis phages and their characteristics.
| Name of phage | Type of life cycle | Short description | Phage host specificity | Possible application |
|---|---|---|---|---|
| Wβ | Lysogenic | Belongs to Siphoviridae. Inability to infect encapsulated cells [4]. | Infects all 171 tested nonencapsulated strains [50], but does not infect other Bacillus strains. | Preparing bioluminescent reporter bacteriophage for B. anthracis detection in clinically relevant samples [56] and providing an antibiotic susceptibility profile [4]. |
|
| ||||
| Gamma phage (γ) | Lytic | Belongs to Siphoviridae [57]. Cannot bind to GamR receptor on bacterial surface and does not encode a PDGA depolymerase. Encodes a fosfomycin resistance gene [58]. |
B. anthracis 1584; 211; SL 1809; Sterne 34F2 [51]. Not active against B. anthracis Ames strain that produces capsule. Strains that do not encode the pX01 plasmid are more susceptible to phage γ than strains that possess the plasmid [62]. |
Identification of B. anthracis strains and its differentiation from other similar strains from B. cereus group. |
|
| ||||
| AP50 | Lytic | Belongs to Tectiviridae [55], isolated from soil. Infects only B. anthracis strains. Does not lyse strains belonging to different Bacillus spp. The lysogenic mutant AP50c is characterized by very high killing efficiency [63]. | Narrow host range [64]. Lyses 33% of B. anthracis strains [1]. This phage may infect bacterial strains that are resistant to γ phage [63]. It does not infect the B. cereus ATCC4342 strain, which infects the γ phage. | Probable use in therapy of anthrax. It is suggested to be used in typing and biocontrol of B. anthracis [65]. |
|
| ||||
| Fah | Lytic | Belongs to Siphoviridae [66]. | B. anthracis 1584; 211; SL 1809; Sterne 34F2 [54]. Narrower lytic spectrum. Lyses 73–89% of B. anthracis strains [1, 66]. | Probable use in therapy of anthrax. |
|
| ||||
| Worm intestinal phage 1 (Wip1) | Lytic | Belongs to Tectiviridae [67]. It was isolated from the intestinal tract of Eisenia fetida worms. [52]. | Exhibits a narrow host range highly specific to B. anthracis [67]. Does not infect the B. cereus ATCC4342 strain, which infectstheγ phage [52]. | Potentially useful diagnostic tool for efficient identification of B. anthracis; may be labelled and applied in organism for rapid readout [61]. |
|
| ||||
| Giraffe phage | ? | Belongs to Siphoviridae isolated from giraffe faeces in a zoo (Long Island) [68]. This phage shows a rapid lysis phenotype. | Lyses the ciprofloxacin-resistant B. anthracis strain HS2-7 [68]. | Possible use in therapy when infection is caused by antibiotic-resistant B. anthracis strain [67]. |
|
| ||||
| F7 | Lytic | Isolated from bovine faeces. Belongs to Siphoviridae [51]. | B. anthracis 1584; 211; SL 1809; Sterne 34F2; B. cereus ATCC13472; B. cereus ATCC 10876; B. thuringiensis ATCC 33679 [51]. | Probable use in therapy of anthrax. |
|
| ||||
| F9 | Lytic | Isolated from bovine faeces. Belongs to Siphoviridae [51]. | B. anthracis 1584; 211; SL 1809; Sterne 34F2; B. cereus ATCC13472; B. cereus ATCC 10876; B. thuringiensis ATCC 33679 [51]. | Probable use in therapy of anthrax. |
|
| ||||
| vB_BanS-Tsamsa | Lysogenic | Isolated from carcasses in Etosha National Park in Namibia. Belongs to Siphoviridae. Has the largest sequenced genomes of Bacillus siphovirus.Purified endolysin encoded in genome of this phage has broader spectrum than the phage. The largest siphovirus known to infect Bacillus strains [54]. | Infects also strains belonging to B. cereus and B. thuringiensis [54]. Did not lyse the B. anthracis PAK-1 strain (resistant to both γ and cherry phage). Moderate specificity to B. anthracis. | Use of purified phage endolysin in B. anthracis biocontrol. |
Bacteriophages, as well as lysins (encoded in phage genomes), could be useful in the treatment of infections caused by B. anthracis, destruction of B. anthracis germinated spores, and environmental disinfection. Treatments with phages or lysins may be extremely important because of being potentially safe for humans infected with anthrax and threatened with death caused by those bacilli. Bacteriophage-based methods for identification and/or treatment of anthrax may be methods of the future. This common and well-investigated tool—which bacteriophages constitute—is also very useful in molecular biology. There are methods of B. anthracis strain identification, for example, the γ test approved by the FDA in 2005 [1] or the bioluminescence test based on light detection after the application of a phage with the lux AB gene. Possible phenotypic alterations of temperate phages in B. anthracis include an influence on bacterial sporulation (the prophage state may induce rapid sporulation phenotype), biofilm formation, and induction of exopolysaccharide production [69]. However, bacteriophages may be used not only as antiterrorism tools, but also aspotential bioterrorism agents [70]. For example, lysogenic bacteriophages that contain virulence or drug resistance genes may be used for genetic manipulation, enabling the modification of nonpathogenic bacteria into a strain that would be resistant to available antimicrobial drugs. Despite the intensive studies on isolation and characterization of B. anthracis phages, many questions still remain unanswered.
Apart from previously described possible phage applications, bacteriophages can be also used in controlling bacterial pathogens from the B. cereus group in food and food processing environments. A summary of the potential use of phages active against bacteria from the Bacillus cereus group, in the case of potential use of these bacteria as a biological weapon, is presented in Figure 1.
Figure 1.
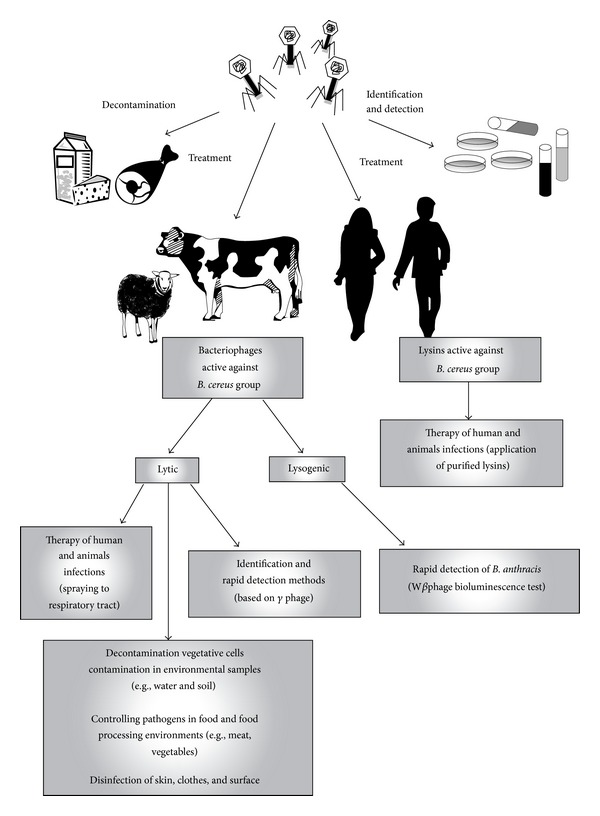
The possibility of using bacteriophages and lysins against bacteria from Bacillus cereus group.
One of the advantages of bacteriophages specific for B. anthracis is their narrow activity against the bacterial host, being restricted to strains of B. anthracis—not active against closely related strains of the Bacillus genus (such as B. cereus or B. thuringiensis). But bacteria from the B. cereus group are very closely related. Bacillus cereus and B. anthracis share many common phage parasites [71]. Close relatedness between B. anthracis and bacteria from the B. cereus group enables certain phages active against B. anthracis to show activity also against B. cereus and vice versa [72].
In our opinion, when the usefulness of anthrax phages is considered a tool for therapy and the detection of bacteria, the specificity (narrow host range) is an advantage. If the aim is decontamination, the broad lytic spectrum may be helpful in case of elimination of both B. anthracis and other species belonging to the B. cereus group is the objective.
4. Identification of B. anthracis
Should a bioterrorism attack occur, there must be a possibility for its rapid detection and identification in an average microbiological laboratory. Such work requires the biological safety level 3 use (BSL-3) [28]. To work with agents that may cause serious or potentially lethal diseases (e.g., B. anthracis), especially through the inhalation route of exposure, the laboratory should be designed to ensure the personnel safety. It has to, for example, be self-closing and entered through an airlock or anteroom and have double-door access and a hand washing sink near the laboratory exit; the air cannot be recirculated, and there must be negative airflow into the laboratory [73].
B. anthracis may be isolated from different animal body specimens (blood cultures, cerebrospinal fluid, stool, respiratory specimens, and cutaneous lesions), but their source depends on the type of anthrax [10].
Methods used for identifying B. anthracis should offer rapid detection even at low concentration of the pathogen, with no crossreactivity. They should be simple to perform and possible to perform at the site of sampling [19]. Moreover, the assay should enable the detection of both spores and vegetative forms. Therefore, the real challenge is to optimize the B. anthracis foolproof detection system for protecting public health.
Van Tongeren et al. studied the microbial community of the interior human environment of the International Space Station [74]. They isolated from one microbial sample multiple strains belonging to the B. cereus group, including B. anthracis. The authors emphasized that there is a real challenge in rapid detection of anthrax bacilli from that type of microbiological material.
Differentiating B. anthracis from other strains of the Bacillus genus may cause diagnostic difficulties. Standard microbiological methods used in laboratories take 24–96 h [5, 62]. Despite the introduction of the Ground Anthrax Bacillus Refined Isolation (GABRI) method to analyze environmental samples, which enables the detection of low levels of B. anthracis [75], this method also requires 24 or 48 h of incubation. Public security requires shorter times of detection of anthrax contamination. Methods depending on antigen detection allow the result to be obtained within several hours [19] but may show a lack of sensitivity and specificity as well as crossreaction with other strains of the Bacillus genus, thus giving false positive results. The nucleic acid based method (e.g., polymerase chain reaction) is highly specific but does not discriminate between live and dead bacteria [76] and clean starting samples are required [19]. So far, there is no method that can be considered reliable.
4.1. Detection of B. anthracis
Phages may have potential to be used in B. anthracis detection in clinical, environmental, or food samples [70]. Most phage-based assays exploit the γ phage [77]. They are based on high specificity of phages to certain bacteria species, and their detection limit is 103–105 cfu/mL. It is possible to identify anthrax bacilli as quickly as within 60–120 min.
The phage γ test is a standard method for identification of B. anthracis strains and differentiates them from other closely related strains from the Bacillus genus [78]. This routine identification test takes 2–4 days [5]. The presence of a polypeptide capsule inhibiting B. anthracis infection by lytic γ phage constitutes a serious problem in using this method. The synthesis of the capsule blocks the GamR receptor on the bacterial cell surface responsible for phage binding [79].
Based on the differences between phages' lytic spectrum, it is supposed that the identification/typing test using the γ phage is probably less sensitive when compared with the Wip1 phage [58, 80]. Additionally, Wip1 plaques can be detected after merely 12 h after bacterial infection.
Detection of B. anthracis by using Wβ phage bioluminescence enables the detection of a signal as soon as after 16 min from the moment of commencing the infection of B. anthracis cells with the Wβ phage possessing an incorporated luxAB reporter gene [62]. The method allows for direct detection of B. anthracis in clinical specimens (e.g., blood, stool, and sputum) [77] and excludes the detection of members belonging to the B. cereus group closely related to B. anthracis [4, 62]. It detects only live bacteria (~103 cfu/mL within 60 min) and B. anthracis germinated spores (within 60 min). Spores are refractory to phage because they do not show the GamR on their surface; therefore spores may be detected only in the germinating state. A higher phage titer gives a stronger detection signal. The limitations of the bioluminescent Wβ phage-based method may result from B. anthracis' resistance to phage infection and no possibility of the reporter phage to infect encapsulated strains. Abshire et al. found that only 2 strains out of 51 tested isolates of B. anthracis were resistant to the lysis caused by the γ phage [65]. It may indicate that natural phage resistance of B. anthracis strains is not common.
Kan et al. identified the ligand on the Wip1 bacteriophage that is highly specific to the receptor on B. anthracis [80]. They observed that the gene product p23 of the Wip1 bacteriophage is a receptor-binding protein on the phage surface. The presence of this protein and narrow host range of the Wip1 phage may provide new tools for the identification of B. anthracis strains.
The anthrax spores should be detected before the occurrence of symptoms, especially by the use of continuous monitoring of spore content in the air [81]. The system should be sensitive and selective to avoid false alarms of bioterrorist attack. Brigati et al. proposed a method based on landscape pIII phage-display libraries (that contain thousands of copies of peptides best binding to a specific antigen) and phages expressing a specific peptide used as a probe that specifically binds to B. anthracis spores [81]. This method is not ideal due to the possibility of clones crossreacting to other species belonging to the Bacillus genus. But the most specific phage display spore binding peptide EPRLSPHS bound 3.5- to 70-fold more strongly to the B. anthracis Sterne spores than to other strains. Also, sensors that use filamentous phages may be useful in B. anthracis spore identification, and wireless magnetostrictive sensors showed binding affinity to B. anthracis that was better than to B. cereus and to B. subtilis spores [82]. Applying filamentous phages in these methods is justified for these phages are suspected to be the most stable nucleoproteins in nature. They are extremely resistant to high temperature (even up to 80°C), acids and alkaline solutions, organic solvents (50% alcohol), and denaturing agents (6–8 mg/L urea) [81, 83]. The detection limit of the described method is at 103 spores/mL [84]. Detection of anthrax spores in water using phage as a bioprobe and magnetostrictive mili/microcantilevers (MSMC) designed as a sensor platform was developed by Fu et al. [85]. This method enabled in situ detection. Schuch et al. prepared a rapid and highly specific system for detecting spores [86]. The detection is based on light emission in the presence of luciferin and luciferase and the release of ATP from lysed bacterial cells. It is based on the ability of PlyG to kill germinating spores and is applied using a hand-held luminometer. The signal was detected only 10 min after the addition of germinating spores of the RSVF1 strain. What is more is that the light was emitted only 5 min after adding PlyG. Moreover, a method based on the binding of B. anthracis vegetative cells has also been developed [87].
Shabani et al. presented a phage-modified electrode microarray method for rapid and direct impedimetric detection of B. anthracis [88]. It is based on the immobilization of the γ phage and its high specificity to B. anthracis species and provides a low-cost platform for direct identification of B. anthracis. Its detection limit is 103 cfu/mL with a sample volume of merely 40 μL.
5. Treatment of Anthrax
Without immediate treatment, inhalation of anthrax spores is usually lethal (within the first 24 h from observed symptoms, it may result in death). Therefore, therapeutic intervention should be initiated as early as possible [89]. The antimicrobial chemotherapy recommended for the treatment of patients with inhalational anthrax is effective, but long-term therapy may cause antibiotic resistance in B. anthracis [90]. Drugs used for postexposure prophylaxis are penicillin G, amoxicillin, doxycycline, ciprofloxacin, and ofloxacin administered for 60 days or more [24].
Penicillin has been considered the drug of choice, and it is very rare that resistance to this antibiotic is found in naturally occurring strains [9]. Ciprofloxacin, penicillin, and doxycycline are recommended for the treatment of humans and as prophylactics after exposure to the spores [91]. Many in vitro studies show that B. anthracis is susceptible to penicillins, fluoroquinolones, tetracycline, chloramphenicol, aminoglycosides, macrolides, imipenem/meropenem, rifampicin, and vancomycin [9, 91, 92]. However, the organism is resistant to cephalosporins, trimethoprim, and sulphonamides. B. anthracis is usually sensitive to a broad range of antibiotics. Cavallo et al. tested its sensitivity to antibiotics in 96 strains of B. anthracis isolated from humans (1), animals (28), and the environment (67) in France [89]. 11.5% of strains were resistant to penicillin G and amoxicillin. All of them were resistant to cotrimoxazole but susceptible to antibiotics such as doxycycline, vancomycin, clindamycin, rifampicin, imipenem, or teicoplanin.As a result of long-term antibiotic treatment B. anthracis strains may be converted into antibiotic resistant strains [90]. It was observed that only 11% of natural/environmentally isolated strains of B. anthracis were resistant to penicillin G [89].
In the case of B. cereus, the bacteria—due to β-lactamase production—are insensitive to penicillin-related antibiotics (merely 1% of strains are susceptible to penicillin) and show resistance to erythromycin and tetracycline, for example, carbapenem [61, 93, 94]. We suppose that, due to problems with antibiotic treatments and improvement in bacterial drug resistance, these strains may be used as potential biowarfare agents. Therefore, for public safety, there must be known an agent to which these bacteria are susceptible.
Treatment with antibiotics beginning 1 day after the exposure to an aerosol with anthrax spores can protect against death. However, optimal protection isprovided bycombining antibiotics with vaccination. Vaccination is the best form of mass protection. The first anthrax animal vaccine was developed by Pasteur in 1881. Pasteur attenuated B. anthracis strains and proved that these strains could protect sheep from fully virulent strains [95]. Human vaccines emerged in the middle of the 20th century [9]. Human anthrax vaccine (anthrax vaccine adsorbed, AVA), currently licensed for use in the United States and the United Kingdom, consists primarily of protective antigen (PA) absorbed onto aluminum hydroxide [96, 97]. This vaccine was tested in guinea pigs, rabbits, and rhesus macaques by Fellows et al. [98].
According to FDA prescribing information concerning the observed side effects of AVA (BioThrax), local adverse reactions have been observed (especially at injection site), for example, tenderness, pain, erythema, edema, and arm motion limitation; (≥5%) as well as systemic adverse reactions: fatigue headache and muscle aches [99]. The currently available vaccines have a chemically complicated composition and it is believed that they are insufficiently purified [100].
AVA was originally prepared for individuals in high-risk occupations, like veterinarians, farmers, and laboratory personnel working with B. anthracis but was also used for military personnel [96]. About 150 000–200 000 American soldiers sent in 1991 to the war in the Persian Gulf were vaccinated against anthrax [101].
The use of appropriate animal models provides better understanding of the pathogenesis of human anthrax and the development of appropriate methods of prevention and treatment. Rabbits and nonhuman primates (NHPs), for example, rhesus macaques, are commonly used as animal models of inhalational anthrax. The pathological changes observed in rabbits and NHPs are similar to those observed in humans [102]. Savransky et al. showed that the pathology caused by the inhaled form of anthrax in guinea pigs is similar to that in both rabbits and NHPs, as well as in humans. Guinea pigs have alsobeen used in anthrax vaccine studies.
Another popular animal model used to test the sensitivity to virulent B. anthracis is the mouse. The mouse model is useful in studies on host resistance to anthrax and on pathogenesis, how the agent establishes infection in the host, and characteristics of the spore and vegetative bacilli. It is known that different mouse strains have various sensitivities to infection by both B. anthracis and anthrax toxin [103]. For instance, the BALB/c mouse strain is highly resistant, and strains such as A/J and DBA/2J are highly susceptible to infection [12, 99]. Interestingly, the susceptibility of mouse strains to lethal toxin (LT) does not necessarily correlate with its susceptibility to infection. For example, the susceptibility of A/J mice to anthrax toxin appeared to differ from the susceptibility to infection [99]. The rat and hamster, meanwhile, are important animal models for understanding the B. anthracis exotoxins, both LT and EF [12].
5.1. The Potential Use of Phage in Anthrax Treatment
The first phage therapy studies on B. anthracis were conducted by Cowles and Hale on mice [104]. The B. anthracis Thomas strain and bacteriophages which had been isolated from a malignant pustule, which were applied as therapeutics, were used in the experiment. The animals were inoculated (intraperitoneally) with 0.1 mL of bacteria (106 cfu/mL) and 0.1 mL of bacteriophage (109-1010 pfu/mL). The authors found that, only in the group inoculated with B. anthracis and bacteriophage mixture incubated 25 min before injection, 100% of mice survived. The results of this study also showed that only the phage, in high titer, quickly and permanently lysed the strain of anthrax used in the experiments.
Phages may be applied in phage therapy in the case of B. anthracis (also drug-resistant) infections [70]. For better effectiveness of therapy, phages active against B. anthracis should encode capsule depolymerases, to degrade the PDGA capsule that may be present in the bacterial surface. In this case phages may bind to the cell surface receptor of the bacteria and destroy these dangerous bacteria [54, 105].
Besides the whole phage particles, also endolysins can be applied in the therapy of anthrax. Endolysins are enzymes encoded in the bacteriophage genome and specifically lyse the peptidoglycan of the bacterial cell wall during the phage lytic cycle [106]. The enzymes may create new opportunities for the construction and production of genetically engineered enzymes for bacteria elimination, biocontrol, and experimental therapies. The endolysin PlyG isolated from the γ phage may be applied against B. anthracis (e.g., used as abiowarfare agent) [86]. Susceptibility of B. anthracis strains to γ phage infection and purified PlyG lysin isolated from this phage indicated that both of these agents have a narrow bacteriolytic spectrum—they especially showed high activity against almost only B. anthracis strains [86]. The authors decided to use isolates of streptomycin-resistant B. cereus RSVF1 strain because of the similarity of this strain to the B. anthracis. Lytic activity of lysin against this strain was the same as in the case of B. anthracis strains. In the study of Schuch et al., (2002) BALB/c mice were intraperitoneally infected with B. cereus RSVF1 (1.0 × 106 cfu/mL) and, 15 min later, treated with 50 and 150 U PlyG. The application of lysin significantly rescued mice in comparison to untreated animals. Moreover, resistance to PlyG was not observed in vitro in either RSVF1 or EMS RSVF1 mutagenized strains (mutagenesis with the use of ethyl methanesulfonate). However, both Novobiocin (3.5 μg/mL−1) and streptomycin (150 μg/mL−1) resulted in bacterial resistance to these antibiotics. What is more is that the authors have demonstrated that RSVF1 strain that became resistant to the phage remains sensitive to PlyG. In bacterial culture, application of lysin caused morphological changes of bacterial cells and ultimately led to cell lysis. Also, purified lysin encoded by the Tsamsa phage is suggested to be used in B. anthracis biocontrol due to its broad lytic spectrum that lysed more strains belonging to the B. cereus group than complete phage and which goes outside B. anthracis strains [56]. Inal suggested that in the case of anthrax infections lysin should be applied as soon as possible, before the lethal level of toxin is reached [32].
Porter et al. described PlyB lysin which showed lytic activity against a B. anthracis-like strain (ATCC 4342). The enzyme has muramidase activity, whereas PlyG is an amidase [107]. It is presumed that this lysin may be a new defensive tool in the face of bioterrorism danger. Lysins have some advantages over phages as the capsule is not an obstacle for PlyG to access the bacterial cell wall and may destroy encapsulated forms of bacilli. They show high specificity, not disturbing another bacterial species, and strong enzymatic activity; moreover the enzymes allow destruction of bacteria within seconds or minutes [108]. In in vivo experiments it was showed that PlyG applied in mice intraperitoneally did not cause evident toxic effects [86]. Another prevalence of these enzymes is that the resistance to them is induced rarely or not at all in comparison with whole phage particles. What is more is that it was observed that purified lysin isolated from Tsamsa phage was characterized by broader lytic activity than it was observed in the case of phage host range [56]. This phenomenon may be useful for biocontrol and decontamination not only in the case of B. anthracis threat but also in the instances of other B. cereus group bacteria contamination.
Sozhamannan et al. suggested that applying a combination of two different phages (γ and AP50c) with different lytic spectra may be a better alternative for therapy of anthrax, phage-based diagnostics, and disinfection of areas contaminated with anthrax bacilli [66]. Similarly, Inal stated that a phage cocktail (which has the ability to lyse most B. anthracis strains) should be prepared and tested as an optimal antianthrax agent [32]. Also, Porter et al. proposed feasible application of the combination of two different lysins, PlyB and PlyG, which exhibit different lytic activity and cleave different peptidoglycan bonds [107].
It was suggested that phages, especially a combination of different phages, may be used in a spray form applied to skin and clothes surface and into the respiratory tract [86].
5.2. B. anthracis Spore Decontamination
Although the use of phagesagainst B. anthracis is mainly limited to vegetative forms of the bacteria, there are phages that may be used for removing anthrax spores. Anthrax spores are not metabolically active, and they may be inactivated by physical methods (gamma irradiation, ultraviolet light, and high pressure) that are not safe for humans [71, 109]. There is a need to find a method of disinfection that is highly effective and safe. This form of B. anthracis is the most dangerous one as a potential terrorist bioweapon.
The spore cortex is protected by a proteinous coat against, for example, lysozyme. In the germinating state the porosity of coat is increased (even during 10 minutes of incubation in conditions inducing germination) [86]. Fu et al., usingcryoelectron tomography, describedthe structure of the SBP8a phage active against both vegetative and spore forms of B. anthracis and the molecular mechanism of phage infection [110]. The phage showed the possibility to recognize and adhere to the surface of spores and eject its DNA inside the spore by the conformational changes of phage structures (at high SBP8a concentration, approximately 108 pfu/mL).
Application of phages (isolated from soil) in the aerosol form to germinated spores of the B. anthracis Sterne strain caused effective destruction of spores, but the effect was mainly observed when high titer lysate was applied (2.8 × 108 pfu/mL, 3.5 × 108 pfu/mL) [59]. The B. anthracis Sterne strain is a surrogate for virulent B. anthracis, which enables safe conduct of experiments on the avirulent B. anthracis Sterne strain and, according to data, the substitution does not significantly change or limit the results of the studies [71]. But using this strain guarantees safety—especially laboratory personnel who work on the B. anthracis are exposed to the risk of anthrax infection—and gives the possibility to conduct research on these dangerous bacteria.
As was observed, phages that are used against anthrax spores should be resistant to harsh environmental conditions, for example, dryness, ultraviolet radiation, extreme temperatures, and bodily fluids,to maintain ability to kill bacteria [71]. This feature would be important especially in the case of the disinfection application of spores (because of their high resistance to different factors).
6. Bacteriophages in Foodborne Pathogen Disinfection
There may exist the possibility to use other pathogens belonging to the B. cereus group in a bioterrorism attack. Bacteriophage typing may be useful for detecting food contamination with B. cereus [111], due to the fact that this method is cheap and convenient and seems to be fairly accurate [72]. The FDA approved the use of bacteriophages in order to guarantee food disinfection [112, 113]. There is a possibility and permission to apply bacteriophages providing food safety. To inhibit B. cereus contamination, the use of BCP78 phage isolated from fermented food was proposed [112].
Bacteriophages infecting B. cereus may be helpful in destroying this foodborne pathogen. For example, two phages, FWLBc1 and FWLBc2, which were isolated from soil, reduced the pathogen in mashed potato (by >6 log10 cfu/mL during 24 h). Because of the phages' narrow lytic activity, it has been suggested to use them as a component of phage cocktails [114]. This high specificity may constitute a disadvantage in using phages against foodborne pathogens, due to the complex composition of bacteria that contaminate food. A broad spectrum of inhibition of bacterial growth has been shown for Bc431v3 phage. It lysed bacteria belonging to the B. cereus group and B. licheniformis, B. megaterium, and B. psychrosaccharolyticus. The BPS10C and BPS13 phages that showed lytic activity against B. cereus were able to completely inhibit bacterial growth (bacteria belonging to the B. cereus group) for up to 6 h [115]. New phages with proven activity against B. cereus are still being isolated [116]. But it is extremely important that in their genomes phages do not encode genes responsible for lysogeny, toxin production, and genes affecting the pathogenicity of bacteria and antibiotic resistance [72]. The lack of them makes phage application safe for humans and increases phage application as a strategy of biocontrol of bacteria belonging to the B. cereus group.
Endolysins may be successfully applied in the case of B. cereus contamination [108]. For example, the LysB4 lysin isolated from the B4 bacteriophage was reported as the first endopeptidase among endolysins obtained from the B. cereus phages. Interestingly, the enzyme not only shows broad lytic activity against B. cereus strains but also lyses Gram-negative strains, for example, E. coli strains, in comparison with the phage lytic spectrum, which, most frequently, is limited to one B. cereus strain. This feature enables the enzyme to be an effective antibacterial agent active especially against foodborne pathogens. Furthermore, the lysin destroyed bacteria in merely 15 min and, according to Lee et al., this enzyme seems to be a perfect candidate as a biocontrol agent in the case of B. cereus contamination [61]. Endolysin BPS13 isolated from the BPS13 phage was highly temperature-stable; for example, it displayed lytic activity even at 100°C (suspended in glycerol) [115]. Yuan et al. isolated PlyBtSC33 endolysin from the B. thuringiensis BtSC33 phage [117]. The authors showed that this agent may be potentially used for disinfection purposes, had high temperature resistance, and showed a broad lytic spectrum (low lytic activity against B. thuringiensis but higher activity against B. anthracis and B. cereus strains). High thermostability may be useful in lysin application against food poisoning caused by B. cereus, especially in the heat treatment process. This endolysin may also be considered in anthrax treatment.
The lytic protein E33L that caused the lysis of B. anthracis was isolated from the genomeof B. cereus [118]. It was an N-acetylmuramoyl-L-alanine amidase, active against both B. anthracis and closely related strains belonging to the B. cereus group. This enzyme induced complete lysis already in nanomolar concentrations in vitro (almost 99% lysis of B. anthracis was achieved at 50 nM in 60 min). What is more is that the protein was active against B. cereus strains. An advantage of this agent is that the enzyme does not seem to be degradable by bacterial proteases, and furthermore it showed significantly higher lytic activity than Bacillus-phage-encoded endolysins.
The biothreat danger is a real possibility, and regardless of how the attack occurs (through water, air, mail, food contamination, soil, insects, and public transport) people should have a foolproof tool for rapid detection and identification and a possibility to treat patients from these dangerous (probably drug-resistant) pathogens. The control of B. cereus group bacteria, especially B. anthracis, is important in prevention and detection of bioterrorist attacks involving food contamination with regard to human health safety and economic reasons. We suggest that phages (whole particles or their purified endolysins) may constitute a good prospect in this area.
7. Concluding Remarks
The past two decades have proved that bioterrorism is a real threat which needs to be properly controlled. Recent developments in phage therapy confirm that it may provide a reliable countermeasure preventing serious consequences of a terrorist attack using deadly bacteria, especially those resistant to antibiotics. Phage-mediated elimination of Bacillus cereus group bacteria, especially B. anthracis, seems to be an efficient tool against the potential use of such bacteria as a terrorist bioweapon.
Acknowledgment
This work was supported by the project “Innovative Bacteriophage Preparation for the Treatment of Diabetic Foot” no. POIG.01.03.01-02-048/12 founded by The National Centre for Research and Development.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Filippov AA, Sergueev KV, Nikolich MP. Bacteriophages against biothreat bacteria: diagnostic, environmental and therapeutic applications. Journal of Bioterrorism Biodefense. 2013;S3(article 010) [Google Scholar]
- 2.Daniszewski P. Bacillus anthracis as biological weapons. International Letters of social and Humanistic Sciences. 2013;9:74–83. [Google Scholar]
- 3.World Health Organization Emerging and other Communicable Diseases. Surveillance and Control Guidelines for the Surveillance and Control of Anthrax in Humans and Animals. WHO/EMC/ZDI/98.6, http://www.fas.org/nuke/intro/bw/whoemczdi986.htm.
- 4.Schofield DA, Sharp NJ, Vandamm J, et al. Bacillus anthracis diagnostic detection and rapid antibiotic susceptibility determination using “bioluminescent” reporter phage. Journal of Microbiological Methods. 2013;95(2):156–161. doi: 10.1016/j.mimet.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Turnbull PCB, Bőhm R, Cosivi O, et al. Guidelines for the Surveillance and Control of Anthrax in Humans and Animals. 3rd edition. 1998. (World Health Organization EMC/ZDI./98.6). [Google Scholar]
- 6.Międzybrodzki R, Borysowski J, Weber-Dabrowska B, et al. Clinical aspects of phage therapy. Advances in Virus Research. 2012;83:73–121. doi: 10.1016/B978-0-12-394438-2.00003-7. [DOI] [PubMed] [Google Scholar]
- 7.Borysowski J, Miedzybrodzki R, Górski A, et al. Phage Therapy: Current Research and Applications. Caister Academic Press; 2014. [Google Scholar]
- 8.McIntyre L, Bernard K, Beniac D, Isaac-Renton JL, Naseby DC. Identification of Bacillus cereus group species associated with food poisoning outbreaks in British Columbia, Canada. Applied and Environmental Microbiology. 2008;74(23):7451–7453. doi: 10.1128/AEM.01284-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spencer RC. Bacillus anthracis. Journal of Clinical Pathology. 2003;56(3):182–187. doi: 10.1136/jcp.56.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klietmann WF, Ruoff KL. Bioterrorism: implications for the clinical microbiologist. Clinical Microbiology Reviews. 2001;14(2):364–381. doi: 10.1128/CMR.14.2.364-381.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Titball RW, Manchee RJ. Factors affecting the germination of spores of Bacillus anthracis . Journal of Applied Bacteriology. 1987;62(3):269–273. doi: 10.1111/j.1365-2672.1987.tb02408.x. [DOI] [PubMed] [Google Scholar]
- 12.Twenhafel NA. Pathology of inhalational anthrax animal models. Veterinary Pathology. 2010;47(5):819–830. doi: 10.1177/0300985810378112. [DOI] [PubMed] [Google Scholar]
- 13.Conly JM, Shafran SD. Anthrax and biological warfare revisited. Canadian Journal of Infectious Diseases. 1988;9(2):65–67. [Google Scholar]
- 14.Fouet A, Sirard JC, Mock M. Virulence gene determinants. Salisbury Medical Bulletin, Special Supplement. 1996;87:84–85. [Google Scholar]
- 15.Mizak L. Wąglik-stale aktualne zagrożenie dla ludzi i zwierząt. Przegląd Epidemiologiczny. 2004;58:335–342. [PubMed] [Google Scholar]
- 16.Tonello F, Zornetta I. Bacillus anthracis factors for phagosomal escape. Toxins. 2012;4(7):536–553. doi: 10.3390/toxins4070536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piris-Gimenez A, Corre J, Jouvion G, Candela T, Khun H, Goossens PL. Encapsulated Bacillus anthracis interacts closely with liver endothelium. Journal of Infectious Diseases. 2009;200(9):1381–1389. doi: 10.1086/644506. [DOI] [PubMed] [Google Scholar]
- 18.Kamal SM, Rashid AKMM, Bakar MA, Ahad MA. Anthrax: an update. Asian Pacific Journal of Tropical Biomedicine. 2011;1(6):496–501. doi: 10.1016/S2221-1691(11)60109-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rao SS, Mohan KVK, Atreya CD. Detection technologies for Bacillus anthracis: prospects and challenges. Journal of Microbiological Methods. 2010;82(1):1–10. doi: 10.1016/j.mimet.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Schneider KR, Parish ME, Goodrich RM, Cookingham T. Preventing Foodborne Illness: Bacillus cereus and Bacillus anthracis . http://edis.ifas.ufl.edu/pdffiles/FS/FS10300.pdf.
- 21.Opinion of the Scientific Panel on Biological Hazards on Bacillus cereus and other Bacillus spp in foodstuffs. The EFSA Journal. 2005;175:1–48. [Google Scholar]
- 22.Ehling-Schulz M, Guinebretiere M, Monthán A, Berge O, Fricker M, Svensson B. Toxin gene profiling of enterotoxic and emetic Bacillus cereus . FEMS Microbiology Letters. 2006;260(2):232–240. doi: 10.1111/j.1574-6968.2006.00320.x. [DOI] [PubMed] [Google Scholar]
- 23.Granum PE. Bacillus cereus . In: Doyle MP, Beuchat LR, editors. Food Microbiology: Fundamentals and Frontiers. 3rd edition. Washington, DC, USA: ASM Press; 2007. pp. 445–455. [Google Scholar]
- 24.Inglesby TV, O’Toole T, Henderson DA, et al. Anthrax as a biological weapon, 2002: updated recommendations for management. Journal of the American Medical Association. 2002;287(17):2236–2252. doi: 10.1001/jama.287.17.2236. [DOI] [PubMed] [Google Scholar]
- 25.Watson A, Keir D. Information on which to base assessments of risk from environments contaminated with anthrax spores. Epidemiology and Infection. 1994;113(3):479–490. doi: 10.1017/s0950268800068497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kanafani ZA, Ghossain A, Sharara AI, Hatem JM, Kanj SS. Endemic gastrointestinal anthrax in 1960s Lebanon: clinical manifestations and surgical findings. Emerging Infectious Diseases. 2003;9(5):520–525. doi: 10.3201/eid0905.020537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kramer JM, Gilbert RJ. Bacillus cereus and other Bacillus species. In: Doyle MP, editor. Foodborne Bacterial Pathogens. chapter 2. New York, NY, USA: Marcel Dekker; 1989. pp. 21–70. [Google Scholar]
- 28.Lindeque PM, Turnbull PC. Ecology and epidemiology of anthrax in the Etosha National Park, Namibia. Onderstepoort Journal of Veterinary Research. 1994;61(1):71–83. [PubMed] [Google Scholar]
- 29.Riedel MD. Biological warfare and bioterrorism: a historical review. Proceedings. 2004;17(4):400–406. doi: 10.1080/08998280.2004.11928002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reardon S. Researcher reassigned in wake of disease centre’s anthrax scare. Nature. 2014;511(7509):263–376. [Google Scholar]
- 31.Schmitt K, Zacchia NA. Total decontamination cost of the anthrax letter attacks. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2012;10(1):98–107. doi: 10.1089/bsp.2010.0053. [DOI] [PubMed] [Google Scholar]
- 32.Inal JM. Phage therapy: a reappraisal of bacteriophages as antibiotics. Archivum Immunologiae et Therapiae Experimentalis. 2003;51(4):237–244. [PubMed] [Google Scholar]
- 33.Smith KL, DeVos V, Bryden H, Price LB, Hugh-Jones ME, Keim P. Bacillus anthracis diversity in Kruger National Park. Journal of Clinical Microbiology. 2000;38(10):3780–3784. doi: 10.1128/jcm.38.10.3780-3784.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kournikakis B, Ho J, Duncan S. Anthrax letters: personal exposure, building contamination, and effectiveness of immediate mitigation measures. Journal of Occupational and Environmental Hygiene. 2009;7(2):71–79. doi: 10.1080/15459620903389558. [DOI] [PubMed] [Google Scholar]
- 35.Kournikakis B, Martinez KF, McCleery RE, Shadomy SV, Ramos G. Anthrax letters in an open office environment: effects of selected CDC response guidelines on personal exposure and building contamination. Journal of Occupational and Environmental Hygiene. 2011;8(2):113–122. doi: 10.1080/15459624.2011.547454. [DOI] [PubMed] [Google Scholar]
- 36.Hendrix RW. Bacteriophages: evolution of the majority. Theoretical Population Biology. 2002;61(4):471–480. doi: 10.1006/tpbi.2002.1590. [DOI] [PubMed] [Google Scholar]
- 37.Hendrix RW, Smith MCM, Burns RN, Ford ME, Hatfull GF. Evolutionary relationships among diverse bacteriophages and prophages: all the world’s a phage. Proceedings of the National Academy of Sciences of the United States of America. 1999;96(5):2192–2197. doi: 10.1073/pnas.96.5.2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Abedon ST. Communication among phages, bacteria and soil environments. In: Witzany G, editor. Biocommunication in Soil Microorganisms. Heidelberg, Germany: Springer; 2011. pp. 37–65. [Google Scholar]
- 39.Zheng C, Wang G, Liu J, Song C, Gao H, Liu X. Characterization of the major capsid genes (g23) of T4-type bacteriophages in the wetlands of northeast China. Microbial Ecology. 2013;65(3):616–625. doi: 10.1007/s00248-012-0158-z. [DOI] [PubMed] [Google Scholar]
- 40.Prigent M, Leroy M, Confalonieri F, Dutertre M, DuBow MS. A diversity of bacteriophage forms and genomes can be isolated from the surface sands of the Sahara Desert. Extremophiles. 2005;9(4):289–296. doi: 10.1007/s00792-005-0444-5. [DOI] [PubMed] [Google Scholar]
- 41.Sulakvelidze A, Alavidze Z, Morris JGJr. Bacteriophage therapy. Antimicrobial Agents and Chemotherapy. 2001;45(3):649–659. doi: 10.1128/AAC.45.3.649-659.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Łusiak-Szelachowska M, Żaczek M, Weber- Dąbrowska B. Phage neutralization by sera of patients receiving phage therapy. Viral Immunology. 2014;27(6):1–10. doi: 10.1089/vim.2013.0128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Loc-Carrillo C, Abedon ST. Pros and cons of phage therapy. Bacteriophage. 2011;1(2):111–114. doi: 10.4161/bact.1.2.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chhibber S, Kaur T, Kaur S. Co-therapy using lytic bacteriophage and linezolid: effective treatment in eliminating methicillin resistant staphylococcus aureus (MRSA) from diabetic foot infections. PLoS ONE. 2013;8(2) doi: 10.1371/journal.pone.0056022.e56022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vinodkumar CS, Srinivasa H, Basavarajappa KG, Geethalakshmi S, Bandekar N. Isolation of bacteriophages to multi-drug resistant Enterococci obtained from diabetic foot: a novel antimicrobial agent waiting in the shelf. Indian Journal of Pathology and Microbiology. 2011;54(1):90–95. doi: 10.4103/0377-4929.77333. [DOI] [PubMed] [Google Scholar]
- 46.Biswas B, Adhya S, Washart P, et al. Bacteriophage therapy rescues mice bacteremic from a clinical isolate of vancomycin-resistant Enterococcus faecium . Infection and Immunity. 2002;70(1):204–210. doi: 10.1128/IAI.70.1.204-210.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Górski A, Borysowski J, Międzybrodzki R, Weber-Dąbrowska B. Bacteriophages in medicine. In: Mc Grath S, van Sinderen D, editors. Bateriophage: Genetics and Microbiology. Norfolk, UK: Academic Press; 2007. pp. 125–158. [Google Scholar]
- 48.Kutter E, de Vos D, Gvasalia G, et al. Phage therapy in clinical practice: treatment of human infections. Current Pharmaceutical Biotechnology. 2010;11(1):69–86. doi: 10.2174/138920110790725401. [DOI] [PubMed] [Google Scholar]
- 49.Hanlon GW. Bacteriophages: an appraisal of their role in the treatment of bacterial infections. International Journal of Antimicrobial Agents. 2007;30(2):118–128. doi: 10.1016/j.ijantimicag.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 50.Redmond C, Henderson I, Turnbull PCB, Bowen J. Phage from different strains of Bacillus anthracis . Salisbury Med Bull-Special Supplement. 1996;87:60–63. [Google Scholar]
- 51.McCloy EW. Studies on a lysogenic Bacillus strain. I. A bacteriophage specific for B. anthracis . Journal of Hygiene. 1951;49(2):114–125. doi: 10.1017/s0022172400015412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCloy Ew. Unusual behavior of a lysogenic bacillus strain. Journal of General Microbiology. 1951;5(3):14–15. [PubMed] [Google Scholar]
- 53.Brown ER, Cherry WB. Specific identification of Bacillus anthracis by means of a variant bacteriophage. The Journal of Infectious Diseases. 1955;96(1):34–39. doi: 10.1093/infdis/96.1.34. [DOI] [PubMed] [Google Scholar]
- 54.Negus D, Burton J, Sweed A, Gryko R, Taylor P. Poly-γ-D-glutamic acid capsule interferes with lytic infection of Bacillus anthracis by B. anthracis-specific bacteriophages. Applied and Environmental Microbiology. 2013;79(2):714–717. doi: 10.1128/AEM.02682-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Walter MH, Baker DD. Three Bacillus anthracis bacteriophages from topsoil. Current Microbiology. 2003;47(1):55–58. doi: 10.1007/s00284-002-3899-y. [DOI] [PubMed] [Google Scholar]
- 56.Ganz HH, Law C, Schmuki M, et al. Novel giant siphovirus from Bacillus anthracis features unusual genome characteristics. PLoS ONE. 2014;9(1) doi: 10.1371/journal.pone.0085972.e85972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nagy E. A highly specific phage attacking Bacillus anthracis strain Sterne. Acta Microbiologica Academiae Scientiarum Hungaricae. 1974;21(3-4):257–263. [PubMed] [Google Scholar]
- 58.Schuch R, Pelzek AJ, Kan S, Fischetti VA. Prevalence of Bacillus anthracis-like organisms and bacteriophages in the intestinal tract of the earthworm Eisenia fetida . Applied and Environmental Microbiology. 2010;76(7):2286–2294. doi: 10.1128/AEM.02518-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Henry M, Biswas B, Vincent L, et al. Development of a highly throughput assay for indirectly measuring phage growth using the OmniLog system. Bacteriophage. 2012;2(3):159–167. doi: 10.4161/bact.21440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Inal JM, Karunakaran KV. φ20, a temperate bacteriophage isolated from Bacillus anthracis exists as a plasmidial prophage. Current Microbiology. 1996;32(4):171–175. doi: 10.1007/s002849900030. [DOI] [PubMed] [Google Scholar]
- 61.Lee JH, Shin H, Ryu S. Characterization and comparative genomic analysis of bacteriophages infecting members of the Bacillus cereus group. Archives of Virology. 2014;159(5):871–884. doi: 10.1007/s00705-013-1920-3. [DOI] [PubMed] [Google Scholar]
- 62.Schofield DA, Westwater C. Phage-mediated bioluminescent detection of Bacillus anthracis . Journal of Applied Microbiology. 2009;107(5):1468–1478. doi: 10.1111/j.1365-2672.2009.04332.x. [DOI] [PubMed] [Google Scholar]
- 63.Watanabe T, Morimoto A, Shiomi T. The fine structure and the protein composition of gamma phage of Bacillus anthracis . Canadian Journal of Microbiology. 1975;21(11):1889–1892. doi: 10.1139/m75-275. [DOI] [PubMed] [Google Scholar]
- 64.Schuch R, Fischetti VA. Detailed genomic analysis of the Wβ and γ phages infecting Bacillus anthracis: implications for evolution of environmental fitness and antibiotic resistance. Journal of Bacteriology. 2006;188(8):3037–3051. doi: 10.1128/JB.188.8.3037-3051.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abshire TG, Brown JE, Ezzell JW. Production and validation of the use of gamma phage for identification of Bacillus anthracis . Journal of Clinical Microbiology. 2005;43(9):4780–4788. doi: 10.1128/JCM.43.9.4780-4788.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sozhamannan S, McKinstry M, Lentz SM, et al. Molecular characterization of a variant of Bacillus anthracis-specific phage AP50 with improved bacteriolytic activity. Applied and Environmental Microbiology. 2008;74(21):6792–6796. doi: 10.1128/AEM.01124-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nagy E, Ivanovics G. Association of probable defective phage particles with lysis by bacteriophage AP50 in Bacillus anthracis . Journal of General Microbiology. 1977;102(1):215–219. doi: 10.1099/00221287-102-1-215. [DOI] [PubMed] [Google Scholar]
- 68.Minakhin L, Semenova E, Liu J, et al. Genome sequence and gene expression of Bacillus anthracis bacteriophage Fah. Journal of Molecular Biology. 2005;354(1):1–15. doi: 10.1016/j.jmb.2005.09.052. [DOI] [PubMed] [Google Scholar]
- 69.Schuch R, Fischetti VA. The secret life of the anthrax agent Bacillus anthracis: bacteriophage-mediated ecological adaptations. PLoS ONE. 2009;4(8) doi: 10.1371/journal.pone.0006532.e6532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Fan H, Tong Y. Potential dual-use of bacteriophage in bioterrorism and biodefense. Journal of Bioterrorism and Biodefense. 2012;3(3) [Google Scholar]
- 71.Walter MH. Efficacy and durability of Bacillus anthracis bacteriophages used against spores. Journal of Environmental Health. 2003;66(1):9–15. [PubMed] [Google Scholar]
- 72.El-Arabi TF, Griffiths MW, She Y, Villegas A, Lingohr EJ, Kropinski AM. Genome sequence and analysis of a broad-host range lytic bacteriophage that infects the Bacillus cereus group. Virology Journal. 2013;10, article 48 doi: 10.1186/1743-422X-10-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chosewood LC, Wilson DE. Biosafety in Microbiological and Biomedical Laboratories (BMBL) 5th edition. U.S. Department of Health and Human Services, HHS Publication no. (CDC) 21-1112; 2009. [Google Scholar]
- 74.van Tongeren SP, Roest HIJ, Degener JE, Harmsen HJM. Bacillus anthracis-like bacteria and other B. cereus group members in a microbial community within the international space station: a challenge for rapid and easy molecular detection of virulent B. anthracis . PLoS ONE. 2014;9(6) doi: 10.1371/journal.pone.0098871.e98871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fasanella A, Di Taranto P, Garofolo G, et al. Ground Anthrax Bacillus Refined Isolation (GABRI) method for analyzing environmental samples with low levels of Bacillus anthracis contamination. BMC Microbiology. 2013;13, article 167 doi: 10.1186/1471-2180-13-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bell CA, Uhl JR, Hadfield TL, et al. Detection of Bacillus anthracis DNA by LightCycler PCR. Journal of Clinical Microbiology. 2002;40(8):2897–2902. doi: 10.1128/JCM.40.8.2897-2902.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schofield DA, Sharp NJ, Westwater C. Phage-based platforms for the clinical detection of human bacterial pathogens. Bacteriophage. 2012;2(2):105–283. doi: 10.4161/bact.19274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brown ER, Moody MD, Treece EL, Smith CW. Differential diagnosis of Bacillus cereus, Bacillus anthracis, and Bacillus cereus var. mycoides. Journal of Bacteriology. 1958;75(5):499–509. doi: 10.1128/jb.75.5.499-509.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Davison S, Couture-Tosi E, Candela T, Mock M, Fouet A. Identification of the Bacillus anthracisγ phage receptor. Journal of Bacteriology. 2005;187(19):6742–6749. doi: 10.1128/JB.187.19.6742-6749.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kan S, Fornelos N, Schuch R, Fischetti VA. Identification of a ligand on the Wip1 bacteriophage highly specific for a receptor on Bacillus anthracis . Journal of Bacteriology. 2013;195(19):4355–4364. doi: 10.1128/JB.00655-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Brigati J, Williams DD, Sorokulova IB, et al. Diagnostic probes for Bacillus anthracis spores selected from a landscape phage library. Clinical Chemistry. 2004;50(10):1899–1906. doi: 10.1373/clinchem.2004.038018. [DOI] [PubMed] [Google Scholar]
- 82.Wan J, Fiebor B, Chin BA. Landscape phage-based magnetostrictive biosensor for detecting Bacillus anthracis spores. Proceedings of the IEEE Sensors; 2005; Los Alamitos, Calif, USA. IEEE; pp. 1308–1311. [Google Scholar]
- 83.Petrenko VA, Vodyanoy VJ. Phage display for detection of biological threat agents. Journal of Microbiological Methods. 2003;53(2):253–262. doi: 10.1016/s0167-7012(03)00029-0. [DOI] [PubMed] [Google Scholar]
- 84.Huang S, Yang H, Lakshmanan RS, et al. Sequential detection of Salmonella typhimurium and Bacillus anthracis spores using magnetoelastic biosensors. Biosensors and Bioelectronics. 2009;24(6):1730–1736. doi: 10.1016/j.bios.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 85.Fu L, Li S, Zhang K, et al. Detection of Bacillus anthracis spores using phage-immobilized magnetostrictive milli/micro cantilevers. IEEE Sensors Journal. 2011;11(8):1684–1691. [Google Scholar]
- 86.Schuch R, Nelson D, Fischetti VA. A bacteriolytic agent that detects and kills Bacillus anthracis . Nature. 2002;418(6900):884–889. doi: 10.1038/nature01026. [DOI] [PubMed] [Google Scholar]
- 87.Rao SS, Mohan KVK, Nguyen N, et al. Peptides panned from a phage-displayed random peptide library are useful for the detection of Bacillus anthracis surrogates B. cereus 4342 and B. anthracis Sterne. Biochemical and Biophysical Research Communications. 2010;395(1):93–98. doi: 10.1016/j.bbrc.2010.03.145. [DOI] [PubMed] [Google Scholar]
- 88.Shabani A, Marquette CA, Mandeville R, Lawrence MF. Carbon microarrays for the direct impedimetric detection of Bacillus anthracis using Gamma phages as probes. Analyst. 2013;138(5):1434–1440. doi: 10.1039/c3an36830k. [DOI] [PubMed] [Google Scholar]
- 89.Cavallo J-D, Ramisse F, Girardet M, Vaissaire J, Mock M, Hernandez E. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis isolated in France between 1994 and 2000. Antimicrobial Agents and Chemotherapy. 2002;46(7):2307–2309. doi: 10.1128/AAC.46.7.2307-2309.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Athamna A, Athamna M, Abu-Rashed N, Medlej B, Bast DJ, Rubinstein E. Selection of Bacillus anthracis isolates resistant to antibiotics. Journal of Antimicrobial Chemotherapy. 2004;54(2):424–428. doi: 10.1093/jac/dkh258. [DOI] [PubMed] [Google Scholar]
- 91.Mohammed MJ, Marston CK, Popovic T, Weyant RS, Tenover FC. Antimicrobial susceptibility testing of Bacillus anthracis: comparison of results obtained by using the National Committee for Clinical Laboratory Standards broth microdilution reference and etest agar gradient diffusion methods. Journal of Clinical Microbiology. 2002;40(6):1902–1907. doi: 10.1128/JCM.40.6.1902-1907.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Habrun B, Racic I, Kompes G, et al. The antimicrobial susceptibility and virulence factors of Bacillus anthracis strains isolated in Croatia. Veterinarni Medicina. 2011;56(1):22–27. [Google Scholar]
- 93.Rusul G, Yaacob NH. Prevalence of Bacillus cereus in selected foods and detection of enterotoxin using TECRA-VIA and BCET-RPLA. International Journal of Food Microbiology. 1995;25(2):131–139. doi: 10.1016/0168-1605(94)00086-l. [DOI] [PubMed] [Google Scholar]
- 94.Kiyomizu K, Yagi T, Yoshida H, et al. Fulminant septicemia of Bacillus cereus resistant to carbapenem in a patient with biphenotypic acute leukemia. Journal of Infection and Chemotherapy. 2008;14(5):361–367. doi: 10.1007/s10156-008-0627-y. [DOI] [PubMed] [Google Scholar]
- 95.LaForce FM. Anthrax. Clinical Infectious Diseases. 1994;19(6):1009–1014. doi: 10.1093/clinids/19.6.1009. [DOI] [PubMed] [Google Scholar]
- 96.Friedlander AM, Little SF. Advances in the development of next-generation anthrax vaccines. Vaccine. 2009;27(4) supplement 5:D28–D32. doi: 10.1016/j.vaccine.2009.08.102. [DOI] [PubMed] [Google Scholar]
- 97.Ivins BE, Pitt MLM, Fellows PF, et al. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine. 1998;16(11-12):1141–1148. doi: 10.1016/s0264-410x(98)80112-6. [DOI] [PubMed] [Google Scholar]
- 98.Fellows PF, Linscott MK, Ivins BE, et al. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine. 2001;19(23-24):3241–3247. [Google Scholar]
- 99.BioThrax (Anthrax Vaccine Adsorbed) Emergent BioSolutions. June 2014, http://www.fda.gov/downloads/BiologicsBloodVaccines/BloodBloodProducts/ApprovedProducts/LicensedProductsBLAs/UCM074923.pdf.
- 100.Turnbull PCB. Anthrax vaccines: past, present and future. Vaccine. 1991;9(8):533–539. doi: 10.1016/0264-410x(91)90237-z. [DOI] [PubMed] [Google Scholar]
- 101.Rockefeller JD, de Concini M, Mitchell GJ, et al. Is military research hazardous to veterans’ health? Lessons spanning half a century. A staff report prepared for the Committee on Veterans’ Affairs. Proceedings of the 103rd Congress, 2nd Session—Committee Print; 1994; United States Senate; pp. 103–197. [Google Scholar]
- 102.Savransky V, Sanford DC, Syar E, et al. Pathology and pathophysiology of inhalational anthrax in a guinea pig model. Infection and Immunity. 2013;81(4):1152–1163. doi: 10.1128/IAI.01289-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis . Infection and Immunity. 1986;51(3):795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cowles PB, Hale MW. Effect of bacteriophage on experimental anthrax in white mice. Journal of Infectious Diseases. 1931;49(3):264–269. [Google Scholar]
- 105.Scorpio A, Chabot DJ, Day WA, et al. Poly-γ-glutamate capsule-degrading enzyme treatment enhances phagocytosis and killing of encapsulated Bacillus anthracis . Antimicrobial Agents and Chemotherapy. 2007;51(1):215–222. doi: 10.1128/AAC.00706-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tišáková L, Godány A. Bacteriophage endolysins and their use in biotechnological processes. Journal of Microbiology, Biotechnology and Food Sciences. 2014;3(2):164–170. [Google Scholar]
- 107.Porter CJ, Schuch R, Pelzek AJ, et al. The 1.6 A crystal structure of the catalytic domain of PlyB, a bacteriophage lysin active against Bacillus anthracis . Journal of Molecular Biology. 2007;366(2):540–550. doi: 10.1016/j.jmb.2006.11.056. [DOI] [PubMed] [Google Scholar]
- 108.Son B, Yun J, Lim J, Shin H, Heu S, Ryu S. Characterization of LysB4, an endolysin from the Bacillus cereus-infecting bacteriophage B4. BMC Microbiology. 2012;12, article 33 doi: 10.1186/1471-2180-12-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Koper OB, Klabunde JS, Marchin GL, Klabunde KJ, Stoimenov P, Bohra L. Nanoscale powders and formulations with biocidal activity toward spores and vegetative cells of Bacillus species, viruses, and toxins. Current Microbiology. 2002;44(1):49–55. doi: 10.1007/s00284-001-0073-x. [DOI] [PubMed] [Google Scholar]
- 110.Fu X, Walter MH, Paredes A, Morais MC, Liu J. The mechanism of DNA ejection in the Bacillus anthracis spore-binding phage 8a revealed by cryo-electron tomography. Virology. 2011;421(2):141–148. doi: 10.1016/j.virol.2011.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ahmed R, Sankar-Mistry P, Jackson S, Ackermann H, Kasatiya SS. Bacillus cereus phage typing as an epidemiological tool in outbreaks of food poisoning. Journal of Clinical Microbiology. 1995;33(3):636–640. doi: 10.1128/jcm.33.3.636-640.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lee JH, Shin H, Son B, Ryu S. Complete genome sequence of Bacillus cereus bacteriophage BCP78. Journal of Virology. 2012;86(1):637–638. doi: 10.1128/JVI.06520-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Cairns BJ, Payne RJH. Bacteriophage therapy and the mutant selection window. Antimicrobial Agents and Chemotherapy. 2008;52(12):4344–4350. doi: 10.1128/AAC.00574-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lee W-J, Billington C, Hudson JA, Heinemann JA. Isolation and characterization of phages infecting Bacillus cereus . Letters in Applied Microbiology. 2011;52(5):456–464. doi: 10.1111/j.1472-765X.2011.03023.x. [DOI] [PubMed] [Google Scholar]
- 115.Shin H, Lee JH, Park J. Characterization and genome analysis of the Bacillus cereus-infecting bacteriophages BPS10C and BPS13. Archives of Virology. 2014;159(8):2171–2175. doi: 10.1007/s00705-014-2030-6. [DOI] [PubMed] [Google Scholar]
- 116.Grose JH, Jensen JD, Merrill BD. Genome sequences of three novel Bacillus cereus bacteriophages. Genome Announcements. 2014;2(1) doi: 10.1128/genomeA.01118-13.01118-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yuan Y, Peng Q, Gao M. Characteristics of a broad lytic spectrum endolysin from phage BtCS33 of Bacillus thuringiensis . BMC Microbiology. 2012;12, article 297 doi: 10.1186/1471-2180-12-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Bourguet FA, Souza BE, Hinz AK, Coleman MA, Jackson PJ. Characterization of a novel lytic protein encoded by the Bacillus cereus E33L gene ampD as a Bacillus anthracis antimicrobial protein. Applied and Environmental Microbiology. 2012;78(8):3025–3027. doi: 10.1128/AEM.06906-11. [DOI] [PMC free article] [PubMed] [Google Scholar]


