Abstract
Little is known about the relationship between traumatic head injury (THI) and psychiatric morbidity in torture survivors. We examine the relationship between THI and depression, PTSD, post-concussive syndrome (PCS), disability and poor health status in Vietnamese ex-political detainees who survived incarceration in Vietnamese re-education camps. A community sample of ex-political detainees (n=337) and a non-THI, non-ex-detainee comparison group (n=82) were surveyed. 78% of the ex-political detainees had experienced THI. 90.6% of the ex-political detainees and 3.6% of the comparison group had experienced 7 or more trauma events. Depression and PTSD were greater in ex-detainees than the comparison group (40.9% vs 23.2% and 13.4% vs 0%). Dose-effect relationships for THI and trauma/torture in the ex-political detainee group were significant. Logistic regression in the pooled sample of ex-detainees and the comparison group confirmed the independent impact of THI from trauma/torture on psychiatric morbidity (OR for PTSD=22.4; 95% CI: 3.0-165.8). These results demonstrate important effects of THI on depression and PTSD in Vietnamese ex-detainees who have survived torture.
Keywords: THI, traumatic brain injury, PTSD, depression, Vietnamese, ex-political detainees
Traumatic head injury (THI) is a common form of torture and human degradation that occurs during war and other forms of mass violence. Thygesen, Hermann and Willanger [1] demonstrated significant neurological and psychiatric morbidity in concentration camp survivors associated with the most commonly reported torture, blows and kicks to the head. Clinical studies have documented chronic neuropsychiatric findings in torture survivors including cerebral atrophy. [2] Rasmussen [3] found that 64% (N=200) of torture survivors revealed neurological impairments (2/3 with head injury). Other studies of torture survivors and survivors of mass violence have linked psychiatric symptoms, neurological impairment, and traumatic brain injury (TBI). [4-8]
Very little research has been conducted that establishes the relationship between THI and psychiatric disorders such as depression and posttraumatic stress disorder (PTSD) and related physical disability and health status in tortured persons. [9] A study of refugee survivors of torture with self-reported head injury found an increased risk of negative physical consequences among those with possible TBI. [10] A recent review of the literature in non-torture survivors concluded that there is significant overlap between TBI and PTSD, mild TBI may increase a person's risk for PTSD, and stress reactions following mild TBI rather than any neurological damage itself might be a key contributor to impairment. [11] In a random sample of U.S. Vietnam-era veterans in the community, mild TBI sustained after military discharge was associated with higher rates of headaches, memory and sleep problems and was found to prolong or complicate recovery from pre-existing PTSD. [12] Depression was found to be common in TBI rehabilitation patients aged 16 or older, and to be associated with worsening of quality of life and participation in society. [13] Mild TBI and ongoing stressors increased the risk of developing delayed symptoms of PTSD in a hospitalized sample. [14]
Systematic, well-designed studies of the impact of THI on the physical and mental health of traumatized persons who have experienced extreme violence are urgently needed so that affected individuals can be appropriately identified and treated. [15-16] Manley and Mass [17] call for a broad-based multidisciplinary effort focused on longitudinal investigations of TBI's natural history, the underlying TBI biology and mechanisms, risk factors, and developing effective treatment approaches.
Our group was in an ideal situation to conduct a community study of torture survivors exposed to THI. The Harvard Program in Refugee Trauma (HPRT) has worked with Indochinese survivors of torture and mass violence since 1981. [18] Between July 1990 and 1992, HPRT with its Vietnamese community partner, the Vietnamese American Civic Association (VACA), conducted the first study of Vietnamese ex-political detainees resettled in the United States. [19] These political prisoners had been severely tortured in Vietnamese re-education camps and subjected to THI. [20-21]
In our present large-scale community study, we describe the prevalence of THI, the relationship between THI and other related forms of psychiatric morbidity, PCS, functional disability, and poor health status in a population that has experienced extreme violence. A dose-effect relationship between THI and trauma/torture events was also examined. We tested our hypothesis that effects of THI in Vietnamese torture survivors would be independent of non-THI trauma/torture events in their relationship to depression and PTSD. We have already reported on the brain structural abnormalities found in a subsample of this study associated with THI. [22] The study conducted by Hoge et al. [23] on the relationship between mild THI to PTSD and depression in Iraqi veterans returning home further supports our tentative hypotheses related to the mental health impact of THI in Vietnamese ex-political detainees.
Methods
Study population and procedures
The study population included a sample of Vietnamese ex-political detainees resettled in the greater Boston area and a comparison group. We conducted a complete census of 419 ex-political detainees and comparison participants that had received services at VACA. Ex-political detainees were only recruited if they came into the United States under the U.S. Department of State's Humanitarian Operations program for resettling Vietnamese ex-political detainees. Participants were randomly ordered prior to being contacted to avoid selection bias.
Additional recruitment procedures included: (1) a “snowball” approach in which current ex-political detainees were asked to pass on recruitment information to friends and acquaintances, (2) VACA counselors contacted past ex-political detainee clients, (3) a public announcement in Vietnamese in the local Vietnamese newspapers, and (4) a flyer/poster in Vietnamese that was distributed to family and friends of potential ex-political detainees at churches and pagodas.
A comparison group was recruited from VACA's client population. Subjects were men greater than 45 years of age with no history of head injury. Based on our pilot study experience, we knew that it would be impossible to find a non-traumatized Vietnamese control group. Exclusion criteria for both groups included institutionalization, hospitalization, and gross medical or neurological disease. Initial recruitment screens were conducted in Vietnamese by trained VACA staff via telephone. Fifteen percent of potential study participants from both cohorts refused to participate or were ineligible.
Interviews took approximately 2 hours and were administered in Vietnamese by VACA's professional staff. All research staff were trained in human subjects protection according to the standardized protocol of the Massachusetts General Hospital. The Human Subjects Review Committee of the Massachusetts General Hospital approved informed consent and study design. All subjects participated with informed, voluntary, written consent and the research was completed in accordance with the Helsinki Declaration.
Instruments
The survey instrument was expanded and adapted from our pilot study [19] to construct a valid Vietnamese version of the final questionnaire using standard methods of cross-cultural research. [24-25] Data on risk factors, including personal history, military and wartime work experience, re-education camp experience, migration and resettlement experience, stressful life events, trauma, torture, and head injury were collected.
A detailed THI history questionnaire included a checklist of 24 types of THI events including vehicular accident, accidental falls, physical assaults, and combat-related THI. Since self-report of THI is presumptive evidence for TBI, three other TBI events were included in the THI survey which are known to be associated with potential brain injury in torture survivors (i.e., suffocation, drowning and strangulation). [9,26] Each THI event, associated neurological symptoms, and loss of consciousness was assessed: 1) Before the Vietnam War (before 1954); 2) During the Vietnam War (1954-1975); 3) In Re-education Camp (ex-political detainees only); 4) In Vietnam after the war or the re-education camp; and 5) After leaving Vietnam and resettling in the United States.
The trauma history was derived from the Vietnamese version of the Harvard Trauma Questionnaire (HTQ). [27] Measures of cumulative trauma were constructed from responses to questions about trauma events during: 1) the Vietnam War (1954-1975); 2) Re-education Camp (ex-political detainees only); and 3) Other times. Affirmative responses were summed for 40 non-THI trauma events and 27 torture events.
Outcome measures included the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [28] symptoms of depression and PTSD, functional disability, symptoms of post-concussive syndrome, self-reported general health status, chronic medical condition and physical disabilities.
Psychological symptoms were measured using a 15-item section of the Hopkins Symptom Checklist – 25 (HSCL-25) measuring depressive symptoms [29] and a 16-item section of the HTQ [27] made up of 16 of the 17 diagnostic criteria for PTSD in DMS-IV. Respondents were asked whether they were bothered by each symptom “not at all” (1), “a little” (2), “quite a bit” (3), or “extremely” (4) in the past week. Both instruments have been widely translated and used in a number of studies among diverse cultural groups [30-34] and validated against clinical diagnoses. [27,35-38]
Scale cut-off points for the HSCL-25 and HTQ for depression and PTSD are greater than or equal to 1.75 and 2.50, respectively. [35,38-39]
Functional disability was measured using the six item physical functioning scale of the Medical Outcomes Study 20-Item Short-Form Health Survey (MOS SF-20), which has been tested for its reliability and validity in a large number of disease settings, countries, and languages. [40-42] A World Health Organization (WHO) physical functioning scale, [43] a measure of perceived energy level, [44] and a measure of self-perceived health [45] and the Medical Outcome Study Short Form (MOS SF-8) were included. [46]
The self-report of general health status used in our multivariate analyses correlated moderately to strongly (0.44 to 0.49) with our WHO survey measures of health status (i.e., health/energy for work, recreation, and education/training). The general health item correlated 0.43 with normed mental health SF-8 and 0.62 with normed physical health SF-8 (norms are with general US population, mean = 50, SD=10).
The self-reported presence of 25 chronic medical conditions (e.g. high blood pressure) and 6 chronic physical disabilities (e.g. blind in 1 or both eyes) were assessed. A six item scale from the MOS SF-20 measured limitations in physical functioning due to health on a 3-point scale (1, limited for more than 3 months; 2, limited for 3 months or less; and 3, not limited at all). The item responses were summed and then transformed linearly to a 0 (poorest physical functioning) through 100 (no limitations in physical functioning) scale.
A dichotomous variable from the 100-point functional impairment scale was created for the logistic regression analysis. The cutoff point of 50 was selected as a conservative estimate of functional disability (lower than the 91.7 used by Stewart et al. [40] which would have classified 86% of our respondents as functionally impaired).
The post-concussive symptom scale (PC Symptom Scale) was adapted from Cicerone and Kalmar. [47] There are 22 items representing four clusters of symptoms, physical (somatic), cognitive, affective, and sensory. We asked how much of the time the symptoms bothered the participants on a 4-point Likert scale (0=not at all, 1=some of the time, 2=most of the time, 3=all of the time) during the last 2 weeks. The median number of symptoms experienced in our sample was 12 (inter-quartile range [IQR]=5-17, maximum=22).
For analysis of post-concussive symptoms, the PC Symptom Scale summed the 22 item scores with the maximum possible score of 66. For the logistic analyses, we considered a participant to have post-concussive syndrome if he scored above the median of all study participants (> 15; in our sample of n=433, the inter-quartile range of the sum of items scored was 6-23 and the maximum score was 55). Scales proved valid, with split-half reliability (Cronbach alpha) on standardized scores of 0.84 (MOS), 0.92 (HSCL for depression), 0.94 (HTQ for PTSD) and 0.95 (PC Symptom Scale for post-concussive symptoms).
Inter-rater reliability was computed for all survey items from the outcome scales in 28 quality control interviews that were conducted in the presence of an independent observer. We found 100% agreement for most items. The simple kappa exceeded 0.91 and the weighted kappa statistic exceeded 0.94 for all items in the depression, HTQ, MOS and post-concussive scales. The kappa for the categorized trauma and torture variables (none, first-4th quartiles) exceeded 0.84 (weighted kappas exceeded 0.90). Kappas for the dichotomized torture and trauma summary scores (none vs. any) exceeded 0.84 for simple and 0.90 for weighted kappas. Kappas for the case definition of depression, PTSD and disability exceeded 0.92.
We considered a participant to be head-injured if they reported at least one head injury during any time period. The total number of different types of THI events were counted for all time periods and each type of THI event was weighted by its actual frequency and the weighted frequencies were then summed up for all time periods. Only the number of different types of non-THI trauma and torture were counted relative to each time period. In spite of our initial screen, some members of the comparison group self-reported head injuries (n=14) and were eliminated as comparison subjects. Neuroimaging results, reported elsewhere, confirmed that participants were classified accurately as head-injured or not. [22]
Statistical Methods
Differences between the ex-political detainees and comparison group were described using chi-square tests, non-parametric Wilcoxon rank sum tests, and t-tests. We analyzed the independent effect of THI on depression and PTSD in ex-political detainees. The ex-political detainees were categorized into groups based on a median split or quartiles according to the frequency of trauma/torture events and THI events. Linear dose-response effects were evaluated using trend analysis of quartiles.
Because all of the Vietnamese subjects studied have been traumatized, we explored whether or not THI increases the risk of poor psychiatric or health outcome independently from trauma and torture experience through a series of multiple logistic regression analyses on the pooled sample, combining all survey respondents. [48] First, we estimated the unadjusted odds ratio of poor psychiatric or health outcome for those head injured versus not head-injured participants. Secondly, we adjusted the odds ratios for marital status (married vs. not), age at interview, years of education received in Vietnam, the number of years in the USA and living situation (alone vs. not). Thirdly, we analyzed the separate impact of head injury versus trauma and torture experience, with a dichotomized indicator of any traumatic event (one covariate representing any torture or trauma experience). Finally, we assessed the effect of the number of types of trauma events, torture events and the number of head injuries, including a single degree of freedom interaction term between any traumatic event and any THI.
All analyses were performed with SAS statistical analysis software, version 8.2 and tests were considered to be significant if p < 0.05. [49-50]
Results
A total of 337 Vietnamese ex-political detainees and 82 members of the comparison group aged 45 years of age and older were included in this analysis. Table 1 provides basic characteristics and comparison of both respondent groups. The ex-political detainees were primarily between the ages of 45 and 65, while the comparison subjects were either younger than 55 or older than 65 years of age. Participants in the comparison group had less education; otherwise the basic demographic characteristics were comparable. Depression and PTSD were greater in ex-detainees.
Table 1. Demographic Characteristics of Survey Respondents: Vietnamese Comparison Group and Ex-Political Detainees.
| Characteristic | Comparison Group (N = 82) | Detainees (N = 337) | P-value | ||
|---|---|---|---|---|---|
| Gender – Male – N (%) | 82 | (100) | 337 | (100) | n/a |
| Age, y – Mean (SD) | 62.4 | (11.2) | 60.5 | (7.4) | 0.16‡ |
| 45-55 | 26 | 31.7% | 80 | 23.7% | 0.21† |
| >55-60 | 9 | 11.0% | 107 | 31.8% | |
| >60-65 | 12 | 14.6% | 72 | 21.4% | |
| >65 | 35 | 42.7% | 78 | 23.1% | |
| Years in USA – Mean (SD) | 11.6 | (8.0) | 9.5 | (4.3) | 0.02*‡ |
| Citizenship | |||||
| No | 39 | 47.6% | 79 | 23.4% | <0.001* |
| Yes | 43 | 52.4% | 258 | 76.6% | |
| Marital Status | |||||
| Currently Married | 62 | 75.6% | 269 | 79.8% | 0.01* |
| Separated, Divorced | 8 | 9.8% | 45 | 13.4% | |
| Widowed | 4 | 4.9% | 16 | 4.7% | |
| Never Married | 8 | 9.8% | 7 | 2.1% | |
| Religion | |||||
| Buddhist | 50 | 61.0% | 191 | 56.7% | 0.25 |
| Christian | 18 | 22.0% | 103 | 30.6% | |
| Other | 14 | 17.0% | 43 | 12.8% | |
| Living Alone | |||||
| No | 71 | 86.6% | 293 | 86.9% | 0.93 |
| Yes | 11 | 13.4% | 44 | 13.1% | |
| Education (y) | |||||
| 1-8 | 39 | 47.6% | 46 | 13.6% | <0.001*† |
| 9-12 | 34 | 41.5% | 226 | 67.1% | |
| ≥13 | 9 | 11.0% | 65 | 19.3% | |
| Someone to rely on for support in USA+ | |||||
| No | 19 | 23 2% | 76 | 22 7% | 0 93 |
| Yes | 63 | 76 8% | 259 | 77 3% | |
|
| |||||
| English Language Ability | |||||
| Moderately or Very Well | 30 | 36 6% | 154 | 45 7% | 014 |
| Little or Not at all | 52 | 63 4% | 183 | 54 3% | |
| Currently Employed | |||||
| No | 55 | 67 1 % | 248 | 73 6% | 0 24 |
| Yes | 27 | 32 9% | 89 | 26 4% | |
| Employed in last years (current or past) | |||||
| No | 38 | 46 3% | 197 | 58 5% | 0 05 |
| Yes | 44 | 53 7% | 140 | 41 5% | |
|
| |||||
| Prevalence of Depression & PTSD | |||||
|
| |||||
| Depression | |||||
| No | 63 | 76 8% | 199 | 59 1 % | 0 003* |
| Yes | 19 | 23 2% | 138 | 40 9% | |
|
| |||||
| PTSD | |||||
| No | 82 | 100% | 292 | 86 6% | <0 001** |
| Yes | 0 | 0% | 45 | 13 4% | |
2-sided Wilcoxon rank-sum test (normal approximation)
2-sided Student's t-test (unequal variances)
p< 0.05,
p < 0.001
2 ex - detainees with missing data
Unless indicated, p-values were for Pearson Chi Square test.
Secondary to the design of the survey, the comparison group had never been in a reeducation camp. The ex-political detainees lived an average of 6.5 years in a communist reeducation camp (Table 2). The comparison group had experienced less trauma and torture; some comparison group members reported torture (N=20, 24%) although most reported fewer than 4 events (N=17). A considerable number had been traumatized (N=52; 63%). The common occurrence of trauma and torture related to the Vietnam War found in Vietnamese resettled in the United States is similar to that shown in our previous pilot study. [19] In contrast, nearly all of the ex-political detainees had experienced traumatic events and they reported higher levels of cumulative torture (e.g. N=97, 29%, with more than 10 torture events) and trauma (e.g. N=105, 31%, with more than 15 trauma events).
Table 2. Trauma, Torture and Head Injury Characteristics of Survey Respondents: Vietnamese Comparison Group and Ex-Political Detainees.
| Characteristic | Comparison Group (N =82) |
Detainees (N = 337) |
P-value | |||
|---|---|---|---|---|---|---|
| Time in re-education camp (years) | ||||||
| Mean (SD)a | 0 | 6.5 | (3.6) | n/a | ||
| Median (IQ Range) | 0 | 6.4 | (4.9, 8.1) | n/a | ||
| Number of torture events | ||||||
| Median (IQ Range) | 0 | (0, 0) | 7 | (5, 11) | ||
| 0 torture events | 62 | 75.6% | 3 | 0.9% | <0.001 † | |
| 1-3 torture events | 17 | 20.7% | 37 | 11.0% | ||
| 4-6 torture events | 3 | 3.7% | 109 | 32.3% | ||
| 7-10 torture events | 0 | 0 | 91 | 27.0% | ||
| More than 10 torture events | 0 | 0 | 97 | 28.8% | ||
| Number of Trauma Events | ||||||
| Median (IQ Range) | 1 | (0, 3) | 13 | (10, 16) | ||
| 0 trauma events | 30 | 36.6% | 1 | 0.3% | <0.001 † | |
| 1-6 trauma events | 49 | 59.8% | 31 | 9.2% | ||
| 7-11 trauma events | 2 | 2.4% | 104 | 30.9% | ||
| 12-15 trauma events | 1 | 1.2% | 96 | 28.5% | ||
| More than 15 trauma events | 0 | 0% | 105 | 31.2% | ||
| Any head injury | ||||||
| No | 82 | 100% | 74 | 22.0% | <0.001* | |
| Yes | 0 | 0% | 263 | 78.0% | ||
| Any loss of consciousness associated with head injury | n/a | N=263b | ||||
| No | 79 | 30.2% | n/a | |||
| Yes | 183 | 69.8% | ||||
Notes:
95% CI for mean years in camp is: 6.1, 6.9
1 participant had unknown LOC value.
p < 0.05
2-sided Wilcoxon rank-sum test (normal approximation)
Unless indicated, p-values were for Pearson Chi Square test.
As per study design, no members of the comparison admitted to THI, while THI among ex-political detainees was common (78%, N=263). This was confirmed by neuroimaging. [22] Consistent with presumptive evidence of TBI, 70% (N=183) of all participants with THI had unconsciousness associated with their THI events.
Table 3 demonstrates the shift from combat related THI during the Vietnam War to beatings to the head and suffocation during the re-education camp experience in the ex-political detainees. There is dramatic fall off in THI events post re-education camps, with vehicle accidents and falls presenting as the most common cause of THI after leaving Vietnam.
Table 3. Head Injury Experiences of the Vietnamese Ex-Political Detainees by time period (N=337).
| During War (1954-1975) | Re-Education | In VN after War or after Re-Education | After Leaving VN | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| N | % | N | % | N | % | N | % | ||||
| Explosion | 154 | 45.7 | Beaten on head | 56 | 16.6 | Fall for other reason | 7 | 2.1 | Hit head against dash | 14 | 4.2 |
| Shrapnel | 58 | 17.2 | Near Suffocation | 43 | 12.8 | Beaten on head | 4 | 1.2 | Fall for other reason | 12 | 3.6 |
| Fall from vehicle | 35 | 10.4 | Fall from fatigue | 28 | 8.3 | Fall from vehicle | 3 | 0.9 | Whiplash* | 7 | 2.1 |
| Fall for other reason | 21 | 6.2 | Fall for other reason* | 14 | 4.2 | Unexplained fainting, LOC+* | 2 | 0.6 | Fall from fatigue | 7 | 2.1 |
| Beaten on head | 9 | 2.7 | Fainting, LOC*+ | 12 | 3.6 | Fall from fatigue | 2 | 0.6 | Unexplained fainting, LOC*+ | 7 | 2.1 |
| Shot in head | 7 | 2.1 | Work accident | 12 | 3.6 | Near Suffocation | 2 | 0.6 | Beaten on head | 3 | 0.9 |
| Hit head on dash | 6 | 1.8 | Explosion | 4 | 1.2 | Work accident | 3 | 0.9 | |||
|
|
|||||||||||
| Near drowning | 5 | 1.5 | Hit on head during escape | 2 | 0.6 | Fall from vehicle | 2 | 0.6 | |||
| Near strangulation | 3 | 0.9 | Near strangulation | 2 | 0.6 | Near suffocation | 2 | 0.6 | |||
|
|
|||||||||||
| Near Suffocation | 2 | 0.6 | Near drowning | 2 | 0.6 | ||||||
|
| |||||||||||
| Also 1 each: Hit by vehicle; whiplash*, fall from fatigue; other head injury | Also 1 each: Fall out of vehicle, hit by vehicle, whiplash* | Also 1 each: Hit head against dash, Other head injury, Drowning. | Also 1 each: Hit by vehicle, Other head injury, Near strangulation | ||||||||
Note: There were reports of 10 events during the period prior to 1954: Falls for other reasons (4); Other head injury (2); Drowning (2); Fall out of vehicle (1), Unexplained fainting or LOC (1).
Note:
1-3 missing values not counted in denominator
Note:
Unexplained fainting or LOC was not counted as head injury event in analysis
Table 4 shows summary data on the types and frequency of THI events for the ex-political detainees across time periods. Combat and human rights violation-related THI were most common with explosion (158; 47%), beatings to the head (68; 20%) and shrapnel head injury (58; 17%), the most common THIs. About one fourth (N=74; 22%) of the ex-political detainees had no THI events. Of those reporting any THI (N=162), 58% had 2 or more events and 26% (n=73) had 3 or more.
Table 4. The Number and Percent of Vietnamese Ex-Political Detainees Reporting Each Type of Head Injury Across Time.
| Type of Head Injury | Ex-Political Detainees (N=337) | |
|---|---|---|
|
| ||
| N | % | |
| Explosion | 158 | 46.88 |
| Beaten on head | 68 | 20.18 |
| Shrapnel | 58 | 17.21 |
| Fall for other reason | 55 | 16.32 |
| Suffocation | 47 | 13.95 |
| Fall out of vehicle | 40 | 11.87 |
| Fall from fatigue | 36 | 10.68 |
| Hit head against dashboard | 19 | 5.64 |
| Work accident | 15 | 4.45 |
| Drowning | 9 | 2.67 |
| Whiplash | 9 | 2.67 |
| Shot in head | 7 | 2.08 |
| Strangulation | 6 | 1.78 |
| Other head injury | 5 | 1.48 |
| Hit by vehicle | 3 | 0.89 |
| Hit head while trying to escape from camp | 2 | 0.59 |
Table 5 shows the additive effect of THI events and trauma/torture events on depression and PTSD. Figure 1 reveals the interaction effect between THI events and trauma/torture events on the risks of having psychiatric disorders. Psychiatric disorders were more prevalent and the risk for psychiatric disorders increased more steeply in response to the trauma/torture exposure in the ex-detainees with THI events.
Table 5. Additive Effects of Trauma/Torture Events and Traumatic Head Injury events on Depression and PTS D in Ex-Political Detainees.
| Depression | PTSD | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Symptom Class | N | Number (%) Defined as Case | Odds Ratio (95% CI) a | N | Number (%) Defined as cases | Odds ratio (95% CI) a |
| Traumatic Head Injury Events | ||||||
| 0-2 THI | 170 | 46 (27.1%) | 1.0 | 166 b | 8 (4.82%) | 1.0 |
| ≥3 THI | 167 | 92 (55.1%) | 3.35 (2.09 to 5.35) d | 167 | 37 (22.16%) | 3.35 (2.09 to 5.35) d |
| Other Trauma/Torture Events | ||||||
| 0-13 trauma/torture events | 75 | 15 (20.0%) | 1.0 | 73 b | 0 (0%) | NA |
| 14-18 trauma/torture events | 81 | 21 (25.9%) | 1.51 (0.69 to 3.33) | 81 | 2 (2.47%) | 1.0 |
| 19-25 trauma/torture events | 74 | 37 (50.0%) | 4.25 (1.98 to 9.10) d | 74 | 11 (14.86%) | 7.59 (1.54 to 37.35) c |
| ≥26 trauma/torture events | 88 | 54 (61.4%) | 7.70 (3.61 to 16.4) d | 88 | 29 (32.95%) | 24.90 (5.18 to 119.84) d |
| Interaction between Trauma/Torture and Traumatic Head Injury Events | ||||||
| 0-2 THI (1-13 trauma/torture) | 65 | 13 (20.0%) | 1.0 | 63 | 0 (0%) | NA |
| 0-2 THI (14-18 trauma/torture) | 46 | 10 (21.7%) | 1.28 (0.49 to 3.38) | 46 | 0 (0%) | NA |
| 0-2 THI (19-25 trauma/torture) | 37 | 14 (37.9%) | 2.56 (1.00 to 6.56) c | 37 | 3 (8.1%) | 1.0 |
| 0- 2 THI (>26 trauma/torture) | 16 | 7 (43.8%) | 3.59 (1.07 to 12.06) c | 16 | 5 (31.3%) | 6.48 (1.26 to 33.18) c |
| ≥3 THI (1-13 trauma/torture) | 10 | 2 (20.0%) | 0.91 (0.16 to 5.25) | 10 | 0 (0%) | NA |
| ≥3 THI (14-1 8 trauma/torture) | 35 | 11 (31.4%) | 1.83 (0.68 to 4.89) | 35 | 2 (5.7%) | 0.56 (0.083 to 3.80) |
| ≥3 THI (19-25 trauma/torture | 37 | 23 (62.2%) | 6.85 (2.68 to 17.49) d | 37 | 8 (21.6%) | 3.18 (0.75 to 13.39) |
| ≥3 THI (>26 trauma/torture) | 72 | 47 (65.3%) | 9.06 (3.98 to 2 to .62) d | 72 | 24 (33.3%) | 6.48 (1.75 to 24.03) c |
Abbreviations: PTSD, posttraumatic stress disorder; CI, confidence interval; NA, not applicable.
Adjustment was performed using multiple logistic regression with covariates for marital status (married vs. not married), age at interview, education in Vietnam, current living status (with spouse or children vs. other situations), and years in USA.
Subjects of no trauma exposure were excluded in producing PTSD odds ratio.
p<0.05,
p<0.001.
Cases with any missing items on trauma and torture evaluation were excluded.
Figure 1. Frequency of Traumatic Head Injury Events and Trauma/Torture Events Associated with Psychiatric Disorders.
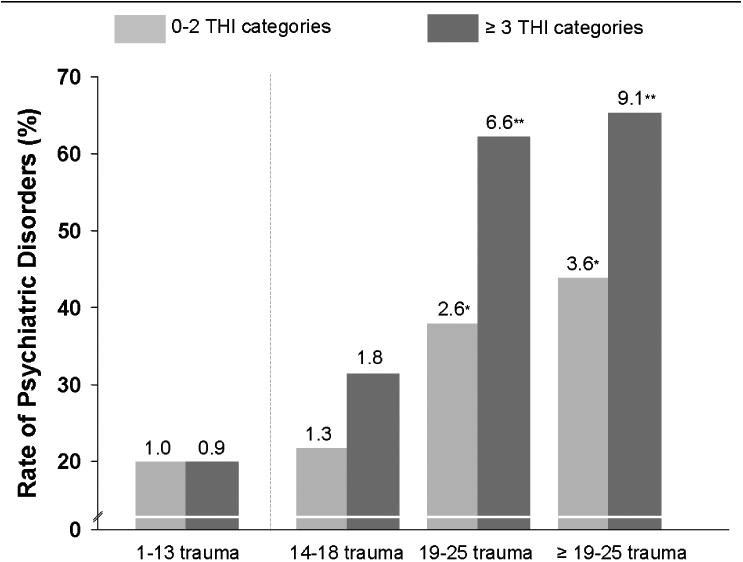
Abbreviation: THI, traumatic head injury.
Cases with any missing items on trauma and torture evaluation were excluded.
Traumatic head injury events, which include both the type and frequency information, were categorized into two groups of bitiles. Trauma/torture events were categorized into quartiles.
Subjects of no trauma exposure were excluded in producing PTSD odds ratio.
Adjustment was performed using multiple logistic regression with covariates for marital status (married vs. not married), age at interview, education in Vietnam, current living status (with spouse or children vs. other situations) and years in USA.
Associated increases in risk of depression are shown at the top of each vertical bar.
* p<0.05, ** p<0.001.
THI events had a dose-response effect on the risks of psychiatric disorders (depression and/or PTSD) even after controlling for trauma/torture events and other potential confounding factors (Figures 2a and 2b). Post hoc trend analysis revealed the presence of linear trend for depression (p=0.001) and PTSD (p=0.023). Standard errors (vertical lines) and confidence intervals are significant.
Figure 2a. Odds Ratio for Depression in South Vietnamese Ex-Political Detainees.
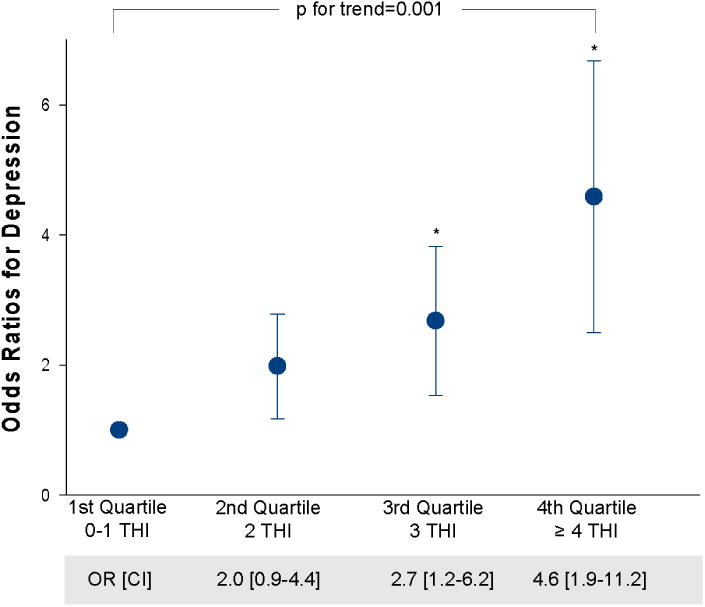
Error bars indicate standard error.
Cases with any missing items on trauma and torture evaluation were excluded
Figure 2b. Odds Ratio for Posttraumatic Stress Disorder (PTSD) in South Vietnamese Ex-Political Detainees.
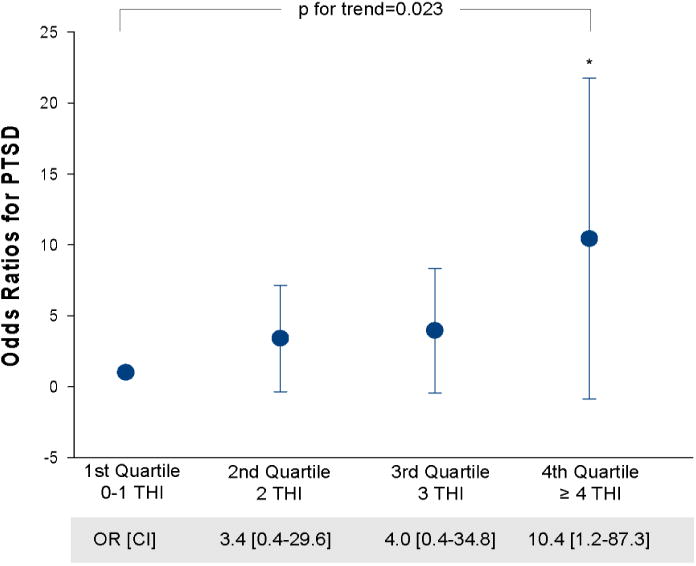
Error bars indicate standard error.
Cases with any missing items on trauma and torture evaluation were excluded.
Table 6 reveals the increased psychiatric morbidity associated with ex-political detainees status as compared to comparison subjects.
Table 6. Psychiatric and Health Status of Vietnamese Comparison Group and Ex-Political Detainees.
| Comparison Group (N=82) | Ex-Detainees (N=337) | ||||
|---|---|---|---|---|---|
|
| |||||
| N | % | N | % | p-value | |
|
| |||||
| Depression | |||||
| No | 63 | 76.8% | 199 | 59.1% | 0.003* |
| Yes | 19 | 23.2% | 138 | 40.9% | |
|
| |||||
| PTSD | |||||
| No | 82 | 100% | 292 | 86.6% | <0.001 Ψ* |
| Yes | 0 | 0 | 45 | 13.4% | |
|
| |||||
| Disability | |||||
| No | 52 | 63.4% | 169 | 50.2% | 0.03 |
| Yes | 30 | 36.6% | 168 | 49.8% | |
|
| |||||
| Post-concussive Syndrome | |||||
| No | 68 | 82.9% | 154 | 45.7% | <0.001* |
| Yes | 14 | 17.1% | 183 | 54.3% | |
|
| |||||
| General Health Status, past 4 weeks | |||||
| Excellent, Good | 21 | 25.6% | 42 | 12.5% | 0.002† |
| Fair | 38 | 46.3% | 157 | 46.6% | |
| Poor, Very Poor | 23 | 28.1% | 138 | 40.9% | |
|
| |||||
| Number of Chronic Medical Conditions | |||||
| 0 to 2 | 62 | 75.6% | 156 | 46.3% | <0.001* |
| 3 or more | 20 | 24.4% | 181 | 53.7% | |
|
| |||||
| Number of Physical Disabilities | |||||
| None | 19 | 23.2% | 61 | 18.1% | 0.29 |
| One or more | 63 | 76.8% | 276 | 81.9% | |
Fisher's Exact Test
2-sided Wilcoxon rank-sum test
Unless indicated, p-values were for Pearson Chi Square test.
In order to sort out the independent contribution of THI and trauma/torture in our entire study population of traumatized resettled Vietnamese refugees we pooled the sample of all respondents. [51] Table 7 presents the results for a series of four analyses for each outcome measure, showing the unadjusted and adjusted odds ratios (OR) for association between all respondents with and without THI. The adjusted odds ratios for trauma/torture were highest for PTSD (22.4; 95% CI: 3.0-165.8) and the lowest for number of physical disabilities (1.6; 95% CI: 0.9-2.8). THI respondents had a higher likelihood of being in poor health than non-THI respondents.
Table 7.
Odds Ratios for the association between psychiatric disorders, disability, post-concussive syndrome and health outcomes in THI vs. non-THI respondents based upon univariable and multivariable logistic regression models.
| Total | Head Injured Status | Relative probability of outcome for head injured vs. uninjured | Relative probability of outcome for each additional reported head injury | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No head injuries (N=156) | 1 or more head injury (N=277) | |||||||||
| N | % | N | % | N | % | Odds Ratio (95% CL) | ||||
| Unadjusted | Adjusted a | Adjusted for torture and trauma b | Adjusted, with continuous head injury, torture, trauma covariates c | |||||||
| Depression | ||||||||||
| No | 271 | 62.58% | 126 | 80.76% | 145 | 52.34% | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 162 | 37.41% | 30 | 19.23% | 132 | 47.65% | 3.8 (2.4,6.1)* | 3.3 (2.1,5.4)* | 3.1 (1.9, 5.2)* | 1.7 (1.3,2.3)* |
| PTSD | ||||||||||
| No | 388 | 89.60% | 155 | 99.35% | 233 | 84.11% | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 45 | 10.39% | 1 | 0.64% | 44 | 15.88% | 29.3 (4.0,214.7)* | 26.4 (3.6, 195.5) * | 22.4 (3.0, 165.8)* | 1.5 (1.1,2.1) * |
| Disability | ||||||||||
| No | 227 | 52.42% | 97 | 62.17% | 130 | 46.93% | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 206 | 47.57% | 59 | 37.82% | 147 | 53.06% | 1.9 (1.2,2.8)* | 2.2 (1.4,3.4)* | 2.2 (1.3,3.5)* | 1.4 (1.1,1.8)* |
| Post-concussive Syndrome | ||||||||||
| No | 229 | 52.88% | 126 | 80.76% | 103 | 37.18% | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 204 | 47.11% | 30 | 19.23% | 174 | 62.81% | 7.1 (4.4, 11.3)* | 6.7 (4.1,10.8)* | 5.9 (3.9,8.9) * | 1.7 (1.2,2.3) * |
| General health status during the past 4 weeks‡ | ||||||||||
| excellent to good | 63 | 14.54% | 36 | 23.07% | 27 | 9.74% | 1.0 | 1.0 | 1.0 | 1.0 |
| Fair | 199 | 45.95% | 76 | 48.71% | 123 | 44.40% | ||||
| poor, very poor | 171 | 39.49% | 44 | 28.20% | 127 | 45.84% | 2.2 (1.4,3.3)* | 2.2 (1.4,3.5)* | 2.1 (1.3, 3.4)* | 1.3 (1.0,1.6) * |
| Number of chronic med conditions | ||||||||||
| 0 to 2 (median) | 227 | 52.42% | 117 | 75.00% | 110 | 39.71% | 1.0 | 1.0 | 1.0 | 1.0 |
| 3 or more | 206 | 47.57% | 39 | 25.00% | 167 | 60.28% | 4.6 (2.9,7.0)* | 5.0 (3.1,8.0)* | 4.9 (3.0, 8.1)* | 1.4 (1.1,1.9)* |
| Number of physical disabilities | ||||||||||
| None | 81 | 18.70% | 37 | 23.71% | 44 | 15.88% | 1.0 | 1.0 | 1.0 | 1.0 |
| One or more | 352 | 81.29% | 119 | 76.28% | 233 | 84.11% | 1.6 (1.01,2.7)* | 1.5 (0.9,2.5) | 1.6 (0.9,2.8) | 1.1 (0.8,1.5) |
Note:
p < 0.05
Odds computed as probability of poor health status to fair, good or excellent.
Note:
Adjustment was performed using multiple logistic regression with covariates for marital status (married vs. not married), age at interview, education in VN, current living status (with spouse or children vs. other situations), yrs in USA, head injury status.
These analyses adjusted for covariates noted in (a). In addition, they included one covariate representing any traumatic experience (trauma or torture experience). For PTSD we only included participants who had experienced at least some torture or trauma (excluding 32 participants who reported no torture or trauma). For the other outcomes, we excluded 3 participants with head injury but no torture or trauma and report results for the additive models because it was then not possible computationally to include the interaction . When interaction effects were first included in the analyses of the full dataset for depression, PCS, general health status and chronic medical conditions, they were non-statistically significant.
The final set of models adjusted for covariates noted in (a) and also for the number of trauma, torture and head injury events. They also included the single degree of freedom interaction effect between head injury and any traumatic experience, represented by a 0/1 indicator covariate. The odds ratios for THI represent increased risk with each additional reported event.
There are overlapping items on the PCS, HTQ and HSCL (and these symptom scores are highly correlated), which raised concerns that the PCS may not be distinguishable from depression and anxiety symptoms associated with PTSD. Sensitivity analyses were performed. The association between PCS and THI, controlling for depression and PTSD, were also analyzed with PCS as a continuous measure. The results were consistent. Although there are differences according to the analysis whether we analyze subscale or total post-concussive syndrome (PCS) score, overall, the results are consistent and show higher risk for PCS in THI participants, even after controlling for depression and PTSD. This result is most consistent across our sensitivity analyses for the somatic and cognitive subscales but also holds for the sensory subscales in the additive indicator logistic regression.
Discussion
This study confirms that THI are commonly reported in South Vietnamese ex-political detainees who survived torture in communist re-education camps and that THI is highly associated with major mental health sequelae including depression and posttraumatic stress disorder. [19,22,52-54] This data supports the brutal and graphic description of Vietnamese ex-political detainees of their re-education camp torture experience and supports the idea that THI as a human rights violation can be embedded within a scenario of multiple trauma and torture events of all types and is not a single isolated event. [55]
As Goldfield et al. [26] suggested as early as 1988, THI is a common form of torture whose presence and related health consequences must be considered in all persons who have been subjected to human rights violations. The effects of THI on psychiatric outcomes in populations that have lived through extreme violence have not been firmly established since the pioneering studies of concentration camp survivors resettled in Norway after World War II that found mechanical impairments, toxic and traumatized brains, and cerebral organic changes. [6,56-58] In a large random sample of Cambodian refugees, Mollica et al. [9] found that THI explained 20% of the variance in symptom scores for depression and 8% for PTSD, respectively.
Our study adds new insight into the THI/trauma/torture relationship. Survey results reveal that THI is synergistic with trauma/torture events in ex-political detainees illustrating that as the number of trauma/torture events increase concurrently with increases in THI events, the presence of depression and PTSD also increases. While this dose-effect relationship has been previously demonstrated in traumatized refugee populations for trauma and torture, this study illustrates the important contribution of THI. [59] THI is demonstrated in the ex-political detainees, as well as in the pooled sample of detainees and the comparison group, to have a major impact on mental health outcomes independent of the effects of trauma and torture events. The pooled sample analysis also revealed the impact on indices of health and disability.
The higher prevalence of PTSD in the THI ex-political detainee group as compared to the non-THI ex-political detainee group and the comparison group is especially important to note. The relatively low rate of PTSD in our comparison group is consistent with the low risk of past-year mental illness found in a population based study of trauma-exposed Vietnamese refugees resettled for ten years in Australia. [60] Those exposed to more than three traumas were at greater risk, however, compared to those who had not been exposed to traumatic events. [60] The recent debate that PTSD may not be occurring due to loss of consciousness in THI survivors may not be a relevant issue in those individuals who have experienced THI and loss of consciousness during episodes of extreme violence that include multiple traumatic life events. [61-63] The high co-morbidity of depression with PTSD and post-concussive syndrome in THI respondents is some indication of the severity of THI-related psychiatric illness. Our study clearly indicates that in traumatized groups who have experienced extreme violence and torture, the presence of PTSD might be masking an underlying traumatic brain injury secondary to THI, especially as PTSD in this study has been shown to be an independent result of THI, when all other non-THI trauma and torture events are controlled for. In particular, PTSD might be a specific marker for THI, and quite possibly TBI. Our neuroimaging study of this population further addresses this issue, and documents the association between structural brain abnormalities in Vietnamese ex-political detainees with THI and symptom severity of depression. [22] This is consistent with other studies in non-torture survivors. THI in non-traumatized populations is associated with brain structural abnormalities in the pre-frontal temporal cortices. [64] These areas of the brain are known to be associated with regulation of mood, affect, and the processing of traumatic memories.
Our results are consistent with mental health findings in mainstream non-traumatized general populations. [47,65-72] Similarly, in studies of combat veterans, THI is associated with PTSD, [73] depression, [74] and health problems. [23] THI also appears to increase the risk of post-concussive syndrome (PCS) and poor health status. While the symptoms of PCS are highly correlated with PTSD and depression, our analysis reveals that PCS, like PTSD, is also independently associated with THI. The potential health risks for THI survivors are far-reaching. Our study reveals increased risk for disability, self-perception of poor health status, and increased number of medical and physical illnesses in THI survivors, consistent with the literature. [75] PCS and poor health status may be partially mediated through chronic depression and PTSD. [23,76-80] Some combat veteran researchers, however, claim that THI events are not unique but are similar to other types of trauma that cause PTSD and mediate mental health outcomes through stress responses in contrast to direct brain changes. [11,81] Our current data and neuroimaging results do not support this viewpoint. Our results suggest that it would be clinically remiss not to consider THI-related neurological and cognitive changes in persons who have a history of extreme violence, and therefore possible THI. [22,82] In any event, a history of THI and the possibility of TBI in a torture survivor must be considered and identified using neuropsychiatric testing and neuroimaging. [82] Determining underlying brain disease will lead to more effective evidence-based treatment. [83-84] THI survivors and their family members must receive education regarding the cause of the patient's symptoms and the rationale for TBI treatment since they are most likely unaware of the clinical importance of THI [82,85] and given the enormous psychological and other stress faced by caregivers of those with TBI. [86-87]
Limitations
A cross-sectional retrospective study such as ours cannot establish causal mechanisms between THI and psychiatric morbidity. It is our hypothesis, supported by our results, that THI mediated brain injuries contribute to the development of PTSD and depression as suggested in the model by Flannelly, Koenig, Galek, and Ellison. [88] Kay, Newman, Cavallo, Ezrachi, and Resnick [89] provide a clear exposition of the possible neuropsychological processes by which mild THI can lead to negative mental health outcomes. Our neuroimaging studies of a random sample of ex-detainees and comparison subjects published elsewhere strongly support the role of the prefrontal temporal lobes, damaged in THI, being linked to PTSD and depression. [22] Our results also show that associations between THI, post-concussive syndrome (PCS), disability and poor health status exist. These relationships, however, are poorly understood and require considerable research attention including a prospective long-term follow-up of THI damaged torture survivors.
Another limitation of the study is the possibility that the Vietnamese ex-political detainees surveyed were a biased sample. There may be something special about the nature of the THI they suffered that is accounting for our results. Few ex-political detainees had THI without multiple traumas, therefore we studied dose-effect and controlled for trauma/torture events. THI events had an independent relationship to mental health outcomes.
The Vietnamese comparison group was selected to be as similar to the ex-political detainees as possible except for the absence of THI. It is almost impossible to find Vietnamese men resettled in the USA who have not had traumatic life experiences before arriving in America, [19] so we adjusted for this by comparing detainees to a non-THI comparison group and secondly by pooling all participants, estimating the effects of THI after controlling for torture and trauma experience. [51]
Determining the relative severity of events in populations who have experienced extreme and multiple traumas is difficult using self-report. Twenty-five years of research conducted by our Harvard research team and others have shown the validity of measuring the self-reports of extreme trauma and torture events. When we developed the HTQ, we decided to limit respondent distress by including only those trauma and torture events that would beyond doubt have a major psychological impact on the victim/survivor. [38] Hatch and Dohrenwend [90] support this view, stating, “simple recall over long periods of time is not feasible for all but major traumatic and other large stressful events” (p. 329).
The issue of recall biases related to THI and other trauma/torture events has been a perceived limitation of all studies using retrospective memories of traumatic life events. [91-93] We have addressed this recall biases critique in our longitudinal study of Bosnian refugees using measurements that were also applied in this study [94] and suspect that there was an underreporting of all events over-time.
The self-reporting of THI in our survey may be inaccurate. [72] Amnesia associated with THI may be contributing to poor memory of THI events. Amnesia is not pathognomonic of mild THI and it is hard to imagine a scenario in which so many individuals falsely report THI at various times in their past. Objective history of the nature and severity of the THI events and possible TBI sequelae does not exist since Vietnamese re-education camps did not keep records on the health status of their inmates and the medical records of the South Vietnamese Army were also not available. Our THI-affected survey respondents gave histories of head injury events commonly associated with loss of consciousness that suggest the possibility of TBI. [95-97] These events were independently associated with brain changes on our neuroimaging study, [22] helping to validate the accuracy of self-reporting in our survey groups by providing an independent and objective measure of THI and trauma/torture.
Conclusion
For the first time since the original work of Eitinger [56-57] immediately after World War II, THI and presumptive TBI (objectively presented in our neuroimaging study [22]) have been demonstrated to be strongly related to psychiatric morbidity, disability, and poor health status in survivors of extreme violence. THI events such as “beatings to the head” are unfortunately common instruments of human cruelty. The brain is an extremely sensitive organ that can be readily damaged without obvious indications of a penetrating wound or major neurological deficit. [64] These invisible wounds, however, can have major emotional, social, and health consequences over time. Screening for and the treatment of THI health and mental health sequelae must become standard operating practice in the care of those individuals affected by mass violence and torture.
Box 1. Definitions of Key Terms.
| Traumatic Head Injury (THI)a | Concussion-associated THI, with 1 or more occasions during which all 3 postconcussive symptoms (loss of consciousness, posttraumatic transient amnesia, and any neurologic deficits) occurred. |
| Traumatic Brain Injury (TBI)b | TBI entails damage to the brain resulting from an external force (e.g., brain laceration, intracranial hematoma, intracranial hypertension, hypoxia, anemia, contusion, metabolic anomalies, shearing of the fibers of nerves, and contrecoup injuries). It is not due to a degenerative or congenital insult to the brain. It may lead to temporary or permanent impairment of cognitive, physical, and psychosocial functions, with associated altered or reduced state of consciousness. |
| Post Concussive Syndrome (PCS)b | A syndrome that includes fatigue, sensitivity to light or sound, headache, dizziness, sleep disturbance, and concentration problems. The symptoms of PCS overlap with some of the symptoms of PTSD. |
Notes: Definitions vary from source to source.
Definition is from Mollica RF, Lyoo IK, Chernoff MC, Bui HX, Lavelle J, Yoon SJ, et al. Brain structural abnormalities and mental health sequelae in South Vietnamese ex-political detainees who survived traumatic head injury and torture. Arch Gen Psychiatry. 2009;66(11):1221-1232.
Definition is from Bryant R. Posttraumatic stress disorder vs. traumatic brain injury. Dialogues in Clinical Neuroscience. 2011;13(3):251-262.
Box 2. What is a dose effect relationship?
A dose-effect relationship is “a relationship in which a change in the amount, intensity, or duration of exposure is associated with a change in risk of a specified outcome” (Farlex, 2012). In the present study, we tested our hypothesis that effects of THI in Vietnamese torture survivors would be independent of non THI trauma/torture events in their relationship to depression and PTSD.
Source: Farlex (2012). Farlex Partner Medical Dictionary. Retrieved from http.//medical-dictionary.thefreedictionary.com/dose-response+relationship
Acknowledgments
Research for this manuscript was made possible by Grant #MH R01-059559-04 from the National Institute of Health, Bethesda, Maryland.
Footnotes
There are no conflicts of interest.
- Vietnamese American Civic Association (VACA)
- Daniel H. Hovelson, BA, Harvard Program in Refugee Trauma
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Richard F. Mollica, Email: rmollica@partners.org.
Miriam C. Chernoff, Email: miriam.chernoff@juno.com.
S. Megan Berthold, Email: megan.berthold@uconn.edu.
James Lavelle, Email: jlavelle@partners.org.
In Kyoon Lyoo, Email: inkylyoo@ewha.ac.kr.
Perry Renshaw, Email: Perry.Renshaw@hsc.utah.edu.
References
- 1.Thygesen P, Hermann K, Willanger R. Concentration camp survivors in Denmark: Persecution, disease, disability, compensation. A 23-year follow-up. A survey of the long-term effects of severe environmental stress. Dan Med Bull. 1970;17:65–108. [PubMed] [Google Scholar]
- 2.Jensen TS, Genefke IK, Hyldebrandt N, Pedersen H, Petersen HD, Weile B. Cerebral atrophy in young torture victims. N Engl J Med. 1982;307:1341. doi: 10.1056/NEJM198211183072112. [DOI] [PubMed] [Google Scholar]
- 3.Rasmussen OV. Medical aspects of torture. Dan Med Bull. 1990;37(Suppl 1):1–88. [PubMed] [Google Scholar]
- 4.Petersen HD, Jacobsen P. Psychical and physical symptoms after torture: A prospective controlled study. Forensic Sci Int. 1985;29:179–89. doi: 10.1016/0379-0738(85)90111-2. [DOI] [PubMed] [Google Scholar]
- 5.Strom A. Norwegian concentration camp survivors. Oslo, Norway: Oslo University Press; 1984. [Google Scholar]
- 6.Strom A, Refsum SB, Eitinger L, Gronvik O, Lonnum A, Engeset A, et al. Examination of Norwegian ex-concentration-camp prisoners. J Neuropsychiatr. 1962;4:43–62. [PubMed] [Google Scholar]
- 7.Sutker P, Vasterling JJ, Brailey K, Allain A. Memory, attention, and executive deficits in POW survivors: Contributing biological and psychological factors. Neuropsychology. 1995;9:118–125. [Google Scholar]
- 8.Sutker PB, Winstead DK, Galina ZH, Allain AN. Assessment of long-term psychosocial sequelae among POW survivors of the Korean Conflict. J Pers Assess. 1990;54:170–80. doi: 10.1080/00223891.1990.9673984. [DOI] [PubMed] [Google Scholar]
- 9.Mollica RF, Henderson DC, Tor S. Psychiatric effects of traumatic brain injury events in Cambodian survivors of mass violence. Br J Psychiatry. 2002;181:339–47. doi: 10.1192/bjp.181.4.339. [DOI] [PubMed] [Google Scholar]
- 10.Keatley E, Ashman T, Im B, Rasmussen A. Self-reported head injury among refugee survivors of torture. J Head Trauma Rehabil. 2013;28(6):E8–E13. doi: 10.1097/HTR.0b013e3182776a70. [DOI] [PubMed] [Google Scholar]
- 11.Bryant R. Posttraumatic stress disorder vs. traumatic brain injury. Dialogues in Clinical Neuroscience. 2011;13(3):251–262. doi: 10.31887/DCNS.2011.13.2/rbryant. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vanderploeg RD, Belanger HG, Curtiss G. Mild traumatic brain injury and posttraumatic stress disorder and their association with health symptoms. Archives of Physical Medicine and Rehabilitation. 2009;90:1084–9s3. doi: 10.1016/j.apmr.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 13.Hart T, Brenner L, Clark AN, Bogner JA, Novack TA, Chervoneva I, et al. Major and minor depression after traumatic brain injury. Arch Phys Med Rehabil. 2011;92:1211–9. doi: 10.1016/j.apmr.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 14.Bryant RA, O'Donnell ML, Creamer M, McFarlane AC, Silove D. A multisite analysis of the fluctuating course of posttraumatic stress disorder. JAMA Psychiatry. 2013;70(8):839–846. doi: 10.1001/jamapsychiatry.2013.1137. [DOI] [PubMed] [Google Scholar]
- 15.Burnett A, Peel M. Asylum seekers and refugees in Britain: The health of survivors of torture and organized violence. BMJ. 2001;322:606–9. doi: 10.1136/bmj.322.7286.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacDonald BK, Mummery CJ, Heaney D. Health needs of asylum seekers and refugees: Head injury needs to be taken into consideration in survivors of torture. BMJ. 2001;323:230. [PubMed] [Google Scholar]
- 17.Manley GT, Maas AIR. Traumatic brain injury: An international knowledge-based approach. JAMA. 2013;310(5):473–474. doi: 10.1001/jama.2013.169158. [DOI] [PubMed] [Google Scholar]
- 18.Mollica R, Lavelle J. Southeast Asian refugees. In: Comas-Diaz L, Griffith E, editors. Clinical guidelines in cross-cultural mental health. New York: J. Wiley and Sons; 1988. pp. 262–304. [Google Scholar]
- 19.Mollica RF, McInnes K, Pham T, Smith Fawzi MC, Murphy E, Lin L. The dose-effect relationships between torture and psychiatric symptoms in Vietnamese ex-political detainees and a comparison group. J Nerv Ment Dis. 1998;186:543–53. doi: 10.1097/00005053-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Amnesty International. Vietnam: “Renovation” (Doi Moi) the law and human rights in the 1980s. London: Author; 1990. [Google Scholar]
- 21.Weiss L. Immigrants: Timing is everything. Atlantic Monthly. 1994 Jan;:32–44. [Google Scholar]
- 22.Mollica RF, Lyoo IK, Chernoff MC, Bui HX, Lavelle J, Yoon SJ, et al. Brain structural abnormalities and mental health sequelae in South Vietnamese ex-political detainees who survived traumatic head injury and torture. Arch Gen Psychiatry. 2009;66(11):1221–1232. doi: 10.1001/archgenpsychiatry.2009.127. [DOI] [PubMed] [Google Scholar]
- 23.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. N Engl J Med. 2008;358:453–63. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 24.Flaherty JA, Gaviria FM, Pathak D, Mitchell T, Wintrob R, Richman, et al. Developing instruments for cross-cultural psychiatric research. J Nerv Ment Dis. 1988;176:257–63. [PubMed] [Google Scholar]
- 25.Westermeyer J. Psychiatric diagnosis across cultural boundaries. Am J Psychiary. 1985;142:798–805. doi: 10.1176/ajp.142.7.798. [DOI] [PubMed] [Google Scholar]
- 26.Goldfeld AE, Mollica RF, Pesavento BH, Faraone SV. The physical and psychological sequelae of torture: Symptomatology and diagnosis. JAMA. 1988;259:2725–9. [PubMed] [Google Scholar]
- 27.Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire: Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Ment Dis. 1992;180:111–6. [PubMed] [Google Scholar]
- 28.American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington, DC: Author; 1994. [Google Scholar]
- 29.Mollica RF, Wyshak G, de Marneffe D, Khuon F, Lavelle J. Indochinese versions of the Hopkins Symptom Checklist-25: A screening instrument for the psychiatric care of refugees. Am J Psychiatry. 1987;144:497–500. doi: 10.1176/ajp.144.4.497. [DOI] [PubMed] [Google Scholar]
- 30.Gorst-Unsworth C, Goldenberg E. Psychological sequelae of torture and organised violence suffered by refugees from Iraq: Trauma-related factors compared with social factors in exile. Br J Psychiatry. 1998;172:90–4. doi: 10.1192/bjp.172.1.90. [DOI] [PubMed] [Google Scholar]
- 31.Mollica RF, Donelan K, Tor S, Lavelle J, Elias C, Frankel M, et al. The effect of trauma and confinement on functional health and mental health status of Cambodians living in Thailand-Cambodia border camps. JAMA. 1993;270:581–6. [PubMed] [Google Scholar]
- 32.Rasekh Z, Bauer HM, Manos MM, Iacopino V. Women's health and human rights in Afghanistan. JAMA. 1998;280:449–55. doi: 10.1001/jama.280.5.449. [DOI] [PubMed] [Google Scholar]
- 33.Shrestha NM, Sharma B, Van Ommeren M, Regmi S, Makaju R, Komproe I, et al. Impact of torture on refugees displaced within the developing world: Symptomatology among Bhutanese refugees in Nepal. JAMA. 1998;280:443–8. doi: 10.1001/jama.280.5.443. [DOI] [PubMed] [Google Scholar]
- 34.Sinnerbrink I, Silove D, Field A, Steel Z, Manicavasagar V. Compounding of premigration trauma and postmigration stress in asylum seekers. J Psychol. 1997;131:463–70. doi: 10.1080/00223989709603533. [DOI] [PubMed] [Google Scholar]
- 35.Fawzi MC, Pham T, Lin L, Nguyen TV, Ngo D, Murphy E, Mollica RF. The validity of posttraumatic stress disorder among Vietnamese refugees. J Trauma Stress. 1997;10:101–8. doi: 10.1023/a:1024812514796. [DOI] [PubMed] [Google Scholar]
- 36.Hollander AC, Ekblad S, Mukhamadiev D, Muminova R. The validity of screening instruments for posttraumatic stress disorder, depression, and other anxiety symptoms in Tajikistan. J Nerv Ment Dis. 2007;195:955–8. doi: 10.1097/NMD.0b013e318159604b. [DOI] [PubMed] [Google Scholar]
- 37.Mollica RF, Wyshak G, de Marneffe D, Khuon F, Lavelle J. Indochinese Versions of the Hopkins Symptom Checklist-25: A Screening Instrument for the Psychiatric Care of Refugees. Am J Psychiatry. 1987;144:497–500. doi: 10.1176/ajp.144.4.497. [DOI] [PubMed] [Google Scholar]
- 38.Mollica RF, McDonald LS, Massagli MP, Silove DM. Measuring trauma, measuring torture: Instructions and guidance on the utilization of the Harvard Program in Refugee Trauma's Versions of the Hopkins Symptom Checklist-25 (HSCL-25) & The Harvard Trauma Questionnaire (HTQ) Cambridge, MA: Harvard Program in Refugee Trauma; 2004. [Google Scholar]
- 39.Kleijn WC, Hovens JE, Rodenburg JJ. Posttraumatic stress symptoms in refugees: Assessments with the Harvard Trauma Questionnaire and the Hopkins Symptom Checklist-25 in different languages. Psychol Rep. 2001;88(2):527–32. doi: 10.2466/pr0.2001.88.2.527. [DOI] [PubMed] [Google Scholar]
- 40.Stewart AL, Hays RD, Ware JE., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988;26:724–35. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 41.VonKorff M, Ustun TB, Ormel J, Kaplan I, Simon G. Self-report disability in an international primary care study of psychological illness. Journal of Clinical Epidemiology. 1996;49:297–303. doi: 10.1016/0895-4356(95)00512-9. [DOI] [PubMed] [Google Scholar]
- 42.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 43.World Health Organization. International classification of impairments, disabilities, and handicaps: A manual of classification relating to the consequences of disease. Geneva [Albany, NY[: Author; 1980. [Google Scholar]
- 44.Stulemeijer M, van der Werf S, Bleijenberg G, Biert J, Brauer J, Vos PE. Recovery from mild traumatic brain injury: A focus on fatigue. J Neurol. 2006;253:1041–7. doi: 10.1007/s00415-006-0156-5. [DOI] [PubMed] [Google Scholar]
- 45.Idler EL, Kasl S. Health perceptions and survival: Do global evaluations of health status really predict mortality? J Gerontol. 1991;46:S55–65. doi: 10.1093/geronj/46.2.s55. [DOI] [PubMed] [Google Scholar]
- 46.Ware J, Kosinski M, Dewey J, Gandek B. How to score and interpret single-item health status measures: A manual for users of the SF-8 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2001. [Google Scholar]
- 47.Cicerone KD, Kalmar K. Persistent postconcussion syndrome: The structure of subjective complaints after mild traumatic brain injury. Journal of Head Trauma Rehabilitation. 1995;1995;10:1–17. [Google Scholar]
- 48.Lemeshow S, Hosmer DW., Jr A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. 1982;115:92–106. doi: 10.1093/oxfordjournals.aje.a113284. [DOI] [PubMed] [Google Scholar]
- 49.SAS Institute. SAS/STAT user's guide, version 8. Cary NC: SAS Institue Inc; 1999. [Google Scholar]
- 50.SAS Institute. SAS/STAT software: Changes and enhancements, release 82. Cary, NC: SAS Institute Inc; 2001. [Google Scholar]
- 51.Michael M, III, Boyce WT, Wilcox AJ. Biomedical bestiary: An epidemiologic guide to flaws and fallacies in the medical literature. Boston, MA: Little, Brown and Co; 1984. [Google Scholar]
- 52.Jacobs U, Iacopino V. Torture and its consequences: A challenge to clinical neuropsychology. Professional Psychology: Research and Practice. 2001;32:458–464. [Google Scholar]
- 53.Moreno A, Grodin MA. Torture and its neurological sequelae. Spinal Cord. 2002;40:213–23. doi: 10.1038/sj.sc.3101284. [DOI] [PubMed] [Google Scholar]
- 54.Quiroga J, Jaranson J. Politically-motivated torture and its survivors: A desk study review of the literature. Torture. 2006;15:1–111. [Google Scholar]
- 55.Hendrickson P. The living and the dead: Robert McNamara and five lives of a lost war. New York: Alfred A Knopf; 1996. [Google Scholar]
- 56.Eitinger L. Concentration camp survivors in Norway and Israel. Isr J Med Sci. 1965;1:883–95. [PubMed] [Google Scholar]
- 57.Eitinger L. Mortality and mobidity after excessive stress. Oslo, Norway: Oslo University Press; 1973. [Google Scholar]
- 58.Strom ACS. Norwegian concentration camp survivors. Oslo, New York: Universitetsforlaget; Humanities Press; 1968. [Google Scholar]
- 59.Mollica RF, McInnes K, Poole C, Tor S. Dose-effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. Br J Psychiatry. 1998;173:482–8. doi: 10.1192/bjp.173.6.482. [DOI] [PubMed] [Google Scholar]
- 60.Steel Z, Silove D, Phan T, Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: A population-based study. Lancet. 2002;360:1056–62. doi: 10.1016/S0140-6736(02)11142-1. [DOI] [PubMed] [Google Scholar]
- 61.Bryant RA. Posttraumatic stress disorder and traumatic brain injury: Can they co-exist? Clin Psychol Rev. 2001;21:931–48. doi: 10.1016/s0272-7358(00)00074-x. [DOI] [PubMed] [Google Scholar]
- 62.Gil S, Caspi Y, Ben-Ari IZ, Koren D, Klein E. Does memory of a traumatic event increase the risk for posttraumatic stress disorder in patients with traumatic brain injury? A prospective study. Am J Psychiatry. 2005;162:963–9. doi: 10.1176/appi.ajp.162.5.963. [DOI] [PubMed] [Google Scholar]
- 63.Joseph S, Materson J. Posttraumatic stress disorder and traumatic brain injury: Are they mutually exclusive? J Trauma Stress. 1999;12:437–53. doi: 10.1023/A:1024762919372. [DOI] [PubMed] [Google Scholar]
- 64.Ropper AH, Gorson KC. Clinical practice: Concussion. N Engl J Med. 2007;356:166–72. doi: 10.1056/NEJMcp064645. [DOI] [PubMed] [Google Scholar]
- 65.Alexander MP. Mild traumatic brain injury: Pathophysiology, natural history, and clinical management. Neurology. 1995;45:1253–60. doi: 10.1212/wnl.45.7.1253. [DOI] [PubMed] [Google Scholar]
- 66.Armstrong C. Emotional changes following brain injury: Psychological and neurological components of depression, denial and anxiety. Journal of Rehabilitation. 1991;57(2):8. [Google Scholar]
- 67.Binder LM. Persisting symptoms after mild head injury: A review of the postconcussive syndrome. J Clin Exp Neuropsychol. 1986;8:323–46. doi: 10.1080/01688638608401325. [DOI] [PubMed] [Google Scholar]
- 68.Fann JR, Katon WJ, Uomoto JM, Esselman PC. Psychiatric disorders and functional disability in outpatients with traumatic brain injuries. Am J Psychiatry. 1995;152:1493–9. doi: 10.1176/ajp.152.10.1493. [DOI] [PubMed] [Google Scholar]
- 69.Gualtieri C. The problem of mild brain injury. Neuropsychiatry, Neuropsychology, and Behavioral Neurology. 1995;8:127–136. [Google Scholar]
- 70.Jorge RE, Robinson RG, Moser D, Tateno A, Crespo-Facorro B, Arndt S. Major depression following traumatic brain injury. Arch Gen Psychiatry. 2004;61:42–50. doi: 10.1001/archpsyc.61.1.42. [DOI] [PubMed] [Google Scholar]
- 71.Koponen S, Taiminen T, Portin R, Himanen L, Isoniemi H, Heinonen H, et al. Axis I and II psychiatric disorders after traumatic brain injury: A 30-year follow-up study. Am J Psychiatry. 2002;159:1315–21. doi: 10.1176/appi.ajp.159.8.1315. [DOI] [PubMed] [Google Scholar]
- 72.Moore EL, Terryberry-Spohr L, Hope DA. Mild traumatic brain injury and anxiety sequelae: A review of the literature. Brain Inj. 2006;20:117–32. doi: 10.1080/02699050500443558. [DOI] [PubMed] [Google Scholar]
- 73.Chemtob CM, Muraoka MY, Wu-Holt P, Fairbank JA, Hamada RS, Keane TM. Head injury and combat-related posttraumatic stress disorder. J Nerv Ment Dis. 1998;186:701–8. doi: 10.1097/00005053-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 74.Vasterling JJ, Constans JI, Hanna-Pladdy B. Head injury as a predictor of psychological outcome in combat veterans. J Trauma Stress. 2000;13:441–51. doi: 10.1023/A:1007781107513. [DOI] [PubMed] [Google Scholar]
- 75.Kowlakowsky-Hayner SA, Murphy MP, Carmine H. Long-term health implications of individuals with TBI: A rehabilitation perspective. NeuroRehabilitation. 2012;31(1):85–94. doi: 10.3233/NRE-2012-0777. [DOI] [PubMed] [Google Scholar]
- 76.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 77.Cassano P, Fava M. Depression and public health: An overview. J Psychosom Res. 2002;53:849–57. doi: 10.1016/s0022-3999(02)00304-5. [DOI] [PubMed] [Google Scholar]
- 78.Eaton WW, Armenian H, Gallo J, Pratt L, Ford DE. Depression and risk for onset of type II diabetes: A prospective population-based study. Diabetes Care. 1996;19:1097–102. doi: 10.2337/diacare.19.10.1097. [DOI] [PubMed] [Google Scholar]
- 79.Freedland K. Section II: Hypothesis 1: Depression is a risk factor for the development of type 2 diabetes. Diabetes Spectrum. 2004;17:150–152. [Google Scholar]
- 80.King H, Keuky L, Seng S, Khun T, Roglic G, Pinget M. Diabetes and associated disorders in Cambodia: Two epidemiological surveys. Lancet. 2005;366:1633–9. doi: 10.1016/S0140-6736(05)67662-3. [DOI] [PubMed] [Google Scholar]
- 81.Bryant RA. Disentangling mild traumatic brain injury and stress reactions. N Engl J Med. 2008;358:525–7. doi: 10.1056/NEJMe078235. [DOI] [PubMed] [Google Scholar]
- 82.Weinstein CS, Fucetola R, Mollica R. Neuropsychological issues in the assessment of refugees and victims of mass violence. Neuropsychol Rev. 2001;11:131–41. doi: 10.1023/a:1016650623996. [DOI] [PubMed] [Google Scholar]
- 83.Cicerone KD, Mott T, Azulay J, Friel JC. Community integration and satisfaction with functioning after intensive cognitive rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2004;85:943–50. doi: 10.1016/j.apmr.2003.07.019. [DOI] [PubMed] [Google Scholar]
- 84.Hunter JV, Wilde EA, Tong KA, Holshouser BA. Emerging imaging tools for use with traumatic brain injury research. J Neurotrauma. 2012;29(4):654–671. doi: 10.1089/neu.2011.1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McAllister TW. Evaluation of brain injury related behavioral disturbances in community mental health centers. Community Ment Health J. 1997;33:341–58. doi: 10.1023/a:1025055426260. [DOI] [PubMed] [Google Scholar]
- 86.Doyle ST, Perrin PB, Sosa DMD, Jove IGE, Lee GK, Arango-Lasprilla JC. Connecting family needs and TBI caregiver mental health in Mexico City, Mexico. Brain Injury. 2013;27(12):1441–1449. doi: 10.3109/02699052.2013.826505. [DOI] [PubMed] [Google Scholar]
- 87.Verhaeghe S, Defloor T, Grypdonck M. Stress and coping among families of patients with traumatic brain injury: A review of the literature. Journal of Clinical Nursing. 2005;14:1004–1012. doi: 10.1111/j.1365-2702.2005.01126.x. [DOI] [PubMed] [Google Scholar]
- 88.Flannelly KJ, Koenig HG, Galek K, Ellison CG. Beliefs, mental health, and evolutionary threat assessment systems in the brain. J Nerv Ment Dis. 2007;195:996–1003. doi: 10.1097/NMD.0b013e31815c19b1. [DOI] [PubMed] [Google Scholar]
- 89.Kay T, Newman H, Cavallo M, Ezrachi O, Resnick M. Toward a neuropsychological model of functional disability after mild traumatic brain injury. Neuropsychology. 1992;6:371–384. [Google Scholar]
- 90.Hatch SL, Dohrenwend BP. Distribution of traumatic and other stressful life events by race/ethnicity, gender, SES and age: A review of the research. Am J Community Psychol. 2007;40:313–32. doi: 10.1007/s10464-007-9134-z. [DOI] [PubMed] [Google Scholar]
- 91.King BS, Gupta R, Narayan RK. The early assessment and intensive care unit management of patients with severe traumatic brain and spinal cord injuries. Surg Clin North Am. 2000;80(3):855–70. doi: 10.1016/s0039-6109(05)70100-6. [DOI] [PubMed] [Google Scholar]
- 92.Roemer L, Litz BT, Orsillo SM, Ehlich PJ, Friedman MJ. Increases in retrospective accounts of war-zone exposure over time: The role of PTSD symptom severity. J Trauma Stress. 1998;11:597–605. doi: 10.1023/A:1024469116047. [DOI] [PubMed] [Google Scholar]
- 93.Southwick SM, Morgan CA, Nicolaou AL, Charney DS. Consistency of memory for combat-related traumatic events in veterans of Operation Desert Storm. Am J Psychiatry. 1997;154(2):173–7. doi: 10.1176/ajp.154.2.173. [DOI] [PubMed] [Google Scholar]
- 94.Mollica RF, Caridad KR, Massagli MP. Longitudinal study of posttraumatic stress disorder, depression, and changes in traumatic memories over time in Bosnian refugees. J Nerv Ment Dis. 2007;195(7):572–9. doi: 10.1097/NMD.0b013e318093ed2c. [DOI] [PubMed] [Google Scholar]
- 95.Centers for Disease Control and Prevention. Heads up: Facts for physicians about mild traumatic brain injury. Atlanta, GA: Author; 2004. [Google Scholar]
- 96.Kay T, Harrington D, Adams R. Definition of mild traumatic brain injury. Journal of Head Trauma Rehabilitation. 1993;8(3):86–87. [Google Scholar]
- 97.Ruff RM, Jurica P. In search of a unified definition for mild traumatic brain injury. Brain Inj. 1999;13(12):943–52. doi: 10.1080/026990599120963. [DOI] [PubMed] [Google Scholar]


