Abstract
Damage to the medial meniscus root, for example by a complete radial tear, destroys the ability of the knee to withstand hoop strain, resulting in contact pressure increases and kinematic alterations. For these reasons, several techniques have been developed to repair the medial meniscus posterior root tear (MMPRT), many of which have shown complete healing of the repaired MMPRT. However, efforts to standardize or optimize the treatment for MMPRT are much needed. When planning a surgical intervention for an MMPRT, strict surgical indications regarding the effect of pullout strength on the refixed root, bony degenerative changes, mechanical alignment, and the Kellgren-Lawrence grade should be considered. Although there are several treatment options and controversies, the current trend is to repair the MMPRT using various techniques including suture anchors and pullout sutures if the patient meets the indications. However, there are still debates on the restoration of hoop tension and prevention of arthritis after repair and further biomechanical and clinical studies should be conducted in the future. The aim of this article was to review and summarize the recent literature regarding various diagnosis and treatment strategies of MMPRT, especially focusing on conflict issues including whether repair techniques can restore the main function of normal meniscus and which is the best suture technique to repair the MMPRT. The authors attempted to provide a comprehensive review of previous studies ranging from basic science to current surgical techniques.
Keywords: Knee, Medial meniscus, Root tear, Suture techniques
Introduction
The meniscus has an important multifunctional role in load transmission, shock absorption, joint stability and lubrication, proprioception, and nutrient supply to maintain overall function of the knee1,2). Of these, the most important function for the prevention of arthritis is the maintenance of hoop tension that allows correct intraarticular load transmission for which the medial meniscus is approximately 90% responsible and the lateral meniscus is approximately 70% responsible3,4). The medial meniscus posterior root tear (MMPRT) leads to loss of hoop tension and, thus, loss of load transmissibility of the meniscus, which results in a biomechanical condition much like total meniscectomy5). Ultimately, the increased contact pressure in the weight bearing portion leads to accelerated joint degeneration5,6,7). For these reasons, several techniques have been developed to repair the MMPRT, many of which have shown efficacy in complete healing of the repaired meniscal root8,9). However, there is still controversy over the restoration of hoop tension and prevention of arthritis after repair and efforts to standardize or optimize the treatment for MMPRTs are much needed.
The aim of this article was to review and summarize the recent literature regarding various diagnosis and treatment strategies of MMPRTs, especially focusing on conflict issues including whether repair techniques can restore the main function of normal meniscus and which is the best suture technique for MMPRT repair. The authors attempted to provide a comprehensive review of previous studies ranging from basic science to current surgical techniques.
Clinical Characteristics of MMPRT
The first case of MMPRT was reported in 1991 by Pagnani et al.10). The MMPRT is usually a radial tear located within 10 mm from the posterior root insertion of the meniscus. Such tears are common in Eastern countries, such as Korea, where a floor-based lifestyle is habitual and traditional11). In these populations, the proportion of MMPRT may take up around 20%-30% of all medial meniscus tears. The prevalence of MMPRT among those treated for meniscal tears was recorded as 27.8% by Bin et al.11), 18% by Nha et al.12), and 20.4% by Moon et al.13). It occurs mostly in the aged population: the age of onset is usually over 50 years of age. The average age of onset was reported as 56.2 years (range, 46 to 76 years) by Habata et al.14), 51.2 years (range, 23 to 58 years) by Lee et al.9), and 55.2 years (range, 42 to 65 years) by Kim et al.8).
The long-term hyper-flexion of the knee under weight-bearing required for their floor-based lifestyle in the older population is thought to be closely linked to the prevalence of MMPRT. Chronic and repetitive hyper-flexion of the knee under weight-bearing may lead to excessive pressure on the meniscus posterior root and its subsequent impingement and degeneration4,11,14). A controlled clinical study is required to scientifically substantiate this hypothesis. Previously, Bin et al.11) demonstrated an association between posterior meniscus impingement and its degeneration that makes the meniscus susceptible to tear upon even trivial injury. Posterior root tear tends to occur more in the medial than lateral meniscus. This may be because, during knee flexion, the lateral meniscus moves posteriorly by 19 mm on average, whereas more limited movement of an average of 4 mm occurs in the medial meniscus; thus, the latter becomes more vulnerable to impingement between the femoral condyle and tibial plateau, which, in turn, leads to an increased risk of meniscal damage4,15).
Sometimes, patients feel a popping sensation in the knee joint when first exposed to trivial injury, then severe pain develops in the knee rendering normal walking difficult14,16). Although the pain resolves and normal activity is resumed, intermittent residual pain and popping sound remain and signs of early degenerative diseases are seen14,16). The natural course of MMPRT is unknown, but premature and extensive degeneration is a common feature5,6,7,17). Sung et al.18) compared the incidence of spontaneous osteonecrosis between patients with MMPRTs and those with medial meniscus posterior horizontal tears: the incidence of osteonecrosis and the extent of meniscal extrusion were significantly greater in the knees with MMPRTs. In a study that investigated the association between medial meniscus tears and arthritic degeneration, Henry et al.17) showed statistically significant relationship between root and radial/flap tears and degenerative changes in the medial femoral condyle and between root and complex tears and degeneration of the medial tibial condyle. According to the multi-center arthritis study by Guermazi et al.19), the meniscal tears that were combined with severe articular damages were of root tear origin in 76.7% and different origins in 19.7%, and the relative association of meniscal damage with root tears was greater than that with other types of tears (2.03:1.84). They concluded from their clinical findings that arthritis in the medial compartment is closely linked to the development of MMPRT. Hwang et al.20) reported that the risk of MMPRT was higher by 5.9 times in females than males, 4.9 times if body mass index was more than 30 kg/m2, 3.3 times in knees with a varus mechanical axis, and 2.7 times in patients with a lower level of sports activities.
Biomechanical Studies on MMPRT
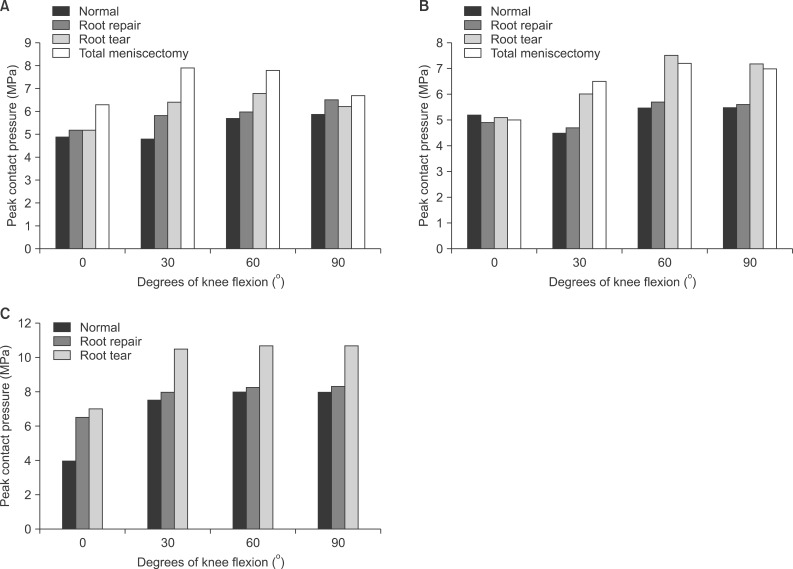
Biomechanical studies to analyze the effects of MMPRT on load transmission capacity of the knee have been reported with the increasing interest in the treatment of MMPRT (Fig. 1). Allaire et al.5) assessed the contact area and peak contact pressure in four different meniscal conditions (normal, MMPRT, repaired MMPRT, and total meniscectomy) using 9 independent cadavers. Meniscal loading of 1,000 N was placed on the knee using a Fuji Sensor at 0°, 30°, 60°, or 90° of flexion, and the two factors were measured and compared between the 4 groups. The levels of decrease in the contact area and increase in the contact pressure in the MMPRT group were significantly similar to those in the total meniscectomy group. In comparison, the values of the repaired meniscus group were similar to those of the normal group, indicating restoration of the weight-bearing function of the knee. In a similar study by Kim et al.21) using 7 cadavers, the same degree of loss of function of the knee was noted in the MMPRT and total meniscectomy groups, but repairs in both groups led to an enhancement of function (especially when the degree of flexion was large), although full restoration to the level of a normal meniscus was not possible. In contrast to Allaire et al.5), they used a novel sensor to exert pressure on the medial femoral condyle, and real-time measurement allowed the experimental condition to mimic the patient's natural clinical state. However, the one disadvantage was that the sensor could evaluate only up to a maximum of 300 N load. On the other hand, in a cadaveric study using pig specimens, Seo et al.22) found a statistically significant increase in contact pressure when the knee was at 0° to 15° of extension after MMPRT repair that was performed at 30° to 90° of knee flexion. This study raised the issue that the currently implemented MMPRT repair would not be a complete treatment considering the risk of mechanical failure during knee extension that occurs in normal gait. Although pig cadavers were used and a meniscal coronary ligament was excised to insert a K-Scan 6900 sensor (Tekscan Inc., Boston, MA, USA) into the tibia, their experiment used a sufficient load of pressure of 1,000 N and gained statistical power by real-time measurement.
Fig. 1.
The histograms show the peak contact pressure in the medial compartment at various knee angles under different meniscal conditions: (A) the study of Kim et al.21); (B) the study of Allaire et al.5); and (C) the study of Seo et al.22).
Taking all the biomechanical studies into consideration, MMPRTs exhibited a similar extent of increase in the articular load and decrease in contact surface area as that in the total meniscectomized knee. A repair of MMPRT is yet insufficient to restore knee function to those seen in normal meniscal conditions. A more effective treatment method for MMPRTs is needed through analysis of knee function using variously modified and improved experimental approaches and enhanced MMPRT reparative methods.
Diagnosis of MMPRT
1. Clinical Symptoms and Patient Questionnaires
Clinical symptoms of MMPRTs described in various studies are consistent with those mentioned above. Habata et al.14) reported that patients heard a popping sound of the knee in response to a trivial injury. Nha et al.23) reported on the transition of initial pain of the knee from acute to chronic. Clinical symptoms are important for the diagnosis of MMPRT, especially popping sound at the onset of pain in the posterior knee has shown to be a very good indicator. Bae et al.16) calculated the diagnostic value of a popping accompanied by pain for MMPRT among middle-aged to elderly Asian population that has adopted the floor-based lifestyle: it had a positive predictive value of 96.5%, a negative predictive value of 81.8%, a sensitivity of 35.0%, a specificity of 99.9%, and a diagnostic accuracy of 77.9%. Thus, a thorough questioning of the patient is advised at initial examination, especially for the presence of popping sound, which is of critical diagnostic importance.
2. Plain Radiographic Examination
Plain radiographic examination of the knee under loading conditions is recommended when examining patients with meniscal tears. Meniscal extrusion after an MMPRT often leads to clinical symptoms such as early joint space narrowing, swift progression of arthritis, and varus deformity of the knee17,24). Particularly, measurement of the joint space from the 450 of flexion standing anteroposterior view (Rosenberg view) before and after the surgery is critical for diagnosis. Lower extremity scanogram is also recommended for examination of the lower extremity upon loading25). Moon et al.26) reported that 35.3% of the knees with MMPRTs had a varus alignment of over 5°. Hwang et al.20) revealed that varus alignment was one of the risk factors for MMPRT and the mean mechanical axis angle was 4.5° in the patients with MMPRTs.
3. Magnetic Resonance Imaging (MRI) Examination
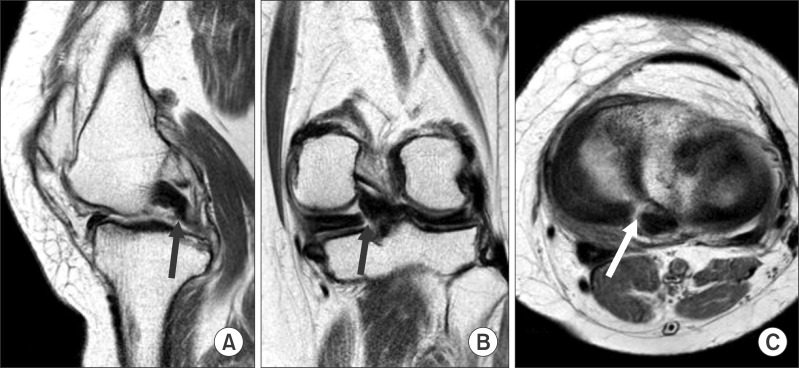
It is easy to overlook the presence of an MMPRT by MRI examination. A study by Bin et al.11) showed that the sensitivity of MRI as a diagnostic tool to detect a posterior root tear was only 66.3%, and did not have the specificity to discern the nature of the tear. They stated that posterior root is difficult to assess by MRI and prone to diagnostic errors because images seemingly show even a single tear as bundles of multiple tears. However, recent reports contributed to raising awareness and interest in the application of MRI for the diagnosis of MMPRTs27,28,29,30,31). Lee et al.31) proposed that the MMPRT would not be difficult to diagnose if the diagnosis is based on three different discriminatory features on MRI-plane images along with clinical symptoms: the ghost sign from the sagittal plane (detection rate of 100%), the vertical linear defect (signs of truncation) on the coronal plane (100%), and the radial linear defect on the axial plane (94%) (Fig. 2). Similarly, Choi et al.29) suggested that the sensitivity and specificity of MRI diagnosis of MMPRTs could be high if the diagnosis is based on the presence of radial tears on the axial plane, signs of truncation and extrusion on the coronal plane, and the ghost sign from the sagittal plane. Especially, they reported MRI exhibited a 100% positive value for the diagnosis of radial tears on the axial plane.
Fig. 2.
The magnetic resonance images show features of medial meniscus posterior root tear. (A) On sagittal image, the posterior medial meniscus root tear is recognized by loss of shape and signal intensity, so called ghost sign (black arrow). (B) On coronal image, the posterior medial meniscus root tear is recognized as a vertical linear defect (black arrow). (C) On axial image, the radial linear defect (white arrow) is detected at the posterior medial meniscus root insertion.
4. Miscellaneous
An in-depth physical examination and MRI are commonly required for the diagnosis of MMPRTs. If further diagnostic methods are necessary to confirm the presence of arthritis or articular damage, single-photon emission computed tomography can be used32).
Treatment of MMPRT
There are several treatment options for MMPRTs including conservative treatment and surgical treatment using various repair techniques. However, there is no consensus on the optimal treatment method for the MMPRT, and efforts to standardize treatment strategies are much needed. The current trend is to repair the MMPRT using various techniques including suture anchors and pullout sutures if the patient meets the indications of procedures aimed at restoring the main function of the meniscus.
1. Conservative Treatment of MMPRT
Biomechanical studies on MMPRT have shown that the extents of articular compression increase and contact surface area decrease are similar to those of the knee after total meniscectomy5,6). However, no prospective studies have been systematically carried out to measure how quickly and to what extent articular degeneration proceeds if a diagnosis is missed. Nevertheless, the clinical results of MMPRT treatment can be satisfying with early diagnosis and proper conservative treatment. Lim et al.33) compared clinical outcomes of non-operative treatment, either drug therapy or physiotherapy, that was prescribed to 30 patients for 8 weeks. At an average of 36 months of follow-up, the authors found a statistically significant enhancement in both groups when compared to the placebo group. Neogi et al.34) carried out exercise therapies for 12 weeks on 37 patients, and also found that after an average follow-up period of 35 months, the knee function was improved, although some signs of progression of arthritis were seen. As aforementioned, the MMPRT generally exhibits popping of the knee at the initial onset of pain, and then acute pain proceeds. Although this acute pain subsides after a certain period of time, progression of arthritis is observed16,26).
Conservative treatment techniques are not just confined to drug therapy using NSAIDs to resolve the initial pain, but include other approaches to ensure satisfactory long-term results, such as active muscle strengthening exercises of the knee, correction of the habit of hyperflexion, weight loss, and management of arthritis. Well devised conservative treatment approaches can be recommended as well as active treatments, and they deserve to be addressed in prospective studies to confirm their advantages.
2. Meniscectomy
When an MMPRT occurs, loading at the junction of the radial tear area and the joint capsule causes expansion, and unstable posterior root impingement results in acute pain and locking of the knee at flexion11). Under these circumstances, partial meniscectomy can be effective in reducing the posterior fallout and improving mechanical symptoms. Bin et al.11) and Habata et al.14) reported that MMPRT patients obtained good clinical outcomes after partial meniscectomy.
However, partial meniscectomy cannot address the biomechanical changes resulting from MMPRTs. Rather, it increases the pressure on the residual meniscus and tends to worsen subsequent articular degeneration35,36). In a study by Han et al.36), after partial meniscectomy for MMPRTs, 56% saw total resolution of pain and 67% were satisfied by the outcome; however, progression of arthritis was noted in 35% in the radiological examination at 5 to 6 years after surgery.
3. Meniscus Repair
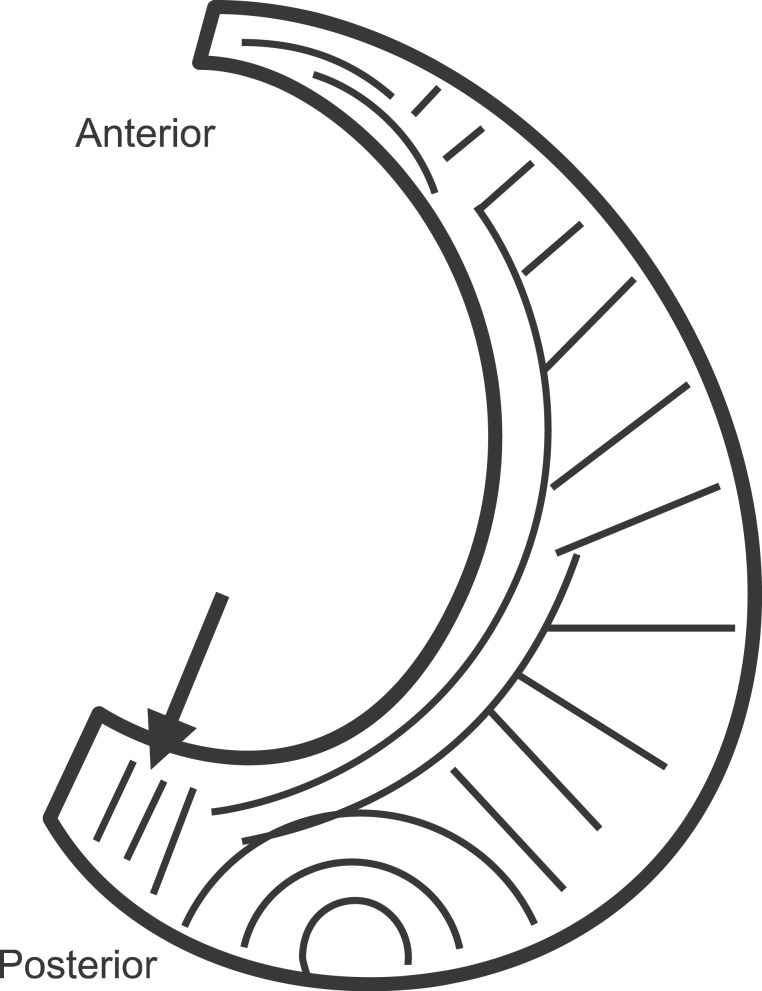
Growing dissatisfaction with partial meniscectomy as a treatment for MMPRTs has led to an increasing interest in meniscal repair7,8,36). According to Arnoczky and Warren37) the posterior root has better blood supply via the perimeniscal capillary plexus and small vessels through the bony attachment site compared to the middle horn. In addition, due to the distinctive anatomical feature of the radial direction of collagen from the root, enough tensile strength can be maintained during suture repair, which allows for repair of the posterior root of the medial meniscus (Fig. 3)38). Further, the effort to restore hoop tension via suture has been shown to be important for delaying the progression of arthritis. Thus, this treatment protocol has been recommended for the past decade5,6,7).
Fig. 3.
The illustration shows collagenous fibrils of the medial meniscus. The black arrow indicates radial direction of collagenous fibrils at the posterior horn.
1) Surgical indications (Table 1)
Table 1.
Indications for Repair of Medial Meniscus Posterior Root Tears
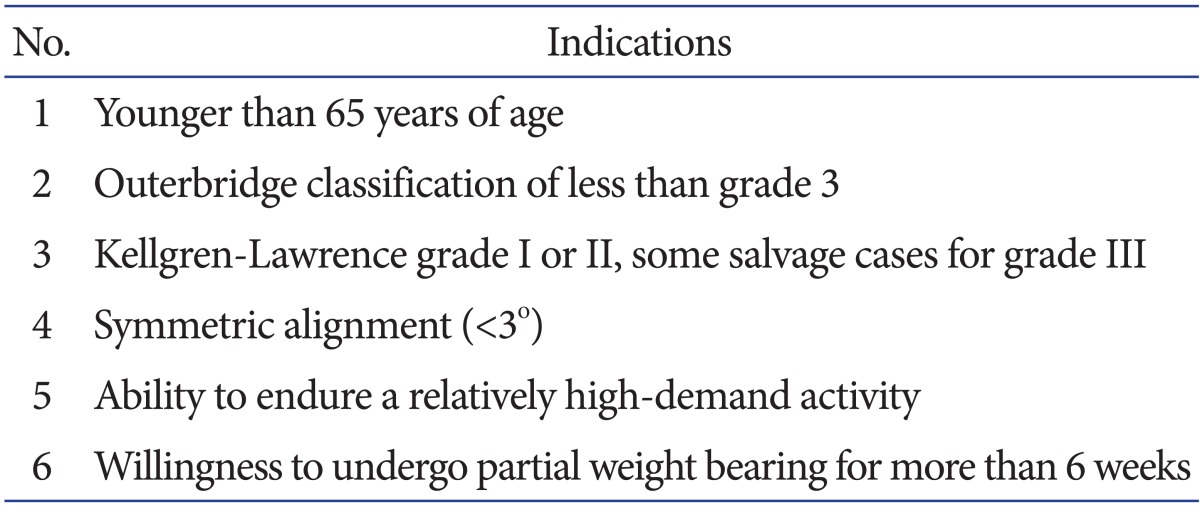
Since the MMPRT is a degenerative process, it is difficult to expect all tears to be fully repairable. Further, as suturing is a difficult technique, tears to be sutured must be selectively determined and high quality suturing should be executed7). In general, the candidates for meniscus repair are those who are active, have a standard alignment of lower extremity (less than 3° varus), mild progression of arthritis (below Kellgren-Lawrence grade II), mild subluxation of the meniscus, or symptoms persistent for 1-3 months even after conservative treatment, and agree to partial weight bearing with a crutch for 6 weeks and postoperative rehabilitation for 3 months7,8,9,24,26). Those with severe medial joint space narrowing, more than 3° of varus deformity, grade 3 or 4 arthrosis are not suitable for suture repair6,7,39). Thus, careful consideration should be taken.
2) Surgical techniques and clinical results
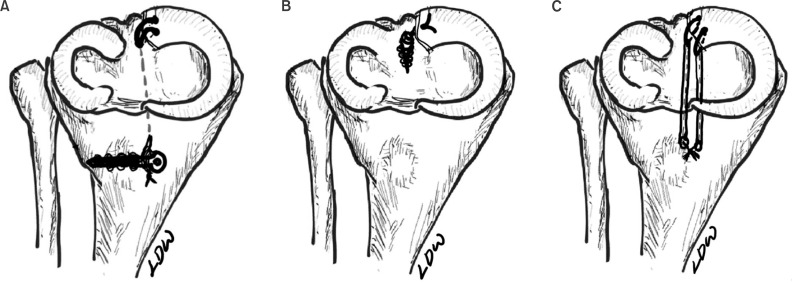
Most MMPRT repairs involve suturing around the region of tear where the sutures are pulled out and fixed around the tibia through simple stitches8,9,40,41). Shino et al.42) first introduced the idea of pull-out repair of the posterior attachment of the lateral meniscus by making a 5-mm trans-tibial hole. Raustol et al.43) used a similar method on a young patient for refixation of the medial meniscal ossicle. Recently, pull-out suture methods have been described in comprehensive studies on MMPRT repairs. For example, Kim et al.44) used two Ethibond No.2 sutures that were pulled out and fixed to the medial side of the tibia as in a post-tie technique using cortical screws (Fig. 4A). In other approaches, Choi et al.45) used a suture anchor for fixation of the MMPRT (Fig. 4B), and Ahn et al.46) used two tibial tunnels to fix PDS sutures (Johnson & Johnson Company, Somerville, NJ, USA) on the opposite side of the MMPRT (Fig. 4C). Unfortunately, the limited and non-overlapping clinical data in these reports make informative comparison difficult.
Fig. 4.
The illustrations demonstrate different surgical techniqes for MMPRT: (A) pullout suture repair with simple stitches and cortical screw fixation; (B) suture anchor repair; and (C) double trans-osseous pullout suture repair with simple stitches.
Most of the recent clinical studies on the repair of MMPRTs used 2-3 sutures (PDS or Ethibond) for radial tears in the pull-out suture technique, where the sutures are fixed to the medial tibia through the tibial guide tunnel, and some others used suture anchors (Table 2).
Table 2.
Overview of Surgical Techniques and Results of Medial Meniscus Posterior Root Tear Repair
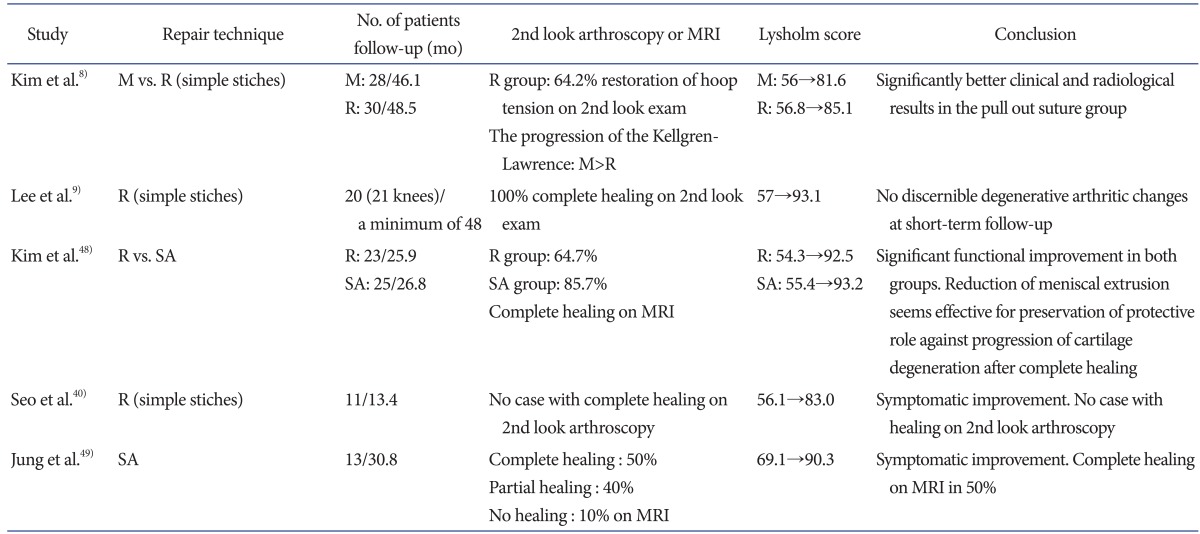
MRI: magnetic resonance imaging, M: partial meniscectomy, R: pull out suture, SA: suture anchor.
After surgical repair using the above-described technique, Kim et al.8) found enhanced clinical results in patients who underwent a meniscal repair, as opposed to those who had partial meniscectomy, in terms of the Lysholm score, radiological findings, joint space narrowing, and level of arthritis progression as determined by Kellgren-Lawrence grade change. The clinical findings were gathered at a mean follow-up period of 46.1 months from 30 and 28 patients who underwent either meniscal repair or partial meniscectomy, respectively. Among the patients who underwent a meniscal repair, 93.3% had MRI evidence of complete healing, and 14 of these underwent 2nd look arthroscopy, which showed normal fixed intensity in 64.3% and restoration of hoop tension in 71.4%. Along with the results of the patients they had performed repair on, they analyzed the results of other studies on MMPRT repair in particularly young patients with combined multiple ligament injuries: they found that clinical results were better in young patients than in older patients. Thus, they recommended active treatment for those with multiple ligament injuries and meniscal damage if they were especially of young age47). Lee et al.9) evaluated 20 patients for a minimum follow-up of 24 months after meniscal repair using simple stitches. They confirmed complete healing in 100% of the patients, enhancement of Lysholm score from 57 to 93.1, and no progression of arthritis. Kim et al.48) compared the pull-out suture technique group and the suture anchor technique group and found MRI evidence of complete healing in 64.7% and 83.7%, respectively and improvement of Lysholm score in 92.5% and 93.2%, respectively. Although the clinical findings did not show any difference between the two groups, a greater degree of healing was seen in the suture anchor technique group. In contrast, Seo et al.40) reported that in spite of the improvement of Lysholm score from 56.1 to 83.0 in 11 patients at a mean postoperative follow-up of 13.4 months, complete healing was not observed in any of the cases in the second-look arthroscopy evaluation, which only showed 5 loose repairs, 4 scar tissue induced repairs, and 2 failed repairs.
Jung et al.49) used suture anchors for the repair of MMPRTs and reported that the average Lysholm score was improved from 69.1 to 90.3 at a mean postoperative follow-up of 30.8 months, although only 50% of the 13 patients showed complete healing on the follow-up MRI.
Despite good clinical results of MMPRT repairs, actual anatomic reconstruction is not achieved and the risk of arthritis remains due to weak tensile strength of simple stitches and inability of degenerative tears to recover by the natural healing process8,11,26,39,40,50,51). After meniscus repair using simple stitches, Seo et al.40) found suture relaxation, tissue slack and degeneration, and loose healing in the second-look arthroscopy evaluation.
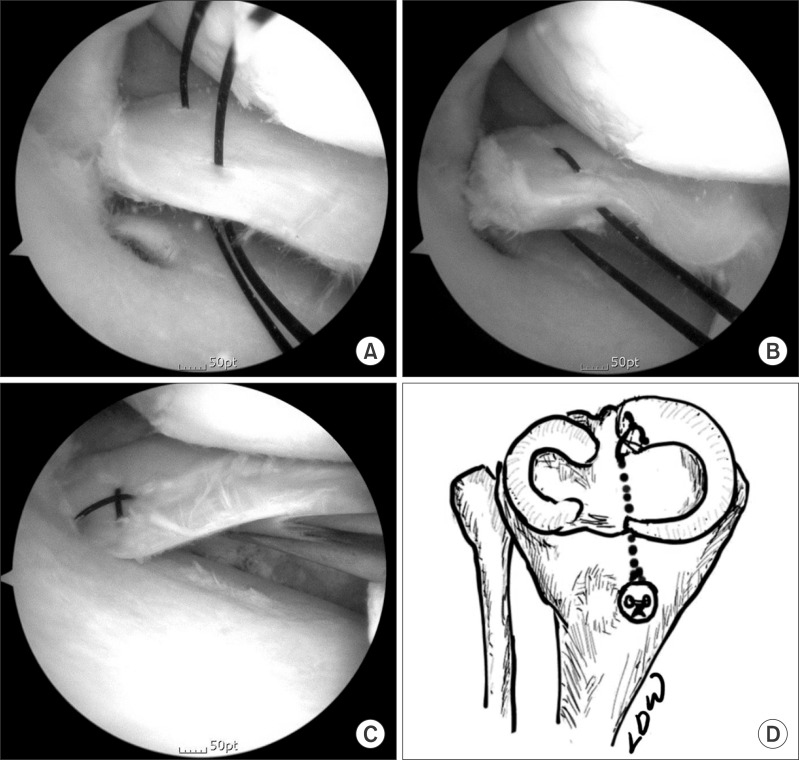
To overcome such problems, arthroscopic MMPRT repair methods with greater holding power and tensile strength should be investigated. The surgical methods used for repair of the rotator cuff of the shoulder are similar to those for MMPRT repairs. Among simple stitches, horizontal stitches, and the modified Mason-Allen approach, the Mason-Allen approach has been known to show the strongest tensile strength and holding power in rotator cuff repairs50,51,52,53). Its adaptability to MMPRT treatment is feasible as the simple surgical method allows easy application to the knee50,51,52,53). Lee et al.53) reported the use of this modified Mason-Allen stitch in MMPRT repair was successful (Fig. 5).
Fig. 5.
The modified Mason-Allen stitch was used for repair of the medial meniscus root tear of the right knee. (A) Two simple vertical stitches were placed 3-5 mm medial to the torn margin. (B) A horizontal loop was made by using the shuttle relay method of tying the superior ends of the vertical sutures and pulling out the inferior ends of the vertical sutures. (C) A simple vertical stitch was placed across the center of the horizontal loop, and then a cruciate-shaped stitch, so called modified Mason-Allen stitch, was made. (D) The illustration shows the ends of the strands are tied to a Henson button with adequate tension to allow physiological excursion instead of rigid fixation.
4. High Tibial Osteotomy
Moon et al.26) reported that the patients with >5° varus alignment showed poorer results in terms of Lysholm scores and VAS satisfaction than those with <5° varus alignment after pullout repair of MMPRTs. Nha et al.54) found that high tibial corrective osteotomy in patients with combined MMPRT and varus deformity resulted in acceptable clinical improvements in 20 patients. Of these, 10 patients showed complete repair at a second-look arthroscopic examination, while 6 showed incomplete repair. Their results imply that even without a meniscal repair, medial decompression through corrective osteotomy and appropriate conservative treatment can exert positive effects on the MMPRT.
There may be debates on which surgical option is more effective for patients with combined MMPRT and varus deformity, either isolated high tibial osteotomy or concomitant repair for MMPRT.
Future Research Directions
The biomechanical and clinical consequences of the MMPRT have been recently elucidated. The pathophysiology, clinical outcomes of treatment, and appropriate treatment methods for MMPRT have yet to be investigated comprehensively7,11,20,39). Presently, it is obvious that the MMPRT is more prevalent in the floor-based lifestyle areas and in the older generation who has presumably adopted the floor-based lifestyle for a longer period than the younger generation. Another characteristic mark of the MMPRT is its vulnerability to even a trivial injury due to age-dependent degeneration in the susceptible population. Despite the high incidence of MMPRTs, the awareness of the need for proper treatment is a relatively recent phenomenon. Helpful clinical data on repairs using novel treatment methods have become available in the recent years7,8,9,48,53). In the future, multi-center randomized prospective trials should be implemented to compare the clinical outcomes of various methods for the repair of MMPRTs and to ultimately determine the standard procedure for MMPRT repair.
Conclusions
The MMPRT results in the inability to withstand hoop stress and requires repair. Although the understanding of the biomechanical properties of the MMPRT has been increasing and diagnosis rates are improving, there are still controversies whether repair techniques can restore the main function of the normal meniscus and which suture technique is the most effective for MMPRT repair.
The current trends of the MMPRT repair are suture anchors and pullout sutures if the patient meets the indications. Further advances in surgical techniques should continue to be made so as to restore near normal knee kinematics.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Villegas DF, Hansen TA, Liu DF, Donahue TL. A quantitative study of the microstructure and biochemistry of the medial meniscal horn attachments. Ann Biomed Eng. 2008;36:123–131. doi: 10.1007/s10439-007-9403-x. [DOI] [PubMed] [Google Scholar]
- 2.Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16:849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 3.Kan A, Oshida M, Oshida S, Imada M, Nakagawa T, Okinaga S. Anatomical significance of a posterior horn of medial meniscus: the relationship between its radial tear and cartilage degradation of joint surface. Sports Med Arthrosc Rehabil Ther Technol. 2010;2:1. doi: 10.1186/1758-2555-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vedi V, Williams A, Tennant SJ, Spouse E, Hunt DM, Gedroyc WM. Meniscal movement. An in-vivo study using dynamic MRI. J Bone Joint Surg Br. 1999;81:37–41. doi: 10.1302/0301-620x.81b1.8928. [DOI] [PubMed] [Google Scholar]
- 5.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 6.Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus: surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2):257–270. doi: 10.2106/JBJS.I.00500. [DOI] [PubMed] [Google Scholar]
- 7.Vyas D, Harner CD. Meniscus root repair. Sports Med Arthrosc. 2012;20:86–94. doi: 10.1097/JSA.0b013e31825186ca. [DOI] [PubMed] [Google Scholar]
- 8.Kim SB, Ha JK, Lee SW, Kim DW, Shim JC, Kim JG, Lee MY. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27:346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25:951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7:297–300. doi: 10.1016/0749-8063(91)90131-g. [DOI] [PubMed] [Google Scholar]
- 11.Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20:373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Nha KW, Oh HK, Kim DH, Kim YH. MR findings of the radial tear of medial meniscus. J Korean Knee Soc. 2005;17:147–152. [Google Scholar]
- 13.Moon JS, Shim JC, Seo JG, Kim JG. MRI findings of root tear of medial meniscus. J Korean Knee Soc. 2005;17:160–164. [Google Scholar]
- 14.Habata T, Uematsu K, Hattori K, Takakura Y, Fujisawa Y. Clinical features of the posterior horn tear in the medial meniscus. Arch Orthop Trauma Surg. 2004;124:642–645. doi: 10.1007/s00402-004-0659-4. [DOI] [PubMed] [Google Scholar]
- 15.Thompson WO, Thaete FL, Fu FH, Dye SF. Tibial meniscal dynamics using three-dimensional reconstruction of magnetic resonance images. Am J Sports Med. 1991;19:210–215. doi: 10.1177/036354659101900302. [DOI] [PubMed] [Google Scholar]
- 16.Bae JH, Paik NH, Park GW, Yoon JR, Chae DJ, Kwon JH, Kim JI, Nha KW. Predictive value of painful popping for a posterior root tear of the medial meniscus in middle-aged to older Asian patients. Arthroscopy. 2013;29:545–549. doi: 10.1016/j.arthro.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 17.Henry S, Mascarenhas R, Kowalchuk D, Forsythe B, Irrgang JJ, Harner CD. Medial meniscus tear morphology and chondral degeneration of the knee: is there a relationship? Arthroscopy. 2012;28:1124–1134. doi: 10.1016/j.arthro.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 18.Sung JH, Ha JK, Lee DW, Seo WY, Kim JG. Meniscal extrusion and spontaneous osteonecrosis with root tear of medial meniscus: comparison with horizontal tear. Arthroscopy. 2013;29:726–732. doi: 10.1016/j.arthro.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 19.Guermazi A, Hayashi D, Jarraya M, Roemer FW, Zhang Y, Niu J, Crema MD, Englund M, Lynch JA, Nevitt MC, Torner JC, Lewis CE, Felson DT. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology. 2013;268:814–821. doi: 10.1148/radiol.13122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ, Jung KA. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40:1606–1610. doi: 10.1177/0363546512447792. [DOI] [PubMed] [Google Scholar]
- 21.Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ, Ra HJ. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21:2121–2125. doi: 10.1007/s00167-012-2182-4. [DOI] [PubMed] [Google Scholar]
- 22.Seo JH, Li G, Shetty GM, Kim JH, Bae JH, Jo ML, Kim JS, Lee SJ, Nha KW. Effect of repair of radial tears at the root of the posterior horn of the medial meniscus with the pullout suture technique: a biomechanical study using porcine knees. Arthroscopy. 2009;25:1281–1287. doi: 10.1016/j.arthro.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 23.Nha KW, Jo JH, Lee DB. Clinical results of the radial tear of posterior root of medial meniscus. J Korean Arthrosc Soc. 2007;11:128–133. [Google Scholar]
- 24.Kim YM, Joo YB, Cha SM, Hwang JM. Role of the mechanical axis of lower limb and body weight in the horizontal tear and root ligament tear of the posterior horn of the medial meniscus. Int Orthop. 2012;36:1849–1855. doi: 10.1007/s00264-012-1596-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shelbourne KD, Dickens JF. Digital radiographic evaluation of medial joint space narrowing after partial meniscectomy of bucket-handle medial meniscus tears in anterior cruciate ligament-intact knees. Am J Sports Med. 2006;34:1648–1655. doi: 10.1177/0363546506288019. [DOI] [PubMed] [Google Scholar]
- 26.Moon HK, Koh YG, Kim YC, Park YS, Jo SB, Kwon SK. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40:1138–1143. doi: 10.1177/0363546511435622. [DOI] [PubMed] [Google Scholar]
- 27.Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26:1602–1606. doi: 10.1016/j.arthro.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Lee SY, Jee WH, Kim JM. Radial tear of the medial meniscal root: reliability and accuracy of MRI for diagnosis. AJR Am J Roentgenol. 2008;191:81–85. doi: 10.2214/AJR.07.2945. [DOI] [PubMed] [Google Scholar]
- 29.Choi SH, Bae S, Ji SK, Chang MJ. The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc. 2012;20:2098–2103. doi: 10.1007/s00167-011-1794-4. [DOI] [PubMed] [Google Scholar]
- 30.De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192:480–486. doi: 10.2214/AJR.08.1300. [DOI] [PubMed] [Google Scholar]
- 31.Lee YG, Shim JC, Choi YS, Kim JG, Lee GJ, Kim HK. Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr. 2008;32:452–457. doi: 10.1097/RCT.0b013e31812f4eb0. [DOI] [PubMed] [Google Scholar]
- 32.Piscaer TM, Sandker M, van der Jagt OP, Verhaar JA, de Jong M, Weinans H. Real-time assessment of bone metabolism in small animal models for osteoarthritis using multi pinhole-SPECT/CT. Osteoarthritis Cartilage. 2013;21:882–888. doi: 10.1016/j.joca.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 33.Lim HC, Bae JH, Wang JH, Seok CW, Kim MK. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2010;18:535–539. doi: 10.1007/s00167-009-0891-0. [DOI] [PubMed] [Google Scholar]
- 34.Neogi DS, Kumar A, Rijal L, Yadav CS, Jaiman A, Nag HL. Role of nonoperative treatment in managing degenerative tears of the medial meniscus posterior root. J Orthop Traumatol. 2013;14:193–199. doi: 10.1007/s10195-013-0234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Magee T, Shapiro M, Williams D. Prevalence of meniscal radial tears of the knee revealed by MRI after surgery. AJR Am J Roentgenol. 2004;182:931–936. doi: 10.2214/ajr.182.4.1820931. [DOI] [PubMed] [Google Scholar]
- 36.Han SB, Shetty GM, Lee DH, Chae DJ, Seo SS, Wang KH, Yoo SH, Nha KW. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26:1326–1332. doi: 10.1016/j.arthro.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 37.Arnoczky SP, Warren RF. Microvasculature of the human meniscus. Am J Sports Med. 1982;10:90–95. doi: 10.1177/036354658201000205. [DOI] [PubMed] [Google Scholar]
- 38.Petersen W, Tillmann B. Collagenous fibril texture of the human knee joint menisci. Anat Embryol (Berl) 1998;197:317–324. doi: 10.1007/s004290050141. [DOI] [PubMed] [Google Scholar]
- 39.Kim YM, Joo YB. Pullout failure strength of the posterior horn of the medial meniscus with root ligament tear. Knee Surg Sports Traumatol Arthrosc. 2013;21:1546–1552. doi: 10.1007/s00167-012-2131-2. [DOI] [PubMed] [Google Scholar]
- 40.Seo HS, Lee SC, Jung KA. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39:99–107. doi: 10.1177/0363546510382225. [DOI] [PubMed] [Google Scholar]
- 41.Park YS, Moon HK, Koh YG, Kim YC, Sim DS, Jo SB, Kwon SK. Arthroscopic pullout repair of posterior root tear of the medial meniscus: the anterior approach using medial collateral ligament pie-crusting release. Knee Surg Sports Traumatol Arthrosc. 2011;19:1334–1336. doi: 10.1007/s00167-011-1435-y. [DOI] [PubMed] [Google Scholar]
- 42.Shino K, Hamada M, Mitsuoka T, Kinoshita H, Toritsuka Y. Arthroscopic repair for a flap tear of the posterior horn of the lateral meniscus adjacent to its tibial insertion. Arthroscopy. 1995;11:495–498. doi: 10.1016/0749-8063(95)90207-4. [DOI] [PubMed] [Google Scholar]
- 43.Raustol OA, Poelstra KA, Chhabra A, Diduch DR. The meniscal ossicle revisited: etiology and an arthroscopic technique for treatment. Arthroscopy. 2006;22:687. doi: 10.1016/j.arthro.2005.12.022. [DOI] [PubMed] [Google Scholar]
- 44.Kim YM, Rhee KJ, Lee JK, Hwang DS, Yang JY, Kim SJ. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006;22:795. doi: 10.1016/j.arthro.2005.12.040. [DOI] [PubMed] [Google Scholar]
- 45.Choi NH, Son KM, Victoroff BN. Arthroscopic all-inside repair for a tear of posterior root of the medial meniscus: a technical note. Knee Surg Sports Traumatol Arthrosc. 2008;16:891–893. doi: 10.1007/s00167-008-0581-3. [DOI] [PubMed] [Google Scholar]
- 46.Ahn JH, Wang JH, Lim HC, Bae JH, Park JS, Yoo JC, Shyam AK. Double transosseous pull out suture technique for transection of posterior horn of medial meniscus. Arch Orthop Trauma Surg. 2009;129:387–392. doi: 10.1007/s00402-008-0639-1. [DOI] [PubMed] [Google Scholar]
- 47.Kim YJ, Kim JG, Chang SH, Shim JC, Kim SB, Lee MY. Posterior root tear of the medial meniscus in multiple knee ligament injuries. Knee. 2010;17:324–328. doi: 10.1016/j.knee.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 48.Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27:1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 49.Jung YH, Choi NH, Oh JS, Victoroff BN. All-inside repair for a root tear of the medial meniscus using a suture anchor. Am J Sports Med. 2012;40:1406–1411. doi: 10.1177/0363546512439181. [DOI] [PubMed] [Google Scholar]
- 50.Ma CB, MacGillivray JD, Clabeaux J, Lee S, Otis JC. Biomechanical evaluation of arthroscopic rotator cuff stitches. J Bone Joint Surg Am. 2004;86:1211–1216. doi: 10.2106/00004623-200406000-00013. [DOI] [PubMed] [Google Scholar]
- 51.Baleani M, Ohman C, Guandalini L, Rotini R, Giavaresi G, Traina F, Viceconti M. Comparative study of different tendon grasping techniques for arthroscopic repair of the rotator cuff. Clin Biomech (Bristol, Avon) 2006;21:799–803. doi: 10.1016/j.clinbiomech.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 52.Gerber C, Schneeberger AG, Beck M, Schlegel U. Mechanical strength of repairs of the rotator cuff. J Bone Joint Surg Br. 1994;76:371–380. [PubMed] [Google Scholar]
- 53.Lee DW, Jang SH, Ha JK, Kim JG, Ahn JH. Meniscus root refixation technique using a modified Mason-Allen stitch. Knee Surg Sports Traumatol Arthrosc. 2013;21:654–657. doi: 10.1007/s00167-012-1992-8. [DOI] [PubMed] [Google Scholar]
- 54.Nha KW, Lee YS, Hwang DH, Kwon JH, Chae DJ, Park YJ, Kim JI. Second-look arthroscopic findings after open-wedge high tibia osteotomy focusing on the posterior root tears of the medial meniscus. Arthroscopy. 2013;29:226–231. doi: 10.1016/j.arthro.2012.08.027. [DOI] [PubMed] [Google Scholar]