Abstract
Background
Three distinct shortages of the generic drug leucovorin, a reduced form of folic acid used in several chemotherapy regimens, were reported by the US Food and Drug Administration (FDA) between 2008 and 2014. Levoleucovorin, an alternative therapy to leucovorin, failed to demonstrate superiority over leucovorin in clinical trials and is substantially more expensive.
Objective
To calculate the impact of the leucovorin shortages on primary treatment costs to patients and a health plan, and to present strategies for health plans to deal with future drug shortages.
Methods
This retrospective descriptive study was conducted using Humana's Medicare Advantage prescription drug plan administrative claims database between January 1, 2009, and December 31, 2012. A total of 1542 patients with at least 1 medical or pharmacy claim for either leucovorin or levoleucovorin during the first 3 months of the respective plan year (between 2009 and 2012) who had continuous enrollment for the entirety of the same plan year, were included in this study. Trends in primary treatment costs—defined as the drug cost of leucovorin or levoleucovorin—over the 4-year evaluation period were assessed. The mean annual patient out-of-pocket (OOP) costs and the mean plan-paid per member per month (PMPM) costs were also calculated.
Results
The percentage of patients receiving leucovorin decreased annually, with a 15.8% drop from 2010 to 2011. This reduction was accompanied by a 6.6% increase in patients receiving levoleucovorin. The mean annual patient OOP costs were $167 to $714 higher for levoleucovorin than for leucovorin. Similarly, the mean plan-paid PMPM costs were higher (up to $1667 PMPM) for levoleucovorin than for leucovorin. The aggregate costs for the 2 drugs increased steadily, including the patient OOP costs and the plan-paid PMPM costs. The most prominent cost increase occurred between 2010 and 2011, with a 3.8-fold increase in patient OOP costs and a 5-fold increase in the plan-paid PMPM costs. This corresponded to the timing of the second leucovorin shortage announcement by the FDA in June 2010.
Conclusions
Health plans can play an important role in minimizing the impact of drug shortages by identifying the affected patient population, identifying therapeutic alternatives, assisting providers with alternative sourcing strategies when possible, adjusting approval processes, and implementing quality management or pathway programs.
Drug shortages continue to be a growing challenge in the United States, adversely affecting the quality of care and contributing to the rising healthcare costs. According to the US Food and Drug Administration (FDA), the number of annual drug shortages tripled from 61 in 2005 to 178 in 2010.1 More than 80% of these shortages were for lower-cost generic medications or injectable therapies used in critical therapeutic areas, such as oncology, infectious diseases, and central nervous system disorders.2,3 The negative clinical impact of drug shortages is manifested in the form of delays in therapy, increased risk for medication errors, and drug-related adverse events.4,5
The economic implications of shortages include increased medication and labor costs.4,5 It is estimated that drug shortages contribute $216 million annually to the rising healthcare costs because of the increased time and effort required to manage the shortages.6 A Drug Shortages Summit that was convened in 2010 by the American Society of Health-System Pharmacists (ASHP), the American Society of Anesthesiologists, the American Society of Clinical Oncology, and the Institute for Safe Medication Practices concluded that the causes of drug shortages are multifactorial.3 Although regulatory and legislative factors play a role, the most frequently cited causes are related to the drug supply chain.3 Upon the initial approval of the abbreviated or new drug applications, the FDA timeliness of drug approval can be unpredictable, which contributes to uncertainty in market demand and associated drug production capability. In addition, during drug production, manufacturers must comply with Good Manufacturing Practices, as well as with their own quality metrics; inability to comply with these standards is a major contributor to drug shortages. Finally, the business climate for marketing a medication can also affect drug shortages, such as a lower priority by a manufacturer being assigned to low profit margin generic drugs, agents being produced by a small number of manufacturers, and manufacturers choosing to discontinue a medication.3
KEY POINTS
-
▸
Drug shortages continue to be a challenge in the United States, adversely affecting the quality of care and contributing to the rising healthcare costs.
-
▸
This is the first study to calculate the economic impact of the shortages of generic leucovorin (a reduced form of folic acid used in several chemotherapy regimens) from 2009 to 2012 to patients and to a health plan.
-
▸
Levoleucovorin, which was approved by the FDA during the initial leucovorin shortage, failed to demonstrate clinical superiority to leucovorin and is marketed at a much higher price.
-
▸
During the 4-year study period, the rate of patients receiving leucovorin decreased annually, while the rate of patients receiving levoleucovorin increased.
-
▸
The mean annual patient OOP costs were $167 to $714 higher for levoleucovorin than for leucovorin.
-
▸
Similarly, the annual plan-paid costs per member for folic acid analogs increased significantly during the study period.
-
▸
Health plans can play an important role in minimizing the impact of drug shortages by identifying therapeutic alternatives, adjusting approval processes, and implementing quality management or pathway programs.
The causes of drug shortages are often interconnected.3 For example, if a generic drug is produced by only a few manufacturers, and one of them encounters production issues, the other manufacturers may experience increased demand for the drug, followed by insufficient production capacity, thus perpetuating the initial shortage.3 This interconnectedness is demonstrated by a shortage of the generic drug leucovorin, a reduced form of folic acid used in several chemotherapy regimens.7
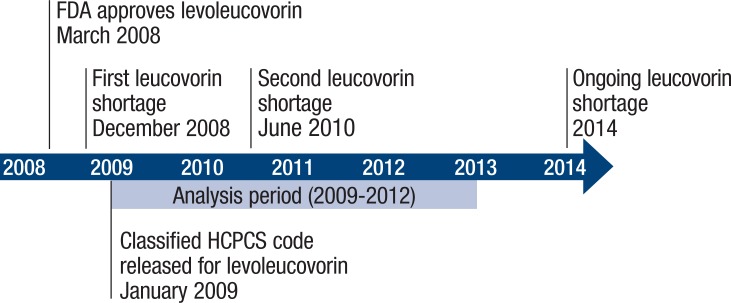
A shortage of leucovorin was first reported by the FDA in late 2008, citing manufacturing delays by Bedford Laboratories8 (Figure 1). Approximately 1 month later, Teva Pharmaceuticals, the only other manufacturer of leucovorin at that time, reported a shortage because of an increase in demand.9 This shortage was reported to be resolved by the spring of 2009, only to resurface 1 year later.10,11 Manufacturing delays were again cited as the cause of the 2010 shortage.11 The 2010 shortage was never clearly resolved, because Teva Pharmaceuticals and Bedford Laboratories could not meet the demand. In 2014, the FDA has reported that the leucovorin shortage remains ongoing.12
Figure 1.
Leucovorin Shortage Time Line
FDA indicates US Food and Drug Administration; HCPCS, Healthcare Common Procedure Coding System.
During the year of the initial leucovorin shortage in 2008, the FDA approved levoleucovorin (Fusilev), an active levo isomer that is marketed as an alternative to leucovorin.13 Although the availability of levoleucovorin reduces disruptions to patients, the levo isomer does not provide incremental clinical benefit. In a randomized controlled trial, a chemotherapy regimen containing levoleucovorin failed to demonstrate superiority to a regimen containing leucovorin in overall survival in patients with advanced metastatic colorectal cancer.14,15
In addition, a 2009 systematic literature review of 125 studies concluded that levoleucovorin had similar efficacy and tolerability compared with racemic leucovorin.16 Despite the lack of clinical benefits over leucovorin, levoleucovorin is priced substantially higher than leucovorin. In 2013, the Medicare allowable monthly price of levoleucovorin treatment was nearly $2500 compared with less than $200 for leucovorin.17 Therefore, patients who were unable to get leucovorin during the shortage did have access to an alternative therapy, albeit a therapy with a substantially higher price, and with no demonstrated incremental efficacy or tolerability benefits.
Previous surveys of health system pharmacy directors have concluded that drug shortages result in increased medication and labor costs4,5; however, no study to our knowledge has directly quantified the impact of a single drug shortage on treatment costs to the payer and the patient. Therefore, the objective of this study was to evaluate the impact of the leucovorin shortage on primary treatment costs during a 4-year period. In addition, we discuss strategies for health plans to manage drug shortages.
Methods
Design and Data Source
This retrospective descriptive study was conducted using the Medicare Advantage prescription drug plan population from Humana's administrative claims database between January 1, 2009, and December 31, 2012. The start date was selected to correspond with the first leucovorin shortage announcement in December 2008. In addition, the levoleucovorin Healthcare Common Procedure Coding System (HCPCS) billing code was released on January 1, 2009; before this date, claims for levoleucovorin could not have been accurately identified in the data set.
The Humana research database includes pharmacy claims, medical claims, and enrollment data for approximately 6 million members from all 50 states. Pharmacy claims data include adjudication information from the pharmacy related to the member's prescription, including the drug name, national drug codes, date of prescription fill, quantity and day supply of medication plan-paid amount, and member out-of-pocket (OOP) costs for the prescription.
For this study, drug claims were also identified through outpatient physician office medical claims using the HCPCS codes (J0640 for leucovorin; J0641 for levoleucovorin). The plan-paid amount and member OOP costs were available for all claims included in the analysis. Enrollment data include information on the member demographics and coverage start and end dates. This retrospective descriptive study was approved by the Schulman Associates Institutional Review Board.
Study Population Selection
Patients included in the analysis were aged 19 to 89 years and had to have at least 1 medical or pharmacy claim (individuals aged <65 years with disabilities may be covered by Medicare; depending on the plan benefit design, leucovorin and levoleucovorin may be processed through medical or pharmacy claims) for leucovorin or for levoleucovorin during the first 3 months of each respective plan year and continuous enrollment for the entirety of the same plan year. The medical or pharmacy claim was required to be in the first 3 months of a respective plan year so that a continuous treatment cost trend could be established throughout each plan year. Patients were excluded if they had at least 1 inpatient or outpatient hospital claim for leucovorin or levoleucovorin in which the cost of the medication was not itemized.
Overall, 3 cohorts were defined based on receipt of the drug index in the respective plan year—(1) leucovorin only, (2) levoleucovorin only, and (3) mixed treatment (ie, patients who received leucovorin and levoleucovorin during the plan year). The number of patients receiving leucovorin in 2008 was reported as the reference point.
Outcomes and Analyses
Trends in the primary treatment costs during the 4-year evaluation period are reported. The primary treatment costs were defined as the drug cost of leucovorin or levoleucovorin identified through medical or pharmacy claims, depending on which benefit covered the drug in the various plan designs.
The primary treatment costs to the patient and to the plan are reported separately. The patient OOP costs were defined as the costs incurred by the member either as a copay or coinsurance for each treatment, and are reported as mean annual costs. The plan-paid costs were defined as the amount paid by the plan (ie, drug cost minus patient OOP cost) and are reported as the mean per member per month (PMPM) costs. The mean annual patient OOP costs and the mean plan-paid PMPM costs are reported for each study year and for each of the 3 cohorts. The results are also reported in aggregate for the folic acid analogs combined. All analyses were performed using SAS Enterprise Guide, version 4.3 (SAS Institute; Cary, NC).
Results
Patient Characteristics
A total of 1542 unique patients received a folic acid analog between January 2009 and December 2012 (Table). The average age of the study population was 71 years and the majority (57.8%) of them were male. More than 60% of the patients resided in the southern region of the United States, a trend that is consistent with the geographic distribution of the health plan. During the study period, the percentage of patients receiving low-income subsidy ranged from 17.0% to 18.7%, and the percentage of patients who were dual-eligible for Medicare and Medicaid ranged from 0.6% to 1.9%.
Table.
Study Population Characteristics
| Characteristic | Year 1: 2009 (N = 359) | Year 2: 2010 (N = 395) | Year 3: 2011 (N = 365) | Year 4: 2012 (N = 423) |
|---|---|---|---|---|
| Age at first claim, mean (SD) | 71 (7.7) | 71 (6.6) | 70 (6.9) | 71 (6.9) |
| Female, % | 43.7 | 42.5 | 37.3 | 45.4 |
| Caucasian, % | 77.2 | 83.8 | 81.9 | 83.7 |
| Dual-eligible for Medicare + Medicaid, % | 0.6 | 1.3 | 1.9 | 1.7 |
| Low-income subsidy, % | 17.0 | 18.7 | 17.5 | 18.0 |
| Geographic region | ||||
| Northeast, % | 1.9 | 1.0 | 1.1 | 1.7 |
| Midwest, % | 24.2 | 22.3 | 20.5 | 23.4 |
| South, % | 62.7 | 68.9 | 69.9 | 65.7 |
| West, % | 11.1 | 7.8 | 8.5 | 9.2 |
| Primary treatment | ||||
| Leucovorin only, N (%) | 326 (90.8) | 364 (92.2) | 279 (76.4) | 294 (69.5) |
| Levoleucovorin only, N (%) | 6 (1.7) | 3 (0.8) | 27 (7.4) | 76 (18.0) |
| Mixed treatment, N (%) | 27 (7.5) | 28 (7.1) | 59 (16.2) | 53 (12.5) |
SD indicates standard deviation.
Folic Acid Utilization
There were 380 patients who received leucovorin in the reference year (ie, 2008). During the evaluation period, there was a decreasing trend in the percentage of patients receiving leucovorin from 2010 to 2011 (absolute value of 15.8%; Table). This was accompanied by an increase in the percentage of patients receiving levoleucovorin (6.6%) and mixed treatment (9.1%). These trends for leucovorin and levoleucovorin persisted in 2012.
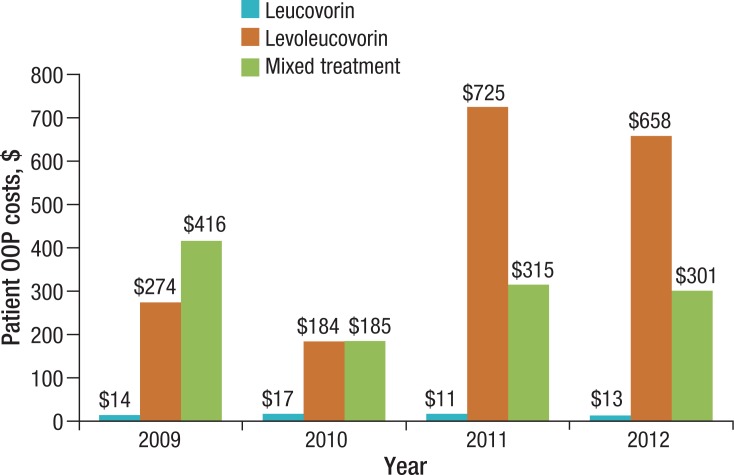
Patient OOP Costs
The mean annual patient OOP costs were between $167 and $714 higher for levoleucovorin than for leucovorin (Figure 2). Between 2009 and 2011, the mean annual patient OOP costs for levoleucovorin increased from $275 to $725, a 2.65-fold increase. Costs in the mixed-treatment group fluctuated during the 4-year period, and in 2009 the mean annual patient OOP costs were higher for the mixed-treatment group ($416) than for either the leucovorin-alone ($14) or the levoleucovorin-alone ($274) cohort.
Figure 2.
Mean Annual Patient OOP Primary Treatment Costs
OOP indicates out-of-pocket.
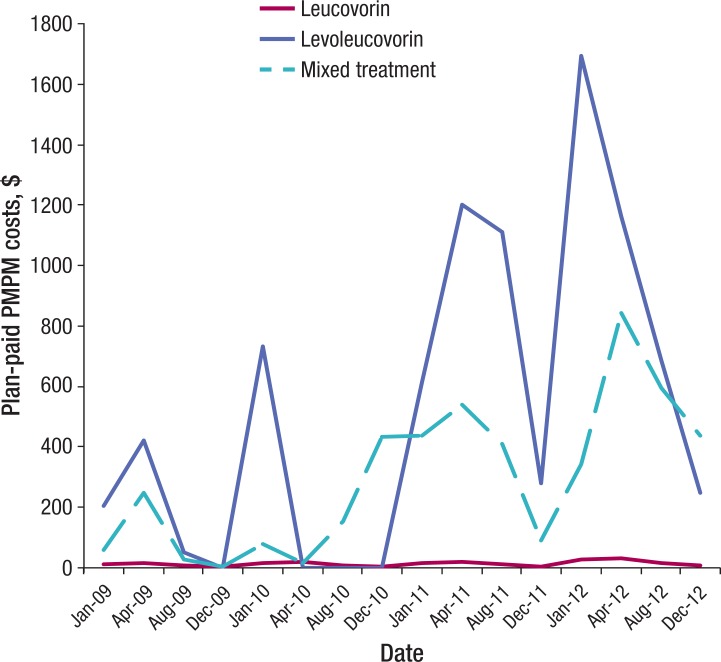
Plan-Paid Costs
Similar to the trends in the mean annual patient OOP costs, the mean plan-paid PMPM costs for levoleucovorin were higher (up to $1667 PMPM higher) than for leucovorin (Figure 3). The plan-paid costs for levoleucovorin and the mixed-treatment group increased steadily over time, with noticeable peaks in the first quarter of each year.
Figure 3.
Mean Plan-Paid PMPM Primary Treatment Costs
PMPM indicates per member per month.
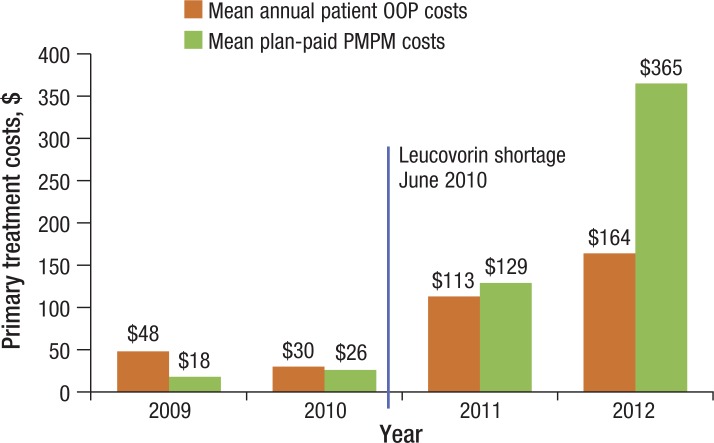
Aggregate Folic Acid Analog Costs
When the combined costs of leucovorin and levoleucovorin were considered in aggregate, the mean annual patient OOP costs and the mean plan-paid PMPM costs increased annually between 2009 and 2012 (Figure 4). The most prominent increase occurred between 2010 and 2011, with a 3.8-fold increase in patient OOP costs and a 5-fold increase in plan-paid PMPM costs, corresponding to the timing of the second leucovorin shortage announcement by the FDA.11
Figure 4.
Primary Treatment Costs for Folic Acid Analogs
OOP indicates out-of-pocket; PMPM, per member per month.
Discussion
This retrospective descriptive analysis of a Medicare Advantage prescription drug plan population reveals trends in the patient OOP costs and plan costs for leucovorin and levoleucovorin during a 4-year period of sequential leucovorin shortages. We found that patients and the health plan experienced an annual increase in costs for therapy. The most notable increase occurred between 2010 and 2011, which corresponded to the second leucovorin shortage (in June 2010) and to a shift from leucovorin to levoleucovorin use in the study population.
Several factors may have contributed to the trends reported in this study. First, plan benefit designs directly affect patient OOP costs. Traditionally, patients covered by Medicare have a 20% coinsurance for medications that are covered by Medicare Part B; therefore, patient OOP costs directly correlate with medication unit costs. However, this study population was highly concentrated in the southern United States; the most common benefit design of Humana in that region includes a 0% coinsurance for preferred Part B medications. During the study period, leucovorin was eligible for 0% coinsurance, but levoleucovorin was not. Therefore, patients receiving leucovorin had little fluctuation in their OOP costs, but those receiving levoleucovorin were greatly affected by price changes. These variations in benefit design may also explain the fluctuations observed in OOP costs for the mixed-treatment cohort.
Price fluctuations during the study period might have also contributed to the observed trends. For example, the Medicare allowable price for levoleucovorin was reduced during the second and third quarters of 2010 to provide relief at the onset of the second leucovorin shortage.18 In late 2010, the levoleucovorin price began to increase steadily, from an average selling price of $0.69 in July 2010 to $1.73 in July 2011.18 This increase coincided with the FDA approval of a new indication for levoleucovorin for use in combination chemotherapy with 5-fluorouracil for the palliative management of patients with advanced metastatic colorectal cancer in April 2011.19 The newly approved indication might have been another factor related to the increased use of levoleucovorin beginning in 2011.
Health Plan Strategies to Address Drug Shortages
Opportunities exist for health plans to consider alternative strategies to mitigate the effects of drug shortages. ASHP offers guidelines for the management of drug shortages in hospitals and in other health systems.20 Although there are no parallel guidelines for health plans, Humana and its insured population have benefited from implementing these concepts in the health plan setting. For example, Humana proactively worked to identify alternative sources for providers who did not have access to leucovorin through their usual suppliers, when possible. Then, Humana pharmacists conducted a therapeutic assessment to identify the affected patient population and the therapeutic alternative. The clinical review process was also adjusted to facilitate approval when pre-scribers indicated that they were using levoleucovorin because of the shortage.
In addition, it is important for health plans to monitor drug shortages even after these shortages are resolved. Under some reimbursement models, physicians may lack financial incentive to return patients to generic medications, even though returning to the original medication could result in reduced costs for the patient and the plan. Therefore, health plans may need to implement strategies that help facilitate the reutilization of the original medication once a shortage is resolved, unless it is not clinically warranted. Traditional pharmacy utilization management techniques, such as step therapy, may not be possible for some drugs and are prohibited for drugs billed through Medicare Part B benefits. One possible strategy is to adjust the approval duration (eg, from 6 months to 3 months) to allow for reassessment of a drug supply during a drug shortage.
Alternative methods include quality management or pathway programs, which often incentivize providers to use the most cost-effective therapy supported by an evidence-based approach. Humana has an Oncology Quality Management Program that is based on evidence-based care standards and uses a counseling model within traditional preauthorization management.21 The program is administered by New Century Health and Oncology Analytics in different markets.21,22 Future research should evaluate the impact of such programs in relation to drug shortages.
Limitations
This is a descriptive study of trends in patient and health plan costs during a 4-year period and has important limitations. First, given the descriptive nature of this study, we do not attempt to assign association or causation of cost trends to the leucovorin shortage alone.
The study design might have influenced some observations. Specifically, monthly analysis of mean plan-paid PMPM costs revealed peaks during the first quarter of each year, particularly for the levoleucovorin and mixed treatment cohorts. This pattern was likely associated with the requirement that all patients have a claim during the first 3 months of the year, and may have also been influenced by variability in the individuals’ chemotherapy cycles and discontinuation of therapy during the year.
In addition, this study is subject to limitations of claims-based analyses, including missing data, miscoded claims, and inability to identify information not included in the database, such as reasons for discontinuation.
Finally, patients were excluded if they had nonitemized hospital claims for the study drugs; this exclusion criterion might have affected the cohorts disproportionally, creating a selection bias.
Conclusions
Drug shortages continue to threaten patient access to critical medications. Through the example of the persisting leucovorin shortage, this study highlights that the effects of drug shortages extend beyond the clinical consequences to include increased costs to the patient and to the health plan. Health plans play an important role in assisting providers with identifying alternative sourcing strategies and choosing the best course of treatment once the shortage is resolved. Future studies should evaluate the impact of drug shortages on health outcomes.
Stakeholder Perspective
Drug Shortages Are Costly to Patients and to Payers
By Joseph P. Fuhr, Jr, PhD
Professor of Economics, Widener University, Chester, PA
Drug shortages are an increasing problem in the United States and have many implications for different stakeholders. In this issue of the journal, Hayes and colleagues present a study of shortages of generic leucovorin, which is used in various chemotherapy regimens.1 The study, which uses data from a Medicare Advantage population from a national health plan, adds valuable insight into the problems that a drug shortage can cause, and how payers can help alleviate some of these problems.
PATIENTS: When drug shortages occur, patients can be faced with the inability to take their normally prescribed drug. This can result in unfavorable outcomes and increased out-of-pocket (OOP) costs. In some cases, patients have to postpone procedures. In their study, Hayes and colleagues estimate that the mean annual added OOP cost for levoleucovorin, a nongeneric substitute for leucovorin, was between $167 and $714 higher than for leucovorin, which can be a significant increased cost burden for the patient.
PROVIDERS: Medical professionals have increased their use of labor resources in an attempt to find drugs affected by shortages and to find alternatives for these drugs. Providers who are using less familiar treatment alternatives for drugs in shortage can be more prone to medical errors.
PAYERS: Third-party payers have experienced higher drug prices related to drug shortages. A grey market has evolved for these drugs, leading to considerably higher prices. In addition, the grey market has increased the potential for counterfeit drugs to enter the supply chain. The reasons for the drug shortages are multifaceted and have become a major public health issue.
The initial reason for the shortage of leucovorin was manufacturing delays by 1 of the 2 manufacturers of the generic drug. There was also no incentive to increase production of leucovorin, because of the relatively low price of the generic drug. An alternative for leucovorin, levoleucovorin, was found; however, according to results of clinical trials, levoleucovorin was not superior to the generic drug, yet it was substantially more expensive.
The study by Hayes and colleagues examines the various ways that health plans can minimize the impact of drug shortages, by taking an active role in helping patients. The authors note several strategies that payers can use to help alleviate problems created by drug shortages, such as identifying affected patients, finding alternative drugs, assisting providers in finding the drug, and adjusting the payers’ drug coverage process.
One tactic that payers could have taken in the case of leucovorin was to give the generic companies an incentive to supply more of the drug, by increasing the generic price. This would have increased the supply of the drug, and also might have lowered overall spending, as long as the negotiated price was below the price of the alternative drug. Payers and Medicare need to have more flexibility in drug pricing when a shortage occurs. Such flexibility will help eliminate the grey market, help alleviate the shortage, and will decrease the negative impact on consumers, providers, payers, and the overall healthcare cost.
Hayes and colleagues estimate the additional cost of using a higher-priced, but not superior, drug substitute. Drug shortages can result in postponed procedures to patients and can contribute to less favorable outcomes; the authors did not measure the costs for this, which should be done by future research. The present study is indeed very informative, but it represents only a first step in addressing drug shortages and estimates only a portion of the cost of shortages to patients and to payers.
References
- 1.Hayes MS, Ward MA, Slabaugh SL, Xu Y. Lessons from the leucovorin shortages between 2009 and 2012 in a Medicare Advantage population: where do we go from here? Am Health Drug Benefits. 2014; 7: 264–270 [PMC free article] [PubMed] [Google Scholar]
Acknowledgments
The authors wish to recognize Tyler Whisman, a clinical pharmacist at Humana, Inc, for his contributions to the concept and design of this study.
Contributor Information
Mary S. Hayes, Clinical Pharmacist, Humana Inc, Louisville, KY.
Melea A. Ward, Clinical Pharmacist, Humana, Inc, Louisville, KY, at the time this work was completed.
S. Lane Slabaugh, Researcher, Comprehensive Health Insights, Humana Inc, Louisville, KY..
Yihua Xu, Researcher, Comprehensive Health Insights, Humana Inc, Louisville, KY..
Funding Source
This study was funded by Humana, Inc.
Author Disclosure Statement
Dr Hayes, Dr Ward, and Dr Xu reported no conflicts of interest. Dr Slabaugh owns stocks in Humana, Inc.
References
- 1.US Food and Drug Administration. FDA and manufacturers work to prevent drug shortages. Updated June 9, 2011. www.fda.gov/drugs/drugsafety/drugshortages/ucm257746.htm Accessed March 10, 2014.
- 2.IMS Institute for Healthcare Informatics. Drug shortages: a closer look at products, suppliers and volume volatility. Executive summary. November 2011. www.imshealth.com/deployedfiles/ims/Global/Content/Insights/IMS%20Institute%20for%20Healthcare%20Informatics/Static%20Files/IIHI_Drug_Shortage_Media_ExecSumm.pdf Accessed March 10, 2014.
- 3.American Society of Health-System Pharmacists. Drug shortages summit: summary report; November 5, 2010. January 10, 2011. www.ashp.org/drugshortages/summitreport Accessed May 12, 2013.
- 4.McLaughlin M, Kotis D, Thomson K, et al. Effects on patient care caused by drug shortages: a survey. J Manag Care Pharm. 2013; 19: 783–788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McBride A, Holle LM, Westendorf C, et al. National survey on the effect of oncology drug shortages on cancer care. Am J Health Syst Pharm. 2013; 70: 609–617 [DOI] [PubMed] [Google Scholar]
- 6.Kaakeh R, Sweet BV, Reilly C, et al. Impact of drug shortages on U.S. health systems. Am J Health Syst Pharm. 2011; 68: 1811–1819 [DOI] [PubMed] [Google Scholar]
- 7.Fight Colorectal Cancer. Tag archives: leucovorin shortage. http://fightcolorectalcancer.org/tag/leucovorin_shortage/ Accessed March 11, 2014.
- 8.Fight Colorectal Cancer. Leucovorin shortage threatens colorectal cancer treatment. December 15, 2008. http://fightcolorectalcancer.org/leucovorin_shortage_threatens_colorectal_cancer_treatment/ Accessed July 15, 2014.
- 9.Fight Colorectal Cancer. Leucovorin shortage update. January 22, 2009. http://fightcolorectalcancer.org/leucovorin_shortage_update/ Accessed July 15, 2014.
- 10.Fight Colorectal Cancer. Colorectal cancer news in brief: May 8. May 8, 2009. http://fightcolorectalcancer.org/colorectal_cancer_news_in_brief_may_8/ Accessed July 15, 2014.
- 11.Fight Colorecal Cancer. New leucovorin shortage should be fixed soon. June 24, 2010. http://fightcolorectalcancer.org/new_leucovorin_shortage_should_be_fixed_soon/ Accessed July 15, 2014.
- 12.US Food and Drug Administration. Current and resolved drug shortages and discontinuations reported to FDA: leucovorin calcium lyophilized powder for injection. Search results. www.accessdata.fda.gov/scripts/drugshortages/dsp_ActiveIngredientDetails.cfm?AI=Leucovorin%20Calcium%20Lyophilized%20powder%20for%20Injection&st=c# Accessed July 21, 2014.
- 13.US Center for Drug Evaluation and Research. Levoleucovorin approval letter. March 7, 2008. www.accessdata.fda.gov/drugsatfda_docs/nda/2008/020140s000Approv.pdf Accessed March 11, 2014.
- 14.Goldberg RM, Hatfield AK, Kahn M, et al. Prospectively randomized North Central Cancer Treatment Group trial of intensive-course fluorouracil combined with the l-isomer of intravenous leucovorin, oral leucovorin, or intravenous leucovorin for the treatment of advanced colorectal cancer. J Clin Oncol. 1997; 15: 3320–3329 [DOI] [PubMed] [Google Scholar]
- 15.Fusilev (levoleucovorin) injection [prescribing information]. Irvine, CA: Spectrum Pharmaceuticals, Inc; April 2011.
- 16.Kovoor PA, Karim SM, Marshall JL. Is levoleucovorin an alternative to racemic leucovorin? A literature review. Clin Colorectal Cancer. 2009; 8: 200–206 [DOI] [PubMed] [Google Scholar]
- 17.Centers for Medicare & Medicaid Services. Payment allowance limits for Medicare Part B drugs. Updated November 25, 2013. www.cms.gov/apps/ama/license.asp?file=/McrPartBDrugAvgSalesPrice/downloads/Apr-13-ASP-Pricing-file.zip Accessed May 20, 2013.
- 18.RJ Health Systems Reimbursement Codes. Leucovorin and levoleucovorin pricing tables. http://reimbursementcodes.com Accessed March 11, 2014.
- 19.Spectrum Pharmaceuticals. FDA approves FUSILEV® for use in patients with colorectal cancer. Press release. April 29, 2011. http://investor.spectrumpharm.com/releasedetail.cfm?ReleaseID=573364 Accessed July 16, 2014.
- 20.Fox ER, Birt A, James KB, et al. ASHP Guidelines on managing drug product shortages in hospitals and health systems. Am J Health Syst Pharm. 2009; 66: 1399–1406 [DOI] [PubMed] [Google Scholar]
- 21.Humana. Chemotherapy—New Century Health. www.humana.com/provider/medical-providers/education/referral/chemotherapy-new-century-cincy Accessed March 11, 2014.
- 22.Humana. Chemotherapy—Oncology Analytics. www.humana.com/provider/medical-providers/education/referral/chemotherapy-oncology-tampa Accessed March 11, 2014.