Sirs,
Nephronophthisis (NPHP) is an autosomal recessive cystic kidney disease that constitutes the most frequent genetic cause for end-stage renal disease (ESRD) in the first three decades of life. Homozygous deletions in the NPHP1 gene account for approximately 21% of all NPHP cases, whereas the other genes contribute less than 3% each. Interestingly, positional cloning of the nine genes (NPHP 1 through 9) and functional characterization of their encoded proteins (nephrocystins) have contributed to a unifying theory that defines cystic kidney diseases as “ciliopathies” [1].
Since there are no clinical or molecular data about NPHP in Egyptian children, we investigated the prevalence of homozygous NPHP1 deletion among a cohort of children with presumptive diagnosis of NPHP at Center of Pediatric Nephrology & Transplantation (CPNT), Cairo University.
We studied 20 children, from 17 independent families, fulfilling the clinical and the ultrasonographic criteria of NPHP. All patients had full ophthalmologic examination, brain MRI was carried out in children with neurological involvement. Analysis for a homozygous deletion of the NPHP1 gene was performed by multiplex polymerase chain reaction (PCR) approach on genomic DNA of patients described earlier [2]. Sex distribution among affected patients showed a slight preponderance of females, with a ratio of 1.2:1 (11 females and 9 males). Seventy five percent of our study patients were the products of consanguineous marriages, the percentage of affected siblings was strikingly high 65% (13/20 patients) and 40% (8/20 patients) had a history of sibling death due to a similar condition.
Fifteen of 20 patients (75%) presented with signs of ESRD. All the patients suffered from anemia and growth retardation when they first came to medical attention. Nineteen of 20 patients (95%) had a history typical of nephronophthisis, with symptoms of polydipsia, polyuria, and secondary enuresis. Four of 20 patients (20%) were hypertensive with elevated blood pressure above the 95th percentile for age, gender, and height.
Clinically, study patients were best categorized as: 13/20 (65%) patients with isolated juvenile NPHP, 3/20 (15%) patients as infantile NPHP, while the remaining 4/20 (20%) patients had extrarenal associations (molar tooth sign on brain MRI, ataxia, mental retardation, retinal dystrophy, oculomotor apraxia, and facial dysmorphy) hence were clinically categorized as Joubert Syndrome Related Disorder (JSRD). The mean age at diagnosis 87.5 + 45.4 months was significantly late as compared to the age of onset of symptoms 43.8 ± 29.7 months (P <0.01).
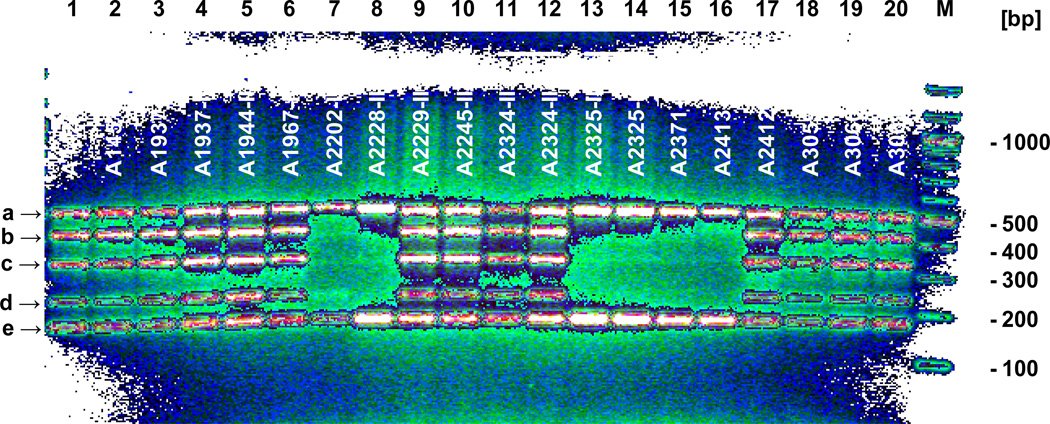
Homozygous deletions in the NPHP1 gene were identified in 6 patients from 5 independent families out of the 17 studied families (29.4%), thereby confirming the diagnosis of type 1 nephronophthisis (Fig. 1). This does not seem to differ from reported figures in Western countries. Five patients had isolated NPHP whereas the sixth patient was among the JSRD group with the distinct MTS detected in his brain MRI images, ataxia, retinitis pigmentosa and dysmorphic facies. This confirms that NPHP1 deletions can indeed be responsible for JSRD as previously reported [3].
Figure 1.
Screening for homozygous NPHP1 deletions. 20 patients (lane 1–20) from 17 independent families were analyzed using a multiplex PCR approach amplifying 5 different markers. Two control markers (a, e) and 3 NPHP1 exon markers [arrow “d” (exon 7, 236 bp), arrow “c” (exon 5, 339 bp), arrow “b” (exon 20, 436 bp)] were amplified in a single multiplex PCR. Fragments were separated on a 1.5% agarose gel for 3 hours at 120 V. Note that patients in lane 7, 8, 13, 14, 15, and 16 lack the bands for the respective NPHP1 exons indicating a homozygous NPHP1 deletion and confirming the diagnosis NPHP type 1. White bars indicate sibling cases. Lane M, 100 bp ladder DNA size Marker (New England Biolabs).
Moreover we report one patient with the homozygous NPHP1 deletion presenting with an infantile onset phenotype. In the literature, Infantile NPHP frequently caused by mutations in the NPHP2/inversin gene differs from the other types of NPHP in the early age of onset of ESRD usually <5 years in all reported cases, whereas the median age of ESRD in juvenile NPHP (NPHP type 1 or type 4) is about 13 years [4]. Renal cortical microcysts is another criterion where detailed analysis of a murine model of NPHP2/inversin demonstrates cystic dilatation of Bowman’s capsule, proximal tubule, thick ascending limb and collecting duct [5].
Although homozygous NPHP1 deletions is the most frequent NPHP1 mutation known, nevertheless, in more than 6% of all NPHP1 cases the underlying mutation has been found to be a heterozygous deletion combined with a single point mutation [2]. As for the patients with no homozygous NPHP1 deletion we will investigate for heterozygous deletions in a future study. Further analysis of all other NPHP loci for potential homozygosity in consanguineous families and sequencing all exons of NPHP genes located within regions of significant homozygosity is crucial to identify the underlying genetic defect.
Our infantile NPHP patient showed most of the clinical and histopathological features of NPHP type 2 previously reported in the literature [4]: (1) the characteristic cortical cysts in a normal sized hyperechogenic kidneys on renal sonogram, (2) distinct renal microcysts in the kidney histopathological examination, (3) clinical manifestations started in the first year of life and progressed to ESRD at the age of 32 months. In conclusion, homozygous deletions in the NPHP1 gene do not seem to differ in Egypt from reported figures in Western countries. Most likely this is the first report of a homozygous NPHP1 deletion in an infantile onset NPHP patient.
Contributor Information
Neveen A Soliman, Department of Pediatrics, Center of Pediatric Nephrology & Transplantation (CPNT), Cairo University, Egyptian Group for Orphan Renal Diseases (EGORD), 99 El-Manial St, Manial, Cairo, 11451 – EGYPT, Tel: +2016-2132300, Fax: +202-23630039, neveenase@yahoo.com, nsoliman@kasralainy.edu.eg.
Friedhelm Hildebrandt, Department of Pediatrics, University of Michigan, Howard Hughes Medical Institute.
Susan J Allen, Department of Pediatrics, University of Michigan.
Edgar A Otto, Department of Pediatrics, University of Michigan.
Marwa M Nabhan, Department of Pediatrics, Center of Pediatric Nephrology & Transplantation (CPNT), Cairo University.
Ahmed M Badr, Department of Pediatrics, Center of Pediatric Nephrology & Transplantation (CPNT), Cairo University.
REFERENCES
- 1.Hildebrandt F, Attanasio M, Otto E. Nephronophthisis: Disease Mechanisms of a Ciliopathy. J Am Soc Nephrol. 2009;20:23–35. doi: 10.1681/ASN.2008050456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Otto EA, Helou J, Allen SJ, O'Toole JF, Wise EL, Ashraf S, Attanasio M, Zhou W, Wolf MT, Hildebrandt F. Mutation analysis in nephronophthisis using a combined approach of homozygosity mapping, CEL I endonuclease cleavage, and direct sequencing. Hum Mutat. 2008;29:418–426. doi: 10.1002/humu.20669. [DOI] [PubMed] [Google Scholar]
- 3.Parisi MA, Bennett CL, Eckert ML, Dobyns WB, Gleeson JG, Shaw DW, McDonald R, Eddy A, Chance PF. The NPHP1 gene deletion associated with juvenile nephronophthisis is present in a subset of individuals with Joubert syndrome. Am J HumGenet. 2004;75:82–91. doi: 10.1086/421846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simms RJ, Eley L, Sayer JA. Nephronophthisis. Eur J Hum Genet. 2009;17:406–416. doi: 10.1038/ejhg.2008.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips CL, Miller KJ, Filson AJ, Nürnberger J, Clendenon JL, Cook GW, Dunn KW, Overbeek PA, Gattone VH, Bacallao RL. Renal cysts of inv/inv mice resemble early infantile nephronophthisis. J Am Soc Nephrol. 2004;15:1744–1755. doi: 10.1097/01.asn.0000131520.07008.b3. [DOI] [PubMed] [Google Scholar]