Abstract
Background: The high prevalence and incidence of obesity and eating disorders in US adolescent girls are serious health problems. Because of the shared risk factors for obesity and eating disorders, a targeted prevention of both conditions is a priority.
Objective: We determined whether an adapted interpersonal psychotherapy prevention program is more efficacious for reducing excess weight gain and worsening disordered eating than health education in adolescent girls at high risk of obesity and eating disorders.
Design: A parallel-group, randomized controlled trial was conducted between September 2008 and January 2013 in a university-based laboratory and a federal research hospital. The study included 113 adolescent (12–17-y-old) girls deemed at high risk of adult obesity and eating disorders because of a body mass index (BMI) between the 75th and 97th percentiles and reports of episodes of a loss of control over their eating. Girls were randomly assigned to participate in an adapted interpersonal psychotherapy or a health-education group program for 12 weekly 90-min group sessions. Follow-up assessments occurred immediately after group programs and at 6 and 12 mo.
Results: Participation in both conditions was associated with decreases in expected BMI gain, age-adjusted BMI metrics, the percentage of fat by using dual-energy X-ray absorptiometry, symptoms of depression and anxiety, and the frequency of loss-of-control eating over 12 mo of follow-up (Ps < 0.001) with no group difference. In follow-up analyses, interpersonal psychotherapy was more efficacious than health education at reducing objective binge eating at the 12-mo follow-up (P < 0.05).
Conclusions: The intervention with adolescent girls with loss-of-control eating is associated with lower age-adjusted BMI and percentage of adiposity as well as improved mood symptoms over 1 y. Interpersonal psychotherapy further reduced objective binge eating. Additional research is needed to elucidate the mechanisms by which physical and psychological improvements were observed. This trial was registered at clinicaltrials.gov as NCT00680979.
INTRODUCTION
More than 30% of US adolescent girls are overweight or obese (1). High body weight in youth is a robust predictor of adult obesity (2, 3). Unfortunately, sustained weight loss is especially challenging in adolescents (4). Targeted preventive approaches for susceptible subgroups of youth may have a potential for greater effects than standard weight-management programs (5). Furthermore, interventions focused on producing weight maintenance or a less-than-expected gain (6) in targeted pediatric subgroups may help to prevent adult obesity.
Obesity and eating disorders appear to have shared risk factors (7, 8); thus, their coordinated prevention has been proposed (9–12). One potentially modifiable target that has been shown to promote both conditions is the report of loss-of-control (LOC)6 eating episodes during childhood. Such episodes are characterized by a subjective lack of control over eating regardless of the amount of food reportedly consumed (13). The presence of LOC episodes predicts excessive weight gain (14–17) and increases risk of binge-eating disorder (18, 19), which is a diagnosis that requires classic binge-eating episodes that involve the consumption of unambiguously large amounts of food and the experience of LOC (20).
Because interpersonal psychotherapy (IPT) has shown short--term efficacy and long-term efficacy in adults to reduce binge eating (21–23), and adolescent girls have reported overeating in response to unsatisfactory interpersonal interactions (24), we carried out a pilot study to test the feasibility of an adapted prevention version of IPT (24) for the reduction of LOC eating and excess weight gain in high-risk adolescent girls (25). Results suggested that, compared with girls randomly assigned to a health-education (HE) group program, participants who received IPT were more likely to reduce LOC-eating episodes and experience less-than-expected weight gain. Because of the preliminary positive results of this pilot study, we conducted an adequately powered trial to test the efficacy of IPT for the prevention of excess weight gain and worsening disordered eating. We administered an adapted version of IPT or a HE program to adolescent girls deemed at high risk of both outcomes as a result of their current body weight and reports of LOC eating. We hypothesized that, compared with girls assigned to receive HE, those who received IPT would gain less age-adjusted BMI and percentage of adiposity, engage in fewer LOC- and binge-eating episodes, and improve psychosocial functioning.
SUBJECTS AND METHODS
Participants
Healthy adolescent girls aged 12–17 y were recruited for participation in a randomized, controlled, clinical trial at the Uniformed Services University of the Health Sciences and the NIH Hatfield Clinical Research Center (Bethesda, MD). Participants were deemed at risk of excess weight gain because of BMI between 75th and 97th percentiles (3) and the report of at least one episode of LOC eating in the past 1 mo (16). Individuals were excluded if they had a major medical condition (eg, diabetes), a current or lifetime diagnosis of a Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision or Diagnostic and Statistical Manual, 5th Edition eating disorder (other than binge-eating disorder) or any current Axis I or Axis II psychiatric condition (eg, major depressive disorder or psychosis), were simultaneously participating in a structured weight-loss program or psychotherapy, or were taking medications (eg, selective serotonin reuptake inhibitors, neuroleptics, tricyclics, or stimulants) known to affect body weight or appetite. Girls who were taking oral contraceptives were included provided that the contraceptive had been used ≥2 mo before participating in the prevention groups. Pregnant girls and those who had lost >5% of their body weight in the 3 mo before assessment were also excluded.
Adolescents were recruited through the NIH clinical trials website, local area community flyer postings, and direct mailings to homes within a 50-mile radius of Bethesda, Maryland. Recruitment materials were directed to parents who were concerned about their daughter's body weight and eating behavior. Girls were compensated for the time and inconvenience of study assessments and received a bonus for attending >80% of group program visits. The study was approved by the Uniformed Services University of the Health Sciences and Eunice Kennedy Shriver National Institute of Child Health and Human Development Institutional Review Boards.
Procedure
Parents and daughters provided written consent and assent, respectively. At a baseline screening, height and fasting weight were measured. The percentage of body fat mass was assessed by using dual-energy X-ray absorptiometry (DXA) with a Hologic QDR-4500A or Discovery (Hologic) instrument. See Supplemental Material under “Supplemental data” in the online issue for detailed procedures. The Eating Disorder Examination Version 14 OD/C.2 (26) was administered to assess the presence of eating disorders and the presence and number of LOC- and binge-eating episodes over the past 3 mo. Adolescents completed the Social Adjustment Scale–Self-Report (27), the Beck Depression Inventory, Second Version (28), and the State-Trait Anxiety Inventory for Children–A Trait Scale (29).
A computer program that used a random-number generator was used to assign participants to IPT or HE groups (see Supplemental Material under “Supplemental data” in the online issue). The programs involved an individual 1.5-h meeting with each girl followed by 12 consecutive weekly 90-min group sessions. IPT was adapted from IPT-Adolescent Skills Training for the prevention of depression (30) and group IPT for binge-eating disorder (31). HE was based on the HEY-Durham manual for high-school students (32). See Supplemental Material under “Supplemental data” in the online issue for details of program specifics. Leader training and program fidelity have been described (24, 25). In brief, each group was cofacilitated by a PhD-level clinical psychologist and a graduate student in clinical psychology. Group leaders rotated so that each psychologist led both types of groups during different cohorts. All leaders were trained before conducting group sessions. Ongoing weekly supervision, including a review of audiotaped sessions, ensured intervention consistency with the respective manuals. Twenty percent of randomly selected audiotapes (10% of IPT and another 10% of HE group sessions) across cohorts and interventionists were evaluated by 2 independent raters who were blinded to the study program. The raters, both of whom were PhD-level clinical psychologists, completed integrity checklists that assessed the unique topics and approaches of group interventions. Ratings formed indexes that assesses the adherence and competence of group leaders. Example items rated highly for IPT and distinguished from HE included “Were the group members’ LOC eating/mood symptoms reviewed?” “Was a linkage made between current interpersonal problems and eating disorder symptoms?” “Did the leaders help clarify the participants’ communications with others?” “Did the leaders elicit affect during the session?” and “Did the leaders encourage work at home to practice interpersonal skills?”
Follow-up assessments took place at the end of the 12-wk interventions at 6 mo and at 12-mo after the initiation of programs. DXA data were collected at baseline and a 12-mo follow-up. All other procedures were repeated at all follow-up visits. At each visit, height, weight, and DXA were obtained by staff blinded to intervention assignments.
Statistical analysis
On the basis of estimates from prospective data for BMI change in children (16) and allowing for 25% attrition, a total sample size of 110 participants was estimated for 80% power to detect group differences in weight gain at P ≤ 0.05. See Supplemental Material under “Supplemental data” in the online issue for power-estimate details. Analyses were performed with SPSS 20.0 software (IBM) on the full intention-to-treat sample. Primary analyses were linear mixed models with repeated measures by using a full-information maximum-likelihood estimation for the handling of missing data to examine group differences over time in continuous outcomes. Multiple imputation, the last observation carried forward, or a list-wise deletion yielded the same results for primary analyses; thus, for parsimony, only full-information maximum-likelihood results are presented. The primary outcome was the weight trajectory in growing girls of various ages, which was calculated as the difference between the expected BMI change (on the basis of CDC pediatric growth-chart data) and actual BMI change at each follow-up (25). Residualized change scores were created by regressing BMI at each follow-up onto baseline BMI. We also examined the change over time in the BMI z score, BMI percentile, BMI, and percentage of body fat as well as the number of LOC- and classic objective binge-eating episodes, social adjustment, and depressive and anxiety symptoms. The independent variable was the group condition, and the repeated measure was the interval (baseline, postintervention, and 6- and 12-mo follow-ups). A repeated-measures ANCOVA that used the last observation carried forward to handle missing values was used to evaluate the dependent variable of the percentage of body fat because DXA was measured only at baseline and the 12-mo follow-up. Binary logistic regressions were used to test group differences in dichotomous 12-mo follow-up outcomes of weight maintenance (more- compared with less-than-expected BMI growth), LOC-eating status, and binge-eating status (presence compared with absence). The independent variable in each model was the group. See Supplemental Material under “Supplemental data” in the online issue for a description of covariates for all analyses. On the basis of findings from clinical trials in which eating disorders in adults were treated (23, 33), we tested race-ethnicity (non-Hispanic white compared with other) as a moderator of observed effects of the group condition on LOC and binge eating. We also explored baseline age as a moderator of group effects on body measurements, but because these effects were exploratory and nonsignificant, they are not presented. Effects were considered significant at P ≤ 0.05. Results are presented in the following order: program and follow-up attendance and intervention fidelity; age-adjusted BMI and DXA; LOC-eating, binge-eating, and eating-disorder developments; and psychosocial functioning.
RESULTS
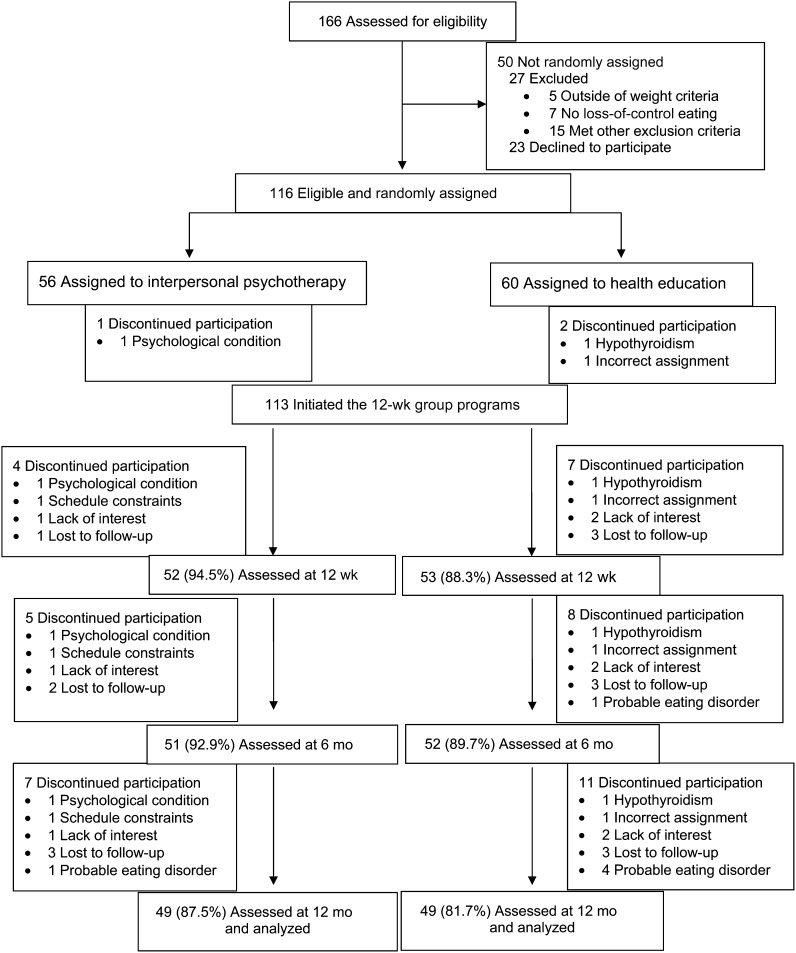
We randomly assigned 116 girls to IPT or HE. After random assignment, 3 girls were excluded; 2 girls were identified as meeting study exclusion criteria, and 1 girl was incorrectly randomly assigned (Figure 1). Baseline characteristics for 113 girls are shown in Table 1. By design, all girls reported the presence of LOC-eating episodes, whereas 37 participants (32.7%) also reported binge eating. The median group size was 5 girls/group (range: 3–9 girls/group). The median program attendance for IPT was higher than for HE [11 of 12 sessions (91.7%; 95% CI: 79.8%, 90.5%) compared with 10 of 12 sessions (83.3%; 95% CI: 72.4%, 83.1%; P = 0.01)]. Said differently, a greater percentage of girls in IPT than in HE attended ≥80% of sessions (≥10 of 12 sessions) (85.5% compared with 65.5%, respectively; Fisher's P = 0.02). Independent ratings of randomly selected IPT and HE sessions indicated excellent adherence to the respective program (all Ps ≤ 0.01). Few participants left the study, and the dropout rate did not differ between groups (Ps ≥ 0.47; Figure 1). Girls who did not complete the final 12-mo follow-up had attended fewer group sessions than did those who were seen at 12 mo (5 compared with 11 sessions attended, respectively; P = 0.003). Completers and dropouts did not differ significantly in race-ethnicity, socioeconomic status, baseline BMI-derived metrics, adiposity, LOC eating, or binge eating (Ps ≥ 0.14).
FIGURE 1.
Study participant flow.
TABLE 1.
Baseline demographic, anthropometric, and psychosocial characteristics of adolescent girls in IPT and HE groups1
| Variable | Total (n = 113) | IPT (n = 55) | HE (n = 58) | P |
| Age (y) | 14.5 ± 1.72 | 14.2 ± 1.5 | 14.8 ± 1.7 | 0.05 |
| Race-ethnicity ( %) | 0.84 | |||
| Non-Hispanic black | 23.9 | 25.5 | 22.4 | |
| Non-Hispanic white | 56.6 | 52.7 | 60.3 | |
| Hispanic | 8.8 | 9.1 | 8.6 | |
| Other | 10.6 | 12.7 | 8.6 | |
| Socioeconomic status3 | 2.0 | 2.0 | 2.0 | 0.80 |
| BMI | 27.0 ± 2.5 | 26.9 ± 2.6 | 27.1 ± 2.4 | 0.63 |
| BMI z score | 1.5 ± 0.3 | 1.5 ± 0.3 | 1.5 ± 0.3 | 0.65 |
| BMI percentile | 92.2 ± 4.7 | 92.4 ± 4.6 | 92.2 ± 4.4 | 0.79 |
| Body fat percentage | 36.5 ± 5.1 | 36.5 ± 5.0 | 36.4 ± 5.3 | 0.97 |
| LOC episodes | 6.2 (5.6, 6.9)4 | 4.7 (4.1, 5.4) | 8.0 (6.9, 9.2) | 0.01 |
| Binge episodes | 0.6 (0.5, 0.7) | 0.4 (0.3, 0.5) | 0.8 (0.6, 1.1) | 0.05 |
| Binge presence (%) | 31.9 | 25.5 | 37.9 | 0.17 |
| Social adjustment | 2.5 ± 0.8 | 2.4 ± 0.8 | 2.6 ± 0.8 | 0.21 |
| Depressive symptoms | 10.6 ± 6.6 | 10.1 ± 6.9 | 11.2 ± 6.3 | 0.36 |
| Anxiety symptoms | 34.1 ± 6.8 | 33.3 ± 7.1 | 34.9 ± 6.3 | 0.20 |
t Tests were used to analyze all continuous variables, and chi-square tests were used to analyze all categorical variables. HE, health education; IPT, interpersonal psychotherapy; LOC, loss of control.
Mean ± SD (all such values).
All values are medians.
Geometric mean of log-transformed scores; 95% CI in parentheses (all such values).
Weight maintenance, BMI indexes, and percentage of adiposity
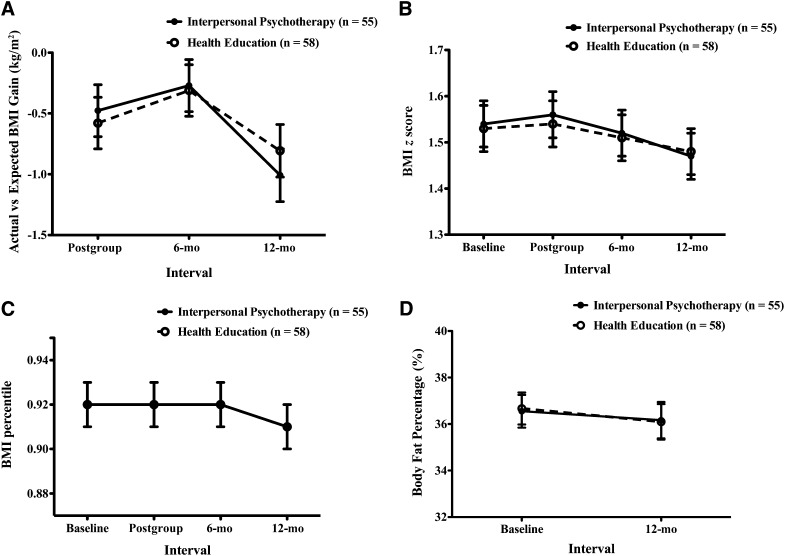
Girls in both groups gained less-than-expected BMI throughout the study (F[2,199] = 10.70; P < 0.001; Figure 2A). When considered categorically, girls in HE had a nonsignificant, 1.59-times (95% CI: 0.67, 3.79) greater odds of gaining more-than-expected BMI at 12 mo relative to those of girls in IPT (P = 0.30). As expected, all girls showed gains in BMI, on average, over the study interval (F[3,308] = 8.40, P < 0.001). However, they experienced significant decreases over time in age-adjusted BMI metrics of the BMI z score (F[3,309] = 4.88, P = 0.003) and BMI percentile (F[3,312] = 6.88, P < 0.001; Figure 2, B and C). The main effect of group was not significant in any model (Ps ≥ 0.86), nor was the group-by-interval effect significant (Ps > 0.49). Approximately one-half of girls in both conditions were nonobese at baseline and continued to be nonobese 1 y later (54.5% of girls in IPT compared with 53.4% of girls in HE; Fisher's P = 1.00), 9.1% of girls in IPT and 8.6% of girls in HE were obese at baseline and nonobese at 12 mo (Fisher's P = 1.00), and approximately one-third in each group remained obese throughout the study (34.5% of girls in IPT compared with 27.6% of girls in HE; Fisher's P = 0.54). A small percentage of girls became obese (1.8% of girls in IPT compared with 10.3% of girls in HE; Fisher's P = 0.11). In clinical terms, the number needed to treat (34) with IPT to prevent obesity onset was 1 of 12 girls. There was a significant within-subject effect for decreases in the percentage of adiposity from baseline to the 12-mo follow-up (F[1,109] = 6.91, P = 0.01) but no significant group-by-interval effect (F[1,109] = 0.03, P = 0.85; Figure 2D).
FIGURE 2.
Linear mixed models with repeated measures with the use of maximum-likelihood estimation were used to examine mean (±SE) changes in actual compared with expected BMI gain (P-group = 0.94, P-interval < 0.001, P-group × interval = 0.50) (A), BMI z score (P-group = 0.91, P-interval = 0.003, P-group × interval = 0.91) (B), BMI percentile (P-group = 0.91, P-interval < 0.001, P-group × interval = 0.96) (C), and the percentage fat mass (P-group = 0.90, P-interval = 0.01, P-group × interval = 0.85) (D) over the course of the study by group assignment.
Because of the lack of group-condition differences in BMI indexes and adiposity, we examined to what extent improvements in social functioning, negative mood, and LOC- and binge-eating episodes during the intervention (ie, posttreatment minus baseline variable) were predictive of 12-mo body measurements regardless of the group assignment. Improvements in social functioning predicted significantly lower BMI at the 12-mo follow-up with the group assignment and baseline BMI (F = 8.32, P = 0.005) or postintervention BMI (F = 6.77, P = 0.01) controlled for. The same effect was observed for adiposity (F = 10.80, P = 0.001). Changes in negative mood or eating episodes were not significantly predictive of 12-mo body measurements.
LOC eating and binge eating
LOC eating
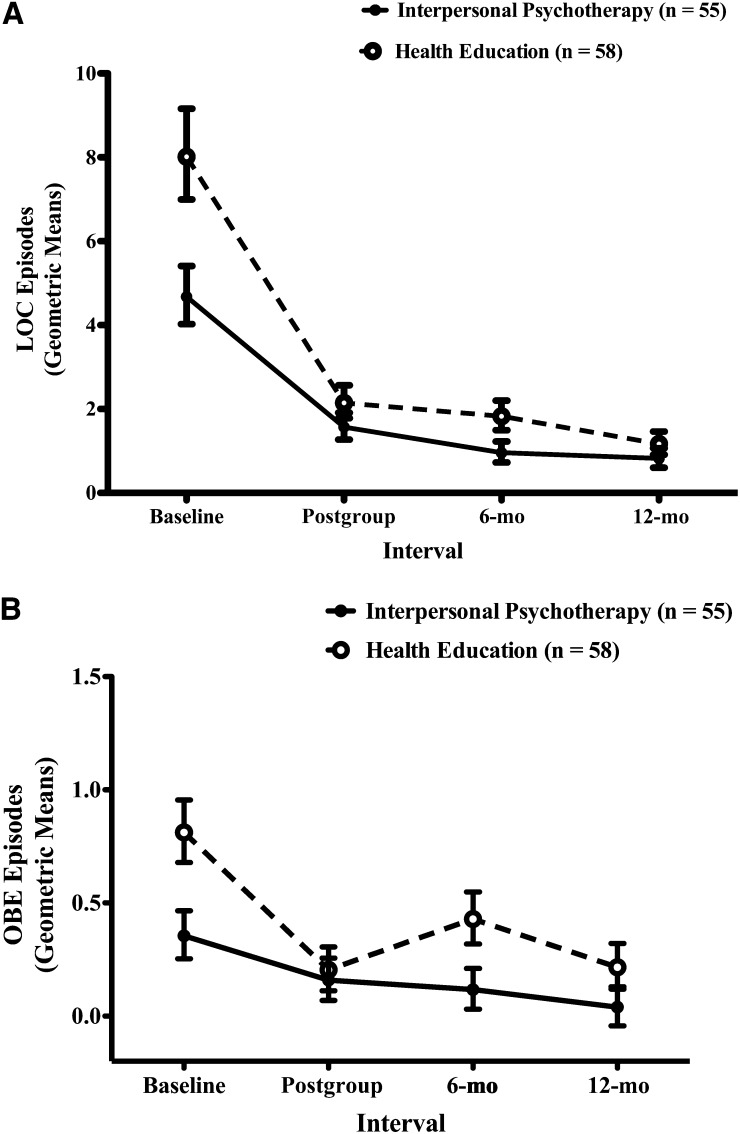
Girls in both groups reported significant reductions in the average number of LOC episodes (F[3,310] = 78.33, P < 0.001) with no group-by-interval effect (F[3,310] = 1.10, P = 0.35; Figure 3A). Race was a significant moderator of the effect of group on reductions in LOC episodes between baseline and the 12-mo follow-up (F[1,105] = 4.51, P = 0.036). Racial-ethnic minority girls in HE (n = 19) had more LOC episodes, on average, at the 12-mo follow-up (geometric mean: 1.39; −1 SE, +1 SE: 0.99, 1.87) than any other group did, including racial-ethnic minority girls in IPT (n = 26; geometric mean: 0.74; −1 SE, +1 SE: 0.46, 1.08), non-Hispanic white girls in HE (n = 39; geometric mean: 0.90; −1 SE, +1 SE: 0.61, 1.23), or non-Hispanic white girls in IPT (n = 29; geometric mean: 0.74; −1 SE, +1 SE: 0.46, 1.08). When considered by the presence or absence of LOC eating, there was no effect of the group on the likelihood of having any LOC eating at 12 mo (47.3% of girls in IPT compared with 41.4% of girls in HE; P = 0.65). Regardless of the intervention group, girls who were abstinent from LOC eating at the 12-wk follow-up (immediately after groups ended) were nearly 5 times less likely to report LOC 1 y later (OR: 4.85; 95% CI: 2.02, 11.65; P < 0.001). Results were not statistically different when LOC was operationalized as the presence or absence of frequent LOC eating (at least once per week for 3 mo); at the 12-mo follow-up, 1.8% of girls in IPT reported frequent LOC eating, whereas in HE, 10.3% of girls endorsed frequent LOC (Fisher's P = 0.11). Likewise, when baseline LOC frequency status was controlled for, the group did not predict the 12-mo LOC frequency presence or absence (P = 0.43).
FIGURE 3.
Linear mixed models with repeated measures with the use of maximum-likelihood estimation were used to examine mean (±SE) changes in LOC-eating episodes in the past 3 mo (P-group = 0.03, P-interval < 0.001, P-group × interval = 0.35) (A) and classic OBE episodes in the past 3 mo (P-group = 0.02, P-interval < 0.001, P-group × interval = 0.26) (B) over the course of the study by group assignment. Geometric means of disordered eating episodes are displayed. LOC, loss of control; OBE, objective binge eating.
Binge eating
There was a significant main effect for the group (F[1,94] = 5.86, P = 0.02) and interval (F[3,296] = 9.26, P < 0.0001) but a nonsignificant group-by-interval effect on reported binge eating (P = 0.26; Figure 3B). Because of the observed group difference in the number of baseline binge-eating episodes, we conducted secondary analyses after controlling for the number of binge-eating episodes measured at the 12-wk follow-up, which did not differ by group. IPT girls had fewer binge-eating episodes at the 12-mo follow-up (geometric mean: 0.04; −1 SE, +1 SE: 0.00, 0.09) than HE girls did (geometric mean: 0.16; −1 SE, +1 SE: 0.14, 0.23; P = 0.03). No group effect was observed for other follow-up intervals (Ps ≥ 0.18), and race did not serve as a moderator of the group effect (P = 0.46). When binge eating was considered categorically, girls who participated in HE were >7 times more likely to endorse binge eating at 12 mo than were girls who took part in IPT with posttreatment binge-eating status accounted for (OR: 7.32; 95% CI: 1.57, 34.18; P = 0.01). Regardless of the group, girls who reported binge eating at the 12-wk postintervention follow-up were 19 times more likely to have binge eating 1 y later (OR: 19.25; 95% CI: 4.90, 75.60; P < 0.001).
When the presence or absence of frequent binge eating was explored (1 times/wk for 3 mo), only 3.4% of girls (n = 2) in HE reported frequent binge eating at the 12-mo follow-up, and no girls in IPT reported frequent binge eating at the 12-mo follow-up (Fisher's P = 0.50). Because of the very small number with frequent binge eating, group did not predict binge-eating frequency status at 12 mo with baseline binge status controlled for (P = 0.99).
Eating disorders
In Eating Disorder Examination interviews, one girl reported binge-eating disorder at the 12-mo follow-up; this participant was randomly assigned to HE and had reported binge-eating disorder at baseline. Over the course of the follow-up time frame, 5 additional girls developed probable eating disorders (determined without an in-person assessment because a parent reported that the participant had entered treatment of an eating disorder). Of these girls, 4 were assigned to HE, 3 of whom appeared to have a bulimia nervosa–type disorder, and 1 girl had an anorexia nervosa–type disorder. One girl in IPT developed a probable anorexia nervosa–type disorder. With the exclusion of girls who reported a binge-eating disorder at baseline, there was no main effect of the group on the odds of developing a suspected eating disorder during the 1 y after interventions (P = 0.20; OR for HE compared with IPT: 4.27; 95% CI: 0.46, 39.60). The number needed to treat (34) with IPT to prevent a probable eating disorder at the 1-y follow-up was 1 of 15 girls. When we explored how these 5 girls differed at baseline relative to the rest of the sample, we showed that they reported higher depressive and anxiety symptoms (Ps < 0.05). All 5 girls were initially overweight or obese and had Beck Depression Inventory scores ≥10, which is indicative of mild to moderate depression.
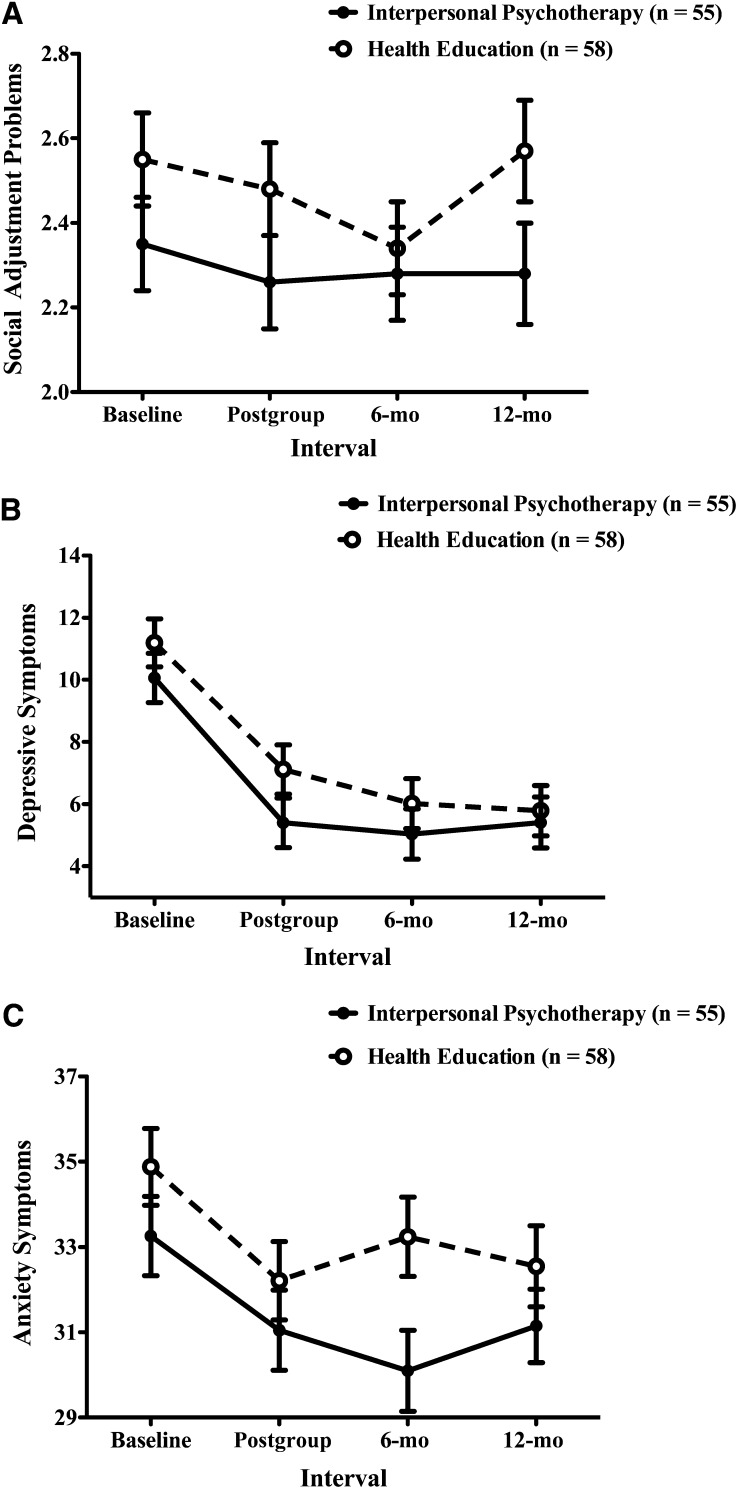
Psychosocial functioning
Social functioning did not significantly change over the course of the study period overall (F[3,319] = 0.72, P = 0.54) or by group by interval (F[3,319] = 0.42, P = 0.74; Figure 4A). There was a main effect of the group on social adjustment; on average, girls in HE reported more social problems across all time points than did girls in IPT (F[1,112] = 4.34, P = 0.04). Regardless of the group assignment, on average, girls experienced significant reductions in depressive symptoms throughout the study (F[3,315] = 37.54, P < 0.001; Figure 4B), with no group or group-by-interval effect (Ps ≥ 0.23). Anxiety symptoms also improved in both groups during the study (F[3,311] = 9.06, P < 0.001; Figure 4C) with no group or group-by-interval effect (Ps ≥ 0.10).
FIGURE 4.
Linear mixed models with repeated measures with the use of maximum-likelihood estimation were used to examine mean (±SE) changes in social adjustment (Social Adjustment Scale; P-group = 0.04, P-interval = 0.54, P-group × interval = 0.74) (A), depressive symptoms (Beck Depression Inventory, Second Version; P-group = 0.23, P-interval < 0.001, P-group × interval = 0.71) (B), and anxiety symptoms (State-Trait Anxiety Inventory for Children-A Trait Version; P-group = 0.11, P-interval < 0.001, P-group × interval = 0.29) (C) over the course of the study by group assignment. For all measures, higher scores were indicative of poorer functioning.
DISCUSSION
This randomized, controlled, clinical trial aimed to prevent excessive weight gain and worsening disordered eating by targeting adolescent girls of above-average weight who also reported LOC eating, which is a behavior that has been shown to predict both outcomes (14–17). The 12-wk experimental and active comparison groups experienced similar improvements in age-adjusted body-weight assessments, mood, and reductions in LOC-eating episodes by the 1-y follow-up. In girls of ethnic-racial minorities, IPT was more beneficial than HE at reducing LOC eating . Moreover, IPT may be more effective than HE in reducing classic binge-eating episodes.
Regardless of the group, the expected weight gain, age-adjusted BMI indexes, and percentage of adiposity were significantly reduced by 1 y after the initiation of interventions in our cohort of girls deemed at high risk of excessive weight gain because of both their current body weights and LOC eating (14–17). Because of recent population trends that indicate a stabilization of pediatric overweight and obesity prevalence rates (1), the impact of our programs is unclear because there was no untreated contemporaneous control group. However, it is possible that both groups were effective in reducing or decreasing the rate of gain for these metrics. Indeed, it is notable that the percentage of adiposity was slightly but significantly reduced during a developmental stage when girls typically increase body fat (35).
Both programs were effective at reducing LOC-eating episodes and negative mood by 1 y. Because data consistently have shown that pediatric LOC-eating predicts worsening disordered eating and mood symptoms (14, 18, 19), these results speak to the importance of identifying and intervening with youth who report such behaviors. Although unexpected, our active comparison condition, which involved an individual pregroup meeting and weekly group sessions with same-sex peers of similar body weight and eating pathology appeared to provide sufficient nonspecific socioemotional support to improve psychological functioning and LOC eating. Although the content and process of groups distinctly differed, the HE program likely involved many identified curative factors including group cohesion, a sense of universality, and an opportunity to disrupt social isolation (36) that are frequently reported by girls with LOC eating (37, 38). These common therapeutic variables likely improved mood and set up positive expectancies for improvement. Future studies would benefit from direct measurement of program expectancies. Moreover, our sample was comprised of generally healthy, prevention-seeking adolescents. Data have suggested that, for mild forms of psychopathology, human contact with genuine, authentic, and empathic leaders may be sufficient for positive changes (39). Therefore, HE may offer some practical advantages over IPT in that delivery could be provided with less training. However, unlike IPT, which has been effectively delivered by nonclinicians (40), this potential advantage would require testing because the HE program in the current study was delivered by psychologists and advanced graduate students whose therapeutic style may be different from individuals without or with minimal clinical training. Although non-Hispanic white girls appeared to reduce LOC eating regardless of the group assignment, in girls belonging to racial-ethnic minority groups (most of whom were African American), those randomly assigned to IPT experienced significantly greater reductions in LOC episodes at 1 y than did those assigned to HE. This finding supports previous speculation that IPT, which is a modality that focuses on improving familial and peer connectivity, may be particularly salient for reducing eating pathology in racial-ethnic minority groups with binge-type eating disorders (23, 35).
It is possible that IPT may be superior to HE in the reduction and abstinence of the classic binge-eating episodes that characterize binge-eating disorder and bulimia nervosa. Although, in the current study, girls in HE reported slightly but significantly more baseline episodes than did participants in IPT, the observed improvements in binge eating were consistent with our pilot-study results, in which girls randomly assigned to IPT reported more baseline episodes than did those in HE (25). These data parallel adult studies (21–23) and suggest that IPT may be an effective approach for reducing binge-eating episodes in at-risk adolescent girls. Classic binge-eating episodes in youth predict a number of adverse psychological outcomes (14, 41, 42), excess adiposity gain (43), and components of the metabolic syndrome over 5–6 y (44). The observed reductions in binge-eating may ultimately prevent the development or worsening of these problems. Nevertheless, because only one-third of girls reported binge-eating at baseline, and the finding was based on a follow-up analysis, these results require replication. The development of binge-eating disorder throughout the course of the follow-up period was rare; however, 5 girls developed probable anorexia nervosa–type or bulimia nervosa–type eating disorders, 4 girls of whom were assigned to HE. Because the study was not powered to detect group differences in the development of these eating disorders, it was unsurprising that this finding did not reach significance. Because IPT is acceptable to therapists (45) and has been previously delivered with high fidelity and effectiveness by community leaders with limited counseling experience (40), studies should determine whether group IPT is a cost-effective approach for simultaneously reducing adolescent binge eating and preventing undue weight gain in community settings.
Neither reductions in LOC-eating nor improvements in mood predicted the observed changes in BMI indexes or adiposity. However, social functioning improvements during the programs, regardless of the group assignment, were associated with lower BMI at 1 y. This effect is consistent with data from adults (46) and children (47) that indicated that social support facilitates maintenance after weight loss. Because, on average, social functioning did not significantly change over time across groups, but individual changes in social functioning predicted improvements in BMI, it is possible that, in adolescent girls with LOC eating, girls with with significant difficulties in interpersonal relationships may be especially responsive to programs that provide positive social support regardless of the intervention type.
Strengths of the study included its theoretical foundation, use of a comparison group matched for time and attention, and a racially/ethnically diverse sample. Moreover, we had high therapist adherence to the intervention and comparison manuals and very good retention. We also used interview-based measures of disordered eating and objective measurements of weight and adiposity. Limitations include the relatively short follow-up interval of 1 y. Effects of IPT on body weight and adiposity may take longer for group differences to emerge. Indeed, there have been some adult data to suggest that IPT's impact on eating pathology takes longer than other programs (48), and at least one study showed that group differences do not emerge until 4 y after therapy (49).
In conclusion, intervening with adolescent girls of above-average weight with LOC eating appears to have a beneficial impact on age-adjusted BMI and the percentage of adiposity and reduces disordered-eating episodes and negative mood symptoms. IPT may have additional benefits; specifically, reducing classic binge-eating episodes as well as decreasing LOC-eating in racial-ethnic minority girls. Future research is required to determine whether IPT may be more effective than a nonintervention control or compared with HE for reducing eating pathology and weight trajectories in girls specifically reporting objectively large binge-eating episodes.
Supplementary Material
Acknowledgments
The authors’ responsibilities were as follows—MT-K: designed the study; oversaw the entire study including recruitment, data collection, and group-intervention programs; supervised the delivery of the program; had full access to all data in the study; took responsibility for the integrity of data and accuracy of the data analysis; and drafted the manuscript; LBS: was involved in all aspects of data collection, conducted intervention programs, had full access to data, managed and analyzed data, and assisted in drafting the manuscript and interpretation of study findings; DEW and JFY: provided feedback on the study design, supervised the experimental program, and were involved in the interpretation of study findings; TS and MS: assisted in carrying out group programs and were involved in the interpretation of study findings; LMR, CE, RMR, and AV: conducted assessments and intervention programs and were involved in the interpretation of study findings; SB: conducted physical examinations and was involved in the interpretation of study findings; EJB, RO, and SSB: conducted intervention programs and were involved in the interpretation of study findings; CO: oversaw the data analysis, had full access to data, and was involved in the interpretation of study findings; MK: was involved in the study design, data collection, and the interpretation of study findings; JCR: oversaw the body-composition data collection and interpretation of study findings; and JAY: designed the study, oversaw the entire study, had full access to data, and assisted in drafting the manuscript and interpretation of study findings. JAY and MK are commissioned officers in the US Public Health Service. MS is active duty in the US Navy. None of the authors had a conflict of interest.
Footnotes
Abbreviations used: DXA, dual-energy X-ray absorptiometry; HE, health education; IPT, interpersonal psychotherapy; LOC, loss of control.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nader PR, O'Brien M, Houts R, Bradley R, Belsky J, Crosnoe R, Friedman S, Mei Z, Susman EJ. Identifying risk for obesity in early childhood. Pediatrics 2006;118:e594–601. [DOI] [PubMed] [Google Scholar]
- 3.Field AE, Cook NR, Gillman MW. Weight status in childhood as a predictor of becoming overweight or hypertensive in early adulthood. Obes Res 2005;13:163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilfley DE, Tibbs TL, Van Buren DJ, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychol 2007;26:521–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Field AE, Camargo CA, Jr, Ogino S. The merits of subtyping obesity: one size does not fit all. JAMA 2013;310:2147–8. [DOI] [PubMed] [Google Scholar]
- 6.Goldschmidt AB, Wilfley DE, Paluch RA, Roemmich JN, Epstein LH. Indicated prevention of adult obesity: how much weight change is necessary for normalization of weight status in children? JAMA Pediatr 2013;167:21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haines J, Kleinman KP, Rifas-Shiman SL, Field AE, Austin SB. Examination of shared risk and protective factors for overweight and disordered eating among adolescents. Arch Pediatr Adolesc Med 2010;164:336–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull 2004;130:19–65. [DOI] [PubMed] [Google Scholar]
- 9.Neumark-Sztainer D. Can we simultaneously work toward the prevention of obesity and eating disorders in children and adolescents? Int J Eat Disord 2005;38:220–7. [DOI] [PubMed] [Google Scholar]
- 10.Irving LM, Neumark-Sztainer D. Integrating the prevention of eating disorders and obesity: feasible or futile? Prev Med 2002;34:299–309. [DOI] [PubMed] [Google Scholar]
- 11.Neumark-Sztainer D. Preventing obesity and eating disorders in adolescents: what can health care providers do? J Adolesc Health 2009;44:206–13. [DOI] [PubMed] [Google Scholar]
- 12.Yanovski SZ. Binge eating disorder and obesity in 2003: could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord 2003;34(suppl):S117–20. [DOI] [PubMed] [Google Scholar]
- 13.Tanofsky-Kraff M, Yanovski SZ, Yanovski JA. Loss of control over eating in children and adolescents. In: Striegel-Moore R, Wonderlich SA, Walsh BT, Mitchell JE, eds. Developing an Evidence-Based Classification of eating disorders: scientific findings for DSM-5. Washington, DC: American Psychiatric Association Press, 2011:221–36.
- 14.Sonneville KR, Horton NJ, Micali N, Crosby RD, Swanson SA, Solmi F, Field AE. Longitudinal associations between binge eating and overeating and adverse outcomes among adolescents and young adults: does loss of control matter? JAMA Pediatr 2013;167:149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stice E, Cameron RP, Killen JD, Hayward C, Taylor CB. Naturalistic weight-reduction efforts prospectively predict growth in relative weight and onset of obesity among female adolescents. J Consult Clin Psychol 1999;67:967–74. [DOI] [PubMed] [Google Scholar]
- 16.Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord 2009;42:26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Field AE, Austin SB, Taylor CB, Malspeis S, Rosner B, Rockett HR, Gillman MW, Colditz GA. Relation between dieting and weight change among preadolescents and adolescents. Pediatrics 2003;112:900–6. [DOI] [PubMed] [Google Scholar]
- 18.Hilbert A, Hartmann AS, Czaja J, Schoebi D. Natural course of preadolescent loss of control eating. J Abnorm Psychol 2013;122:684–93. [DOI] [PubMed] [Google Scholar]
- 19.Tanofsky-Kraff M, Shomaker LB, Olsen C, Roza CA, Wolkoff LE, Columbo KM, Raciti G, Zocca JM, Wilfley DE, Yanovski SZ, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol 2011;120:108–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association, 2013. [Google Scholar]
- 21.Wilfley DE, Agras WS, Telch CF, Rossiter EM, Schneider JA, Cole AG, Sifford LA, Raeburn SD. Group cognitive-behavioral therapy and group interpersonal psychotherapy for the nonpurging bulimic individual: a controlled comparison. J Consult Clin Psychol 1993;61:296–305. [DOI] [PubMed] [Google Scholar]
- 22.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, Dounchis JZ, Frank MA, Wiseman CV, Matt GE. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch Gen Psychiatry 2002;59:713–21. [DOI] [PubMed] [Google Scholar]
- 23.Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry 2010;67:94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanofsky-Kraff M, Wilfley DE, Young JF, Mufson L, Yanovski SZ, Glasofer DR, Salaita CG. Preventing excessive weight gain in adolescents: interpersonal psychotherapy for binge eating. Obesity (Silver Spring) 2007;15:1345–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tanofsky-Kraff M, Wilfley DE, Young JF, Mufson L, Yanovski SZ, Glasofer DR, Salaita CG, Schvey NA. A pilot study of interpersonal psychotherapy for preventing excess weight gain in adolescent girls at-risk for obesity. Int J Eat Disord 2010;43:701–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fairburn CG, Cooper Z. eds. The Eating Disorder Examination. 12th ed. New York, NY: Guilford Press, 1993. [Google Scholar]
- 27.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry 1976;33:1111–5. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation, 1996. [Google Scholar]
- 29.Spielberger CD. Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press, 1983. [Google Scholar]
- 30.Young JF, Mufson L, Davies M. Efficacy of Interpersonal Psychotherapy-Adolescent Skills Training: an indicated preventive intervention for depression. J Child Psychol Psychiatry 2006;47:1254–62. [DOI] [PubMed] [Google Scholar]
- 31.Wilfley DE, MacKenzie KR, Welch RR, Ayres VE, Weissman MM. Interpersonal psychotherapy for group. New York, NY: Basic Books, 2000. [Google Scholar]
- 32.Bravender T. Health, education, and youth in Durham: HEY-Durham curricular guide. 2nd ed. Durham, NC: Duke University, 2005. [Google Scholar]
- 33.Chui W, Safer DL, Bryson SW, Agras WS, Wilson GT. A comparison of ethnic groups in the treatment of bulimia nervosa. Eat Behav 2007;8:485–91. [DOI] [PubMed] [Google Scholar]
- 34.Chatellier G, Zapletal E, Lemaitre D, Menard J, Degoulet P. The number needed to treat: a clinically useful nomogram in its proper context. BMJ 1996;312:426–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Goulding A, Taylor RW, Gold E, Lewis-Barned NJ. Regional body fat distribution in relation to pubertal stage: a dual-energy X-ray absorptiometry study of New Zealand girls and young women. Am J Clin Nutr 1996;64:546–51. [DOI] [PubMed] [Google Scholar]
- 36.Yalom ID, Leszcz M. The theory and practice of group psychotherapy. 5th ed. New York, NY: Basic Books, 2005. [Google Scholar]
- 37.Haines J, Neumark-Sztainer D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res 2006;21:770–82. [DOI] [PubMed] [Google Scholar]
- 38.Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: a 2-year prospective investigation. Health Psychol 2002;21:131–8. [PubMed] [Google Scholar]
- 39.Karver MS, Handelsman JB, Fields S, Bickman L. Meta-analysis of therapeutic relationship variables in youth and family therapy: the evidence for different relationship variables in the child and adolescent treatment outcome literature. Clin Psychol Rev 2006;26:50–65. [DOI] [PubMed] [Google Scholar]
- 40.Bass J, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, Ndogoni L, Speelman L, Weissman M, Bolton P. Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes. Br J Psychiatry 2006;188:567–73. [DOI] [PubMed] [Google Scholar]
- 41.Skinner HH, Haines J, Austin SB, Field AE. A prospective study of overeating, binge eating, and depressive symptoms among adolescent and young adult women. J Adolesc Health 2012;50:478–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Presnell K, Stice E, Seidel A, Madeley MC. Depression and eating pathology: prospective reciprocal relations in adolescents. Clin Psychol Psychother 2009;16:357–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, Keil M, Reynolds JC, Yanovski JA. A prospective study of psychological predictors of body fat gain among children at high risk for adult obesity. Pediatrics 2006;117:1203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tanofsky-Kraff M, Shomaker LB, Stern EA, Miller R, Sebring N, Dellavalle D, Yanovski SZ, Hubbard VS, Yanovski JA. Childrenaposs binge eating and development of metabolic syndrome. Int J Obes (Lond) 2012;36:956–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tanofsky-Kraff M, Wilfley DE. Interpersonal psychotherapy for eating disorders. In: Agras WS, ed. Oxford handbook of eating disorders. Oxford, United Kingdom: Oxford University Press, 2010:348–72.
- 46.Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol 1999;67:132–8. [DOI] [PubMed] [Google Scholar]
- 47.Wilfley DE, Stein RI, Saelens BE, Mockus DS, Matt GE, Hayden-Wade HA, Welch RR, Schechtman KB, Thompson PA, Epstein LH. Efficacy of maintenance treatment approaches for childhood overweight: a randomized controlled trial. JAMA 2007;298:1661–73. [DOI] [PubMed] [Google Scholar]
- 48. National Institute for Health and Clinical Excellence. Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. Leicester, United Kingdom: NICE, 2004. [PubMed]
- 49.Hilbert A, Bishop ME, Stein RI, Tanofsky-Kraff M, Swenson AK, Welch RR, Wilfley DE. Long-term efficacy of psychological treatments for binge eating disorder. Br J Psychiatry 2012;200:232–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.