Abstract
Background:
The aim of this study was to evaluate the effect of Filmed modeling in comparison with commonly used Tell-Show-Do technique (T.S.D) on the anxious and cooperative behavior of 4-6 years old children during dental practice.
Materials and Methods:
Forty six children aged 4-6 years were enrolled in this study and randomly allocated into two groups. Group I: At the first visit, the procedure of Tell-Show-Do, and at the second visit, the treatment procedures were performed by the dentist for the children. Group II: At the first visit, children watched a film consisting of the procedure of Tell-Show-Do performed on a child model. At the second visit, treatment procedures were performed. In both groups, during the treatment procedure, index of heart rate was measured and behaviors of children were recorded. The children's anxious and cooperative behaviors on the recordings were quantified according to Venham and Frankl rating scales, respectively. The data were compared between two groups using T-test method. All statistical references were made at 0.05.
Results:
There were no statistically significant differences in heart rate measures, clinical anxiety and cooperative behavior scores of children between the two groups (P = 0.6).
Conclusion:
Filmed modeling can be an efficient alternative method to Tell-Show-Do technique in pre-appointment preparation of the 4-6 years old children during dental treatment.
Keywords: Cooperative behavior, dental anxiety, film modeling, pediatric dentistry
INTRODUCTION
Dental appointment is a stressful situation, which raises children's anxiety level and avoidance behavior. Children's dental anxiety is an intense but situational and transient anxiety.[1] If it is not managed, it will possibly continue to adulthood.[2] Several communicative, advanced and pharmacological interventions have been developed to manage children's anxious and cooperative behaviors.[3] The American Academy of Paediatric Dentistry (AAPD) recommended focusing more on non-pharmacologic intervention in future studies.[4]
The first dental visit is crucial in the formation of the child's attitude toward dentistry and future treatment success. Tell-Show-Do technique is commonly used by pediatric dentists in management of children's anxiety at a pre-treatment visit. It dictates that before anything is done, the child be told what will be done and then shown by some sort of simulation exactly what will happen before the procedure is started. Tell-Show-Do technique is based on principle of learning theory;[5,6] and is performed by the dentists themselves in the operatory room.
Other methods such as desensitization, observational modeling and play therapy have also been recognized for the modification of children's behavior.[6] Modeling refers to learning by observation and children may reproduce behavior exhibited by the model in the same situation. It was described by Bandura in 1967 as a process which can reduce children's fear and avoidance behavior.[5] Modeling can be performed in two forms: live or filmed one. Studies on modeling have demonstrated its therapeutic effect in management of anxiety[7,8] and educational effect in improving coping skills of children in medical stressful situations.[9] Modeling can have a deserving educational effect in patient with different intelligence quotient.[10,11]
It has been suggested to use the live or Filmed modeling technique as an effective intervention to prepare the child for a dental visit.[12] Live models such as peers, siblings or parents are used for pre- appointment teaching of the expected behavior to the child patient.[13,14,15] Several studies have evaluated the efficiency of the modeling through a film in the reduction of child's dental anxiety.[16,17,18,19,20,21,22] It has been shown that Filmed modeling can be effective as well as live modeling and also desensitization methods.[16,18] Contrary to other social learning-based methods, Filmed modeling does not take time by the dentist and dental team; although it has not achieved its proper situation.[12]
The aim of this study was to evaluate the effectiveness of Filmed modeling in comparison with common and effective Tell-Show-Do technique in a group of Iranian children and to introduce an alternative time saving method to practitioners.
MATERIALS AND METHODS
This randomized clinical trial study was approved by Ethics Committee of Zahedan University of Medical Sciences and conducted in pediatric clinic of Zahedan dental school in 2010.
Among the patients referred to the clinic, 46 children aged 4-6 years (±2 months) were enrolled in the study according to the inclusion criteria [Figure 1]. They had caries lesion in one of the primary mandibular molars and needed a pulpotomy with restoration treatment. It was confirmed that they have no previous experience of hospitalization and dental visit. The children with systemic diseases and developmental disorders were excluded from the study. The examination was completed and the necessary radiographs were prescribed.
Figure 1.
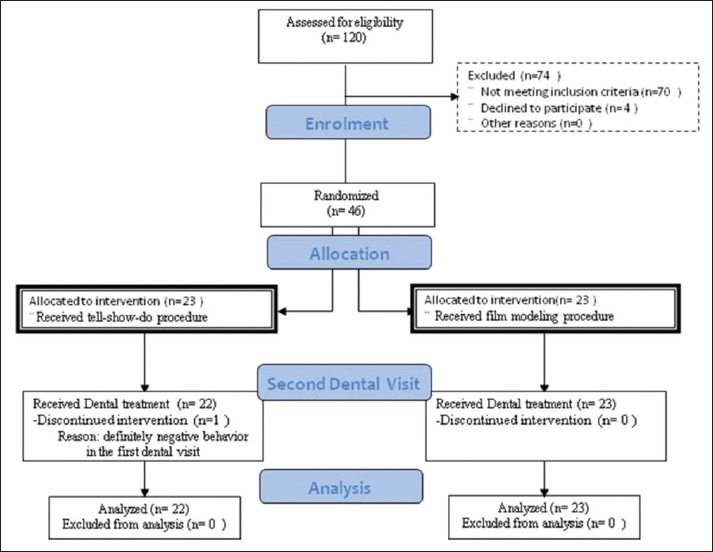
Flowchart of patient's selection and randomization in two study groups (Tell-Show- Do and Filmed modeling groups)
Each child's parent was asked to complete the informed consent and a questionnaire gathering demographic characteristics of the child and family. Then, the child was enrolled in one of the study groups based on balanced block randomization as follows:
Group I (Tell-Show-Do Group) (Control): Children came in the operation room. Tell-Show-Do, prophylaxis with paste and rubber cap and fluoride therapy was performed by the dentist for each participant to increase their familiarity with dental procedures. The duration of the appointment was about 20 minutes and constant for all children. At the end of the first visit, the child was rewarded and the date of the second treatment visit was set for one week later. A child in the first group was excluded from the study because of his definitely negative behavior (Score I in Frankl index).
In the second session, the child entered the operating room alone. A video-camera located on the top of the dental unit light pole under a covering cloth was focused on the child's head and hands and started to record child's behavior.
The required injection including the use of topical anesthesia and a mandibular alveolar nerve block technique was performed by the dentist. The heart beat rate of each child was recorded manually before and following the injection by the dentist. Then, the occlusal cavity was prepared for pulpotomy and restoration of the teeth. The treatment protocol was the same for all the participants.
In all children, parameters such as the attending dentist, his assistant, the working environment, time and duration (30 minutes for each child) of work, and the type of dialogues were all the same. Care was taken to make sure that the children were not tired, hungry, or did not have a common cold.
Group II (Filmed modeling group): The children were directed to a quiet and comfort room to watch a film presented by a dental assistant. The film showed the same procedure consisting of Tell-Show-Do, prophylaxis with paste and rubber cap and fluoride therapy on a 5-year-old child model with a time of 20 minutes. The child in the film was cooperative and was reinforced by a reward at the end of the procedure. The produced film had been approved by 3 pediatric dentists.
The second treatment session was set for one week later. Dental procedures, measurement of the heart rate and recording of the behaviors were all performed as in Group I.
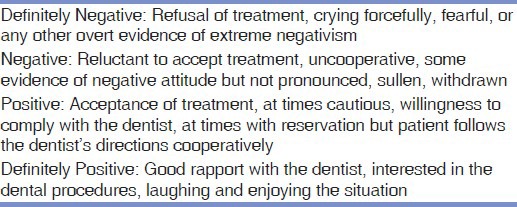
The recorded videotapes of all children were independently evaluated by 2 pediatric dentists who were blind to the grouping of the children. Children's anxiety reactions and cooperative behaviors were scored based on Venham Scale and Frankle Index, respectively [Tables 1 and 2]. The viewers were asked to rate the child's responses in two stages: At the injection of local anesthesia and at the beginning of the tooth preparation.
Table 1.
Venham 6-point Index used to quantify the anxious behavior of 4-6-year-old children in the Tell-Show-Do and Filmed modeling groups
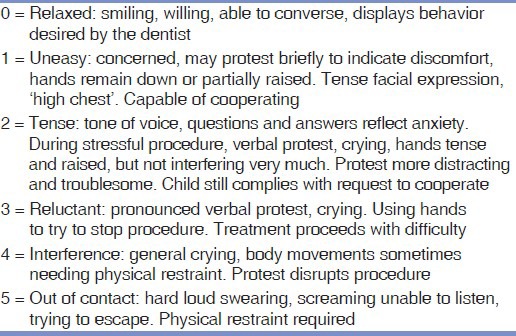
Table 2.
Frankle 4-point Index used to quantify the cooperative behavior of 4-6 year old children in the Tell-Show-Do and Filmed modeling groups
Statistical analysis
Mean of heart rate measurements and behavioral ratings were used for statistical analyses. Data analysis was performed applying t-test method in software package of statistical analysis (SPSS-15, SPSS Inc., Chicago, IL, USA). All statistical references were made at 0.05.
RESULTS
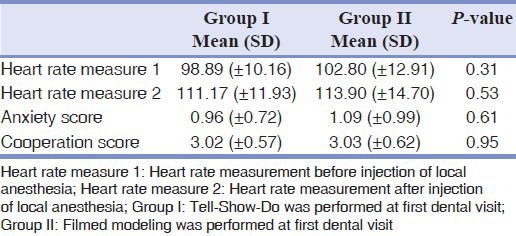
A total number of 46 children, 22 boys and 24 girls, participated in the study and allocated between Tell-Show-Do (n = 23) and Filmed modeling (n = 23) groups. At the first visit, a child in Group I showed definite negative behavior of score level I based on Frankle index and was excluded from the study. Data revealed that both groups were the same in demographic characteristics including their sex, mean age, parental education and age, parental dental experiences, number of children in the family, and participation in kindergarten. Table 3 shows the mean and standard deviation (SD) for the heart beat rate, anxiety level, and cooperative behavior of children during treatment in two groups. Accordingly, heart rate mean scores (before and after local anesthesia injection) showed no significant differences between two groups (P = 0.6). Moreover, there were no statistically significant differences for the anxious and cooperative behavioral mean scores between two groups (P > 0.05).
Table 3.
Comparison of heart rate measures, anxiety and cooperation level of 4-6-year-old children between Tell-Show-Do and Filmed modeling Groups
DISCUSSION
Establishment of communication is the key for developing sound rapport with any patient.[3] Based on Piaget's classification, children aged 4-6 years are in the pre-operational phase. The increment in vocabulary, attention, and concentration abilities in this period are signs of their readiness for social communications such as a dental visit.[23]
Tell-Show-Do technique is the backbone of the child's education and behavior guidance and is commonly used in the first appointment. Several epidemiological inquiries have revealed its positive effect on the reduction of dental anxiety;[24] but, performance of Tell-Show-Do needs the time constraints of both the dentist and the parents.
This study was designed to evaluate the efficiency of the videotaped model to familiarize the child patient with the dental visit. The results of this study showed that Filmed modeling is as efficient as Tell-Show-Do technique in the reduction of 4-6 years’ old children anxiety and increase their cooperative behavior during dental treatment.
The film was produced about a peer model in the same dental situation. It has been confirmed that a videotape showing a peer model coping with the similar dental procedures is more effective in reducing disruptive behavior and anxiety in comparison with an unrelated film. It also prevents more information to be imparted and the child patients were sensitized to the procedures.[17,19,20]
It was attempted to prepare the film in conditions like that the children in Group I experienced. The operatory room and the dentist in the film were the same as in Group I. In the film, model's mother left the operatory room like the children in Group I who experienced parental absence. The parent's absence/presence in the dentistry operation room has no impact on the cooperation and anxiety of the preschool children who have had no previous dental presentation.[25] Hence, the mothers were asked to leave the room to prevent the child — parent interactions.
At the end of the film, it was shown that the model was rewarded. Along with the presentation of proper information to the child, reinforcement of the appropriate behavior of the model is an important element of modeling procedure. It prompts the learning and performance of that behavior in the child to receive the rewards.[1,26]
Studies by Machen and Johnson,[16] Melamed et al.[17,19] and Yahaya and Salam[22] have found the effectiveness of Filmed modeling in comparison to desensitization in various patients.
Fields and Pinkham, and Rouleau et al.[18,20] performed the procedure of prophylaxis at the first visit and presented a videotaped model to children at the following visits. They concluded that the presentation of a model through a film causes the children manifest relatively little negative verbalization and behavior and also request less parental presence. It seems that the procedure of prophylaxis before the film presentation can have positive effects on the child's familiarization and dental behaviors.
In this study, for the evaluation of the specific effects of the modeling through a film, children in group II did not experience the prophylaxis procedure before the film presentation. Furthermore, the operator dentist was absent throughout the film presentation and the treatment procedure was performed one week later after watching the film. When the children visited the dentist at second appointment, they didn’t exhibit signs of severe anxiety and negative verbalization or behavior more than the children who were familiarized to the dentist and experienced Tell-Show-Do procedure. It seems that the information presented in the film was efficient in the familiarization of the child to the dentist and the description about the procedure. Therefore, the children in group II showed the behavior expected to do in a dental visit.
In previous studies, the clinical behaviors of the children have been assessed. The behavior of the child is not enough to detect the child's anxiety. In evaluating anxiety and cooperation levels of children in this study, the physiological and behavioral indexes were used simultaneously. The physiological index included the heart beat rate. It has been shown that this index is more in line with the anxiety experienced in dental visits.[27]
For assessing the child's behavior in the dental visit, the treatment appointment was recorded through a video-camera, and then the child's behavioral reactions were quantified by an unaware observer (the blind method) using two scales. The scales used in our study were that of Frankle scale for cooperative behaviors and Venham Scale for anxious behaviors. These are very easy and quick methods with a reliability and validity for statistical analyses.[25]
At the first visit, a child in Group I showed definite negative behavior with a score level I based on Frankle index and was excluded from the study. Accordingly, further investigations are suggested to evaluate the effectiveness of Filmed modeling on the children with negative behaviors including scores I and II of Frankle index.
CONCLUSION
Filmed modeling is as efficient as Tell-Show-Do technique to control 4-6 years old children anxiety and cooperative behavior during dental treatment and may be a proper alternative method for Tell-Show-Do technique in some situations. Manifesting no more negative verbalization/behavior especially during child — mother separation and taking less time in comparison with Tell-Show-Do technique are the advantages of providing a model through films.
ACKNOWLEDGMENT
This study is based on a thesis to the graduate faculty, Faculty of Dentistry, Zahedan University of Medical Sciences, in partial fulfillment of the requirements for the M.S. degree. It has been reviewed and published in clinicaltrial.gov website (Identifier number: NCT01908127).
Footnotes
Source of Support: Zahedan University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Graziano AM, DeGiovanni IS, Garcia KA. Behavioural treatment of children's fears: A review. Psychol Bull. 1979;86:804–30. [PubMed] [Google Scholar]
- 2.Locker D, Thomson WM, Poulton R. Onset of and patterns of change in dental anxiety in adolescence and adulthood: A Birth Cohort Study. Community Dent Health. 2001;18:99–104. [PubMed] [Google Scholar]
- 3.Wilson S. Non-pharmacologic issues in pain perception and control. In: Casa Massimo PS, Fields HW, McTigue DJ, Nowak AJ., editors. Paediatric dentistry - Infancy through adolescence. 5th ed. Philadelphia: Elsevier Saunders; 2013. p. 94. [Google Scholar]
- 4.Adair SM. Behaviour management conference panel I report-Rationale for behaviour management techniques in paediatric dentistry. Paediatr Dent. 2004;26:167–70. [PubMed] [Google Scholar]
- 5.Wright GZ, Stigers JI. Non-pharmacologic management of children's behaviors. In: Dean JA, Avery DR, McDonald RE, editors. Dentistry for the Child and Adolescence. 9th ed. St. Louis: CV Mosby Co; 2011. p. 30. [Google Scholar]
- 6.Townsend JA. Behaviour guidance of the paediatric dental patient. In: Casa Massimo PS, Fields HW, McTigue DJ, Nowak AJ., editors. Paediatric Dentistry — Infancy through Adolescence. 5th ed. Philadelphia: Elsevier Saunders; 2013. p. 358. [Google Scholar]
- 7.Melamed BG, Siegel LJ. Reduction of anxiety in children facing hospitalization and surgery by use of filmed modelling. J Consult Clin Psychol. 1975;43:511–21. doi: 10.1037/h0076896. [DOI] [PubMed] [Google Scholar]
- 8.Peterson L, Schultheis K, Ridley-Jonson R, Miller DJ, Tracy K. Comparison of three modeling procedures on the pre-surgical and post surgical reaction of children. Behav Ther. 1984;15:197–203. [Google Scholar]
- 9.Krouse HJ. Video modelling to educate patients. J Adv Nurs. 2001;33:748–57. doi: 10.1046/j.1365-2648.2001.01716.x. [DOI] [PubMed] [Google Scholar]
- 10.Boudreau E, Entremont B. Improving the pretend play skills of preschoolers with autism spectrum disorders: The effects of video modelling. J Dev Phys Disabil. 2010;22:415–31. [Google Scholar]
- 11.Charlop-Christy MH, Le L, Freeman KA. A comparison of video modelling with in vivo modelling for teaching children with autism. J Autism Dev Disord. 2000;30:537–52. doi: 10.1023/a:1005635326276. [DOI] [PubMed] [Google Scholar]
- 12.Greenbaum PE, Melamed BG. Pre-treatment modelling: A technique for reducing children's fear in the dental operatory. Dent Clin North Am. 1988;32:693–704. [PubMed] [Google Scholar]
- 13.Stokes TF, Kennedy SH. Reducing child uncooperative behaviour during dental treatment through modelling and reinforcement. J Appl Behav Anal. 1980;13:41–9. doi: 10.1901/jaba.1980.13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farhat-McHayleh N, Harfouche A, Souaid P. Techniques for managing behaviour in pediatric dentistry: Comparative study of live modelling and Tell-Show-Do based on children's heart rates during treatment. J Can Dent Assoc. 2009;75:283. [PubMed] [Google Scholar]
- 15.Howard KE, Freeman R. An evaluation of the PALS after treatment modelling intervention to reduce dental anxiety in child dental patients. Int J Paediatr Dent. 2009;19:233–42. doi: 10.1111/j.1365-263X.2009.00977.x. [DOI] [PubMed] [Google Scholar]
- 16.Machen B, Johnson R. Desensitization, model learning and the dental behaviour of children. J Dent Res. 1974;53:83–6. doi: 10.1177/00220345740530013701. [DOI] [PubMed] [Google Scholar]
- 17.Melamed BG, Hawes RR, Heiby E, Glick J. Use of filmed modelling to reduce uncooperative behaviour of children during dental treatment. J Dent Res. 1975;54:797–801. doi: 10.1177/00220345750540041701. [DOI] [PubMed] [Google Scholar]
- 18.Fields H, Pinkham J. Videotape modelling of the child dental patient. J Dent Res. 1976;55:958–63. doi: 10.1177/00220345760550064601. [DOI] [PubMed] [Google Scholar]
- 19.Melamed BG, Yurcheson R, Flees EL, Hutcherson S, Hawes R. Effects of film modelling on reduction of anxiety-related behaviours in individuals varying in level of previous experience in the stress situation. J Consult Clin Psychol. 1978;46:1357–67. doi: 10.1037//0022-006x.46.6.1357. [DOI] [PubMed] [Google Scholar]
- 20.Rouleau J, Ladouceur R, Dufour L. Pre-exposure to the first dental treatment. J Dent Res. 1981;60:30–4. doi: 10.1177/00220345810600010601. [DOI] [PubMed] [Google Scholar]
- 21.Klingman A, Melamed BG, Cuthbert MI, Hermecz DA. Effects of participant modelling on information acquisition and skill utilization. J Consult Clin Psychol. 1984;52:414–22. doi: 10.1037//0022-006x.52.3.414. [DOI] [PubMed] [Google Scholar]
- 22.Yahaya WAJ, Salam SNA. Usability design strategies for children: Developing children learning and knowledge in decreasing children dental anxiety. Proceedings of the International Conference on Primary Education, Hong Kong. 2009 Nov 25-27; [Google Scholar]
- 23.Casamassimo PS, Adair SM. The Dynamics of Change. In: Casa Massimo PS, Fields HW, McTigue DJ, Nowak AJ., editors. Paediatric Dentistry - Infancy through Adolescence. 5th ed. Philadelphia: Elsevier Saunders; 2013. p. 252. [Google Scholar]
- 24.Klingberg G, Raadal M, Arnrup K. Dental fear and Behavior management problems. In: Koch G, Paulsen S, editors. Pediatric dentistry — a clinical approach. 2st ed. USA: Wiley-Blackwell Publishing Ltd; 2009. pp. 32–43. [Google Scholar]
- 25.Afshar H, Baradaran Nakhjavani Y, Mahmoudi-Gharaei J, Paryab M, Zadhoosh S. the effect of parental presence on the 5 year-old children's anxiety and cooperative behavior in the first and second dental visit. Iran J Pediatr. 2011;21:193–200. [PMC free article] [PubMed] [Google Scholar]
- 26.Baghdadi ZD. Principles and application of learning theory in child management. Quintessence Int. 2001;32:135–41. [PubMed] [Google Scholar]
- 27.Lewis TM, Law DB. Investigation of certain autonomic responses of children to a specific dental stress. J Am Dent Assoc. 1958;57:769–78. doi: 10.14219/jada.archive.1958.0226. [DOI] [PubMed] [Google Scholar]


