Abstract
Respiratory syncytial virus (RSV) is the leading cause of respiratory infection in infants and young children. Severe clinical manifestation of RSV infection is a bronchiolitis, which is common in infants under six months of age. Recently, RSV has been recognized as an important cause of respiratory infection in older populations with cardiovascular morbidity or immunocompromised patients. However, neither a vaccine nor an effective antiviral therapy is currently available. Moreover, the interaction between the host immune system and the RSV pathogen during an infection is not well understood. The innate immune system recognizes RSV through multiple mechanisms. The first innate immune RSV detectors are the pattern recognition receptors (PRRs), including toll-like receptors (TLRs), retinoic acid-inducible gene-I (RIG-I)-like receptors (RLRs), and nucleotide-biding oligomerization domain (NOD)-like receptors (NLRs). The following is a review of studies associated with various PRRs that are responsible for RSV virion recognition and subsequent induction of the antiviral immune response during RSV infection. [BMB Reports 2014; 47(4): 184-191]
Keywords: Interferon-beta promoter stimulator 1 (IPS-1), Pattern recognition receptor (PRR), Respiratory syncytial virus (RSV), Retinoic acid-inducible gene-I (RIG-I), Toll-like receptor (TLR)
INTRODUCTION
RSV is a major cause of respiratory illness in young children, contributing significantly to morbidity and mortality worldwide. Most infants are infected with RSV at least once within first two years of life. In some cases, RSV provokes severe lower respiratory tract illness, such as pneumonia or bronchiolitis. As a result, many of these patients are plagued by recurrent childhood wheezing or asthma. Moreover, RSV infection is well known to recur many times throughout life, but the mechanism of innate immune responses against RSV infection is unclear. RSV is now recognized as an important cause of respiratory infection in elderly patients who are immunocompromised or have cardiovascular disease.
RSV was first isolated from chimpanzees as a chimpanzee coriza agent in 1955 (1). Shortly after, a similar virus was recovered from infants with respiratory illness and designated RSV (2,3). RSV is an enveloped negative sense single-strand RNA (ssRNA) virus of the Paramyxoviridae family and belongs to the subfamily Pneumovirinae. RSV consists of a single serotype and two antigenic subtypes, A or B. The RSV genome is about 15 kb nucleotides in length and encodes nine structural proteins and two non-structural proteins (4). Three envelop glycoproteins, G, F and SH, are present on both the viral membrane and infected cells. F and G are the only RSV proteins that induce neutralizing antibodies (5,6). The name RSV was given because the F proteins on the viral surface cause the membranes on nearby cells to merge, forming syncytia. NS1 and NS2 inhibit the type I interferon (IFN) host response by interrupting the janus kinase-signal transducers and activators of the transcription 1 (JAK-STAT) pathway (7-9).
The incidence of RSV infection is elevated from winter to early spring. Unlike the seasonal influenza virus, there is no licensed vaccine against RSV. The only prevention method for high-risk infants is monthly injections of palivizumab, RSV neutralizing monoclonal antibodies, during the epidemic season. Many attempts have been made for vaccine development. In the mid-1960s, a formalin-inactivated (FI) vaccine candidate caused the deaths of two infants who were enrolled in a clinical trial (10). Even today, no live attenuated vaccines or live virus vectored vaccines exist. Recently, other types of vaccines, purified proteins, virus-like particles (VLPs), nanoparticles, and DNA or vectors expressing RSV proteins, are being developed for various target populations (11-13). Nonetheless, no vaccine is currently applicable. Moreover, therapeutic methods are limited in that the nucleoside analog ribavirin is only used to treat RSV infection in the pediatric population. In addition, studies have shown that the ribavirin has limited efficacy and can induce hemolytic anemia as a side effect (14).
Similar to other respiratory viruses, RSV infection or uptake by airway epithelial cells, alveolar macrophages, and intraepithelial dendritic cells incites a direct antiviral response through cytokines and chemokines and initiates an adaptive immune response. Sentinel cells, like dendritic cells (DCs) or macrophages, have pattern recognition receptors (PRRs), toll-like receptors (TLRs), retinoic acid-inducible gene-I (RIG-I)-like receptors (RLRs), or nucleotide-biding oligomerization domain (NOD)-like receptors (NLRs), which recognize pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) on the pathogen (15). These PRRs recognize many different PAMPs and activate transcription factor nuclear factor (NF)-κB, a member of the interferon regulatory factor (IRF) family, which regulates the expression of proinflammatory cytokines and type I interferon. This review focuses on the role of these various PRRs, which are responsible for recognizing the RSV virion and inducing the antiviral immune response during RSV infection.
RSV-SPECIFIC PATTERN RECOGNITION RECEPTORS
TLR2/6
TLR2 is located on the cell surface and recognizes cell wall compartments, such as peptidoglycan or lipoprotein. Recognition leads to subsequent innate immune activation via the MyD88 mediated pathway (Fig. 1). Studies have shown that TLR2 expression is upregulated in RSV-infected airway epithelial cells (16,17). In addition, TLR2 blocking antibodies suppressed heat-inactivated RSV-induced proinflammatory cytokines in airway epithelial cells (18). Peritoneal macrophages obtained from TLR2- or TLR6-deficient mice showed impaired production of proinflammatory cytokines and chemokines; however, production of type I IFN was not affected by RSV infection (19). TLR2-deficient mice actually showed uncontrolled viral replication in the RSV-infected lung as well as impaired neutrophil migration and DC activation. It appears that TLR2 plays a role in innate immune activation, but does not contribute to the production of type I IFN. How TLR2 recognizes the RSV virion remains unknown.
Fig. 1. Role of Toll-like receptors during RSV infection. Stimulation of TLR4 with RSV F glycoprotein in a TRIF- or MyD88-dependent signaling pathway induces production of type I interferon or proinflammatory cytokines. TLR2/6, which are activated by RSV, enhance production of type I interferon or proinflammatory cytokines through a MyD88-mediated pathway. TLR7, localized in the endosome, recognizes the RSV ssRNA genome and activates expression of type I interferon and proinflammatory cytokine genes via a MyD88-mediated signaling pathway. Endosomal TLR3 detects RSV dsRNA, an RSV replication intermediate, and then induces production of type I interferon or proinflammatory cytokines in a TRIF-dependent signaling pathway. Abbreviations: TLR, Toll-like receptor; MyD88, myeloid differentiation primary response 88; TRIF, TIR-domain-containing adaptor-inducing interferon-beta; IRF, interferon regulatory factor; NF-κB, nuclear factor-κB.
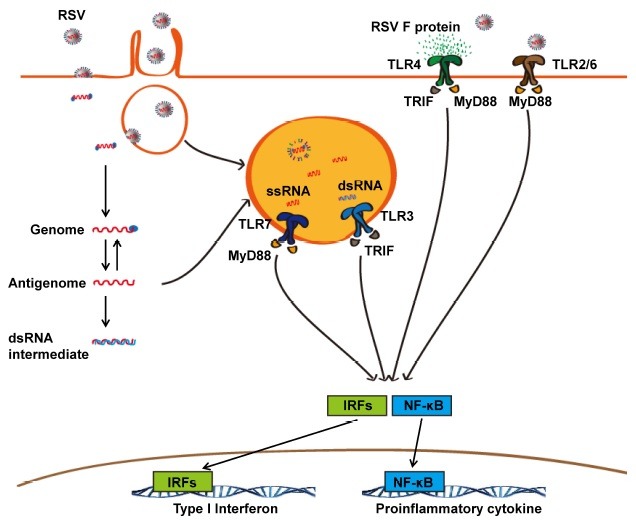
TLR4
Because TLR4 was the first known RSV sensor among the PRRs, it has been studied extensively. TLR4 recognizes gram negative lipopolysaccharide (LPS) on the cell surface. TLR4-mediated signals are transmitted through TRIF- or MyD88-mediated pathways (Fig. 1). Kurt-Jones et al. showed in vitro that the RSV fusion protein was recognized by TLR4 and CD14 as a co-receptor and produced proinflammatory cytokine IL-6. Furthermore, RSV infected TLR4-deficient mice (C57BL10/ ScCr) showed prolonged viral clearance in the lung (20). RSV infected TLR4-deficient mice (C57BL10/ScNCr) showed diminished NK cell and CD14+ cell recruitment, impaired cytotoxic NK cell function, decreased inflammatory cytokine expression, and delayed viral clearance (21). In another functional TLR4-deficient mice (C3H/HeJ), the RSV-inducible early NF-κB response was dependent on TLR4 expression in lung (22). However, Ehl et al. have shown that the absence of TLR4 (C57BL10/ScN and BALB/c lps) had no impact on NK cell recruitment or the activity and recruitment of other pulmonary inflammatory cells. In addition, TLR4 deficiency did not affect viral clearance or RSV-specific T cell responses (23).
Others have reported that RSV infection induces the upregulated expression and membrane localization of TLR4 in airway epithelial cells (24). In infants with RSV bronchiolitis, TLR4 expression is upregulated in blood monocytes, and the degree of TLR4 expression has been correlated with disease severity (25). However, a biological role for TLR4 in RSV-specific immunity remains a question. Direct interaction between intact RSV particles, not including the RSV F protein, and the human TLR4 receptor complex were not found to play an important role in RSV pathogenesis in vitro. In the hTLR4 cell line model, the TLR4 complex played no role in RSV-induced NF-κB activation, viral entry, or replication (26).
Many studies of TLR4 polymorphisms have been conducted compared to other PRRs. Indeed, TLR4 mutations (Asp299Gly and Thr399Ile) have been associated with severe RSV bronchiolitis (27). Both single nucleotide polymorphisms (SNPs) encoding Asp299Gly and Thr399Ile substitutions in the TLR4 polymorphism were highly associated with symptomatic RSV disease in premature infants (28). Others found that the TLR4 amino acid variant (Asp259Gly) is marginally associated with RSV infection (29). However, Paulus et al. showed that the Asp299Gly TLR4 polymorphism does not affect receptor function and does not induce severe RSV infection (30). Despite that great effort has been made to define how TLR4 contributes to RSV infection, the biological role of TLR4 in RSV immunity remains controversial.
TLR3
On endosomal compartments, TLR3 recognizes double-stranded RNA (dsRNA) or polyinosine-polycytidylic acid (poly IC), a synthetic analog of dsRNA. It also induces an innate immune response through the TRIF-mediated pathway. Although RSV belongs to the ssRNA virus genetically, it can generate dsRNA intermediates during replication in the cytoplasm. The dsRNA replication intermediates are taken up by the endosome, allowing TLR3 to sense the RSV virus.
Generally, RSV initiates a more severe disease course than human metapneumovirus (hMPV), another common cause of respiratory infection in children. Dou et al. showed that severe clinical RSV syndrome was caused by TLR3 activation and production of TNF-α in vitro and in mouse lung (31). TLR3 expression was also upregulated in RSV-infected airway epithelial and lung fibroblast cells (32,33). Moreover, lung cells from RSV-infected BALB/c mice had both upregulated TLR3 expression and NF-κB activation (34). In airway epithelial cells with down-regulated TLR3 through small interfering RNA (siRNA), lesser amounts of chemokines, such as CXCL10 and CCL-5, were produced compared to RSV-infected mock cells (32). However, in these cell lines, RSV infection and replication was not affected by TLR3. Others have shown that siRNA-mediated TLR3 knockdown inhibited IFN-β, IFN-inducible protein 10 (IP-10), CCL5, and IFN-stimulated gene 15 (ISG15) expression and significantly reduced NF-κB/ RelA transcription (17). NF-κB is known to be a nuclear phosphoprotein with activating sites at serine residues 276 and 536 (35-38). Liu et al. have suggested that activation of the TLR3 pathway in airway epithelial cells controls the phosphorylation of RelA at serine 276 (17).
An interaction between the TLR3 signaling pathway and the production of type I IFN is possible. One study has shown that RSV affected type I IFN production through poly IC stimulation in HEK293 cells (39). The authors suggested that RSV G protein or soluble G proteins inhibited TLR3/4-mediated type I IFN production by blocking the TRIF/TICAM-1 pathway.
Viral clearance was not affected, but Th2 biased immune responses, including goblet hyperplasia, eosinophil infiltration, and increased IL-5 and IL-13 production of T cells, occurred in TLR3 deficient mice (40). Taken together, it appears that TLR3 partially contributes to both the innate and adaptive immune responses against RSV infection. However, TLR3 is likely not required for viral clearance. TLR3 may play a supplementary role in pathogen sensing and the initiation of the immune response.
TLR7
RSV, which contains ssRNA as a genome, enters the cytoplasm through membrane fusion. The ssRNA genome is transferred to the endosome, where it can be detected by TLR7 on the endosomal compartment. In addition, virions engulfed by endocytosis can also be recognized by TLR7 on the endosomal compartment. RSV-activated TLR7 transmits signals via the MyD88 mediated pathway.
Marozin et al. have shown that RSV has the capacity to shut down type I IFN production in TLR7/9 agonist stimulated human plasmacytoid dendritic cells (pDCs) (41). This paper suggested an interaction between RSV and the TLR7/9 signaling pathway in pDCs. In a pneumonia virus of mice (PVM) infected mouse model, which mimics RSV infection, the TLR7-MyD88 mediated pathway was required for the CD8+ T cell response as well as the induction of type I IFN and proinflammatory cytokines in pDCs (42). In addition, upregulated TLR7 expression was observed in splenocytes from hyper-eosinophilic mice (43). This study demonstrated that eosinophils can contribute to innate antiviral immunity and promote virus clearance against RSV in vivo through the TLR7-MyD88 mediated pathway. Moreover, lung cells from RSV-infected BALB/c mice exhibit upregulated TLR7 expression and subsequent activation of NF-κB (34).
A more pathologic RSV infection has been observed in TLR7 deficient mice, including mucus production, goblet cell hyperplasia, and pulmonary inflammation. TLR7 deficient bone marrow derived DCs (BM-DC) preferentially produced Th17 promoting cytokines, but decreased Th1 promoting cytokines. After restimulating lung cells obtained from RSV-infected TLR7 deficient mice with RSV, a significant increase in the Th17 cytokine IL-17A production was observed, as well as elevation of Th2 cytokines IL-4 and IL-13 (44). However, IRF-1 expression was not affected by TLR7 deficiency. Considering the RSV life cycle, TLR7 likely plays a crucial role in RSV detection and subsequent innate immune initiation. Further study is necessary to determine whether the TLR7-MyD88 mediated pathway is required for type I IFN induction during RSV infection.
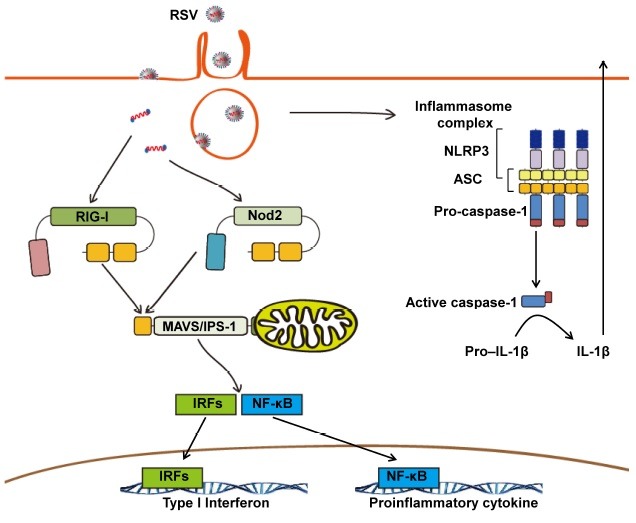
RIG-I and MAVS (IPS-1)
RLRs, which consist of melanoma differentiation-associated protein 5 (MDA5), retinoic acid-inducible gene-I (RIG-I) and laboratory of genetics and physiology 2 (LGP2), are a type of intracellular pattern recognition receptor. The RLRs, including RIG-I and MDA5, bind viral dsRNA or 5’-triphosphorylated uncapped viral RNA in the cytosol (45-47). In particular, RIG-I recognizes ssRNA viral genomes bearing 5’-triphosphates (48). Viral RNA can be detected by RIG-I or MDA5, which activate the downstream NF-κB and IRF3 pathways by interacting with the mitochondrial antiviral-signaling protein (MAVS; IFN-β promoter stimulator 1 (IPS-1)) adaptor molecules (Fig. 2). In theory, the RSV genome consists of ssRNA, and RSV replicates in the cytoplasm. Therefore, RIG-I has the advantage of detecting actively replicating RSV.
Fig. 2. Role of intra-cytoplasmic pattern recognition receptors during RSV infection. Activated RIG-I, which forms a panhandle structure with the ssRNA RSV genome, interacts with the adaptor MAVS, and then enhances expression of type I interferon and proinflammatory cytokine genes. Intracellular Nod2 recognizes the ssRNA genome and induces production of type I interferon or proinflammatory cytokines in a MAVS-dependent signaling pathway. In the activated inflammasome complex, active caspase-1 enhances IL-1β production. Abbreviations: Nod2, nucleotide-binding oligomerization domain containing 2; RIG-I, retinoic acid-inducible gene I; MAVS, mitochondrial antiviral signaling protein; NLRP3, nucleotide-binding domain and leucine-rich-repeat-containing (NLR) family, pyrin domain-containing 3; ASC, apoptosis-associated speck-like protein containing a CARD; IRF, interferon regulatory factor; NF-κB, nuclear factor-κB.
In a mouse fibroblast model, RIG-I was essential for initiating innate immune defenses against RSV, but MDA5 was not (49). Liu et al. have shown that RSV induced IFN-β, IP-10, CCL5, and ISG15 expression levels were decreased in a RIG-I-silenced airway epithelial cell line very early in the infection (17). In nasal pharyngeal washes from infants with RSV associated bronchiolitis, gene expression levels for MDA-5, RIG-I, TLR-7, and TLR-8 were relatively higher in infants with RSV infection. However, there was a significant positive correlation only between RSV viral load and RIG-I mRNA levels (50). In blood mononuclear cells from neonates, young children, and adults, human pDCs from healthy adult donors produced IFN-α in RSV infection through a RIG-I dependent pathway. However, those from young and premature infants did not produce IFN-α in a RIG-I dependent manner (51).
The other paper mentioned that MAVS was required for RSV-induced type I IFN and proinflammatory lung cytokine responses in vivo as well as in lung fibroblasts, bone marrow derived macrophages (BM-DM) and BM-DCs in vitro (52). However, RSV viral clearance and CD8+ T cell responses were not affected in MAVS deficient mice during RSV infection. Interestingly, in IPS-1 deficient mouse lungs, RSV infection reduced inflammatory resolution, prolonged viral clearance, and increased the activation of T cells with a predominant Th1 profile (53). However, in bone marrow chimera experiments that restored IPS-1 signaling, viral clearance and lung pathology were rescued in the nonimmune and immune compartments.
We previously mentioned that RIG-I and the MAVS complex activate the downstream NF-κB and IRF3 pathways. NF-κB is controlled either by a canonical pathway, which releases sequestered RelA complexes from the IκBα inhibitor, and by a noncanonical pathway, which releases RelB from the 100-kDa NF-κB2 complex (54-57). However, RelA activation in response to RSV infection was induced, in part, by a cross-talk pathway involving the noncanonical NIK-IKKα complex downstream of RIG-I and the MAVS adaptor (58). Other study showed that RelA activation was mediated by RelA Ser-276 phosphorylation and cytoplasmic mitogen- and stress-related kinase-1 (MSK1) activation (59). In addition, when RSV is sensed by RIG-I, it triggers a signaling cascade involving the MAVS and TRAF6 adaptors ultimately leading to p65 phosphorylation at Ser536 by IKKβ kinase (60). Thus, RSV mediated NF-κB p65 phosphorylation at Ser536 is dependent on RIG-I, TRAF6 and IKKβ. Collectively, it appears that the RIG-I and MAVS pathway plays a crucial role in activating the innate immune response. However, further study is necessary to understand the function of RIG-I and MAVS in RSV infection.
Nod2
As a cytoplasmic viral sensor, nucleotide-binding oligomerization domain 2 (Nod2) can detect the ssRNA genome and trigger innate immune activation by binding with the adaptor MAVS. Nod2 was shown to be required for IRF3 activation and IFN-β production in RSV infection in vitro (61). Moreover, nod2-deficient mice failed to produce adequate type I IFN, induce viral clearance, and resolve pathology against RSV infection in vivo.
Another paper focused on muramyl dipeptide (MDP), which is a peptidoglycan constituent of both gram positive and negative bacteria that is recognized by Nod2 (62). Vissers et al. insists that IFN-β induction by RSV RNA is an essential first step in the augmented nod2-mediated proinflammatory response to MDP (63). This means that a synergistic response to stimulation with RSV and MDP was observed, which was dependent on a Nod2 mediated pathway. The function of Nod2 during RSV infection has not yet been fully elucidated. Thus, further research is warranted to assess the role of Nod2 in the immune response against RSV infection.
Inflammasome
The inflammasome is a multiple protein complex, including NLRs, their adaptor proteins and pro-caspase-1. The complex stimulates caspase-1 activation to promote the processing and secretion of proinflammatory cytokines IL-1β and IL-18 as well induce cell death. Some research has shown that influenza virus can induce the activation of the inflammasome (64). Others have reported that RSV infection an also activate the inflammasome (65-67).
In human alveolar epithelial cells, live RSV activated the IL-1β-converting enzyme (caspase-1) gene and led to subsequent protein production, possibly implicating the inflammasome in the response to RSV infection (65). Segovia et al. showed that NLRP3/ASC inflammasome activation was crucial for IL-1β production during RSV infection (67). Their studies emphasized the requirement of reactive oxygen species (ROS)/potassium efflux (second signal) as well as the TLR2/MyD88/NF-κB pathway (first signal) for NLRP3/ASC inflammasome formation. This leads to caspase-1 activation and subsequent IL-1β secretion during RSV infection in BM-DMs.
Another group showed that the small hydrophobic (SH) RSV viroporin localized within lipid rafts in the Golgi induced permeability by disrupting membrane architecture and forming ion channels. It then triggered NLRP3 trafficking from the cytoplasm to the Golgi in primary human lung epithelial cells. This SH RSV viroporin was used as viral recognition pathway to signal inflammasome activation (66). Thus, it appears that the inflammasome plays an important role in viral recognition and the initiation of antiviral responses during RSV infection. However, the precise function of the inflammasome in RSV infection is not yet known, and the mechanism of NLRP3 activation also remains unclear.
CONCLUSION
Over the past several decades, RSV vaccine development studies have advanced. Despite these efforts, there is currently no licensed vaccine against RSV infection besides palivizumab. Recent studies have demonstrated that various PRRs, including extracellular TLRs, endosomal TLRs, RLRs, NLRs and the inflammasome recognize RSV infection and induce immune activation through several pathways. However, limited information is available regarding the role of PRRs in RSV infection. Because cell types express different PRR subtypes, antiviral responses against RSV infection can vary by PRR or cell type. To better understand these processes, it will be necessary to determine which PRRs predominate the antiviral immune response against RSV infection. The interaction between PRRs and RSV likely represents the first step in the immune response leading to viral clearance. Therefore, studies investigating the PRR-mediated antiviral response to RSV will be important for aiding vaccine and therapeutic agent development.
Acknowledgments
This work was supported by the National Research Foundation (NRF-2013R1A1A2063347, NRF-2012R1A1A2046001, NRF-2012M3A9B4028274) and the Converging Research Center Program (2011K000864) funded by the Ministry of Science, ICT and Future Planning of Korea.
References
- 1.Blount R. E., Jr., Morris J. A., Savage R. E. Recovery of cytopathogenic agent from chimpanzees with coryza. Proc. Soc. Exp. Biol. Med. (1956);92:544–549. doi: 10.3181/00379727-92-22538. [DOI] [PubMed] [Google Scholar]
- 2.Chanock R., Roizman B., Myers R. Recovery from infants with respiratory illness of a virus related to chimpanzee coryza agent (CCA). I. Isolation, properties and characterization. Am. J. Hyg. (1957);66:281–290. doi: 10.1093/oxfordjournals.aje.a119901. [DOI] [PubMed] [Google Scholar]
- 3.Chanock R., Finberg L. Recovery from infants with respiratory illness of a virus related to chimpanzee coryza agent (CCA). II. Epidemiologic aspects of infection in infants and young children. Am. J. Hyg. (1957);66:291–300. doi: 10.1093/oxfordjournals.aje.a119902. [DOI] [PubMed] [Google Scholar]
- 4.Collins P. L., Graham B. S. Viral and host factors in human respiratory syncytial virus pathogenesis. J. Virol. (2008);82:2040–2055. doi: 10.1128/JVI.01625-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walsh E. E., Hall C. B., Briselli M., Brandriss M. W., Schlesinger J. J. Immunization with glycoprotein subunits of respiratory syncytial virus to protect cotton rats against viral infection. J. Infect. Dis. (1987);155:1198–1204. doi: 10.1093/infdis/155.6.1198. [DOI] [PubMed] [Google Scholar]
- 6.Connors M., Collins P. L., Firestone C. Y., Murphy B. R. Respiratory syncytial virus (RSV) F, G, M2 (22K), and N proteins each induce resistance to RSV challenge, but resistance induced by M2 and N proteins is relatively short-lived. J. Virol. (1991);65:1634–1637. doi: 10.1128/jvi.65.3.1634-1637.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lo M. S., Brazas R. M., Holtzman M. J. Respiratory syncytial virus nonstructural proteins NS1 and NS2 mediate inhibition of Stat2 expression and alpha/beta interferon responsiveness. J. Virol. (2005);79:9315–9319. doi: 10.1128/JVI.79.14.9315-9319.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Conzelmann K. K. Transcriptional activation of alpha/beta interferon genes: interference by nonsegmented negative-strand RNA viruses. J. Virol. (2005);79:5241–5248. doi: 10.1128/JVI.79.9.5241-5248.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramaswamy M., Shi L., Monick M. M., Hunninghake G. W., Look D. C. Specific inhibition of type I interferon signal transduction by respiratory syncytial virus. Am. J. Respir. Cell. Mol. Biol. (2004);30:893–900. doi: 10.1165/rcmb.2003-0410OC. [DOI] [PubMed] [Google Scholar]
- 10.Fulginiti V. A., Eller J. J., Sieber O. F., Joyner J. W., Minamitani M., Meiklejohn G. Respiratory virus immunization. I. A field trial of two inactivated respiratory virus vaccines; an aqueous trivalent parainfluenza virus vaccine and an alum-precipitated respiratory syncytial virus vaccine. Am. J. Epidemiol. (1969);89:435–448. doi: 10.1093/oxfordjournals.aje.a120956. [DOI] [PubMed] [Google Scholar]
- 11.Crowe J. E., Jr. Respiratory syncytial virus vaccine development. Vaccine. (2001);20(Suppl 1):S32–37. doi: 10.1016/S0264-410X(01)00287-0. [DOI] [PubMed] [Google Scholar]
- 12.Chang J. Current progress on development of respiratory syncytial virus vaccine. BMB Rep. (2011);44:232–237. doi: 10.5483/BMBRep.2011.44.4.232. [DOI] [PubMed] [Google Scholar]
- 13.Haynes L. M. Progress and challenges in RSV prophylaxis and vaccine development. J. Infect. Dis. (2013);208(Suppl 3):S177–183. doi: 10.1093/infdis/jit512. [DOI] [PubMed] [Google Scholar]
- 14.Ventre K., Randolph A. G. Ribavirin for respiratory syncytial virus infection of the lower respiratory tract in infants and young children. Cochrane Database Syst. Rev. (2007):Cd000181. doi: 10.1002/14651858.CD000181.pub3. [DOI] [PubMed] [Google Scholar]
- 15.Kumar H., Kawai T., Akira S. Pathogen recognition by the innate immune system. Int. Rev. Immunol. (2011);30:16–34. doi: 10.3109/08830185.2010.529976. [DOI] [PubMed] [Google Scholar]
- 16.Arnold R., Konig W. Peroxisome proliferator-activated receptor-gamma agonists inhibit the replication of respiratory syncytial virus (RSV) in human lung epithelial cells. Virology. (2006);350:335–346. doi: 10.1016/j.virol.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 17.Liu P., Jamaluddin M., Li K., Garofalo R. P., Casola A., Brasier A. R. Retinoic Acid-Inducible Gene I Mediates Early Antiviral Response and Toll-Like Receptor 3 Expression in Respiratory Syncytial Virus-Infected Airway Epithelial Cells. J. Virol. (2007);81:1401–1411. doi: 10.1128/JVI.01740-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Inoue Y., Shimojo N., Arima T., Kohno Y. Toll-Like Receptor 2 as a Functional Receptor to Respiratory Syncytial Virus. J. Allergy Clin. Immunol. (2006);117:S210. doi: 10.1016/j.jaci.2005.12.828. [DOI] [Google Scholar]
- 19.Murawski M. R., Bowen G. N., Cerny A. M., Anderson L. J., Haynes L. M., Tripp R. A., Kurt-Jones E. A., Finberg R. W. Respiratory syncytial virus activates innate immunity through Toll-like receptor 2. J. Virol. (2009);83:1492–1500. doi: 10.1128/JVI.00671-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurt-Jones E. A., Popova L., Kwinn L., Haynes L. M., Jones L. P., Tripp R. A., Walsh E. E., Freeman M. W., Golenbock D. T., Anderson L. J., Finberg R. W. Pattern recognition receptors TLR4 and CD14 mediate response to respiratory syncytial virus. Nat. Immunol. (2000);1:398–401. doi: 10.1038/80833. [DOI] [PubMed] [Google Scholar]
- 21.Haynes L. M., Moore D. D., Kurt-Jones E. A., Finberg R. W., Anderson L. J., Tripp R. A. Involvement of toll-like receptor 4 in innate immunity to respiratory syncytial virus. J. Virol. (2001);75:10730–10737. doi: 10.1128/JVI.75.22.10730-10737.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haeberle H. A., Takizawa R., Casola A., Brasier A. R., Dieterich H., van Rooijen N., Gatalica Z., Garofalo R. P. Respiratory Syncytial Virus-Induced Activation of Nuclear Factor-κB in the Lung Involves Alveolar Macrophages and Toll-Like Receptor 4-Dependent Pathways. J. Infect. Dis. (2002);186:1199–1206. doi: 10.1086/344644. [DOI] [PubMed] [Google Scholar]
- 23.Ehl S., Bischoff R., Ostler T., Vallbracht S., Schulte-Mönting J., Poltorak A., Freudenberg M. The role of Toll-like receptor 4 versus interleukin-12 in immunity to respiratory syncytial virus. Eur. J. Immunol. (2004);34:1146–1153. doi: 10.1002/eji.200324449. [DOI] [PubMed] [Google Scholar]
- 24.Monick M. M., Yarovinsky T. O., Powers L. S., Butler N. S., Carter A. B., Gudmundsson G., Hunninghake G. W. Respiratory Syncytial Virus Up-regulates TLR4 and Sensitizes Airway Epithelial Cells to Endotoxin. J. Biol. Chem. (2003);278:53035–53044. doi: 10.1074/jbc.M308093200. [DOI] [PubMed] [Google Scholar]
- 25.Gagro A., Tominac M., KrŠUloviĆ-HreŠIĆ V., BaĆE A., MatiĆ M., DraŽEnoviĆ V., MlinariĆ-GalinoviĆ G., Kosor E., Gotovac K., BolanČA I., Batinica S., RabatiĆ S. Increased Toll-like receptor 4 expression in infants with respiratory syncytial virus bronchiolitis. Clin. Exp. Immunol. (2004);135:267–272. doi: 10.1111/j.1365-2249.2004.02364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marr N., Turvey S. E. Role of human TLR4 in respiratory syncytial virus-induced NF-κB activation, viral entry and replication. Innate. Immun. (2012);18:856–865. doi: 10.1177/1753425912444479. [DOI] [PubMed] [Google Scholar]
- 27.Tal G., Mandelberg A., Dalal I., Cesar K., Somekh E., Tal A., Oron A., Itskovich S., Ballin A., Houri S., Beigelman A., Lider O., Rechavi G., Amariglio N. Association between common Toll-like receptor 4 mutations and severe respiratory syncytial virus disease. J. Infect. Dis. (2004);189:2057–2063. doi: 10.1086/420830. [DOI] [PubMed] [Google Scholar]
- 28.Awomoyi A. A., Rallabhandi P., Pollin T. I., Lorenz E., Sztein M. B., Boukhvalova M. S., Hemming V. G., Blanco J. C., Vogel S. N. Association of TLR4 polymorphisms with symptomatic respiratory syncytial virus infection in high-risk infants and young children. J. Immunol. (2007);179:3171–3177. doi: 10.4049/jimmunol.179.5.3171. [DOI] [PubMed] [Google Scholar]
- 29.Puthothu B., Forster J., Heinzmann A., Krueger M. TLR-4 and CD14 polymorphisms in respiratory syncytial virus associated disease. Dis. Markers. (2006);22:303–308. doi: 10.1155/2006/865890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paulus S. C., Hirschfeld A. F., Victor R. E., Brunstein J., Thomas E., Turvey S. E. Common human Toll-like receptor 4 polymorphisms-Role in susceptibility to respiratory syncytial virus infection and functional immunological relevance. Clin. Immunol. (2007);123:252–257. doi: 10.1016/j.clim.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 31.Dou Y., Zhao Y., Zhang Z. Y., Mao H. W., Tu W. W., Zhao X. D. Respiratory syncytial virus infection induces higher Toll-like receptor-3 expression and TNF-alpha production than human metapneumovirus infection. PLoS One. (2013);8:e73488. doi: 10.1371/journal.pone.0073488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rudd B. D., Burstein E., Duckett C. S., Li X., Lukacs N. W. Differential Role for TLR3 in Respiratory Syncytial Virus-Induced Chemokine Expression. J. Virol. (2005);79:3350–3357. doi: 10.1128/JVI.79.6.3350-3357.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Groskreutz D. J., Monick M. M., Powers L. S., Yarovinsky T. O., Look D. C., Hunninghake G. W. Respiratory Syncytial Virus Induces TLR3 Protein and Protein Kinase R, Leading to Increased Double-Stranded RNA Responsiveness in Airway Epithelial Cells. J. Immunol. (2006);176:1733–1740. doi: 10.4049/jimmunol.176.3.1733. [DOI] [PubMed] [Google Scholar]
- 34.Huang S., Wei W., Yun Y. Upregulation of TLR7 and TLR3 gene expression in the lung of respiratory syncytial virus infected mice. Wei Sheng Wu Xue Bao. (2009);49:239–245. [PubMed] [Google Scholar]
- 35.Chen L. F., Williams S. A., Mu Y., Nakano H., Duerr J. M., Buckbinder L., Greene W. C. NF-kappaB RelA phosphorylation regulates RelA acetylation. Mol. Cell. Biol. (2005);25:7966–7975. doi: 10.1128/MCB.25.18.7966-7975.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sasaki C. Y., Barberi T. J., Ghosh P., Longo D. L. Phosphorylation of RelA/p65 on serine 536 defines an I{kappa}B{alpha}-independent NF-{kappa}B pathway. J. Biol. Chem. (2005);280:34538–34547. doi: 10.1074/jbc.M504943200. [DOI] [PubMed] [Google Scholar]
- 37.Vermeulen L., De Wilde G., Van Damme P., Vanden Berghe W., Haegeman G. Transcriptional activation of the NF-kappaB p65 subunit by mitogen- and stress-activated protein kinase-1 (MSK1). EMBO J. (2003);22:1313–1324. doi: 10.1093/emboj/cdg139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhong H., Voll R. E., Ghosh S. Phosphorylation of NF-kappa B p65 by PKA stimulates transcriptional activity by promoting a novel bivalent interaction with the coactivator CBP/p300. Mol. Cell. (1998);1:661–671. doi: 10.1016/S1097-2765(00)80066-0. [DOI] [PubMed] [Google Scholar]
- 39.Shingai M., Azuma M., Ebihara T., Sasai M., Funami K., Ayata M., Ogura H., Tsutsumi H., Matsumoto M., Seya T. Soluble G protein of respiratory syncytial virus inhibits Toll-like receptor 3/4-mediated IFN-beta induction. Int. Immunol. (2008);20:1169–1180. doi: 10.1093/intimm/dxn074. [DOI] [PubMed] [Google Scholar]
- 40.Rudd B. D., Smit J. J., Flavell R. A., Alexopoulou L., Schaller M. A., Gruber A., Berlin A. A., Lukacs N. W. Deletion of TLR3 Alters the Pulmonary Immune Environment and Mucus Production during Respiratory Syncytial Virus Infection. J. Immunol. (2006);176:1937–1942. doi: 10.4049/jimmunol.176.3.1937. [DOI] [PubMed] [Google Scholar]
- 41.Schlender J., Hornung V., Finke S., Günthner-Biller M., Marozin S., Brzózka K., Moghim S., Endres S., Hartmann G., Conzelmann K. Inhibition of Toll-Like Receptor 7- and 9-Mediated Alpha/Beta Interferon Production in Human Plasmacytoid Dendritic Cells by Respiratory Syncytial Virus and Measles Virus. J. Virol. (2005);79:5507–5515. doi: 10.1128/JVI.79.9.5507-5515.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davidson S., Kaiko G., Loh Z., Lalwani A., Zhang V., Spann K., Foo S. Y., Hansbro N., Uematsu S., Akira S., Matthaei K. I., Rosenberg H. F., Foster P. S., Phipps S. Plasmacytoid dendritic cells promote host defense against acute pneumovirus infection via the TLR7-MyD88-dependent signaling pathway. J. Immunol. (2011);186:5938–5948. doi: 10.4049/jimmunol.1002635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Phipps S., Lam C. E., Mahalingam S., Newhouse M., Ramirez R., Rosenberg H. F., Foster P. S., Matthaei K. I. Eosinophils contribute to innate antiviral immunity and promote clearance of respiratory syncytial virus. Blood. (2007);110:1578–1586. doi: 10.1182/blood-2007-01-071340. [DOI] [PubMed] [Google Scholar]
- 44.Lukacs N. W., Smit J. J., Mukherjee S., Morris S. B., Nunez G., Lindell D. M. Respiratory Virus-Induced TLR7 Activation Controls IL-17-Associated Increased Mucus via IL-23 Regulation. J. Immunol. (2010);185:2231–2239. doi: 10.4049/jimmunol.1000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hornung V., Ellegast J., Kim S., Brzozka K., Jung A., Kato H., Poeck H., Akira S., Conzelmann K. K., Schlee M., Endres S., Hartmann G. 5'-Triphosphate RNA is the ligand for RIG-I. Science. (2006);314:994–997. doi: 10.1126/science.1132505. [DOI] [PubMed] [Google Scholar]
- 46.Pichlmair A., Schulz O., Tan C. P., Naslund T. I., Liljestrom P., Weber F., Reis e Sousa C. RIG-I-mediated antiviral responses to single-stranded RNA bearing 5'-phosphates. Science. (2006);314:997–1001. doi: 10.1126/science.1132998. [DOI] [PubMed] [Google Scholar]
- 47.Wu B., Peisley A., Richards C., Yao H., Zeng X., Lin C., Chu F., Walz T., Hur S. Structural basis for dsRNA recognition, filament formation, and antiviral signal activation by MDA5. Cell. (2013);152:276–289. doi: 10.1016/j.cell.2012.11.048. [DOI] [PubMed] [Google Scholar]
- 48.Rehwinkel J., Tan C. P., Goubau D., Schulz O., Pichlmair A., Bier K., Robb N., Vreede F., Barclay W., Fodor E., Reis e Sousa C. RIG-I detects viral genomic RNA during negative-strand RNA virus infection. Cell. (2010);140:397–408. doi: 10.1016/j.cell.2010.01.020. [DOI] [PubMed] [Google Scholar]
- 49.Loo Y. M., Fornek J., Crochet N., Bajwa G., Perwitasari O., Martinez-Sobrido L., Akira S., Gill M. A., Garcia-Sastre A., Katze M. G., Gale M., Jr. Distinct RIG-I and MDA5 signaling by RNA viruses in innate immunity. J. Virol. (2008);82:335–345. doi: 10.1128/JVI.01080-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scagnolari C., Midulla F., Pierangeli A., Moretti C., Bonci E., Berardi R., De Angelis D., Selvaggi C., Di Marco P., Girardi E., Antonelli G. Gene expression of nucleic acid-sensing pattern recognition receptors in children hospitalized for respiratory syncytial virus-associated acute bronchiolitis. Clin. Vaccine Immunol. (2009);16:816–823. doi: 10.1128/CVI.00445-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Marr N., Wang T. I., Kam S. H., Hu Y. S., Sharma A. A., Lam A., Markowski J., Solimano A., Lavoie P. M., Turvey S. E. Attenuation of Respiratory Syncytial Virus-Induced and RIG-I-Dependent Type I IFN Responses in Human Neonates and Very Young Children. J. Immunol. (2014);192:948–957. doi: 10.4049/jimmunol.1302007. [DOI] [PubMed] [Google Scholar]
- 52.Bhoj V. G., Sun Q., Bhoj E. J., Somers C., Chen X., Torres J. P., Mejias A., Gomez A. M., Jafri H., Ramilo O., Chen Z. J. MAVS and MyD88 are essential for innate immunity but not cytotoxic T lymphocyte response against respiratory syncytial virus. Proc. Natl. Acad. Sci. U. S. A. (2008);105:14046–14051. doi: 10.1073/pnas.0804717105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Demoor T., Petersen B. C., Morris S., Mukherjee S., Ptaschinski C., De Almeida Nagata D. E., Kawai T., Ito T., Akira S., Kunkel S. L., Schaller M. A., Lukacs N. W. IPS-1 signaling has a nonredundant role in mediating antiviral responses and the clearance of respiratory syncytial virus. J. Immunol. (2012);189:5942–5953. doi: 10.4049/jimmunol.1201763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zandi E., Karin M. Bridging the gap: composition, regulation, and physiological function of the IkappaB kinase complex. Mol. Cell Biol. (1999);19:4547–4551. doi: 10.1128/mcb.19.7.4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dejardin E., Droin N. M., Delhase M., Haas E., Cao Y., Makris C., Li Z. W., Karin M., Ware C. F., Green D. R. The lymphotoxin-beta receptor induces different patterns of gene expression via two NF-kappaB pathways. Immunity. (2002);17:525–535. doi: 10.1016/S1074-7613(02)00423-5. [DOI] [PubMed] [Google Scholar]
- 56.Xiao G., Fong A., Sun S. C. Induction of p100 processing by NF-kappaB-inducing kinase involves docking IkappaB kinase alpha (IKKalpha) to p100 and IKKalpha-mediated phosphorylation. J. Biol. Chem. (2004);279:30099–30105. doi: 10.1074/jbc.M401428200. [DOI] [PubMed] [Google Scholar]
- 57.Xiao G., Harhaj E. W., Sun S. C. NF-kappaB-inducing kinase regulates the processing of NF-kappaB2 p100. Mol. Cell. (2001);7:401–409. doi: 10.1016/S1097-2765(01)00187-3. [DOI] [PubMed] [Google Scholar]
- 58.Liu P., Li K., Garofalo R. P., Brasier A. R. Respiratory syncytial virus induces RelA release from cytoplasmic 100-kDa NF-kappa B2 complexes via a novel retinoic acid-inducible gene-I{middle dot}NF- kappa B-inducing kinase signaling pathway. J. Biol. Chem. (2008);283:23169–23178. doi: 10.1074/jbc.M802729200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Jamaluddin M., Tian B., Boldogh I., Garofalo R. P., Brasier A. R. Respiratory syncytial virus infection induces a reactive oxygen species-MSK1-phospho-Ser-276 RelA pathway required for cytokine expression. J. Virol. (2009);83:10605–10615. doi: 10.1128/JVI.01090-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yoboua F., Martel A., Duval A., Mukawera E., Grandvaux N. Respiratory syncytial virus-mediated NF-kappa B p65 phosphorylation at serine 536 is dependent on RIG-I, TRAF6, and IKK beta. J. Virol. (2010);84:7267–7277. doi: 10.1128/JVI.00142-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sabbah A., Chang T. H., Harnack R., Frohlich V., Tominaga K., Dube P. H., Xiang Y., Bose S. Activation of innate immune antiviral responses by Nod2. Nat. Immunol. (2009);10:1073–1080. doi: 10.1038/ni.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Inohara N., Ogura Y., Fontalba A., Gutierrez O., Pons F., Crespo J., Fukase K., Inamura S., Kusumoto S., Hashimoto M., Foster S. J., Moran A. P., Fernandez-Luna J. L., Nunez G. Host recognition of bacterial muramyl dipeptide mediated through NOD2. Implications for Crohn's disease. J. Biol. Chem. (2003);278:5509–5512. doi: 10.1074/jbc.C200673200. [DOI] [PubMed] [Google Scholar]
- 63.Vissers M., Remijn T., Oosting M., de Jong D. J., Diavatopoulos D. A., Hermans P. W., Ferwerda G. Respiratory syncytial virus infection augments NOD2 signaling in an IFN-beta-dependent manner in human primary cells. Eur. J. Immunol. (2012);42:2727–2735. doi: 10.1002/eji.201242396. [DOI] [PubMed] [Google Scholar]
- 64.Pang I. K., Iwasaki A. Inflammasomes as mediators of immunity against influenza virus. Trends Immunol. (2011);32:34–41. doi: 10.1016/j.it.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Takeuchi R., Tsutsumi H., Osaki M., Haseyama K., Mizue N., Chiba S. Respiratory syncytial virus infection of human alveolar epithelial cells enhances interferon regulatory factor 1 and interleukin-1beta-converting enzyme gene expression but does not cause apoptosis. J. Virol. (1998);72:4498–4502. doi: 10.1128/jvi.72.5.4498-4502.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Triantafilou K., Kar S., Vakakis E., Kotecha S., Triantafilou M. Human respiratory syncytial virus viroporin SH: a viral recognition pathway used by the host to signal inflammasome activation. Thorax. (2013);68:66–75. doi: 10.1136/thoraxjnl-2012-202182. [DOI] [PubMed] [Google Scholar]
- 67.Segovia J., Sabbah A., Mgbemena V., Tsai S. Y., Chang T. H., Berton M. T., Morris I. R., Allen I. C., Ting J. P., Bose S. TLR2/MyD88/NF-kappaB pathway, reactive oxygen species, potassium efflux activates NLRP3/ASC inflammasome during respiratory syncytial virus infection. PLoS One. (2012);7:e29695. doi: 10.1371/journal.pone.0029695. [DOI] [PMC free article] [PubMed] [Google Scholar]


