Abstract
A growing body of research demonstrates that psychosocial factors play an important role in the development of hypertension. Previous reviews have identified several key factors (i.e., occupational stress) that contribute to the onset of hypertension, however they are now outdated. In this review, we provide an updated synthesis of the literature from 2010 to April 2014. We identified 21 articles for inclusion in the review, of which there were six categories of psychosocial stressors: occupational stress, personality, mental health, housing instability, social support/isolation, and sleep quality. Sixteen of the studies reported an association between the psychosocial stressor and blood pressure. While several findings were consistent with previous literature, new findings regarding mediating and moderating factors underlying the psychosocial-hypertension association help to untangle inconsistences reported in the literature. Moreover, sleep quality is a novel additional factor that should undergo further exploration. Areas for future research based on these findings are discussed.
Keywords: Psychosocial factors, Incident hypertension, Review, Occupational stress, Mental health, Housing instability, Social support, Sleep quality
Introduction
Hypertension (HTN) is the single most important factor driving the high rates of CVD-related mortality and health care expenditures [1]. Recent estimates indicate that approximately 30% of the U.S. population has HTN, which is expected to rise by 7.2% by 2030.[1] While research shows that HTN management is improving,[2] we still lack a comprehensive understanding of the factors that contribute to the disease onset. It is now well-established that the total variability in the etiology of HTN cannot solely be explained by physiological, genetic, and lifestyle factors. A substantial body of evidence supports the role of psychosocial factors (i.e., occupational stress) as primary risk factors for HTN.[3–5] As a result, national HTN guidelines recommend psychosocial intervention as a means to prevent or delay the onset of HTN.[6–8]
While several reviews have addressed the role of psychosocial factors in the development of HTN, they are now outdated.[3–5, 9] Recent advancements in assessment methods as well as the aging U.S. population (adults > 65 years of age) and demographic shift to an increasingly racial/ethnically diverse population may have uncovered new psychosocial factors not captured in previous reviews. Thus, the aim of this review is to provide an updated synthesis of the literature from 2010 to present in order to enhance our understanding of the psychosocial risk factors that contribute to the development of HTN.
Methods
Selection of Studies
To identify manuscripts that met inclusion criteria for this review, we searched the PubMed and OVID Medline databases from 2010 to April 17, 2014 for our concepts. Additional strategies included searching the bibliographies of eligible articles and searching other systematic reviews and meta-analyses for relevant articles. The concepts for psychosocial stress, hypertension, and longitudinal (i.e., prospective cohort, retrospective case-control) study designs were included in the search with several keyword synonyms. We did not impose any limit on language of the publication. However, studies were limited to adults at least 18 years of age. For a full search strategy, see Appendix A.
Studies were eligible for the review if they met the following criteria: 1) there was an assessment of psychosocial stress defined as psychological traits (hostility), psychological states (depression), psychological interaction with the organization of work (job strain), and social networks; 2) the primary outcome was diagnosis of hypertension defined as a binary outcome of incident HTN, sustained elevated blood pressure (BP; defined as clinic systolic BP ≥140 mm Hg or daytime ambulatory systolic BP≥135 mm Hg, and/or clinic diastolic BP ≥90 mm Hg or daytime ambulatory diastolic BP ≥85 mm Hg), participant report of having been told by a physician that they had high BP, or if they were taking an antihypertensive medication; and 3) the study assessed the predictive relationship between the presence of the psychosocial stressor in a healthy population and diagnosis of HTN/elevated BP at follow-up. Articles were excluded if an unspecified “stress” was reported, an acute stressor was induced in a laboratory setting, or the article did not give details of precisely which measurement scale was used to assess the psychosocial stressor. We also excluded studies with cross-sectional designs as we were interested in determining the causal relationships between psychosocial factors and incident HTN.
Results
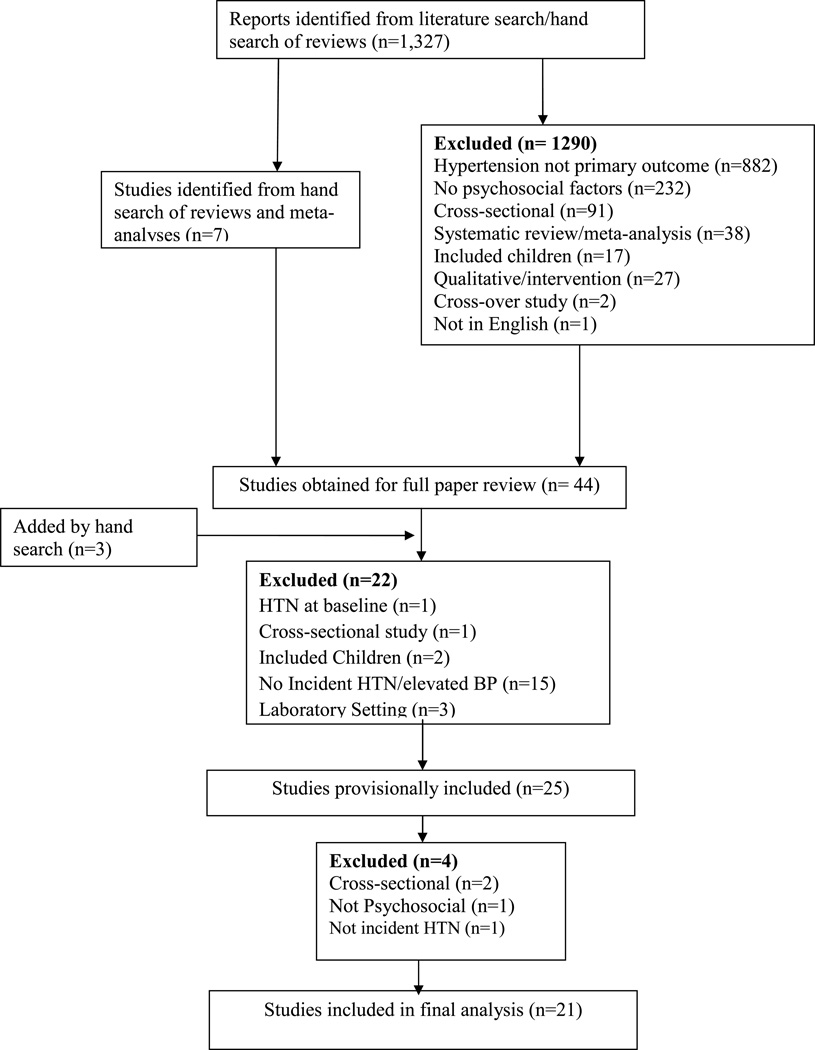
Figure 1 summarizes our literature search results. A total of 1,327 articles were identified, 47 of which were extracted for full review. Twenty-six of these studies were excluded for one of the following reasons: the study was cross-sectional, [10–12] the study was conducted in children,[13, 14] a psychosocial factor was not assessed,[15] incident HTN/sustained elevated BP was not the primary outcome,[16–32] or the stressor was induced in a laboratory setting.[33– 35] Thus, 21 studies were included in this review. The characteristics of the included studies are shown in Table 1. Majority of the included studies were prospective cohort studies [36–54]; three were retrospective case-control studies.[47, 55, 56] Approximately two-thirds of the studies (n=13) were conducted in the United States.[38–41, 43, 46, 47, 50–53, 56] The number of individuals per study ranged from 88 –17,410 (median: 4,156). The duration of follow-up ranged from 2–22 years (median: 6.5 years).
Figure 1.
Review flow chart.
Table 1.
Characteristics of the included trials (N=22)
| Study Reference |
Country | Study Design | Study Duration |
Number of Patients |
Psychological Risk Factor/Assessment Measure |
Hypertension Measure |
Statistical Association |
Outcome |
|---|---|---|---|---|---|---|---|---|
| Occupational Stress | ||||||||
| Landsbergis et al. 2013 | United States | Retrospective Case Control |
6 years | 9224 | Long work hours and Assembly line work/ company data |
ICD-9 codes | Significant | Long work hours associated with increased risk of hypertension |
| Smith et al. 2013 | Canada | Prospective Cohort |
9 years | 6611 | Psychosocial Working Conditions /Job Content Questionnaire (JCQ) and self-reported behaviors |
ICD-9 codes | Significant for job control only |
Elevated risk of hypertension among men with low levels of job control |
| Johansson et al. 2012 | Sweden | Prospective Cohort |
5 years | 88 | Hours Driving a Bus in an Urban Setting/Self Report |
Blood Pressure | Significant | Longer hours spent driving a bus in an urban setting associated with higher diastolic blood pressure |
| Leigh et al. 2012 | United States | Prospective | 2 years | 17,295 | Low wages/ Panel Study of Income Dynamics |
Self-Report | Significant | Low wage was associated with hypertension among women and individuals 25–44 |
| Modrek et al. 2013 | United States | Retrospective | 5 years | 13,000 | Downsizing and Job insecurity/ company data and Bureau of Labor Statistics |
ICD-9 codes | Significant | Individuals working at plants that were downsizing had an increased risk of HTN |
| Wright et al. 2011 | United States | Prospective | 7 years | 1123 | Career as a Law Enforcement Office/ Self- reported |
Blood Pressure | Significant | Occupation as a Law Enforcement Officer predictive of Systolic Blood Pressure |
| Mental Health | ||||||||
| Gangwisch et al. 2010 | United States | Prospective cohort |
10 years | 4913 | Depression/CES-D | Blood Pressure/ Physician or Hospital Diagnosis/Self Report |
Significant | Depression associated with increased risk of developing hypertension |
| Chaudieu et al. 2011 | France | Retrospective | 2 years | 1662 | Lifetime Trauma/ The Watson PTSD Inventory and The Mini-International Neuropsychiatric Interview |
Self Report | Significant | Individuals reporting trauma had higher blood pressure than non-traumatized individuals |
| Ginty et al. 2013 | Netherlands | Prospective Cohort |
5 years | 455 | Depression and Anxiety/Hospital Anxiety and Depression Scale |
Blood Pressure and Self-Report |
Significant | Anxiety and Depression associated with hypertension diagnosis. |
| Delaney et al. 2010 | United States | Prospective | 2 years | 6814 | Depressive Symptoms/CES-D |
Blood Pressure/Antihypertensive Medication Use/Physician Diagnosis |
Not Statistically Significant |
No association was found between depressive symptoms and incident hypertension |
| Hildrum et al. 2011 | United States | Prospective | 22 years | 17,410 | Anxiety and Depression/Hopkins Symptoms Checklist-25 and the Hospital Anxiety and Depression Scale |
Blood Pressure | Significant | Anxiety and depression lowered blood pressure |
| Nabi et al. 2011 | England | Prospective Cohort |
24 year | 10,308 | Depression/ General Health Questionnaire Depression subscale or Prescription of antidepressant medications |
Blood Pressure/ Use of Antihypertensive Medication |
Significant | Risk of hypertension increases with the number of depressive episodes |
| Personality | ||||||||
| Mommersteeg et al. 2011 | Germany | Prospective Cohort |
7 years | 1224 | Type D personality (Negative Affect and Social Inhibition) /DS14 and The Hospital Anxiety and Depression Scale (HADS) |
Blood Pressure/ Hypertension Medication |
Not statistically significant |
No association found between Type D personality and blood pressure |
| Turiano et al. 2011 | United States | Prospective | 10 years | 3990 | Personality Trait Level and Change/The Big Five & Subtracting trait score from first and second wave of study |
Self-Reported | Significant | Higher levels of conscientiousness predicted lower blood pressure, and higher neuroticism predicted higher blood pressure. |
| Housing Instability | ||||||||
| Vijayaraghavan et al. 2012 | United States | Prospective Cohort |
15 years | 5115 | Housing Instability/self- report |
Blood Pressure/ Self-reported Medication |
Significant but only among White Women |
White women with unstable housing had a greater risk of developing hypertension |
| Social Support/Isolation | ||||||||
| Yang et al. 2013 | United States | Prospective Cohort |
14 years | 4323 | Social Integration/Berkman Social Network Index |
Blood Pressure | Significant | High social integration decreased the odds of high blood pressure |
| Croezen et al. 2012 | Netherlands | Prospective Cohort |
10 years | 4724 | Social Support/Social Experiences Checklist |
Blood Pressure | Not Statistically Significant |
Positive and Negative Experiences of social support were not associated with hypertension |
| Hawkley et al. 2010 | United States | Prospective Cohort |
5 years | 229 | Loneliness/ UCLA Loneliness Scale-Revised |
Blood Pressure | Significant | Loneliness associated with higher systolic blood pressure at 2, 3, and 4 years |
| Sleep | ||||||||
| Fung et al. 2013 | United States | Prospective Cohort |
3.4 years | 853 | Total Sleep Time and Sleep Characteristics/Polysomnography |
Blood Pressure/Medications /Self-Report |
Not Statistically Significant |
Total Sleep Time and Secondary sleep predictors not statistically associated with hypertension |
| Fernandez-Mendoza et al. 2012 | United States | Prospective | 7.5 years | 1395 | Insomnia and Short Sleep Duration/polysomnogrpahy, respiration, self-reported measures |
Self Report of taking Blood pressure medication |
Significant only for insomnia |
Chronic insomnia was a risk factor for hypertension. No association between poor sleep and hypertension |
| Fung et al. 2011 | United States | Prospective | 3.4 years | 784 | Slow wave Sleep/Polysomnography |
Self-reported/Blood Pressure |
Significant | Short wave sleep was associated with an increased incidence of hypertension. |
Most commonly, incident HTN was operationalized as BP measurements using standardized procedures (n=13). [36, 37, 39–45, 48, 51–54] Seven studies used a combination of assessments (i.e., BP measurement, ICD codes, patient report of taking an antihypertensive medication)[37–41, 48, 51] while three studies solely used patient self-report of a HTN diagnosis.[46, 50, 55] Six categories of psychosocial stressors were examined across the 21 studies: six studies examined the effects of mental health (i.e., depression, anxiety, PTSD);[37, 41, 42, 44, 54, 55] two examined personality factors;[48, 50] three examined social support/isolation;[36, 43, 53] six examined occupational stress;[45–47, 49, 52, 56] one examined housing instability;[51] and three examined the role of sleep quality.[38–40] The definition of psychosocial stressors within each category varied widely, with only two studies using the same assessment tool (i.e., CES-D to assess depression).[37, 41] Of the 22 included studies, 16 reported statistically significant associations between a psychosocial stressor and BP, although more stress was not always associated with higher hypertension risk.[41–43, 45–47, 49–56] Below we review the included studies and the impact on incident HTN grouped by the psychosocial stressor category.
Occupational Stress
All six of the studies examining the predictive role of occupational stress reported a significant association with incident HTN.[45–47, 49, 52, 56] The studies examined common aspects of occupational stress across diverse work settings including job insecurity, work hours, job quality (job strain, job control) and wages. For example, in one study of urban bus drivers, increases in the average number of hours worked per week was associated with elevated diastolic BP, after controlling for gender and baseline levels of BP.[45] Similarly, in a cohort of automobile manufacturer employees, higher levels of overtime work and job strain were associated with higher rates of incident HTN [56]. Specifically, working ten overtime hours per week was associated with 3.29 more claims for incident HTN per 1,000 employees per year. Moreover, female assembly-line workers experienced significantly higher rates of HTN as compared to female skilled trade workers (Rate Ratio (RR): 1.68) whereas male assembly-line workers were more likely to develop HTN than those working in an operations position (RR: 1.2 95% Confidence Interval [95CI]: 1.0–1.4). Law enforcement officers also experienced higher systolic BP as compared to non-law enforcement officers (i.e., health care workers, educators).[52] Consistent with previous research, Smith et al.[49] documented a stronger association between low job control and risk of incident HTN among men than women (11.8% vs. 1.2%, respectively).[49] However, there was no association between high job strain and incident HTN among men or women.
In examining the health consequences of downsizing, Modrek and Cullen[47] found that higher job insecurity, assessed as the percentage of layoffs at high and low layoff companies, was only associated with incident HTN among hourly workers that survived the layoffs (Odds Ratio [OR]: 1.48, 95CI: 0.97–2.05). Salaried workers and tenured union hourly workers did not experience the adverse consequences of working at a high layoff company.[47] Finally, in a sample of working adults, low annual wages were associated with incident HTN particularly in younger (ages 25–44 years) and female subgroups, independent of educational attainment.[46] Doubling annual wages (100% increase) was associated with a 16% decrease in the chance of HTN in the overall cohort and 25–30% decrease in the odds of reporting HTN in the younger subgroup.[46]
Mental Health
Similar to previous reviews, the association between mental health and incident HTN was inconsistent across the included studies. In the current review, four of the six studies documented an association between mental health and BP.[41, 42, 54, 55] One retrospective study examined the association between history of exposure to traumatic events and frequency of HTN among community-dwelling adults.[55] In this study, participants who reported re-experiencing trauma-related symptoms exhibited significantly higher rates of HTN than participants who reported no symptom reoccurrence (OR: 1.32, 95CI: 0.96,1.82 vs. OR: 0.86, 95CI: 0.68,1.10, respectively).[55]
The five remaining studies examined the role of depression on incident HTN, of which two also assessed anxiety. Depression, assessed by the CES-D, was not associated with risk of incident HTN (assessed with BP measurements) over a two year time period in a multi-ethnic, population-based study in the United States.[37] However, symptoms of depression and anxiety assessed separately at baseline with the Hospital Anxiety and Depression Scale (HADS) was associated with self-reported HTN diagnosis at the five year follow-up among participants from the Dutch Famine Birth Cohort Study (depression OR: 1.18, 95CI: 1.06–1.31; anxiety OR: 1.14, 95CI: 1.03–1.25).[42] Alternatively, when a combined measure of the HADS was assessed over multiple time points, there was a negative association with incident HTN such that higher symptomatology (≥80th percentile) was associated with a reduced odds for sustained elevated BP (BP≥140/90 mm Hg; OR: 0.80, 95CI: 0.70–0.92) and a higher odds for hypotension (BP<120/75 mm Hg; OR: 1.20, 95CI: 1.05–1.36) at the 22 year follow-up.[44]
To help explain these inconsistent findings, two studies examined potential mechanisms that may be driving the association between depression and risk of incident HTN. In a longitudinal analysis of the Whitehall II Cohort Study, participants who were 35–39 years of age and reported an increasing number of depressive episodes over time exhibited a 25% lower risk of HTN as compared to those who reported no or few depressive episodes (OR: 0.75, 95CI: 0.61–0.92).[54] However, for every 5-year increase in age after that time point, the ‘increasing depressive episodes’ group experienced an excess increase of 7% (95CI: 3.0, 12.0) in the odds of developing HTN. This pattern was stronger in men than women.
Using data from the First National Health and Nutrition Examination Survey (NHANES I 1982–1992), Gangwisch et al. [41] examined the mediating effects of sleep duration and insomnia on the depression-HTN association. Similar to the above studies, the researchers found that the results were dependent on the age of the cohort. Specifically, middle-aged subjects (ages: 32–59 years) with depression versus those without depression had a 44% greater risk of being diagnosed with HTN over the 10 year follow-up period (Hazards Ratio (HR): 1.44, 95CI: 1.15–1.80). Moreover, middle-aged subjects who reported sleeping ≤ 5 hours per night were 50% more likely to be diagnosed with HTN than subjects that report 7–8 hours per night (HR: 1.50, 95CI: 1.11–2.02). Finally, each one unit increase in middle-aged subject’s insomnia score was associated with a 5% increase in the odds of being diagnosed with HTN (HR: 1.05, 95CI: 1.01–1.09). There was no association between depression, sleep quality and incident HTN in elderly subjects (ages: 60–86 years).
Personality
Examination of personality factors on risk of incident HTN also yielded mixed results.[48, 50] Type D personality characterized by high levels of negative affectivity and high social inhibition was not associated with elevated systolic and diastolic BP among German airplane manufacturer employees after a 6 year follow-up.[48] However, lower levels of conscientiousness (i.e., characterized by disorganization, irresponsibility, and being undisciplined) and higher levels of neuroticism (i.e., characterized by negative emotions and overreaction to stressors) were associated with self-reported HTN over a 10 year time period within a national sample of Americans.[50]
Housing Instability
Only one study examined the role of housing instability on incident HTN.[51] Housing instability was assessed as the frequency of moving, house crowding, and currently occupying a residence without paying rent or money among young men and women (ages 18–30 years) participating in the CARDIA study. After adjusting for confounding variables, there was no difference in incidence rate of HTN among those in stable housing as compared to unstable house situations in the overall study population (Incidence rate ratio (IRR): 1.1, 95CI: 2.4–9.2).[51] However, there were significant variations by participant race and gender. White women with unstable housing had four times the rate of incident HTN than white women with stable housing (IRR: 4.7, 95CI:2.4–9.2).
Social support/isolation
Three articles assessed the role of social factors on the development of HTN.[36, 43, 53] A high level of social integration, defined as having four to five social ties across five domain of social activities (marital status; contact with parents, children, and neighbors; and volunteer activities) was associated with a 41% decreased odds of developing elevated BP among participants in the Health and Retirement Study.[53] These effects were more pronounced among participants under age 65 years, males, whites, and those of lower-income and educational status. Hawkley et al.[43] examined the role of loneliness, defined as the feelings that accompany the perceived discrepancy between one’s desired and actual social relationships, on repeated measures of systolic BP over a 4-year period among a multi-ethnic sample of middle-aged and older adults (ages: 50–68 years). Results showed a cumulative effect such that higher loneliness scores at baseline were associated with a 3.6mm Hg increase in systolic BP each year of follow-up. This equated to a 14.4 mm Hg greater increase in systolic BP among participants with higher baseline loneliness scores as compare to those with lower scores. Finally, in a study examining social support, the researchers found no association between negative or positive experiences of support and risk of incident HTN over a 10-year period.[36]
Sleep
Three studies of sleep quality, broadly defined as studies including sleep duration, sleep complaints, and sleep disorders were included in this review.[38–40] All of the studies revealed a significant association with incident HTN. In a 2011 study, Fung et al.[40] examined the role of sleep-disordered breathing, sleep duration, and sleep architecture determined by in home polysomnography on incident HTN in older men (age≥65 years). After adjusting for known cardiovascular risk factors and a wide range of sleep variables individuals with poor sleep architecture, men in the lowest percentile of slow wave sleep (SWS), had a 1.8 (95CI: 1.18–2.85) fold increase in incident HTN compared to men with highest SWS. In another investigation with the same cohort of men, Fung et al. [39] found no association between total sleep time, percent sleep (an estimate of sleep efficiency), sleep latency, and wake after sleep onset and incident HTN suggesting that there are particular dimensions of sleep that may not be implicated in the development of HTN. Of note, this study used actigraphy-measured sleep variables.
Individuals with chronic insomnia (complaint of insomnia with a duration of ≥1 year) in combination with objective short sleep duration exhibited a 4-fold increase in incident HTN compared to normal sleepers who slept ≥6 hours (OR: 3.75, 95CI: 1.58–8.95) in a sample of 1,741 community-dwelling men and women.[38] Moreover, individuals who reported poor sleep (moderate-to-severe complaint of difficulty falling asleep, difficulty staying asleep, early final awakening, or non-restorative sleep) and had objective short sleep duration, exhibited nearly two times the odds of developing incident HTN over the 7.5 years of follow-up (OR: 1.80, 95CI: 1.04–3.12). This association became marginally significant after controlling for obesity (OR: 1.62, 95CI: 0.92–2.83). Alternatively, participants that reported chronic insomnia or poor sleep, but who also had objective sleep duration ≥6 hours had no increased risk of HTN. Interestingly, these finding suggest that the objective measures of sleep duration rather than the subjective nature of sleep complaints is of clinical significance.
Conclusions
The objective of this review was to provide a synthesis of the existing literature and an assessment of the psychosocial risk factors that may increase the risk of developing HTN. We reviewed 21 articles published between 2010 and 2014, and identified six categories of psychosocial factors: 1) occupational stress, 2) mental health, 3) personality, 4) housing instability, 5) social support/isolation, and 6) sleep quality. Consistent with previous literature,[57–59] our results indicate that measures of occupational stress such as unemployment, extended work hours, job stability/control, low wages, downsizing, and job strain increased the risk of developing HTN. Low social integration, loneliness, and housing instability were also significantly associated with incident HTN. A recent addition to the psychosocial literature was the examination of poor sleep quality and other sleep-related behaviors. Specifically, we found that sleep duration, sleep architecture, and chronic insomnia were linked to an increased risk of HTN. Studies examining personality-related factors and mental health had mixed findings.
The mixed findings across the personality studies may be partially explained by the methods used to assess participants’ personality traits. For example, the Mommersteeg et al.[48] study examined the role of Type D personality, which is considered a blend of traits that are subsumed under the Big Five Traits (agreeableness, conscientiousness, openness, extraversion and neuroticism)[60] examined by Turiano et al.[50] Thus, it is plausible that the lack of association documented by Mommersteeg et al.[48] could be a byproduct of not accounting for other dimensions of personality that in combination with Type D personality have been linked to negative health outcomes.[61] Future research will need to examine whether Type D personality is predictive of incident HTN when controlling for the remaining five factor traits.
Similar to previous research,[62–64] findings across the studies examining mental health were mixed and often dependent on characteristics of the study design (i.e., duration of follow-up, number of assessments, definition of HTN, source of study sample). For example, the sample sizes and duration of the included studies varied widely ranging from 80 to 17,410 participants over the course of two to 29 years of follow-up. We also found differences in the ages of study participants: one study included participants as young as 19 years old [44] while another enrolled participants up to 97 years old.[41] Additionally, studies applied a variety of methods to assess the psychosocial factors. All of the studies with negative findings assessed anxiety and/or depression only at baseline [37, 44] while studies that reported significant associations took repeated assessments. Similarly, while two of the studies used the CES-D to assess depression,[37, 41] the remaining studies used different scales to measure depression and anxiety (both combined and as separate constructs),[42, 44, 54] limiting the ability to systematically compare findings across studies.
Although there is growing evidence that sleep is associated with HTN, these studies are not without limitations. First, the majority of the existing research has focused on sleep duration, and sleep-disordered breathing, and to a lesser extent, insomnia, as indicated in this review. There is a need to examine a broader range of sleep quality including sleep latency, excessive sleepiness, and subjective sleep complaints, all of which are associated with sympathetic overactivity and inflammation.[6] Second, these studies have limited generalizability, (i.e., they included primarily older men, non-Hispanic whites, and sleep laboratory testing). Indeed, sleep laboratory testing is not recommended for routine evaluation of insomnia unless there is clinical uncertainty.[7] Third, none of the studies utilized 24-hour ambulatory blood pressure measurement, which has important clinical significance. Finally, careful consideration must be given to measurement, as any in depth understanding of adverse health outcomes including HTN, would require researchers to select the best method: actigraphy-measured, polysomnography measured, and perceived sleep complaints, to avoid bias and possible confounding factors.
This review also highlighted several novel approaches for examining psychosocial risk factors for HTN. By examining moderating or mediating variables, several studies were able to identify specific subgroups that are at a higher risk for developing HTN. Such analyses were particularly important when researchers failed to find an overall cohort effect between the psychosocial factor and incident HTN, as in the mental health studies. For example, Vijayaraghavan et al.[51] found that White women with unstable housing experienced the greatest risk for developing HTN as compared to all other races and males. Similarly, Gangwisch et al et al. [41] found that associations between depression and incident HTN were exacerbated in middle-aged men who reported sleeping ≤ 5 hours per night and higher chronic insomnia scores; no associations were found in elderly men. These studies underscore the importance of conducting more sophisticated analyses to provide novel insights into the various ways psychosocial factors may influence risk of HTN. More importantly, such research can be used to develop targeted interventions that can reduce the risk of HTN in these vulnerable groups.
Several limitations of this review warrant mention. First, our study was limited to articles that were published in adults ages 18 and older between 2010 and 2014. While we conducted an extensive search of the literature, it is possible that we did not identify all articles that examined psychosocial risk factors for hypertension. Another limitation is related to our psychosocial factors, as psychosocial stress is broadly defined and can include other factors such as, cultural identity and acculturation and perceived discrimination that we may have missed in our search. Finally, the included studies used a variety of methods for measuring HTN, psychosocial risk factors, and included populations that varied in terms or racial/ethnic makeup, therefore our findings may not be generalizable to all populations.
Implications
The current review highlights gaps in the existing literature and potential areas for examination in future studies. Perhaps the most important and innovative aspect of this review was the addition of sleep quality. The idea that sleep quality could lead to HTN is receiving increasing attention. Sleep quality is related to overall health and well-being and is inextricably linked with many of the traditional psychosocial variables considered in this review. Thus, this review provides a unique opportunity to explore the relationship linking sleep quality to risk of incident hypertension. There is convincing evidence that sleep disturbances are implicated in adverse well-being and health outcomes including hypertension.[65] Although the potential pathways of the sleep-HTN relationship are unknown, the research suggests that it may involve hyperactivity of the sympathetic nervous system, but this causal pathway remains elusive, as sleep quality is likely due to a number of underlying issues including depression, obesity and other chronic conditions. As such, a broader examination into a variety of sleep-related complaints that may increase the risk of HTN is warranted, if not overdue. Recognizing that both conditions are complex and involve a number of pathogeneses, disentangling the relationship would involve large-scale sophisticated epidemiological studies, with objective and subjective measures, and diverse patient cohorts. Of note, the studies in this review consisted of majority non-Hispanic white samples, signaling that diverse study samples are urgently needed, as non-Hispanic blacks have the highest prevalence of HTN.[66] Given what is known, these findings have important implications for public health and point to the need of screening for sleep complaints in the general population but especially among hypertensive, and at-risk populations.
After review of the evidence, it is clear that psychosocial factors play a significant and meaningful role in the development of HTN and our understanding of these factors has grown significantly. However, a number of challenges persist. First, it is critically important to determine the role of moderating and mediating factors that could either disentangle or confound the psychosocial-HTN association since, as demonstrated by several studies in this review, there would be differing results with varied implications. Second, the extent to which these factors contribute to disease progression overtime as well as possible implications in disease management including medication adherence is limited. This would be particularly important in developing innovative behavioral approaches for primary and secondary prevention of HTN. Relatedly, despite being prospective in nature, many studies only assessed psychosocial factors at baseline. However, preliminary evidence from this review suggest that it is more advantageous to assess the cumulative effect of psychosocial factors overtime as this has significant implications for the directionality and significance of the association with HTN. Third, few studies involve community-dwelling adults that include a diverse cohort of gender, age, and race/ethnicity, which is essential to assess variations by demographic characteristics. Few studies have examined whether these factors operate differently in African Americans and Latinos compared to whites, especially in sleep quality. Fourth, psychosocial factors often are present with individuals who will eventually suffer from a number of chronic conditions including hypertension, diabetes, and obesity. Additional research is needed to determine whether individuals will benefit from multi-level behavioral interventions that target psychosocial stressors along with multiple chronic conditions and include individuals, families, and neighborhoods.
Acknowledgments
We would like to acknowledge Ms. Karen Yacobucci for her assistance in developing the search strategy for this review. Preparation of this article was supported in part by the National, Heart, Lung and Blood Institute, National Institutes of Health grants K23 HL098564-01 and K24 HL111315-02. The sponsor had no role in the study design; in the collection, analysis, or interpretation of the findings, in writing the present report, or in the decision to submit the manuscript for publication.
Appendix A. Search Strategies
Pubmed
((((((((((hypertension[MeSH Terms]) OR hypertension[Text Word]) OR blood pressure[Text Word]) OR blood pressure[MeSH Terms]) OR hypertension development[Text Word]) OR prehypertension[Text Word]) OR prehypertension[MeSH Terms])) AND (((((risk factors[MeSH Terms]) OR risk[Text Word]) OR risk[MeSH Terms]) OR prognosis[MeSH Terms]) OR prognosis[Text Word])) AND (((((((((((((((((((((((psychology[MeSH Terms]) OR Affective Symptoms/physiopathology*[MeSH Terms]) OR Anxiety/physiopathology[MeSH Terms]) OR depression[MeSH Terms]) OR depression[Text Word]) OR Depression/diagnosis[MeSH Terms]) OR Depression/epidemiology[MeSH Terms]) OR Depression/physiopathology[MeSH Terms]) OR Depression/psychology*[MeSH Terms]) OR emotions[MeSH Terms]) OR emotions[Text Word]) OR Emotions/physiology*[MeSH Terms]) OR mental disorders[Text Word]) OR mental disorders[MeSH Terms]) OR Mental Disorders/diagnosis[MeSH Terms]) OR Mental Disorders/epidemiology[MeSH Terms]) OR Mental Disorders/etiology*[MeSH Terms]) OR mood[Text Word]) OR psychosocial[Text Word]) OR social support[MeSH Terms]) OR stress[Text Word]) OR Stress, Psychological[MeSH Terms]) OR Stress, Physiological[MeSH Terms])) AND (((((Prospective Studies[MeSH Terms]) OR Cohort Studies[MeSH Terms]) OR Followup Studies[MeSH Terms]) OR Longitudinal Studies[MeSH Terms]) AND Cross Sectional Studies[MeSH Terms])
Ovid Medline
exp Hypertension/ or hypertension.mp. limit 1 to yr="2010 -Current" blood pressure.mp. or exp Blood Pressure/ hypertension development.mp. prehypertension.mp. or exp Prehypertension/ 1 or 3 or 4 or 5 limit 6 to yr="2010 -Current" 6 and 7 exp Risk Factors/ or risk.mp. or exp Risk/ prognosis.mp. or exp Prognosis/ 9 or 10 limit 11 to yr="2010 - Current" 7 and 12 exp Psychology/ exp Affective Symptoms/pp [Physiopathology] exp Anxiety/pp [Physiopathology] exp Depression/ or depression.mp. exp Depression/di, ep, ph, pp [Diagnosis, Epidemiology, Physiology, Physiopathology] emotions.mp. or exp Emotions/ exp Emotions/ph [Physiology] mental disorders.mp. or exp Mental Disorders/ exp Mental Disorders/di, ep, et [Diagnosis, Epidemiology, Etiology] mood.mp. psychosocial.mp. or exp Social Support/ exp Stress, Psychological/ or exp Stress, Physiological/ or stress.mp. 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 limit 26 to yr="2010 -Current" exp Prospective Studies/ exp Cohort Studies/ exp Follow-Up Studies/ exp Longitudinal Studies/ exp Cross-Sectional Studies/ 28 or 29 or 30 or 31 or 32 7 and 12 and 27 and 33 limit 34 to yr="2010 -Current"
Footnotes
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
Antoinette Schoenthaler, Chinwe Ogedegbe, Gbenga Ogedegbe, and Natasha J. Williams declare no conflicts of interest.
References
Papers of particular interest have been highlighted below as:
◦Of importance
- 1.Go AS, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gu Q, et al. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126(17):2105–2114. doi: 10.1161/CIRCULATIONAHA.112.096156. [DOI] [PubMed] [Google Scholar]
- 3.Sparrenberger F, et al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J Hum Hypertens. 2009;23(1):12–19. doi: 10.1038/jhh.2008.74. [DOI] [PubMed] [Google Scholar]
- 4.Spruill TM. Chronic psychosocial stress and hypertension. Curr Hypertens Rep. 2010;12(1):10–16. doi: 10.1007/s11906-009-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steptoe A. Psychosocial factors in the development of hypertension. Ann Med. 2000;32(5):371–375. doi: 10.3109/07853890008995940. [DOI] [PubMed] [Google Scholar]
- 6.Chobanian AV, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 7.The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157(21):2413–2446. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 8.The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V) Arch Intern Med. 1993;153(2):154–183. [PubMed] [Google Scholar]
- 9.Gasperin D, et al. Effect of psychological stress on blood pressure increase: a meta-analysis of cohort studies. Cad Saude Publica. 2009;25(4):715–726. doi: 10.1590/s0102-311x2009000400002. [DOI] [PubMed] [Google Scholar]
- 10.Chouchou F, et al. Sympathetic overactivity due to sleep fragmentation is associated with elevated diurnal systolic blood pressure in healthy elderly subjects: the PROOF-SYNAPSE study. European Heart Journal. 34(28):2122–2131. doi: 10.1093/eurheartj/eht208. 2131a. [DOI] [PubMed] [Google Scholar]
- 11.Fiest KM, et al. Chronic conditions and major depression in community-dwelling older adults. Journal of Affective Disorders. 131(1–3):172–178. doi: 10.1016/j.jad.2010.11.028. [DOI] [PubMed] [Google Scholar]
- 12.Chaix B, et al. Individual/neighborhood social factors and blood pressure in the RECORD Cohort Study: which risk factors explain the associations? Hypertension. 55(3):769–775. doi: 10.1161/HYPERTENSIONAHA.109.143206. [DOI] [PubMed] [Google Scholar]
- 13.Schreier HM, Chen E. Socioeconomic status in one's childhood predicts offspring cardiovascular risk. Brain, Behavior, & Immunity. 24(8):1324–1331. doi: 10.1016/j.bbi.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Kohler S, et al. Temporal evolution of cognitive changes in incident hypertension: prospective cohort study across the adult age span. Hypertension. 63(2):245–251. doi: 10.1161/HYPERTENSIONAHA.113.02096. [DOI] [PubMed] [Google Scholar]
- 15.Lucke JC, et al. Health across generations: findings from the Australian Longitudinal Study on Women's Health. Biological Research for Nursing. 12(2):162–170. doi: 10.1177/1099800410373804. [DOI] [PubMed] [Google Scholar]
- 16.Alastalo H, et al. Cardiovascular morbidity and mortality in Finnish men and women separated temporarily from their parents in childhood--a life course study. Psychosomatic Medicine. 74(6):583–587. doi: 10.1097/PSY.0b013e31825b3d76. [DOI] [PubMed] [Google Scholar]
- 17.D'Antono B, Moskowitz DS, Nigam A. The metabolic costs of hostility in healthy adult men and women: cross-sectional and prospective analyses. J Psychosom Res. 2013;75(3):262–269. doi: 10.1016/j.jpsychores.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Epstein NU, et al. Cognitive dysfunction and greater visit-to-visit systolic blood pressure variability. Journal of the American Geriatrics Society. 61(12):2168–2173. doi: 10.1111/jgs.12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Findley P, Shen C, Sambamoorthi U. Multimorbidity and persistent depression among veterans with diabetes, heart disease, and hypertension. Health & Social Work. 36(2):109–119. doi: 10.1093/hsw/36.2.109. [DOI] [PubMed] [Google Scholar]
- 20.Gao S, et al. Increase in blood pressure precedes clinical depression in elderly primary care patients. International Journal of Geriatric Psychiatry. 28(10):1099–1100. doi: 10.1002/gps.3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Godin O, Elbejjani M, Kaufman JS. Body mass index, blood pressure, and risk of depression in the elderly: a marginal structural model. American Journal of Epidemiology. 176(3):204–213. doi: 10.1093/aje/kws003. [DOI] [PubMed] [Google Scholar]
- 22.Haukkala A, et al. Hostility, anger control, and anger expression as predictors of cardiovascular disease. Psychosomatic Medicine. 72(6):556–562. doi: 10.1097/PSY.0b013e3181dbab87. [DOI] [PubMed] [Google Scholar]
- 23.Joas E, et al. Blood pressure trajectories from midlife to late life in relation to dementia in women followed for 37 years. Hypertension. 59(4):796–801. doi: 10.1161/HYPERTENSIONAHA.111.182204. [DOI] [PubMed] [Google Scholar]
- 24.McEvoy LK, et al. Changes in alcohol intake and their relationship with health status over a 24-year follow-up period in community-dwelling older adults. J Am Geriatr Soc. 2013;61(8):1303–1308. doi: 10.1111/jgs.12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Molander L, Gustafson Y, Lovheim H. Longitudinal associations between blood pressure and dementia in the very old. Dementia & Geriatric Cognitive Disorders. 30(3):269–276. doi: 10.1159/000320252. [DOI] [PubMed] [Google Scholar]
- 26.Peters R, et al. Association of depression with subsequent mortality, cardiovascular morbidity and incident dementia in people aged 80 and over and suffering from hypertension. Data from the Hypertension in the Very Elderly Trial (HYVET) Age & Ageing. 39(4):439–445. doi: 10.1093/ageing/afq042. [DOI] [PubMed] [Google Scholar]
- 27.Steptoe A, et al. Socioeconomic status and subclinical coronary disease in the Whitehall II epidemiological study. PLoS ONE [Electronic Resource] 5(1):e8874. doi: 10.1371/journal.pone.0008874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whisman M, Uebelacker LA. A longitudinal investigation of marital adjustment as a risk factor for metabolic syndrome. Health Psychology. 31(1):80–86. doi: 10.1037/a0025671. [DOI] [PubMed] [Google Scholar]
- 29.Traian MG, et al. Stress: from symptom to disease. Revista Medico-Chirurgicala a Societatii de Medici Si Naturalisti Din Iasi. 117(1):72–77. [PubMed] [Google Scholar]
- 30.Buckley T, et al. Haemodynamic changes during early bereavement: potential contribution to increased cardiovascular risk. Heart, Lung & Circulation. 20(2):91–98. doi: 10.1016/j.hlc.2010.10.073. [DOI] [PubMed] [Google Scholar]
- 31.Tanabe N, et al. Daytime napping and mortality, with a special reference to cardiovascular disease: the JACC study. International Journal of Epidemiology. 39(1):233–243. doi: 10.1093/ije/dyp327. [DOI] [PubMed] [Google Scholar]
- 32.Shah MT, Zonderman AB, Waldstein SR. Sex and age differences in the relation of depressive symptoms with blood pressure. American Journal of Hypertension. 26(12):1413–1420. doi: 10.1093/ajh/hpt135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carroll D, et al. Systolic blood pressure reactions to acute stress are associated with future hypertension status in the Dutch Famine Birth Cohort Study. International Journal of Psychophysiology. 85(2):270–273. doi: 10.1016/j.ijpsycho.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 34.Hamer M, Steptoe A. Cortisol responses to mental stress and incident hypertension in healthy men and women. Journal of Clinical Endocrinology & Metabolism. 97(1):E29–E34. doi: 10.1210/jc.2011-2132. [DOI] [PubMed] [Google Scholar]
- 35.Desideri G, et al. Benefits in cognitive function, blood pressure, and insulin resistance through cocoa flavanol consumption in elderly subjects with mild cognitive impairment: the Cocoa, Cognition, and Aging (CoCoA) study. Hypertension. 60(3):794–801. doi: 10.1161/HYPERTENSIONAHA.112.193060. [DOI] [PubMed] [Google Scholar]
- 36.Croezen S, et al. Do positive or negative experiences of social support relate to current and future health? Results from the Doetinchem Cohort Study. BMC Public Health. 12:65. doi: 10.1186/1471-2458-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Delaney JA, et al. Baseline depressive symptoms are not associated with clinically important levels of incident hypertension during two years of follow-up: the multi-ethnic study of atherosclerosis. Hypertension. 55(2):408–414. doi: 10.1161/HYPERTENSIONAHA.109.139824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernandez-Mendoza J, et al. Insomnia with objective short sleep duration and incident hypertension: the Penn State Cohort. Hypertension. 60(4):929–935. doi: 10.1161/HYPERTENSIONAHA.112.193268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fung MM, et al. Total sleep time and other sleep characteristics measured by actigraphy do not predict incident hypertension in a cohort of community-dwelling older men. Journal of Clinical Sleep Medicine. 9(6):585–591. doi: 10.5664/jcsm.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fung MM, et al. Decreased slow wave sleep increases risk of developing hypertension in elderly men. Hypertension. 58(4):596–603. doi: 10.1161/HYPERTENSIONAHA.111.174409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gangwisch JE, et al. Insomnia and sleep duration as mediators of the relationship between depression and hypertension incidence. American Journal of Hypertension. 23(1):62–69. doi: 10.1038/ajh.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ginty AT, et al. Depression and anxiety are associated with a diagnosis of hypertension 5 years later in a cohort of late middle-aged men and women. Journal of Human Hypertension. 27(3):187–190. doi: 10.1038/jhh.2012.18. [DOI] [PubMed] [Google Scholar]
- 43.Hawkley LC, et al. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132–141. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hildrum B, Romild U, Holmen J. Anxiety and depression lowers blood pressure: 22-year follow-up of the population based HUNT study, Norway. BMC Public Health. 11:601. doi: 10.1186/1471-2458-11-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Johansson G, et al. The effects of urban bus driving on blood pressure and musculoskeletal problems: a quasi-experimental study. Psychosomatic Medicine. 74(1):89–92. doi: 10.1097/PSY.0b013e31823ba88f. [DOI] [PubMed] [Google Scholar]
- 46.Leigh JP, Du J. Are low wages risk factors for hypertension? European Journal of Public Health. 22(6):854–859. doi: 10.1093/eurpub/ckr204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Modrek S, Cullen MR. Health consequences of the 'Great Recession' on the employed: evidence from an industrial cohort in aluminum manufacturing. Social Science & Medicine. 92:105–113. doi: 10.1016/j.socscimed.2013.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mommersteeg PM, et al. Type D personality and metabolic syndrome in a 7-year prospective occupational cohort. J Psychosom Res. 2011;71(5):357–363. doi: 10.1016/j.jpsychores.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 49.Smith PM, et al. Comparing the risk associated with psychosocial work conditions and health behaviours on incident hypertension over a nine-year period in Ontario, Canada. Canadian Journal of Public Health. Revue Canadienne de Sante Publique. 104(1):e82–e86. doi: 10.1007/BF03405661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Turiano NA, et al. Personality trait level and change as predictors of health outcomes: findings from a national study of Americans (MIDUS) Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 67(1):4–12. doi: 10.1093/geronb/gbr072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vijayaraghavan M, et al. Housing instability and incident hypertension in the CARDIA cohort. Journal of Urban Health. 90(3):427–441. doi: 10.1007/s11524-012-9729-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wright BR, Barbosa-Leiker C, Hoekstra T. Law enforcement officer versus non-law enforcement officer status as a longitudinal predictor of traditional and emerging cardiovascular risk factors. Journal of Occupational & Environmental Medicine. 53(7):730–734. doi: 10.1097/JOM.0b013e318220c2da. [DOI] [PubMed] [Google Scholar]
- 53.Yang YC, Li T, Ji Y. Impact of social integration on metabolic functions: evidence from a nationally representative longitudinal study of US older adults. BMC Public Health. 13:1210. doi: 10.1186/1471-2458-13-1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nabi H, et al. Trajectories of depressive episodes and hypertension over 24 years: the Whitehall II prospective cohort study. Hypertension. 2011;57(4):710–716. doi: 10.1161/HYPERTENSIONAHA.110.164061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chaudieu I, et al. Late-life health consequences of exposure to trauma in a general elderly population: the mediating role of reexperiencing posttraumatic symptoms. J Clin Psychiatry. 2011;72(7):929–935. doi: 10.4088/JCP.10m06230. [DOI] [PubMed] [Google Scholar]
- 56.Landsbergis PA, et al. Disability rates for cardiovascular and psychological disorders among autoworkers by job category, facility type, and facility overtime hours. American Journal of Industrial Medicine. 56(7):755–764. doi: 10.1002/ajim.22191. [DOI] [PubMed] [Google Scholar]
- 57.Guimont C, et al. Effects of job strain on blood pressure: a prospective study of male and female white-collar workers. Am J Public Health. 2006;96(8):1436–1443. doi: 10.2105/AJPH.2004.057679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Markovitz JH, et al. Increases in job strain are associated with incident hypertension in the CARDIA Study. Ann Behav Med. 2004;28(1):4–9. doi: 10.1207/s15324796abm2801_2. [DOI] [PubMed] [Google Scholar]
- 59.Ohlin B, et al. Job strain in men, but not in women, predicts a significant rise in blood pressure after 6.5 years of follow-up. J Hypertens. 2007;25(3):525–531. doi: 10.1097/HJH.0b013e32801220fa. [DOI] [PubMed] [Google Scholar]
- 60.Watson D. Toward a comprehensive hierarchical structure. Health Psychology Review. 2012;2011(16):333–345. [Google Scholar]
- 61.Ferguson E, et al. Health specific traits beyond the Five Factor Model, cognitive processes and trait expression: replies to Watson (2012), Matthews (2012) and Haslam, Jetten, Reynolds, and Reicher (2012) Health Psychol Rev. 2013;7(Suppl 1):S85–S103. doi: 10.1080/17437199.2012.701061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paterniti S, et al. Low blood pressure and risk of depression in the elderly. A prospective community-based study. Br J Psychiatry. 2000;176:464–467. doi: 10.1192/bjp.176.5.464. [DOI] [PubMed] [Google Scholar]
- 63.Barrett-Connor E, Palinkas LA. Low blood pressure and depression in older men: a population based study. BMJ. 1994;308(6926):446–449. doi: 10.1136/bmj.308.6926.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Meng L, et al. Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies. J Hypertens. 2012;30(5):842–851. doi: 10.1097/HJH.0b013e32835080b7. [DOI] [PubMed] [Google Scholar]
- 65.Steptoe A, Cropley M. Persistent high job demands and reactivity to mental stress predict future ambulatory blood pressure. J Hypertens. 2000;18(5):581–586. doi: 10.1097/00004872-200018050-00011. [DOI] [PubMed] [Google Scholar]
- 66.Ritz T, et al. Emotions and stress increase respiratory resistance in asthma. Psychosom Med. 2000;62(3):401–412. doi: 10.1097/00006842-200005000-00014. [DOI] [PubMed] [Google Scholar]