Summary
Despite a steady increase in total blood collections and voluntary non-remunerated blood donors, China continues to have many challenges with its blood donation system. The country's donation rate remains low at 9%o, with over 60% of donors being first-time donors. Generally there is a lack of adequate public awareness about blood donation. The conservative donor selection criteria, the relatively long donation interval, and the small donation volume have further limited blood supply. To ensure a sufficient and safe blood supply that meets the increasing clinical need for blood products, there is an urgent need to strengthen the country's blood donor management. This comprehensive effort should include educating and motivating more individuals especially from the rural areas to be involved in blood donation, developing rational and evidence-based selection criteria for donor eligibility, designing a donor follow-up mechanism to encourage more future donations, assessing the current donor testing strategy, improving donor service and care, building regional and national shared donor deferral database, and enhancing the transparency of the blood donation system to gain more trust from the general public. The purpose of the review is to provide an overview of the key process of and challenges with the blood donor management system in China.
Keywords: Blood donors, Blood supply, China
Introduction
According to the National Blood Donation Law, the blood service system in China is led and coordinated by the central and local government. The Ministry of Health and Family Planning (MOHFP), previously the Ministry of Health (MOH), sets national standards and policies while local public health bureaus manage the day-to-day operations and planning for blood donation, mainly through the Blood Donation Office. Blood centers/stations are the only authorized establishments to collect blood and supply blood for civilian clinical use. They also play an important role in mobilizing and recruiting blood donors, in partnership with local Blood Donation Offices. In 2011, there were 452 blood establishments nationwide, including 32 provincial blood centers, 321 regional blood centers/stations, and 99 county blood stations [1].
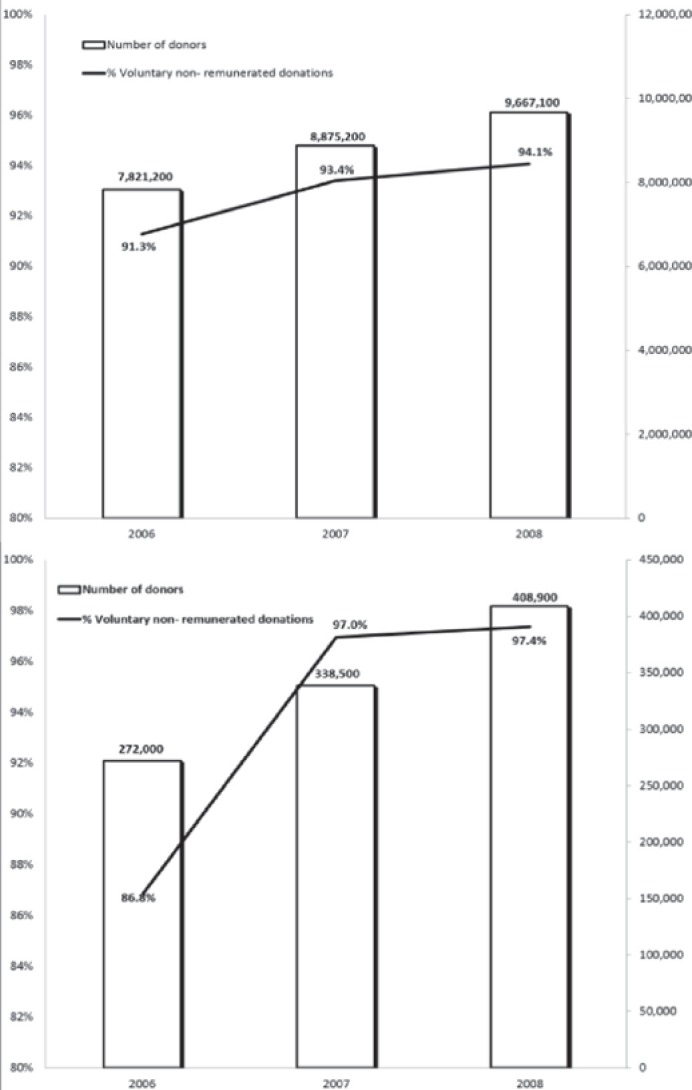
Data from a national survey among 355 blood centers/stations showed that whole blood collection volume increased at an annual rate of 14.3% between 2006 and 2008. The average annual growth rate was 11.2%, and 22.6% in the number of whole blood donors and in that of platelet apheresis donors, respectively [2]. As shown in figure 1, the number of donors and the proportion of voluntary non-remunerated donations has increased over time, for both whole blood and platelets [2]. 2011 statistics reveal the country's total whole blood collection volume at 4,164 tons (approximately 12.32 million whole blood donations) and voluntary non-remunerated donations at 99%, with many cities having achieved 100% [3].
Fig. 1.
Changes in a whole blood and b platelet apheresis donations in China between 2006 and 2008 [2].
Despite a steady increase in total blood collections and voluntary non-remunerated blood donors, China still faces many challenges with its blood donor management system. For example, the blood donation rate in China is still low at 9%o of the whole population, which is much lower than the WHO-recommended level of 10–30%o [3]. The required donation interval between whole blood donations is relatively long, and whole blood donation volume per donation is relatively small when compared to other countries. The percentage of repeat donors among all donors is lower than in most developed countries. Several critical factors hinder the country's progress towards achieving a safe and adequate blood supply; these factors include cultural and social barriers to blood donation, lack of high-quality donor service and care, conservative selection criteria which eliminate many otherwise eligible donors, and lack of a national/regional blood donation information system which would allow blood centers to conduct donor follow-up in order to encourage future donations for a highly mobile young donor population.
The purpose of this review is to provide an overview of the key components of blood donor management in China. The concept of donor cycle which was developed by Donor Management IN Europe (DOMAINE) is used to examine the key process of donor management. As described in the DOMAINE study, the donor cycle includes: i) donor recruitment, ii) donor invitation, iii) donor selection, iv) donation procedures, and v) donor retention [4].
Donor Recruitment
According to the concept of donor cycle, the potential donor pool consists of prospective donors who are interested in or willing to donate blood. Donor recruitment targets this group of prospective donors [4]. Donor recruitment was not actively implemented in China until a decade ago. The blood donation system in China has developed over time in three major phases. The first phase lasted through the early 1990s, featured by paid or commercial blood donors. During this phase, recruitment efforts were minimal because blood donors were motivated by monetary reimbursement in exchange for the donation. Many of the private, underground plasma collection sites employed unsafe practices, resulting in the spread of transfusion-transmissible viral infections (TTVI) among donors and recipients [5]. The second phase began in 1998 when China established the National Blood Donation Law banning commercial blood collection. During this phase blood collection was dependent on compulsory, employer-organized donation. State-run work units were assigned donation quotas, and employees were mandated to donate with minimal compensation [6]. During this phase, recruitment efforts were mainly targeted at public sector employees, college students, and military personnel. Although a step in the right direction, this practice raised concerns that employer-organized donors may not be the safest source of blood due to the wide use of employer's incentives and coercion in some cases [6]. The third phase started in 2004, when the then MOH mandated employer-organized donations to be phased out within 3–5 years [7]. Since then, China's blood donation system has transitioned to voluntary, non-remunerated donation. During this phase, blood centers have been actively engaged in donor mobilization and recruitment targeted to the general population. Recruitment efforts include the use of mass and social media, including television, radio, billboard advertisement, newspaper, web blogging, and cellphone. The goal of the marketing campaign is to disseminate information on the social value and clinical need for blood donation. Previous studies in China have shown that the major channel for the public to obtain knowledge and information on blood donation is through interpersonal communication [8, 9]. Many blood centers have recruited repeat donors as volunteers to promote voluntary blood donation in their communities [10, 11]. Among the 355 surveyed blood centers, 43.7% of them have used repeat donors as volunteers to help with recruitment and post-donation care. Nationally there are about 93,800 volunteers registered in the network; however, only about 47% are acting effectively [11]. This indicates that there is great potential to improve volunteer service and involvement by including training peer recruiters, increasing their involvement in recruitment, and providing help to donors during and after donation.
In China, several incentives have been widely used to enhance donor recruitment, including provision of light refreshments, small gifts, recognition of contribution from the blood center and the government, and a blood credit which allows a donor or a donor's direct relative to receive a blood transfusion for free when needed. Most whole blood units are collected through blood mobiles. During blood shortage seasons (winter, summer, and national holidays), additional blood drives are organized in universities, work places, and on-site at the blood centers. Celebrities and government officials sometimes participate in such drives to lend ‘star power’ to the events. According to a national survey among 355 blood centers on their recruitment strategies during shortage seasons, 84.7% used mass media, 83.7% sent cellphone text message, 83.4% contacted registered donors to make an appointment for blood donation, 82.4% implemented on-site recruitment campaigns, 81.7% used their back-up donor team, and 79.7% organized blood drives at universities and military bases [12].
With the increasing challenge of meeting the clinical need for blood, some blood centers recently have turned to recruiting family replacement donors, especially during shortage seasons. In Nanjing, family replacement donation represented 6.6% of all blood collected. During seasonal shortage, the proportion of family replacement donation has been as high as 9.9% [13]. The way family replacement donation works is as follows: When a patient needs a transfusion (usually patients for elective surgeries), the family is informed that a family member or friend needs to donate blood in order to help ensuring the availability of blood for the patient. Blood collected from replacement donors enters into the general inventory instead of being reserved only for the particular patient. According to the studies in sub-Saharan Africa (SSA), family replacement donors are comparable to the first-time voluntary non-remunerated blood donors in terms of prevalence of TTVI [14, 15]. Nevertheless, there is a need to evaluate the safety issue of family replacement donors in China. Even though blood centers apply the same donor selection and screening criteria when accepting the replacement donors, these donors are obviously different from the general volunteer donors because at least for some of them, the donation may not be entirely ‘voluntary’ and they can also be under pressure to withhold risk behavior information during the health history screening. There is the possibility for families with no available family replacement donors to pay ‘professional’ blood donors to donate posing as family replacement donors. Since the safety of replacement donors in China has not been formally assessed, there should be close scrutiny on the use of these replacement donors. If family replacement donors are proven to be a relatively safe source of blood, family replacement donation may be a pragmatic additional approach to augment China's blood supply. The real challenge is to convert safe first-time replacement donors into regular, repeat donors [15]. In Hainan province, 13.6% of donors are family replacement donors, among them 14.2% were voluntary donors previously and 6.8% became repeat donors after family replacement donation [16]. Doctors and blood center staff play a key role in recruiting family replacement donors. It is important for them to provide information to patients and their family members about the status of blood supply shortage and the need for family replacement donation [13].
In order to optimize the donor recruitment efforts and effectively recruit prospective donors, it is important to understand the cultural, social, institutional, and personal factors that may influence potential donors’ attitudes towards blood donation. Several motivating factors in Chinese blood donors having been identified, including:
Altruism: In a study, 75.2% of voluntary donors were willing to donate because they wanted to help people in need of blood [17]. Another survey among 600 voluntary donors found that 54.8% donated blood because they wanted to help people improve their health [8]. A survey among platelet apheresis donors found 44.1% of donors were motivated by the feeling of helping other people and social responsibility [18].
Reciprocity: It was reported that 23.7% of the surveyed platelet apheresis donors engaged in blood donation because their family members or themselves had received blood products in the past. They therefore would like to donate to help someone else [18, 19].
Self-approval and self-respect: A study found 67.1% of whole blood donors were interested in donation because donating blood made them feel good about themselves [17]. Another study reported 23.0% of the surveyed platelet apheresis donors felt proud of themselves by blood donation [18].
Perceived health benefits: A study found 72.8% of donors felt that blood donation is beneficial to their own health; 30.2% thought donating blood could help get rid of fat [17]. Another survey found that 37.4% of voluntary donors believed that blood donation would produce positive health effects on themselves [8].
Free TTVI testing: A study found that 16.7% of donors admitted to using blood donation as a method to receive free blood test results on infectious disease [17]. This practice may pose threats to the safety of the blood supply as some of the test seekers are at high risk of TTVI. To reduce the number of test seekers, the government should increase and publicize the availability of free confidential testing for TTVI. According to the new blood donation regulations published by the Chinese government in 2013, during the informed consent process before collecting blood from donors, donors should be notified that donation is for altruism only; and that local CDC can provide free confidential testing for HIV.
Peer influence: A study reported 7.6% of platelet apheresis donors were prompted by friends or family members [18]. A survey among 600 donors at mobile collection vehicles found that 288 were accompanied by friends, and 128 of the friends went on to donated blood at the site [20].
Curiosity: This is mainly observed in young donors who donate blood out of an impulse to gain a novel experience [19].
There are several deterrents of blood donation identified among Chinese blood donors, including:
Fear of the risk of contracting TTVI through donation: A study found 16.2% of donors were concerned about unsafe collection practice in the blood center, and nearly 40% of voluntary donors did not feel completely safe from contracting TTVI from donating blood [17]. A survey among 279 college students found that 50% of them worried about infection through blood donation [21]. These data suggest there remains a pervasive concern among prospective and former donors of the safety of the Chinese blood collection system and that the incidence of unsafe donation practices in the past continues to resonate with the population.
Chinese traditional beliefs: There is a deeply rooted traditional belief in China that blood is associated with Qi, or life vitality, and therefore blood donation will result in irreversible loss of blood and Qi, and have a long-term negative impact on health and energy [5, 22, 23, 24]. In a study 21.9% of the surveyed donors thought that the loss of any amount of blood would have a detrimental effect on health; 8.6% thought that blood donation would substantially weaken health, vitality or overall immunity, and 3.1% thought the blood lost from a donation is enough to affect the flow of Qi. In addition, 36.8% would like to receive blood transfusion if he/she was hospitalized even if they did not need a blood transfusion, because they believed blood transfusion could be beneficial to improving health in general [17]. As the survey was conducted in one of the largest cities in China and among individuals who had already decided to donate, the prevalence and influence of traditional beliefs may be even greater among the general Chinese population, especially among rural populations [17].
Inconvenience: 24.7% of donors felt that the location and/or operating hours of the collection sites made it difficult to donate [17].
Social distrust: Several scandals related to Chinese Red Cross and blood services have caused public distrust of the blood collection system. For example, many people stopped donating blood right after the scandal of Guo Meimei, a business general manager at the Red Cross of China who publicly displayed her luxurious life on her microblog and aroused public concerns about the accountability of Chinese Red Cross’ fiscal management [25]. In addition, there is no publicly accessible information system in national or local blood banking system. The lack of information and transparency has raised the public's concern that the blood they donated may have been misused for profit [26].
Overall, there is a low rate of participation by the general public in blood donation; partially as a result of the lack of public awareness and interest, and a lack of trust in the safety and integrity of the Chinese blood collection system. To meet the ongoing and continuingly increasing clinical demand for blood, further efforts are needed to raise public awareness and involvement in blood donation. Efforts should concentrate on increasing the transparency of the blood banking system and educating the public about the pressing need for blood, and the improving donor recruitment process.
Donor Invitation
According to the concept of donor cycle, when a prospective donor decides to donate, he/she will come to a blood establishment and be registered as a new donor. As defined by the DOMAINE study, donor invitation is when blood establishments send invitations to registered and eligible donors requesting them to make a donation [4]. Unlike some European countries such as France and Finland, China does not have a registry for potential donors; first-time whole blood donors come to a blood establishment spontaneously and make donation right away; therefore, donor invitation in China only applies to repeat whole blood and platelet apheresis donors. For platelet apheresis donors, they come to blood collection sites and register themselves as a platelet apheresis donor, or they have been whole blood donors and already registered in the donor database. When there is a clinical need for platelets, blood centers will send an invitation to the registered platelet donors who have passed pre-screening tests [27]. Blood centers usually use telephone, text message, email, and online message systems to invite donors to donate. Use of donor invitation has greatly improved the likelihood of the prospective donor to donate and improved donor retention. A study in China showed that after the implementation of donor invitation, repeat donors increased from 27.5% in 2010 to 48.6% in 2011 [28].
Invited donors may or may not respond to the invitation. According to a study in a regional Chinese blood center, invitations to donors who had made a donation within the past 6 months resulted in 30% of them returned to donate. For the 70% who did not return, reasons include lost to follow-up due to change of contact information, negative previous donation experience, other commitments or busy schedule, and difficulty with transportation [29]. Another study among no-show donors found that reasons for not responding to the invitation included lost to follow-up such as in graduated college students (26.3%) or relocated military personnel (8.9%), personal reasons such as having no time (23.0%), medical conditions (11.7%), and having accumulated enough blood credit which made them eligible for lifetime free use of blood (10.5%). The blood center invited these no-show donors again through telephone calls, text message, and online communication. Among those no-show donors due to busy schedule, the re-invitation brought 75.1% of them back to donate. In addition, 66.5% of no-show donors due to health reason and 92.6% of donors who had accumulated free blood credit for lifetime showed up to donate [30]. This suggests that repeat invitation to no-show donors can greatly improve the chance of donation.
Donor Selection
Before donors make a blood donation, they need to undergo pre-donation screening to determine their eligibility as a part of the donor selection process [4]. In China, after obtaining the informed consent, the prospective donors provide basic demographic information and complete a health history questionnaire. They will receive brief physical exam, including weight, blood pressure, pulse, body temperature, and general condition. After passing the physical exam, they will give a blood sample for rapid testing which may include ABO typing, hemoglobin level, hepatitis B surface antigen (HBsAg) and alanine aminotransferase (ALT) [5]. Apheresis platelet donors will also be tested for platelet count before donation. Only donors with qualifying rapid testing results will proceed to donate blood.
Donor selection is to protect the safety of both the blood donor and the transfusion recipient [31]. Donor selection in China has been enforced through the national regulations established by the MOHFP. The following criteria are used in donor selection:
Age: Although most countries set 18–65 years and above as the age limit for donation and the USA does not set the upper limit for donor age, until a few years ago China only allowed people aged 18–55 years to donate blood. In 2012, the MOHFP issued the new Whole Blood and Component Donor Selection Requirements (GB 18467–2011), which allows people aged 55–60 years to donate blood, but only if they have made at least three blood donations in the past without any side effects. The rigorous requirement on the upper age limit was formulated with the purpose of protecting the safety of older donors. However, previous studies have shown that donation reactions are generally observed in donors of younger age. Among donors older than 30 years, the donation reaction rate is low and does not increase with age [31]. In addition, there is no evidence to support setting different age limit for first-time donors (up to 55 years) and repeat donors (up to 60 years) [31].
Several studies in China have suggested that Chinese blood donors are mostly young. A study in the five Chinese blood centers participating in the Retroviral Epidemiological Donor Study II International – China (REDS-II China) found that among the 226,489 whole blood donors, the majority (94%) of them were younger than 45 years, and half (52%) were younger than 25 years [7]. The result is comparable to a study in four large blood centers which found that approximately half (49%) of the donors were 25 years or younger, and only 8% were older than 45 years [3]. A study in a province capital blood center found that among the 381,185 donors who donated whole blood between 2008 and 2012, 61% of them were younger than 25 years [32]. Another study in a regional blood station reported 70% of their whole blood donors aged 20–40 yeas [33].
As for platelet apheresis donors, a study at a province blood center reported a mean age of 27.2 years, with 74% younger than 30 years, 16% between 30–40 years, and only 10% older than 40 years [34]. Another study found that 63% of platelet apheresis donors were younger than 30 years, 23% aged 30–40 years, and only 14% older than 40 years [18].
The predominance of young donors in China may be partially explained by its conservative age limit in blood donors. In addition, the traditional beliefs on the detrimental effect of blood donation on Qi and vitality are more deeply rooted in older people, while young people tend to be more open-minded.
Donation interval: Previously, the donation interval requirement was at least 6 months between whole blood donations, 4 weeks between platelet apheresis donations, and 6 months between platelet apheresis donation and previous whole blood donation. The 2012 donor selection requirements shortened the interval between platelet apheresis donations to 2 weeks, but no more than 24 platelet apheresis donations a year are allowed. The interval between platelet apheresis donation and previous whole blood donation was shortened to 3 months, while the interval between two whole blood donations remained at 6 months for donation volume of 400 ml or more. The donation interval requirement in China is very conservative compared to many countries. For example, the donation interval in the USA is 56 days for whole blood donation and 2 days for platelet apheresis [35]. China should re-examine the conservative donation interval requirement by conducting studies on the effect of donation on donor blood cell recovery and donor health. If the required donation interval time can be shortened without compromising donor’ health, it will help to alleviate the nation's chronic blood shortage.
Health history: The MOHFP introduced a new Donor History Questionnaire (DHQ) in 2012. This new DHQ is currently in use in most blood centers in China. Many items in the DHQ are formulated to maximize the safety of the recipient by eliminating donors at high risk of TTVI or taking medication which may harm the recipient. Some items are designed to protect the safety of the donor by eliminating donors with medical conditions which may increase the risk of adverse reactions or pose a health risk to the donor. The DHQ contains a total of 23 medical conditions that will permanently defer the donor from donation, including chronic respiratory diseases (chronic obstructive pulmonary disease, respiratory failure, bronchiectasis, etc.), circulatory system diseases (heart diseases, stenosis of pre-cerebral arteries, hypertension, hypotension, etc.), urinary system diseases (chronic nephritis or pyelonephritis, acute or chronic renal failure), autoimmune diseases (rheumatoid arthritis or insulin-dependent diabetes), blood system diseases, chronic skin disease, allergic diseases, neurological and mental diseases, infectious diseases, parasite disease, cancers, occupational diseases, transplant, and high-risk behaviors such as drug use, male-male sex and multiple sexual partners. The DHQ also contains 16 health conditions for temporary deferral, such as dental cleaning, tooth extraction, surgery, abortion, delivery, breastfeeding, upper respiratory infection, acute gastroenteritis, receipt of blood/blood components/blood products, and receipt of vaccines, etc.
Weight: According to the new donor selection requirement issued by the MOHFP in 2012, the minimal weight requirement is 50 kg for male and 45 kg for female. In order to reduce donation reaction, some blood centers require platelet apheresis donors to weigh over 55 kg. Previous studies have found that adverse donation reactions are more prevalent in donors of low body weight. A study among 12,703 Chinese college students found that donation reaction was 6.2% among donors with body weight less than 60 kg, compared to 3.6% in those weighing more than 60 kg [36].
Blood pressure: The MOHFP regulation has a requirement for a donor's systolic blood pressure to be between 90 and 140 mm Hg, diastolic blood pressure to be between 60 and 90 mmHg, and a pulse pressure of at least 30 mm Hg. Although studies in other countries revealed that blood pressure is not associated with adverse donation reaction, there is no such evidence in China [31]. China should re-examine the blood pressure restrictions as this criterion is not evidence-based and is likely too stringent.
Heart rate: China uses 60–100 beats/min as the allowable pulse range for donation; for athletes the lower limit of pulse is 50 beats/min. It has been reported that high pulse is associated with a slight increase in adverse reaction, although no such studies have been done in Chinese donors [31].
Hemoglobin: The minimal hemoglobin requirement in China is 120 g/l for men and 115 g /l for women; lower than the requirement of 125 g/l in the USA and Canada. A study found that nearly 10% of Chinese female donors were deferred due to low hemoglobin [32].
There are more male than female donors for both whole blood and platelet apheresis donations in China. Different studies have reported 57–60% of whole blood donors and 69–75% of platelet apheresis donors were males [3, 7, 33, 34, 37]. However, a study found an approximately equal number of male and female at donation registration. More female donors were deferred by low hemoglobin and body weight [32].
It has been shown that repeat donation is associated with iron deficiency [38]. The purpose of setting a minimal hemoglobin level is to exclude anemic donors from donation, thus protecting their health [31]. A study of repeat female donors in Canada found that 67% of donors with hemoglobin greater than 115 g/l were actually iron-deficient [39]. Research is needed to evaluate the prevalence of iron deficiency among Chinese female donors to help select the appropriate hemoglobin cut-off for donation for the protection of the donors.
HBsAg and ALT: Many Chinese blood centers perform rapid testing on HBsAg and ALT during pre-donation screening. The 2012 donor selection requirements issued by the MOHFP provide the gender-specific cut-off values for ALT. Many otherwise eligible donors are deferred regularly at many blood centers due to elevated ALT; however, elevated ALT can be caused by lifestyle factors such as exercise, alcohol drinking, being tired, overweight/obesity, and taking certain medicines [40]. A study in Chinese donors found that elevated ALT did not predict HBV infection [41]. With accumulated evidence against the sensitivity, specificity, and predictive value of ALT, the use of ALT testing and selection according to its cut-off value in blood centers should be re-examined to avoid substantial donor loss.
As shown above, some screening criteria are arbitrary or precautionary without having been evaluated for their effectiveness; some criteria have shown no or low association with an increased risk of donation reactions. The current policy should be systematically evaluated and further refined to eliminate those that lead to the unnecessary deferral of large numbers of blood donors. Some regional blood centers have been experimenting with modified donor selection criteria. For example, Hainan province passed a new regulation on blood donation in 2012. They relaxed whole blood donation interval to 3 months for male and 4 months for female donors, and the upper limit of age was raised to 60 years, without distinguishing first-time and repeat donors. After the implementation of the regulation, blood collection increased by 14.1% in a year [42]. Coordinated research on donor health and blood safety issues will help to direct the process of improving the donor selection process.
A donor may be temporarily or permanently deferred during pre-donation screening. The pre-donation deferral rate among whole blood donors varied between 5.7% and 10.0% in different studies in China [43, 44]. The major reasons for pre-donation deferral included i) age and short donation interval; ii) medical illness that were identified by health history questionnaire, including receipt of vaccines, tooth extraction, minor surgery, menstrual period, and taking medications such as aspirin; iii) low weight and high blood pressure that were identified during physical exam, iv) abnormal testing results such as low hemoglobin, high blood lipids, and elevated ALT found during rapid pre-screening, and v) certain blood types were excessive in blood bank stock at the time of donation [40, 45, 46]. Pre-donation deferral rate among platelet apheresis donors is higher because they have more requirements than whole blood donors, including HCT ≥ 0.36, platelet count before donation between 150 and 450 × 109 /l and after donation expected to be ≥100 × 109 /l. Studies in China have reported 14.7–24.4% of platelet apheresis donors were deferred before donation, mainly due to low platelet count, elevated ALT, abnormal WBC count, high blood lipids, HBsAg positivity and low hemoglobin [47, 48].
It should be noted that even a temporary deferral can result in substantial donor attrition because it may dampen the enthusiasm of the donor or arouse their confusion and anger, thereby reducing the chance of returning for a subsequent blood donation. A study among 2,220 temporarily deferred donors found that only 559 (25.2%) came back to donate. The major reason for not returning was that they felt rejected, were distressed by knowing the testing results, or were puzzled by the relevance of some questions on their ability to donate blood [45]. Another study among 18,025 donors found that among the donors who were temporarily deferred due to failing the pre-donation screening such as low hemoglobin, elevated ALT, hyperlipidemia, medical conditions, use of some medication, or recent vaccination, the deferral aroused strong discomfort, fear, and resistance. Therefore, only 30.0% of them came back to donate. For donors who were temporarily deferred by the blood center to avoid unnecessary overstocking of certain a blood type, 77.2% of them came back to donate [44]. Therefore, blood centers should pay attention to the psychological stress of deferred donors. They should explain the rationale for the deferral, explain the difference in sensitivity and specificity of blood center testing versus hospital testing, answer questions from donors, provide support and consultation, and assist the donor in making an appointment to return at a later date for donation. A study reported that by using these strategies, a blood center had 69% of temporarily deferred donors return for blood donation [43].
Potential donors may be concerned about disclosing sensitive health information and abnormal testing results in front of their friends or family members [44]. Pre-donation screening and disclosure of the results should be conducted in a private setting to encourage truthful disclosure of risk factors and to protect the donor privacy and confidentiality.
Donation Process
Prospective donors who pass the donor selection can proceed to make a donation. Whole blood collection occurs at mobile collection vehicles or fixed collection facilities (either at the blood centers or blood collection satellite stations/cabins). According to a national survey in 2009 (table 1), there were a total of 1,159 mobile collection vehicles in the surveyed 355 blood centers. Beijing topped the list with 35 vehicles. Less than half (44%) of the surveyed blood centers had satellite collection stations or cabins. In total there were 307 satellite collection stations/cabins, 254 in urban areas and 53 in suburban areas [49]. As there are no satellite collection stations or cabins installed in rural areas, a blood drive utilizing a mobile collection vehicle may be the best way to collect blood in rural communities. Currently blood donation made by the rural population is very low. In a province capital city with 31.8% of its population living in rural areas, only 1.6% of donors were rural residents [32]. In a non-capital city with a 54% rural population, only 3% of donors were from rural area [50]. Mobile blood collection vehicles should be dispatched to rural communities to increase the visibility and awareness of blood donation, and improve the access to blood donation in rural areas.
Table 1.
A national survey on mobile blood collection vehicles and satellite stations among 355 blood centers (2009) [49]
| Average number of facilities | Average number of staff each facility | Average work hours, hours/day | Average collection, units/day | |
|---|---|---|---|---|
| Province level blood centers (n = 31) | ||||
| Mobile collection vehicles | 5.6 | 5.4 | 8.1 | 59.8 |
| Satellite collection stations/cabins | 3.0 | 5.3 | 8.5 | 56.1 |
| Regional/county level blood stations (n = 324) | ||||
| Mobile collection vehicles | 2.9 | 5.0 | 9.3 | 38.4 |
| Satellite collection stations/cabins | 0.7 | 4.6 | 9.7 | 37.6 |
In China, blood is mostly collected at mobile collection vehicles or satellite stations/cabins. According to the REDS-II study, 97.9% of whole blood donors donated at vehicles or satellite collection sites [7]. Another study found that 53.4% of donors donated on vehicles [3]. The collection volume and proportion of donations made at mobile or satellite sites have been increasing steadily [51].
Compared to mobile collection vehicles, donation at satellite collection cabins increases the likelihood of repeat donation. It was reported that 65.9% of donors who donated at a satellite collection cabin came back again for donation; this rate is much higher than the 39.8% return rate of donors who donated at a mobile collection vehicle [52]. One of the reasons is that the donation environment is much better at a cabin than on a vehicle, which helps to improve the donation experience and reduce the risk of donation reaction. A study showed that 3.5% of Chinese donors who donated at a satellite collection cabin had donation reaction, whereas the donation reaction rate among donors donating on a vehicle is much higher (13.8%) [52]. Blood centers have made great efforts to improve donation environment, including providing free wireless internet, TV, magazines, and snacks [33]. These efforts will help to enhance the donation experience and improve donor recruitment and retention.
It is also important for blood centers to provide high-quality donor care. Anxiety and distress among blood donors are associated with an increased risk of donation reaction. A study showed that pre- and post-donation care relieved donor's anxiety and consequently reduced adverse reaction rate to 1.2% among first-time component donors, being much lower than the rate of 3.2% without donor care [53].
To improve the adequacy of the blood supply, it is necessary to promote higher volume donation. Traditionally, Chinese blood donors donate 200 ml whole blood at each donation. The 2012 regulations allow higher-volume whole blood donations; a whole blood donor can donate 200 ml, 300 ml, or 400 ml [37]. It is estimated that nationwide 400 ml donation accounts for approximately a half of whole blood donations, while the rest half of donations are 200 ml or 300 ml. There has been an increase in large-volume donations. The REDS-II study found that approximately 76% of whole blood donors donated higher-volume units [7]. The survey among 4 blood centers found that 56% of the donations were 400 ml donations. Another study in a province capital blood center found that 21.0% of donors donated 300 ml and 68.3% 400 ml, while only 10.2% donated 200 ml [54]. The transition from small-volume donation to large-volume donation will greatly increase the blood supply and reduce the number of donors to which recipients are exposed.
After donation, the blood will undergo two rounds of enzyme-linked immunosorbent assay (ELISA) testing for HBsAg, anti-HIV, HCV antibody (anti-HCV), and syphilis antibodies using kits produced by two different manufacturers. If found to be positive in any round of ELISA, the blood is disqualified for transfusion [5]. A study showed that 18.8% of blood samples had discordant ELISA testing results (one negative while the other positive) in ALT, 17.0% in HBsAg, 25.2% in anti-HCV, 65.1% in anti-HIV, and 7.2% in anti-TP. Altogether 17.5% of samples had discordant results [55]. False-positive results have been a major concern of this approach. It was reported that among the blood samples positive in one round of ELISA, 84.1% of HBsAg-positive and 79.8% of anti-HCV-positive samples were false-positive; while among the blood samples positive in both rounds of ELISA, 28.0% of HBsAg-positive and 32.0% of anti-HCV-positive samples were false-positive [56]. Another study found that among ELISA-positive samples, the false-positive rate was 52.3% for HBsAg, 60.8% for anti-HCV, and 66.7% for anti-HIV [57]. The findings of the remarkable discrepancies between the two rounds of ELISA testing results and the high false-positive rate urge the need of assessing the current donor testing strategy.
Blood donors with positive HBsAg, anti-HCV, anti-TP, or anti-HIV in ELISA screening are permanently deferred by Chinese blood centers. Because Chinese blood centers do not routinely perform confirmatory testing except for HIV, false-positive screening donors are permanently deferred, resulting in the loss of some eligible donors. Implementing routine confirmatory testing for all TTVI markers for screening testing-positive donors will help to reduce unnecessary permanent deferral of healthy donors. Providing confirmatory testing results to donors will also enhance the quality of donor service. As most blood centers do not have the authority to notify blood donors of their HIV confirmatory testing results, blood donors have to go to local CDC for confirmatory testing and consultation. The inability to provide confirmatory testing results to donors is currently a major limitation of the ability of blood centers to provide better donor service.
Although the majority of platelets are collected by automated apheresis, many blood centers also use platelet concentrates that are derived from whole blood donations when there is a shortage in apheresis-derived platelets. Strict process and procedures are used, including sterile, closed system and leukocyte reduction technique, to reduce bacterial contamination, HLA immunization, and febrile reactions.
Donor Retention
Donor retention aims at having donors donate regularly; repeat donors play a critical role in ensuring an adequate and safe blood supply. In China, the majority of donors donate only once in their lifetime. According to the REDS-II study, 67.9% of whole blood donors were first-time donors, which is consistent with the 63.3% rate of first-time donors reported by a survey among 4 blood centers [3, 7]. Another large-scale study among 381,185 voluntary donors between 2008 and 2012 found that only 18.9% of donors were repeat donors [32].
There tends to be more repeat donors in platelet apheresis donations. In a province capital city, 44% of platelet apheresis donors were repeat donors, in contrast to only 18.1% in whole blood donors [54]. A study in 2006 reported that 39.1% of platelet apheresis donors were repeat donors [18]. It has been observed that there is an increasing trend in repeat donations. One study reported that the proportion of repeat donors among platelet apheresis donors increased from 45% in 2007, to 57% in 2008, 63% in 2009, and 67% in 2010 [33].
Negative donation experiences, such as unpleasant environment of the collection site, dissatisfaction with the service of blood collection staff, a long wait time, and the lack of interactions with the staff, have been the most frequently cited reason for not returning for repeat donation. A study among platelet apheresis donors found that the major reasons for not donating again were long wait/collection time (55.7%) and donation reaction (15.2%) [58]. In another study among platelet apheresis donors, the reasons for not donating again were donation reaction (37.9%), long collection time (29.8%), long waiting time (19.6%), and dissatisfaction with donation service (5.1%) [59]. Therefore, in order to retain blood donors, improving the donation environment and service is critically important. Blood centers have employed different strategies to improve donor retention, including follow-up visit after donation, extending work hours and work days, shortening waiting time, club for repeat donors, improving donation environment, and enhancing donor care [18, 33].
There has been a debate on the effects of free blood credit on donor retention. Donors who have donated at least 800 ml are entitled to the free use of blood for lifetime. Although a study found that the use of accumulated points for blood credit helped increase donor retention from 46.4% in 2009 to 60.5% in 2011 [60], another study showed that free blood credit may have negative impact on retention among those whose accumulated donations had met the lifetime free blood credit requirement as some of them may have no motivation to donate any more [61]. Furthermore, with more and more voluntary non-remunerated donors donating blood, there has been an increasing number of people who are eligible for free blood credit. A study showed that the free use of blood increased by 40% every year, which made it difficult to keep up the need of the free use of blood [62]. The current policy on free blood credit should be further evaluated and modified as appropriate to enhance donor recruitment and retention while being realistic and sustainable.
Conclusion
As China moves towards a goal of meeting the nation's blood need with 100% voluntary, non-remunerated blood donations, it has encountered many challenges within the blood donation system. To meet the increasing clinical demand for blood and ensure a safe and adequate blood supply, there is an urgent need to strengthen the country's blood donor management, including educating and motivating more individuals (especially people from the rural areas) to be involved in blood donation, using rational and evidence-based selection criteria to assess the eligibility of donors, implementing timely donor follow-up and proactively scheduling appointment for donation, improving testing strategy and donor test result notification, and providing high-quality donor service and care. It is important to build a regional and national shared donor registry which will help to identify high-risk test-seeking donors who have already tested positive at other blood centers, and build a national and local donation information system to enhance the transparency of the donation system to gain more trust from the general public. Improving clinical blood utilization and strengthening patient blood management will also help counteract blood supply shortage in China [63].
Disclosure Statement
The authors have no conflicts of interest to declare.
References
- 1.Yu X, Huang Y, Qu G, Xu J, Hui S. Safety and current status of blood transfusion in China. Lancet. 2010;375:1420–1421. doi: 10.1016/S0140-6736(10)60003-7. [DOI] [PubMed] [Google Scholar]
- 2.An W. A survey on voluntary non-remunerated donation among 355 blood centers in China between 2006–2008 (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):22. [Google Scholar]
- 3.Li C, Xiao X, Yin H, He M, Li J. Prevalence and prevalence trends of transfusion transmissible infections among blood donors at four Chinese regional blood centers between 2000 and 2010. J Transl Med. 2012;10:176. doi: 10.1186/1479-5876-10-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Veldhuizen I, Folléa G, de Kort W. Donor cycle and donor segmentation: new tools for improving blood donor management. Vox Sang. 2013;105:28–32. doi: 10.1111/vox.12018. [DOI] [PubMed] [Google Scholar]
- 5.Shan H, Wang J, Ren F, Zhang Y, Zhao H, Gao G, Ji Y, Ness P. Blood banking in China. Lancet. 2002;360:1770–1775. doi: 10.1016/S0140-6736(02)11669-2. [DOI] [PubMed] [Google Scholar]
- 6.Gao F. Meeting the challenges in China. Transfus Int. 2000;79:10–11. [Google Scholar]
- 7.Wang J, Guo N, Guo X, Li J, Wen GX, Yang T, Yun Z, Huang Y, Schreiber GB, Kavounis K, et al. Who donates blood at five ethnically and geographically diverse blood centers in China in 2008. Transfusion. 2010;50:2686–2694. doi: 10.1111/j.1537-2995.2010.02722.x. [DOI] [PubMed] [Google Scholar]
- 8.Bi QY. Analysis on donation knowledge and donation motivators among voluntary blood donors (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):22. [Google Scholar]
- 9.Feng LQ. Discussion on strategies in recruiting low-risk blood donors (in Chinese) Yi Yao Lun Tan Za Zhi. 2011;32:118–120. [Google Scholar]
- 10.Li HW, Yang BC, Zhu WG, Lu L, Yang SQ. Establishment and Management of a Network of Volunteers in Chinese Blood Donors (in Chinese); in The 6th National Congress of the CSBT. China: Guangzhou, Guangdong; 2012. [Google Scholar]
- 11.Wang L. Management of voluntary blood donor volunteers (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):34. [Google Scholar]
- 12.Zhou SH. Survey on blood donor recruitment during seasonal shortage in Chinese blood centers (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):22. [Google Scholar]
- 13.Li GM, Liu QZ, Luo Y. Discussion on education and recruitment of family replacement donors (in Chinese) Zhong Guo Wu Zhen Za Zhi. 2011;11:8935–8937. [Google Scholar]
- 14.Tagny CT, Owusu-Ofori S, Mbanya D, Deneys V. The blood donor in sub-Saharan Africa: a review. Transfus Med. 2010;20:1–10. doi: 10.1111/j.1365-3148.2009.00958.x. [DOI] [PubMed] [Google Scholar]
- 15.Allain JP. Moving on from voluntary nonremunerated donors: who is the best blood donor? Br J Haematol. 2011. doi: 10.1111/j.1365-2141.2011.08708.x. [DOI] [PubMed]
- 16.Hou HF, Cai YX. Analysis on family replacement donation in Hainan Province in 2011 (in Chinese) Zhong Guo Shu Xue Za Zhi. 2012;25(suppl):5. [Google Scholar]
- 17.Tison GH, Liu C, Ren F, Nelson K, Shan H. Influences of general and traditional Chinese beliefs on the decision to donate blood among employer-organized and volunteer donors in Beijing, China. Transfusion. 2007;47:1871–1879. doi: 10.1111/j.1537-2995.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 18.Zhang XY, Wu XM, Xu J, Xu Y. Discussion on the key elements in apheresis donor recruitment and retention (in Chinese) Zhe Jiang Yi Xue. 2007;29:991–992. [Google Scholar]
- 19.Zhao CP, Wang XF, Song HY. Psychological factors in voluntary blood donation: recruitment of voluntary blood donors in different populations (in Chinese) Yi Xue Xin Xi. 2011;1:307. [Google Scholar]
- 20.Lin Y, Pei H, Zhang YH. Application of conformity in blood donor recruitment (in Chinese) She Qu Yi Xue Za Zhi. 2006;4:30–32. [Google Scholar]
- 21.Xu XM, Chen YX, Liao RX, Wang CY, Mao AM. A survey on attitudes towards voluntary blood donation among 279 college students (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):39. [Google Scholar]
- 22.Erwin K. The circulatory system: blood procurement, AIDS, and the social body in China. Med Anthropol Q. 2006;20:139–159. doi: 10.1525/maq.2006.20.2.139. [DOI] [PubMed] [Google Scholar]
- 23.Zaller N, Nelson KE, Ness P, Wen G, Bai X, Shan H. Knowledge, attitude and practice survey regarding blood donation in a Northwestern Chinese city. Transfus Med. 2005;15:277–286. doi: 10.1111/j.0958-7578.2005.00589.x. [DOI] [PubMed] [Google Scholar]
- 24.Zaller N, Nelson KE, Ness P, Wen G, Kewir T, Bai X, Shan H. Demographic characteristics and risks for transfusion-transmissible infection among blood donors in Xinjiang autonomous region, People's Republic of China. Transfusion. 2006;46:265–271. doi: 10.1111/j.1537-2995.2006.00711.x. [DOI] [PubMed] [Google Scholar]
- 25.Yan Z, Xu Y, Wang YM. Coping strategy for the trust crisis in blood donation (in Chinese) Zhong Guo Shu Xue Za Zhi. 2012. p. 194.
- 26.Zhou YL. Control of Social Credit Risk in Blood Collection and Supply (in Chinese); in The 6th National Congress of the CSBT. China: Guangzhou, Guangdong; 2012. [Google Scholar]
- 27.Xuan HX, Niu CL, Zhang MP, Gao LF. Strategies for recruiting apheresis donors (in Chinese) Lin Chuang Shu Xue Yu Jian Yan. 2007;9:151–152. [Google Scholar]
- 28.Liu M. Impact of after-donation follow up on donor retention (in Chinese) Lin Chuang Shu Xue Yu Jian Yan. 2012;9:3018–3019. [Google Scholar]
- 29.Wang YM, Zeng QJ. Recruitment and management of voluntary blood donors through information categorization (in Chinese) Yi Xue Xin Xi. 2011;3:1159. [Google Scholar]
- 30.Du LS, Liu XL, Li TJ. Strategies for donor recruitment and retention (in Chinese) Lin Chuang Shu Xue Yu Jian Yan. 2010;12:257. [Google Scholar]
- 31.Eder A, Goldman M, Rossmann S, Waxman D, Bianco C. Selection criteria to protect the blood donor in North America and Europe: past (dogma), present (evidence), and future (hemovigilance) Transfus Med Rev. 2009;23:205–220. doi: 10.1016/j.tmrv.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Wu JS. Analysis on Voluntary Blood Donors in Hefei City (in Chinese); in The 6th National Congress of the CSBT. China: Guangzhou, Guangdong; 2012. [Google Scholar]
- 33.Sun Z. Analysis on recruitment and service of apheresis donors in Yichang (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):32. [Google Scholar]
- 34.Yi ZM, Li RQ, Zhao SM. Analysis on recruiting voluntary blood donors on mobile collection vehicles (in Chinese) Chong Qing Yi Xue. 2010;39:2990–2991. [Google Scholar]
- 35.Kessler D. Blood donor, donation process, and technical aspects of blood collection. In: Shaz B, Hillyer C, Roshal M, Abrams C, editors. Transfusion Medicine and Hemostasis: Clinical and Laboratory Aspects. 2nd. London: Elseviery; 2013. pp. 37–44. [Google Scholar]
- 36.Wang L. Analysis on reasons for donation reactions among college students (in Chinese) Zhong Guo Shu Xue Za Zhi. 2012;25(suppl):31. [Google Scholar]
- 37.Yang D. Survey on voluntary blood donors in Qianjiang (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):40. [Google Scholar]
- 38.Cable RG, Glynn SA, Kiss JE, Mast AE, Steele WR, Murphy EL, Wright DJ, Sacher RA, Gottschall JL, Tobler LH, et al. Iron deficiency in blood donors: the REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion. 2012;52:702–711. doi: 10.1111/j.1537-2995.2011.03401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pi DW, Krikler SH, Sparling TG, Carter CJ, Wadsworth LD. Reappraisal of optimal hemoglobin standards for female blood donors in Canada. Transfusion. 1994;34:7–10. doi: 10.1046/j.1537-2995.1994.34194098609.x. [DOI] [PubMed] [Google Scholar]
- 40.Zheng WC, Shen CS, Rong Y, Wen CR, Zhan ZL. Reasons for deferral during rapid screening among voluntary blood donors (in Chinese) Zhong Guo She Hui Yi Xue Za Zhi. 2012;29:442–444. [Google Scholar]
- 41.Ren FR, Wang JX, Huang Y, Yao FZ, Lv YL, Li JL, Wen GX, Wen XQ, Liu J, Dong XD, et al. Hepatitis B virus nucleic acid testing in Chinese blood donors with normal and elevated alanine aminotransferase. Transfusion. 2011;51:2588–2595. doi: 10.1111/j.1537-2995.2011.03215.x. [DOI] [PubMed] [Google Scholar]
- 42.Chen XF. Review on the Process of Development of Voluntary Blood Donation Regulation in Hainan (in Chinese); in The 6th National Congress of the CSBT. China: Guangzhou, Guangdong; 2012. [Google Scholar]
- 43.Feng YQ, Cui X. Recruitment of postponed donors (in Chinese) Yi Xue Xin Xi. 2011;24:5849. [Google Scholar]
- 44.Zhang MP, Chen SF, Zhou XY, Tian ZB. Recruitment of temporarily deferred donors (in Chinese) Lin Chuang Shu Xue Yu Jian Yan. 2010;12:354–355. [Google Scholar]
- 45.Chen CY. Analysis on Temporarily Deferred Donors in Guizhong District (in Chinese); in The 6th National Congress of the CSBT. China: Guangzhou, Guangdong; 2012. [Google Scholar]
- 46.Hu YN. Reasons for temporarily deferred donation in Dalian (in Chinese) Zhong Guo She Hui Yi Xue Za Zhi. 2012;25(suppl):32. [Google Scholar]
- 47.Sheng Q, Li CY, Shen ZL. Pre-donation deferral reasons and recruitment for voluntary blood donors (in Chinese) Shi Yan Yu Jian Yan Yi Xue. 2009;27:699–701. [Google Scholar]
- 48.Wang YM, Wu CN, Meng W. Pre-donation deferral among platelet apheresis donors and their recruitment (in Chinese) Zhong Guo She Hui Yi Xue Za Zhi. 2010;23(suppl):33. [Google Scholar]
- 49.Li YJ, An W, Liang XH. A survey on mobile blood collection vehicles and cabins in 355 blood centers (in Chinese) Zhong Guo She Hui Yi Xue Za Zhi. 2010;23(suppl):20. [Google Scholar]
- 50.Peng JH, Yang QH, Yang YS. Application of 4C promotion theory in blood donor recruitment in rural area (in Chinese) Zhong Guo She Hui Yi Xue Za Zhi. 2009;22:586–589. [Google Scholar]
- 51.Fu YH. Recruitment activities and management of mobile blood collection sites (in Chinese) Zhong Guo Yi Yao Zhi Nan. 2011;9:330–331. [Google Scholar]
- 52.Wu HD, Ying HX, Mao MJ. Effects of blood collection cabins in blood donor recruitment and retention (in Chinese) Zhong Guo Nong Cun Wei Sheng Fu Wu Guan Li. 2011;31:1264–1266. [Google Scholar]
- 53.Zhang J, Song Y, Hu B. Application of donor care in donor retention (in Chinese) Zhong Guo Shu Xue Za Zhi. 2008;21:875–876. [Google Scholar]
- 54.Chen HL, Liu FC, Xu CL, Xie Q. A survey among blood donors in Nanchang (in Chinese) Zhong Guo Shu Xue Za Zhi. 2010;23(suppl):23. [Google Scholar]
- 55.Li R. Blood screening procedures and blood donor retention (in Chinese) Guo Ji Jian Yan Yi Xue Za Zhi. 2013;34:123–124. [Google Scholar]
- 56.Li XJ. The application of nucleic acid testing in keeping blood donor (in Chinese) Guo Ji Jian Yan Yi Xue Za Zhi. 2013;34:1230. [Google Scholar]
- 57.Wang X. NAT Testing on HBV, HCV, and HIV among Voluntary Blood Donors in Tianjin (in Chinese) 2012. in The 6th National Congress of the CSBT. Guangzhou, Guangdong, China,
- 58.Wang RF, Zhu LL, Zhou J. Recruitment and retention of apheresis donors (in Chinese) Zhong Guo Yi Yao Dao Bao. 2011;8:127–129. [Google Scholar]
- 59.Qu Z. Factors influencing retention of platelet apheresis donors (in Chinese) Zhong Guo Shu Xue Za Zhi. 2012;25(suppl):3. [Google Scholar]
- 60.Wang CM, Zhao HX, Liu CY. Effectiveness of accumulated points for retention of low-risk blood donors (in Chinese) Qi Lu Yi Xue Za Zhi. 2013;28:173–175. [Google Scholar]
- 61.Chen X, Zheng PX. Impact of follow-up on blood donor retention (in Chinese) Jian Yi Yi Xue Yu Lin Chuang. 2011;8:1254–1256. [Google Scholar]
- 62.Jiao DF. Discussion on use of free blood credit (in Chinese) Zhong Guo Shu Xue Za Zhi. 2012;25(suppl):31. [Google Scholar]
- 63.Shi L, Wang JX, Stevens L, Ness P, Shan H. Blood safety and availability: continuing challenges in China's blood banking system. Transfusion. 2013;54:471–482. doi: 10.1111/trf.12273. [DOI] [PubMed] [Google Scholar]