Abstract
Under normal conditions, the cornea is avascular, and this transparency is essential for maintaining good visual acuity. Neovascularization (NV) of the cornea, which can be caused by trauma, keratoplasty or infectious disease, breaks down the so called ‘angiogenic privilege' of the cornea and forms the basis of multiple visual pathologies that may even lead to blindness. Although there are several treatment options available, the fundamental medical need presented by corneal neovascular pathologies remains unmet. In order to develop safe, effective, and targeted therapies, a reliable model of corneal NV and pharmacological intervention is required. Here, we describe an alkali-burn injury corneal neovascularization model in the mouse. This protocol provides a method for the application of a controlled alkali-burn injury to the cornea, administration of a pharmacological compound of interest, and visualization of the result. This method could prove instrumental for studying the mechanisms and opportunities for intervention in corneal NV and other neovascular disorders.
Keywords: Medicine, Issue 86, Alkali-burn Injury, Corneal Neovascularization (NV), Corneal Blindness, Angiogenesis, Inflammation, Hemangiogenesis, Lymphangiogenesis
Introduction
Corneal blindness is the fourth most common cause of blindness, responsible for approximately 4% of all cases1. Corneal neovascularization (NV) plays a significant role in many of these pathologies, including herpetic keratitis (the leading infectious cause of blindness in the West) and trachoma (the leading cause of infectious blindness worldwide)2. Current therapies include steroids, nonsteroidal anti-inflammatory drugs (NSAIDs), anti-VEGF therapies, and cyclosporin A as well as conventional or laser surgical techniques3. However, the severely debilitating nature of corneal NV based pathologies, the paucity of surgical facilities capable of treating corneal NV, and the lack of a strongly performing pharmacological option led a recent expert roundtable to conclude that, despite the extant therapies, the fundamental medical need presented by these pathologies remains unmet4.
The human cornea consists of 5 layers, 3 cellular layers (epithelial, stromal and endothelium) and 2 interface (Bowman membrane and Descemet membrane). It functions as a mechanical barrier and refractive surface for the eye. Its transparent nature is the consequence of a delicate balance of its components and is integral to its proper function5. Normally avascular, the cornea receives blood from microvessels running along its outer edge which are fed from the ciliary and ophthalmic arteries. Corneal NV occurs when a stimulus promotes angiogenesis of these vessels allowing them to grow towards the center of the cornea and thus limit vision6. Corneal angiogenesis includes hemangiogenesis and lymphangiogenesis, which result in the ingrowth of blood vessels and lymphatic vessels from the limbal vascular arcade towards the center of the cornea. This leads to a breakdown of corneal "angiogenic privilege", an increase in corneal opacity and fibrosis, disruption of the corneal layers, and edema7. The precise triggers of corneal NV are numerous, ranging from a response to infectious disease such as trachoma to a chemically induced state caused traditional medicines, industrial chemicals, or even chemical warfare agents.
The molecular mechanisms of this process are not, as yet, fully characterized; however, a few key players have been identified. Under normal conditions the cornea possesses a unique ‘angiogenic privilege' maintained by a redundant array of anti-angiogenic factors (such as soluble VEGF-R1)8. However, in response to an external stimulus (such as an injury), there will be a local upregulation of pro-angiogenic factors (e.g. VEGF-A). This tips the balance of pro and anti- angiogenic factors that underlies the cornea's angiogenic privilege, and leads to hemangiogenesis, lymphangeogenesis, and inflammation, therefore causing corneal pathology and even blindness9.
Given the unmet medical need of this highly debilitating pathology, it is of interest to the field to have a reliable animal model of corneal NV. Here we present such a model: controlled alkali-burn injury. Various eye-injury models based on using filter paper rings have been used since 1970s10. In 1989, a group of Harvard Medical School ophthalmologists characterized a standard model of a central corneal alkali-burn injury in rabbit based on soaking a piece of circular filter paper with sodium hydroxide (NaOH) and applying it to the cornea at a specific range of concentrations11. Since then, this technique has been adapted for use in the mouse12-14. Recently, the Wang lab studied the therapeutic effects of the histone deacetylase (HDAC) inhibitor SAHA in the pathogenesis of corneal NV using a mouse corneal alkali-burn injury model15. The methodology of the mouse corneal alkali-burn injury model presented here was built mainly on the prior work of two other papers14,16.
Protocol
Note: The following protocol and representative results use the HDAC inhibitor SAHA as an example compound. However, this protocol is by no means limited to the use of SAHA, and is recommended as a general method to test the effects of soluble compounds on corneal neovascularization. Minor modifications will need to be made for degree of dilution as well as frequency and duration of application. Additionally, compounds that are easily soluble in water will be able to be administered in the absence of DMSO.
Ethical Statement: All animal experiments should only be performed in compliance with national law and institutional regulations. This protocol was approved for use by Tulane University Institutional Animal Care and Use Committee.
1. Preparation of Materials (in Order of Use)
Cut a piece of cellulose filter paper (11 μm) into 2 mm circles.
Prepare a 1 M solution of NaOH by dissolving 20 g of NaOH in 500 ml distilled H2O. Store at room temperature. CAUTION: NaOH solutions are corrosive and can cause alkali-burns.
Prepare an anesthetic cocktail by diluting 10 ml of 100 mg/ml ketamine and 2.5 ml of 20 mg/ml xylazine in 37.5 ml of 1x PBS for a final concentration of 20 mg/ml ketamine and 4 mg/ml xylazine.
Prepare a 0.5% solution of proparacaine hydrochloride (for topical analgesia) by dissolving 500 mg of proparacaine hydrochloride in 100 ml of filtered PBS.
Prepare 1x PBS by dissolving 8 g NaCl, 0.2 g of KCl, 1.44 g Na2HPO4, and 0.23 g of NaH2PO4 in 900 ml of distilled H2O. Adjust to 7.4 pH. Bring the solution to a final volume of 1,000 ml with distilled H2O and filter to ensure sterility.
Prepare 1,000x stock solutions of SAHA at ~100 mM in dimethyl sulfoxide (DMSO) by dissolving 26.4 mg of SAHA in 1 ml of DMSO. Dilute to a 1x (~10 μM) solution in filtered PBS for each use. Store the stock solution at -20 °C for up to one month. CAUTION: DMSO is a known toxin and mutagen.
Prepare a 4% solution of paraformaldehyde (PFA) for fixation. Under a chemical hood, dissolve 4 g of PFA in 90 ml of PBS. Bring the mixture to 65 °C and titrate to a pH of 7.4. Once the PFA has dissolved, bring the solution to a final volume of 100 ml. Store at 4 °C for up to one month. CAUTION: PFA is a known to be allergenic, carcinogenic, and toxic.
Prepare 1x blocking buffer by diluting 5 ml of goat serum and 500 ul of Triton X-100 into 94.5 ml of PBS.
Prepare 1x washing buffer by diluting 500 ul of Triton X-100 into 99.5 ml of PBS.
2. Alkali-Burn Injury & Compound Treatment
Soak a round piece of filter paper, ~2 mm in diameter, in a solution of 1 M NaOH.
Anesthetize the mouse with an injection of 100 mg/kg ketamine and 5 mg/kg xylazine, which is ~100 μl of the anesthetic cocktail from step 1.3 per 25 g mouse. Anesthesia should take ~1-2 min to set in. Depth of anesthesia may be determined by gently pinching the toe or tail of the animal, if anesthesia is sufficient there should be no response. Note: Care should be taken to ensure the mouse does not succumb to anesthesia induced hypothermia.
Using an eyedropper, topically apply a drop of 0.5% proparacaine hydrochloride to the corneal surface for local analgesia.
Using sterile forceps, pick up a piece of NaOH soaked filter paper. If you notice excess NaOH clinging to or dripping from the filter paper, briefly tap the soaked filter paper on a dry piece of filter paper to absorb the excess. Place the piece of NAOH soaked filter paper on the central cornea. Leave it for 30 sec to generate an acute alkali-burn of ~2 x 2 mm2 in area. A surgical microscope is helpful in properly placing the filter paper. Note: Only one eye of the mouse should be injured with the other serving as a control.
Remove the filter paper. Using a 10 ml syringe, gently flush the eye with 10 ml of 1x PBS twice to wash away residual 1 M NaOH.
Immediately apply a drop of 1x SAHA working solution (or a vehicle control consisting of PBS diluted DMSO containing no SAHA) topically to the cornea. Repeat application 3x/day for 14 days. Note: during this period a topical antibiotic ointment is not recommended as it may interfere with the development of the injury and the delivery of the compound. Use a liquid antibiotic solution, such as 3% Gentamicin solution, instead.
Proceed directly to Clinical Assessment (Protocol 3 below) or sacrifice the mouse and enucleate the eyes for corneal flat mount (Protocol 4 below) or conventional paraffin/frozen histology.
3. Clinical Assessment
- Perform a daily examination of the mice in a blinded fashion under a surgical microscope and score corneal NV based on corneal opacity, NV, and vessel size. Use at least two observers and record a final score that is the average of the two.
- Score corneal opacity on a scale of 0-4. 0 = completely clear; 1 = slightly hazy, iris and pupil easily visible; 2 = slightly opaque, iris and pupil still detectable; 3 = opaque, pupils hardly detectable; and 4 = completely opaque with no view of the pupil.
- Score NV on a scale of 0-3. 0 = no neovessels; 1 = neovessels at the corneal limbus; 2 = neovessels spanning the corneal limbus and approaching the corneal center; 3 = neovessels spanning the corneal center.
- Score vessel size on a scale of 0-3. 0 = no neovessels; 1 = neovessels detectable under surgical microscope; 2 = neovessels easily seen under surgical microscope; 3 = neovessels easily seen without the microscope.
Using a digital camera, take representative images of the eye at 7 days and 14 days.
4. Corneal Staining and Flat Mounts
Fix enucleated eye in 4% PFA for at least 1 hr at 4 °C.
Transfer the eye to 1x PBS and use forceps to carefully remove excess tissue.
- With the aid of a surgical microscope, use a needle (18 gauge) or micro-knife to perforate the pericorneal region of the eye (note: this should release fluid from the eye).
- From the perforation made in section 4.3.1 use a pair of surgical scissors to cut the anterior portion of the eye (cornea) from the posterior portion.
Transfer the cornea back into 4% PFA for fixation overnight at 4 °C.
Discard the 4% PFA (CAUTION: PFA is hazardous and must be disposed of in accordance with institutional regulations) and rinse the cornea three times with 1x PBS to remove any residual PFA.
- Incubate in 1x blocking buffer for at least 2 hr at room temperature to permeabilize the tissue and prevent nonspecific binding of the primary antibody.
- Apply primary antibody in 1x blocking buffer, at a 100-500 fold dilution. (e.g. rat anti-mouse-PECAM-1 for detecting blood vessels at 1:100, rabbit anti-mouse-LYVE-1 for detecting lymphatic vessels at 1:500, and/or rat anti-mouse-F4/80 for detecting macrophages at 1:100). Incubate at 4 °C overnight.
- Wash six times with 1x washing buffer for 1 hr each time at room temperature to fully remove unbound primary antibody.
- Apply a secondary antibody in 1x blocking buffer at a 500-1,000 fold dilution. (e.g. a 488 nm fluorescent tagged goat anti-rat-IgG at 1:800 or a 594 nm fluorescent tagged goat anti-rabbit-IgG at 1:800). Incubate at 4 °C overnight.
- Wash three times with 1x PBS for 1 hr each at room temperature to fully remove unbound secondary antibody.
Transfer the cornea into fresh 1x PBS and, with the aid of a surgical microscope, carefully make four incisions from periphery towards the center. This should divide the cornea into four quadrants of approximately equal size (the resulting shape should look rather like a butterfly) and allow it to lie flat on a slide.
Mount with a mounting medium appropriate for fluorescent imaging. For best results, samples should be imaged immediately and digital photographs taken, but may be stored for several weeks protected from light at 4 °C.
Representative Results
After alkali-burn injury, corneal NV occurs in a predictable, time-dependent fashion. Figure 1 demonstrates the stark difference both in neovascularization and corneal opacity between an untreated animal (Figure 1A) and an animal treated with the HDAC inhibitor SAHA (Figure 1B) at the 7 day time point.
Figures 2A and 2B demonstrate a corneal flat mount of an untreated control eye with primary PECAM-1 and LYVE-1 staining and secondary Alexa Fluor 488 and 594 staining (respectively). Figures 2C and 2D show the same staining on an eye treated daily with the HDAC inhibitor SAHA, note the dramatic decrease in both hemangiogenesis and lymphangiogenesis.
Figures 3A and 3B provide a detailed look at the two stains. PECAM-1 serves a marker for the blood vessels (Figure 3A), while LYVE-1 binds specifically to the lymphatic vessels (Figure 3B). An overlay of the two fields is shown in Figure 3C, allowing comparison of hemangiogenesis vs. lymphangiogenesis as well as a comparison of the differing cell morphology.
Following PFA fixation (step 4.1), you can use conventional sectioning protocols (not detailed in the protocol above) to generate either frozen or paraffin embedded sections of the eye. While this does not allow the same level of quantification of invasion that a flat mount does, sagittal sections of the cornea can show you corneal thickness and relative depth of the tubes within the eye. Figures 3D-F shows sagittal, frozen sections of the cornea and either F4/80 (macrophage staining), DAPI (nuclear staining), or a merged image.
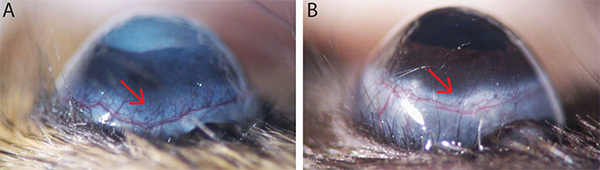 Figure 1. Progression of corneal neovascularization seven days after alkali-burn injury. (A) Representative image of an untreated eye. (B) Representative image of an eye treated three times per day with our compound of interest (the HDAC inhibitor SAHA). Note the difference in corneal opacity and neovascularization. Please click here to view a larger version of this figure.
Figure 1. Progression of corneal neovascularization seven days after alkali-burn injury. (A) Representative image of an untreated eye. (B) Representative image of an eye treated three times per day with our compound of interest (the HDAC inhibitor SAHA). Note the difference in corneal opacity and neovascularization. Please click here to view a larger version of this figure.
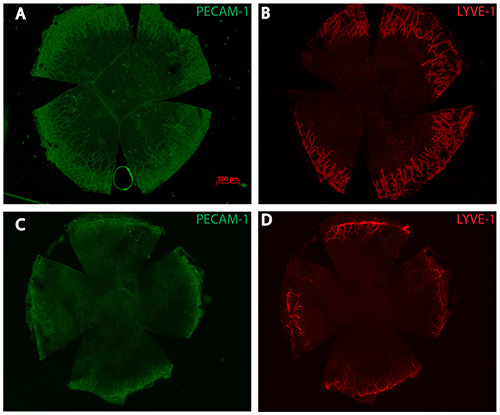 Figure 2. Representative images of an untreated control (A and B) and a SAHA treated (C and D) cornea seven days after alkali-burn injury. (A and C) Wide field image of vascular endothelial cell staining with PECAM-1. (B and D) Wide field image of lymphatic endothelial cell staining with LYVE-1. Please click here to view a larger version of this figure.
Figure 2. Representative images of an untreated control (A and B) and a SAHA treated (C and D) cornea seven days after alkali-burn injury. (A and C) Wide field image of vascular endothelial cell staining with PECAM-1. (B and D) Wide field image of lymphatic endothelial cell staining with LYVE-1. Please click here to view a larger version of this figure.
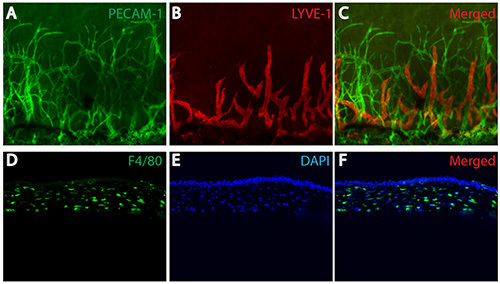 Figure 3.(A) Vascular endothelial cell staining with PECAM-1. (B) Lymphatic endothelial cell staining with LYVE-1. (C) Merged PECAM-1/LYVE-1 staining. (D) F4/80 staining of macrophages in a sagittal frozen section. (E) DAPI staining of cell nucleus in a sagittal cut frozen section. (F) Merged F4/80 and DAPI staining. Please click here to view a larger version of this figure.
Figure 3.(A) Vascular endothelial cell staining with PECAM-1. (B) Lymphatic endothelial cell staining with LYVE-1. (C) Merged PECAM-1/LYVE-1 staining. (D) F4/80 staining of macrophages in a sagittal frozen section. (E) DAPI staining of cell nucleus in a sagittal cut frozen section. (F) Merged F4/80 and DAPI staining. Please click here to view a larger version of this figure.
Discussion
The protocol presented here results in reproducible levels of hemangiogenesis, lymphangiogenesis, and inflammation, making it an ideal system to study these three (interrelated) processes. While this method produces centralized corneal NV, several methods that have been developed to cause more directed NV, namely suturing of the cornea17 and implanted growth-factor expressing pellets18, might also be of interest. Our protocol is designed for use in the adult mouse, providing an easy to use animal model while also allowing a lab to take full advantage of a host of molecular and transgenic techniques not yet available for larger mammals. The above protocol and representative results detail the use of mice on a C57bl/6J background. Albino mice would also be suitable and may provide for easier imaging; however, a recent study indicates that the neovascular response of albino mice may not be as dramatic19. Further, unlike several other neovascularization models, corneal NV can be scored with examination through a surgical microscope or even by the naked eye. If a more rigorous quantification of the extent of neovascularization is required, digital images of the stained flat mount can be analyzed via a number of software packages, an example of how to do so with photoshop CS4 can be seen in Conner, et al. recent Nature Protocols paper "Quantification of oxygen-induced retinopathy in the mouse" 20.
Proparacaine hydrochloride is an amino ester analgesic applied as a topical solution (it is possible that other members of this family would be equally acceptable). Even though the animal is placed under general anesthesia for the procedure, we deem additional topical analgesia an ethical necessity to prevent undo pain to the cornea. It is imperative that the PBS used to dilute your compound and flush the eye be filtered and kept clean throughout the procedure (check for visible signs of contamination before each use). PBS is called for based on individual lab tradition; any equivalent balanced salt solution should achieve the desired result. Likewise, revisions of the immunohistochemistry protocol presented here may be called for if antibodies from other sources are used (i.e. the degree of dilution required).
The most technically challenging portions of this procedure are the initial placement of the NaOH soaked filter paper and the dissection of the cornea. We recommend that both techniques be practiced prior to the actual procedure. Filter paper must be placed in the center of the corneal in order to promote an equal level of neovascularization from all sides. Any degree of offset will create a high level of variability from mouse to mouse. Corneal dissection requires a good deal of manual dexterity. The eye is likely to deform in response to an attempt to perforate the pericorneal region. We recommend using a sharp, small gauge needle to make the initial cut and release the pressure inside. After an initial puncture is made, a pair of surgical scissors can be inserted into the hole and used to cut along an imaginary line separating the anterior of the eye from the posterior eye cup. Working slowly and carefully should yield an intact cornea.
It should be noted that while the primary purpose of this protocol is to assay the efficacy of various compounds in treating corneal alkali-burn injury it also has the potential to be used to study corneal wound re-epitheliaztion, corneal fibrosis, and limbal epithelial stem cell renewal. Furthermore, it serves as a general model to explore the mechanisms of pathological hemangiogenesis, lymphangiogenesis, and inflammation. The relative ease with which the protocol can be performed, as well as its noninvasive nature, presents an appealing opportunity for in vivo compound screening, efficacy tests, and characterization of transgenic mouse models with respect to pathological angiogenesis.
Disclosures
The authors have nothing to disclose.
Acknowledgments
We are grateful for Dr. Xinyu Li's help in preparing the manuscript. S.W. was supported by a Startup fund from Tulane University, President's Research Council New Investigator Award from UT Southwestern Medical Center, NIH Grant EY021862, a career development award from the Research to Prevent Blindness foundation, and a Bright Focus Award in Age Related Macular Degeneration Research.
References
- Pascolini D, Mariotti S. Global estimates of visual impairment. Br. J. Ophthalmol. 2010;96(5):614–618. doi: 10.1136/bjophthalmol-2011-300539. [DOI] [PubMed] [Google Scholar]
- Whitcher J, Srinivasan M, Upadhyay M. Corneal Blindness: A Global Perspective. Bull. World Health Org. 2003;79(3):214–221. [PMC free article] [PubMed] [Google Scholar]
- Gupta D, Illingworth C. Treatments for corneal neovascularization: a review. Cornea. 2011;30(8):927–938. doi: 10.1097/ICO.0b013e318201405a. [DOI] [PubMed] [Google Scholar]
- Cursiefen C, et al. Consensus statement on indications for anti-angiogenic therapy in the management of corneal diseases associated with neovascularisation: outcome of an expert roundtable. Br. J. Ophthalmol. 2012;96(1):3–9. doi: 10.1136/bjo.2011.204701. [DOI] [PubMed] [Google Scholar]
- Delmonte D, Kim T. Anatomy and Physiology of the Cornea. J. Cataract Refract. Surg. 2011;37(3):588–598. doi: 10.1016/j.jcrs.2010.12.037. [DOI] [PubMed] [Google Scholar]
- Cursiefen C, Seitz B, Dana MR, Streilein JW. Angiogenesis and lymphangiogenesis in the cornea. Pathogenesis, clinical implications and treatment options. Der Ophthalmologe. 2003;100(4):292–229. doi: 10.1007/s00347-003-0798-y. [DOI] [PubMed] [Google Scholar]
- Chang J, Gabison E, Kato T, Azar D. Corneal Neovascularization. Curr. Opin Ophthalmol. 2001;12(4):242–249. doi: 10.1097/00055735-200108000-00002. [DOI] [PubMed] [Google Scholar]
- Ambati B, et al. Corneal Avascularity is due to Soluble VEGF Receptor-1. Nature. 2006;443(7114):993–997. doi: 10.1038/nature05249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cursiefen C, et al. VEGF-A Stimulates Lymphangiogenesis and Hemangiogenesis in Inflammatory Neovascularization via Macrophage Recruitment. J. Clin. Invest. 2004;113(7):1040–1050. doi: 10.1172/JCI20465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiri O. Paper Strips and Rings as Simple Tools for Standardization of Experimental Eye Injuries. Ophthal. Res. 2009;1975(7):363–367. [Google Scholar]
- Ormerod L, Abelson M, Kenyon K. Standard Models of Corneal Injury Using Alkali-Immersed Filter Discs Invest. Ophthalmol. Vis. Sci. 1989;30(10):2148–2153. [PubMed] [Google Scholar]
- Saika S, et al. Therapeutic effects of adenoviral gene transfer of bone morphogenic protein-7 on a corneal alkali injury model in mice. Lab. Invest. 2005;85(4):474–486. doi: 10.1038/labinvest.3700247. [DOI] [PubMed] [Google Scholar]
- Ferrari G, Bignami F, Giacomini C, Franchini S, Rama P. Safety and efficacy of topical infliximab in a mouse model of ocular surface scarring. Invest. Ophthalmol. Vis. Sci. 2013;54(3):1680–1688. doi: 10.1167/iovs.12-10782. [DOI] [PubMed] [Google Scholar]
- Sosne G, Christopherson P, Barrett R, Fridman R. Thymosin-beta4 modulates corneal matrix metalloproteinase levels and polymorphonuclear cell infiltration after alkali injury.Invest. Ophthalmol. Vis. Sci. 2005;46(7):2388–2395. doi: 10.1167/iovs.04-1368. [DOI] [PubMed] [Google Scholar]
- Li X, et al. Inhibition of Multiple Pathogenic Pathways by Histone Deacetylase Inhibitor SAHA in a Corneal Alkali-Burn Injury Model. Mol. Pharm. 2013;10(1):307–318. doi: 10.1021/mp300445a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoeruek E, et al. Safety, penetration and efficacy of topically applied bevacizumab: evaluation of eyedrops in corneal neovascularization after chemical burn. Acta Ophthalmol. 2008;86(3):322–328. doi: 10.1111/j.1600-0420.2007.01049.x. [DOI] [PubMed] [Google Scholar]
- Bucher F, Parthasarathy A, Bergua A, Onderka J, Regenfuß B, Cursiefen C, Bock F. Topical Ranibizumab inhibits inflammatory corneal hem- and lymphangiogenesis. Acta Ophthalmol. 2012. [DOI] [PubMed]
- Hajrasouliha A, Sadrai Z, Chauhan S, Dana R. b-FGF induces corneal blood and lymphatic vessel growth in a spatially distinct pattern. Cornea. 2012;31(7):804–809. doi: 10.1097/ICO.0b013e31823f8b5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers M, et al. The albino mutation of tyrosinase alters ocular angiogenic responsiveness. Angiogenesis. 2013;16(3):639–646. doi: 10.1007/s10456-013-9342-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor K, et al. Quantification of oxygen-induced retinopathy in the mouse: a model of vessel loss, vessel regrowth and pathological. Nat. Protoc. 2009;4(11):1565–1573. doi: 10.1038/nprot.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]


