Abstract
Background
The cerebrospinal fluid (CSF) biomarkers total tau, abnormally phosphorylated tau and amyloid β 1-42 are strongly associated with Alzheimer's disease (AD). Apart from the pathologic hallmarks that these biomarkers represent, other processes such as inflammation and microglial activation are present in the brains of patients with AD. New biomarkers related to these processes could be valuable for the diagnosis and follow-up of AD patients and for the evaluation of inflammation-related pathologies.
Aim
The aim of this study was to evaluate the association of inflammatory CSF biomarkers with AD.
Methods
Twenty-five AD patients and 25 controls who had a pathological and normal CSF profile of the core AD biomarkers, respectively, were included in this study. CSF levels of chitotriosidase, YKL-40 (also known as chitinase-3-like protein 1) and monocyte chemoattractant protein-1 (MCP-1) were quantified and the levels compared between the groups.
Results
AD patients had increased CSF levels of chitotriosidase and YKL-40 (both approximately twice higher than in controls), while the levels of MCP-1 were similar in the AD and control groups.
Conclusion
The results indicate that chitotriosidase and YKL-40 may be helpful for the evaluation of cerebral inflammatory activity in AD patients.
Key Words: Alzheimer's disease, Cerebrospinal fluid, Biomarkers, Inflammation
Introduction
Alzheimer's disease (AD) is a progressive neurodegenerative disorder that is characterized by neuronal loss, extracellular deposits of amyloid β (Aβ) and intracellular accumulations of abnormally phosphorylated tau (P-tau) protein [1]. These features increase during the course of the disease and can be visualized upon autopsy of the brain [2]. However, indirect evidence of these changes can be acquired while the patient is still alive through brain imaging and cerebrospinal fluid (CSF) biomarkers. The CSF levels of total tau (T-tau) and abnormal P-tau protein are increased in AD patients, while levels of CSF Aβ42 are decreased [3]. A large number of studies have shown that a profile with pathological levels of these three biomarkers is highly associated with AD and development of AD in patients with mild cognitive impairment (MCI) [4]. At present, there are insufficient data to evaluate their accuracy in predicting incipient AD in cognitively healthy individuals [5]. The biomarker profile can be used in research to increase the probability that a dementing process is caused by AD, thus adding strength to further disease-specific analyses [6].
Apart from the above-mentioned pathological hallmarks, cerebral processes related to inflammation are highly present in AD patients. These processes may contribute to neuronal dysfunction and cell death in AD [7]. Epidemiological studies have shown delayed onset of AD in subjects using non-steroidal anti-inflammatory drugs [8,9]. Data from ultrastructural studies have shown an association between brain amyloid deposits and microglia as well as astrocytes [10,11]. Microglia are the main phagocytic immune cells in the CNS, but their role in relation to AD is not clear. Some evidence points towards an important role in the clearance of Aβ [12], while other evidence suggests that microglia may contribute to the build-up of amyloid plaques [13,14]. Other theories state that microglial activation might mediate the neurodegeneration seen in the brain of AD patients [15]. Astrocytes have a trophic function for neurons. They can also modulate the activity of microglia and influence their reactivity to Aβ [16].
Biomarkers reflecting inflammatory processes may provide new ways of evaluating patients with AD. The recent finding of a missense mutation in TREM2 that may render microglia overactive to brain amyloid pathology and increases the AD risk about 4-fold [17,18], has raised the interest in the role of microglia in the AD process. In this study, we wanted to investigate the association between AD and three candidate inflammatory CSF biomarkers.
The enzyme chitotriosidase is secreted by activated macrophages, and patients with Gaucher's disease (a disease characterized by malfunctioning lysosomal storage) have increased levels in plasma [19]. CSF levels of the enzyme have been assessed in AD patients and nondemented controls, with increased levels found in the former group, although with an overlap between the groups [20,21]. Another inflammatory biomarker is YKL-40 (also known as chitinase-3-like protein 1), a glycoprotein that structurally resembles chitotriosidase [22], and is mainly expressed in astrocytes in the brain [23,24]. Some [24,25], but not all [20], studies have found increased levels of YKL-40 in AD patients. The monocyte chemoattractant protein-1 [MCP-1, also known as chemokine CC motif ligand 2 (CCL2)] can be produced by microglia and is involved in the recruitment of monocytes in the central nervous system. Studies measuring the levels of MCP-1 have given contradictory results with either increased levels in patients with AD [26,27] and MCI [26] or no differences between AD patients and controls [20]. Some of the inconsistent data may be explained by heterogeneous AD and control groups.
The aim of this study was to quantify these three inflammatory biomarkers in AD patients with a pathological profile of T-tau, P-tau and Aβ42, and in cognitively healthy controls with a normal CSF profile to detect differences between the groups in which the biomarker-supported diagnostics minimises the risk of including preclinical AD patients in the control group and patients with AD-like memory impairment but without AD neuropathology in the AD group.
Methods
Study Participants
The AD and the control group were selected based on the core CSF biomarker profile in accordance with the International Work Group criteria for the diagnosis of AD [28] to yield highly specific clinical diagnosis with regard to neuropathological characteristics. The AD patients and controls were prospectively recruited from the Alzheimer's Disease and Other Cognitive Disorders Unit, Hospital Clinic, Barcelona, Spain. All subjects underwent clinical and neuropsychological assessment and lumbar puncture. Subjects with a history of stroke or seizure, parkinsonism, epilepsy or other neurological disease were not included in the study. The study was approved by the Hospital Clinic's ethics committee, and all participants gave written informed consent to participate in the study. Controls were healthy elderly individuals who presented no evidence of cognitive impairment (below 1.5 standard deviation) in any of the neuropsychological tests administered, and had a Mini-Mental State Examination (MMSE) score between 24 and 30 and a Clinical Dementia Rating (CDR) scale score of 0. The AD patients were diagnosed with dementia according to the DSM-IV criteria for dementia [1] and met the criteria of probable AD, as defined by the NINCDS-ADRDA criteria [30]. They had a median MMSE score of 21, which indicates mild-to-moderate dementia. Patients with AD had a positive CSF biomarker profile with low levels of Aβ42 and increased levels of T-tau and P-tau (Aβ42 <450 pg/ml, T-tau >500 pg/ml and P-tau >75 pg/ml), while the controls displayed a negative profile. Demographics and clinical characteristics are given in table 1.
Table 1.
Clinical characteristics and comparisons of biomarker values between AD patients and controls
| AD | Controls | p values | |
|---|---|---|---|
| Age | 67.15 (59.90–74.31) | 60.56 (56.74–63.90) | |
| Gender, n (male/female) ApoE, % | 9/16 | 9/16 | |
| ε 2/3 | 4 | 4 | |
| ε 3/3 | 36 | 96 | |
| ε 3/4 | 48 | 0 | |
| ε 4/4 | 12 | 0 | |
| MMSE | 21.00 (18.00–24.00) | 29.00 (28.00–30.00) | |
| Chitotriosidase, nkat/l | 2.89 (1.39–3.84) | 1.24 (0.73–1.68) | 0.0007 |
| MCP-1, pg/ml | 613.00 (537.00–722.00) | 569.00 (474.00–645.00) | n.s. |
| YKL-40, ng/ml | 199,211.00 (165,877.00–25,572.00) | 112,631.00 (83,709.00–138,258.00) | <0.0001 |
| Aβ42, pg/ml | 326.00 (273.70–370.00) | 750.00 (663.92–851.10) | <0.0001 |
| T-tau, pg/ml | 873.50 (713.90–1,059.90) | 206.50 (155.89–240.66) | <0.0001 |
| P-tau, pg/ml | 121.70 (100.68–144.85) | 46.40 (40.50–59.00) | <0.0001 |
Values are medians with interquartile ranges in parentheses, except where otherwise indicated. ApoE = Apolipoprotein E; n.s. = not significant.
Biomarker Measurements
The chitotriosidase activity in CSF was measured using an enzymatic assay, as described previously [19,20]. MCP-1 levels in CSF were measured using the Meso Scale Discovery technique (MSD Human MCP-1; Meso Scale Discovery, Gaithersburg, Md., USA). Levels of YKL-40 were determined using a sandwich enzyme-linked immunosorbent assay (ELISA) (R&D Systems, Minneapolis, Minn., USA), which has been well validated in CSF [20,25,31,32]. CSF Aβ1-42 (called Aβ42 in this study) was quantified with a sandwich ELISA (Innotest β-amyloid1-42; Innogenetics, Ghent, Belgium) using a monoclonal antibody specific of the 42nd C-terminal amino acid on Aβ for capture and a biotinylated monoclonal antibody specific of the first five N-terminal amino acids for detection, as described previously in detail [33]. CSF levels of T-tau were determined with a sandwich ELISA using monoclonal capture antibodies (Innotest hTAU-Ag; Innogenetics), as presented previously [34]. Levels of tau phosphorylated at threonine 181 (P-tau) were measured with a sandwich ELISA (Innotest Phospho-Tau[181P]; Innogenetics), as described previously in detail [35].
All measurements were performed in one round of analyses using one batch of reagents by board-certified laboratory technicians who were blind to the clinical characteristics of patients and controls. Intra-assay coefficients of variation were below 10%.
Statistical Analyses
The software SAS version 9.3 (SAS Institute Inc., Cary, N.C., USA) was used for statistical analysis and graphs, together with GraphPad Prism 5 (GraphPad Software Inc., La Jolla, Calif., USA). Since data were skewed, group comparisons were made using the Mann-Whitney U test. Correlations were examined using Spearman rank correlation coefficient test. A p value <0.05 was considered statistically significant. Receiver operating characteristic (ROC) curves for the differentiation of AD patients and controls were constructed, and the area under the ROC curve (AUROC) was calculated for the individual markers.
Results
Biomarker Levels
Patients with AD had significantly higher CSF levels of chitotriosidase (133% increase) and YKL-40 (77% increase) compared with controls (table 1, fig. 1). Levels of MCP-1 were not significantly different between groups. The significant group differences for chitotriosidase and YKL-40 remained also when outliers were removed from the groups (data not shown).
Fig. 1.
Levels of chitotriosidase (a), YKL-40 (b) and MCP-1 (c) in AD patients and controls. Bars represent medians and interquartile ranges.
Correlations
Correlations between biomarkers, age and MMSE scores are shown in table 2. There were significant correlations between MCP-1 and YKL-40 in both AD patients and controls (r = 0.53, p < 0.01 and r = 0.64, p < 0.01, respectively). No biomarker, except for T-tau in controls (r = 0.40, p < 0.05), correlated significantly with age. In addition, no biomarker correlated with MMSE score.
Table 2.
Correlations between biomarkers, gender and age
| AD | Controls |
|||||||
|---|---|---|---|---|---|---|---|---|
| T-tau | P-tau | Aβ42 | MCP-1 | chitotriosidase | YKL-40 | MMSE | age | |
| T-tau | 0.75c | 0.58b | 0.17 | 0.18 | 0.31 | 0.13 | 0.40a | |
| P-tau | 0.82c | 0.74c | 0.19 | 0.21 | 0.34 | 0.24 | 0.09 | |
| Aβ42 | 0.35 | 0.26 | 0.15 | 0.26 | 0.15 | 0.19 | 0.02 | |
| MCP-1 | 0.00 | 0.17 | 0.11 | 0.06 | 0.64b | −0.26 | 0.31 | |
| Chitotriosidase | 0.33 | 0.29 | 0.06 | 0.21 | 0.21 | 0.33 | 0.25 | |
| YKL-40 | 0.12 | 0.10 | 0.36 | 0.53b | 0.22 | −0.07 | 0.25 | |
| MMSE | −0.08 | 0.09 | −0.13 | 0.33 | 0.09 | −0.18 | −0.60b | |
| Age | −0.39 | −0.24 | 0.09 | 0.24 | 0.15 | 0.27 | 0.18 | |
p < 0.05
p < 0.01
p < 0.0001.
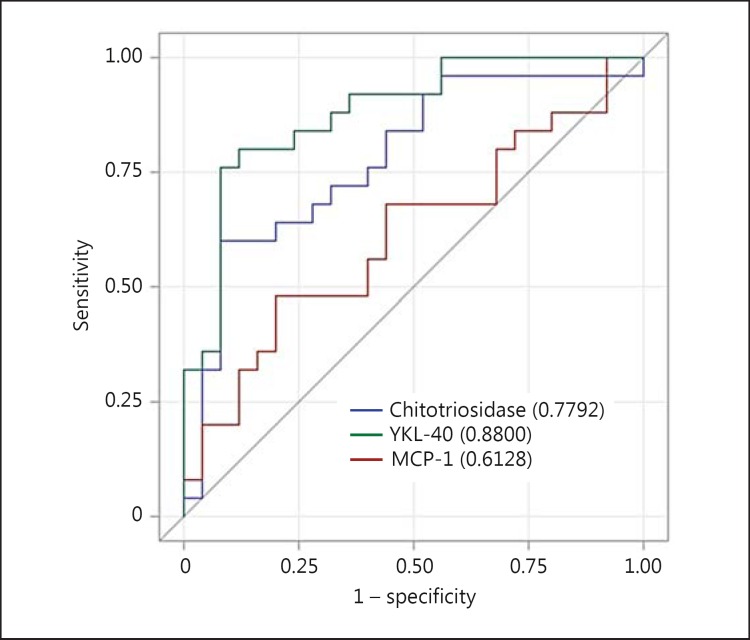
ROC Analysis
ROC plots for the biomarkers are shown in figure 2. The AUROC was 0.78 [95% confidence interval (CI) 0.65-0.91] for chitotriosidase, 0.88 (95% CI 0.78-0.98) for YKL-40 and 0.61 (95% CI 0.45-0.77) for MCP-1 for discriminating AD patients from controls.
Fig. 2.
ROC curves of the inflammatory biomarkers for the differentiation between AD patients and controls.
Discussion
Today, there are three CSF biomarkers, T-tau, P-tau and Aβ42, which have proven to be strongly associated with AD [4]. New biomarkers are important to improve the diagnosis and prediction as well as follow-up of AD patients. In this study, we evaluated inflammatory CSF biomarkers and found that patients with AD had higher levels of chitotriosidase and YKL-40 compared with controls, while the levels of MCP-1 were similar between the groups.
We confirmed earlier reported differences in CSF chitotriosidase levels between AD patients and controls [20,21]. Even though there was an overlap in the biomarker levels between the groups, it was not as prominent as could be seen in one of the previous studies [20]. This is most likely due to the fact that in the present study, patients were included if having a positive CSF AD biomarker profile, which increases the certainty of including patients with AD pathology in the AD group and excluding patients with this pathology in the control group. This gives more reliable and biologically relevant results. The approach of biomarker-supported AD diagnostics is also in line with recently proposed revised criteria for AD [28].
Similar reasoning applies to studies of YKL-40. Two previous studies report elevated CSF levels of YKL-40 in AD patients in early disease stages [24,36]. In both of these studies, Aβ42 and T-tau were used for selecting patients. Another study found elevated levels in AD patients but not in MCI patients with incipient AD [25]. However, upon stratification according to an AD-indicative profile of Aβ42 and T-tau, higher levels of YKL-40 were found in MCI patients who developed AD, compared with stable MCI patients with a normal profile. We corroborate these findings by presenting elevated YKL-40 levels in AD patients. In another study in which biomarker criteria were not applied in the selection of patients, no differences in YKL-40 levels were found between AD patients and controls [20]. Here, YKL-40 achieved an acceptable AUROC of 0.88.
The findings of unaltered MCP-1 levels in AD patients compared with controls are in line with some earlier findings [20], while other studies have found increased levels in AD patients [26,27]. Further studies are needed to clarify these discrepancies. A potential confounding factor may be the age of the participants. One study found that AD patients had increased levels of MCP-1 compared with controls, but that the levels correlated with age, and the subjects in the AD group were older than the controls [37]. Moreover, when comparing different methods for MCP-1, suboptimal correlations have been seen [20]. This could either be an indication that the methods detect different fragments of the protein or that there is a need for harmonization of MCP-1 methods. Thus, the divergent results across studies may depend on assay selection.
No inflammatory biomarker correlated with MMSE. The AD patients were older than the controls. However, this probably had no major effect on the results, since no inflammatory biomarker correlated with age. There were no correlations between inflammatory and core AD biomarkers, which indicates that they can provide independent information.
One shortcoming of the study was that only patients with AD were included in the disease group. Hence, we cannot determine the ability of these biomarkers to discriminate AD from other neurodegenerative diseases.
Conclusion
Patients with AD had higher CSF levels of the inflammatory biomarkers chitotriosidase and YKL-40 compared with controls, while the levels of MCP-1 were similar between the groups. These findings indicate that chitotriosidase and YKL-40 may be used for evaluating inflammatory activity in AD patients.
Acknowledgements
This is an EU Joint Programme – Neurodegenerative Disease Research (JPND) project (www.jpnd.eu< http://www.jpnd.eu/>). The project is supported through the ISCIII (PI11/03023 to J.L.M.) under the aegis of the JPND. We also gratefully acknowledge the support of the Swedish Research Council, the Alzheimer's Association, the Knut and Alice Wallenberg Foundation and the Leonard Wolfson Experimental Neurology Centre. We thank Dzemila Secic, Monica Christiansson, Åsa Källén and Sara Hullberg for their excellent technical assistance.
References
- 1.Blennow K, de Leon MJ, Zetterberg H. Alzheimer's disease. Lancet. 2006;368:387–403. doi: 10.1016/S0140-6736(06)69113-7. [DOI] [PubMed] [Google Scholar]
- 2.Braak H, Braak E. Diagnostic criteria for neuropathologic assessment of Alzheimer's disease. Neurobiol Aging. 1997;18:S85–S88. doi: 10.1016/s0197-4580(97)00062-6. [DOI] [PubMed] [Google Scholar]
- 3.Mattsson N, Zetterberg H, Hansson O, Andreasen N, Parnetti L, Jonsson M, Herukka SK, van der Flier WM, Blankenstein MA, Ewers M, Rich K, Kaiser E, Verbeek M, Tsolaki M, Mulugeta E, Rosen E, Aarsland D, Visser PJ, Schroder J, Marcusson J, de Leon M, Hampel H, Scheltens P, Pirttila T, Wallin A, Jonhagen ME, Minthon L, Winblad B, Blennow K. CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA. 2009;302:385–393. doi: 10.1001/jama.2009.1064. [DOI] [PubMed] [Google Scholar]
- 4.Blennow K, Hampel H, Weiner M, Zetterberg H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol. 2010;6:131–144. doi: 10.1038/nrneurol.2010.4. [DOI] [PubMed] [Google Scholar]
- 5.Rosen C, Hansson O, Blennow K, Zetterberg H. Fluid biomarkers in Alzheimer's disease – current concepts. Mol Neurodegener. 2013;8:20. doi: 10.1186/1750-1326-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011;7:263–269. doi: 10.1016/j.jalz.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heneka MT. Inflammation in Alzheimer's disease. Clin Neurosci Res. 2006;6:247–260. [Google Scholar]
- 8.Breitner JC, Welsh KA, Helms MJ, Gaskell PC, Gau BA, Roses AD, Pericak-Vance MA, Saunders AM. Delayed onset of Alzheimer's disease with nonsteroidal anti-inflammatory and histamine H2 blocking drugs. Neurobiol Aging. 1995;16:523–530. doi: 10.1016/0197-4580(95)00049-k. [DOI] [PubMed] [Google Scholar]
- 9.Breitner JC, Gau BA, Welsh KA, Plassman BL, McDonald WM, Helms MJ, Anthony JC. Inverse association of anti-inflammatory treatments and Alzheimer's disease: initial results of a co-twin control study. Neurology. 1994;44:227–232. doi: 10.1212/wnl.44.2.227. [DOI] [PubMed] [Google Scholar]
- 10.Wisniewski HM, Wegiel J, Wang KC, Lach B. Ultrastructural studies of the cells forming amyloid in the cortical vessel wall in Alzheimer's disease. Acta Neuropathol. 1992;84:117–127. doi: 10.1007/BF00311383. [DOI] [PubMed] [Google Scholar]
- 11.Wisniewski HM, Wegiel J. Spatial relationships between astrocytes and classical plaque components. Neurobiol Aging. 1991;12:593–600. doi: 10.1016/0197-4580(91)90091-w. [DOI] [PubMed] [Google Scholar]
- 12.Lee CY, Landreth GE. The role of microglia in amyloid clearance from the AD brain. J Neural Transm. 2010;117:949–960. doi: 10.1007/s00702-010-0433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perlmutter LS, Barron E, Chui HC. Morphologic association between microglia and senile plaque amyloid in Alzheimer's disease. Neurosci Lett. 1990;119:32–36. doi: 10.1016/0304-3940(90)90748-x. [DOI] [PubMed] [Google Scholar]
- 14.Frackowiak J, Wisniewski HM, Wegiel J, Merz GS, Iqbal K, Wang KC. Ultrastructure of the microglia that phagocytose amyloid and the microglia that produce beta-amyloid fibrils. Acta Neuropathol. 1992;84:225–233. doi: 10.1007/BF00227813. [DOI] [PubMed] [Google Scholar]
- 15.Neniskyte U, Neher JJ, Brown GC. Neuronal death induced by nanomolar amyloid beta is mediated by primary phagocytosis of neurons by microglia. J Biol Chem. 2011;286:39904–39913. doi: 10.1074/jbc.M111.267583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.von Bernhardi R, Eugenin J. Microglial reactivity to beta-amyloid is modulated by astrocytes and proinflammatory factors. Brain Res. 2004;1025:186–193. doi: 10.1016/j.brainres.2004.07.084. [DOI] [PubMed] [Google Scholar]
- 17.Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, Cruchaga C, Sassi C, Kauwe JS, Younkin S, Hazrati L, Collinge J, Pocock J, Lashley T, Williams J, Lambert JC, Amouyel P, Goate A, Rademakers R, Morgan K, Powell J, St George-Hyslop P, Singleton A, Hardy J. TREM2 variants in Alzheimer's disease. N Engl J Med. 2013;368:117–127. doi: 10.1056/NEJMoa1211851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, Bjornsson S, Huttenlocher J, Levey AI, Lah JJ, Rujescu D, Hampel H, Giegling I, Andreassen OA, Engedal K, Ulstein I, Djurovic S, Ibrahim-Verbaas C, Hofman A, Ikram MA, van Duijn CM, Thorsteinsdottir U, Kong A, Stefansson K. Variant of TREM2 associated with the risk of Alzheimer's disease. N Engl J Med. 2013;368:107–116. doi: 10.1056/NEJMoa1211103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hollak CE, van Weely S, van Oers MH, Aerts JM. Marked elevation of plasma chitotriosidase activity. A novel hallmark of Gaucher disease. J Clin Invest. 1994;93:1288–1292. doi: 10.1172/JCI117084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mattsson N, Tabatabaei S, Johansson P, Hansson O, Andreasson U, Mansson JE, Johansson JO, Olsson B, Wallin A, Svensson J, Blennow K, Zetterberg H. Cerebrospinal fluid microglial markers in Alzheimer's disease: elevated chitotriosidase activity but lack of diagnostic utility. Neuromolecular Med. 2011;13:151–159. doi: 10.1007/s12017-011-8147-9. [DOI] [PubMed] [Google Scholar]
- 21.Watabe-Rudolph M, Song Z, Lausser L, Schnack C, Begus-Nahrmann Y, Scheithauer MO, Rettinger G, Otto M, Tumani H, Thal DR, Attems J, Jellinger KA, Kestler HA, von Arnim CA, Rudolph KL. Chitinase enzyme activity in CSF is a powerful biomarker of Alzheimer disease. Neurology. 2012;78:569–577. doi: 10.1212/WNL.0b013e318247caa1. [DOI] [PubMed] [Google Scholar]
- 22.Hakala BE, White C, Recklies AD. Human cartilage gp-39, a major secretory product of articular chondrocytes and synovial cells, is a mammalian member of a chitinase protein family. J Biol Chem. 1993;268:25803–25810. [PubMed] [Google Scholar]
- 23.Bonneh-Barkay D, Wang G, Starkey A, Hamilton RL, Wiley CA. In vivo CHI3L1 (YKL-40) expression in astrocytes in acute and chronic neurological diseases. J Neuroinflammation. 2010;7:34. doi: 10.1186/1742-2094-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craig-Schapiro R, Perrin RJ, Roe CM, Xiong C, Carter D, Cairns NJ, Mintun MA, Peskind ER, Li G, Galasko DR, Clark CM, Quinn JF, D'Angelo G, Malone JP, Townsend RR, Morris JC, Fagan AM, Holtzman DM. YKL-40: a novel prognostic fluid biomarker for preclinical Alzheimer's disease. Biol Psychiatry. 2010;68:903–912. doi: 10.1016/j.biopsych.2010.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Olsson B, Hertze J, Lautner R, Zetterberg H, Nagga K, Hoglund K, Basun H, Annas P, Lannfelt L, Andreasen N, Minthon L, Blennow K, Hansson O. Microglial markers are elevated in the prodromal phase of Alzheimer's disease and vascular dementia. J Alzheimers Dis. 2013;33:45–53. doi: 10.3233/JAD-2012-120787. [DOI] [PubMed] [Google Scholar]
- 26.Galimberti D, Schoonenboom N, Scheltens P, Fenoglio C, Bouwman F, Venturelli E, Guidi I, Blankenstein MA, Bresolin N, Scarpini E. Intrathecal chemokine synthesis in mild cognitive impairment and Alzheimer disease. Arch Neurol. 2006;63:538–543. doi: 10.1001/archneur.63.4.538. [DOI] [PubMed] [Google Scholar]
- 27.Correa JD, Starling D, Teixeira AL, Caramelli P, Silva TA. Chemokines in CSF of Alzheimer's disease patients. Arq Neuropsiquiatr. 2011;69:455–459. doi: 10.1590/s0004-282x2011000400009. [DOI] [PubMed] [Google Scholar]
- 28.Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, Delacourte A, Frisoni G, Fox NC, Galasko D, Gauthier S, Hampel H, Jicha GA, Meguro K, O'Brien J, Pasquier F, Robert P, Rossor M, Salloway S, Sarazin M, de Souza LC, Stern Y, Visser PJ, Scheltens P. Revising the definition of Alzheimer's disease: a new lexicon. Lancet Neurol. 2010;9:1118–1127. doi: 10.1016/S1474-4422(10)70223-4. [DOI] [PubMed] [Google Scholar]
- 29.DSM-III-R. ed 3. Washington: American Psychiatric Association; 1987. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 30.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ASRSA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 31.Malmestrom C, Axelsson M, Lycke J, Zetterberg H, Blennow K, Olsson B. CSF levels of YKL-40 are increased in MS and replaces with immunosuppressive treatment. J Neuroimmunol. 2014;269:87–89. doi: 10.1016/j.jneuroim.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 32.Rosen C, Rosen H, Andreasson U, Bremell D, Bremler R, Hagberg L, Rosengren L, Blennow K, Zetterberg H. Cerebrospinal fluid biomarkers in cardiac arrest survivors. Resuscitation. 2014;85:227–232. doi: 10.1016/j.resuscitation.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 33.Vanderstichele H, Van Kerschaver E, Hesse C, Davidsson P, Buyse MA, Andreasen N, Minthon L, Wallin A, Blennow K, Vanmechelen E. Standardization of measurement of beta-amyloid(1-42) in cerebrospinal fluid and plasma. Amyloid. 2000;7:245–258. doi: 10.3109/13506120009146438. [DOI] [PubMed] [Google Scholar]
- 34.Blennow K, Wallin A, Agren H, Spenger C, Siegfried J, Vanmechelen E. Tau protein in cerebrospinal fluid: a biochemical marker for axonal degeneration in Alzheimer disease? Mol Chem Neuropathol. 1995;26:231–245. doi: 10.1007/BF02815140. [DOI] [PubMed] [Google Scholar]
- 35.Vanmechelen E, Vanderstichele H, Davidsson P, Van Kerschaver E, Van Der Perre B, Sjogren M, Andreasen N, Blennow K. Quantification of tau phosphorylated at threonine 181 in human cerebrospinal fluid: a sandwich ELISA with a synthetic phosphopeptide for standardization. Neurosci Lett. 2000;285:49–52. doi: 10.1016/s0304-3940(00)01036-3. [DOI] [PubMed] [Google Scholar]
- 36.Perrin RJ, Craig-Schapiro R, Malone JP, Shah AR, Gilmore P, Davis AE, Roe CM, Peskind ER, Li G, Galasko DR, Clark CM, Quinn JF, Kaye JA, Morris JC, Holtzman DM, Townsend RR, Fagan AM. Identification and validation of novel cerebrospinal fluid biomarkers for staging early Alzheimer's disease. PloS One. 2011;6:e16032. doi: 10.1371/journal.pone.0016032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blasko I, Lederer W, Oberbauer H, Walch T, Kemmler G, Hinterhuber H, Marksteiner J, Humpel C. Measurement of thirteen biological markers in CSF of patients with Alzheimer's disease and other dementias. Dement Geriatr Cogn Disord. 2006;21:9–15. doi: 10.1159/000089137. [DOI] [PubMed] [Google Scholar]