Abstract
Varicose veins in the vulvar and peri-vulvar area are seen in 4% of women and most commonly seen during pregnancy. It is thought to be as a direct result of the presence of ovarian and pelvic varicosities. Diagnostic modalities used in the investigation of this condition included pelvic ultrasound, computed venography, magnetic resonance venography and catheter-directed venography. The treatment options in the past were hysterectomy and/or ligation of ovarian veins by open or laparoscopic approach. Modern techniques involve embolization of the varicosity via radiological techniques. In this case the patient presented with vulval and upper thigh varices associated with pelvic pain. They were located to be from the superficial external pudendal vein, which is not a common source but worth considering with other causes. They were treated successfully with fluoroscopy-guided embolization.
CASE REPORT
A 44-year-old fit and well female presented to the vascular clinic with symptoms of pain radiating down the right leg with an associated sensation of pelvic heaviness. The symptoms were worse at the end of day. On examination she had prominent veins in the upper and inner thigh extending up to the vulva where obvious varicosities were present. The symptoms and signs were consistent with a diagnosis of pelvic congestion syndrome (PCS).
Initial investigations included duplex scan, followed by magnetic resonance scan. Duplex scanning demonstrated a competent sapheno-femoral (SFJ) and Sapheno-popliteal (SPJ) junctions bilaterally; however, did raise suspicion of a pelvic origin of the vulval varices with congested pelvic veins. Magnetic resonance venogram aided the diagnosis by demonstrating the communication of the vulval varices to the upper thigh veins with contribution from the internal iliac vein. In this case there was no evidence of ovarian varices (Fig. 1). Catheter venography was unable to confirm the contributing vein with certainty but computed pelvic venography showed a likely connection through the superficial external pudendal vein (Fig. 2).
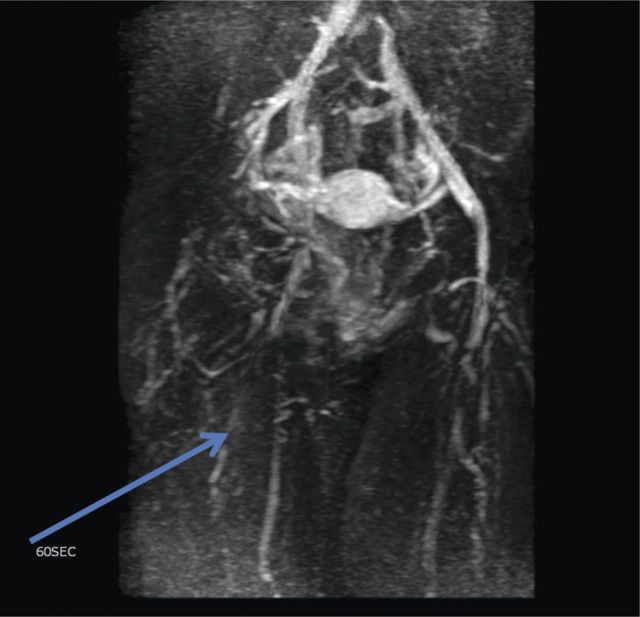
Figure 1:
Magnetic resonance venogram showing communication of thigh veins to vulval varices (blue arrow).
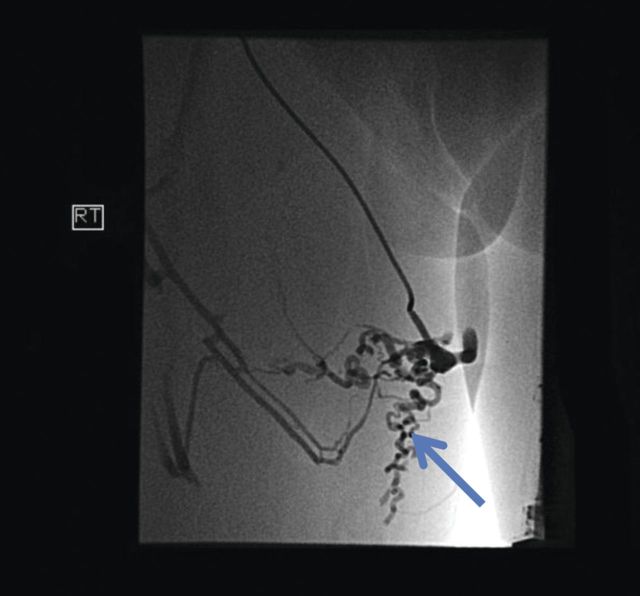
Figure 2:
Computed pelvic venography showing communication of thigh veins to vulval varices (blue arrow).
This was an atypical presentation of PCS as the source of vulval varices was not associated with ovarian varices. However, discussion at the multidisciplinary team meeting concluded that with the patient's symptoms, the vulval varices and a likely origin from the superficial external pudendal vein, radiological embolization was an appropriate treatment option.
The superficial external pudendal vein was embolized with 1% sodium tetradecyl sulphate and then coiled through a contralateral puncture under fluoroscopic guidance (Figs 3 and 4). The procedure went uneventfully with successful obliteration of the communicating thigh veins to vulval varices (Fig. 5) and the patient was discharged home the same day.
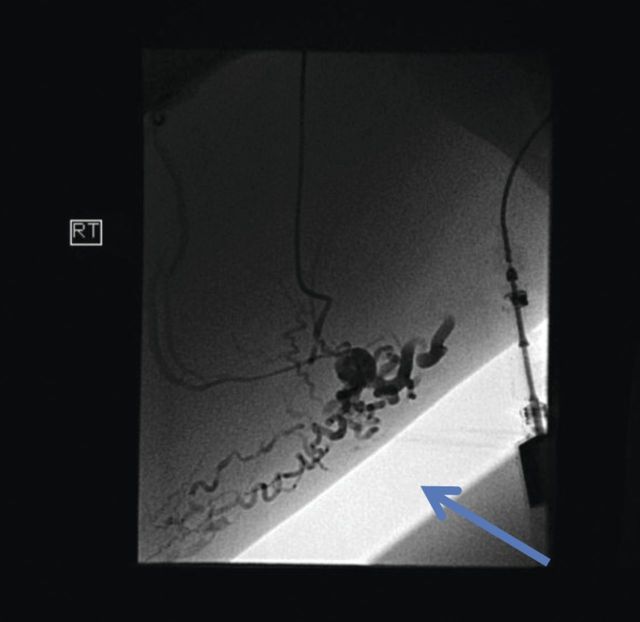
Figure 3:
Pre-embolization fluoroscopy showing communication of thigh veins to vulval varices (blue arrow).
Figure 4:
Pre-embolization fluoroscopy showing communication of thigh veins to vulval varices (blue arrow).
Figure 5:
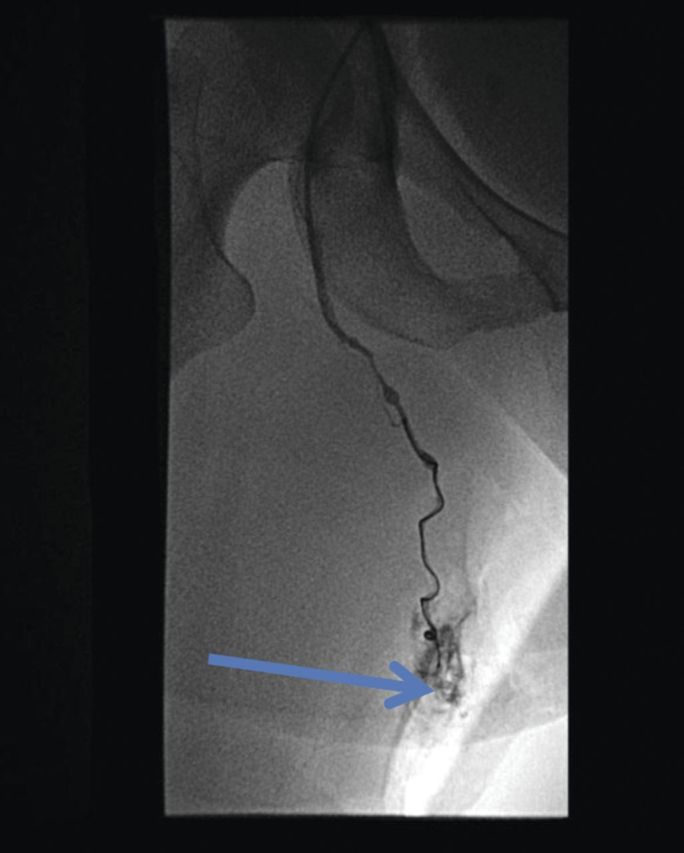
Post-procedure fluoroscopy showing successful obliteration of communication of thigh veins to vulval varices (blue arrow).
The patient was reviewed in clinic at 2 months post-procedure and was found to be symptom free and very satisfied with the outcome of the procedure.
DISCUSSION
Varicose veins in the vulvar and peri-vulvar area are seen in 4% of women [1]. Varicose veins of the vulva are most commonly seen during pregnancy. They usually appear during the third or fourth month of gestation and regress spontaneously after delivery. Vulvar varicose veins are rare in non-pregnant women. When present, they can be seen alone, associated with leg varices, or associated with venous malformations of the labia, clitoral area or vagina. In this case the patient presented with vulval and upper thigh varices associated with pelvic heaviness and pain radiating down the leg.
The association of varices plus chronic pelvic pain can be secondary to PCS [2]. PCS was originally described by Gooch in 1831 [3]. It is thought to be as a direct result of the presence of ovarian and pelvic varicosities. There are no specific diagnostic criteria for PCS; however, there are characteristic findings on radiological imaging. Assessed on venography, specific findings include an ovarian vein diameter of >10 mm along with congestion of the ovarian plexus [4]. The reflux of blood and dilatation of the veins is due to an absence of functioning valves, particularly in the ovarian veins. However, there are other veins that can be responsible for vulval varicosities. In this case a rare finding of varicosity originating from the superficial external pudendal vein was present.
Diagnostic modalities used in the investigation of this condition include pelvic ultrasound (transabdominal and transvaginal), computed venography, magnetic resonance venography and catheter-directed venography. Catheter venography is invasive and is used to confirm the diagnosis immediately before embolization.
The traditional treatment for PCS was hysterectomy and/or ligation of the ovarian veins. This has since been replaced with laparoscopic ligation of the ovarian veins. However, this approach can result in transaction of the nerves to the pelvis and still leave the possibility of establishing collateral channels resulting in symptomatic recurrence [5, 6].
The most commonly performed technique now is embolization of the responsible veins using interventional radiology. The technique was described by Edwards in 1993 and has gained popularity by both clinicians and patients since [7]. Transcatheter embolotherapy is now the preferred treatment for PCS. This is performed with a combination of sclerosant foam and/or coils to embolize the source veins. Clinical success is achieved in 70–85% of treated patients [8–10].
In this case the more traditional approach of hysterectomy or ligation of the ovarian veins would not have provided a curative treatment as the origin of varicosities causing PCS was the superficial external pudendal vein. Therefore, it was imperative to gain detailed imaging and target embolization. The option of sapheno-femoral ligation along with disruption of tributaries including superficial external pudendal vein was considered. However, there would be a high chance of persistence of symptoms as communicating veins may have been left unaddressed. Due to which in this case the selective embolization of the superficial external pudendal vein lead to treatment success.
CONSENT
The authors obtain written informed consent from the patient for submission of this manuscript for publication.
CONFLICT OF INTEREST STATEMENT
The authors declare that they do not have any competing interests.
ACKNOWLEDGEMENT
Andrew Hughes, radiographer, at Queen Elizabeth Hospital who helped provision of images after removing the patient's details.
REFERENCES
- 1.Bell D, Kane PB, Liang S, Conway C, Tornos C. Vulvar varices: an uncommon entity in surgical pathology. Int J Gynecol Pathol. 2007;26:99–101. doi: 10.1097/01.pgp.0000215304.62771.19. [DOI] [PubMed] [Google Scholar]
- 2.Smith OC. The outcome of treatment for pelvic congestion syndrome. Phlebology. 2012;27(Suppl 1):74–7. doi: 10.1258/phleb.2011.012s01. [DOI] [PubMed] [Google Scholar]
- 3.Gooch R. In: An Account of Some of the Most Important Diseases Peculiar to Women. Murray J, editor. London: Murray: 1831: 1829. [Google Scholar]
- 4.Geier B, Barbera L, Mumme A, Köster O, Marpea B, Kaminsky C, et al. Reflux patterns in the ovarian and hypogastric veins in patients with varicose veins and signs of pelvic venous incompetence. Chir Ital. 2007;59:481–8. [PubMed] [Google Scholar]
- 5.Chronic Pelvic Pain: An Integrated Approach Monograph. Educational Series on Women's Health Issues. Interdisciplinary Women's Health Education Retreat 2000. Washington, DC: Association of Professors of Gynecology and Obstetrics APGO. Chronic Pelvic Pain; 2000. [Google Scholar]
- 6.Rundqvist E, Sandholm LE, Larsson G. Treatment of pelvic varicosities causing lower abdominal pain with extraperitoneal resolution of left ovarian vein. Ann Chir Gynaecol. 1984;73:339–41. [PubMed] [Google Scholar]
- 7.Edwards RD, Robertson JR, MacLean AB, Hemmingway AP. Case report: pelvic pain syndrome—successful treatment of a case by ovarian vein embolization. Clin Radiol. 1993;47:429–31. doi: 10.1016/s0009-9260(05)81067-0. [DOI] [PubMed] [Google Scholar]
- 8.Venbrux AC, Chang AH, Kim HS, Montague BJ, Hebert JB, Arepally A, et al. Pelvic congestion syndrome (pelvic venous incompetence): impact of ovarian and internal iliac vein embolotherapy on menstrual cycle and chronic pelvic pain. J Vasc Interv Radiol. 2002;13(Pt1):171–8. doi: 10.1016/s1051-0443(07)61935-6. [DOI] [PubMed] [Google Scholar]
- 9.Kim HS, Malhotra AD, Rowe PC, Lee JM, Venbrux AC. Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Interv Radiol. 2006;17:289–97. doi: 10.1097/01.RVI.0000194870.11980.F8. [DOI] [PubMed] [Google Scholar]
- 10.Maleux G, Stockx L, Wilms G, Marchal G. Ovarian vein embolization for the treatment of pelvic congestion syndrome: long term technical and clinical results. J Vasc Interv Radiol. 2000;11:859–64. doi: 10.1016/s1051-0443(07)61801-6. [DOI] [PubMed] [Google Scholar]