Abstract
Background
Most programs addressing psychosocial concerns of cancer survivors are in-person programs that are expensive to deliver, have limited availability, and seldom deal with caregivers’ concerns.
Objective
This study examined the feasibility of translating an efficacious nurse-delivered program (FOCUS Program) for patients and their caregivers to a tailored, dyadic web-based format. Specific aims were to: (i) test the preliminary effects of the web-based intervention on patient and caregiver outcomes, (ii) examine participants’ program satisfaction, and (iii) determine the feasibility of using a web-based delivery format.
Intervention/Methods
A Phase II feasibility study was conducted with cancer patients (lung, breast, colorectal, prostate) and their family caregivers (N=38 dyads). The web-based intervention provided information and support tailored to the unique characteristics of each patient, caregiver, and their dyadic relationship. Primary outcomes were emotional distress and quality of life (QOL). Secondary outcomes were benefits of illness/caregiving, communication, support, and self-efficacy. Analyses included descriptive statistics and repeated measures ANOVA.
Results
Dyads had a significant decrease in emotional distress, increase in QOL, and perceived more benefits of illness/caregiving. Caregivers also had significant improvement in self-efficacy. There were no changes in communication. Participants were satisfied with program usability, but recommended additional content.
Conclusions
It was possible to translate a clinician-delivered program to a web-based format that was easy to use and had positive effects on dyadic outcomes.
Implications for Practice
The web-based program is a promising way to provide psychosocial care to more patients and caregivers using fewer personnel. It needs further testing in a larger RCT.
Introduction
There are over 13 million cancer survivors in the U.S. whose needs for psychosocial care are not being met 1,2. Although some evidence-based programs address their emotional concerns and quality of life, most programs are expensive to deliver, not broadly available, and seldom target the shared concerns of both patients and their family caregivers. As use of the Internet increases across broad segments of the U.S. population, it has become a viable and cost effective approach for delivering programs to large numbers of cancer patients and their family caregivers 3,4.
The Internet has been used to deliver interventions to cancer patients alone 5–10, but it has seldom been used to deliver interventions to patients and their family caregivers as the unit of care 11,12. Family caregivers often report as much emotional distress as patients but receive little support from others 13. Since cancer patients’ and their family caregivers’ responses to illness are significantly related 14,15, intervening with them as a dyad (i.e., pair) helps both of them to manage cancer-related stress, improve their communication and support, and maintain their quality of life 16–18. There is a critical need for more dyadic intervention research with cancer patients and their family caregivers that uses the Internet to provide them both with education and support.
Cancer patients who participated in previous web-based interventions reported better outcomes than controls such as higher health status 6, support 5, sexual function 12, and QOL 5,10, as well as lower fatigue 7,10, insomnia 7, global symptom distress 8 anxiety 10 , and depression 9. Caregivers in the few web-based studies that have been conducted with them reported an increase in sexual function/satisfaction 12 and less caregiver burden and negative mood 19. These studies have laid important groundwork, but more web-based interventions are needed that target patient-caregiver dyads, use tailored messages to increase the relevance of intervention content to participants 4, and assess participants’ satisfaction with the web-based intervention.
The purpose of this study was to examine the feasibility of translating an efficacious nurse-delivered, psycho-educational program for cancer patients and their caregivers to a tailored, web-based delivery format. The original in-person program (i.e., FOCUS Program) was tested in three prior randomized clinical trials (RCTs) 20–22. Although the program had positive outcomes for both patients and their family caregivers, home-based, in-person programs are more expensive to deliver and reach fewer people than web-based programs. To make the FOCUS Program available to more people, we translated the central module of the program (i.e., Family Involvement Module) into a tailored, web-based delivery format (see Zulman 23 for details on the translation process) and tested the effect of the new web-based program on outcomes for patients and their caregivers.
The specific aims for this Phase II, pre- and post-intervention feasibility study were as follows: 1) to examine the preliminary effects of a tailored web-based program on primary outcomes (emotional distress, QOL) and secondary outcomes (benefits of illness/caregiving, communication, social support, self-efficacy) for patients and caregivers as dyads from pre- to post-intervention, 2) to evaluate patients’ and caregivers’ satisfaction with the web-based program, and 3) to determine the feasibility of using a web-based format to deliver the original nurse-delivered FOCUS Program based on enrollment and retention rates and preliminary estimates of effect size.
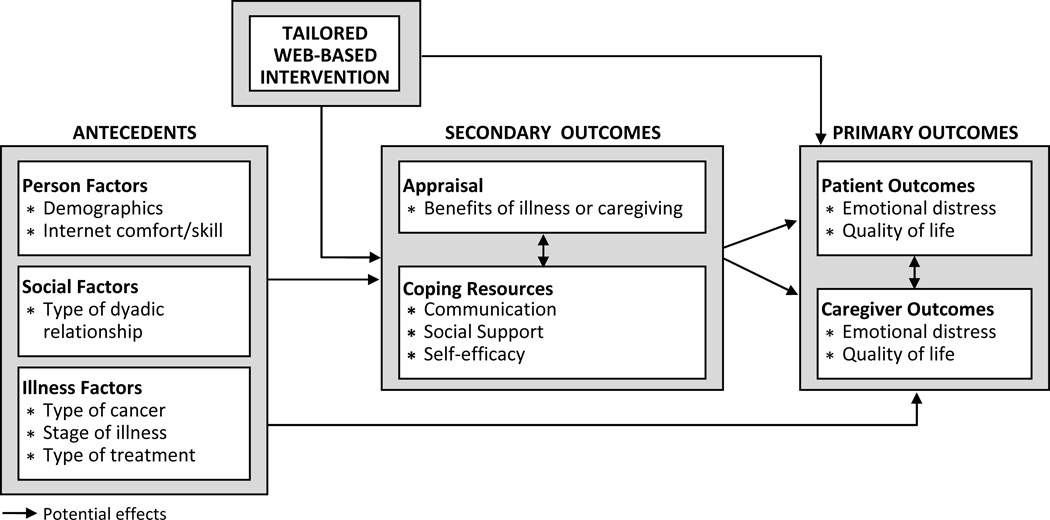
Stress-coping theory 24 guided the study and selection of the variables measured (see Figure 1). We hypothesized that the tailored, web-based intervention would 1) decrease patients’ and caregivers’ (i.e., dyads’) emotional distress and increase their quality of life (primary outcomes), and 2) improve their positive appraisals (i.e., increase perceived benefits of illness/caregiving) and coping resources (i.e., communication, support, and self-efficacy) (secondary outcomes).
Figure 1.
Theoretical framework and study variables
Methods
Participants
When we tested the effects of our original nurse-delivered, face-to-face FOCUS Program, we found that it was efficacious for patients and caregivers managing one of the four major types of cancer (lung, colorectal, breast, prostate) and also for patients with newly diagnosed and advanced disease20–22 . Based on those findings, we chose a sample for this feasibility study that was composed of patients with the same types and stages of cancer as in our prior efficacy trials.
Patient eligibility included: age 18 or older; diagnosed with lung, colorectal, breast, or prostate cancer; and with either early (Stage I or II) or advanced (Stage III or IV) cancer. Patients with early stage disease had to be diagnosed within 2 to 12 months prior to enrollment; and patients with advanced stage disease had to be diagnosed with metastatic cancer or with further progression of their cancer within 2 to 12 months prior to enrollment. We established these narrow windows of eligibility to obtain dyads who were dealing with a change in the patient’s health status (i.e., new diagnosis or disease progression) and who were likely to benefit from the web-based psycho-educational intervention. Other patient criteria included having one family caregiver who was willing to participate in all phases of the study and having access to the Internet.
“Family caregiver” was the family member or significant other identified by the patient as his or her primary source of emotional and/or physical support during the current cancer experience. The caregiver had to be age 18 or older and willing to complete the web-based program with the patient. Family caregivers who were diagnosed with cancer in the previous year or receiving active treatment for cancer were excluded.
Power analysis was conducted to determine sample size for this feasibility study based on Cohen’s definitions of effect sizes 25 and we used computations by PASS software 26. The power analysis for repeated measures ANOVA (Time 1 versus Time 2) with a medium effect size based on our prior studies 21 and an alpha of .05 two-tailed, indicated that a sample of 38 dyads would provide 85% power for Aim 1.
Procedures
A pre- and post-intervention feasibility study was conducted to examine the feasibility of using a web-based format to deliver the FOCUS Program 27. Eligible patient-caregiver dyads were informed about the study by clinic staff at three cancer centers in the Midwest. Research staff contacted dyads who indicated an interest in the study. Those willing to participate signed a consent form approved by the Institutional Review Board at their cancer center. After obtaining their signed consents, each patient and caregiver was emailed a unique username and a temporary password prior to starting the study. They also received a link to the Time 1 (baseline) web-based questionnaires. After patients and caregivers completed their questionnaires separately, they received an email asking them to start the web-based program together. After each session, a tailored email was sent that summarized and reinforced key content. Two weeks after finishing all three sessions, participants received an email asking them to complete Time 2 post-intervention questionnaires separately. Figure 2 illustrates the procedures for each week of the study. All participants received the intervention and there was no control group.
Figure 2.
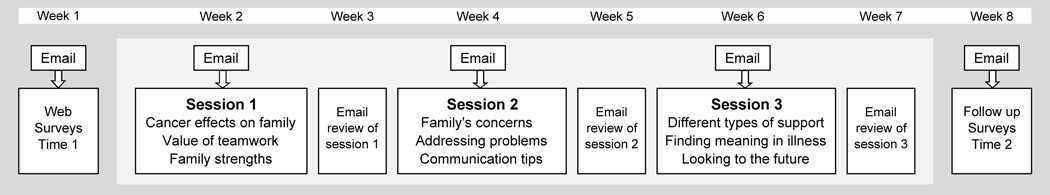
Study design and flow of intervention
Tailored Web-based Intervention
The web-based program was designed to create opportunities for patients and caregivers to obtain information and interact with one another as previous dyads experienced in the original face-to-face FOCUS Program delivered by nurses. The original FOCUS Program contained five modules that spelled the acronym FOCUS: family involvement, optimistic outlook, coping effectiveness, uncertainty reduction, and symptom management. For this feasibility study, we translated only the Family Involvement Module to the web-based format because it was considered to be the central module of the dyadic program that facilitated patients’ and caregivers’ communication, support, and ability to manage the demands associated with the illness.
The web-based program consisted of three sessions that were offered over a six week period, with each session two weeks apart to enable patient-caregiver dyads to learn information in a sequential manner, and to have practice time between sessions. Information presented in each web-based session is shown in Figure 2. Dyads logged on to the program and completed sessions together, sitting side-by-side at the computer, as instructed during enrollment. To keep program delivery costs at a minimum, we developed a self-managed program, rather than clinician-guided program. However, the program had a “Help” button that dyads could use at any time for help with any technical, personal, or dyad problems they encountered while completing the program. The “Help” button generated an email message which was sent to the project director (clinician). Dyads were also given the project director’s phone number and could call as needed.
Developing Tailored Messages
Our program used tailored messages to deliver program content. Tailoring enhances the efficacy of an intervention by providing participants with information that is personally relevant to them 28. Tailoring involves: 1) assessing participants at baseline using measures of key study variables and b) then constructing algorithms that use this assessment data to generate tailored messages that are geared to a specific person’s or dyad’s needs (e.g., need for more dyadic support)28 . Based on the information patients and caregivers provided at baseline and during the web-based sessions, they received tailored individual and dyadic messages according to their own demographic and medical characteristics (i.e., age, gender, race, type of dyad, type of cancer) to help personalize the intervention for them. They also received tailored messages according to their baseline scores on selected measures (i.e., benefits of illness/caregiving, communication, support, and self-efficacy) to enhance the relevance of the intervention message. For example, if a dyad scored low on dyadic support at baseline, they received tailored feedback during the intervention that suggested ways to increase their support to one another. Conversely, if they scored high on dyadic support at baseline, they received tailored messages that affirmed and encouraged them to continue the supportive nature of their relationship. Tailored messages in our program were written at an 8th grade reading level, using principles of plain language (i.e., easy to read and understand).
Selecting Tailoring Variables
The tailoring variables used for the study were measured with theoretically-grounded, validated measures of selected variables specified in our theoretical framework. Cut points on these measures, that determined if the person or dyad scored high or low on the particular instrument prior to intervention, were based on cut-points reported in the literature and on analysis of these variables in our prior RCTs.
Implementing Tailoring Strategies
Three tailoring strategies 29 were used to develop the web program: 1) personalization, 2) tailored feedback and 3) content matching (see Table 1). The program also provided participants with tailored links to other websites (e.g., National Alliance for Caregiving, Cancer Support Community) that addressed dyads’ specific concerns (e.g., finances, managing symptoms). Finally, dyads were offered a choice of tailored activities to complete between web sessions that were designed to promote dyadic interactions (e.g., plan night out together).
Table 1.
Example of Tailoring Strategies and Tailored Messages
| Strategy | Sample Message (tailored elements in bold) |
|---|---|
| Personalization | |
| Cancer type and dyad relationship |
When someone has prostate cancer it affects the whole family, especially the spouse When someone has breast cancer, it affects the whole family, includin the adult children. |
| Feedback | |
| High communication |
Compared to other married couples, you have strong communication. You share your feelings with each other and know how important it is to be open. |
| Low communication |
Talking about personal feelings is not easy for everyone. As you face cancer together, it may be important to find ways to let each other know how you are feeling. |
| Content-Matching | Example: communication barriers: You’ve told us that [barrier] is a challenge for you. You might be interested in some ways other couples managed this same issue. |
| Hiding feelings |
Sometimes it helps to start by sharing just one feeling. It can help to start slowly to “get practice” talking about how you feel. |
| Too critical |
Try to use “I” statements Say how you are feeling and try not to blame the other person. For example, say “I’m frustrated that the house is so messy,” instead of “You never clean up.” |
| Finding time |
Try making an “appointment” to talk to each other about important topics. Having a set time on the calendar can help especially when everyone feels so busy. |
Instruments
Validated instruments were used to assess major study variables. Internal consistency reliability alphas were assessed pre- and post-intervention for patients and caregivers.
Primary Outcomes
Emotional distress was measured with the 30-item Profile of Mood States (POMS)( short form), a self-report adjective rating scale that assesses six moods (Tension-Anxiety, Depression-Dejection, Anger-Hostility, Fatigue-Inertia, Confusion-Bewilderment, and Vigor-Activity) 30. This instrument has been used widely to assess affective states as an outcome of psychosocial interventions. The reliability estimates of the instrument using coefficient alpha ranged from 0.69 to 0.92 in this study. Higher total mood scores (with Vigor reversed) indicate higher mood disturbance or emotional distress. Quality of life (QOL) was measured with the Functional Assessment of Cancer Therapy (FACT-G version 4), a 27-item cancer-specific instrument that assesses QOL and four domains: emotional, social, functional, and physical well-being 31. Caregivers reported on their own QOL, using a slightly modified version of the FACT-G 13. The FACT-G, which has been used frequently in studies with cancer patients, has established validity 31 and demonstrated high internal consistency in our prior studies with cancer patients and their family caregivers 21, 22. The alpha coefficient for the total QOL score was 0.90 in this study and alpha coefficients for the subscales ranged from 0.71 to 0.83. Higher scores indicated better QOL.
Secondary Outcomes
Appraisal was measured with an 11-item, modified Benefits of Illness Scale 32 that assessed benefits arising from the illness or caregiving experience (e.g., “Having cancer has brought my family closer together”). The original scale was developed by Tomich and Helgeson who examined the psychometric properties of the scale and reported it was a unidimensional scale with high internal consistency 32. The alpha coefficient in this study was 0.92. Higher scores indicated more perceived benefits of illness/caregiving.
Coping resources were measured with three instruments with higher scores indicating more available resources. Communication was measured with the 23-item version of the Lewis Mutuality and Interpersonal Sensitivity Scale that assessed patients’ and caregivers’ degree of open communication and ability to share feelings about the illness (e.g., “We are comfortable sharing feelings about the cancer with each other”) 33. The original scale developed by Lewis, has established validity and demonstrated high internal consistency in our prior studies with patients and caregivers 21–22. The alpha reliability of the scale in this study was 0.93 33. Social support was measured with a 9-item, brief version of the Social Support Scale that assessed patients’ and caregivers’ perceived support from one another 34 (e.g., “My family supports me as I try to cope with the illness”). Evidence of concurrent validity and high internal consistency was reported with the original, longer version of the scale 34.The alpha reliability was 0.87 in the present study. Self-efficacy was assessed with the 17-item version Lewis Cancer Self-efficacy Scale that assessed patients’ and caregivers’ confidence about managing the illness 33 (e.g., “I am confident that I can use information and resources to cope with the demands of cancer”). Evidence of content and criterion validity of the original scale was reported by Lewis 33. The modified version of the scale demonstrated high internal consistency reliability in our prior studies 21–22. The alpha reliability coefficient in this study was 0.95.
Process Evaluation and Other Measures
Evaluation of participants’ satisfaction with the web-based program was based upon the Technology Acceptance Model 35–37. At Time 2 follow-up, we assessed three characteristics of the web intervention 1) perceived usefulness (e.g., I found the program useful), 2) perceived ease of use and usability (e.g., program ran smoothly) 38 and 3) satisfaction with overall experience. Subscale scores ranged from 1 (low) to 7 (high). Subscale reliability alphas ranged from .81-.96. Participants also were asked if there was any additional content they would add to the program.
Demographic characteristics (e.g., age, education, income, gender, race, dyadic relationship) and medical characteristics (e.g., type and stage of cancer) were also assessed at baseline (Time 1). Participants’ comfort and skill using computers and the Internet were also assessed (Time 1) with a 4-item, researcher-designed questionnaire (e.g., “I feel very comfortable using the Internet”). Higher scores indicated more comfort and/or skill using computers and/or the Internet (internal consistency reliability = .96).
Data Analyses
For Aim 1, repeated measures ANOVA was used to assess changes on study variables from Time 1 to 2, with time and role (patient and caregiver) as within-subject variables to control for the correlated nature of the data. We examined main effects of time (which assesses the overall effectiveness of the intervention for dyads), and also time by role interactions (which assesses differential effectiveness of the intervention between patients and caregivers). For Aim 2, descriptive statistics were used to describe and compare patients’ and caregivers’ ratings of their satisfaction with the web-based intervention. For Aim 3, descriptive statistics were used to examine enrollment and retention rates and effect size estimates (d) were calculated for patients and caregivers.
Results
Sample description
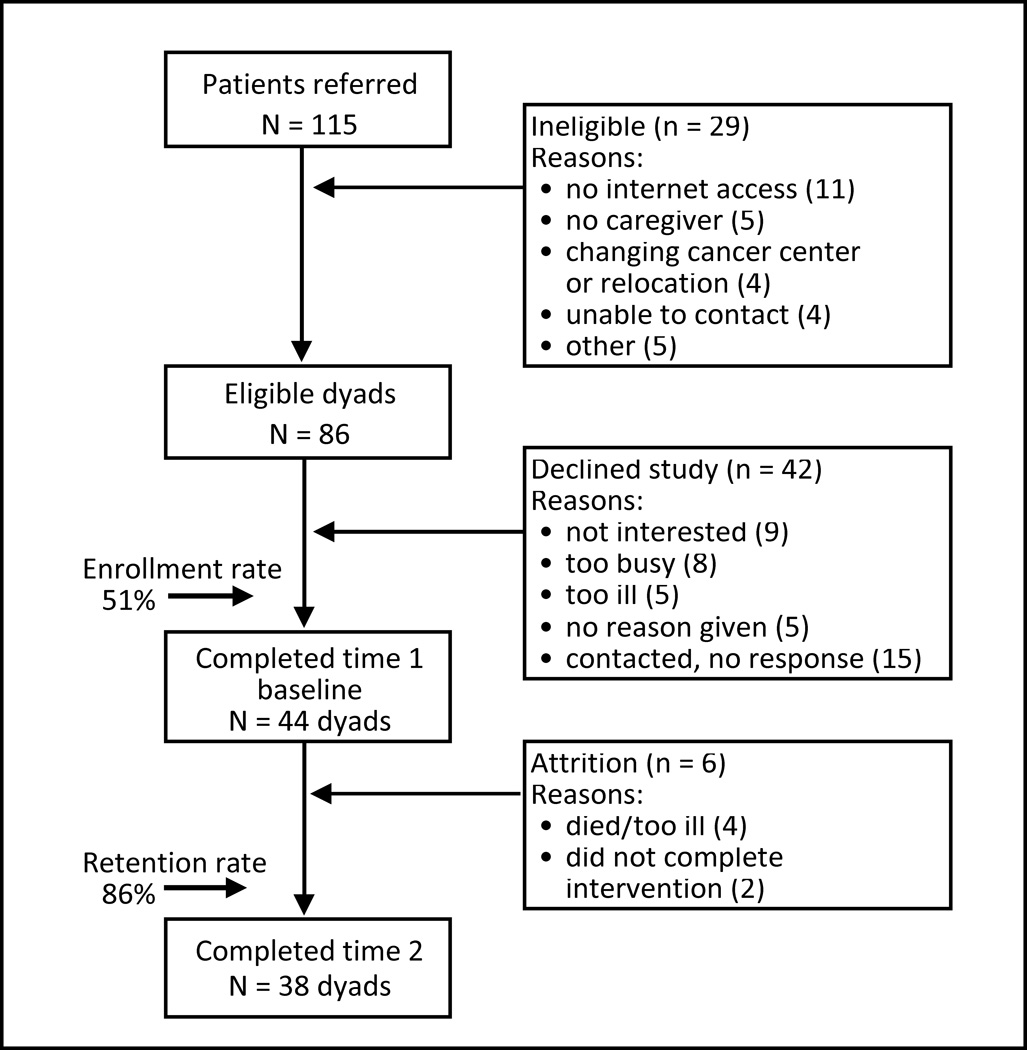
Figure 3 provides a consort diagram that illustrates the flow of participants into the study. Over a period of eight months, 115 patients and their caregivers were referred to the study from three cancer centers; 29 of these dyads were ineligible primarily due to no Internet access or no family caregiver. From the remaining 86 eligible dyads, 44 dyads consented and completed baseline questionnaires (enrollment rate 51%). Of the patients who refused, significantly more had lung cancer versus other types of cancer and were referred from an urban cancer versus a non-urban center.
Figure 3.
Consort diagram illustrating flow of participants into study
Of the 44 dyads enrolled, 38 dyads completed all three intervention sessions and the Time 2 assessment (retention = 86%). Loss of participants was due to patient death (n=2), patient too ill (n=2), or dyads withdrawing from study (n=2). Table 2 provides the demographic and medical characteristics of the final sample (N=38 dyads) and indicates that over half of the patients (52.6%) had advanced cancer. Table 2 also indicates that most participants felt moderately comfortable and skilled using computers and the Internet. At baseline, patients reported significantly lower physical QOL (p<.001) than caregivers. In contrast, caregivers reported significantly less self-efficacy and support, and more anger than patients (ps<.05). No differences were found between demographic variables (i.e., age, education, gender, comfort or skill using Internet/computers) or medical variables (type and stage of cancer) and participants’ scores on primary and secondary outcomes. However, due to the small sample there may have been insufficient power to detect differences if they existed.
Table 2.
Demographic and Medical Characteristics of Sample
| Characteristics | Patients n=38 |
Caregivers n=38 |
|---|---|---|
| Age, Mean (SD) | 54.8 (12.6) | 50.6 (14.7) |
| Range | 21–73 | 18–75 |
| Education, N (%) | ||
| 9–11th Grade | 0 (0.0) | 1 (2.6) |
| 12th grade | 5 (13.2) | 5 (13.2) |
| Some college | 11 (28.9) | 10 (26.3) |
| College | 9 (23.7) | 6 (15.8) |
| Post college | 13 (34.2) | 16 (42.1) |
| Income, N (%) | ||
| 15K–50K | 8 (21.1) | 6 (15.8) |
| 50,001-100K | 17 (44.7) | 14 (36.8) |
| Over 100K | 8 (21.0) | 12 (31.6) |
| Missing | 5 (13.2) | 6 (15.8) |
| Gender, N(%) | ||
| Male | 16 (42.1) | 15 (39.5) |
| Female | 22 (57.9) | 23 (60.5) |
| Race, N (%) | ||
| Asian | 1 (2.6) | 1 (2.6) |
| African American | 2 (5.3) | 2 (5.3) |
| White | 35 (92.1) | 35 (92.1) |
| Dyad relationship, N (%) | ||
| Spousal | 26 (68.4) | |
| Nonspousal | 12 (31.6) | |
| Marital status, N (%) | ||
| Married/Partnered | 32 (84.1) | 32 (84.2) |
| Divorced | 2 (5.3) | 1 (2.6) |
| Widowed | 2 (5.3) | 0 (0.0) |
| Never married | 2 (5.3) | 5 (13.2) |
|
Comfort using internet & computer, Mean (SD) |
5.6 (1.8) | 6.1 (1.5) |
| Range | 1–7 | 1–7 |
|
Skill at using internet & computer, Mean (SD) |
5.1 (1.8) | 5.6 (1.8) |
| Range | 1–7 | 1–7 |
| Stage, N (%) | ||
| I | 8 (21.1) | |
| II | 10 (26.3) | |
| III | 7 (18.4) | |
| IV | 13 (34.2) | |
| Type of Cancer, N (%) | ||
| Breast | 15 (39.4) | |
| Colorectal | 8 (21.1) | |
| Lung | 7 (18.4) | |
| Prostate | 8 (21.1) | |
Study Outcomes
Analyses indicated several main effects of time (see Table 3). Dyads had significant decreases in their overall (total) emotional distress (p<.05), anger-hostility (p<.01), and fatigue-inertia (p<.05) from pre- to post-intervention. They also reported significant improvements in their overall (total) QOL (p<.05), physical QOL (p<.05), functional QOL (p<.01), and perceived benefits of illness/caregiving (p<.01) from pre- to post-intervention.
Table 3.
Pre- and Post-intervention Results
| Means (SD) |
p-values |
Effect Sizesc |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Patient | Patient | Caregiver | Caregiver | Main Effect | Interaction Effect | Patient | Caregiver | ||
| Outcomes | Reliabilities | Time 1 | Time 2 | Time 1 | Time 2 | Timea | Role by Timeb | d | d |
| Emotional Distress | |||||||||
| Total Emotional | 0.82 | 58.1 (13.0) | 55.5 (15.7) | 58.4 (17.4) | 54.3 (12.3) | <.05 | .57 | 0.18 | 0.28 |
| Distress | |||||||||
| Anxiety -Tension | 0.81 | 8.0 (2.3) | 8.1 (3.0) | 8.7 (4.0) | 7.9 (2.4) | .24 | .10 | 0.03 | 0.22 |
| Depression-Dejection | 0.77 | 6.9 (1.8) | 7.0 (2.8) | 7.5 (3.4) | 6.7 (2.0) | .31 | .09 | 0.04 | 0.30 |
| Anger-Hostility | 0.74 | 6.9 (1.9) | 6.6 (2.3) | 7.8 (2.3) | 6.7 (1.8) | <.01 | .24 | 0.14 | 0.27 |
| Vigor-Activity | 0.92 | 16.1 (4.5) | 15.5 (4.5) | 15.5 (4.8) | 15.3 (4.2) | .22 | .66 | 0.13 | 0.04 |
| Fatigue-Inertia | 0.91 | 11.3 (4.1) | 9.6 (4.1) | 9.9 (4.4) | 9.2 (3.2) | <.05 | .21 | 0.41 | 0.18 |
| Confusion-Bewilderment | 0.69 | 8.7 (2.3) | 8.4 (2.7) | 8.6 (2.5) | 8.4 (2.4) | .35 | .90 | 0.12 | 0.08 |
| Quality of Life | |||||||||
| Total Quality of Life | 0.90 | 83.1 (12.2) | 86.0 (13.0) | 85.8 (12.4) | 88.3 (11.1) | <.05 | .85 | 0.23 | 0.20 |
| Physical | 0.71 | 21.5 (4.8) | 23.4 (4.1) | 25.6 (2.3) | 25.5 (2.7) | <.05 | <.05 | 0.43 | 0.04 |
| Social | 0.83 | 22.3 (3.9) | 22.0 (4.4) | 20.6 (5.6) | 21.4 (5.3) | .59 | .22 | 0.03 | 0.15 |
| Emotional | 0.78 | 19.6 (3.0) | 19.7 (3.3) | 18.5 (5.1) | 19.4 (3.7) | .16 | .23 | 0.03 | 0.20 |
| Functional | 0.81 | 20.1 (4.8) | 21.6 (4.7) | 21.0 (4.3) | 21.8 (3.9) | <.01 | .42 | 0.32 | 0.20 |
| Benefits of Illness | 0.92 | 2.6 (0.7) | 3.1 (0.6) | 2.7 (0.8) | 2.8 (0.8) | <.01 | <.05 | 0.77 | 0.13 |
| Communication | 0.93 | 3.9 (0.7) | 4.0 (0.6) | 3.9(0.6) | 3.9 (0.5) | .10 | .96 | 0.15 | 0.18 |
| Social Support | 0.87 | 4.5 (0.6) | 4.5 (0.5) | 4.2 (0.7) | 4.4 (0.5) | .07 | .19 | 0.01 | 0.33 |
| Self-efficacy | 0.95 | 147.6 (16.4) | 148.6 (25.7) | 141.2 (16.5) | 147.8 (16.9) | .06 | <.05 | 0.05 | 0.40 |
Significant Main Effect by Time ⇒ There is a significant difference over time for patients and caregivers (as a dyad) for the outcome.
Significant Interaction Effect-Role by Time ⇒ The amount of change over time for patients and caregivers is significantly different.
Absolute value of effect sizes is reported.
There were three significant time by role interactions. Patients had significantly greater improvement in their physical QOL (p<.05), and their perceived benefits of illness over time than caregivers (p<.05). However, caregivers had greater improvement in their self-efficacy over time than patients (p<.05). Intervention effect size estimates using d are indicated in Table 3. There were no significant main effects of time or interaction effects for communication or support.
Satisfaction with the Intervention
Potential range of scores on the satisfaction scale was 1 (low) to 7 (high). Dyads’ mean scores on the three subscales were: perceived ease of use and usability (M=6.0, SD=1.1), usefulness (M=4.4, SD=1.4), and general satisfaction (M=4.8, SD=1.7). There were no significant differences between patients’ and caregivers’ satisfaction ratings. Although dyads had a “Help” button to click if they encountered difficulties with the program, very few used it. The few dyads who used the “Help” button needed assistance with passwords for logging on to the web program. Study participants reported no adverse effects completing this web-based program together.
Feasibility of Web-based Intervention Delivery
We examined the enrollment and retention rates as well as preliminary effect sizes as indicators of the feasibility of using a web-based delivery format. The enrollment rate for the web-based program (51%) was lower than the enrollment rates (68–80%) obtained in the original five-module, nurse-delivered program in three prior RCTs20–22. However the retention rate for the web-based program was higher (86%) than the original nurse-delivered program (62–83%) 20–22.
We calculated one-sample effect sizes for patients and caregivers to get preliminary estimates of change from pre- and post-intervention for those exposed to the web-based intervention. Effect sizes for patients ranged in size from large for benefits of illness (d=.77), to medium for fatigue-inertia, emotional distress, physical quality of life, and functional quality of life (ranges d=.32-.43), and small effects for total quality of life and emotional distress (ranges d=.18-.23). Effect sizes for caregivers included medium effect sizes for self-efficacy and social support (ranges d=.33-.40), and small effects for total emotional distress, anxiety-tension distress, depression-dejection distress, anger-hostility distress, fatigue-inertia distress, total quality of life, emotional and functional quality of life (ranges d=.18-.30).
Discussion
This study examined the feasibility of translating an efficacious in-person program (FOCUS Program) for cancer patients and their family caregivers to a tailored, web-based delivery format. An essential component of the translation process was the collaboration between two experienced teams, one with prior experience implementing the original nurse-delivered program and the other with extensive experience developing tailored web-based interventions. The two teams worked together to develop a dyadic Internet platform, similar to the dyadic approach used in the face-to-face program, and to construct tailored messages based on original program content.
Outcomes for Patients and Caregivers
Using a pre-post intervention feasibility design, we found that dyads completing the web-based program reported a significant decrease in emotional distress and increase in quality of life (primary outcomes) similar to findings in our prior RCTs for caregivers21–22. Participants also perceived more benefits of illness and caregiving (secondary outcome) from pre- to post-intervention. The web-based program prompted patients and caregivers to share concerns and offered them tailored feedback about ways they could address these concerns. This interactive process was designed to help them to share worries and clarify misunderstandings which may have lowered their distress and improved their QOL. The program also prompted them to discuss possible benefits of illness/caregiving, as individuals and dyads, which could have increased their awareness of benefits from pre- to post-intervention.
In addition, we also found three intervention effects that were different for patients and caregivers. Patients, in contrast to caregivers, reported a significant increase in their physical quality of life over time. This improvement may have been due to the intervention, but could also be due to gradual improvement in patients’ physical well-being over time (e.g., maturation). Patients also reported greater improvement in their perceived benefits of illness than caregivers, similar to findings by Mellon and colleagues 39. Caregivers, in contrast to patients, reported significant improvement in their self-efficacy from pre-to post-intervention consistent with findings in our two prior RCTs 21–22. Studies with caregivers indicate that they often lack confidence and information necessary to provide high of quality care in the home, and are particularly unsure of how to address patients’ emotional concerns 40.The dialogue prompted by the interactive web-based program may have given caregivers a better understanding of patients’ needs. Additionally, the tailored information and website referrals that caregivers’ received may have enhanced caregivers’ knowledge and confidence about more effective ways to help patients.
It is important to note that because this was a feasibility study without a control group, it is possible that some of these positive findings could have occurred by chance or maturation. Nevertheless, the findings were in the expected direction and consistent with findings (e.g., better quality of life, greater caregiver self-efficacy), obtained using the same variables and instruments as in prior RCTs with the nurse-delivered FOCUS Program 21–22.
One unexpected finding was the lack of significant change in patients’ or caregivers’ dyadic communication. We expected that the interactive nature of the program would enhance their support and communication with one another, but that was not the case. However, dyads’ scores on the support and communication scales were generally positive prior to the intervention, and higher than baseline scores we obtained on these scales in our prior RCTs 21, and may have had little room for improvement. In our prior nurse-delivered RCT with prostate cancer patients and their spouses, we found significant improvement in communication for dyads in the FOCUS intervention versus control condition. It is possible that communication is a greater problem for couples facing prostate cancer as suggested in the literature 21 or that a nurse facilitator may need to be added to the web-based program to help foster patient-caregiver dyadic communication.
Program Satisfaction
This study also examined patients’ and caregivers’ satisfaction with the dyadic web-based delivery format. Dyads reported high satisfaction with the program’s ease of use and usability, which is an important finding given that few dyadic, tailored, web-based platforms have been developed or tested in prior intervention research with cancer patients and their caregivers 18. We collaborated with expert designers of web interventions and did usability testing on the prototype version 23, which likely increased the usability of the program tested in this study. In addition, our study participants were generally well-educated and moderately skilled using computers /Internet (see Table 2). These sample characteristics may have contributed to positive usability ratings.
Participants’ ratings of the program’s usefulness (4.4) and their general program satisfaction (4.8) were higher than midpoint (3.5) on the seven-point scale, but not as high as their usability ratings. These lower scores may be due to the fact that we translated only one module (Family Involvement Module) of the original five-module FOCUS Program for this feasibility program, making this web program much narrower in scope. Some participants reported that they would have liked more information about symptom management and coping, both modules in the original program. It is possible that if we had translated some content from all five modules from the original program that participants’ usefulness and satisfaction ratings would have been higher. In addition, we chose to use a generally self-managed web program to decrease future implementation costs rather than a clinician-managed web program that included active nurse involvement. However, greater contact with a nurse may have improved their satisfaction scores. Future research needs to compare participants’ satisfaction with fully versus partially self-managed web-based programs.
Feasibility of using a web-based delivery format for intervention delivery
We examined recruitment and retention rates and effect sizes obtained in the web versus nurse-delivered programs. We found that it was more difficult to recruit patient-caregiver dyads to the web-based program (enrollment 51%) than to our prior nurse-delivered programs (68–80%)20,21 However, the retention rate for the web-program (86%) was higher than retention rates for our five-module, nurse-delivered program across three RCTs (62–83%) suggesting that once participants enrolled in the web program, they were likely to complete it. Participants reported that they liked being able to complete the web program in their own home at a time that was convenient for them which may have enhanced retention.
The effect sizes obtained with the web-based program were generally small to medium in size for both patients and caregivers. These effects are similar to effect sizes reported in a recent meta-analysis of other psycho-educational interventions for cancer patients and their family caregivers18, including our prior nurse-delivered FOCUS Program 21–22. However, the effect sizes obtained with this web-based program are preliminary and need to be viewed with caution because of the small sample size.
Limitations
There were a few limitations to the study. Without a control group, factors other than the intervention could have influenced study results. Study enrollment was lower than we anticipated limiting the generalizability of study findings. However, this is not unique to our study, since other investigators also have reported problems recruiting participants to web-based interventions 8,11. Furthermore, trying to recruit patient-caregiver dyads to research studies is more difficult than recruiting patients only, because both members of the dyad have to be willing and able to participate in the study.
Conclusions
In spite of these limitations, our findings suggest that is it feasible to translate content from an efficacious nurse-delivered intervention to a web-based format and have positive intervention effects. The generally positive effects could be due to a number of factors. First, the basic content of the web-program was derived from an established nurse-delivered program for patients and caregivers. Second, the program used tailored rather than non-tailored messages, which according to considerable research increases the relevance of intervention messages for participants 28. Third, the program was offered to dyads as the unit of care, rather to individual patients or caregivers. Since patients’ and caregivers’ emotional responses to cancer are interdependent 14,15, treating them together may have created a positive, synergistic effect, enhancing the intervention effects.
Even though our program is promising, it needs further testing in a large, multisite RCT. Future research needs to examine the cost-benefit ratio of incorporating clinicians into the delivery of web-based programs. There also needs to be ways to make web-based programs available to others with limited access to high-speed Internet services. Nevertheless, web-based programs are a promising new way to offer psycho-educational interventions to patients and their caregivers in the future.
Acknowledgments
The study was funded by a grant from the National Cancer Institute R21CA138725 to L. Northouse (PI). Dr. Song’s work is sponsored by the Clinical and Translational Sciences Award (CTSA), University of North Carolina-Chapel Hill (KL2TR001109).
The authors wish to acknowledge valuable consultations with Darlene Mood PhD from Wayne State University, and Edward Saunders MS from Center for Health Communication Research at the University of Michigan.
Footnotes
Conflicts of interest and sources of funding. The authors have no conflicts of interest to disclose.
References
- 1.American Cancer Society. [Accessed February 5, 2013];Cancer Facts and Figures. 2013 http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf.
- 2.Edler NE, Page AE, editors. Institute of Medicine. Cancer Care for the Whole Patient: Meeting Psychosocial Needs. Washington, DC: The National Academy of Science; 2008. [Google Scholar]
- 3.National Alliance for Caregiving. e-Connected Family Caregiver: Bringing Caregiving into the 21st Century. Bethesda, MD: 2011. [Accessed February 5, 2013]. http://www.caregiving.org/data/FINAL_eConnected_Family_Caregiver_ Study_Jan20, 2011.pdf. Published January 2011. [Google Scholar]
- 4.Strecher VJ. Internet methods for delivering behavioral and health-related interventions (eHealth) Annu Rev Clin Psychol. 2007;3:53–76. doi: 10.1146/annurev.clinpsy.3.022806.091428. [DOI] [PubMed] [Google Scholar]
- 5.Gustafson DH, Hawkins R, McTavish F, et al. Internet-based interactive support for cancer patients: Are integrated systems better? J Commun. 2008;58:238–257. doi: 10.1111/j.1460-2466.2008.00383.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owen JE, Klapow JC, Roth DL, et al. Randomized pilot of a self-guided internet coping group for women with early-stage breast cancer. Ann Behav Sci Med Educ. 2005;30(1):54–64. doi: 10.1207/s15324796abm3001_7. [DOI] [PubMed] [Google Scholar]
- 7.Ritterband LM, Bailey ET, Thorndike FP, Lord HR, Farrell-Carnahan L, Baum LD. Initial evaluation of an Internet intervention to improve the sleep of cancer survivors with insomnia. Psychooncology. 2012 Jul;21(7):695–705. doi: 10.1002/pon.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruland CM, Andersen T, Jeneson A, et al. Effects of an internet support system to assist cancer patients in reducing symptom distress: a randomized controlled trial. Cancer Nurs. 2012;36(1):6–17. doi: 10.1097/NCC.0b013e31824d90d4. [DOI] [PubMed] [Google Scholar]
- 9.Winzelberg AJ, Classen C, Alpers GW, et al. Evaluation of an internet support group for women with primary breast cancer. Cancer. 2003;97(5):1164–1173. doi: 10.1002/cncr.11174. [DOI] [PubMed] [Google Scholar]
- 10.Yun YH, Lee KS, Kim YW, et al. Web-based tailored education program for disease-free cancer survivors with cancer-related fatigue: a randomized controlled trial. J Clin Oncol. 2012;30(12):1296–1303. doi: 10.1200/JCO.2011.37.2979. [DOI] [PubMed] [Google Scholar]
- 11.DuBenske LL, Gustafson DH, Shaw BR, Cleary JF. Web-based cancer communication and decision making systems: Connecting patients, caregivers, and clinicians for improved health outcomes. Med Decis Making. 2010;30(6):732–744. doi: 10.1177/0272989X10386382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schover LR, Yuan Y, Sui D, Neese L, Jenkins R, Rhodes MM. A randomized trial of internet-based versus traditional sexual counseling for couples after localized prostate cancer treatment. Cancer. 2011;118(2):500–509. doi: 10.1002/cncr.26308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Northouse LL, Mood D, Kershaw T, et al. Quality of life of women with recurrent breast cancer and their family members. J Clin Oncol. 2002;20(19):4050–4064. doi: 10.1200/JCO.2002.02.054. [DOI] [PubMed] [Google Scholar]
- 14.Hodges LJ, Humphris GM, Macfarlane G. A meta-analytic investigation of the relationship between the psychological distress of cancer patients and their carers. Soc Sci Med. 2005;60:1–12. doi: 10.1016/j.socscimed.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 15.Segrin C, Badger T, Dorros SM, Meek P, Lopez AM. Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psychooncology. 2007;16:634–643. doi: 10.1002/pon.1111. [DOI] [PubMed] [Google Scholar]
- 16.Hartmann M, Bazner E, Wild B, Eisler I, Herzog W. Effects of interventions involving the family in the treatment of adult patients with chronic physical diseases: A meta-analysis. Psychother Psychosom. 2010;79:136–148. doi: 10.1159/000286958. [DOI] [PubMed] [Google Scholar]
- 17.Martire LM, Schulz R, Helgeson VS, Small BJ, Saghafi EM. Review and meta-analysis of couple-oriented interventions for chronic illness. Ann Behav Med. 2010;40:325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Northouse LL, Katapodi MC, Song L, Zhang L, Mood D. Interventions with caregivers of cancer patients: Meta-analysis of randomized trials. CA Cancer J Clin. 2010;60:317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DuBenske LL, Gustafson DH, Namkoong K, et al. CHESS's impact on lung cancer caregivers' burden and mood: results from an eHealth RCT. Health Psychol. 2013 Nov 18; doi: 10.1037/a0034216. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Northouse L, Kershaw T, Mood D, Schafenacker A. Effects of a family intervention on the quality of life of women with recurrent breast cancer and their family caregivers. Psychooncology. 2005;14:478–491. doi: 10.1002/pon.871. [DOI] [PubMed] [Google Scholar]
- 21.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a family intervention for prostate cancer patients and their spouses. Cancer. 2007;110:2809–2818. doi: 10.1002/cncr.23114. [DOI] [PubMed] [Google Scholar]
- 22.Northouse LL, Mood DW, Schafenacker A, et al. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology. 2013;22:555–563. doi: 10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zulman DM, Schafenacker A, Barr KL, et al. Adapting an in-person patient-caregiver communication intervention to a tailored web-based format. Psychooncology. 2012;21(3):336–341. doi: 10.1002/pon.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lazarus RS, Folkman S, editors. Stress, Appraisal, and Coping. New York: Springer; 1984. [Google Scholar]
- 25.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, N.J: Lawrence Erlbaum; 1988. [Google Scholar]
- 26.Hintz JL. PASS 2000 User's Guide. Kaysville, Utah: Number Cruncher Statistical Systems; 2000. [Google Scholar]
- 27.Northouse LL, Walker J, Schafenacker A, et al. A family-based program of care for women with recurrent breast cancer and their family members. Oncol Nurs Forum. 2002;29(10):1411–1419. doi: 10.1188/02.ONF.1411-1419. [DOI] [PubMed] [Google Scholar]
- 28.Kreuter MW, Farrell D, Olevitch L, Brennan L. Tailoring Health Messages:Customizing Communication Using Computer Technology. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 29.Hawkins R, Krueter MW, Resnicow K, Resnisow K, Fishbein M, Dijkstra A. Understanding tailoring in communicating about health. Health Educ Res. 2008;23(3):454–466. doi: 10.1093/her/cyn004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McNair D, Lorr M, Droppleman L. Profile of Mood States. San Diego: Education and Industrial Testing Service; 1971. [Google Scholar]
- 31.Cella D, Tulsky D, Gray G, et al. The functional assessment of cancer therapy scale:development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 32.Tomich PL, Helgeson V. Is finding something good in bad always good? Benefit finding among women with breast cancer. Health Psychol. 2004;23:16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- 33.Lewis FM. Family Home Visitation Study Final Report. National Cancer Institute: National Intitutes of Health; 1996. [Google Scholar]
- 34.Northouse LL. Social support in patients' and husbands' adjustment to breast cancer. Nurs Res. 1988;37(2):91–95. [PubMed] [Google Scholar]
- 35.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quart. 1989;13:319–340. [Google Scholar]
- 36.Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: Toward a unified view. MIS Quart. 2003;27:425–478. [Google Scholar]
- 37.Zheng K, Padman R, Johnson MP, Diamond HS. Evaluation of healthcare IT applications: the user acceptance perspective. Studies in Computational Intelligence (SCI) 2007:49–78. [Google Scholar]
- 38.U.S. Department of Health and Human Services. [Accessed May 10, 2010];Usability.gov: Your guide for developing usable & useful Web sites. http://www.usability.gov.
- 39.Mellon S, Northouse LL, Weiss LK. A population-based study of the quality of life of cancer survivors and their family caregivers. Cancer Nurs. 2006;29:120–131. doi: 10.1097/00002820-200603000-00007. [DOI] [PubMed] [Google Scholar]
- 40.van Ryn M, Sanders S, Kahn K, et al. Objective burden, resources, and other stressors among informal caregivers: A hidden quality issue? Psychooncology. 2011;20:44–52. doi: 10.1002/pon.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]