Abstract
Purpose
The patient-centered approach to health care does not seem to be sufficiently developed in the Italian context, and is still characterized by the biomedical model. In addition, there is a lack of validated outcome measures to assess outpatient experience as an aspect common to a variety of settings. The current study aimed to evaluate the factorial validity, reliability, and invariance across sex of the Health Services OutPatient Experience (HSOPE) questionnaire, a short ten-item measure of patient-centeredness for Italian adult outpatients. The rationale for unidimensionality of the measure was that it could cover global patient experience as a process common to patients with a variety of diseases and irrespective of the phase of treatment course.
Patients and methods
The HSOPE was compiled by 1,532 adult outpatients (51% females, mean age 59.22 years, standard deviation 16.26) receiving care in ten facilities at the Santa Maria alle Scotte University Hospital of Siena, Italy. The sample represented all the age cohorts. Twelve percent were young adults, 57% were adults, and 32% were older adults. Exploratory and confirmatory factor analyses were conducted to evaluate factor structure. Reliability was evaluated as internal consistency using Cronbach’s α. Factor invariance was assessed through multigroup analyses.
Results
Both exploratory and confirmatory analyses suggested a clearly defined unidimensional structure of the measure, with all the ten items having salient loadings on a single factor. Internal consistency was excellent (α=0.95). Indices of model fit supported a single-factor structure for both male and female outpatient groups. Young adult outpatients had significantly lower scores on perceived patient-centeredness relative to older adults. No significant difference emerged on patient-centeredness between male and female outpatients.
Conclusion
The HSOPE questionnaire seemed to be a tool with high acceptability and excellent psychometric properties to measure patient-centeredness as a unidimensional construct. Limitations and implications for future research are discussed.
Keywords: patient-centered care, health care services, psychometric properties, patient-reported outcomes
Introduction
The patient-centeredness framework in health care services
In the last few decades, the patient-centeredness framework (PCF) has developed as a new approach to diagnosis and treatment in health care settings. This approach was conceived to overcome limitations of the traditional biomedical model.1,2 In contrast with the latter, the PCF highlights the importance of a symmetrical relationship between the patient and health profession staff.1 In the biomedical model, a role asymmetry existed in the difference in authority between health professionals and the patient. The first were considered experts, while the patient was a passive recipient of prescriptions.
According to Epstein et al,3 a definition of the concept of patient-centeredness includes the following aspects:
eliciting and understanding the patient’s perspective – concerns, ideas, expectations, needs, and feelings
understanding the patient within his/her unique psychosocial context
reaching a shared understanding of the problem and its treatment with the patient that is concordant with the patient’s values
helping patients to share power and responsibility by involving them in choices to the degree that they wish for disease self-management.
Research has demonstrated that a patient-centered approach to services may have several advantages in terms of clinical efficacy and policy making. Indeed, patient-centered care is a predictor of different patient-related outcomes, including reductions in symptom burden or relapses, length of hospital stay and rates of referrals, increases in treatment adherence, and importantly improvement in patient satisfaction and quality of life.4–11 Given its relation with health outcomes, patient-centeredness appears to be an important process of care, particularly for the increasingly widespread chronic diseases, which involve long-term treatments and a more active role of patients in symptom self-management. Indeed, some evidence suggests that about 70% of patients only partially follow medical prescriptions, and approximately 30% do not adhere to treatment regimens at all.12 In addition, patient-centered care has been shown to be associated with time-efficient delivery of care and cost-effective use of health care resources. For example, some authors have observed that medical staff using patient-centered communication skills tended to have lower expenditures on diagnostic testing.13 Consequently, the evaluation of patient-centered care with valid and reliable tools has become a crucial field of research in the last decades.
Evaluation and measurement of patient-centered care in outpatient settings
Since the development of the PCF, many instruments have been constructed as outcome measures of the health care pathway.14 The majority of these tools measure only a specific aspect of patient-centeredness: the patient’s satisfaction as subjective judgment of satisfaction with regard to the received service.15 Satisfaction and dissatisfaction are not considered fully adequate measures of the quality of care, because they are affected by such a wide array of different factors.14 However, patient-centeredness has been viewed as a multidimensional construct that cannot be understood only by observing care directly or asking patients to express satisfaction judgments about care.16
In addition, this measurement approach is based on rating scale-type questions, requiring the respondent to provide an assessment of aspects of the service received, eg, on a scale from “very poor” to “excellent”. Even though this approach is the most developed method today, it has received some criticism.16,17 Some studies have shown that patient expectations have only an indirect effect on satisfaction, and that patients tend to be satisfied even if their personal expectations have not been fully met.18 Moreover, satisfaction judgments tend to produce overly positive representations of the service, and do not provide a sensitive measure of the specific problems experienced by the patient during treatment.18 Consequently, assessing satisfaction cannot allow to identify which health care processes need to be addressed to improve patient-related outcomes.17,18 Some psychosocial variables seem related to specific aspects that have to do with the treatment course, such as the quality of communication with health care operators and the degree of control and involvement experienced by the patient during treatment.19
In line with these shortcomings, other types of instruments were developed as outcomes of patient-centered care, encompassing all the domains posited by the PCF.20 In the Anglo-American health care context, there is an extensive body of research on valid and reliable outcome measures of patient-centeredness in outpatient settings. For example, in the US, the Patient-Perceived Patient-Centeredness Scale was developed21 as a self-report measure for assessing to what extent health care communication focuses on patient’s needs. The measure consists of 14 items measuring two domains. The “eliciting illness experience” domain covers health care providers’ ability to take into account the point of view of the patient. The second domain – finding common ground – assesses health care providers’ ability to enhance patient participation in decision making during the health care pathway.21
Despite the fact that the PCF was developed in the Anglo-American health care context, several measures were developed and evaluated as outcomes of patient-centered care in non-English-speaking countries for a variety of settings, including hospital outpatient facilities.22 For example, in the French context, Gasquet et al22 developed a 27-item tool with satisfactory psychometric properties, measuring outpatients’ satisfaction with hospital care. The measure consists of four subscales reflecting appointment making, reception facilities, waiting time, and doctor consultation. However, consultation with the doctor is covered by half of the items, and quality of communication is limited to the doctor-consultation domain.
Despite most of the available measures in the literature assessing patient-centeredness as a multidimensional construct, short measures could be useful for routine clinical practice, and they could overcome some problems related to an inadequate ratio of items to dimensions, which is in contrast with the psychometric theory of instrument development.23
Recently, researchers have developed short-form questionnaires in non-English-speaking health care contexts. In the Norwegian context, Oltedal et al24 created a six-item measure for inpatient settings, which principal-component analyses suggested as having a single-factor structure. In a national survey Skudal et al25 developed the Nordic Patient Experience Questionnaire (NORPEQ), a six-item short measure of health care global experience. The questionnaire was mailed to large samples of Norwegian, Swedish, Finnish, and Faroe Island inpatients. Findings from the analyses showed a single-factor structure measuring global experience of inpatient health care.25
Unidimensional measures of patient-centeredness have also been developed for specific health care contexts. For example, in the Turkish context, Coban and Kasikci26 developed a unidimensional scale for experience of nursing care: the Patient Perception of Hospital Experience of Nursing Care. The tool was administered to 150 patients, who were discharged from medical and surgical units. Results of factor analyses suggested a single-factor structure, measuring global experience of nursing care.
Evaluation of patient-centered care in the Italian context
In the Italian context, the patient-centeredness of care is still understudied, and to date there has been a lack of research on psychometric tools to assess this construct. Ruggeri et al27 developed and evaluated the Verona Services Satisfaction Scale, a self-report measure assessing satisfaction with psychiatric outpatient services, covering six dimensions (professional skills behavior, information, access, efficacy, interventions, and relatives’ involvement). Gigantesco et al28 developed a 15-item self-report questionnaire to measure satisfaction with hospital and community outpatient services. However, some limitations of these instruments should be considered. First, they focused on satisfaction with mental health services exclusively. Moreover, the authors recruited small samples of outpatients; therefore, the ratio of number of respondents to number of items was inadequate according to recommendations.23,29 In addition, in these studies, the factor structure of the measures was not tested.
Gremigni et al30 developed a 13-item measure – the Health Care Communication Questionnaire – a self-report questionnaire measuring outpatients’ experience with the patient-centered communication of nonmedical hospital staff. The questionnaire measures four domains of patient-centered communication with nonmedical staff: problem solving, respect, lack of hostility, and nonverbal immediacy. However, this instrument focuses on patient-centeredness aspects related to communication with staff.
More recently, Cioffi et al31 validated a self-report measure – the Quality Perception Questionnaire – on a large sample of patients recruited in different hospital facilities. Despite this measure demonstrating very good psychometric properties, it was developed for inpatient settings. In addition, it assessed exclusively satisfaction judgments with doctors, nursing staff, auxiliary staff, and hospital structures, but did not assess aspects related to patient-centeredness, such as information about diagnosis and treatment, communication, or involvement in decision making.
Rationale for the current study
Previous findings have shown that patient-centered care is interpreted and enacted differently between cultures, suggesting that the concept and practice of patient-centered care may be influenced by sociocultural factors. In the Italian health care context, the patient-centered health care framework is not sufficiently developed, as the doctor–patient relationship is still considered asymmetrical, with the latter having the role of passive recipients of medical instructions.32 Lamiani et al33 observed differences in conceptual components of patient-centeredness between US doctors and Italian doctors. Respecting the patient’s autonomy was identified as a core aspect of patient-centered care by only the US doctors. The Italian group demonstrated a more implicitly paternalistic approach.
As outlined by some authors,34 there is a lack of tools with valid and reliable psychometric properties that can be used as a global measure to assess patient-centeredness in different outpatient facilities. This issue appears of strong relevance in light of the link between the patient-centered approach and health outcomes found in the literature.1
Objectives
The current study aimed to present a psychometric evaluation of the Health Services OutPatient Experience (HSOPE) questionnaire, a self-report global measure for assessing patient-centeredness of health care services in Italian outpatient settings. Specifically, the aims were:
to evaluate exploratory factorial validity and reliability of the HSOPE questionnaire on a large sample of Italian adult outpatients
to evaluate confirmatory factorial validity of the measure and factor invariance across sex on another large sample of adult outpatients
to test which aspects of patient-centeredness (measured by the HSOPE questionnaire items) could predict overall satisfaction with the health care service.
Patients and methods
Participants
The HSOPE questionnaire was administered to 1,532 adult outpatients. All the participants received care in outpatient facilities at the Santa Maria alle Scotte University Hospital of Siena, Italy. Of these, 13 (0.84%) were eliminated due to missing data on more than three items of the measure. Therefore, the total final sample consisted of 1,519 outpatients.
Participants were excluded from the study if they were younger than 16 years. Fifty-one percent of the sample were females. The mean age was 59.22 years (standard deviation [SD] =16.26 years), ranging from 17 to 93 years. Twelve percent of the sample were young adults, 57% were adults, and 32% were older adults.
The total sample was randomly split in two subsamples with homogeneous sample size, subsample 1 (n=788) and subsample 2 (n=731), which were used to perform exploratory factor analysis (EFA) and confirmatory factor analysis (CFA), respectively. Participants’ distribution in the total sample across the outpatient facilities is provided in Table 1.
Table 1.
Demographic characteristics and number of participants for each of the outpatient facilities in the total sample (n=1,519)
| Demographic characteristics | Mean (SD; range) |
|---|---|
| Age, years | 59.22 (16.26; 17–93) n (%) |
|
| |
| Age cohort | |
| Young adults | 182 (12) |
| Adults | 865 (57) |
| Older adults | 486 (32) |
| Females | 775 (51) |
| Outpatient facilities | |
| Surgery | 217 (14.30) |
| Cardiology | 276 (18.20) |
| Gynecology | 9 (1.00) |
| Orthopedics | 71 (4.70) |
| Internal medicine | 469 (30.90) |
| Odontostomatology | 123 (8.10) |
| Oncology | 9 (1.00) |
| Otorhinolaryngology and ophthalmology | 151 (9.90) |
| Rehabilitation | 171 (11.30) |
| Dermatology and rheumatology | 22 (1.40) |
Abbreviation: SD, standard deviation.
Development of the Health Services OutPatient Experience questionnaire
The survey was designed by a multidisciplinary research group consisting of academic researchers and health care professionals with over 10 years’ experience in the measurement of satisfaction. Specifically, the group consisted of a sociologist (AC), a senior statistician and methodologist (FF), a statistician (FL), and a psychologist (AP).
Two main aims were followed during the scale development. First, the questionnaire needed to include the most important aspects of the patient’s experience identified within the international and the Italian literature that are relevant to outpatients irrespective of the disease and the stage of the treatment course. Second, it needed to be a short tool, which could be easily administered by the nursing staff after the visit.
The HSOPE questionnaire is a paper-and-pencil self-administered brief tool, which was developed as a global outcome measure of perceived patient-centeredness of the outpatient health care pathway. The questionnaire is composed of three sections. The first section is composed of two subsections. The first one consists of ten statements that reflect experience associated with regard to a variety of aspects of outpatient visits (eg, feeling informed regarding modalities of the outpatient visit, feeling involved in decision making about treatment, feeling informed on the visit outcomes and the course of the health care pathway, feeling provided with clear information when asking questions). Question responses are in a 5-point Likert scale self-report format (“never” =1, “always” =5). The second subsection consists of one item on a 10-point rating scale response format (ranging from “very dissatisfied” =1 to “very satisfied” =10). The choice of this response format was motivated by the aim of measuring overall satisfaction also with regard to the outpatient visit.
The second section of the HSOPE questionnaire consists of three questions in a closed-response format in which the outpatient is asked to provide sociodemographic information (sex, age, and residence). In the third section one question asks suggestions to improve outpatient visits in terms of patient-centeredness.
In our study, the HSOPE questionnaire was administered to the outpatients by the nursing staff of each unit immediately after the visit. The development of the questionnaire followed previous literature on the identification of domains and items of relevance to outpatient experience. Two main aims were followed during the scale’s development. First, the questionnaire needed to include the most important aspects of patient’s experience identified within the international and the Italian literature that are relevant to outpatients irrespective of the disease and the stage of the treatment course. Second, it needed to be a short tool, which can be easily administered by the nursing staff after the visit.
During the first phase of the instrument’s construction, the Anglo-American and Italian online literature was searched for aspects related to experience with regard to outpatient settings. Through face-to-face meetings, the contents of some questionnaires used in previous surveys in English-speaking countries and in Italy were reviewed, including provision of information on the visit and treatment course, humanization of care, outpatient involvement in decision making, perception of competence, management of continuity of care, privacy, and overall satisfaction. In particular, the following multidimensional and unidimensional questionnaires were examined: the Picker Patient Experience Questionnaire35 developed by Gasquet et al,22 the Nordic Patient Experience Questionnaire,25 and the questionnaire developed by Oltedal et al24 for foreign contexts: the Quality Perception Questionnaire31 and the Verona Satisfaction Scale27 for the Italian context. In addition, some reviews and papers on theoretical models of patient-centeredness were examined.1–6
During meetings, a preliminary list of items was created by the research staff, composed of psychologists, statisticians, and methodologists, and other health care professionals, according to their relevance to the Italian health care context. Subsequently, the questionnaire was piloted through cognitive interviews with 30 outpatients from facilities of the Santa Maria alle Scotte University Hospital. The outpatients completed the questionnaire, and were asked to comment on the relevance of the domains covered and clarity, including the response options. Since this version of the questionnaire was considered clear and comprehensible by the respondents, it was used for the study on its psychometric properties. The theoretical model of the HSOPE questionnaire is based on viewing patient-centeredness as a unidimensional construct. A unidimensional model of the patient’s experience construct was adopted following the recent development of measures in other non-English-speaking countries.24,25 In the present study, psychometric properties of the first subsection of the HSOPE questionnaire were assessed. A copy of the measure can be requested from the corresponding author.
Statistical analysis
Item distributional properties
Item distributional properties were tested on the total sample (n=1519). HSOPE questionnaires missing more than three items were excluded from analysis, with up to three missing items replaced with the mean response for that individual. The distributional properties of the HSOPE questionnaire items were examined by conducting the Kolmogorov– Smirnov test and by inspecting the skewness and kurtosis indices of the items’ distributions. The amount of missing data per item was low (1.0%–3.8%).
Exploratory factor analysis and reliability
EFA was conducted to evaluate the factor structure of the HSOPE questionnaire on subsample 1 (n=788). Reliability was evaluated as internal consistency using Cronbach’s α-coefficients.36 Reliability coefficients were evaluated according to Nunnally and Bernstein37 (α.0.70= acceptable, α.0.80= good, α.0.90= excellent). The EFA and reliability analysis were performed using SPSS version 21.
Confirmatory factor analysis (CFA) and multisample analysis
CFA was carried out using a structural equation-modeling approach.38 Based on the results found with the EFA, we tested a model in which all the ten items loaded on a single factor. To evaluate goodness of fit of the model to the data, χ2 values were computed.38 In addition, as recommended by Floyd and Widaman,23 the following fit indices were used: the Adjusted Goodness-of-Fit Index (AGFI), the Goodness of Fit Index (GFI), the Bentler–Bonett Normed Fit Index (NFI), and the Bollen Relative Fit Index (RFI).38 For these indices, values close to 1 represent a good fit. In addition, the root mean square residual (RMR) was used as an index of fit. For the RMR, values less than 0.08 represent acceptable fit, and values less than 0.05 represent good fit.39 A series of multisample CFA was also conducted to test for the invariance of the HSOPE questionnaire factor structure across sex. CFA was performed with AMOS version 21.
HSOPE questionnaire items as predictors of overall satisfaction
To test which aspects of patient-centeredness could predict overall satisfaction, a multiple linear regression analysis was conducted using the stepwise method, in which each of the HSOPE questionnaire items were entered as independent variables and satisfaction scores as dependent variables.
Results
Item distributional properties of the HSOPE questionnaire
Item distributional properties of the HSOPE questionnaire were tested on the total sample (n=1,519). To evaluate the normality of items of the HSOPE questionnaire, Kolmogorov–Smirnov tests were conducted. Results indicated that the distribution of the items was significantly different from a normal distribution. In addition, an inspection of kurtosis and skewness indices for all the HSOPE questionnaire items was conducted. An absolute value on these indices falling out of the recommended range between −1 and +1 indicates a substantial deviance from normal distribution.37 Eight of the ten items showed a kurtosis or skewness value out of the recommended range, suggesting that data for these items were abnormally distributed. This observation was also supported by inspection of the patterns of response frequencies, which revealed that the number of participants endorsing these items as “always” or “often” ranged from 74.90% to 86.40%.
Differences in the outpatient experience as a function of sex and age-group
Differences in the HSOPE questionnaire scores were examined as a function of sex and age group for the total sample (n=1519). Independent-sample t-test analyses showed that HSOPE questionnaire scores did not significantly differ between female and male outpatients (t=1.34, P<0.001). Between-group differences on the HSOPE questionnaire scores were tested as a function of age-group. We used three group categories to present data by age-group (young adults, adults, older adults). The young adult group comprised individuals aged between 16 and 39 years, the adult group individuals aged between 40 and 69 years, and the older adult individuals aged over 69 years. Results of a one-way analysis of variance showed a significant difference between young adults, adults, and older adults (F=6.20, P<0.01). Specifically, young adults had significantly lower scores on the HSOPE questionnaire than older adults. Means and standard deviations for the total sample as a function of sex and age cohort are provided in Table 2.
Table 2.
Means and standard deviations (SDs) on the HSOPE questionnaire as a function of sex and age-group for the total sample (n=1,519)
| Sex
|
Age-group
|
Total sample (n=1,519) |
||||
|---|---|---|---|---|---|---|
| Males (n=700) |
Females (n=740) |
Young adults (n=153) |
Adults (n=742) |
Older adults (n=416) |
||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| HSOPE | 43.15 (7.48) | 42.61 (7.71) | 41.35 (8.29) | 42.98 (7.64) | 43.80 (6.58) | 42.88 (7.62) |
Note: The young adult group consisted of 16- to 39-year-old participants, the adult group consisted of 40- to 69-year-old participants, and the older adult group consisted of participants aged over 69 years.
Abbreviation: HSOPE, Health Services OutPatient Experience.
Objective 1: Factorial validity and reliability of the HSOPE questionnaire
Exploratory factor analysis (EFA)
The EFA was conducted on subsample 1 (n=788). In subsample 1, the mean age was 59.32 years old (SD =16.12 years), ranging from 18 to 91 years. Forty-nine percent were female outpatients. According to the age-groups previously identified, 12% were young adults, 57% were adults, and 31% were older adults.
Prior to the extraction of factors, the assumptions required for the EFA were tested. The Kaiser–Meyer–Olkin index of sampling adequacy40 result was 0.96, suggesting that the correlation matrix was appropriate for performing EFA, since it has been proposed that Kaiser–Meyer–Olkin values should be equal or above |0.60| in order to interpret an EFA solution satisfactorily.40 Bartlett’s sphericity test41 resulted in significance, indicating that the data matrix was not an identity matrix (χ245=6,628.04, P=0.001), and thus suitable for EFA.
Given the abnormality of two of the HSOPE questionnaire items, factor extraction was carried out using the principal axis-factoring technique, as recommended by Floyd and Widaman.24 Using the criterion of eigenvalue greater than 1.0, only one factor met this requirement. This factor yielded an eigenvalue of 6.97, and accounted for a total of 66.37% of the variance in all the ten items. The second and third factors yielded eigenvalues of 0.58 and 0.46, respectively.
Following recommendations from Floyd and Widamann,24 the number of factors to be extracted was also determined by visual inspection of the scree test, which suggested the extraction of one factor. The scree plot of the HSOPE questionnaire items is presented in Figure 1.
Figure 1.
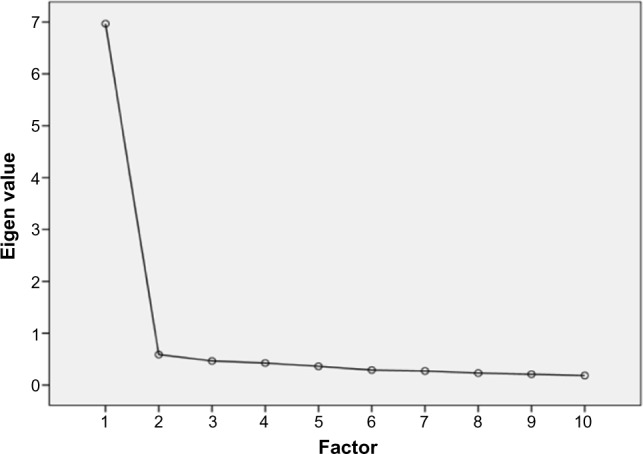
Scree plot of eigenvalues of the ten HS OPE items.
Abbreviation: HS OPE, Health Services OutPatient Experience.
Based on these findings, one factor was extracted. The inspection of the factor-loading matrix showed that all ten items had salient loadings (at least |0.50|) on the factor extracted according to recommendations.42 Consistent with Floyd and Widaman’s recommendations,24 all values of the communalities were greater than 0.50. Factor loadings and communalities of each item of the HSOPE questionnaire for the single-factor solution are presented in Table 3.
Table 3.
Loading (λ1) on a single factor and communalities (h2) of the ten items of the HSOPE questionnaire in subsample 1 (n=788)
| HSOPE questionnaire items | λ1 | h2 |
|---|---|---|
| Did you receive clear and comprehensible information from the staff when you asked questions? | 0.88 | 0.77 |
| Did you feel at ease in dealing with the staff? | 0.86 | 0.74 |
| Did you feel that your concerns were taken into account by the staff? | 0.84 | 0.71 |
| Were you informed by the staff about the outcome of the visit and the course of the health care pathway? | 0.84 | 0.71 |
| Were the staff competent during the outpatient visit? | 0.82 | 0.67 |
| Did you feel involved in decision making regarding treatment? | 0.81 | 0.66 |
| Were the staff courteous and helpful? | 0.81 | 0.65 |
| Where necessary, were you able to find a doctor who was willing to give you the information you needed? | 0.78 | 0.60 |
| Were you adequately informed about the outpatient visit modalities? | 0.75 | 0.57 |
| Did the staff respect your privacy needs during the visit? | 0.74 | 0.56 |
Abbreviation: HSOPE, Health Services OutPatient Experience.
Reliability
Reliability was analyzed as internal consistency for sub-sample 1 (n=788). Cronbach’s α estimate for the HSOPE questionnaire score was 0.95 (range of corrected item-total correlations =0.73–0.85), suggesting excellent internal consistency according to criteria proposed by Nunnally and Bernstein.37 In addition, all the corrected item-total score correlations were greater than 0.20, as recommended by Nunnally and Bernstein.37
Confirmatory factor analysis
CFA was performed with subsample 2 (n=731) to test the single-factor model found with the EFA. In subsample 2, the mean age was 59.05 years (SD =16.37 years), ranging from 17 to 93 years. Forty-eight percent were female outpatients. Eleven percent were young adults, 59% were adults, and 28% were older adults. Since the assumption of multivariate normality was violated, the estimation method of unweighted least squares was employed to conduct the CFA.
The χ2 test result was significant (χ235=18.22, P<0.01). However, as suggested by Jöreskog et al,43 the χ2 test is an index depending upon the sample size. Consequently, all the other indices were considered for goodness of fit. All the indices suggested good fit of the model to the data (GFI =0.99, AGFI =0.99, NFI =0.99, RFI =0.99, RMR =0.021).
Since the single-factor model showed good fit in all the considered indices, the results seemed to support the theoretical assumption of unidimensionality of the measure. An overview of fit indices for the single-factor model of the HSOPE questionnaire specified is provided in Table 4.
Table 4.
Fit indices of the HSOPE questionnaire for a single-factor model tested on subsample 2 (n=731)
| Model tested | χ2 (P-value) | GFI | AGFI | NFI | RFI | RMR |
|---|---|---|---|---|---|---|
| Single-factor model | 18.22* (0.001) | 0.99 | 0.99 | 0.99 | 0.99 | 0.021 |
Note:
P<0.05.
Abbreviations: HSOPE, Health Services OutPatient Experience; GFI, Goodness-of-Fit Index; AGFI, Adjusted GFI; NFI, Normed Fit Index; RFI, Relative Fit Index; RMR, root mean square residual.
Objective 2: Factor invariance across sex
A series of multisample CFA were conducted to simultaneously test the invariance of the single-factor structure of the HSOPE questionnaire across female and male outpatients. Subsample 2 was split into two groups based on sex: male outpatient group (n=351) and female outpatient group (n=380).
The χ2 test result for both the groups was significant. However, all the other indices supported a single factor for both the male and the female outpatient groups. An overview of fit indices for a single-factor model of the HSOPE questionnaire is provided in Table 5 for the male female outpatient groups.
Table 5.
Comparison of fit indices for a single-factor model of the HSOPE questionnaire across the male outpatient group and the female outpatient group extracted from subsample 2 (n=731)
| Model tested | χ2 (P-value) | GFI | AGFI | NFI | RFI | RMR |
|---|---|---|---|---|---|---|
| Single-factor model | ||||||
| Male outpatient group (n=351) | 11.73* (0.001) | 0.99 | 0.99 | 0.99 | 0.99 | 0.025 |
| Single-factor model | ||||||
| Female outpatient group (n=380) | 12.71* (0.001) | 0.99 | 0.99 | 0.99 | 0.99 | 0.026 |
Note:
P<0.05.
Abbreviations: HSOPE, Health Services OutPatient Experience; GFI, Goodness-of-Fit Index; AGFI, Adjusted GFI; NFI, Normed Fit Index; RFI, Relative Fit Index; RMR, root mean square residual.
Objective 3: HSOPE questionnaire items as predictors of overall satisfaction
Multiple linear regression analysis was conducted for the total study sample (n=1,519) to examine which HSOPE questionnaire items were significant predictors of overall satisfaction. Results suggested that item 9 (“Did you receive clear and comprehensible information from the staff when you asked questions?”), item 1 (“Were you adequately informed about the outpatient visit modalities?”), item 3 (“Were the staff competent during the outpatient visit?”), item 10 (“Were the staff courteous and helpful?”), item 2 (“Where necessary, were you able to find a doctor who was willing to give you the information you needed?”), item 4 (“Did you feel that your concerns were taken into account by the staff?”), and item 6 (“Did you feel involved in decision making regarding treatment?”), but not the other items of the questionnaire, significantly predicted overall satisfaction. An overview of estimates of the stepwise regression analysis is provided in Table 6.
Table 6.
Summary of statistics of regression analysis for the total study sample (n=1,519)
| Model | β | t | P-value | R2 |
|---|---|---|---|---|
| Constant | ||||
| Item 9 | 0.12 | 3.15 | 0.002 | |
| Item 1 | 0.18 | 5.48 | 0.001 | |
| Item 3 | 0.09 | 2.58 | 0.010 | 0.35 |
| Item 10 | 0.11 | 3.10 | 0.002 | |
| Item 4 | 0.11 | 2.92 | 0.004 | |
| Item 2 | 0.07 | 2.04 | 0.041 | |
Notes: HSOPE questionnaire items were entered as predictors, and overall satisfaction as the dependent variable. Only the items that resulted in significant predictors of satisfaction are reported.
Abbreviation: HSOPE, Health Services OutPatient Experience.
Discussion
In outpatient settings, the patient-centered care pathway is related to health outcomes in terms of clinical efficacy, treatment adherence, and cost efficiency.5–9 However, in the Italian health care field, patient-centeredness appears to be still understudied, and there is a lack of tools to measure the outcome of outpatient health care pathways from the patient’s perspective. Some research suggests that in our context, the doctor–patient relationship is still asymmetrical, with the latter being considered by health professionals to be a passive recipient of medical prescriptions.33 To our knowledge, in the Italian context, there is a lack of tools with reliable psychometric properties to assess the construct of patient-centeredness as a global concept.
In addition, to our knowledge, available instruments lack adequate psychometric evidence, due to the small size of samples and lack of data on factor structure from EFA or CFA analyses.28 Moreover, some of these tools focused only on patient-centered care in specific settings, such as psychiatric outpatient services,27 assessed satisfaction judgments exclusively,31 or assessed only the aspects of patient-centeredness related to communication.30
The current study presented a psychometric evaluation of the self-administered HSOPE questionnaire. Specifically, factorial validity and reliability were assessed. The HSOPE questionnaire is a general patient-centered outcome measure, aimed at assessing patient-centeredness as a global construct considered to be common to different types of outpatient settings. The HSOPE questionnaire is a brief tool, which can be administered by nursing staff, and these characteristics can make it suitable for outpatient settings. The measure contains statements related to perceived technical effectiveness of the staff (eg, “Were the staff competent during the outpatient visit?”), to information (eg, “Were you informed by the staff about the outcome of the visit and the course of the health care pathway?”), to relational aspects of outpatient–staff interaction (eg, “Did you feel that your concerns were taken into account by the staff?”), or involvement in decision making (eg, “Did you feel involved in decision making regarding treatment?”).
A strength of our study was that two large samples were used to test for factor structure with EFA and CFA procedures, respectively. Therefore, the ratio of number of participants to the number of items was satisfactory.24 The low rates of nonresponse found in our study suggest that the HSOPE questionnaire is an instrument with strong levels of feasibility and acceptability. The HSOPE questionnaire showed excellent psychometric properties. EFA and CFA strongly supported a single-factor solution of the questionnaire, which showed a clearly defined structure, as all the ten items had salient loadings (λn>|0.50|) on a single factor exclusively, and no cross-loadings were observed. In addition, the magnitude of the communalities suggested that a single factor explained a substantial proportion of variance in all items. A single-factor structure of the HSOPE questionnaire appeared to be invariant across sex, since it was supported for both male and female outpatient groups. Moreover, psychometric properties were supported by reliability as internal consistency, which was excellent. Results of the analyses suggested that patient-centered care may be viewed as a unidimensional construct, encompassing both aspects related to technical effectiveness, information, and relations with the staff and involvement in decision making. These findings appear to be in contrast with previous work on patient-centeredness tools for outpatient settings developed in other non-English-speaking countries,22 which suggested that patient-centered care is a multidimensional construct based on separate but correlated factors, such as communication, information, or clinical effectiveness.
A strength of our work was that the samples recruited represented all the adult age-groups, including young adults, adults, and older adults. Interestingly, young adult outpatients had significantly lower scores on perceived patient-centeredness compared to older adults. These findings appear consistent with the general evidence found in the literature, suggesting that older age is associated with greater satisfaction and perceived patient-centeredness.44,45
In contrast, no significant difference was found on perceived patient-centered care between male and female outpatients. This finding was consistent with previous research indicating that sex is not a significant predictor of satisfaction for outpatient visits.46
Limitations and future directions
Some limitations of the current study should be considered. First, we did not use comparator measures of patient-centeredness to assess the concurrent and discriminant validity of the HSOPE questionnaire. In addition, in our samples, not all the hospital facilities were represented, such as psychiatry facilities. In addition, outpatients from some facilities were underrepresented, such as outpatients from oncology and from gynecology facilities.
Another limitation concerns the fact that all the outpatients who participated in the study were recruited in a single site. Using a multisite design, future research should investigate psychometric properties of the HSOPE questionnaire in samples from community outpatient settings also. Despite an attempt being made in our study to examine differences in patient-centeredness as a function of sex or age-group, future research using the HSOPE questionnaire should investigate additional predictors of patient-centeredness, such as quality of life or self-efficacy in disease self-management. Finally, the HSOPE questionnaire could be adopted as a patient-centered outcome measure in research using randomized controlled trials evaluating the effectiveness of outpatient treatments.
Future research could use the questionnaire as a tool to evaluate efficacy of interventions aimed at increasing relational skills of health care professionals. The tool could also be used as an instrument to assess the efficacy of interventions aimed at improving the organizational well-being of health care professionals. These implications could be related to the close link between patient-centeredness and patient health,47,48 and between patient-centeredness and work-related well-being of the staff.49
In conclusion, the current study is the first to our knowledge to present an instrument to measure patient-centeredness as a global construct for a variety of outpatient settings in the Italian context. The HSOPE questionnaire seems to have reliable psychometric properties and to be a promising tool to inform policy making, since the Italian health care context is still characterized by the biomedical framework.
Acknowledgments
This research was not supported by any institutional grant. The research was approved by Dr Pietro Manzi, MD, director of the Medical Directorate of the Santa Maria alle Scotte University Hospital of Siena. No approval from the ethical committees was requested, since the research involved only the completion of the HSOPE questionnaire through an anonymous format, and did not involve any experiment or intervention on participants. Before completing the questionnaire, all the participants were provided with information on the aims of the study by the nurses who administered the measure.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Mead N, Bower P. Patient-centeredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 2.Mead N, Bower P, Hann M. The impact of general practitioners’ patient-centredness on patients’ post-consultation satisfaction and enablement. Soc Sci Med. 2000;55(2):283–299. doi: 10.1016/s0277-9536(01)00171-x. [DOI] [PubMed] [Google Scholar]
- 3.Epstein RM, Franks P, Fiscella K, et al. Measuring patient-centered communication in patient-physician consultations: theoretical and practical issues. Soc Sci Med. 2005b;61(7):1516–1528. doi: 10.1016/j.socscimed.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 4.Bertakis KD, Azari R. Determinants and outcomes of patient-centered care. Patient Educ Couns. 2011;85(1):46–52. doi: 10.1016/j.pec.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 5.Clever SL, Ford DE, Rubenstein LV, et al. Primary care patients’ involvement in decision-making is associated with improvement in depression. Med Care. 2006;44(5):398–405. doi: 10.1097/01.mlr.0000208117.15531.da. [DOI] [PubMed] [Google Scholar]
- 6.Joosten EA, DeFuentes-Merillas L, de Weert GH, Sensky T, van der Staak CP, de Jong CA. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother Psychosom. 2008;77(4):219–226. doi: 10.1159/000126073. [DOI] [PubMed] [Google Scholar]
- 7.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groene O. Patient centredness and quality improvement efforts in hospitals: rationale, measurement, implementation. Int J Qual Health Care. 2011;23(5):531–537. doi: 10.1093/intqhc/mzr058. [DOI] [PubMed] [Google Scholar]
- 9.Kinmonth AL, Woodcock A, Griffin S, Spiegal N, Campbell MJ. Randomised controlled trial of patient centred care of diabetes in general practice: impact on current well-being and future disease risk. The Diabetes Care From Diagnosis Research Team. BMJ. 1998;317(7167):1202–1208. doi: 10.1136/bmj.317.7167.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70(4):351–379. doi: 10.1177/1077558712465774. [DOI] [PubMed] [Google Scholar]
- 11.van Dam HA, van der Horst F, van den Borne B, Ryckman R, Crebolder H. Provider-patient interaction in diabetes care: effects on patient self-care and outcomes. A systematic review. Patient Educ Couns. 2003;51(1):17–28. doi: 10.1016/s0738-3991(02)00122-2. [DOI] [PubMed] [Google Scholar]
- 12.Gowen CR, 3rd, McFadden KL, Hoobler JM, Tallon WJ. Exploring the efficacy of healthcare quality practices, employee commitment, and employee control. J Oper Manag. 2006;24(6):765–778. [Google Scholar]
- 13.Epstein RM, Franks P, Shields CG, et al. Patient-centered communication and diagnostic testing. Ann Fam Med. 2005;3(5):415–421. doi: 10.1370/afm.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wensing M, Jung HP, Mainz J, Olesen F, Grol R. A systematic review of the literature on patient priorities for general practice care. Part 1: Description of the research domain. Soc Sci Med. 1998;47(10):1573–1588. doi: 10.1016/s0277-9536(98)00222-6. [DOI] [PubMed] [Google Scholar]
- 15.Castle NG, Brown J, Hepner KA, Hays RD. Review of the literature on survey instruments used to collect data on hospital patients’ perceptions of care. Health Serv Res. 2005;40(6 Pt 2):1996–2017. doi: 10.1111/j.1475-6773.2005.00475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Askham J, Chisholm A. What Do You Think of Your Doctor? A Review of Questionnaires for Gathering Patients’ Feedback on Their Doctor. Oxford: Picker Institute Europe; 2006. [Google Scholar]
- 17.Avis M, Bond M, Arthur A. Questioning patient satisfaction: an empirical investigation in two outpatient clinics. Soc Sci Med. 1997;44(8):85–92. [Google Scholar]
- 18.Williams B. Patient satisfaction: a valid concept? Soc Sci Med. 1994;38(4):509–516. doi: 10.1016/0277-9536(94)90247-x. [DOI] [PubMed] [Google Scholar]
- 19.Zolnierek KB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elwyn G, Edwards A, Mowle S, et al. Measuring the involvement of patients in shared decision-making: a systematic review of instruments. Patient Educ Couns. 2001;43(1):5–22. doi: 10.1016/s0738-3991(00)00149-x. [DOI] [PubMed] [Google Scholar]
- 21.Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 22.Gasquet I, Villeminot S, Estaquio C, Durieux P, Ravaud P, Falissard B. Construction of a questionnaire measuring outpatients’ opinion of quality of hospital consultation departments. Health Qual Life Outcomes. 2004;2:43. doi: 10.1186/1477-7525-2-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol Assess. 1995;7(3):286–299. [Google Scholar]
- 24.Oltedal S, Garratt A, Bjertnaes Ø, Bjørnsdottìr M, Freil M, Sachs M. The NORPEQ patient experiences questionnaire: data quality, internal consistency and validity following a Norwegian inpatient survey. Scand J Public Health. 2007;35(5):540–547. doi: 10.1080/14034940701291724. [DOI] [PubMed] [Google Scholar]
- 25.Skudal KE, Garratt AM, Eriksson B, Leinonen T, Simonsen J, Bjertnaes OA. The Nordic Patient Experiences Questionnaire (NORPEQ): cross-national comparison of data quality, internal consistency and validity in four Nordic countries. BMJ Open. 2012;2(3):e000864. doi: 10.1136/bmjopen-2012-000864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coban IG, Kasikci M. Reliability and validity of the scale of patient perception of hospital experience with nursing care in a Turkish population. J Clin Nurs. 2010;19(13–14):1929–1934. doi: 10.1111/j.1365-2702.2009.03125.x. [DOI] [PubMed] [Google Scholar]
- 27.Ruggeri M, Lasalvia A, Dall’Agnola R, et al. Development, internal consistency and reliability of the Verona Service Satisfaction Scale – European version EPSILON Study 7. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl. 2000;177(39):s41–s48. doi: 10.1192/bjp.177.39.s41. [DOI] [PubMed] [Google Scholar]
- 28.Gigantesco A, Chiaia E, Morosini P, Balbi A. Validation study of an instrument for the evaluation of patients and relatives opinion in mental health services. J Psychopathol. 2003;9(1):17–22. Italian. [Google Scholar]
- 29.Tabachnick BG, Fidell LS. Using Multivariate Statistics. New York: Harper Collins; 1996. [Google Scholar]
- 30.Gremigni P, Sommaruga M, Peltenburg M. Validation of the Health Care Communication Questionnaire (HCCQ) to measure outpatients’ experience of communication with hospital staff. Patient Educ Couns. 2008;71(1):57–64. doi: 10.1016/j.pec.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 31.Cioffi R, Coluccia A, Ferretti F, Lorini F, Saggino A, Furnham A. A psychometric study of the Quality Perception Questionnaire. Swiss J Psychol. 2012;71(2):101–106. [Google Scholar]
- 32.Vegni E, Martinoli M, Moja EA. Improving patient-centred medicine: a preliminary experience for teaching communication skills to Italian general practitioners. Educ Health (Abingdon) 2002;15(1):51–57. doi: 10.1080/13576280110107314. [DOI] [PubMed] [Google Scholar]
- 33.Lamiani G, Meyer EC, Rider EA, et al. Assumptions and blind spots in patient-centredness: action research between American and Italian health care professionals. BMC Med Educ. 2008;42(7):712–720. doi: 10.1111/j.1365-2923.2008.03038.x. [DOI] [PubMed] [Google Scholar]
- 34.Goss C, Mosconi P, Renzi C, Deledda G. Participation of patients and citizens in healthcare decisions in Italy. Z Evid Fortbild Qual Gesundhwes. 2011;105(4):277–282. doi: 10.1016/j.zefq.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 35.Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14(5):353–358. doi: 10.1093/intqhc/14.5.353. [DOI] [PubMed] [Google Scholar]
- 36.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. [Google Scholar]
- 37.Nunnally J, Bernstein I. Psychometric Theory. New York: McGraw-Hill; 1994. [Google Scholar]
- 38.Bollen KA. Structural Equations with Latent Variables. New York: John Wiley & Sons; 1989. [Google Scholar]
- 39.Anderson JC, Gerbing DW. Structural equation modeling in practice: a review and recommended two-step approach. Psychol Bull. 1998;103(3):411–423. [Google Scholar]
- 40.Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39(1):31–36. [Google Scholar]
- 41.Bartlett MS. A note on the multiplying factors for various χ2 approximation. J R Stat Soc Series B Stat Methodol. 1954;16:296–298. [Google Scholar]
- 42.Muthén B, Kaplan D. A comparison of some methodologies for the factor analysis of non-normal Likert variables. Br J Math Stat Psychol. 1985;38(2):171–189. [Google Scholar]
- 43.Jöreskog K, Sörbom D, du Toit S, et al. LISREL 8: New Statistical Features. Lincolnwood: Scientific Software International; 2000. [Google Scholar]
- 44.Bauld L, Chesterman J, Judge K. Measuring satisfaction with social care amongst older service users: issues from the literature. Health Soc Care Community. 2000;8(5):316–324. doi: 10.1046/j.1365-2524.2000.00256.x. [DOI] [PubMed] [Google Scholar]
- 45.Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609–620. doi: 10.1016/s0277-9536(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 46.Säilä T, Mattila E, Kaila M, Aalto P, Kaunonen M. Measuring patient assessments of the quality of outpatient care: a systematic review. J Eval Clin Pract. 2008;14(1):148–154. doi: 10.1111/j.1365-2753.2007.00824.x. [DOI] [PubMed] [Google Scholar]
- 47.Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004;2(6):595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Haskard KB, Williams SL, DiMatteo MR, Rosenthal R, White MK, Goldstein MG. Physician and patient communication training in primary care: effects on participation and satisfaction. Health Psychol. 2008;27(5):513–522. doi: 10.1037/0278-6133.27.5.513. [DOI] [PubMed] [Google Scholar]
- 49.Leiter PM, Harvie P, Frizzell C. The correspondence of patient satisfaction and nurse burnout. Soc Sci Med. 1998;47(3):1611–1617. doi: 10.1016/s0277-9536(98)00207-x. [DOI] [PubMed] [Google Scholar]


