Abstract
OBJECTIVE
This study analyzed data from a randomized trial to examine the impact on medication adherence of integrated treatment delivered via assertive community treatment (ACT) versus standard clinical case management (SCCM).
METHOD
Data from the original study included 198 study participants with co-occurring psychotic and substance use disorders who were randomly assigned to receive integrated treatment via ACT or SCCM and were followed for 3 years. We applied mixed-effects logistic regression to estimate group (ACT vs. SCCM) by time effects on a self-report measure of medication adherence. Adherence was dichotomized as 20% or more missed medication days (“poor adherence”) versus less than 20% missed medication days (“adequate adherence”).
RESULTS
Participants who were assigned to ACT reported significant improvement in medication adherence compared with those assigned to SCCM.
CONCLUSIONS
Integrated treatment delivered via ACT may benefit persons with co-occurring psychotic and substance use disorders who are poorly adherent to medications.
Keywords: assertive community treatment (ACT), dual disorders, medication adherence, chronic mental illness
Psychiatric medication can be a core part of treatment for people with severe mental illness. However, because of side effects and clinical factors, the risk of nonadherence to medications is high. Among individuals with schizophrenia, estimates of nonadherence range from 25% to 75% (Nose, Barbui, & Tansella, 2003). Nonadherence rates for individuals with co-occurring severe mental illness and substance use disorders may be even higher because of the added impairment associated with chronic substance use (Mueser, Noordsy, Drake, & Fox, 2003).
Research on integrated treatment shows promising results for individuals with co-occurring disorders in comparison with standard care on several clinical and functional outcomes (Drake, Mueser, Brunette, & McHugo, 2004; Drake, O’Neal, & Wallach, 2008). Because of its strong evidence base (Marshall & Lockwood, 2010; Mueser, Bond, Drake, & Resnick, 1998), assertive community treatment (ACT) has been viewed as an optimal treatment in which to deliver integrated services. ACT is distinct from standard case management (SCM) for several reasons (Phillips et al., 2001). ACT has a lower caseload ratio (approximately 1:10 for ACT compared with 1:20 or higher for SCM), maintains shared caseloads among team members instead of individual caseloads, and delivers services in the community rather than in a clinic. ACT also provides direct services via a multidisciplinary team rather than brokering services to other providers and maintains 24-hour responsibility of care for clients rather than daytime responsibility.
One of the key mechanisms of action that differentiates ACT from SCM is close medication management and monitoring (McGrew, Pescosolido, & Wright, 2003). It is hypothesized that improved clinical outcomes, namely, reducing hospitalization, associated with ACT models may be because of improved medication adherence (Mueser et al., 1998; Zygmunt, Olfson, Boyer, & Mechanic, 2002). However, the effect of ACT on medication adherence is not yet established. Despite more than 30 randomized trials of ACT, few have included assessments of medication adherence (Mueser et al., 1998; Zygmunt et al., 2002).
Among studies that have examined medication adherence as an outcome, the results are promising yet inconclusive, with four of seven studies showing significant improvements in adherence in favor of ACT (Zygmunt et al., 2002). A more recent systematic review of integrated treatments for co-occurring disorders found one of six randomized controlled trials that examined medication adherence as an outcome (Drake et al., 2008). This study compared integrated mental health and substance use case management with usual treatment in a sample of 182 recently released inmates with co-occurring disorders; however, the definition of medication adherence was the mean number of hours of outpatient medication services received instead of whether the medications were taken as prescribed (Chandler & Spicer, 2006). Thus, further research is warranted on the impact of integrated treatment on medication adherence among co-occurring populations. To address this gap in the literature and to evaluate the impact that providing integrated treatment via ACT services had on medication adherence, we examined data from a randomized trial of integrated treatment provided to people with co-occurring disorders via ACT versus standard clinical case management (SCCM; Essock et al., 2006).
Method
We analyzed data from the Connecticut Co-Occurring Disorders Study, a 3-year randomized controlled trial comparing two methods for delivering integrated mental health and substance abuse treatment to 198 individuals with co-occurring psychotic and substance use disorders. The design of the parent study is described fully elsewhere (Essock et al., 2006), and summarized briefly here. All elements of the study protocol, in addition to this secondary analysis, were reviewed and approved by the institutional review boards of the Connecticut Department of Mental Health and Addiction Services, Columbia University, and New York State Psychiatric Institute.
Clients were recruited from two publicly funded outpatient mental health centers in low-income, urban areas of Connecticut (Essock et al., 2006). To be eligible for the study, clients had to have a psychotic disorder; active substance abuse or dependence; high service use in the past 2 years, including two or more of the following: psychiatric hospitalizations, stays in psychiatric crisis or respite program, emergency department visits, or incarceration; been homeless or unstably housed; no pending legal charges, severe medical conditions, or mental retardation; were scheduled for discharge into the community if currently an inpatient; and were willing to provide written informed consent. Participants were enrolled in the study between August 1993 and July 1998, and subsequently followed every 6 months for 3 years.
Through referrals from case managers, eligible and consenting participants completed a baseline interview and were randomized to either ACT or SCCM. Following randomization, self-report data were collected from participants every 6 months for 3 years. Trained clinicians administered the research assessments and attended regular supervision provided by seasoned interviewers. Briefly, 244 of 382 participants met eligibility criteria for the study. There were 205 participants who completed the baseline assessment and were randomly assigned to one of two conditions within both sites. For various administrative reasons (forensic evaluation, different diagnosis on reevaluation, refusal), 7 of these participants discontinued their participation in the study. The final sample size was 198, with 99 in each condition. Of the 198 clients, 179 participated in at least one research assessment every 6 months for a 3-year period. Completion rates for individual follow-up assessments ranged from 86% to 90%. The remaining 19 (10%) of the original 198 clients were lost to follow-up: 5 withdrew from the study or refused to participate, 6 died, and 8 moved to another state without further contact. No significant differences in completion rates of the last assessment at 36 months were found between the treatment conditions. Approximately 13% in the ACT group versus 14% in the SCCM group did not complete the last 36-month assessment.
The ACT condition was structured to optimize treatment engagement and adherence. In this study, ACT was based on standard principles from the original model as described above adapted for co-occurring disorders. Training included direct substance abuse treatment, stagewise treatment for co-occurring disorders, and a team approach with clients with co-occurring disorders.
The SCCM teams consisted of experienced clinicians with a variety of clinical backgrounds. Members of the SCCM team carried individual caseloads as opposed to shared caseloads, although they did emphasize a team approach by meeting together regularly and discussing cases. Although some of the services were provided directly to SCCM clients in the community, most services were referred to other agencies given the higher caseloads for SCCM clinicians (almost twice as the caseloads of ACT clinicians). Both ACT and SCCM were actively in use prior to the start of the study. Staff from both treatment conditions received extensive training and technical assistance in implementing integrated treatment for co-occurring mental health and substance abuse disorders, including comprehensive assessment, motivational interviewing, group treatment, and stagewise interventions (Mueser et al., 2003).
Measurement
We measured psychiatric medication adherence using a self-report measure of the number of missed medication days. At each assessment, participants were asked to report the number of days in the past 6 months they missed any of their prescribed psychiatric medications. For the analysis, we first examined adherence as a count variable. However, because of the highly skewed distributions (>50% in each group reported no missed medication days across the study period), we dichotomized adherence as self-report of 20% or more missed medication days (poor adherence, coded as 1) versus self-report of less than 20% missed medication days (adequate adherence, coded as 0). This definition includes cutoff values that are similar to those identified as clinically meaningful by the American Psychiatric Association (Kane, Leucht, & Carpenter, 2003) and used in other studies (Becker, Young, Ochshorn, & Diamond, 2007; Gilmer et al., 2004).
Data Analysis
We evaluated longitudinal effects using mixed-effects logistic and Poisson regression models, with the repeated observations of a given study participant nested within the individual (Bryk & Raudenbush, 1992). Mixed-effect models account for correlation that is common in longitudinal data sets, including repeated measures of the same person. We treated time as continuous (months following baseline) and transformed the log estimates from the regression models to odds ratios or incidence rate ratios. We evaluated the impact of integrated treatment delivered via ACT versus SCCM on self-reported medication adherence using group by time interactions, because we expected the equivalent groups at baseline to diverge over time. Before building the models, we plotted the distribution of adherence over time to determine whether to fit linear or quadratic time effects. For plots that showed curvilinear patterns, we created quadratic mixed-effects models, including time2 and group by time2 terms. We compared linear with the quadratic models using the chi-square statistic to evaluate the change in log likelihood between the models. As a possible mediating factor of ACT, we explored medication assistance, defined as whether clients had anyone to help them take their medication. A preliminary analysis found no significant treatment differences in medication assistance, a condition necessary for mediation analysis (MacKinnon, Fairchild, & Fritz, 2007). We used the SuperMix program for mixed-effects models to analyze the treatment effects of medication adherence through time.
Results
Sample Characteristics
An earlier publication reported characteristics of the overall sample and by group (Essock et al., 2006). Briefly, participants in each group did not differ in terms of demographics, psychiatric characteristics, and measures of substance use, with one notable exception. On a measure indicating progression in treatment, the Substance Abuse Treatment Scale, participants assigned to ACT were rated by clinicians as having less treatment involvement at baseline compared with those assigned to SCCM.
At baseline, study participants reported that they missed taking their medications an average of 14.4 days/month (SD = 30.5 days/month), those assigned to ACT reported missing an average of 17.9 days/month (SD = 32.3 days/month), and those assigned to SCCM reported missing an average of 11 days/month (SD = 28.4 days/month). Approximately, 21% (n = 20) of participants assigned to ACT reported poor adherence to their medications (i.e., missed 20% or more of their medication days), compared with 11% (n = 10) of participants assigned to SCCM (p < .05). We adjusted for these baseline differences in the mixed-effects regression models. Based on a review of chart data, 52% (n = 103) of clients were on first-generation antipsychotics (FGAs; n = 48 of whom were on long-acting injectables), and 48% (n = 95) were on second-generation antipsychotics (SGAs). The rates of FGAs and SGAs did not differ significantly between the two conditions.
Self-Reported Medication Adherence Through Time
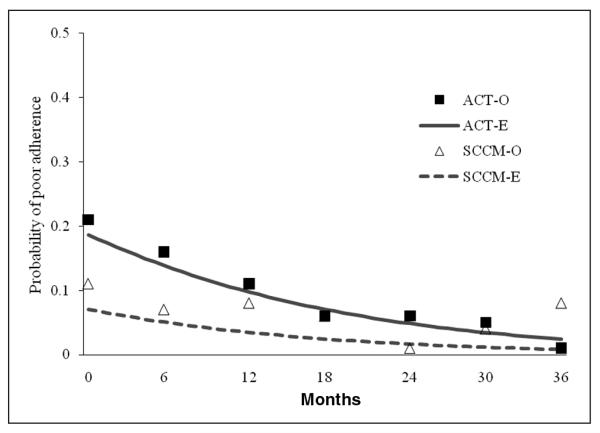
The quadratic models did not yield a significant change in log likelihood over linear models for any of the comparisons; hence we report the linear models here. The mixed-effects logistic regression model found treatment group differences over time. Participants assigned to ACT had a reduced likelihood of poor adherence (e.g., missed 20% or more of their medication days) over time compared with those who were assigned to SCCM (odds ratio [OR] = 0.95; 95% confidence interval [CI] = 0.91-0.99; p < .05; Figure 1). The mixed-effects Poisson model produced similar results, a significant group by time effect favoring ACT (incidence rate ratio = .97; 95% CI = 0.96-0.97, p < .01). We used Cohen’s arcsine calculation for proportions to compare the magnitude of the difference between the two groups and found a moderate effect (−.37), indicating that the ACT group as a whole had a greater decrease in the likelihood of having poor adherence than did the SCM group (Cohen, 1988).
Figure 1.
Estimated (E) and observed (O) probability values of poor adherence over time and treatment group Note. ACT = assertive community treatment; SCCM = standard clinical case management.
Discussion
Integrated treatment for people with co-occurring disorders delivered via ACT improved self-reported adherence to medication at a greater rate through time compared with integrated treatment delivered via SCCM. These findings provide suggestive support and extend previous findings from experimental and quasi-experimental studies that favored ACT over case management with respect to medication adherence (Zygmunt et al., 2002). ACT may be an important vehicle to improve medication adherence among clients with co-occurring disorders, especially those who are least adherent to medications. Although the parent study concluded that integrated treatment for individuals with co-occurring disorders could be successfully delivered either with ACT or SCCM, ACT did offer an advantage in reducing institutionalization in systems where rates of institutionalization were high (Essock et al., 2006). In this report, we see an additional potential advantage for ACT for those who are poorly adherent to psychiatric medications. Because evidence-based treatments such as ACT are in short supply, understanding who benefits from which of these treatments helps with allocation decisions.
Although the study reported here had significant strengths, including its randomized design and high retention rate of study participants through the 3-year follow-up period, there are a number of limitations worth noting. First, psychiatric medication adherence was measured using self-report rather than a more objective assessment. It is notable, however, that a previous analysis of this sample found relatively high concordance (80% to 84% agreement overall) between self-report of drug use and urine toxicology screens (Jackson, Covell, Frisman, & Essock, 2004), suggesting that these participants may have felt comfortable providing accurate information about sensitive topics to the independent raters in this study. Future studies should include multiple methods of assessing medication adherence when possible, with at least one of these being a direct or objective measure of adherence (i.e., pill count, refill monitoring, electronic monitoring, etc.; Velligan et al., 2006).
In addition, the impact that SGA medications had on medication adherence is unknown. Although some research has suggested that SGA medications may be associated with a longer time to discontinuation because of fewer side effects (Osterberg & Blaschke, 2005), other trials have reported similar rates of discontinuation, in most respects, between FGAs and SGAs with the exception of olanzapine (Lieberman et al., 2005). In the current study, we found similar rates of FGAs and SGAs between the treatment conditions, and thus, the potential impact of SGA on adherence, if any, is unlikely.
Finally, it is unfortunate that, by chance, randomization did not balance the two conditions with respect to the baseline measure of adherence. Although we adjusted for baseline differences in the analyses, there was a larger potential for improvement in adherence for those assigned to ACT compared with SCCM, and the improvement seen for SCCM may have been limited by a “floor” effect. Even so, the intervention showed a moderate effect (−.37), decreasing poor adherence rates from 20% to less than 10% (as was the case for participants assigned to ACT) might be experienced as a clinically meaningful improvement. Conversely, individuals assigned to SCCM tended to hover around or just below 10% poor adherence throughout the study. ACT clients are severely impaired with multiple, complex needs, and medication adherence may be more challenging for these individuals compared with those receiving traditional services. Medication management and monitoring are cornerstones of the ACT model and may help clients achieve adherence levels that are similar to those among less severe clients in traditional care. Future research is needed to understand how medication management and adherence strategies are tailored for co-occurring disorders and to examine the benefit of such strategies as a primary outcome of integrated treatment and treatment delivery.
Conclusion
ACT appears to increase medication adherence for clients with co-occurring disorders who are poorly adherent to psychiatric medications. Improved adherence may be a reflection of greater insight and self-management skills, or it may be because of different types of monitoring strategies employed by clinicians. Such strategies as medication delivery and close supervision are commonplace in ACT and may contribute to improved adherence. Our findings did not support medication assistance as an intervening variable, which suggests the possibility of other mechanisms. For example, therapeutic alliance has been touted as critical in discussing medication issues in a collaborative and supportive manner (Aquila, Weiden, & Emmanuel, 1999). Future research should examine the actual practices of medication monitoring in relation to adherence and the extent to which these practices are engaging versus leveraged. Likewise, the contribution of other mechanisms, such as the type of insight, attitudes, and self-management skills, are important to clarify in future studies to gain a better understanding of the intervention effects.
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: This research was supported by the New York State Office of Mental Health Policy Scholar Awards Program and U.S. Public Health Services grants T32-MH-014623, R01-MH-52872 and R01-MH-63463 from the National Institute of Mental Health, R01-AA-10265 from the National Institute on Alcohol Abuse and Alcoholism, and UD3-SM51560, UD3-SM51802, and UD9-MH51958 from the Substance Abuse and Mental Health Services Administration.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
References
- Aquila R, Weiden PJ, Emmanuel M. Compliance and the rehabilitation alliance. Journal of Clinical Psychiatry. 1999;60(Suppl. 19):23–27. [PubMed] [Google Scholar]
- Becker MA, Young MS, Ochshorn E, Diamond R. The relationship of antipsychotic medication class and adherence with treatment outcomes and costs for Florida Medicaid beneficiaries with schizophrenia. Administration of Policy in Mental Health and Mental Health Services Research. 2007;34:307–314. doi: 10.1007/s10488-006-0108-5. [DOI] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models: Applications and data analysis methods. Sage; Newbury Park, CA: 1992. [Google Scholar]
- Chandler D, Spicer G. Integrated treatment for recidivists with co-occurring psychiatric and substance use disorders. Journal of Substance Abuse Treatment. 2006;42:405–425. doi: 10.1007/s10597-006-9055-6. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum; Mahwah, NJ: 1988. [Google Scholar]
- Drake RE, Mueser KT, Brunette MF, McHugo GF. A review of treatments for people with severe mental illnesses and co-occurring substance use disorders. Psychiatric Rehabilitation Journal. 2004;27:360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- Drake RE, O’Neal EL, Wallach MA. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. Journal of Substance Abuse Treatment. 2008;34:123–138. doi: 10.1016/j.jsat.2007.01.011. [DOI] [PubMed] [Google Scholar]
- Essock SM, Mueser KT, Drake RE, Covell NH, McHugo GJ, Frisman LK, Swain K. Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatric Services. 2006;57:185–196. doi: 10.1176/appi.ps.57.2.185. [DOI] [PubMed] [Google Scholar]
- Gilmer TP, Dolder CR, Lacro JP, Folsom DP, Lindamer L, Garcia P, Jeste DV. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. American Journal of Psychiatry. 2004;161:692–699. doi: 10.1176/appi.ajp.161.4.692. [DOI] [PubMed] [Google Scholar]
- Jackson CT, Covell NH, Frisman LK, Essock SM. Validity of self-reported drug use among people with co-occurring mental health and substance use disorders. Journal of Dual Diagnosis. 2004;1:49–63. [Google Scholar]
- Kane JM, Leucht S, Carpenter D. Expert consensus guidelines for optimizing pharmacologic treatment of psychotic disorders. Journal of Clinical Psychiatry. 2003;64:S95–S100. [PubMed] [Google Scholar]
- Lieberman JA, Stroup TS, McEvoy JP, Swartz MP, Rosenheck RA, Perkins DO, Hsiao JK. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine. 2005;353:1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall M, Lockwood A. Assertive community treatment for people with severe mental disorders. Cochrane Database of Systematic Reviews. 2010;3:CD001089. doi: 10.1002/14651858.CD001089. [DOI] [PubMed] [Google Scholar]
- McGrew JH, Pescosolido B, Wright E. Case managers’ perspectives on critical ingredients of assertive community treatment and on its implementation. Psychiatric Services. 2003;54:370–376. doi: 10.1176/appi.ps.54.3.370. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Bond GR, Drake RE, Resnick SG. Models of community care for severe mental illness: A review of research on case management. Schizophrenia Bulletin. 1998;24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Noordsy DL, Drake RE, Fox L. Integrated treatment for dual disorders: A guide to effective practice. Guilford Press; New York, NY: 2003. [Google Scholar]
- Nose M, Barbui C, Tansella M. How often do patients with psychosis fail to adhere to treatment programmes? A systematic review. Psychological Medicine. 2003;33:1149–1160. doi: 10.1017/s0033291703008328. [DOI] [PubMed] [Google Scholar]
- Osterberg L, Blaschke T. Adherence to medication. New England Journal of Medicine. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Phillips SD, Burns BJ, Edgar ER, Mueser KT, Linkins KW, Rosenheck RA, McDonel Herr EC. Moving assertive community treatment into standard practice. Psychiatric Services. 2001;52:771–779. doi: 10.1176/appi.ps.52.6.771. [DOI] [PubMed] [Google Scholar]
- Velligan DI, Lam Y-WF, Glahn DC, Barrett JA, Maples NJ, Ereshefsky L, Miller AL. Defining and assessing adherence to oral antipsychotics: A review of the literature. Schizophrenia Bulletin. 2006;32:724–742. doi: 10.1093/schbul/sbj075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zygmunt A, Olfson M, Boyer CA, Mechanic D. Interventions to improve medication adherence in schizophrenia. American Journal of Psychiatry. 2002;159:1653–1664. doi: 10.1176/appi.ajp.159.10.1653. [DOI] [PubMed] [Google Scholar]