Currently, the 2 forms of peritoneal dialysis (PD) used worldwide are automated peritoneal dialysis (APD) and continuous ambulatory peritoneal dialysis (CAPD). For stable patients in the ambulatory clinic setting, the choice of modality is primarily based on patient and physician preferences. Patients’ choice of modality may depend on lifestyle whereas physicians’ preferences are based on clinical need as well as the logistical preferences of the patient. In addition, studies have suggested that patients’ survival and yearly incidence of infectious complications are similar between the two modalities (1-3). However, some recent studies have suggested an improvement in technical survival in patients receiving APD compared to CAPD (4,5). Based on these cross-sectional studies as well as clinical experience, it is clear that either modality is suitable for stable patients with end-stage renal disease (ESRD) in the chronic ambulatory setting.
Although both modalities of PD are well established in the ambulatory setting, the use of APD and CAPD in patients unable to self-care in the inpatient service is less clear. To date, there is a dearth of studies delineating patient outcomes for the use of either modality in this cohort of patients. Furthermore, patients in the inpatient setting are frequently unable to self-administer APD or CAPD, thereby transferring the burden to nephrology staff at all hours of the day. As an alternative to the traditional APD and CAPD procedures, we propose the use of a manifold procedure for the delivery of inpatient PD. Although employed by nephrologists worldwide, a technical description of the procedure is lacking in the literature. The manifold procedure entails the use of a multi-line tubing set that allows for the connection of 5 to 9 2-L dialysate bags (any volume dialysate bags may be employed). The manifold set is prepared in the PD unit and then transported to the inpatient setting. At the patient bedside, the patient is aseptically connected to the manifold with the hospital floor nurses managing the delivery of the dialysate by unclamping infusion bags. The objective of this report is to describe the manifold procedure in more detail and to report our experience with this technique for the past 2 decades.
Materials and Methods
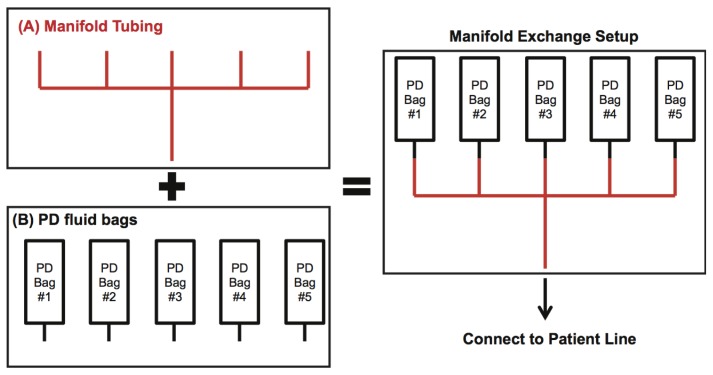
We have streamlined the preparation of manifold exchange to perform it safely with minimal time commitment from the PD nursing staff. Equipment required for the setup of the manifold exchange is listed in Figure 1. After the appropriate PD regimen is prescribed for the patient and all the listed equipment in Figure 1 is acquired, proper setup of the manifold exchange is dependent on the following components in chronological order: preparing the manifold set, priming the manifold set, connecting the manifold set, infusing the dialysate solution, and maintenance of manifold exchange by the floor nurse (Table 1). A video link summarizing the setup is available: http://www.youtube.com/watch?v=efqUKfTXEZM&feature=em-upload_owner-action=share. Prior to using the dialysate bags, they must all be checked for the components listed in Table 1. The preparation of the manifold set is based on the connection of the dialysate bags to the manifold tubing, with all dialysate lines combining to a single distal line, which is connected to the patient line (Figure 2).
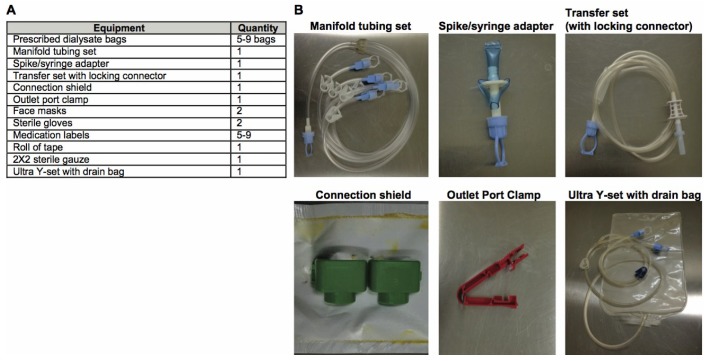
Figure 1 —
Equipment required to set up the manifold exchange. (A) Includes a list of the equipment required to initiate manifold. (B) Images of the key equipment required for initiation of manifold peritoneal dialysis.
TABLE 1.
Flowsheet for Proper Set-Up of Manifold Exchange
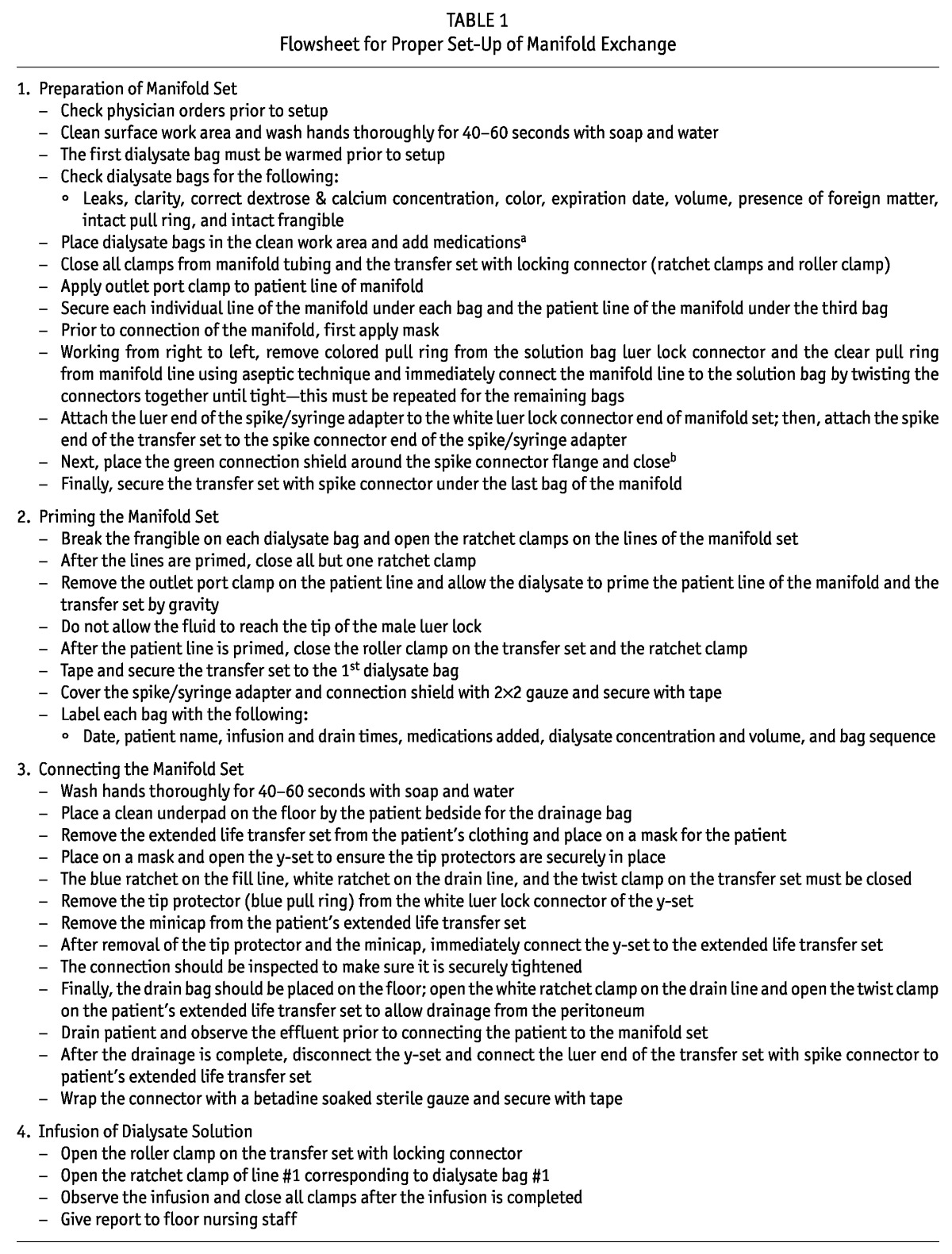
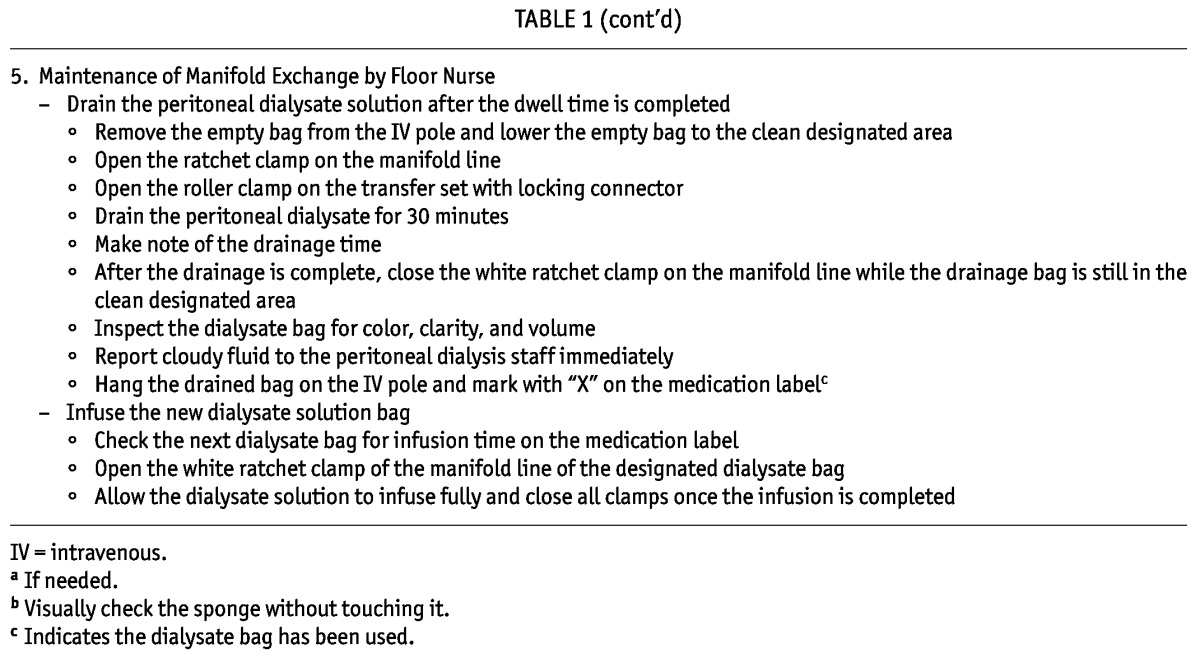
Figure 2 —
Schematic of manifold exchange setup. The manifold exchange setup is based on the connection between the PD dialysate bags to manifold tubing. All lines arising from the connection between the manifold tubing and dialysate bags combine distally to join the patient line. PD = peritoneal dialysis.
Priming the Manifold Exchange
Prior to starting the manifold exchange, each of the dialysate bags must be primed prior to use, thereby eliminating the need to flush the line prior to “filling” the peritoneum later during the exchange. Priming of the manifold set is described in detail in Table 2. After priming the manifold exchange, all bags must be labeled as shown in Figure 3A and transported from the work surface area to the patient’s bedside on a cart as shown in Figure 3B. Finally, each dialysate bag must be hung on the IV pole in reverse order, starting with the last dialysate bag as shown in Figure 3C.
TABLE 2.
Checklist Prior to Leaving the Patient’s Bedside
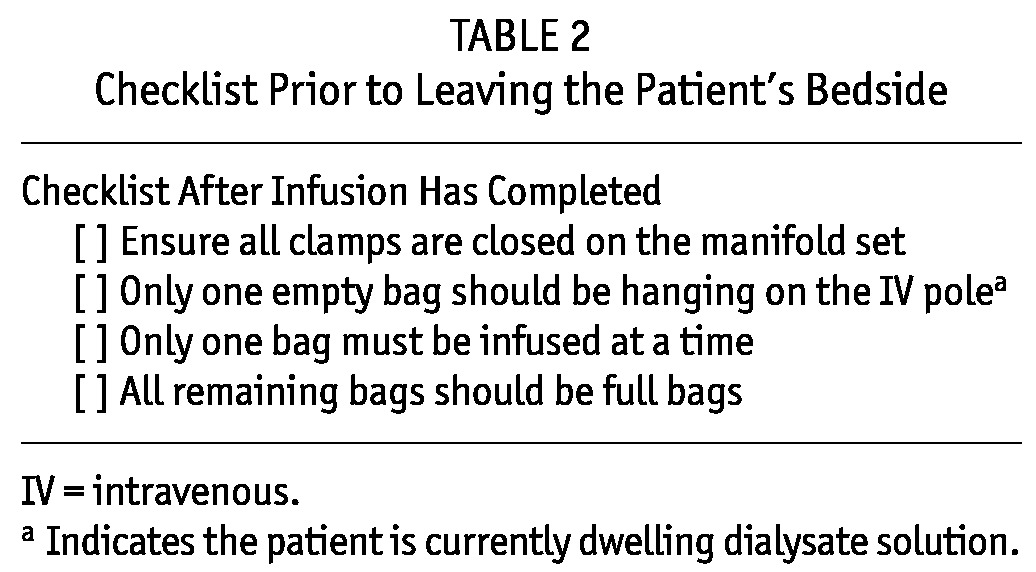
Figure 3 —
Initiation and management of manifold exchange. (A) Preparation of dialysate bags using the manifold tubing set. (B) Transport of manifold set with supplies for connection at patient bedside. (C) Each dialysate bag is hung on the IV pole in reverse order, starting with the last dialysate bag. (D) Connect the transfer set to patient’s extended life transfer set and the connector is wrapped with a betadine-soaked sterile gauze and secured with tape. (E) Patient’s catheter connected to transfer set. (F) Final setup of dialysate bags connected to patient’s transfer set. (G) Drain bags 24 hours post-initiation of manifold exchange. IV = intravenous.
Connecting the Manifold Set to the Patient and Infusing the Dialysate Solution
Steps for connecting the manifold set to the patient are described in Table 1. After connecting the manifold set to the patient, the peritoneum must be drained prior to the infusion of the dialysate. The initial effluent should be assessed prior to connecting the patient to the manifold set. Subsequent to the initial drainage, the connector should be wrapped with a betadine-soaked sterile gauze and secured with tape (Figure 3D). After the infusion of the first dialysate bag, all clamps must be closed and a report should be given to floor nursing. Infusion of dialysate in a patient admitted to the inpatient service is shown in Figure 3E and 3F.
Maintenance of Manifold Exchange by the Floor Nurse
After infusion of the first dialysate bag, the PD nurse will train the primary floor nurse caring for the patient on maintenance of the manifold required for the next 24-hour period as described in Table 1. The floor nurse will be instructed to assess the effluent from each drain and to inform the PD staff immediately if any changes have occurred (Figure 3G). To infuse the next dialysate bag, the floor nurse will be instructed to follow the numbered sequence on the labeled bags. Prior to leaving the patient’s bedside, the checklist in Table 2 should be completed.
Results
We have utilized an inexpensive form of PD manifold exchange in the inpatient setting. Manifold PD can be prepared and performed with the assistance of primary floor nursing with minimal logistical barriers, thereby relieving the burden on PD staff. This system provides 24 hours of continuous PD in patients unable to perform PD on their own in the inpatient service. Assembly and initiation of the manifold exchange is described in greater detail in the methods section.
For the past two decades, the manifold system has been exclusively used to perform PD in all adult ESRD patients admitted to the inpatient service at Mount Sinai Medical Center, a 1,171-bed, tertiary care medical teaching facility with annual patient discharges of 59,495 in New York City. In the past 10 years, manifold has been used an average (± standard error of the mean) of 6 ± 0.5 patient admissions per month with an average (± standard error of the mean) patient length stay of 5.7 ± 0.5 days. During this period, we have observed only 1 episode of inpatient peritonitis. This episode of peritonitis may have been related to an unscheduled discontinuation of the system by one of the floor nurses, thereby contributing to the contamination. These results, combined with the simplified logistical setup, suggest that the manifold system is a very reasonable form of delivering PD for the acutely ill patient in the inpatient service.
Discussion
A large body of evidence exists in the use of APD and CAPD in the management of patients with ESRD in the chronic ambulatory setting. However, limited evidence exists in the use of APD or CAPD in the inpatient setting. Despite the limited evidence in the inpatient setting, the use of either of these modalities is currently accepted worldwide. In this short communication, we provide a technical description of delivering PD in the patients admitted to the inpatient service with minimal burden on the ancillary staff. The use of manifold exchange for more than 2 decades in our institution with a nearly non-existent incidence rate of peritonitis suggests the potential role for its use in patients unable to self-care in the inpatient service. However, we do acknowledge some potential drawbacks with the use of manifold as the primary delivery option for PD in the inpatient service. First, prior to infusion, the dialysate bags may get cooler with time, since they are not continuously on a warmer. If a patient reports discomfort with infusion due to lower temperature of the dialysate, this may warrant switching the patient to APD where dialysate bags are continuously warmed on the cycler. Second, another instance that may warrant the use of APD over manifold includes patients able to self-care and troubleshoot any malfunction with the cycler or patients who have family members trained in APD readily available to assist in troubleshooting. However, we do recognize that at some institutions, management of PD by the patients or their family members may not be permitted. Third, since all dialysate bags are hung on the IV pole (used and unused) to accommodate patient mobility, there is a potential for reinfusion or double infusion of unused dialysate or effluent. We have minimized this concern by training the floor nurse to clearly mark the effluent bags when they are rehung on the IV pole after being drained. However, if there is a persistent risk of reinfusion or double infusion, the use of APD may be warranted over manifold. Fourth, APD may be preferred over manifold in instances where greater control over variable infusion and drain volumes is required. We recognize the need for further studies to compare the incident peritonitis rates, dialysis adequacy, and cost effectiveness between manifold, CAPD, and APD to truly determine the role of manifold in the inpatient service. Nonetheless, we believe this simplified assembly and initiation of manifold exchange by the PD team with subsequent management by the inpatient team is responsible for the extremely low incidence rate of hospital-acquired peritonitis. Furthermore, the training required to manage the manifold by the floor nursing staff is less complex than that of APD (especially in regards to troubleshooting the alarms in APD). The resources required to initiate manifold exchange compared to APD or CAPD in acutely ill patients may make it attractive to institutions worldwide in need of minimizing healthcare costs without sacrificing optimal patient care. Finally, the multidisciplinary approach to managing patients on PD by the inpatient team and PD staff involves all members of the healthcare team, thereby providing the best care for the patient.
Disclosures
The authors have no financial conflicts of interest to declare.
Acknowledgments
We acknowledge all the Mount Sinai Medical Center Peritoneal Dialysis Unit nursing staff for their support and help in the preparation of this manuscript.
References
- 1. Cnossen TT, Usvyat L, Kotanko P, van der Sande FM, Kooman JP, Carter M, et al. Comparison of outcomes on continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis: results from a USA database. Perit Dial Int 2011; 31:679–84 [DOI] [PubMed] [Google Scholar]
- 2. Rabindranath KS, Adams J, Ali TZ, Daly C, Vale L, MacLeod AM. Automated vs continuous ambulatory peritoneal dialysis: a systematic review of randomized controlled trials. Nephrol Dial Transplant 2007; 22(10):2991–8 [DOI] [PubMed] [Google Scholar]
- 3. Rabindranath KS, Adams J, Ali TZ, MacLeod AM, Vale L, Cody J, et al. Continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis for end-stage renal disease. Cochrane Database Syst Rev 2007. April 18; (2):CD006515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guo A, Mujais S. Patient and technique survival on peritoneal dialysis in the United States: evaluation in large incident cohorts. Kidney Int Suppl 2003:S3–12 [DOI] [PubMed] [Google Scholar]
- 5. Mujais S, Story K. Peritoneal dialysis in the US: evaluation of outcomes in contemporary cohorts. Kidney Int Suppl 2006:S21–6 [DOI] [PubMed] [Google Scholar]