Abstract
Background
Cardiac rehabilitation is an important component of recovery from coronary events but uptake and adherence to such programmes are below the recommended levels. This aim is to update a previous non-Cochrane systematic review which examined interventions that may potentially improve cardiac patient uptake and adherence in rehabilitation or its components and concluded that there is insufficient evidence to make specific recommendations.
Objectives
To determine the effects of interventions to increase patient uptake of, and adherence to, cardiac rehabilitation.
Search methods
A previous systematic review identified studies published prior to June 2001. We searched the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (Issue 4 2007), MEDLINE (2001 to January 2008), EMBASE (2001 to January 2008), CINAHL (2001 to January 2008), PsycINFO (2001 to January 2008), Web of Science: ISI Proceedings (2001 to April 2008), and NHS Centre for Reviews and Dissemination (CRD) databases (Health Technology Assessment (HTA) and Database of Abstracts of Reviews of Effects (DARE)) from 2001 to January 2008. Reference lists of identified systematic reviews and randomised control trials (RCTs) were also checked for additional studies.
Selection criteria
Adults with myocardial infarction, coronary artery bypass graft, percutaneous transluminal coronary angioplasty, heart failure, angina, or coronary heart disease eligible for cardiac rehabilitation and randomised or quasi-randomised trials of interventions to increase uptake or adherence to cardiac rehabilitation or any of its component parts. Only studies reporting a measure of adherence were included.
Data collection and analysis
Titles and abstracts of all identified references were screened for eligibility by two reviewers independently and full papers of potentially relevant trials were obtained and checked. Included studies were assessed for risk of bias by two reviewers.
Main results
Ten studies were identified, three of interventions to improve uptake of cardiac rehabilitation and seven of interventions to increase adherence. Meta-analysis was not possible due to multiple sources of heterogeneity. All three interventions targeting uptake of cardiac rehabilitation were effective. Two of seven studies intended to increase adherence had a significant effect. Only one study reported the non-significant effects of the intervention on cardiovascular risk factors and no studies reported data on mortality, morbidities, costs or health care resource utilisation.
Authors’ conclusions
There is some evidence to suggest that interventions to increase the uptake of cardiac rehabilitation can be effective. Few practice recommendations for increasing adherence to cardiac rehabilitation can be made at this time. Interventions targeting patient identified barriers may increase the likelihood of success. Further high quality research is needed.
Medical Subject Headings (MeSH): Angina Pectoris [rehabilitation]; Angioplasty, Balloon, Coronary [rehabilitation]; Coronary Artery Bypass [rehabilitation]; Coronary Disease [* rehabilitation]; Exercise; Heart Failure [rehabilitation]; Myocardial Infarction [rehabilitation]; Patient Acceptance of Health Care [* statistics & numerical data]; Patient Compliance [statistics & numerical data]; Randomized Controlled Trials as Topic
MeSH check words: Adult, Humans, Middle Aged
BACKGROUND
Coronary heart disease (CHD) is a major cause of mortality and morbidity and is a growing problem. Worldwide it is estimated that some 50 million people have existing CHD (Neal 2004) with a one in four (25%) risk of suffering a further serious event in the next 10 years (Law 2002; WHO 1997). Although in recent decades CHD mortality rates have fallen in many developed countries, rates of morbidity are increasing as a result of improved diagnosis and more successful treatment of acute illness which, for example, has led to an increasing number of survivors of myocardial infarction (Law 2002; Neal 2004).
Cardiac rehabilitation is offered to individuals after cardiac events to aid recovery and prevent further cardiac illness. Cardiac rehabilitation has been shown to improve physical health, and decrease subsequent morbidity and mortality (Jolliffe 2001; Taylor 2004). Cardiac rehabilitation programmes typically achieve this through exercise, education, behaviour change, psychological counselling/support, and strategies that are aimed at targeting traditional risk factors for cardiovascular disease. Cardiac rehabilitation is an essential part of the contemporary care of heart disease and is considered a priority in countries with high prevalence of CHD and heart failure (HF) (Balady 2007; Graham 2007; NICE 2007; Stone 2005).
Although the beneficial effects of cardiac rehabilitation have been shown, participation and adherence remain sub-optimal. Surveys across a number of countries have shown 14-43% of potential cardiac patients of participate in rehabilitation programmes (Bethell 2001; Blackburn 2000; Bunker 1999). Some studies report that less than 50% of people who participate in cardiac rehabilitation programmes maintain an exercise regimen for as long as six months after completion (Daly 2002; Moore 2003). Factors reported as predicting adherence include health belief variables (Al-Ali 2004;Fleury 1991; Moore 2003), age (Al-Ali 2004; Daly 2002; Moore 2003), annual income (Al-Ali 2004), level of education (Al-Ali 2004; Daly 2002), cardiac functional status (Moore 2003), mood state (Moore 2003; Ziegelstein 2000) and social support (Moore 2003).
There is a published systematic review in the Journal of Advanced Nursing, in 2005, on improving uptake and adherence in cardiac rehabilitation (Beswick 2005). It was concluded that there were few studies of sufficient quality to make specific recommendations of methods to improve either uptake or participation in cardiac rehabilitation or it component parts. This review aims to update this work, using Cochrane methodology.
OBJECTIVES
To determine the effects, both harms and benefits, of interventions to increase patient uptake of, and adherence to, cardiac rehabilitation.
METHODS
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) either at individual or cluster level or either parallel group, cross-over or quasi-randomised design. Systematic reviews and meta-analyses were identified as a source of additional studies.
Types of participants
Adults with myocardial infarction (MI), coronary artery bypass graft (CABG), percutaneous transluminal coronary angioplasty (PTCA), heart failure (HF), angina, or coronary heart disease (CHD) who are eligible for cardiac rehabilitation, or any of its constituent components. Where the aim of a study is to increase adherence, participants are those who have already registered to take part in a cardiac rehabilitation programme at the start of the study.
Studies of participants with heart transplants and those implanted with either cardiac-resynchronisation therapy (CRT) or implantable defibrillators (ICD) were excluded.
Types of interventions
Any intervention with the specific aim of increasing patient uptake of, or adherence to, cardiac rehabilitation or any of its component parts. Interventions could be targeted at individuals; groups; partners, carers or other family members; or health professionals. Studies evaluating the effects of interventions to improve uptake or adherence to pharmacological treatments alone (i.e. not in conjunction with any other cardiac rehabilitation activities) were excluded. Studies comparing two or more interventions to increase uptake or adherence were only included if the study included a usual care control arm. For studies of uptake, the study population comprised patients who were eligible for cardiac rehabilitation, whereas for adherence studies participants had already agreed to participate in cardiac rehabilitation.
Types of outcome measures
Primary outcomes
Measures of the uptake of, or adherence to, cardiac rehabilitation and its exercise, education and lifestyle components. Adherence was defined as the extent to which the participant’s behavior concurred with the advice given by health professionals (for example, to attend cardiac rehabilitation meetings or to undertake independent exercise). Adherence could be expressed as a dichotomous outcome (i.e. the participant did or did not concord with the advice given) or as a rate (e.g. percentage of weeks during the follow up period in which the participant did the recommended amount of exercise).
Measures such as frequency of exercise, amount of exercise taken, and measures of exercise capacity (strength, peak oxygen uptake) were not considered to be suitable measures of adherence as they do not given an indication of the extent to which participants concurred with the advice given.
Secondary outcomes
Mortality, morbidity, modifiable coronary risk factors (smoking behaviour, blood lipid levels, blood pressure), health-related quality of life, health service utilisation, costs, and any other beneficial or adverse events relevant to the review.
Only studies that reported at least one primary outcome were included.
Search methods for identification of studies
Electronic searches
Randomised and quasi-randomised controlled trials were identified from a previously published non-Cochrane systematic review (Beswick 2005). This list of studies were updated by searching a number of clinical databases - the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (2007 Issue 4), MEDLINE (2001 to January 2008), EMBASE (2001 to January 2008), CINAHL (2001 to January 2008), and PsycINFO (2001 to January 2008). Conference Proceedings were searched on Web of Science: ISI Proceedings (2001 to April 2008). Additional studies were located on NHS Centre for Reviews and Dissemination (CRD) databases (Health Technology Assessment (HTA) and Database of Abstracts of Reviews of Effects (DARE)), which were both searched from 2001 to January 2008.
Searches were limited to RCTs (including quasi-randomised), systematic reviews, and meta-analysis and a filter was applied to limit by humans. No language or other limitations were imposed. Consideration was given to variations in terms used and spellings of terms in different countries so that studies were not missed by the search strategy. Reference lists of all eligible trials and systematic reviews were searched for additional studies. Search strategies were designed with reference to those of the published non-Cochrane systematic review (Beswick 2005) and in accordance with Cochrane Heart Group methods and guidance.
A generic search strategy was carried out as this review forms part of an umbrella review that includes four other Cochrane systematic reviews addressing cardiac rehabilitation (Jolliffe 2001; Rees 2004a; Rees 2004b; Taylor 2010).
Detailed search strategies were developed for each electronic database searched, based on the strategy designed for CENTRAL but revised appropriately. See Appendix 1 for the complete list of search strategies.
A full search of CENTRAL was carried out. All other searches were run from 2001 as this is the earliest date of searches for the previous Cochrane reviews on cardiac rehabilitation (Jolliffe 2001;Rees 2004a; Rees 2004b; Taylor 2010) covered by this umbrella search. This date overlaps the dates of the searches of the previous non-Cochrane review (Beswick 2005).
Data collection and analysis
Selection of studies
Two reviewers (PD and RT) independently screened the references identified by the search strategy by title and abstract. In order to be selected, abstracts had to clearly identify the study design, an appropriate population and relevant components of the intervention as described above. Clearly irrelevant references were excluded. The full-text reports of all remaining trials were obtained and assessed independently for eligibility, based on the defined inclusion criteria, by two reviewers (PD, FT). Studies included in the non-Cochrane review (Beswick 2005) were assessed for inclusion by two reviewers (PD, RT).
Any disagreements were resolved by discussion or, where agreement could not be reached, by consultation with an independent third person (SE, Rod Taylor).
Data extraction and management
A data extraction form was re-designed, based on that used in the non-Cochrane review (Beswick 2005), with the addition of items relating to risk of bias recommended by the updated Cochrane Handbook 2008 (Higgins 2008). Due to time constraints, data extraction was undertaken by a single reviewer (FT) and checked by a second reviewer (PD). Excluded studies and reasons for exclusion are detailed in a Characteristics of excluded studies table.
Assessment of risk of bias in included studies
Factors which were considered included the quality of the random sequence generation and allocation concealment, description of drop-outs and withdrawals (including analysis by intention-to-treat), blinding (participants, personnel and outcome assessment) and selective outcome reporting. The risk of bias in eligible trials was assessed by a single reviewer (FT) and verified by a second (PD).
Data synthesis
Based on the previous non-Cochrane review (Beswick 2005), it was anticipated that a quantitative synthesis would not be possible. The multiple sources of heterogeneity observed across studies (in terms of participants, interventions, and outcomes), together with the small number of studies identified, meant that undertaking a formal meta-analysis was not considered appropriate. Heterogeneity amongst included studies was explored qualitatively (by comparing the characteristics of included studies). Studies were grouped according to whether the interventions were intended to increase uptake of, or adherence to, cardiac rehabilitation (or any of it components).
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
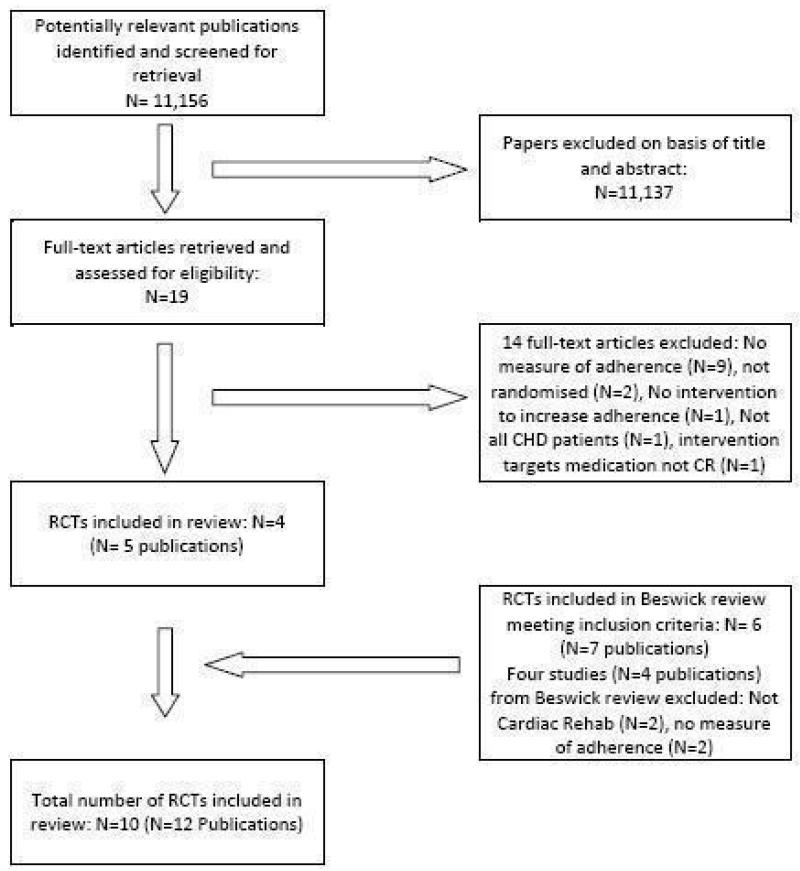
The Beswick systematic review (Beswick 2005) identified ten randomised or quasi-randomised studies, six of which met the inclusion criteria for this Cochrane review (Ashe 1993; Daltroy 1985;Hillebrand 1995; Jolly 1999; Oldridge 1983; Wyer 2001). The search (designed to identify studies for this and four other reviews of cardiac rehabilitation) identified a total 11,156 titles. Of these, 19 full papers were obtained and checked against the inclusion criteria described above. Four studies were identified as suitable for inclusion in the review (Duncan 2002; Izawa 2005; Moore 2006; Sniehotta 2006). The study selection process is illustrated in the flow diagram in Figure 1
Figure 1. Flow diagram of the study selection process.
Included studies
Three RCTs evaluated interventions to increase the uptake of cardiac rehabilitation (Hillebrand 1995; Jolly 1999; Wyer 2001) with a total of 458 participants. All three were identified by the previous non-Cochrane review (Beswick 2005). One study was cluster randomised by general practice (Jolly 1999). Two studies were conducted in the UK (Jolly 1999; Wyer 2001) and one in Germany (Hillebrand 1995). Participants were all MI patients in two studies (Hillebrand 1995; Wyer 2001) and MI or angina patients in the third study (Jolly 1999). The majority of participants in all three studies were male (71 - 89%). Mean age of participants ranged from 52 to 64 years. Two studies evaluated interventions to increase uptake of outpatient cardiac rehabilitation (Jolly 1999;Wyer 2001) and one to increase uptake of a cardiac club following inpatient cardiac rehabilitation (Hillebrand 1995). Wyer 2001 evaluated the effects of motivational letters based on the theory of planned behaviour (Ajzen 1986). In the study by Hillebrand 1995 participants in the intervention group received an in-hospital visit from a social worker and a telephone call at four weeks after discharge (the authors describe the content of these contacts as “motivational”). Jolly 1999 evaluated a multifaceted intervention involving liaison nurses who coordinated the transfer of care between hospital and general practice, together with patient held record cards to prompt and guide follow up. Uptake was variously defined as attendance at least one cardiac rehabilitation session (Jolly 1999), at the first week of cardiac rehabilitation (Wyer 2001), or attendance at cardiac rehabilitation at 12 months (Hillebrand 1995). Jolly 1999 additionally reported serum cholesterol, blood pressure, smoking status and quality of life.
Seven studies (five RCT and two quasi-randomised) evaluated a total of eight interventions to increase adherence to cardiac rehabilitation or its component parts, with a total of 903 participants. Three studies were identified by the previous review (Ashe 1993;Daltroy 1985; Oldridge 1983) and four by the updated search (Duncan 2002; Izawa 2005; Moore 2006; Sniehotta 2006). The unit of allocation for all studies was the individual patient. Length of follow up ranged from two - 12 months. Four studies were conducted in the US (Ashe 1993; Daltroy 1985; Duncan 2002; Moore 2006), and one each in Japan (Izawa 2005), Canada (Oldridge 1983) and Germany (Sniehotta 2006). Participants were all MI patients in one study (Izawa 2005), and all HF in another (Duncan 2002). Five studies included a mix of CHD patients including MI, CABG, PTCA, angina and valve problems (Ashe 1993; Daltroy 1985; Moore 2006; Oldridge 1983; Sniehotta 2006). In five studies over 80% of participants were male (Daltroy 1985; Duncan 2002; Izawa 2005; Oldridge 1983; Sniehotta 2006), 62% were male in one study (Moore 2006) and gender was not reported in (Ashe 1993). The mean age of participants in studies ranged from 51 to 66 years.
In six of the seven studies the intervention was designed to increase adherence to exercise. (Ashe 1993; Daltroy 1985; Duncan 2002;Izawa 2005; Moore 2006; Sniehotta 2006). In two studies participants had agreed to attend supervised exercise sessions (Ashe 1993; Daltroy 1985), whereas in four studies (Duncan 2002; Izawa 2005; Moore 2006; Sniehotta 2006) participants were given a recommended level of exercise which they carried out unsupervised. In all of these studies participants had already taken part in a supervised cardiac rehabilitation programme incorporating exercise sessions. Adherence was variously defined across studies in terms of number of sessions attended, frequency of exercise or duration of exercise. In one study the exact method used to calculate adherence was not entirely clear (Duncan 2002).
The interventions evaluated were varied and often multifaceted. Techniques to increase adherence to exercise included goal setting (Ashe 1993; Duncan 2002; Moore 2006), action planning (Sniehotta 2006), self-monitoring of exercise (Duncan 2002;Izawa 2005; Moore 2006), daily activities (Ashe 1993), body weight (Izawa 2005) or heart rate (Izawa 2005), feedback (Duncan 2002; Izawa 2005), problem-solving and coping strategies (Ashe 1993; Daltroy 1985; Duncan 2001; Moore 2006; Sniehotta 2006), written and oral commitment (Daltroy 1985), stress management (Ashe 1993), persuasive written and telephone communication (Daltroy 1985) and small group interaction and peer modelling (Moore 2006). One study targeted the intervention at participants’ spouses in addition to the participants themselves (Daltroy 1985).
In one study (Oldridge 1983), the intervention targeted adherence to supervised cardiac rehabilitation sessions. The intervention involved self-monitoring of daily activities, body weight and cigarettes smoked and a written commitment to participate.
In addition to adherence, one study also evaluated participants’ quality of life (Duncan 2002).
Excluded studies
A list of excluded studies, together with reasons for exclusion, can be found in the ‘Characteristics of excluded studies table (Characteristics of excluded studies). Four trials that were included in the Beswick review were excluded from this review. All were of interventions to increase adherence. Two of these trials evaluated interventions targeting adherence to nutritional advice, which was not considered to be cardiac rehabilitation (Aish 1996; Duncan 2001) and two did not include a suitable measure of adherence (Hopper 1995; Mahler 1999). Nine studies identified by the updated search did not contain a measure of adherence (Brodie 2005; Carroll 2007; Hughes 2002; Hughes 2007; Kummel 2007;Luszczynska 2006; Sniehotta 2005;Southard 2003; Vestfold 2003; see Primary outcomes for further information on how adherence was defined). Other reasons for exclusion were: not randomised (Moore 2002; Palomki 2002), no intervention to increase adherence (Froelicher 2003), not all participants had CHD (Rejeski 2002) and intervention targeting adherence to medication and medical appointments rather than cardiac rehabilitation (Stromberg 2006).
Ongoing studies
One RCT was identified of an intervention to promote healthy behaviour change in women with CHD (Beckie 2006). The intervention is based on the transtheoretical model and motivational interviewing and involves psychoeducational and exercise sessions delivered over a 12 week period.
Risk of bias in included studies
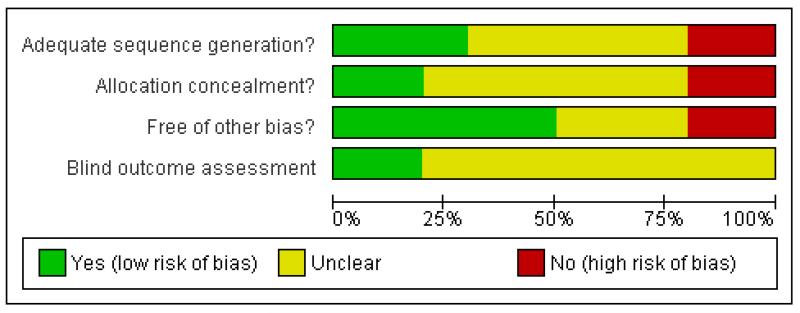
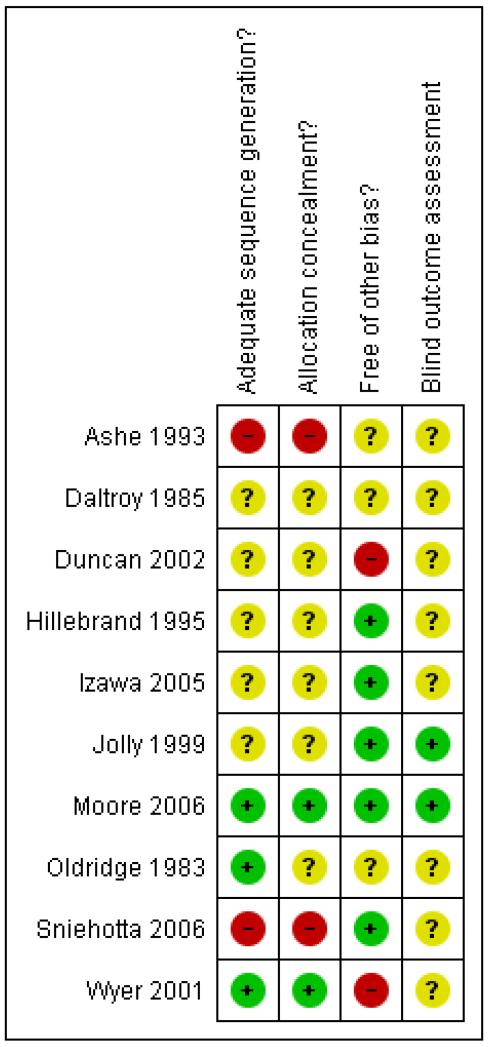
Many of the included studies did not report the design and conduct in sufficient detail to make a full assessment of risk of bias (see Figure 2; Figure 3). All studies were described as randomised but five did not report the method of randomisation (Daltroy 1985;Duncan 2002; Hillebrand 1995; Izawa 2005; Jolly 1999). Two studies employed a weak method of randomisation (Ashe 1993;Sniehotta 2006) and the method of randomisation was satisfactory in three studies (Moore 2006; Oldridge 1983; Wyer 2001). Concealment of allocation prior to entry to the study was either unclear or not done in all but two studies (Moore 2006; Wyer 2001). Due to the nature of the intervention, blinding of participants and personnel to treatment allocation was not deemed possible, but blinding of outcome assessors was possible. Blinding could not be determined in seven studies (Ashe 1993; Daltroy 1985; Duncan 2002; Hillebrand 1995; Izawa 2005; Oldridge 1983; Sniehotta 2006), was carried out in two studies (Jolly 1999; Moore 2006) and was not satisfactory in one study (Wyer 2001). Only one study satisfied all of the quality criteria considered (Moore 2006).
Figure 2. Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Figure 3. Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Due to time constraints, we did not contact authors for clarification of data, thus our review may be at risk of outcome reporting bias. If protocols had been published for the studies included in our review these would have been identified by our search. Only one protocol was identified and this study is currently ongoing (Beckie 2006). Outcome reporting bias most commonly occurs when outcomes are not reported due to no significant effect being found. The likely direction of effect of this bias on our review, therefore, is that there are unpublished studies or data indicating a lack of effect of interventions to increase uptake/adherence. Given that the interventions evaluated were varied (no two studies evaluated interventions based on the same techniques) and that most of the adherence studies were negative, we feel that publication bias is unlikely to have changed the conclusions of our review.
Effects of interventions
Interventions to increase uptake of cardiac rehabilitation
Uptake
Results for the individual studies can be found in Table 1. Three studies looked at the effectiveness of interventions to increase uptake of cardiac rehabilitation (Hillebrand 1995; Jolly 1999; Wyer 2001). In all three studies attendance was significantly higher in the group receiving the intervention. Attendance in the intervention groups ranged from 42 to 86%. Percentage difference in attendance between intervention and comparison groups ranged from 18 to 30%.
Other outcomes
Only one study reported data for any of the secondary outcomes considered by this review (Jolly 1999). Serum cholesterol, blood pressure and smoking status did not differ between groups. None of these three studies identified reported mortality, morbidity, health-related quality of life, health service utilisation or costs of the interventions.
Interventions to increase adherence to cardiac rehabilitation
Adherence
Results for the individual studies can be found in Table 2. Seven studies looked at the effectiveness of interventions to increase adherence to cardiac rehabilitation or any of its components (Ashe 1993; Daltroy 1985; Duncan 2002; Izawa 2005; Moore 2006;Oldridge 1983; Sniehotta 2006).
One study (Oldridge 1983) targeted adherence to supervised cardiac rehabilitation sessions. There was no significant difference in attendance rates between participants in the intervention and comparison groups.
Two studies evaluated interventions to increase adherence to supervised exercise sessions (Ashe 1993; Daltroy 1985). Neither intervention resulted in a significant increase in attendance in the intervention group compared to the control. In the study by Ashe (Ashe 1993), attendance at exercise sessions was very high in both the intervention and comparison groups (90% versus 89%).
Four studies evaluated a total of five interventions to increase adherence to unsupervised exercise (Duncan 2002; Izawa 2005;Moore 2006; Sniehotta 2006). There was no significant difference in adherence between the intervention and control groups in two of these studies (Izawa 2005; Moore 2006). Duncan 2002 evaluated a multifaceted intervention incorporating goal setting, feedback and problem solving in heart failure patients. No significant difference was observed at 12 weeks in adherence to the recommended duration of exercise, but adherence to the recommended frequency of exercise was significantly higher in the intervention group (n = 16, 104% vs 64%, p < 0.01). No information was reported about the method of randomisation, concealment of allocation or blind outcome assessment, therefore, the risk of bias in the study could not be determined. The findings of Duncan can be contrasted with those of Moore et al (Moore 2006), who evaluated an intervention comprising the same techniques plus social interaction and peer modelling but found no significant effect on adherence (measured at 12 months). Sniehotta 2006 evaluated two interventions to increase adherence. Participants in the action planning group were asked to develop three action plans each about when, where and how they intended to exercise and implement extra everyday activities after discharge. Participants in the combined group were asked to develop three coping plans to overcome anticipated barriers (identified by participants themselves), in addition to the action plans.
Whilst there was no difference in adherence between the ‘Action planning’ and control participants (n = 149, 44% versus 42%, not statistically significant), those in the ‘Combined planning’ group were significantly more adherent than both the ‘Action planning’ (n = 130, 71% versus 44%, p < 0.01) and control groups (n = 143, 71% versus 42%, p < 0.001).
Other outcomes
Only one study reported data for any of the secondary outcomes considered by this review - Duncan 2002 reported quality of life. Scores were lower in the intervention group (a lower score indicated higher quality of life) but the difference was not statistically significant. The sample size was small (n = 16) and the study may, therefore, not have been powered to detect a significant effect. None of the studies identified reported mortality, morbidity, modifiable coronary risk factors (smoking behaviour, blood lipid levels, blood pressure), health service utilisation or costs of the interventions.
DISCUSSION
Cardiac rehabilitation is an important component of recovery from coronary events and reduces the risk of future cardiac events. Despite this, both uptake of cardiac rehabilitation and adherence to such programmes are below the recommended levels, especially in certain groups. The aim of this systematic review was to determine the effects of interventions to increase patient uptake of, and adherence to, cardiac rehabilitation.
Summary of main results
Only three RCTs of interventions to improve uptake of cardiac rehabilitation were identified, all of which found significant effects. (Hillebrand 1995; Jolly 1999; Wyer 2001). The interventions evaluated included motivational letters (Wyer 2001), motivational telephone contact and home visits (Hillebrand 1995) and co-ordination of care by a trained nurse, together with patient self-monitoring of contact with health professionals (Jolly 1999). The multifaceted nature of the latter trial meant that it was not possible to identify which were the active components of the intervention that brought about the increase in uptake.
Of the seven studies of interventions to improve adherence one was to a comprehensive cardiac rehabilitation programme (Oldridge 1983) and six to exercise only, either supervised (Ashe 1993;Daltroy 1985) or unsupervised (Duncan 2002; Izawa 2005; Moore 2006; Sniehotta 2006). A wide variety of techniques, and combinations of techniques, were evaluated including goal setting, action planning, self-monitoring (of exercise, daily activities, body weight, heart rate, smoking, and contact with health professionals), feedback, problem-solving and coping strategies, written and oral commitment, stress management, persuasive written and telephone communication, and small group interaction and peer modelling. The majority of studies found no significant effect of the interventions on adherence. Two studies found significant effects (Duncan 2002; Sniehotta 2006) of unsupervised exercise in patients who had previously completed a programme of supervised exercise. It should be noted that the follow up period of these two studies - 10 weeks (Sniehotta 2006) and 12 weeks (Duncan 2002) - were considerably shorter than for the two studies that found no significant effects on unsupervised exercise (Izawa 2005, six months; and Moore 2006 12 months).
Duncan (Duncan 2002), whose intervention comprised of goal setting, self-monitoring of exercise behaviour, feedback and problem solving, found a significant effect on adherence to the recommended frequency of exercise, but not to the recommended duration of exercise. However, the study sample was very small and the risk of bias was difficult to assess to due a lack of information in the study report. Adherence to exercise was determined by selfreport (patients kept diaries) and the exact method of calculating adherence was not clear.
Sniehotta (Sniehotta 2006) found that developing coping plans to overcome anticipated barriers (identified by participants themselves) together with action plans (specifying where, when and how to exercise) was more effective than action planning alone or usual care. Action planning alone was not more effective than usual care, suggesting that coping plans were the most important component in the combined intervention. However, randomisation was achieved by alternate allocation, which is a weak method. Adherence to exercise was self-reported and there was no information within the study report about whether those assessing outcomes were blind to the participants’ treatment allocations. These factors may have introduced bias into the results of the study.
Overall completeness and applicability of evidence
The studies of interventions to increase uptake of cardiac rehabilitation were mainly carried out in MI patients: 100% in two studies (Hillebrand 1995; Wyer 2001) and 71% in Jolly 1999. Hence there is little evidence regarding uptake in other cardiac populations that would also be eligible for cardiac rehabilitation. Five of the seven studies of adherence to cardiac rehabilitation (Ashe 1993; Daltroy 1985; Moore 2006; Oldridge 1983; Sniehotta 2006) recruited mixed CHD populations including MI, CABG, PTCA, angina and valve problems. Only one study identified by the review included HF patients and the sample size was small (13 patients; Duncan 2002). Exercise training is an emerging therapy for heart failure patients and has been shown to be beneficial in people with mild to moderate HF (Rees 2004a), yet such patients may avoid exercise through fear of placing excessive strain on the heart. The identification of effective techniques to increase adherence to exercise recommendations in HF patients may therefore be particularly valuable.
The majority of participants in the studies included in this review were male. One study had a recruitment policy designed to increase the numbers of women recruited (every eligible female was invited to participate and every other eligible male). Thirty eight percent of participants in this study were female (Moore 2006). Although there is no evidence to suggest that women benefit less from participation in cardiac rehabilitation, referral rates and attendance tend to be lower (Jackson 2005). Barriers to participation may differ between women and men and different interventions may therefore be required to increase adherence. One on-going study was identified (Beckie 2006) of an intervention to target women with CHD. Other groups frequently under-represented in cardiac rehabilitation include older participants, ethnic minorities, and those with co-morbidities (Beswick 2004). Ethnicity was rarely reported within the included studies, and advanced age and co morbidities were often reasons for exclusion from trials.
In the majority of the included studies, the intervention was targeted at recruited participants whilst one study also targeted the intervention at participants’ spouses (Daltroy 1985). Despite the fact that physician endorsement has been found to be a strong predictor of uptake (Jackson 2005), only one study was identified that targeted health professionals as well as patients (Jolly 1999). A range of different techniques to increase uptake or adherence have been evaluated in the studies identified. Interventions were usually multifaceted and many different combinations of techniques have been studied. Very few studies evaluated a single intervention strategy. The literature review by Beswick (Beswick 2004) identified a broad range of suggested interventions for increasing uptake and adherence in cardiac rehabilitation, most of which have not been formally evaluated. Interventions rarely targeted barriers to uptake and adherence frequently cited by patients, such as perceptions about their illness and recovery, transport difficulties, family commitments and inconvenient timing (Beswick 2004). Strict definitions of uptake and adherence were used for the purpose of this review and only studies that reported these primary outcomes were included. Very few of the included studies reported any of the secondary outcomes of the review. Only one study reported the effects of the intervention on cardiovascular risk factors (serum cholesterol, blood pressure, smoking status; Jolly 1999). No studies reported mortality or morbidity. The assumption is that improving uptake or adherence to cardiac rehabilitation will lead to an improvement in these outcomes but this relationship was rarely examined by studies. No studies provided information on the costs of the intervention or other resource implications. Only one study reported health-related quality of life (Duncan 2002) and this study had a very small sample size.
Quality of the evidence
Many of the included studies provided insufficient information to assess their risk of bias. Several studies used weak methods of randomisation that would not have adequately concealed treatment allocation prior to enrolment. Very few studies provided information about blinding of outcome assessors. Three of the four studies that evaluated interventions to increase adherence to unsupervised exercise relied upon self-reported exercise levels to determine the effects of the intervention and these measures may have been affected by social desirability or poor recall (Duncan 2002; Izawa 2005; Sniehotta 2006). Use of pedometers and heart monitors to validate self-reported exercise behaviour in such trials would have been desirable.
Only a small number of RCTs of interventions to increase uptake (three trials, 458 participants Hillebrand 1995; Jolly 1999; Wyer 2001) or adherence (seven trials, 908 participants, Ashe 1993; Daltroy 1985; Duncan 2002; Izawa 2005; Moore 2006; Oldridge 1983; Sniehotta 2006) were identified. The interventions evaluated were varied and often multifaceted. The small body of evidence and the multifaceted nature of many of the interventions evaluated means that the consistency of findings could not be determined.
Potential biases in the review process
This Cochrane review focused on the uptake or adherence of cardiac rehabilitation. Other outcome measures, such as frequency of exercise, amount of exercise taken, measures of exercise capacity (strength, peak oxygen uptake), cardiac functional status and potential mediating variables of adherence (e.g. self efficacy, health beliefs) were not considered. It may be the case that some of the interventions evaluated were effective in targeting these outcomes even if the effects on adherence were not significant.
Due to time constraints, authors of studies were not contacted for further information. The primary reason for exclusion of full papers assessed was the lack of a suitable measure of adherence. It may be that adherence rates (or sufficient data to calculate adherence) could have been obtained from study authors had they been contacted, resulting in a greater number of trials of interventions to increase uptake and adherence being included.
AUTHORS’ CONCLUSIONS
Implications for practice
Few practice recommendations can be made at this time, particularly with respect to groups that have been traditionally under-represented in cardiac rehabilitation. A small body of evidence suggests that interventions involving motivational communications delivered through letters, telephone calls and home visits may be effective in increasing uptake of cardiac rehabilitation, as may the use of liaison nurses to support coordination of care. Coping strategies targeting barriers to adherence may be helpful in improving adherence. Barriers to uptake and adherence in cardiac rehabilitation are many and varied and reasons for non-participation may vary between individuals. Individually tailored approaches may increase the likelihood of success.
Implications for research
As there is a good rationale for increasing uptake and adherence to cardiac rehabilitation, further high quality research is needed, particularly in under-represented groups such as women, ethnic minorities, older patients, heart failure patients, and those with co-morbidities. Interventions should be developed with barriers to uptake and adherence in mind. The evaluation of single strategies will make it easier to identify the ‘active ingredients’ of interventions. The effects of interventions on clinical outcomes such as cardiovascular risk factors (smoking behaviour, blood lipid levels, blood pressure), mortality, morbidity and health-related quality of life should be assessed, along with the likely costs and resource implications.
PLAIN LANGUAGE SUMMARY.
Promoting patient uptake and adherence in cardiac rehabilitation
People with coronary heart disease are at an increased risk of experiencing adverse cardiac events such as heart attack. Cardiac rehabilitation programmes aid recovery from a cardiac event or surgery and reduce the likelihood of further illness. Cardiac rehabilitation programmes vary, but usually include one or more of the following: exercise, education, and psychological counselling/support. Despite the benefits of cardiac rehabilitation, not everyone agrees to participate and, of those who do, many people do not adhere to the programme recommended. This Cochrane review evaluated trials of ways to increase the uptake of cardiac rehabilitation and to improve adherence amongst those who choose to participate.
We searched a wide variety of databases and found ten randomised control trials that were suitable for inclusion (three trials of interventions to improve uptake, and seven of interventions to improve adherence). The studies evaluated a variety of techniques to improve uptake or adherence and in many studies a combination of strategies was employed. The quality of studies was generally low. All three interventions targeting uptake of cardiac rehabilitation were effective. Two of seven studies intended to increase adherence to exercise as part of cardiac rehabilitation had a significant effect (one of which was of poor quality). Very few studies reported the effects of the interventions on clinical outcomes or health related quality of life and none provided information about costs or resource implications.
The differences between the strategies used in the studies we identified mean that it is difficult to make recommendations at this stage. Interventions targeting patient identified barriers may increase the likelihood of success. Further high quality research is needed, particularly in under-represented groups such as women, ethnic minorities, older patients, heart failure patients, and those with comorbidities.
ACKNOWLEDGEMENTS
We would like to thank Rod Taylor for his help and support in the design of the original review and the selection of studies for inclusion. Margaret Burke is acknowledged for her contribution to the design of the search strategy of the original review.
SOURCES OF SUPPORT
Internal sources
No sources of support supplied
External sources
NIHR programme grant, UK.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | Parallel group RCT (see notes) | |
| Participants | 41 participants recruited from a phase 2 cardiac rehabilitation programme. Mixed cardiac patients including MI, CABG, angina and patients with valve problems. Mean age 62 (range 33-77) years, gender not reported, 95% white | |
| Interventions | INTERVENTION: Motivational relapse prevention intervention received during the course of the cardiac rehabilitation programme. The cardiac rehabilitation programme consisted of three exercise sessions per week of 30-40 minutes duration for two to three months. The intervention was started after four or five exercise sessions. The intervention was based on Marlatt and Gordon’s model. Patients received individual sessions, one a week for three weeks Session 1: using pretest information, factors found to interfere with adherence were introduced. Patients discussed their perceptions on the value of exercise, listed their goals for the programme and anticipated outcomes Session 2: patients were introduced to decision-making concepts and cognitive interference factors. Discussion with regard to coping with ’slips’ and introduction to appropriate ways to reframe perspectives. Patients filled in daily activity sheets Session 3: focused on the importance of lifestyle balance. Patients were asked to refer to daily activity sheets to introduce concepts of should’s and wants. Stressors were identified that may impact on lifestyle balance and discussed, as was the importance of positive thinking and use of medication. Patients also took part in a stress management exercise and relaxation procedure COMPARISON: During the course of the exercise programme patients received a ’benign’ education intervention, which covered basic exercise concepts, guidelines for proper exercise participation, exercise tips and handouts, and the benefits of exercise |
|
| Outcomes | Total adherence to the maximum number of exercise sessions. | |
| Notes | Weak randomisation - Allocation to groups by presenting patients with a packet containing a form coded A or B | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | Allocation to groups by presenting patients with a packet containing a form coded A or B |
| Allocation concealment? | No | Allocation to groups by presenting patients with a packet containing a form coded A or B |
| Free of other bias? | Unclear | Similarity of groups at baseline unclear. Overall losses to follow up 22% |
| Blind outcome assessment? All outcomes |
Unclear | Not reported. |
| Methods | Parallel group RCT | |
| Participants | 174 patients randomised. Mixed CHD patients, 81% MI, 63% with a history of angina, 17% post-CABG. Mean age 53.8 years, 88% men, 95% white | |
| Interventions | INTERVENTION: Oral persuasive communication and education intervention to improve patient adherence to exercise regimens. Intervention developed from interviews with previous patients and their spouses to elicit the most common beliefs of benefits and drawbacks to the exercise programme. Patients in the intervention group received an oral persuasive communication on the telephone in scripted counselling format to: convince them of the benefits of regular exercise, warn them of likely drawbacks so that expectations would be realistic, acquaint them with methods used by other patients to cope with drawbacks, and elicit an oral commitment to attend at least two classes per week for the first 6 weeks. In addition, patients received a mailed written persuasive communication to reinforce these points. Spouses also received telephone counselling to encourage the patient to attend and discuss methods that other patients spouses found useful. A written communication to reinforce these points was also sent to the spouse to increase the spouse’s support. Patients also received a pamphlet with information on benefits and drawbacks of exercise. All communication was tailored to individual patients based on data collected by questionnaire at baseline COMPARISON: Comparison group patients and spouses received the same pamphlet with information on the benefits and drawbacks of exercise, as the intervention group. This was done so all patients would have the same inducement to enter the programme. It was thought unlikely that this single intervention would produce lasting behavioural change |
|
| Outcomes | Attendance at exercise sessions over three months. | |
| Notes | Subgroup analysis revealed that among the intervention group, attendance was greater among better educated patients. Spouse participation, age, gender and occupation were not associated with attendance, although the numbers in these subgroups are likely to be too small to draw firm conclusions |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not reported |
| Allocation concealment? | Unclear | Not reported |
| Free of other bias? | Unclear | CR nurse not aware of group assigned to; however, no procedure in place to stop patients telling nurse which letter received |
| Blind outcome assessment? All outcomes |
Unclear | Not reported |
| Methods | Parallel group RCT | |
| Participants | Patients with heart failure who had completed a supervised exercise programme. 16 randomised, results available for 13 (adherence) and 14 (QoL), . Mean age 66. 84% male. Duncan 2003 says 16 patients | |
| Interventions | INTERVENTION: Advice from CR staff on home exercise specific to patient’s requirements for 12 weeks. Adherence facilitation (adapted from social learning theory) consisting of goal setting and review of goal setting regarding exercise, graphic feedback and problem solving guidance delivered by a research nurse at 3 week intervals. Positive reinforcement provided if goals were not met with follow-up phone calls. Diaries collecting data on adherence were collected with mailed feed back on progress every 3 weeks COMPARISON: Advice from CR staff on home exercise specific to patients requirements for 12 weeks. Diaries collecting data on adherence was collected at 12 weeks |
|
| Outcomes | Adherence to exercise regimen at 12 weeks. Quality of life (Minnesota Living with Heart Failure questionnaire) | |
| Notes | Duncan 2003 reports that 16 patients were randomised, whereas Duncan 2002 reports 13 were randomised. Two patients died, and two patients dropped out of the control group. Adherence results reported for 11 participants therefore onebvvgg unaccounted for | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not stated |
| Allocation concealment? | Unclear | Not stated |
| Free of other bias? | No | Intervention group were older than the control group and had been diagnosed with heart failure for longer (mean of 2.3 versus 3.1 years). Selection bias: participants had permission from attending cardiologist to participate. 16 patients randomised, 4 withdrawn (two died, two dropped out), one unaccounted for. Not very clear how the outcome was calculated |
| Blind outcome assessment? All outcomes |
Unclear | Not stated |
| Methods | Parallel group RCT, Germany | |
| Participants | 94 patients randomised. Results reported for 87 (4 patients died, three refused follow-up). Post-MI patients attending inpatient CR programme. Mean age 52 (33-60) years, 89% men | |
| Interventions | INTERVENTION: Special outpatient care programme to support blue-collar workers after MI to join coronary groups. The programme consisted of four different conversations between patients and a social worker: at end of rehabilitation programme, telephone contact after four weeks, home visit after three months and telephone contact after six months COMPARISON: No outpatient care programme |
|
| Outcomes | Attendance at cardiac group after 12 months. | |
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not reported |
| Allocation concealment? | Unclear | Not reported |
| Free of other bias? | Yes | |
| Blind outcome assessment? All outcomes |
Unclear | Not reported |
| Methods | Parallel group RCT | |
| Participants | Patients with MI who had completed a cardiac rehab programme. Fifty patients randomised. Results available for 45. Mean age in intervention group 63.9 (s.d. 9.7) and in comparison group 64.5 (s.d. 10.1). 84% male. Percentage white - intervention: 88%, comparison: 67% | |
| Interventions | All patients received a programme of CR delivered by a multi disciplinary team customised for each patient. Patients participated in supervised combined aerobic and resistance exercise twice a week for an hour. At discharge all patients were advised of diet and exercise and CVD risk factors INTERVENTION: Self monitoring approach based on Banduras self efficacy theory. Patients were taught to record body weight, exercise as measured by pedometer and heart rate. Performance was addressed by written feed back |
|
| Outcomes | Exercise maintenance at six months. | |
| Notes | Exercise maintenance determined from a readiness to exercise evaluation based on the Transtheoretical model of exercise behaviour change. Self-efficacy for physical activity and mean number of steps taken per day (measured by pedometer) were significantly higher in the intervention group compared to control at 12 months post-MI | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not stated |
| Allocation concealment? | Unclear | Not stated |
| Free of other bias? | Yes | |
| Blind outcome assessment? All outcomes |
Unclear | Not stated |
| Methods | Cluster-RCT, UK | |
| Participants | 67 general practices in a specified geographical area randomised. 277 patients from randomised intervention practices and 320 from control practices. Patients admitted to hospital with MI (71%) or with angina of recent onset (<3 months) seen in hospital (29%). Patients were judged well enough to participate by medical and nursing staff on the ward or in clinic. 71% male | |
| Interventions | INTERVENTION: Specialist cardiac liaison nurses coordinated the transfer of care between hospital and general practice. The liaison nurse saw patients in hospital and encouraged them to see the practice nurse after discharge. Support was provided to practice nurses by regular contact, including a telephone call shortly before patient discharge to discuss care and book a first follow-up visit to the practice. Practice nurses were encouraged to telephone the liaison nurse to discuss problems or to seek advice on clinical or organisational issues. Each patient was given a patient-held record card which prompted and guided follow-up at standard intervals | |
| Outcomes | Attendance at least one outpatient CRsession. Serum cholesterol. Blood pressure. Smoking | |
| Notes | The difference in attendance was most marked in angina patients (42% vs 10%). Serum cholesterol, blood pressure, distance walked in 6 minutes and smoking cessation did not differ between groups. Body mass index was slightly lower in the intervention group | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not reported |
| Allocation concealment? | Unclear | Not reported |
| Free of other bias? | Yes | |
| Blind outcome assessment? All outcomes |
Yes | Follow-up of patients carried out by a nurse not responsible for delivering the intervention to the patient’s practice |
| Methods | Parallel group RCT | |
| Participants | 259 patients randomised. Results available for 250. Mixed CHD patients, MI 52%, CABG 55%, PTCA 59%. Mean age 62 yrs (range 38 - 86), 62% male. Recruited from three outpatient clinics | |
| Interventions | All participants received usual CR programme of structured exercise and individual and group classes (four) on diet modification and stress reduction. At the end participants were given an exercise prescription that included target heart rate (THR) zone and advice to exercise at least 5 times per week for 30 minutes INTERVENTION: CHANGE programme (,Change Habits by Applying New Goals and Experiences-), based on several cognitive behavioural frameworks (social problem solving model, self efficacy theory, expectancy value theory, relapse prevention theory) . CHANGE program given in three 1/2 hour sessions, once per week in the last three weeks of the CR programme. Two further sessions held at one and two months post CR programme. Sessions were provided by cardiac nurse in small group and centred on: small group social interaction, peer modelling, self assessment, goal setting and problem solving activities reinforced at later stages |
|
| Outcomes | Adherence to exercise amount: (10 hours of moderate intensity exercise a month - 150 min/week) Adherence to exercise frequency: (at least 5 times/week or 20 times/month) Both measured at 12 months. |
|
| Notes | Mean duration of an exercise session among those who exercised was longer than 30 min recommended (mean session length 52 minutes). Men were less likely to discontinue exercise than women. Participants with higher comorbidity scores or more muscle and joint pain were more likely to discontinue exercise | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computerised minimisation stratification randomisation program used managed by program director in which participants were stratified on gender and site of recruitment |
| Allocation concealment? | Yes | The randomisation sequence was concealed until intervention was assigned |
| Free of other bias? | Yes | |
| Blind outcome assessment? All outcomes |
Yes | Exercise measured using portable wristwatch heart rate monitors, backed up by diaries mailed to investigators. Data collectors were blind to study group |
| Methods | Parallel group RCT | |
| Participants | 120 patients randomised. Mixed CHD patients, MI 73%, CABG 16%, angina 12%. Mean age 50.5 years, all male | |
| Interventions | INTERVENTION: Usual comprehensive cardiac rehabilitation programme, plus self-management techniques including an agreement to participate in the programme for six months to be signed by the patient and coordinator, and self-report diaries to complete and be discussed with the coordinator at regular intervals. Diaries included six graphs for plotting self monitored submaximal heart rates each month, at 33%, 50% and 75% of the maximum power output achieved in the previous exercise test, and six 24-hour recall questionnaires of daily activities on a randomly chosen day to be completed each month. In addition, a weight loss diary to fill in each week was given to those who initially agreed to lose weight, and similar diaries to record number of cigarettes smoked each day. Follow-up at the end of the intervention period of six months COMPARISON: Usual comprehensive cardiac rehabilitation programme |
|
| Outcomes | Compliance (defined as attendance at 60% or more of the scheduled 48 supervised cardiac rehabilitation sessions) | |
| Notes | Patients stratified by smoking status, occupation, leisure habits and number of prior infarctions before randomisation. These variables were shown to be predictors of dropout based on previous experience of this group. Attendance of dropouts was similar in the intervention and control groups (21% vs 16%) and was also similar for compliers (74% vs 76%). Not all patients in the intervention group signed the agreement to participate. Compliance was significantly higher in the 48 subjects who signed (65%), than in the 15 who refused (20%) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Random number list |
| Allocation concealment? | Unclear | Not stated |
| Free of other bias? | Unclear | Unclear whether comparison groups were similar at baseline. |
| Blind outcome assessment? All outcomes |
Unclear | Not stated. |
| Methods | Parallel group RCT | |
| Participants | 246 randomised, 211 completed the study. Mixed CHD patients: MI 58%, CABG 9%, PTCA 33%. Mean age 59.3 (s.d. 10, range 31-82), 88% male | |
| Interventions | After discharge from residential CRprogramme all patients were recommended to engage in regular vigorous exercise (at least three times per week for minimum of 30 minutes per unit), and increase their everyday physical activities. Motivation was addressed in psycho educational classes INTERVENTION 1: ’Action planning group’ additionally developed three action plans each about when, where and how they intended to exercise and implement extra every day activities after discharge. Treatments were conducted by trained consultants in a one to one setting and lasted up to 30 minutes INTERVENTON 2: ’Combined planning group’ additionally developed three action plans each about when, where and how they intended to exercise and implement extra every day activities after discharge and three coping plans to overcome anticipated barriers. Treatments were conducted by trained consultants in a one to one setting and lasted up to 30 minutes |
|
| Outcomes | Adherence to exercise (self-reported exercise at least three time per week for at least 30 minutes. Individuals who adhered were classified as ’achievers’). Follow up 10 weeks | |
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | No | Each consultant assigned participants to experimental conditions according to an assignment sheet that followed the order control group, action planning group and combined planning group |
| Allocation concealment? | No | Each consultant assigned participants to experimental conditions according to an assignment sheet that followed the order control group, action planning group and combined planning group |
| Free of other bias? | Yes | |
| Blind outcome assessment? All outcomes |
Unclear | Not stated |
| Methods | Parallel group RCT, UK | |
| Participants | 87 patients randomised. All patients post-MI. Mean age 63 years. 87% male | |
| Interventions | INTERVENTION: Letters based on the theory of planned behaviour (Ajzen and Madden, 1986107) designed to increase attendance at outpatient CR were given to patients 3 days post-MI and sent 3 weeks post-MI. The first letter was designed to influence acceptance and the second was designed to influence attendance. Patients also received a nominal letter of thanks at three days and the standard letter detailing course dates as sent to control patients. After allocation to groups the CR nurse saw all patients for routine assessment and personal invitation to the programme. For patients who declined the offer of a place a brief second letter was sent wishing them well and informing them that they were still welcome to contact the team COMPARISON: Nominal letter of thanks given to patients at three days post-MI and the standard letter detailing course dates |
|
| Outcomes | Uptake (defined as attendance at the outpatient CR programme) | |
| Notes | Women were less likely to attend the programme, but neither age nor distance lived from the programme predicted attendance. Authors note that the intervention may have worked by acting as a fear message, rather than through implementation of theory of planned behaviour | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Allocation by random number assignment |
| Allocation concealment? | Yes | Patients were handed a sealed numbered envelope with a nominal letter. Half of the envelopes also contained an intervention letter. Envelope contents known to a research assistant only |
| Free of other bias? | No | CR nurse not aware of group assigned to; however, no procedure in place to stop patients telling nurse which letter received |
| Blind outcome assessment? All outcomes |
Unclear | Uptake defined as saying yes to cardiac nurse. Participants may have mentioned the letter received |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
| Aish 1996 | Adherence to dietary advice not cardiac rehabilitation. |
| Brodie 2005 | No measure of adherence |
| Carroll 2007 | No measure of adherence |
| Duncan 2001 | Adherence to dietary advice not cardiac rehabilitation. |
| Froelicher 2003 | No intervention to increase adherence. |
| Hopper 1995 | No measure of adherence |
| Hughes 2002 | No measure of adherence |
| Hughes 2007 | No measure of adherence |
| Kummel 2007 | No measure of adherence |
| Luszczynska 2006 | No measure of adherence |
| Mahler 1999 | No measure of adherence |
| Moore 2002 | Non-random allocation to study group |
| Palomki 2002 | Non-random allocation to study group |
| Rejeski 2002 | Not all participants had CHD. |
| Sniehotta 2005 | No measure of adherence |
| Southard 2003 | No measure of adherence |
| Stromberg 2006 | Study targeted adherence to medication and medical appointments not cardiac rehabilitation or any of its components |
| Vestfold 2003 | No measure of adherence |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Beckie 2006 |
| Methods | Parallel group RCT |
| Participants | Women with CHD |
| Interventions | Intervention based on Transtheoretical model and motivational interviewing to promote healthy behaviour change. Intervention involves 10 Psychoeducational sessions and 36 exercise sessions over the course of 12 weeks |
| Outcomes | ,physiological and psychosocial- outcomes |
| Starting date | Not reported |
| Contact information | Theresa M Beckie, College of nursing, University of South Florida, MDC Box 22, 12901 Bruce B. Downs Boulevard, Tampa, FL, USA. tbeckie@hsc.usf.edu |
| Notes | No specific information given about outcomes so not clear whether adherence will be measured |
DATA AND ANALYSES
This review has no analyses.
ADDITIONAL TABLES
Table 1. Studies of interventions to increase uptake of cardiac rehabilitation.
| Study | No patients | Intervention | Comparison | Significance |
|---|---|---|---|---|
| Hillebrand 1995 | 94 | 57% | 27% | p < 0.005 |
| Jolly 1999 | 67 | 42% | 24% | p < 0.001 |
| Wyer 2001 | 87 | 86% | 57% | p < 0.0025 |
Table 2. Studies of interventions to increase adherence to cardiac rehabilitation.
| Study | No of patients/clusters | Intervention | Comparison | Significance |
|---|---|---|---|---|
| Ashe 1993 | 41 | 90% | 89% | n.s. |
| Daltroy 1985 | 174 | 64% | 62% | n.s. |
| Duncan 2002 | 13 | Exercise duration: 109% Exercise frequency: 104% |
Exercise duration: 85% Exercise frequency: 64% |
n.s. p < 0.0.01 |
| Izawa 2005 | 45 | 100% | 81% | n.s. |
| Moore 2006 | 250 | Exercise amount: 29% Exercise frequency: 8% |
Exercise amount: 27% Exercise frequency: 8% |
n.s. n.s. |
| Oldridge 1983 | 120 | 54% | 42% | n.s. |
| Sniehotta 2006 | 246 | Action planning: 44% Combined planning: 2: 71% |
42% | Int 1: n.s. Int 2: p < 0.0 |
n.s. = not significant
Appendix 1. Search Strategies
CENTRAL on The Cochrane Library
#1MeSH descriptor Myocardial Ischemia explode all trees
#2(myocard* NEAR isch*mi*)
#3isch*mi* NEAR heart
#4MeSH descriptor Coronary Artery Bypass explode all trees
#5coronary
#6MeSH descriptor Coronary Disease explode all trees
#7MeSH descriptor Myocardial Revascularization explode all trees
#8MeSH descriptor Myocardial Infarction explode all trees
#9myocard* NEAR infarct*
#10heart NEAR infarct*
#11MeSH descriptor Angina Pectoris explode all trees
#12angina
#13MeSH descriptor Heart Failure, Congestive explode all trees
#14heart and (failure or attack)
#15MeSH descriptor Heart Diseases explode all trees
#16heart and disease*
#17myocard*
#18cardiac*
#19CABG
#20PTCA
#21stent* AND (heart or cardiac*)
#22MeSH descriptor Heart Bypass, Left explode all trees
#23MeSH descriptor Heart Bypass, Right explode all trees
#24(#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23)
#25MeSH descriptor Rehabilitation Centers, this term only
#26MeSH descriptor Exercise Therapy explode all trees
#27MeSH descriptor Sports, this term only
#28MeSH descriptor Exertion explode all trees
#29rehabilitat*
#30(physical* NEAR (fit* or train* or therap* or activit*))
#31MeSH descriptor Exercise explode all trees
#32(train*) near (strength* or aerobic or exercise*)
#33((exercise* or fitness) NEAR/3 (treatment or intervent* or program*))
#34MeSH descriptor Rehabilitation explode all trees
#35MeSH descriptor Patient Education explode all trees
#36(patient* NEAR/3 educat*)
#37((lifestyle or life-style) NEAR/3 (intervent* or program* or treatment*))
#38MeSH descriptor Self Care explode all trees
#39MeSH descriptor Ambulatory Care explode all trees
#40MeSH descriptor Psychotherapy explode all trees
#41psychotherap*
#42psycholog* NEAR intervent*
#43relax*
#44MeSH descriptor Mind-Body and Relaxation Techniques explode all trees
#45MeSH descriptor Counseling explode all trees#46counsel*ing
#47MeSH descriptor Cognitive Therapy explode all trees
#48MeSH descriptor Behavior Therapy explode all trees
#49(behavio*r*) NEAR/4 (modif* or therap* or rehab* or change)
#50MeSH descriptor Stress, Psychological explode all trees
#51stress NEAR manage*
#52cognitive* NEAR therap*
#53MeSH descriptor Meditation explode all trees
#54meditat*
#55MeSH descriptor Anxiety, this term only
#56(manage*) NEAR (anxiety or depres*)
#57CBT
#58hypnotherap*
#59goal NEAR/3 setting
#60(psycho-educat*) or (psychoeducat*)
#61motivat* NEAR interv*
#62MeSH descriptor Psychopathology explode all trees
#63psychopathol*
#64MeSH descriptor Autogenic Training explode all trees
#65autogenic*
#66self near (manage* or care or motivat*)
#67distress*
#68psychosocial* or psycho-social
#69MeSH descriptor Health Education explode all trees
#70(nutrition or diet or health) NEAR education
#71heart manual
#72(#25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37)
#73(#38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71)
#74(#72 OR #73)
#75(#74 AND #24)
MEDLINE DIALOG 1950-WEEK 1 2008
SEARCH: MYOCARDIAL-ISCHEMIA#.DE.
SEARCH: MYOCARD$4 NEAR (ISCHAEMI$2 OR ISCHEMI$2)
SEARCH: (ISCHAEMI$2 OR ISCHEMI$2) NEAR HEART
SEARCH: CORONARY-ARTERY-BYPASS#.DE.
SEARCH: CORONARY.TI,AB.
SEARCH: CORONARY-DISEASE#.DE.
SEARCH: MYOCARDIAL-REVASCULARIZATION#.DE.
SEARCH: MYOCARDIAL-INFARCTION#.DE.
SEARCH: MYOCARD$5 NEAR INFARCT$5
SEARCH: HEART NEAR INFARCT$5
SEARCH: ANGINA-PECTORIS#.DE.
SEARCH: ANGINA.TI,AB.
SEARCH: HEART-FAILURE-CONGESTIVE#.DE.
SEARCH: HEART NEAR FAILURE
SEARCH: 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14
SEARCH: HEART-DISEASES#.DE.
SEARCH: (HEART NEAR DISEASE$2).TI,AB.
SEARCH: MYOCARD$5.TI,AB.
SEARCH: CARDIAC$2.TI,AB.
SEARCH: CABG
SEARCH: PTCA
SEARCH: STENT$4 AND (HEART OR CARDIAC$4)
SEARCH: HEART-BYPASS-LEFT#.DE. OR HEART-BYPASS-RIGHT#.DE.
SEARCH: 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23
SEARCH: REHABILITATION-CENTERS.DE.
SEARCH: EXERCISE-THERAPY#.DE.
SEARCH: REHABILITATION.W..DE.
SEARCH: SPORTS#.W..DE.
SEARCH: EXERTION#.W..DE.
SEARCH: EXERCISE#.W..DE.
SEARCH: REHABILITAT$5.TI,AB.
SEARCH: PHYSICAL$4 NEAR (FIT OR FITNESS OR TRAIN$5 OR THERAP$5 OR ACTIVIT$5)
SEARCH: TRAIN$5 NEAR (STRENGTH$3 OR AEROBIC OR EXERCIS$4)
SEARCH: (EXERCISE$4 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$2 OR THERAPY)
SEARCH: PATIENT-EDUCATION#.DE.
SEARCH: PATIENT$2 NEAR EDUCAT$4
SEARCH: (LIFESTYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)
SEARCH: SELF-CARE.DE.
SEARCH: SELF NEAR (MANAGE$5 OR CARE OR MOTIVAT$5)
SEARCH: AMBULATORY-CARE.DE.
SEARCH: PSYCHOTHERAPY#.W..DE.
SEARCH: PSYCHOTHERAP$2.TI,AB.
SEARCH: PSYCHOLOG$5 NEAR INTERVENT$5
SEARCH: RELAX$6.TI,AB.
SEARCH: RELAXATION-TECHNIQUES#.DE. OR MIND-BODY-AND-RELAXATION-TECHNIQUES#.DE.
SEARCH: COUNSELING#.W..DE.
SEARCH: (COUNSELLING OR COUNSELING).TI,AB.
SEARCH: COGNITIVE-THERAPY#.DE.
SEARCH: BEHAVIOR-THERAPY#.DE.
SEARCH: (BEHAVIOR$4 OR BEHAVIOUR$4) NEAR (MODIFY OR MODIFICAT$4 OR THERAP$2 OR CHANGE)
SEARCH: STRESS-PSYCHOLOGICAL#.DE.
SEARCH: STRESS NEAR MANAGEMENT
SEARCH: COGNITIVE NEAR THERAP$2
SEARCH: MEDITAT$4
SEARCH: MEDITATION#.W..DE.
SEARCH: ANXIETY#.W..DE.
SEARCH: MANAGE$5 NEAR (ANXIETY OR DEPRES$5)
SEARCH: CBT.TI,AB.
SEARCH: HYPNOTHERAP$5
SEARCH: GOAL NEAR SETTING
SEARCH: GOAL$2 NEAR SETTING
SEARCH: PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
SEARCH: MOTIVAT$5 NEAR (INTERVENTION OR INTERV$3)
SEARCH: PSYCHOPATHOLOGY#.W..DE.
SEARCH: PSYCHOPATHOL$4.TI,AB.
SEARCH: PSYCHOSOCIAL$4.TI,AB.
SEARCH: DISTRESS$4.TI,AB.
SEARCH: HEALTH-EDUCATION#.DE.
SEARCH: HEALTH NEAR EDUCATION
SEARCH: HEART ADJ MANUAL
SEARCH: AUTOGENIC-TRAINING#.DE.
SEARCH: AUTOGENIC$5.TI.AB.
SEARCH: 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38
SEARCH: 39 OR 40 OR 41 OR 42 OR 43 OR 44 OR 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 OR 71 OR 72
SEARCH: 15 OR 24
SEARCH: 73 or 74
SEARCH: 75 AND 76
SEARCH: RANDOMIZED-CONTROLLED-TRIALS#.DE.
SEARCH: PT=RANDOMIZED-CONTROLLED-TRIAL
SEARCH: PT=CONTROLLED-CLINICAL-TRIAL
SEARCH: CONTROLLED-CLINICAL-TRIALS#.DE.
SEARCH: RANDOM-ALLOCATION#.DE.
SEARCH: DOUBLE-BLIND-METHOD#.DE.
SEARCH: SINGLE-BLIND-METHOD#.DE.
SEARCH: (RANDOM$ OR PLACEBO$).TI,AB.
SEARCH: ((SINGL$3 OR DOUBL$3 OR TRIPL$3 OR TREBL$3) NEAR (BLIND$3 OR MASK$3)).TI,AB.
SEARCH: RESEARCH-DESIGN#.DE.
SEARCH: PT=CLINICAL-TRIAL#
SEARCH: CLINICAL-TRIALS#.DE.
SEARCH: (CLINIC$3 ADJ TRIAL$2).TI,AB.
SEARCH: 77 AND 90
SEARCH: (ANIMALS NOT HUMANS).SH.
SEARCH: 91 NOT 92
SEARCH: LIMIT 93 TO 2001-DATE
EMBASE DIALOG 1980-WEEK 1 2008
HEART-DISEASE#.DE.
(MYOCARD$4 NEAR (ISCHAEMI$2 OR ISCHEMI$2)).TI,AB.
((ISCHAEMI$2 OR ISCHEMI$2) NEAR HEART).TI,AB.
CORONARY-ARTERY-DISEASE#.DE.
TRANSLUMINAL-CORONARY-ANGIOPLASTY#.DE.
(CORONARY NEAR (DISEASE$2 OR BYPASS$2 OR THROMBO$5 OR ANGIOPLAST$2)).TI,AB.
HEART-INFARCTION#.DE.
(MYOCARD$4 NEAR INFARCT$5).TI,AB.
(HEART NEAR INFARC$5).TI,AB.
HEART-MUSCLE-REVASCULARIZATION#.DE.
ANGINA-PECTORIS#.DE.
ANGINA.TI,AB.
CONGESTIVE-HEART-FAILURE#.DE.
(HEART NEAR FAILURE).TI,AB.
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14
(HEART NEAR DISEASE$2).TI,AB.
CARDIAC$2.TI,AB.
CABG.TI,AB.
PTCA.TI,AB.
STENT$4.TI,AB. AND HEART.TI,AB.
EXTRACORPOREAL-CIRCULATION#.DE.
16 OR 17 OR 18 OR 19 OR 20 OR 21
15 OR 22
PSYCHOTHERAPY#.W..DE.
PSYCHOTHERAP$2.TI,AB.
PSYCHOLOG$5 NEAR INTERVENT$5
RELAX$6.TI,AB.
RELAXATION-TRAINING#.DE.
COUNSELING#.W..DE.
(COUNSELLING OR COUNSELING).TI,AB.
(BEHAVIOR$4 OR BEHAVIOUR$4) NEAR (MODIFY OR MODIFICAT$4 OR THERAPY$2 OR CHANGE)
STRESS-MANAGEMENT#.DE.
STRESS NEAR MANAGEMENT
MEDITATION#.W..DE.
MEDITAT$5.TI,AB.
MANAGE$5 NEAR (ANXIETY OR DEPRES$5)
CBT.TI,AB.
HYPNOTHERAP$2.TI,AB.
GOAL$2 NEAR SETTING
PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
MOTIVAT$5 NEAR INTERVENT$6
PSYCHOSOCIAL-CARE#.DE. OR PSYCHOSOCIAL-REHABILITATION#.DE.
PSYCHOSOCIAL.TI,AB.
HEALTH-EDUCATION#.DE.
HEALTH NEAR EDUCATION
HEART ADJ MANUAL
AUTOGENIC-TRAINING#.DE.
AUTOGENIC.TI,AB.
REHABILITATION#.W..DE.
REHABILITATION-CENTER#.DE.
REHABIL$.TI,AB.
SPORT#.W..DE.
KINESIOTHERAPY#.W..DE.
EXERCISE#.W..DE.
PHYSIOTHERAPY#.W..DE.
PHYSICAL$4 NEAR (FIT OR FITNESS OR TRAIN$5 OR THERAP$5 OR ACTIVIT$5)
TRAIN$5 NEAR (STRENGTH$3 OR AEROBIC OR EXERCIS$4)
(EXERCISE$4 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$2 OR THERAPY)
AEROBIC$4 NEAR EXERCISE$4
(KINESIOTHERAPY OR PHYSIOTHERAPY).TI,AB.
PATIENT-EDUCATION#.DE.
PATIENT$2 NEAR EDUCAT$4
(LIFESTYLE OR LIFE ADJ STYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)
SELF-CARE#.DE.
SELF NEAR (MANAGE$5 OR CARE OR MOTIVAT$5)
AMBULATORY-CARE#.DE.
PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
MOTIVAT$5 NEAR INTERVENT$6
PSYCHOSOCIAL-CARE#.DE. OR PSYCHOSOCIAL-REHABILITATION#.DE.
PSYCHOSOCIAL.TI,AB.
HEALTH-EDUCATION#.DE.
HEALTH NEAR EDUCATION
HEART ADJ MANUAL
AUTOGENIC-TRAINING#.DE.
AUTOGENIC.TI,AB.
PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5
MOTIVAT$5 NEAR INTERVENT$6
PSYCHOSOCIAL-CARE#.DE. OR PSYCHOSOCIAL-REHABILITATION#.DE.
PSYCHOSOCIAL.TI,AB.
HEALTH-EDUCATION#.DE.
HEALTH NEAR EDUCATION
HEART ADJ MANUAL
24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49
50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 OR 71 OR 72 OR 73 OR 74 OR 75 OR 76 OR 77 OR 78 OR 79 OR 80 OR 81 OR 82
83 OR 84
(RANDOM$ OR PLACEBO$).TI,AB.
(SINGL$4 OR DOUBLE$4 OR TRIPLE$4 OR TREBLE$4).TI,AB. AND (BLIND$4 OR MASK$4).TI,AB.
(CONTROLLED ADJ CLINICAL ADJ TRIAL).TI,AB.
RANDOMIZED-CONTROLLED-TRIAL#.DE.
1 OR 2 OR 3 OR 4
23 AND 85
91 AND 92
LIMIT 92 TO 2001-2008
CINAHL DIALOG 1980-WEEK 1 2008
((MYOCARD$4 OR HEART) NEAR (ISCHAEMI$2 OR ISCHEMI$2)).TI,AB.
CORONARY.TI,AB.
((MYOCARD$4 OR HEART) NEAR INFARC$5).TI,AB.
ANGINA.TI,AB.
(HEART NEAR FAILURE).TI,AB.
(HEART NEAR DISEAS$2).TI,AB.
CARDIAC$2.TI,AB.
CABG
PTCA
STENT$4.TI,AB. AND (HEART OR CARDIAC$4).TI,AB.
MYOCARDIAL-ISCHEMIA#.DE.
MYOCARDIAL-INFARCTION#.DE.
CORONARY-ARTERY-BYPASS#.DE.
CORONARY-DISEASE#.DE.
CARDIAC-PATIENTS#.DE.
MYOCARDIAL-DISEASES#.DE.
MYOCARDIAL-REVASCULARIZATION#.DE.
HEART-DISEASES#.DE.
CARDIOVASCULAR-DISEASES#.DE.
HEART-FAILURE-CONGESTIVE#.DE.
ANGINA-PECTORIS#.DE.
1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21
REHABILITATION#.W..DE.
SPORTS#.W..DE.
EXERCISE#.W..DE.
PHYSICAL-ACTIVITY#.DE.
MUSCLE-STRENGTHENING#.DE.
AEROBIC-EXERCISES#.DE.
PHYSICAL-FITNESS#.DE.
PATIENT-EDUCATION#.DE.
THERAPEUTIC-EXERCISE#.DE.
REHABILITAT$5.TI,AB.
(PHYSICAL$4 NEAR (FIT OR FITNESS OR TRAIN$4 OR THERAP$5 OR ACTIVIT$4)).TI,AB.
(TRAIN$4 NEAR (STRENGTH$3 OR AEROBIC OR EXERCIS$4)).TI,AB.
((EXERCISE$4 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$2 OR THERAPY)).TI,AB.
(PATIENT$2 NEAR EDUCAT$4).TI,AB.
((LIFESTYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)).TI,AB.
SELF-CARE#.DE.
(SELF NEAR (MANAGE$5 OR CARE OR MOTIVAT$5)).TI,AB.
AMBULATORY-CARE#.DE.
AEROBIC.TI,AB.
RESISTANCE ADJ TRAIN$4
MUSCLE ADJ STRENGTH$5
AEROBIC.TI,AB.
RESISTANCE ADJ TRAIN$4
MUSCLE ADJ STRENGTH$5
PSYCHOTHERAPY#.W..DE.
PSYCHOTHERAP$2.TI,AB.
(PSYCHOLOG$5 NEAR INTERVENT$5).TI,AB.
RELAX.TI,AB.
RELAXATION-TECHNIQUES#.DE.
(COUNSELLING OR COUNSELING).TI,AB.
COUNSELING#.W..DE.
((BEHAVIOR$4 OR BEHAVIOUR$4) NEAR (MODIFY OR MODIFICAT$4 OR THERAP$2 OR CHANGE)).TI,AB.
STRESS-MANAGEMENT#.DE.
(STRESS NEAR MANAG$5).TI,AB.
(COGNITIVE NEAR THERAP$2).TI,AB.
MEDITATION#.W..DE.
MEDITAT$5.TI,AB.
ANXIETY#.W..DE.
(MANAGE$5 NEAR (ANXIETY OR DEPRESS$5)).TI,AB.
CBT.TI,AB.
HYPNOTHERAP$5.TI,AB.
(GOAL$2 NEAR SETTING).TI,AB.
(PSYCHO-EDUCAT$5 OR PSYCHOEDUCAT$5).TI,AB.
(MOTIVAT$5 NEAR (INTERV$3 OR INTERVENT$5)).TI,AB.
PSYCHOSOCIAL$4.TI,AB.
HEALTH-EDUCATION#.DE.
(HEALTH NEAR EDUCAT$5).TI,AB.
HEART ADJ MANUAL
AUTOGENIC$3.TI,AB.
23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 OR 43 OR 44 OR 45 OR 46
47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 OR 64 OR 65 OR 66 OR 67 OR 68 OR 69 OR 70 OR 71
72 OR 73
22 AND 74
PT=CLINICAL-TRIAL
CLINICAL-TRIALS#.DE.
(RANDOM$5 OR PLACEBO$2).TI,AB.
(SINGL$ OR DOUBLE$ OR TRIPLE$ OR TREBLE$).TI,AB. AND (BLIND$ OR MASK$).TI,AB.
CONTROLLED ADJ CLINICAL ADJ TRIALS
76 OR 77 OR 78 OR 79 OR 80
75 AND 81
LIMIT 82 TO 2001-2008
PsycINFO DIALOG 1972 TO JAN WEEK 1
SEARCH: HEART-DISORDERS#.DE.
SEARCH: MYOCARDIAL-INFARCTIONS.DE.
SEARCH: ISCHEMIA#.W..DE.
SEARCH: HEART-SURGERY.DE.
SEARCH: ANGIOPLASTY
SEARCH: HEART ADJ BYPASS
SEARCH: CORONARY.TI,AB.
SEARCH: (ISCHEMI$3 OR ISCHAEMI$3).TI,AB.
SEARCH: (MYOCARD$5 NEAR INFARCT$5).TI,AB.
SEARCH: (HEART NEAR (INFARC$5 OR FAILURE OR ATTACK)).TI,AB.
SEARCH: ANGINA.TI,AB.
SEARCH: (HEART NEAR DISEASE$2).TI,AB.
SEARCH: MYOCARD$5.TI,AB.
SEARCH: CARDIAC$4.TI,AB.
SEARCH: CABG.TI,AB.
SEARCH: PTCA.TI,AB.
SEARCH: 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16
SEARCH: PHYSICAL-ACTIVITY#.DE.
SEARCH: SPORTS#.W..DE.
SEARCH: PHYSICAL-EDUCATION.DE.
SEARCH: HEALTH-BEHAVIOR#.DE.
SEARCH: PHYSICAL-FITNESS.DE.
SEARCH: (PHYSICAL ADJ EDUCATION).TI,AB.
SEARCH: EXERTION.TI,AB.
SEARCH: REHABILITAT$6.TI,AB.
SEARCH: (PHYSICAL NEAR (FIT$5 OR TRAIN$5 OR THERAP$5 OR ACTIVIT$4)).TI,AB.
SEARCH: (TRAIN$4 NEAR (STRENGTH$4 OR AEROBIC OR EXERCISE$2)).TI,AB.
SEARCH: ((EXERCISE$3 OR FITNESS) NEAR (TREATMENT OR INTERVENT$4 OR PROGRAM$4 OR THERAP$2)).TI,AB.
SEARCH: (PATIENT WITH EDUCATION).TI,AB.
SEARCH: CLIENT-EDUCATION#.DE.
SEARCH: HEALTH-PROMOTION#.DE.
SEARCH: ((LIFESTYLE OR LIFE-STYLE) NEAR (INTERVENT$5 OR PROGRAM$2 OR TREATMENT$2)).TI,AB.
SEARCH: OUTPATIENT-TREATMENT#.DE.
SEARCH: 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33
SEARCH: PSYCHOTHERAPY#.W..DE.
SEARCH: PSYCHOTHERAP$2.TI,AB.
SEARCH: TREATMENT#.W..DE.
SEARCH: (PSYCHOLOG$4 NEAR INTERVENT$5).TI,AB.
SEARCH: COUNSELING#.W..DE.
SEARCH: COPING-BEHAVIOR#.DE.
SEARCH: MEDITATION.W..DE.
SEARCH: AUTOGENIC-TRAINING.DE.
SEARCH: HEALTH-EDUCATION#.DE.
SEARCH: RELAX$6.TI,AB.
SEARCH: (COUNSELLING OR COUNSELING).TI,AB.
SEARCH: ((BEHAVIOUR OR BEHAVIOR) NEAR (MODIF$5 OR THERAP$5 OR REHABILIT$5 OR CHANGE)).TI,AB.
SEARCH: (STRESS NEAR MANAGE$5).TI,AB.
SEARCH: MEDITAT$5.TI,AB.
SEARCH: (MANAGE$5 NEAR (ANXIETY OR DEPRES$5)).TI,AB.
SEARCH: (CBT OR CGNITIV$2 NEAR THERAP$3).TI,AB.
SEARCH: HYPNOTHERAP$3.TI,AB.
SEARCH: (PSYCHO-EDUCAT$6 OR PSYCHOEDUCAT$6).TI,AB.
SEARCH: (MOTIVAT$5 NEAR INTERVENT$5).TI,AB.
SEARCH: (SELF NEAR MANAG$6).TI,AB.
SEARCH: AUTOGENIC$3.TI,AB.
SEARCH: (GOAL NEAR SETTING).TI,AB.
SEARCH: (HEALTH NEAR EDUCATION).TI,AB.
SEARCH: (HEART ADJ MANUAL).TI,AB.
SEARCH: 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 OR 43 OR 44 OR 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58
SEARCH: 17 AND (34 OR 59)
SEARCH: (RANDOM$5 OR PLACEBO$5).TI,AB.
SEARCH: (DOUBLE$4 OR SINGLE$4 OR TRIPLE$4).TI,AB. AND (BLIND$4 OR MASK OR SHAM$4 OR DUMMY).TI,AB.
SEARCH: RCT.TI,AB.
SEARCH: AT=TREATMENT$
SEARCH: 61 OR 62 OR 63 OR 64
SEARCH: 60 AND 66
SEARCH: LIMIT 66 TO YRS=2001-2008
ISI Proceedings
#5 and #6
Databases=STP Timespan=2001-2008 # 6 TS=(rehab* or educat*)
Databases=STP Timespan=2001-2008
# 5 #4 OR #3 OR #2 OR #1 Databases=STP Timespan=2001-2008 # 4 TS=(angina or cardiac* or PTCA or CABG)
Databases=STP Timespan=2001-2008
# 3 TS=((heart) SAME (infarct* or isch?emia or failure or attack))
Databases=STP Timespan=2001-2008
# 2 TS=((coronary* or heart*) SAME (by?pass or disease*))
Databases=STP Timespan=2001-2008
# 1 TS=((myocard*) SAME (isch?emia or infarct* or revasculari?*))
Databases=STP Timespan=2001-2008
HISTORY
Protocol first published: Issue 2, 2008
Review first published: Issue 7, 2010
Footnotes
DECLARATIONS OF INTEREST
None known.
References to studies included in this review
- Ashe 1993 {published data only} .Ashe ED. The effects of a relapse prevention program on adherence to a phase II cardiac exercise program. PhD Thesis. Florida State University; Florida: 1993. Florida: Florida State University. [Google Scholar]
- Daltroy 1985 {published data only} .Daltroy LH. Improving cardiac patient adherence to exercise regimens: a clinical trial of health education. Journal of Cardiac Rehabilitation. 1985;5:40–9. [Google Scholar]
- Duncan 2002 {published data only} .Duncan K, Pozehl B. Staying on course: the effects of an adherence facilitation intervention on home exercise participation. Progress in Cardiovascular Nursing. 2002;17(2):59–65. 71. doi: 10.1111/j.0889-7204.2002.01229.x. [DOI] [PubMed] [Google Scholar]
- Duncan K, Pozehl B. Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabilitation Nursing. 2003;28(4):117–22. doi: 10.1002/j.2048-7940.2003.tb01728.x. [DOI] [PubMed] [Google Scholar]
- Hillebrand 1995 {published data only} .Hillebrand T, Frodermann H, Lehr d, Wirth A. Vermehrte Teilnahme an ambulaten Herzgruppen durch poststation are Nachsorge [Increased participation in coronary groups by means of an outpatient care program] Herz Kreislauf. 1995;27:346–9. [Google Scholar]
- Izawa 2005 {published data only} .Izawa K, Watanabe S, Omiya K, Hirano Y, Oka K, Osada N, et al. Effect of the self-monitoring approach on exercise maintenance during cardiac rehabilitation: a randomized, controlled trial. American Journal of Physical Medicine and Rehabilitation/Association of Academic Physiatrists. 2005;84(5):313–21. doi: 10.1097/01.phm.0000156901.95289.09. [DOI] [PubMed] [Google Scholar]
- Jolly 1999 {published data only} .Jolly K, Bradley F, Sharp S, Smith H, Mant D. Follow-up care in general practice of patients with myocardial infarction or angina pectoris: initial results of the SHIP trial. Southampton Heart Integrated Care Project. Family Practice. 1998;15(0263-2136 (Print), 6):548–55. doi: 10.1093/fampra/15.6.548. [DOI] [PubMed] [Google Scholar]
- Jolly K, Bradley F, Sharp S, Smith H, Thompson S, Kinmonth AL, et al. The SHIP Collaborative Group Randomised controlled trial of follow up care in general practice of patients with myocardial infarction and angina: final results of the Southampton heart integrated care project (SHIP) BMJ. 1999;318(7185):706–11. doi: 10.1136/bmj.318.7185.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore 2006 {published data only} .Moore SM, Charvat JM, Gordon NH, Pashkow F, Ribisl P, Roberts BL, et al. Effects of a CHANGE intervention to increase exercise maintenance following cardiac events. Annals of Behavioral Medicine. 2006;31(1):53–62. doi: 10.1207/s15324796abm3101_9. [DOI] [PubMed] [Google Scholar]
- Oldridge 1983 {published data only} .Oldridge NB, Jones NL. Improving patient compliance in cardiac exercise rehabilitation: effects of written agreement and self-monitoring. Journal of Cardiac Rehabilitation. 1983;3:257–62. [Google Scholar]
- Sniehotta 2006 {published data only} .Sniehotta F, Scholz U, Schwarzer R. Action plans and coping plans for physical exercise: A longitudinal intervention study in cardiac rehabilitation. British Journal of Health Psychology. 2006;11(1):23–37. doi: 10.1348/135910705X43804. [DOI] [PubMed] [Google Scholar]
- Wyer 2001 {published data only} .Wyer SJ, Earll L, Joseph S, Harrison J, Giles M, Johnston M. Increasing attendance rates at a cardiac rehabilitation programme: an intervention study using the Theory of Planned Behaviour. Coronary Health Care. 2001;5:154–9. [Google Scholar]
References to studies excluded from this review
- Aish 1996 {published data only} .Aish AE, Isenberg M. Effects of Orem-based nursing intervention on nutritional self-care of myocardial infarction patients. International Journal of Nursing Studies. 1996;33(3):259–70. doi: 10.1016/0020-7489(95)00059-3. [DOI] [PubMed] [Google Scholar]
- Brodie 2005 {published data only} .Brodie D, Inoue A. Motivational interviewing to promote physical activity for people with chronic heart failure. Journal of Advanced Nursing. 2005;50(5):518–27. doi: 10.1111/j.1365-2648.2005.03422.x. [DOI] [PubMed] [Google Scholar]
- Carroll 2007 {published data only} .Carroll D, Rankin S, Cooper B. The effects of a collaborative peer advisor/advanced practice nurse intervention: cardiac rehabilitation participation and rehospitalization in older adults after a cardiac event. Journal of Cardiovascular Nursing. 2007;22(4):313–9. doi: 10.1097/01.JCN.0000278955.44759.73. [DOI] [PubMed] [Google Scholar]
- Duncan 2001 {published data only} .Duncan K, Pozehl B, Rosado K. The effects of behavioural feedback on adherence to dietary sodium intake for patients with congestive heart failure. Journal of Cardiopulmonary Rehabilitation. 2001;21:304. [Google Scholar]
- Froelicher 2003 {published data only} .Froelicher E, Miller N, Buzaitis A, Pfenninger P, Misuraco A, Jordan S, et al. The Enhancing Recovery in Coronary Heart Disease Trial ENRICHD: strategies and techniques for enhancing retention of patients with acute myocardial infarction and depression or social isolation. Journal of Cardiopulmonary Rehabilitation. 2003;23(4):269–80. doi: 10.1097/00008483-200307000-00004. [DOI] [PubMed] [Google Scholar]
- Hopper 1995 {published data only} .Hopper HL. The effects of telephone contact on the exercise adherence of cardiac patients. PhD Thesis. University of Denver; Denver: 1995. Denver: University of Denver. [Google Scholar]
- Hughes 2002 {published data only} .Hughes A, Gillies F, Kirk A, Mutrie N, Hillis W, Macintyre P. Exercise consultation improves short-term adherence to exercise during phase IV cardiac rehabilitation: a randomized, controlled trial. Journal of Cardiopulmonary Rehabilitation. 2002;22(6):421–5. doi: 10.1097/00008483-200211000-00007. [DOI] [PubMed] [Google Scholar]
- Hughes 2007 {published data only} .Hughes AR, Mutrie N, Macintyre PD. Effect of an exercise consultation on maintenance of physical activity after completion of phase III exercise-based cardiac rehabilitation. European Journal of Cardiovascular Prevention and Rehabilitation. 2007;14(1):114–21. doi: 10.1097/HJR.0b013e3280116485. [DOI] [PubMed] [Google Scholar]
- Kummel 2007 {published data only} .Kummel M, Vahlberg T, Ojanlatva A, Kärki R, Mattila T, Kivelä S. Effects of an intervention on health behaviors of older coronary artery bypass CAB patients. Archives of Gerontology and Geriatrics. 2007;46(2):227–44. doi: 10.1016/j.archger.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Luszczynska 2006 {published data only} .Luszczynska A. An implementation intentions intervention, the use of a planning strategy, and physical activity after myocardial infarction. Social Science & Medicine. 2006;62(4):900–8. doi: 10.1016/j.socscimed.2005.06.043. [DOI] [PubMed] [Google Scholar]
- Mahler 1999 {published data only} .Mahler HI, Kulik JA, Tarazi RY. Effects of a videotape information intervention at discharge on diet and exercise compliance after coronary bypass surgery. Journal of Cardiopulmonary Rehabilitation. 1999;19(3):170–7. doi: 10.1097/00008483-199905000-00004. [DOI] [PubMed] [Google Scholar]
- Moore 2002 {published data only} .Moore S, Charvat J. Using the CHANGE intervention to enhance long-term exercise. The Nursing Clinics of North America. 2002;37(2):273–83. doi: 10.1016/s0029-6465(01)00008-1. [DOI] [PubMed] [Google Scholar]
- Palomki 2002 {published data only} .Palomäki A, Miilunpalo S, Holm P, Mäkinen E, Malminiem K. Effects of preventive group education on the resistance of LDL against oxidation and risk factors for coronary heart disease in bypass surgery patients. Annals of Medicine. 2002;34(4):272–83. doi: 10.1080/078538902320322538. [DOI] [PubMed] [Google Scholar]
- Rejeski 2002 {published data only} .Rejeski WJ, Foy CG, Brawley LR, Brubaker PH, Focht BC, Norris JL, et al. Older adults in cardiac rehabilitation: a new strategy for enhancing physical function. Medicine and Science in Sports and Exercise. 2002;34:1705–13. doi: 10.1097/00005768-200211000-00003. [DOI] [PubMed] [Google Scholar]
- Sniehotta 2005 {published data only} .Sniehotta FF, Scholz U, Schwarzer R, Fuhrmann B, Kiwus U, Völler H. Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. International Journal of Behavioral Medicine. 2005;12(4):244–55. doi: 10.1207/s15327558ijbm1204_5. [DOI] [PubMed] [Google Scholar]
- Southard 2003 {published data only} .Southard B, Southard D, Nuckolls J. Clinical trial of an Internet-based case management system for secondary prevention of heart disease. Journal of Cardiopulmonary Rehabilitation. 2003;23(5):341–8. doi: 10.1097/00008483-200309000-00003. [DOI] [PubMed] [Google Scholar]
- Stromberg 2006 {published data only} .Stromberg A, Dahlstrom U, Fridlund B. Computer-based education for patients with chronic heart failure A randomised, controlled, multicentre trial of the effects on knowledge, compliance and quality of life. Patient Education and Counseling. 2006;64(1-3):128–35. doi: 10.1016/j.pec.2005.12.007. [DOI] [PubMed] [Google Scholar]
- Vestfold 2003 {published data only} .Vestfold Heartcare Study Group Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention programme in patients with coronary heart disease. European Journal of Cardiovascular Prevention and Rehabilitation. 2003;10:429–37. doi: 10.1097/01.hjr.0000107024.38316.6a. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
- Beckie 2006 {published data only} .Beckie TM. A behavior change intervention for women in cardiac rehabilitation. Journal of Cardiovascular Nursing. 2006;21(2):146–53. doi: 10.1097/00005082-200603000-00013. [DOI] [PubMed] [Google Scholar]
Additional references
- Ajzen 1986 .Ajzen I, Madden TJ. Prediction of goal-directed behaviour: attitudes, intentions and perceived behavioural control. Journal of Experimental Social Psychology. 1986;22:453–74. [Google Scholar]
- Al-Ali 2004 .Al-Ali N, Haddad LG. The effect of the health belief model in explaining exercise participation among Jordanian myocardial infarction patients. Journal of Transcultural Nursing. 2004;15(2):114–21. doi: 10.1177/1043659603262484. [DOI] [PubMed] [Google Scholar]
- Balady 2007 .Balady GJ, Williams MA, Ades PA, Bittner V, Comoss P, Foody JM, et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115(20):2675–82. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- Bethell 2001 .Bethell HJ, Turner SC, Evans JA, Rose L. Cardiac rehabilitation in the United Kingdom. How complete is the provision? Journal of Cardiopulmonary Rehabilitation. 2001;21(2):111–5. doi: 10.1097/00008483-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Blackburn 2000 .Blackburn GG, Foody JM, Sprecher DL, Park E, Apperson-Hansen C, Pashkow FJ. Cardiac rehabilitation participation patterns in a large, tertiary care center: evidence for selection bias. Journal of Cardiopulmonary Rehabilitation. 2000;20(3):189–95. doi: 10.1097/00008483-200005000-00007. [DOI] [PubMed] [Google Scholar]
- Bunker 1999 .Bunker S, McBurney H, Cox H, Jelinek M. Identifying participation rates at outpatient cardiac rehabilitation programs in Victoria, Australia. Journal of Cardiopulmonary Rehabilitation. 1999;19(6):334–8. doi: 10.1097/00008483-199911000-00001. [DOI] [PubMed] [Google Scholar]
- Daly 2002 .Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: a critical literature review. Progress in Cardiovascular Nursing. 2002;17(1):8–17. doi: 10.1111/j.0889-7204.2002.00614.x. [DOI] [PubMed] [Google Scholar]
- Fleury 1991 .Fleury JD. Wellness motivation in cardiac rehabilitation. Heart & Lung. 1991;20(1):3–8. [PubMed] [Google Scholar]
- Graham 2007 .Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts) European Journal of Cardiovascular Prevention and Rehabilitation. 2007;14(Suppl 2):S1–113. doi: 10.1097/01.hjr.0000277983.23934.c9. [DOI] [PubMed] [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated September 2008] The Cochrane Collaboration; 2008. Available from www.cochrane-handbook.org. [Google Scholar]
- Jackson 2005 .Jackson L, Leclerc J, Erskine Y, Linden W. Getting the most out of cardiac rehabilitation: a review of referral and adherence predictors. Heart. 2005;91(1):10–4. doi: 10.1136/hrt.2004.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolliffe 2001 .Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercised-based rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews. 2001;(1) doi: 10.1002/14651858.CD001800. DOI: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- Law 2002 .Law MR, Watt HC, Wald NJ. The underlying risk of death after myocardial infarction in the absence of treatment. Archives of Internal Medicine. 2002;162(21):2405–10. doi: 10.1001/archinte.162.21.2405. [DOI] [PubMed] [Google Scholar]
- Moore 2003 .Moore SM, Dolansky MA, Ruland CM, Pashkow FJ, Blackburn GG. Predictors of women’s exercise maintenance after cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 2003;23(1):40–9. doi: 10.1097/00008483-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Neal 2004 .Neal B. Secondary prevention of Cardiovascular Disease: Fixed dose combinations. In: Kaplan W, Laing R, editors. Priority medicines for Europe and the world. World Health Organization; Geneva: 2004. [Google Scholar]
- NICE 2007 .National Institute for Health and Clinical Excellence . MI: Secondary prevention. Secondary prevention in primary and secondary care for patients following a myocardial infarction. National Institute for Health and Clinical Excellence; London, UK: [accessed 18 2 2008]. 2007. Available at http://www.nice.org.uk/CG48. [Google Scholar]
- Rees 2004a .Rees K, Taylor RS, Singh S, Coats AJS, Ebrahim S. Exercise-based rehabilitation for heart failure. Cochrane Database of Systematic Reviews. 2004;(3) doi: 10.1002/14651858.CD003331.pub2. DOI: 10.1002/14651858.CD003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees 2004b .Rees K, Bennett P, West R, Davey Smith G, Ebrahim S. Psychological interventions for coronary heart disease. Cochrane Database of Systematic Reviews. 2004;(2) doi: 10.1002/14651858.CD002902.pub2. DOI: 10.1002/14651858.CD002902.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone 2005 .Stone JA, Arthur HM. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention, second edition, 2004: executive summary. Canadian Journal of Cardiology. 2005;21(Suppl D):3D–19D. [PubMed] [Google Scholar]
- Taylor 2004 .Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. American Journal of Medicine. 2004;116(10):682–92. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Taylor 2010 .Taylor RS, Dalal H, Jolly K, Moxham T, Zawada A. Home-based versus centre-based cardiac rehabilitation. Cochrane Database of Systematic Reviews. 2010;(1) doi: 10.1002/14651858.CD007130.pub2. DOI: 10.1002/14651858.CD007130.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO 1997 .World Health Organization . The World Heath Report: conquering suffering, enriching humanity. Report of the Director-General. World Health Organization; Geneva, Switzerland: 1997. [Google Scholar]
- Ziegelstein 2000 .Ziegelstein RC, Fauerbach JA, Stevens SS, Romanelli J, Richter DP, Bush DE. Patients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarction. Archives of Internal Medicine. 2000;160(12):1818–23. doi: 10.1001/archinte.160.12.1818. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Beswick 2004 .Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR, et al. Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technology Assessment. 2004;8(41) doi: 10.3310/hta8410. [DOI] [PubMed] [Google Scholar]
- Beswick 2005 .Beswick AD, Rees K, West RR, Taylor FC, Burke M, Griebsch I, et al. Improving uptake and adherence in cardiac rehabilitation: literature review. Journal of Advanced Nursing. 2005;49(5):538–55. doi: 10.1111/j.1365-2648.2004.03327.x. [DOI] [PubMed] [Google Scholar]
- * Indicates the major publication for the study