Abstract
Background
In many countries of the industrialised world second generation (atypical) antipsychotics have become first line drug treatments for people with schizophrenia. The question as to whether, and if so how much, the effects of the various second generation antipsychotics differ is a matter of debate. In this review we examine how the efficacy and tolerability of aripiprazole differs from that of other second generation antipsychotics.
Objectives
To evaluate the effects of aripiprazole compared with other atypical antipsychotics for people with schizophrenia and schizophrenia-like psychoses.
Search methods
We searched the Cochrane Schizophrenia Group Trials Register (March 2007) which is based on regular searches of BIOSIS, CENTRAL, CINAHL, EMBASE, MEDLINE and PsycINFO.
Selection criteria
We included all randomised trials comparing oral aripiprazole with oral forms of amisulpride, clozapine, olanzapine, quetiapine, risperidone, sertindole, ziprasidone or zotepine in people with schizophrenia or schizophrenia-like psychoses.
Data collection and analysis
We extracted data independently. For dichotomous data we calculated relative risks (RR) and their 95% confidence intervals (CI) on an intention-to-treat basis based on a random-effects model. We calculated numbers needed to treat/harm (NNT/NNH) where appropriate. For continuous data, we calculated weighted mean differences (MD) again based on a random-effects model.
Main results
The review currently includes four trials with 1404 participants on two out of eight possible comparisons - aripiprazole versus olanzapine and aripiprazole versus risperidone. The overall number of participants leaving the studies early was considerable (38.5%), limiting the validity of the findings, but with no significant differences between groups. Aripiprazole was less efficacious than olanzapine in terms of the general mental state (PANSS total score: n=794, 2 RCTs, MD 4.96 CI 1.85 to 8.06), but it was associated with fewer side-effects such as cholesterol increase, weight gain, sedation and prolactin associated side-effects. Compared with risperidone there was no difference in efficacy (PANSS total score: n=372, 2 RCTs, MD 1.50 CI −2.96 to 5.96). Dystonia, QTc abnormalities, prolactin and cholesterol increase were less frequent in the aripiprazole group, while tremor was more frequent in the aripiprazole group compared with those allocated risperidone.
Authors’ conclusions
Aripiprazole may be somewhat less effective than olanzapine, but more tolerable in terms of metabolic effects and sedation. There is no evidence for a difference in efficacy compared to risperidone, but for better tolerability in terms of dystonias, cholesterol prolactin increase and QTc prolongation. Randomised evidence comparing aripiprazole with other second generation antipsychotic drugs is currently not available.
Medical Subject Headings (MeSH): Antipsychotic Agents [*therapeutic use], Benzodiazepines [therapeutic use], Piperazines [*therapeutic use], Quinolones [*therapeutic use], Randomized Controlled Trials as Topic, Risperidone [therapeutic use], Schizophrenia [*drug therapy]
MeSH check words: Humans
BACKGROUND
Description of the condition
Schizophrenia is usually a chronic and disabling psychiatric disorder which afflicts approximately one per cent of the population world-wide with little gender differences. The annual incidence of schizophrenia averages 15 per 100,000, the point prevalence averages approximately 4.5 per population of 1000 and the risk of developing the illness over one’s lifetime averages 0.7% (Tandon 2008). Its typical manifestations are ’positive’ symptoms such as fixed, false beliefs (delusions) and perceptions without cause (hallucinations), ’negative’ symptoms such as apathy and lack of drive, disorganisation of behaviour and thought, and catatonic symptoms such as mannerisms and bizarre posturing (Carpenter 1994). The degree of suffering and disability is considerable with 80 - 90% not working (Marvaha 2004) and up to 10% dying (Tsuang 1978). In the age group of 15-44 years, Schizophrenia is among the top ten leading causes of disease-related disability in the world (WHO 2001). Conventional antipsychotic drugs, such as chlorpromazine and haloperidol, have traditionally been used as first line antipsychotics for people with schizophrenia (Kane 1993). The re-introduction of clozapine in the United States of America and findings to indicate that clozapine seemed more effective than other drugs, as well as being associated with fewer movement disorders than chlorpromazine (Kane 1988), boosted the development of new/second/atypical generation antipsychotics (SGA).
Description of the intervention
There is no good definition of what constitutes an atypical/second generation antipsychotic, but they were initially said to differ from older generation drugs in that they did not cause movement disorders (catalepsy) in rats at clinically effective doses (Arnt 1998). The terms new or second generation to describe clozapine, a very old drug, are equally poor descriptors. According to treatment guidelines (APA 2004, Gaebel 2006) second generation antipsychotics include drugs such as amisulpride, aripiprazole, clozapine, olanzapine, quetiapine, risperidone, sertindole, ziprasidone and zotepine, although it is unclear whether some old and inexpensive compounds such as sulpiride, perazine or even low dose chlorpromazine, have similar properties (Möller 2000). High expectations were raised for these second generation antipsychotics as regards their superior effects in a number of areas such as compliance, cognitive functioning, negative symptoms, movement disorders, quality of life and treatment of people whose illness had been resistant to treatment.
How the intervention might work
Aripiprazole is currently being marketed by Otsuka pharmaceutical and Bristol-Myers Squibb. It is said to be the prototype of a new and third generation of antipsychotics; the so called dopamine-serotonin system stabilisers. It is reported to exert its antipsychotic effects by acting as a partial agonist at D2 dopamine and 5-HT1a serotonin receptors and as an agonist at 5-HT2 serotonin receptors. It has been postulated that through the above receptor site actions, and hence dopamine and serotonin system stabilisation, a partial D2 agonist would be able to act as an antagonist in path-ways where an abundance of dopamine was producing psychosis, yet it would stimulate receptors as an agonist at sites in which low dopaminergic tone would produce adverse effects (e.g. areas mediating motor movement and prolactin release (Rivas-Vasquez 2003)). Aripiprazole, however, also has an affinity to other receptors including D3, D4, 5-HT2c, 5HT7, alpha-1 adrenergic and histamine receptors. This may explain adverse effects associated with this compound such as somnolence, headache, gastrointestinal upset and light headedness (FDA 2002). The recommended target dose for aripiprazole is 10-15 mg per day (dose range 10-30 mg/day). Phase III trials were initially conducted in Japan in 1995 and the drug was granted Approved Status by the FDA (USA) on the 15 November 2002 for the treatment of schizophrenia. Aripiprazole has since been licensed in most countries worldwide.
Why it is important to do this review
The debate as to how far the second generation antipsychotic drugs improve these outcomes compared to conventional antipsychotics continues (Duggan 2005) and results from recent studies were sobering (Jones 2006, Lieberman 2005). Nevertheless, in some parts of the world, especially in highly industrialised countries, second generation antipsychotics have become the mainstay of treatment. SGAs also differ in terms of their costs, amisulpride and risperidone for example are already generic in many countries. Therefore the question as to whether they differ from each other in their clinical effects becomes increasingly important. In this review we aim to summarise evidence from randomised controlled trials comparing aripiprazole with other second generation antipsychotics. It adds detail to the comparison previously presented in El-Sayeh 2006 and Leucht 2008.
OBJECTIVES
To review the effects of aripiprazole compared to other second generation/atypical antipsychotics for people with schizophrenia.
METHODS
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials. Where a trial was described as ’double-blind’ but it was only implied that the study was randomised, we included these trials in a sensitivity analysis. If there was no substantive difference within primary outcomes (see Types of outcome measures) when these ’implied randomisation’ studies were added, then we included these in the final analysis. If there was a substantive difference, we only used clearly randomised trials and described the results of the sensitivity analysis in the text. We excluded quasi-randomised studies, such as those allocating by using alternate days of the week.
Randomised cross-over studies will be eligible but only data up to the point of first cross-over, because of the instability of the problem behaviours and the likely carry-over effects of all treatments.
Types of participants
We included people with schizophrenia and other types of schizophrenia-like psychoses (e.g. schizophreniform and schizoaffective disorders), irrespective of the diagnostic criteria used. There is no clear evidence that the schizophrenia-like psychoses are caused by fundamentally different disease processes or require different treatment approaches (Carpenter 1994).
Types of interventions
Aripiprazole: any oral form of application, any dose.
Other new/atypical antipsychotic drugs: amisulpride, clozapine, olanzapine, quetiapine, risperidone, sertindole, ziprasidone, zotepine: any oral form of application, any dose.
Types of outcome measures
We grouped outcomes into the short term (up to 12 weeks), medium term (13-26 weeks) and long term (over 26 weeks).
Primary outcomes
No clinically important response as defined by the individual studies (e.g. global impression less than much improved or less than 50% reduction on a rating scale).
Secondary outcomes
-
1.
Leaving the studies early (any reason, adverse events, inefficacy of treatment)
-
2.
Global state
-
2.1
No clinically important change in global state (as defined by individual studies) 2.2 Relapse (as defined by the individual studies)
-
3.
Mental state (with particular reference to the positive and negative symptoms of schizophrenia)
-
3.1
No clinically important change in general mental state score
-
3.2
Average endpoint general mental score
-
3.3
Average change in general mental state score
-
3.4
No clinically important change in specific symptoms (positive symptoms of schizophrenia, negative symptoms of schizophrenia)
-
3.5
Average endpoint specific symptom score
-
3.6
Average change in specific symptom score
-
4
General functioning
-
4.1
No clinically important change in general functioning
-
4.2
Average endpoint general functioning score
-
4.3
Average change in general functioning score
-
5.
Quality of life/satisfaction with treatment
-
5.1
No clinically important change in general quality of life
-
5.2
Average endpoint general quality of life score
-
5.3
Average change in general quality of life score
-
6.
Cognitive functioning
-
6.1
No clinically important change in overall cognitive functioning
-
6.2
Average endpoint of overall cognitive functioning score
-
6.3
Average change of overall cognitive functioning score
-
7.
Service use
-
7.1
Number of patients hospitalised
-
8.
Adverse effects
-
8.1
Number of participants with at least one adverse effect.
-
8.2
Clinically important specific adverse effects (cardiac effects, death, movement disorders, prolactin increase and associated effects, weight gain, effects on white blood cell count)
-
8.3
Average endpoint in specific adverse effects
-
8.4
Average change in specific adverse effects
Search methods for identification of studies
No language restriction was applied within the limitations of the search tools.
Electronic searches
1. Update search
We searched the Cochrane Schizophrenia Group Trials Register (March 2007) using the phrase: [((aripiprazol* AND (amisulprid* OR clozapin* OR olanzapin* OR quetiapin* OR risperidon* OR sertindol* OR ziprasidon* OR zotepin*)) in title, abstract or index terms of REFERENCE) or ((aripiprazol* AND (amisulprid* OR clozapin* OR olanzapin* OR quetiapin* OR risperidon* OR sertindol* OR ziprasidon* OR zotepin*)) in interventions of STUDY)]
This register is compiled by systematic searches of major databases, hand searches and conference proceedings (see Group Module). The Cochrane Schizophrenia Group Trials Register is maintained on Meerkat 1.5. This version of Meerkat stores references as studies. When an individual reference is selected through a search all references which have been identified as the same study are also selected.
2. Previous electronic search
See Appendix 1.
Searching other resources
1. Reference searching
We inspected the reference lists of all studies identified in the search for more trials.
2. Personal contact
We contacted the first author of each included study for missing information.
3. Drug companies
We contacted the manufacturers of all atypical antipsychotics included for additional data.
Data collection and analysis
Selection of studies
We independently inspected all reports. We resolved any disagreement by discussion, and where there was still doubt, we acquired the full article for further inspection. Once the full articles were obtained, we independently decided whether the studies met the review criteria. If disagreement could not be resolved by discussion we sought further information and these trials were added to the list of those awaiting assessment.
Data extraction and management
1. Data extraction
We independently extracted data from selected trials. When disputes arose we attempted to resolve these by discussion. When this was not possible and further information was necessary to resolve the dilemma, we did not enter data and added the trial to the list of those awaiting assessment.
2. Management
We extracted the data onto standard simple forms. Where possible, we entered data in such a way that the area to the left of the line of no effect indicated a favourable outcome for aripiprazole.
3. Rating scales
A wide range of instruments are available to measure outcomes in mental health studies. These instruments vary in quality and many are not validated or are even ad hoc. It is accepted generally that measuring instruments should have the properties of reliability (the extent to which a test effectively measures anything at all) and validity (the extent to which a test measures that which it is supposed to measure) (Rust 1989). Unpublished scales are known to be subject to bias in trials of treatments for schizophrenia (Marshall 2000). Therefore continuous data from rating scales were included only if the measuring instrument had been described in a peer-reviewed journal. In addition, the following minimum standards for instruments were set: the instrument should either be (a) a self-report or (b) completed by an independent rater or relative (not the therapist) and (c) the instrument should be a global assessment of an area of functioning.
Assessment of risk of bias in included studies
Again working independently, KK and SL assessed the risk of bias using the tool described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). This tool encourages consideration of how the sequence was generated, how allocation was concealed, the integrity of blinding at outcome, the completeness of outcome data, selective reporting and other biases.
The risk of bias in each domain and overall were assessed and categorised into:
Low risk of bias: plausible bias unlikely to seriously alter the results (categorised as ’Yes’ in Risk of Bias table)
High risk of bias: plausible bias that seriously weakens confidence in the results (categorised as ’No’ in Risk of Bias table)
Unclear risk of bias: plausible bias that raises some doubt about the results (categorised as ’Unclear’ in Risk of Bias table)
Trials with a high risk of bias (defined as at least three out of five domains were categorised as ’No’) or where allocation was clearly not concealed were not included in the review. If the raters disagreed, the final rating was made by consensus with the involvement of another member of the review group. Where inadequate details of randomisation and other characteristics of trials are provided, authors of the studies were contacted in order to obtain further information. Non-concurrence in quality assessment was reported.
Measures of treatment effect
1. Data types
We assessed outcomes using continuous (for example changes on a behaviour scale), categorical (for example, one of three categories on a behaviour scale, such as ’little change’, ’moderate change’ or ’much change’) or dichotomous (for example, either ’no important changes’ or ’important change’ in a person’s behaviour) measures. Currently RevMan does not support categorical data so we were unable to analyse this.
2. Dichotomous-yes/no-data
We carried out an intention to treat analysis. Everyone allocated to the intervention were counted, whether they completed the follow up or not. It was assumed that those who left early had no change in their outcome. This rule is conservative concerning response to treatment, because it assumes that those discontinuing the studies would not have responded. It is not conservative concerning adverse effects, but we felt that assuming that all those leaving early would have developed side-effects would overestimate risk. Where possible, efforts were made to convert outcome measures to dichotomous data. This can be done by identifying cut-off points on rating scales and dividing participants accordingly into ’clinically improved’ or ’not clinically improved’. It was generally assumed that if there had been a 50% reduction in a scale-derived score such as the Brief Psychiatric Rating Scale (BPRS, Overall 1962) or the Positive and Negative Syndrome Scale (PANSS, Kay 1986), this could be considered as a clinically significant response (Leucht 2005a, Leucht 2005b). If data based on these thresholds were not available, we used the primary cut-off presented by the original authors.
We calculated the relative risk (RR) and its 95% confidence interval (CI) based on the random-effects model, as this takes into account any differences between studies even if there is no statistically significant heterogeneity. It has been shown that RR is more intuitive (Boissel 1999) than odds ratios and that odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). This misinterpretation then leads to an overestimate of the impression of the effect. When the overall results were significant we calculated the number needed to treat (NNT) and the number needed to harm (NNH) as the inverse of the risk difference.
3. Continuous data
3.1 Normal distribution of the data
The meta-analytic formulas applied by RevMan Analyses (the statistical programme included in RevMan) require a normal distribution of data. The software is robust towards some skew but to which degree of skewness meta-analytic calculations can still be reliably carried out is unclear. On the other hand, excluding all studies on the basis of estimates of the normal distribution of the data also leads to a bias, because a considerable amount of data may be lost leading to a selection bias. Therefore, we included all studies in the primary analysis. In a sensitivity analysis we excluded potentially skewed data applying the following rules:
-
a)
When a scale started from the finite number zero the standard deviation, when multiplied by two, was more than the mean (as otherwise the mean is unlikely to be an appropriate measure of the centre of the distribution, Altman 1996).
-
b)
If a scale started from a positive value (such as PANSS which can have values from 30 to 210) the calculation described above was modified to take the scale starting point into account. In these cases skew is present if 2SD>(S-Smin), where S is the mean score and Smin is the minimum score). In large studies (as a cut-off we used 200 participants) skewed data pose less of a problem. In these cases we entered the data in a synthesis and no sensitivity analysis was applied.
-
d)
The rules explained in a) and b) do not apply to change data. The reason is that when continuous data are presented on a scale which includes a possibility of negative values, it is difficult to tell whether data are non-normally distributed (skewed) or not. This is also the case for change data (endpoint minus baseline). In the absence of individual patient data it is impossible to know if data are skewed, though this is likely. After consulting the ALL-STAT electronic statistics mailing list, we presented change data in RevMan Analyses in order to summarise available information. In doing this, it was assumed either that data were not skewed or that the analysis could cope with the unknown degree of skew. Without individual patient data it is impossible to test this assumption. We therefore included change data and did not apply a sensitivity analysis. For continuous outcomes we estimated a mean difference (MD) between groups. MDs were again based on the random-effects model, as this takes into account any differences between studies even if there is no statistically significant heterogeneity. We combined both endpoint data and change data in the analysis because there is no principal statistical reason why end-point and change data should measure different effects (Higgins 2008). When standard errors instead of standard deviations (SD) were presented, we converted the former to standard deviations. If both were missing we estimated SDs from p-values or used the average SD of the other studies (Furukawa 2006).
Unit of analysis issues
1. Cluster trials
Studies increasingly employ cluster randomisation (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Authors often fail to account for intraclass correlation in clustered studies, leading to a unit of analysis error (Divine 1992) whereby p values are spuriously low, confidence intervals unduly narrow and statistical significance over-estimated. This can cause Type I errors (Bland 1997, Gulliford 1999).
Where clustering was not accounted for in primary studies, we presented the data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intraclass correlation coefficients of their clustered data and to adjust for this using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will also present these data as if from a non-cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a design effect. This is calculated using the mean number of participants per cluster (m) and the intraclass correlation coefficient (ICC) [Design effect=1+(m-1)*ICC] (Donner 2002). If the ICC was not reported it was assumed to be 0.1 (Ukoumunne 1999).
If cluster studies had been appropriately analysed taking into account intraclass correlation coefficients and relevant data documented in the report, we synthesised these with other studies using the generic inverse variance technique.
2. Cross-over trials
A major concern of cross-over trials is the carry-over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence on entry to the second phase the participants can differ systematically from their initial state despite a wash-out phase. For the same reason cross-over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in schizophrenia, we will only use data of the first phase of cross-over studies.
3. Studies with multiple treatment groups
Where a study involved more than two treatment groups, if relevant, the additional treatment groups were presented in additional relevant comparisons. Data were not double counted. Where the additional treatment groups were not relevant, these data were not reproduced.
Dealing with missing data
At some degree of loss of follow-up data must lose credibility (Xia 2007). Although high rates of premature discontinuation are a major problem in this field, we felt that it was unclear which degree of attrition leads to a high degree of bias. We, therefore, did not exclude trials on the basis of the percentage of participants completing them. However we addressed the drop-out problem in all parts of the review, including the abstract. For this purpose we calculated, presented and commented on frequency statistics (overall rates of leaving the studies early in all studies and comparators pooled and their ranges).
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all the included studies within any comparison to judge for clinical heterogeneity.
2.Statistical
2.1 Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
2.2 Employing the I2 statistic
Visual inspection was supplemented using, primarily, the I2 statistic. This provides an estimate of the percentage of variability due to heterogeneity rather than chance alone. Where the I2 estimate was greater than or equal to 50% we interpreted this as indicating the presence of considerable levels of heterogeneity (Higgins 2008).
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). These are described in section 10.1 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). We are aware that funnel plots may be useful in investigating small-study effects but are of limited power to detect such effects when there are few studies. We entered data from all identified and selected trials into a funnel graph (trial effect versus trial size) in an attempt to investigate the likelihood of overt publication bias. We did not undertake a formal test for funnel plot asymmetry.
Data synthesis
Where possible for both dichotomous and continuous data we used the random-effects model for data synthesis as this takes into account any differences between studies even if there is no statistically significant heterogeneity. We understand that there is no closed argument for preference for use of fixed or random-effects models. The random-effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This does seem true to us, however, random-effects does put added weight onto the smaller of the studies - those trials that are most vulnerable to bias.
Subgroup analysis and investigation of heterogeneity
If data are clearly heterogeneous we checked that data are correctly extracted and entered and that we had made no unit of analysis errors. If inconsistency was high and clear reasons explaining the heterogeneity were found, we presented the data separately. If not, we commented on the heterogeneity of the data.
Sensitivity analysis
We planned sensitivity analyses a priori for examining the change in the robustness of the sensitivity to including studies with potentially skewed data. A recent report showed that some of the comparisons of atypical antipsychotics may have been biased by using inappropriate comparator doses (Heres 2006). We, therefore, also analysed whether the exclusion of studies with inappropriate comparator doses changed the results of the primary outcome and the general mental state.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
For a substantive description of studies please see Characteristics of included studies and Characteristics of excluded studies tables.
Results of the search
The search yielded 3620 reports of which 28 were closely inspected. After excluding 22 studies, six publications on four trials and two comparisons were included: aripiprazole versus olanzapine (two) and aripiprazole versus risperidone (two).
Included studies
The four included studies randomised 1404 people with the diagnosis of schizophrenia or schizoaffective disorder. All four studies are described as randomised and double-blind. All studies were sponsored by the pharmaceutical company producing aripiprazole.
1. Length of studies
Three of the included studies were short-term studies with a duration of four to six weeks. One study was a medium-term study with a duration of 26 weeks. We did not identify any long-term studies.
2. Setting
Three studies reported the setting as inpatient or originally inpatient, one study described setting as in- and outpatient.
3. Participants
In all studies the participants were diagnosed according to DSM-IV. All studies included participants with an acute exacerbation of the illness, although this was not clearly defined. Three studies mentioned the term “with an acute relapse”. The participants were usually relatively chronic with mean ages in the late thirties. Two short-term studies included participants with schizophrenia and schizoaffective disorder. The other two studies included only people with the diagnosis of schizophrenia.
4. Study size
Three studies included more than 300 people and one study included less than 100 people.
5. Interventions
In two studies the aripiprazole doses were flexible with a range from 15 to 30 mg per day. The other two studies used fixed aripiprazole doses of 15 mg per day and 20 or 30 mg per day.
6. Outcomes
6.1 Leaving the study early
All studies reported on leaving the study early due to any reason, adverse events and lack of efficacy.
6.2 Response to treatment
We prespecified at least 50% PANSS/BPRS total score reduction from baseline as a relevant cut-off to define response but such data were not presented. McQuade 2004 used ’at least much improved on the CGI’ as the primary response criteria and BMS CN 138003 2005 used a ’CGI score of three or less, or at least 20% PANSS total score reduction from baseline’ as the primary response criterion. In Potkin 2003 and Chan 2007 the primary outcome criterion was ’at least much improved on the CGI or at least 30% PANSS total score reduction from baseline’.
6.3 Rating scales
Details of scales that provided usable data are shown below. Reasons for exclusion of data from other instruments are given under ’Outcomes’ in the Characteristics of included studies section.
6.3.1 Global state scales
6.3.1.1 Clinical Global Impression Scale - CGI Scale (Guy 1976)
This is used to assess both severity of illness and clinical improvement, by comparing the conditions of the person standardised against other people with the same diagnosis. A seven-point scoring system is used with low scores showing decreased severity and/or overall improvement.
6.3.2 Mental state scales
6.3.2.1 Positive and Negative Syndrome Scale - PANSS (Kay 1986)
This schizophrenia scale has 30 items, each of which can be defined on a seven-point scoring system varying from one - absent to seven - extreme. It can be divided into three sub-scales for measuring the severity of general psychopathology, positive symptoms (PANSS-P), and negative symptoms (PANSS-N). A low score indicates lesser severity.
6.3.3 Adverse effects scales
6.3.3.1 Abnormal Involuntary Movement Scale - AIMS (Guy 1976)
This scale has been used to assess tardive dyskinesia, a long-term, drug-induced movement disorder and short-term movement disorders such as tremor.
6.3.3.2 Simpson Angus Scale - SAS (Simpson 1970)
This ten-item scale (with a scoring system of zero to four on each item) measures drug-induced parkinsonism, a short-term drug-induced movement disorder. A low score indicates low levels of parkinsonism.
6.3.3.3 Barnes Akathisia Scale - BAS (Barnes 1989)
The scale comprises items rating the observable, restless movements that characterise akathisia, a subjective awareness of restlessness, and any distress associated with the condition. These items are rated from zero (normal) to three (severe). In addition, there is an item for rating global severity (from zero (absent) to five (severe)). A low score indicates low levels of akathisia.
6.4 Adverse effects
Adverse effects were mainly recorded in open interviews. In addition, continuous data were provided for weight, QTc time and cholesterol levels.
Excluded studies
The search strategy yielded 3620 reports of which 28 potentially relevant studies were closely inspected. Twenty-two of them had to be excluded for the following reasons: one not randomised, 18 open label, two pooled analysis.
Awaiting assessment
No studies are awaiting assessment.
Ongoing studies
There appeared to be two studies comparing aripiprazole with olanzapine ongoing (see Characteristics of ongoing studies table).
Risk of bias in included studies
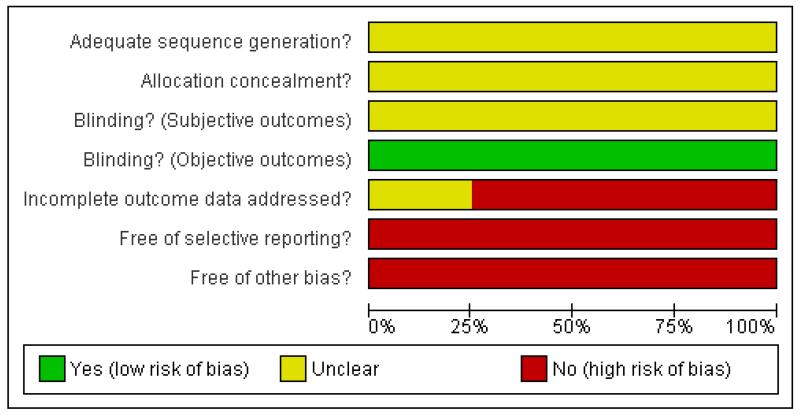
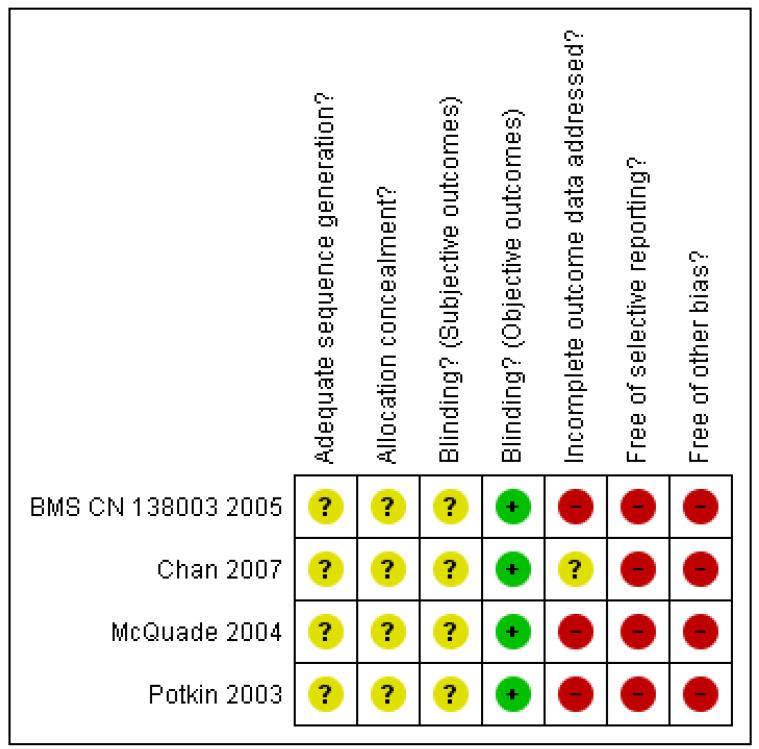
For details please refer to the risk of bias table (Figure 1, Figure 2).
Figure 1 .
Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Figure 2 .
Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Allocation
Only one study gave a few details on the randomisation method (Chan 2007), but this information was so limited that in all four included studies it remained unclear whether there was a risk of bias. No study described the method of allocation concealment.
Blinding
All of the included studies were described as double-blind. Chan 2007 and Potkin 2003 described using identical capsules for blinding. The other two studies did not provide any information on the blinding procedure. No study examined whether blinding was effective. We found that the side-effect profiles of the examined compounds are quite different which may have made blinding difficult. We therefore conclude that the risk of bias for objective outcomes (e.g. death or laboratory values) was low but there was a risk of bias for subjective outcomes.
Incomplete outcome data
In two studies the rates of participants leaving the study early were higher than 30% (McQuade 2004, Potkin 2003), in one of them, McQuade 2004, it was as high as 72% and the overall attrition was 38.5%. All studies applied the last-observation-carried-forward (LOCF) method to account for participants leaving the study early which is an imperfect method. Only McQuade 2004 analysed the study completers in a secondary analysis. It assumes that a participant who left the study prematurely would not have had a change of his condition if he had stayed in the study. This assumption can obviously be wrong.
Selective reporting
In terms of selective reporting there was a high risk of bias in all included studies. Three trials reported only those adverse events that occurred in at least five to ten per cent of the participants (BMS CN 138003 2005, Chan 2007 and Potkin 2003). By this procedure rare but important adverse events can be missed. One study did not report on the PANSS positive subscore (McQuade 2004). In two studies not all secondary outcomes have been reported (BMS CN 138003 2005, McQuade 2004).
Other potential sources of bias
All of the four included studies were sponsored by the manufacturer of aripiprazole. There is evidence that pharmaceutical companies sometimes highlight the benefits of their compounds and tend to suppress their disadvantages (Heres 2006). One study BMS CN 138003 2005 was only available as an interim report.
Effects of interventions
-
1.
COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Two studies fell into this category.
-
1.1
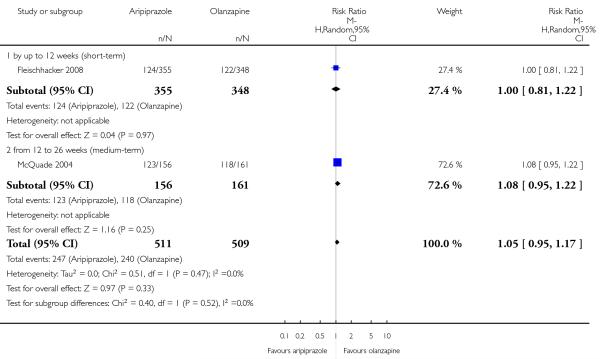
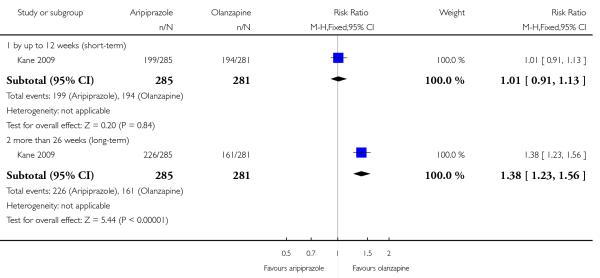
No significant response - as defined by the original studies There was no significant difference (n=1020, 2 RCTs, RR 1.05 CI 0.95 to 1.17).
-
1.2
Leaving the studies early
There was no significant difference between aripiprazole and olanzapine in terms of leaving the study early due to any reason (n= 1020, 2 RCTs, RR 1.15 CI 0.92 to 1.45), due to adverse events (n=317, 1 RCT, RR 1.27 CI 0.83 to 1.95) or due to inefficacy (n= 317,1 RCT, RR 1.70 CI 0.91 to 3.17).
-
1.3
Global state
-
1.3.1
Global state: no clinically important change
One study presented short-term data (BMS CN 138003 2005) and the other one medium-term data (McQuade 2004). There was no significant difference in short-term data (n=703, 1 RCT, RR 1.00 CI 0.81 to 1.22) and medium-term data (n=317,1 RCT, RR 1.08 CI 0.95 to 1.22). In the overall analysis there was no significant difference (n=1020, 2 RCTs, RR 1.05 CI 0.95 to 1.17).
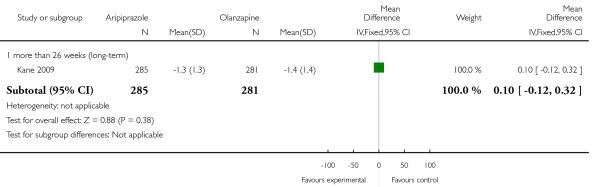
1.4 Mental state
-
1.4.1
General Mental state: PANSS total score
There was a significant difference in favour of olanzapine in the analysis of short-term data (n=703, 1 RCT, MD 5.21 CI 1.91 to 8.51) but not in the medium-term study data (n=91, 1 RCT, MD 3.00 CI −6.21 to 12.21). The overall analysis also indicated a significant difference favouring olanzapine (n=794, 2 RCTs, MD 4.96 CI 1.85 to 8.06).
-
1.5
Adverse effects
-
1.5.1
Cardiac effects - number of participants with QTc prolongation
There was no significant difference in the number of participants with QTc prolongation (n=317, 1 RCT, RR 0.34 CI 0.07 to 1.68).
-
1.5.2
Cardiac effects - mean change of QTc interval from baseline in ms
There was no significant difference in the mean change of the QTc interval (n=317, 1 RCT, MD −3.70 CI −9.51 to 2.11).
-
1.5.3
Cholesterol - number of participants with abnormally high cholesterol
Fewer patients in the aripiprazole group than in the olanzapine group had increased cholesterol levels (n=223, 1 RCT, RR 0.32 CI 0.19 to 0.54, NNH 4 CI 3 to 6).
-
1.5.4
Cholesterol - change from baseline in mg/dl
The mean increase of cholesterol levels was significantly smaller in the aripiprazole group than in the olanzapine group (n=223, 1 RCT, MD −17.43 CI −27.21 to −7.65).
1.5.5 Extrapyramidal side-effects (EPS)
There was no significant difference in various EPS such as akathisia (n=317, 1 RCT, RR 1.86 CI 0.64 to 5.42), extrapyramidal symptoms (n=317, 1 RCT, RR 1.07 CI 0.65 to 1.77) and parkinsonism (n=317, 1 RCT, RR 0.92 CI 0.50 to 1.71).
1.5.6 Glucose - change from baseline in mg/dl
There was no significant difference (n=317, 1 RCT, MD −2.00 CI −10.48 to 6.48).
1.5.7 Prolactin-associated side-effects - abnormally high prolactin value
Fewer participants in the aripiprazole group had increased prolactin levels (n=317, 1 RCT, RR 0.27 CI 0.12 to 0.60, NNT 8 CI 5 to 17).
-
1.5.8
Sedation
There was a significant difference favouring aripiprazole (n=317, 1 RCT, RR 0.33 CI 0.18 to 0.62, NNT 7 CI 4 to 13).
-
1.5.9
Weight gain of 7% or more of total body weight
There was a significant difference in favour of aripiprazole (n=317, 1 RCT, RR 0.37 CI 0.24 to 0.58, NNT 4 CI 3 to 8).
-
1.5.10
Weight gain - change from baseline in kg
There was a significant difference in weight change favouring aripiprazole (n=90, 1 RCT, MD −5.60 CI −9.05 to −2.15).
-
1.6
Publication bias
Due to the small number of included studies a funnel plot analysis was not performed.
-
1.7
Investigation for heterogeneity and sensitivity analysis
The reasons given for the preplanned sensitivity analyses did not apply and therefore they were not undertaken.
-
2.
Comparison 2. ARIPIPRAZOLE versus RISPERIDONE
Two studies provided data for this comparison.
-
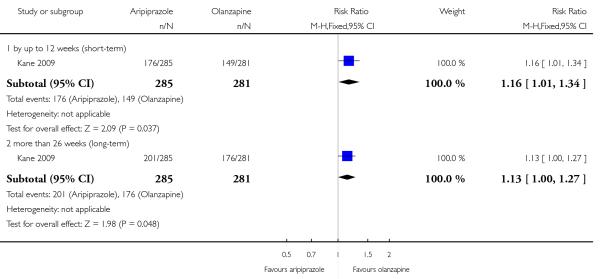
2.1
No significant response: as defined by the original studies
There was no significant difference (n= 384, 2 RCTs, RR 1.14 CI 0.81 to 1.60).
-
2.2
Leaving the studies early
There was no significant difference between aripiprazole and risperidone in leaving the study early due to any reason (n=384, 2 RCTs, RR 0.94 CI 0.71 to 1.26), due to adverse events (n=384, 2 RCTs, RR 1.26 CI 0.62 to 2.56) or due to inefficacy of treatment (n=384, 2 RCTs, RR 1.13 CI 0.52 to 2.46).
-
2.3
Global state
-
2.3.1
Global state: no clinically important change
There was no significant difference (n= 384, 2 RCTs, RR 1.14 CI 0.81 to 1.60).
-
2.4
Mental state
-
2.4.1
General mental state: PANSS total score
There was no significant difference (n=372, 2 RCTs, MD 1.50 CI −2.96 to 5.96).
-
2.4.2
Positive symptoms: PANSS positive subscore
There was no significant difference (n=372, 2 RCTs, MD 1.24 CI −0.26 to 2.74).
-
2.4.3
Negative symptoms: PANSS negative subscore
There was no significant difference (n=372, 2 RCTs, MD −0.45 CI −1.78 to 0.87).
-
2.5
Adverse effects
-
2.5.1
At least one adverse effect
There was no significant difference (n=384, 2 RCTs, RR 0.98 CI 0.92 to 1.05).
-
2.5.2
Cardiac effects - participants with QTc prolongation
There was no significant difference (n=301, 1 RCT, RR 0.07 CI 0.00 to 1.35).
-
2.5.3
Cardiac effects - mean change of the QTc interval from baseline in ms
There was a significant difference favouring aripiprazole (n=383, 2 RCTs, MD −7.19 CI −12.19 to −2.19).
-
2.5.4
Cholesterol - change from baseline in mg/dl
There was a statistically significant difference favouring aripiprazole (n=83, 1 RCT, MD −22.30 CI −39.69 to −4.91).
-
2.5.5
Extrapyramidal side-effects (EPS)
Extrapyramidal side-effects reported as akathisia (n=301, 1 RCT, RR 1.40 CI 0.80 to 2.45), extrapyramidal symptoms (n=384, 2 RCTs, RR 0.84 CI 0.49 to 1.47), parkinsonism (n=301, 1 RCT, RR 7.39 CI 0.43 to 128.08) and use of antiparkinson medication (n=83, 1 RCT, RR 0.59 Ci 0.32 to 1.12) were not significantly different. Dystonia (n=301, 1 RCT, RR 0.14 CI 0.05 to 0.41, NNT 8 CI 5 to 20) was less frequent in the aripiprazole group and tremor occurred less frequently in the risperidone group (n= 301, 1 RCT, RR 4.66 CI 1.11 to 19.59, NNH 14 CI 8 to 50).
2.5.6 Extrapyramidal side-effects - mean scores of rating scales
Dyskinesia (AIMS, n=383, 2 RCTs, MD −0.25, CI −1.24 to 0.75), akathisia (BAS, n=383, 2 RCTs, MD −0.11, CI −0.49 to 0.27) and general EPS (n=383, SAS, 2 RCTs, MD −0.75 CI −2.22 to 0.82) were not significantly different but the results were heterogeneous for unclear reasons.
-
2.5.7
Glucose - mean change from baseline in mg/dl
There was no significant difference (n=83, 1 RCT, MD 6.80 CI −6.10 to 19.70).
2.5.8 Prolactin abnormally high
Significantly fewer participants in the aripiprazole group had prolactin increase (n=301,1 RCT, RR 0.04 CI 0.02 to 0.08, NNH 1 CI not estimable), but there was no difference in dysmenorrhoea (n=91, 1 RCT, RR 3.17 CI 0.17 to 59.43).
-
2.5.9
Prolactin change from baseline in ng/ml
There was a significant difference favouring aripiprazole (n=383, 2 RCTs, MD −54.71 CI −60.06 to −49.36).
-
2.5.10
Weight gain of 7% or more of total body weight
There was no significant difference (n=384, 2 RCTs, RR 0.77 CI 0.33 to 1.82).
-
2.5.11
Weight gain - mean change from baseline in kg
There was no significant difference (n=383, 2 RCTs, MD −0.54 CI −1.24 to 0.15).
-
2.6
Publication bias
Due to the small number of included studies a funnel plot analysis was not performed.
-
2.7
Investigation for heterogeneity and sensitivity analysis
The reasons for the preplanned sensitivity analyses did not apply and they were therefore not performed.
DISCUSSION
There are several general limitations of the evidence. Aripiprazole has to date only been compared with olanzapine and risperidone. Randomised comparisons with other second generation antipsychotics are not available. The overall premature discontinuation rate of 38.5% was considerable clearly limiting the validity of the results. Long-term data (longer than 26 weeks) are not available. All trials were sponsored by aripiprazole’s manufacturer. We showed in a blinded analysis of abstracts that pharmaceutical companies emphasize the positive aspects of their compounds (Heres 2006). Systematic reviews can in part account for this effect by objectively summarizing the data, but they can not cope with omission of outcomes. Indeed, reporting was incomplete. All these factors are far from ideal for judging the comparative effects of aripiprazole and other second generation antipsychotic drugs in schizophrenia.
Summary of main results
1. General
Data from four trials and 1404 people are currently available. The overall number of participants leaving the studies early of 38.5% is considerable and long-term data are not available, calling the validity of the findings into question. The studies provided data on only two out of eight possible comparisons: aripiprazole versus olanzapine and aripiprazole versus risperidone. Aripiprazole was less efficacious than olanzapine in term of the general mental state (PANSS total score change from baseline, n=794, 2 RCTs, MD 4.96 CI 1.85 to 8.06), but aripiprazole was more tolerable in terms of cholesterol levels, weight gain, sedation and prolactin associated side-effects. Aripiprazole was similarly efficacious as risperidone (PANSS total score change from baseline, n=372, 2 RCTs, MD 1.50 CI −2.96 to 5.96). The adverse effects dystonia, QTc prolongation, prolactin increase and cholesterol increase were less frequent in the aripiprazole group. Fewer participants in the risperidone group developed tremor.
2. COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
2.1 Leaving the study early
The overall number of participants leaving the studies early was very high (40.1%) which is a threat for the validity of the findings. Nevertheless, there was no difference between aripiprazole and olanzapine suggesting that both compounds may be similarly acceptable for people with schizophrenia, at least within the confines of a trial.
2.2 Efficacy outcomes (global state, general and specific mental state)
There was no significant difference in the number of participants with a significant response, but only one study presented this outcome. According to two studies olanzapine improved the participants’ in general mental state more than aripiprazole. Although replications of this finding are necessary, olanzapine may be somewhat more efficacious than aripiprazole.
2.3 Adverse effects
Data on extrapyramidal symptoms, cardiac effects, effects on cholesterol, prolactin levels and associated side-effects, weight gain and sedation were available. Among those reported cholesterol increase, weight gain, sedation, and prolactin increase significantly favoured aripiprazole compared to olanzapine. This better tolerability of aripiprazole must be weighed with possibly lower efficacy compared to olanzapine.
3. COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
3.1 Leaving the study early
Again, the number of participants leaving the two studies early was considerable (34.4%), but there was no significant difference between both compounds suggesting that their acceptability is similar.
3.2 Efficacy outcomes (global state, general and specific mental state)
There were no statistically significant differences in global state, general mental state, positive and negative symptoms. The currently available small evidence base does thus not suggest a difference in efficacy between both compounds.
3.3 Adverse effects
Limited data were available on extrapyramidal side-effects, cardiac effects, cholesterol, glucose, prolactin increase, prolactin associated side-effects and weight gain. There was a significant benefit for aripiprazole in terms of dystonia, QTc abnormalities, prolactin increase and cholesterol levels, whereas tremor was less frequent in the risperidone group. Overall aripiprazole’s tolerability profile may be somewhat better than that of risperidone, but this conclusion is drawn from very limited data.
Overall completeness and applicability of evidence
Randomised evidence is available for only two out of eight possible comparisons of aripiprazole with other second generation antipsychotic drugs. Therefore, for most comparisons not a single study was identified and the evidence is very incomplete. In terms of applicability of the evidence we highlight that all of the included studies were ’efficacy’ studies. Large and simple, pragmatic, real-world effectiveness studies are not available, limiting external validity.
Quality of the evidence
All studies were randomised and double-blind, but details were rarely presented. Therefore it is unclear whether randomisation and blinding were really appropriately done. The high number of participants leaving the studies early of 38.5% overall questions the validity of the findings because the results of these people must be estimated by statistical modelling. Long-term studies are not available which is problematic in a chronic, often life-long disorder such as schizophrenia. Overall the review authors consider the overall quality of the evidence to be medium at best.
Potential biases in the review process
We are not aware of any obvious flaws in our review process.
Agreements and disagreements with other studies or reviews
An earlier Cochrane review compared aripiprazole with any other antipsychotic drugs (El-Sayeh 2006). The authors concluded that aripiprazole was not much different from other second generation antipsychotic drugs. However it is difficult to compare the previous review with our findings, because the authors combined olanzapine and risperidone as one group of atypical antipsychotic drugs. We do not think that such a pooling is appropriate, because second generation antipsychotics differ in many aspects.
AUTHORS’ CONCLUSIONS
Implications for practice
1. For people with schizophrenia
For people with schizophrenia it may be important to know that aripiprazole may be slightly less efficacious than olanzapine, but is less associated with adverse effects such as weight gain, cholesterol and prolactin increase and sedation. Its efficacy seems to be similar to that of risperidone, but certain movement disorders, cholesterol and prolactin increase may occur less frequently when taking aripiprazole. Nevertheless, people with schizophrenia should also know that the evidence is only based on a few trials. It may change once more studies have been published.
2. For clinicians
Clinicians should know that randomised, blinded evidence of the effects of aripiprazole compared to other second generation antipsychotic drugs is only available for olanzapine and risperidone. Even this evidence is based on only four randomised controlled trials and can therefore not be considered to be robust. More studies are needed to clarify the role of aripiprazole compared to other second generation antipsychotic drugs.
3. For managers/policy makers
Data that are relevant for policy makers such as service utilisation or functioning in society are unfortunately not available. We are thus unable to make any recommendations for decision makers.
Implications for research
1. General
Outcome reporting remains insufficient in antipsychotic drug trials. Strict adherence to the CONSORT statement (Moher 2001) would make such studies much more informative.
2. Specific
There is a lot of room for further randomised controlled trials comparing aripiprazole with other second generation antipsychotics. Comparisons with amisulpride, clozapine, quetiapine, sertindole, ziprasidone and zotepine are currently missing. We present a suggestion in Table 1.
Table 1. Suggested design of future study.
| Methods | Allocation: randomised - clearly described generation of sequence and concealment of allocation. Blindness: double - described and tested. Duration: six months minimum. |
| Participants | Diagnosis: schizophrenia (operational criteria). N=2700.* Age: any. Gender: both. History: any. |
| Interventions | 1. Aripiprazole: dose ~ 10-30 mg/day. N=300. 2. Amisulpride: dose ~ 400-800 mg/day. N=300. 3. Clozapine: dose ~ 300-800 mg/day. N=300. 4. Olanzapine: dose ~ 10-20 mg/day. N=300. 5. Quetiapine: dose ~300-800 mg/day. N=300. 6. Risperidone: dose ~ 4-8 mg/day. N=300. 7. Sertindole: dose ~ 12-24 mg/day. N=300. 8. Ziprasidone: dose ~ 120-160 mg/day. N=300. 9. Zotepine: dose ~ 100-300 mg/day. N=300. |
| Outcomes | Leaving study early (any reason, adverse events, inefficacy). Service outcomes: hospitalised, time in hospital, attending out patient clinics. Global impression: CGI**, relapse. Mental state: PANSS. Adverse events: UKU. Employment, family satisfaction, patient satisfaction. |
power calculation suggested 300/group would allow good chance of showing a 10% difference between groups for primary outcome.
Primary outcome
PLAIN LANGUAGE SUMMARY.
Aripiprazole versus other atypical antipsychotics for schizophrenia
This review compares aripiprazole with other second generation antipsychotic drugs. There were only four studies on two comparisons - aripiprazole compared to olanzapine and aripiprazole compared to risperidone. On the basis of very limited data aripiprazole was not as effective as olanzapine but as good as risperidone. Aripiprazole was associated with less weight gain, cholesterol increase, sedation and prolactin related effects than olanzapine. Compared to risperidone aripiprazole produced fewer dystonias, cardiac arrhythmias, prolactin and cholesterol increase.
ACKNOWLEDGEMENTS
We would like to thank all members of the Cochrane Schizophrenia Group editorial base for their editorial assistance.
SOURCES OF SUPPORT
Internal sources
Psychiatrische Klinik, Klinikum rechts der Isar, TU München, Freistaat Bayern, Germany.
External sources
Bundesministerium für Bildung und Forschung, Nr FKZ: 01KG 0606,GZ:GF-GFKG01100506, Germany.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: random, no further details. Blindness: double, no further details. Duration: 52 weeks (first six weeks observed). Design: parallel. Location: multicentre. |
|
| Participants | Diagnosis: (DSM-IV) acute schizophrenia, PANSS of 60 or more. N=703. Age: not reported. Gender: not reported. History: duration of illness not reported, age at onset not reported. Setting: in- and outpatient. |
|
| Interventions |
|
|
| Outcomes | Leaving the study early: any reason. Global state: CGI. Mental state: PANSS total score, depression MADRS. Quality of life/satisfaction with treatment: Quality of Life Enjoyment and Satisfaction Questionnaire, Medication adherence scale. Adverse effects: open interviews, EPS (SAS, AIMS, BAS), cardiac effects (ECG), weight gain (BMI) Unable to use - Adverse event outcomes (no data, interim report) |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Random, no further details. |
| Allocation concealment? | Unclear | No further details. |
| Blinding? Subjective outcomes |
Unclear | Double, no further details. Whether blinding was successful has not been examined, but both compounds differ quite substantially in side-effects. This can be a problem for blinding |
| Blinding? Objective outcomes |
Yes | Objective outcomes such as laboratory measures or death are unlikely to have been much affected by problems of blinding |
| Incomplete outcome data addressed? All outcomes |
No | Leaving the study early data within the first six weeks were 25% overall, but data on reason for dropout were not available. The last-observation-carried-forward method was used to account for people leaving the study early |
| Free of selective reporting? | No | Data for the predefined primary outcome are available but secondary outcome measures like 30% PANSS total reduction are missing in the six weeks interim report. Treatment emergent adverse events are hardly addressed in the interim report |
| Free of other bias? | No | The study was industry sponsored by the manufacturer of aripiprazole. Baseline data reporting is insufficient in terms of missing data on age, history of illness |
| Methods | Allocation: random, permuted block randomisation stratified by centre. Blindness: double, identical capsules. Duration: four weeks. Design: parallel. Location: multicentre. |
|
| Participants | Diagnosis: (DSM-IV) schizophrenia (n=80) or schizoaffective disorder (n=3), acute relapse. PANSS total score of 60 or more. N=83. Age: 18-65 years (mean aripiprazole=35.2 years, mean risperidone=35.1 years). Gender: 45 M, 38 F. History: duration of illness not reported, age at onset not reported. Setting: inpatient. |
|
| Interventions |
|
|
| Outcomes | Leaving the study early: any reason, adverse events, inefficacy. Global state: CGI. Mental state: PANSS total score, PANSS positive subscore, PANSS negative subscore. Adverse effects: at least one adverse effect, cardiac effects (QTc), extrapyramidal side-effects (use of antiparkinson medication, extrapyramidal symptoms, AIMS, BAS, SAS),cholesterol increase, glucose elevation, prolactin increase, weight |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Random, permuted block randomisation stratified by centre. |
| Allocation concealment? | Unclear | No further details. |
| Blinding? Subjective outcomes |
Unclear | Double, identical capsules. Whether blinding was successful has not been examined, but both compounds differ quite substantially in side-effects. This can be a problem for blinding |
| Blinding? Objective outcomes |
Yes | Objective outcomes such as laboratory measures or death are unlikely to have been much affected by problems of blinding |
| Incomplete outcome data addressed? All outcomes |
Unclear | Total number of drop-out was 25%. The last-observation-carried-forward method was used to account for people leaving the study early |
| Free of selective reporting? | No | Only adverse events with an incidence of at least 5% in any treatment group were reported, therefore important side effects may have been missed by this procedure |
| Free of other bias? | No | The study was industry sponsored by the manufacturer of aripiprazole |
| Methods | Allocation: random, no further details. Blindness: double, no further details. Duration: 26 weeks. Design: parallel. Location: multicentre. |
|
| Participants | Diagnosis: (DSM-IV) schizophrenia disorganised (n=17), paranoid (n=271), residual (n=3) or undifferentiated (n=26), in acute relapse and hospitalised. PANSS total score of 60 or more. N=317. Age: >17 years (mean=38.4 years). Gender: 229 M, 88 F. History: duration of illness not reported, age at first hospitalisation mean=24.50 years. Setting: originally inpatient. |
|
| Interventions |
|
|
| Outcomes | Leaving the study early: any reason, adverse events, inefficacy. Global state: CGI. Mental state: PANSS total score. Adverse effects: cardiac effects (ECG, QTc abnormalities in ms), extrapyramidal side-effects (akathisia, extrapyramidal symptoms, parkinsonism), laboratory (lipids, glucose (change from baseline in mg/dl, prolactin - increase of prolactin level above upper limit (males >20 ng/ml, females >27 ng/ml)), sedation, weight gain Unable to use - Adverse effects: use of antiparkinson medication (no data). |
|
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Random, no further details. |
| Allocation concealment? | Unclear | No further details. |
| Blinding? Subjective outcomes |
Unclear | Double, no further details. Whether blinding was successful has not been examined, but both compounds differ quite substantially in side-effects. This can be a problem for blinding |
| Blinding? Objective outcomes |
Yes | Objective outcomes such as laboratory measures or death are unlikely to have been much affected by lack of blinding |
| Incomplete outcome data addressed? All outcomes |
No | Quote: “Because of the high number of participants who discontinued the study (72%) results of analysis by time point are described on the observed case (OC) basis (except for primary outcome), as the last observation-carried-forward analysis would have included a large amount of data carried forward from patients who discontinued the study.” Due to the high number of participants leaving the study early, the validity is definitely limited |
| Free of selective reporting? | No | Although inclusion criteria required participants in acute relapse, no data on PANSS positive subscore were available. Data on use of antiparkinson medication were missing |
| Free of other bias? | No | The study was industry sponsored by the manufacturer of aripiprazole |
| Methods | Allocation: random, no further details. Blindness: double, identical capsules. Duration: four weeks. Design: parallel. Location: multicentre. |
|
| Participants | Diagnosis: (DSM-IV) schizophrenia (n=289) or schizoaffective disorder (n=115), hospitalised due to an acute relapse, response to previous antipsychotic treatment other than clozapine, PANSS of 60 or more. N=404. Age: 18-65 years (mean=38.9 years). Gender: 283 M, 121 F. History: duration of illness not reported, age at onset not reported. Setting: inpatient. |
|
| Interventions |
|
|
| Outcomes | Leaving the study early: any reason, adverse events, inefficacy. Global state: CGI. Mental state: PANSS total score, PANSS positive subscore, PANSS negative subscore. Adverse effects: At least one adverse effect, cardiac effects (ECG, QTc prolongation, QTc abnormalities in ms), extrapyramidal side-effects (akathisia, dystonia, parkinsonism, rigor, tremor, AIMS, BAS, SAS), prolactin-associated side-effects (dysmenorrhoea, increase of prolactin level above 23 ng/ml, change from baseline in ng/ml), sedation, weight gain |
|
| Notes | Note: There is a placebo group (n=103), which is not relevant for this review | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Random, no further details. |
| Allocation concealment? | Unclear | No further details. |
| Blinding? Subjective outcomes |
Unclear | Double, identical capsules. Whether blinding was successful has not been examined, but both compounds differ quite substantially in side-effects. This can be a problem for blinding |
| Blinding? Objective outcomes |
Yes | Objective outcomes such as laboratory measures or death are unlikely to have been much affected by lack of blinding |
| Incomplete outcome data addressed? All outcomes |
No | The overall dropout rate was 36.9%. The last-observation-carried-forward method was used to account for people leaving the study early |
| Free of selective reporting? | No | For efficacy outcomes there was no standard deviation or standard error indicated which had to be back calculated. Only adverse events with an incidence of more than 5% were reported. This procedure may have missed important adverse events |
| Free of other bias? | No | The study was industry sponsored by the manufacturer of aripiprazole. The study used a fixed dose regimen, where it is difficult to say which comparator doses may be appropriate |
Diagnostic tool
DSM III-R and DSM-IV - Diagnostic Statistical Manual version 3 Revised and version 4.
ICD 10 - The International Statistical Classification of Diseases and Related Health Problems.
Rating Scales:
Global rating scales:
CGI - Clinical Global Impressions.
CGI-S - Clinical Global Impression-Severity.
CGI-I - Clinical Global Impression-Improvement.
Mental state:
BPRS - Brief Psychiatric Rating Scale.
MADRS - Montgomery-Asberg Depression Rating Scale.
MMSE - Wiing Mini Mental State Examination.
PANSS - Positive and Negative Syndrome Scale.
SANS - Scale for the Assessment of Negative Symptoms.
SAPS- Scale for the Assessment of Positive Symptoms.
Side effects:
AIMS - Abnormal Involuntary Movement Scale.
BAS - Barnes Akathisia Scale.
ESRS - Extrapyramidal Syndrome Rating Scale.
SAS - Simpson-Angus Index - for neurological side effects.
UKU - Udvalg for kliniske ndersogelser Side Effect Rating Scale -side effect rating scale.
Quality of Life:
QLS - Quality of Life Scale.
SWN -Subjective Well-being List.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Beuzen 2005 | Allocation: randomised. Blindness: open-label. |
| Blonde 2004 | Allocation: randomised. Blindness: open-label. |
| Casey 2003 | Allocation: pooled analysis. |
| Chen 2005 | Allocation: not randomised |
| Cornblatt 2002 | Allocation: randomised. Blindness: open-label. |
| Dai 2005 | Allocation: randomised. Blindness: open-label. |
| Fan 2005 | Allocation: randomised. Blindness: open-label. |
| Han 2005 | Allocation: randomised. Blindness: open-label. |
| Kern 2006 | Allocation: randomised. Blindness: open-label. |
| Mai 2005 | Allocation: randomised. Blindness: open-label. |
| McQuade 2003 | Allocation: randomised. Blindness: open-label. |
| Newcomer 2006 | Allocation: pooled analysis. |
| Ray 2004 | Allocation: not randomised, cohort study. |
| Sanchez 2006 | Allocation: randomised. Blindness: open-label. |
| Swanson 2006 | Allocation: randomised. Blindness: open-label. |
| Tandon 2006 | Allocation: randomised. Blinding: open-label. |
| Wang 2005 | Allocation: randomised. Blindness: open-label. |
| Wlodzimiers 2006 | Allocation: randomised. Blindness: open-label. |
| Ye 2005 | Allocation: randomised. Blindness: open-label. |
| Zhi 2005 | Allocation: randomised. Blindness: open-label. |
| Zhu 2005 | Allocation: randomised. Blindness: open-label. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Trial 8047 F1D-MC-HGLB |
| Methods | Allocation: random, no further details. Blindness: double, no further details. Duration: 28 weeks. Design: parallel. Location: not reported. |
| Participants | Diagnosis: schizophrenia. Age 18-65 years. Gender: not reported. History: duration of illness not reported. Setting: in- and outpatient. |
| Interventions |
|
| Outcomes | Long-time effectiveness and tolerability. Global state: CGI, PG-I. General Mental State: PANSS. Depression: MADRS. Quality of life: SWN-S, SF-36. Cognitive functioning: MOS. Sexual functioning: GISF. Health resource utilisation and resource utilisation costs, hospitalisation time. Treatment-emergent adverse events: EPS (SAS, BAS, AIMS). Laboratory values. Vital signs. |
| Starting date | October 2003. |
| Contact information | Eli Lilly and Company. |
| Notes | |
| Trial name or title | Trial 8928 F1D-US-HGLS |
| Methods | Allocation: random, no further details Blindness: double, no further details. Duration: not reported. Design: parallel. Location: not reported. |
| Participants | Diagnosis: schizophrenia, schizoaffective disorder or schizophreniform disorder. Age 18-65 years. Gender: male/female. History: duration of illness not reported. Setting: originally inpatient. |
| Interventions |
|
| Outcomes | Efficacy, safety, side-effects. |
| Starting date | 2004-July. |
| Contact information | Eli Lilly and Company. |
| Notes | |
DATA AND ANALYSES
Comparison 1. COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 No clinically significant response (as defined by the original studies) | 2 | 1020 | Risk Ratio (M-H, Random, 95% CI) | 1.05 [0.95, 1.17] |
| 2 Leaving the study early | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 2.1 Any reason | 2 | 1020 | Risk Ratio (M-H, Random, 95% CI) | 1.15 [0.92, 1.45] |
| 2.2 Adverse events | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 1.27 [0.83, 1.95] |
| 2.3 Inefficacy | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 1.70 [0.91, 3.17] |
| 3 Global State: no clinically important change (as defined by the original studies) | 2 | 1020 | Risk Ratio (M-H, Random, 95% CI) | 1.05 [0.95, 1.17] |
| 3.1 Short term | 1 | 703 | Risk Ratio (M-H, Random, 95% CI) | 1.00 [0.81, 1.22] |
| 3.2 Medium term | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 1.08 [0.95, 1.22] |
| 4 General Mental State: PANSS total score (high=poor) | 2 | 794 | Mean Difference (IV, Random, 95% CI) | 4.96 [1.85, 8.06] |
| 4.1 Short term | 1 | 703 | Mean Difference (IV, Random, 95% CI) | 5.21 [1.91, 8.51] |
| 4.2 Medium term | 1 | 91 | Mean Difference (IV, Random, 95% CI) | 3.0 [−6.21, 12.21] |
| 5 Adverse effects: 1a. Cardiac effects - QTc prolongation | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 0.34 [0.07, 1.68] |
| 6 Adverse effects: 1b. Cardiac effects - QTc abnormalities - change from baseline in ms | 1 | 317 | Mean Difference (IV, Random, 95% CI) | −3.70 [−9.51, 2.11] |
| 7 Adverse effects: 2a. Cholesterol - abnormally high cholesterol value | 1 | 223 | Risk Ratio (M-H, Random, 95% CI) | 0.32 [0.19, 0.54] |
| 8 Adverse effects: 2b. Cholesterol - change from baseline in mg/dl | 1 | 223 | Mean Difference (IV, Random, 95% CI) | −17.43 [−27.21, −7. 65] |
| 9 Adverse effects: 3. Extrapyramidal side effects | 1 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 9.1 Akathisia | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 1.86 [0.64, 5.42] |
| 9.2 Extrapyramidal symptoms | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 1.07 [0.65, 1.77] |
| 9.3 Parkinsonism | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 0.92 [0.50, 1.71] |
| 10 Adverse effects: 4. Glucose - change from baseline in mg/dl | 1 | 317 | Mean Difference (IV, Random, 95% CI) | −2.0 [−10.48, 6.48] |
| 11 Adverse effects: 5. Prolactin-associated side-effects - abnormally high prolactin value | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 0.27 [0.12, 0.60] |
| 12 Adverse effects: 6. Sedation | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 0.33 [0.18, 0.62] |
| 13 Adverse effects: 7a. Weight gain of 7% or more of total body weight | 1 | 317 | Risk Ratio (M-H, Random, 95% CI) | 0.37 [0.24, 0.58] |
| 14 Adverse effects: 7b. Weight gain - change from baseline in kg | 1 | 90 | Mean Difference (IV, Random, 95% CI) | −5.60 [−9.05,−2.15] |
Comparison 2. COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 No clinically significant response (as defined by the original studies) | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 1.14 [0.81, 1.60] |
| 2 Leaving the study early | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 2.1 Any reason | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 0.94 [0.71, 1.26] |
| 2.2 Adverse events | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 1.26 [0.62, 2.56] |
| 2.3 Inefficacy | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 1.13 [0.52, 2.46] |
| 3 Global State: no clinically important change (as defined by the original studies) | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 3.1 Short term | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 1.14 [0.81, 1.60] |
| 4 Mental state: 1. General mental state: PANSS total score (high=poor) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Short term | 2 | 372 | Mean Difference (IV, Random, 95% CI) | 1.5 [−2.96, 5.96] |
| 5 Mental state: 2. Positive symptoms: PANSS positive subscore (high=poor) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Short term | 2 | 372 | Mean Difference (IV, Random, 95% CI) | 1.24 [−0.26, 2.74] |
| 6 Mental state: 3. Negative symptoms: PANSS negative subscore (high=poor) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Short term | 2 | 372 | Mean Difference (IV, Random, 95% CI) | −0.45 [−1.78, 0.87] |
| 7 Adverse effects: 1. At least one adverse effect | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 0.98 [0.92, 1.05] |
| 8 Adverse effects: 2a. Cardiac effects - QTc prolongation | 1 | 301 | Risk Ratio (M-H, Random, 95% CI) | 0.07 [0.00, 1.35] |
| 9 Adverse effects: 2b. Cardiac effects - QTc abnormalities - change from baseline in ms | 2 | 383 | Mean Difference (IV, Random, 95% CI) | −7.19 [−12.19, −2.19] |
| 10 Adverse effects: 3. Cholesterol - change from baseline in mg/dl | 1 | 83 | Mean Difference (IV, Random, 95% CI) | −22.3 [−39.69, −4.91] |
| 11 Adverse effects: 4a. Extrapyramidal side-effects | 2 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 11.1 Akathisia | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 0.64 [0.09, 4.72] |
| 11.2 Dystonia | 1 | 301 | Risk Ratio (M-H, Random, 95% CI) | 0.14 [0.05, 0.41] |
| 11.3 Extrapyramidal symptoms | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 0.84 [0.49, 1.47] |
| 11.4 Parkinsonism | 1 | 301 | Risk Ratio (M-H, Random, 95% CI) | 7.39 [0.43, 128.08] |
| 11.5 Tremor | 1 | 301 | Risk Ratio (M-H, Random, 95% CI) | 4.66 [1.11, 19.59] |
| 11.6 Use of antiparkinson medication | 1 | 83 | Risk Ratio (M-H, Random, 95% CI) | 0.59 [0.32, 1.12] |
| 12 Adverse effects: 4b. Extrapyramidal side-effects | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Abnormal involuntary movement: AIMS (high=poor) | 2 | 383 | Mean Difference (IV, Random, 95% CI) | −0.25 [−1.24, 0.75] |
| 12.2 Akathisia: Barnes Akathisia Scale (high=poor) | 2 | 383 | Mean Difference (IV, Random, 95% CI) | −0.11 [−0.49, 0.27] |
| 12.3 Extrapyramidal symptoms: Simpson-Angus Scale (high=poor) | 2 | 383 | Mean Difference (IV, Random, 95% CI) | −0.70 [−2.22, 0.82] |
| 13 Adverse effects: 5. Glucose - change from baseline in mg/dl | 1 | 83 | Mean Difference (IV, Random, 95% CI) | 6.8 [−6.10, 19.70] |
| 14 Adverse effects: 6a. Prolactin associated side effects | 1 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 14.1 Abnormally high prolactin value | 1 | 301 | Risk Ratio (M-H, Random, 95% CI) | 0.04 [0.02, 0.08] |
| 14.2 Dysmenorrhea | 1 | 91 | Risk Ratio (M-H, Random, 95% CI) | 3.17 [0.17, 59.43] |
| 15 Adverse effects: 6b. Prolactin - change from baseline in ng/ml | 2 | 383 | Mean Difference (IV, Random, 95% CI) | −54.71 [−60.06, −49. 36] |
| 16 Adverse effects: 7a. Weight gain of 7% or more of total body weight | 2 | 384 | Risk Ratio (M-H, Random, 95% CI) | 0.77 [0.33, 1.82] |
| 17 Adverse effects: 7b. Weight gain - change from baseline in kg | 2 | 383 | Mean Difference (IV, Random, 95% CI) | −0.54 [−1.24, 0.15] |
Analysis 1.1. Comparison 1. COMPARISON 1 ARIPIPRAZOLE versus OLANZAPINE, Outcome 1 No clinically significant response (as defined by the original studies).
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 1 Global state: 1. No clinically important change (as defined by the original studies)
 |
Analysis 1.2. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 2 Leaving the study early.
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 2 Global state: 2. Not responded (decline in PANSS of 30% or more)
 |
Analysis 1.3. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 3 Global State: no clinically important change (as defined by the original studies).
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 3 Global state: 3. Remission not achieved (as defined in the study)
 |
Analysis 1.4. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 4 General Mental State: PANSS total score (high=poor).
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 4 Global state: 4. Average change score (CGI-S, decline = best)
 |
Analysis 1.5. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 5 Adverse effects: 1a. CArdiac effects - QTc prolongation.
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 5 Global state: 5. Improvement (CGI-1, high = poor)
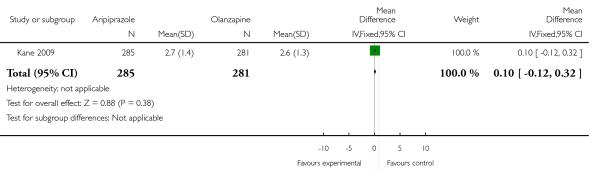 |
Analysis 1.6. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 6 Adverse effects: 1b. Cardiac effects - QTc abnormalities - change from baseline in ms).
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 6 Mental state: 1. General - average total score (PANSS, high = poor)
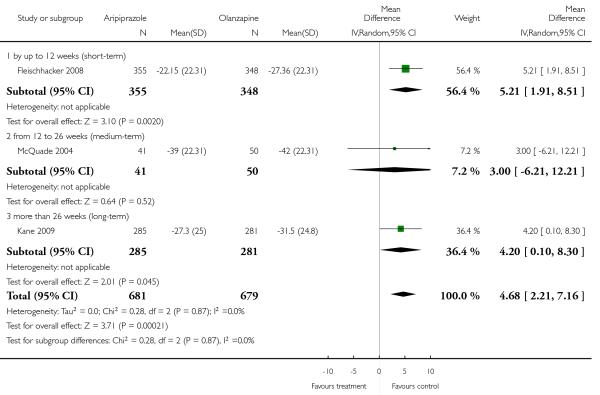 |
Analysis 1.7. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 7 Adverse effects: 2a. Cholesterol - abnormally high cholesterol value.
Review: Aripiprazole versus Other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 7 Mental state: 2. Specific - binary outcomes
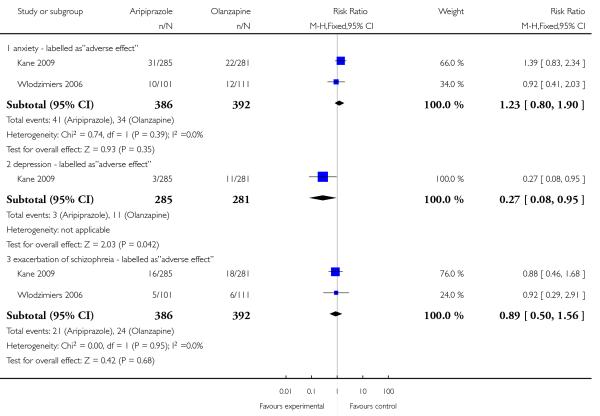 |
Analysis 1.8. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 8 Adverse effects: 2b. Cholesterol - change from baseline in mg/dl.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 8 Mental state: 3. Specific - average positive score (PANSS, high = poor)
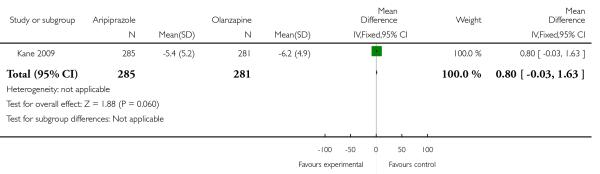 |
Analysis 1.9. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 9 Adverse effects: 3. Extrapyramidal side effects.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 9 Mental state: 4. Specific - average negative score (PANSS, high = poor)
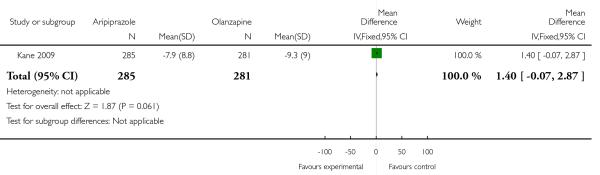 |
Analysis 1.10. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 10 Adverse effects: 4. Glucose - change from baseline in mg/dl.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 10 Leaving the study early
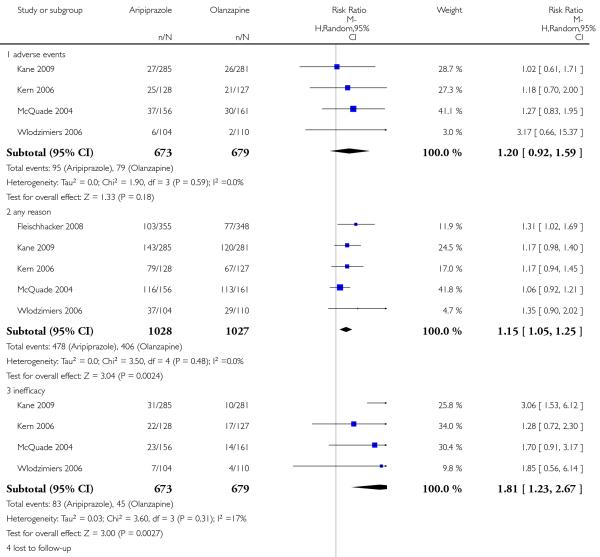 |
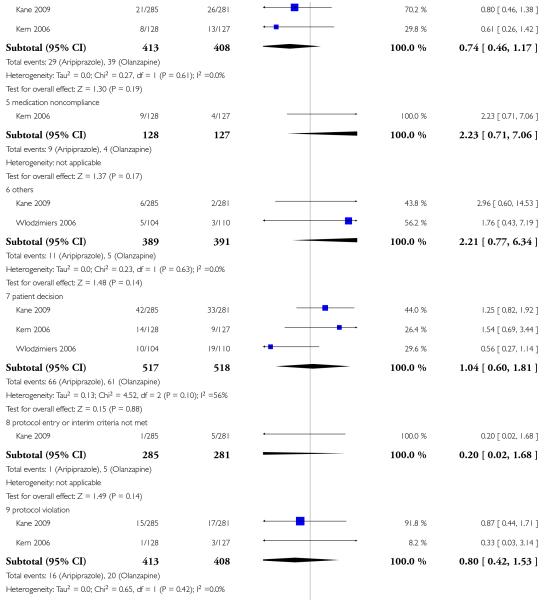 |
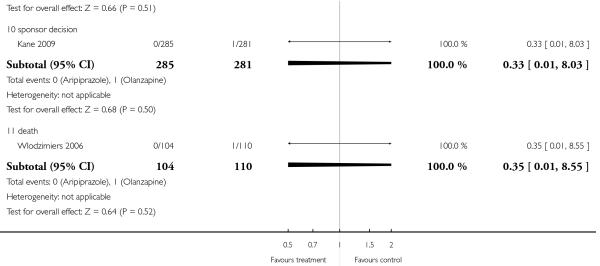 |
Analysis 1.11. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 11 Adverse effects: 5. Prolactin-associated side-effects - abnormally high prolactin value.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 11 Adverse effects: 1a. Cardiac - QTc prolongation
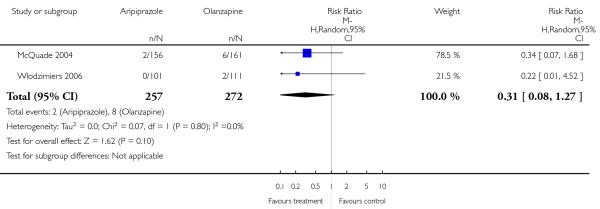 |
Analysis 1.12. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 12 Adverse effects: 6. Sedation.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 12 Adverse effects: 1b. Cardiac - QTc change from baseline (in ms)
 |
Analysis 1.13. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 13 Adverse effects: 7a. Weight gain of 7% or more of total body weight.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 13 Adverse effects: 2. Central nervous system
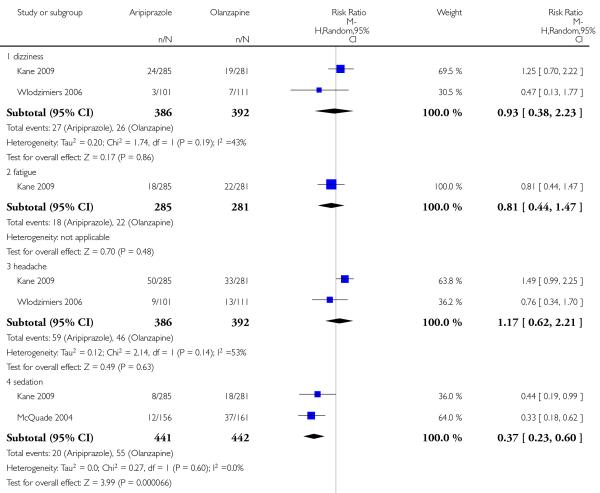 |
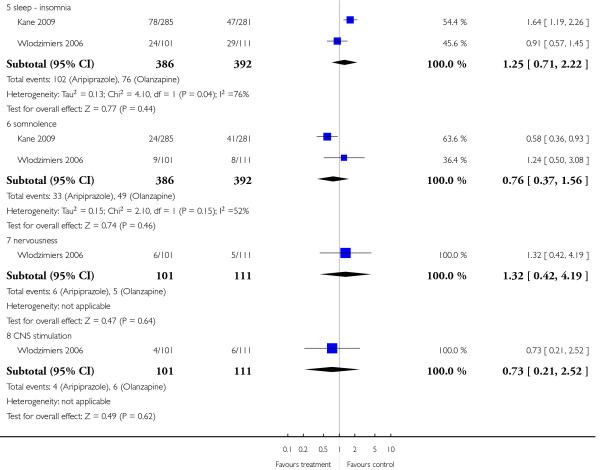 |
Analysis 1.14. Comparison 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE, Outcome 14 Adverse effects: 7b. Weight gain - change from baseline in kg.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 1 COMPARISON 1. ARIPIPRAZOLE versus OLANZAPINE
Outcome: 14 Adverse effects: 3a. Endocrine - Prolactin - abnormally high value
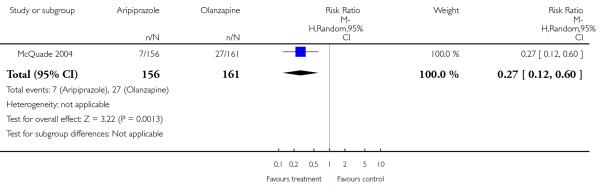 |
Analysis 2.1. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 1 No clinically significant response (as defined by the original studies).
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 1 Global state: Average improvement (BPRS, high = good)
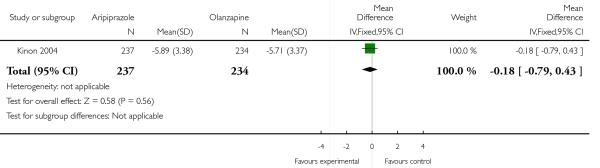 |
Analysis 2.2. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 2 Leaving the study early.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 2 Mental state: Specific - binary outcomes
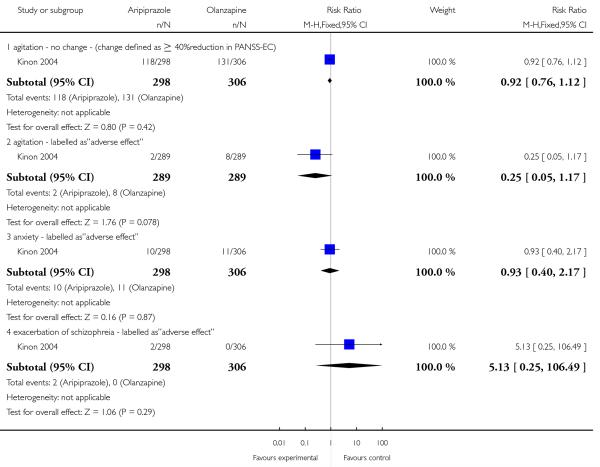 |
Analysis 2.3. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 3 Global State: no clinically important change (as defined by the original studies).
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 3 Leaving the study early
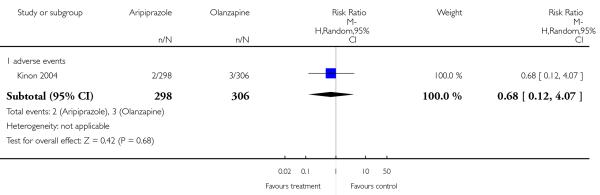 |
Analysis 2.4. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 4 Mental state: 1. General mental state: PANSS total score (high=poor).
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 4 Adverse effects: 1. Central nervous system
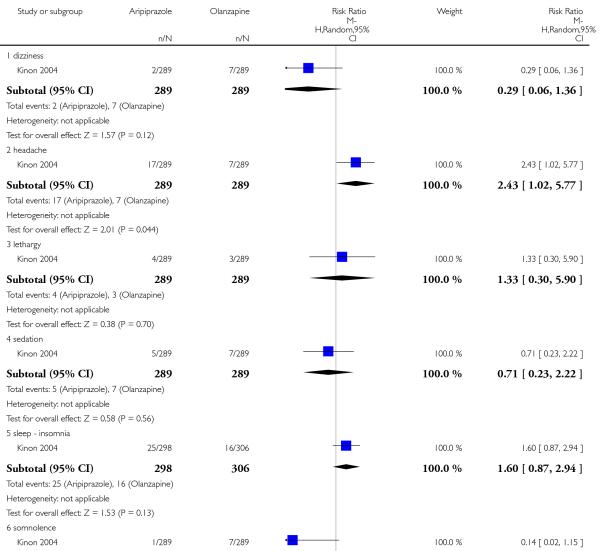 |
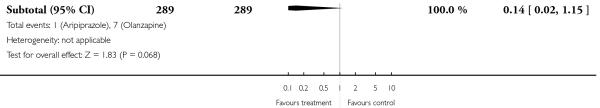 |
Analysis 2.5. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 5 Mental state: 2. Positive symptoms: PANSS positive subscore (high=poor).
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 5 Adverse effects: 2. Endocrine - Prolactin - average increase
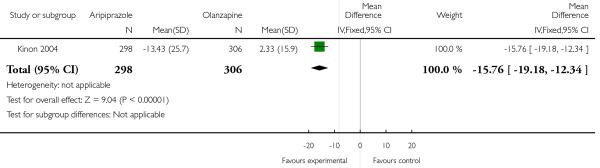 |
Analysis 2.6. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 6 Mental state: 3. Negative symptoms: PANSS negative subscore (high=poor).
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 6 Adverse effects: 3a. Extrapyramidal - various
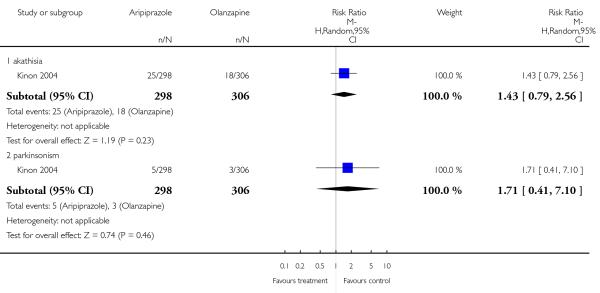 |
Analysis 2.7. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 7 Adverse effects: 1. At least one adverse effect.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 7 Adverse effects: 3b. Extrapyramidal - average score
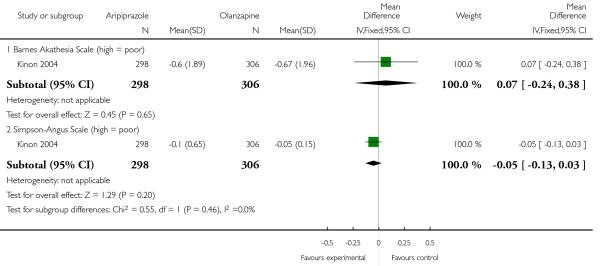 |
Analysis 2.8. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 8 Adverse effects: 2a. Cardiac effects - QTc prolongation.
Review: Aripiprazole versus other atypical antipsychotics for schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus OLANZAPINE (acutely agitated people - all data by 5 days)
Outcome: 8 Adverse effects: 4. Gastrointestinal
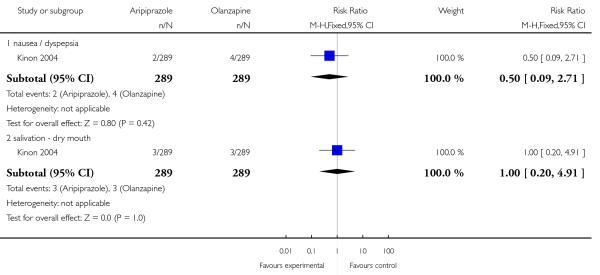 |
Analysis 2.9. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 9 Adverse effects: 2b. Cardiac effects - QTc abnormalities - change from baseline in ms.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 9 Adverse effects: 2b. Cardiac effects - QTc abnormalities - change from baseline in ms
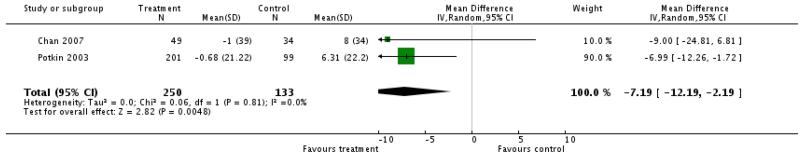 |
Analysis 2.10. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 10 Adverse effects: 3. Cholesterol - change from baseline in mg/dl.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 10 Adverse effects: 3. Cholesterol - change from baseline in mg/dl
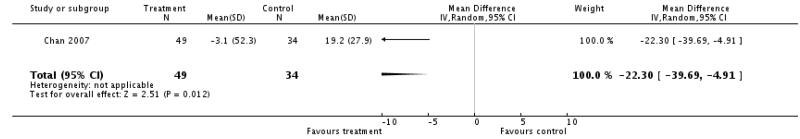 |
Analysis 2.11. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 11 Adverse effects: 4a. Extrapyramidal side-effects.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 11 Adverse effects: 4a. Extrapyramidal side-effects
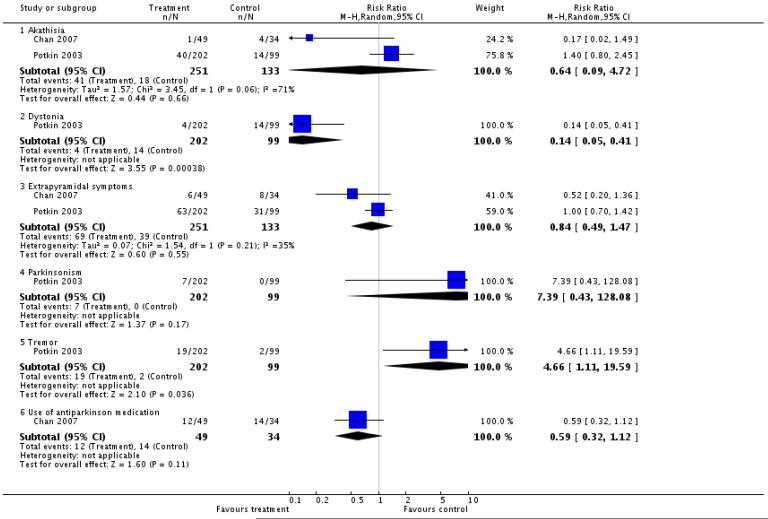 |
Analysis 2.12. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 12 Adverse effects: 4b. Extrapyramidal side-effects.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 12 Adverse effects: 4b. Extrapyramidal side-effects
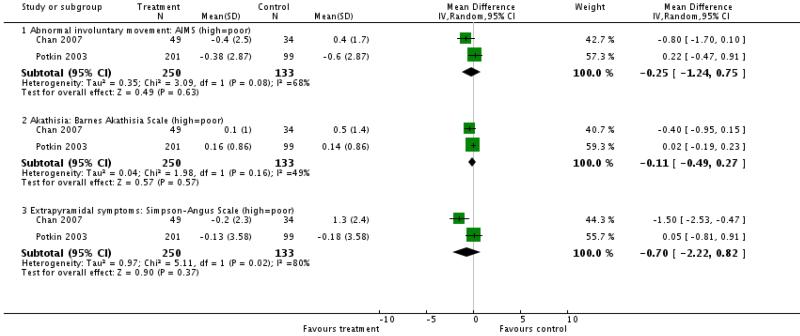 |
Analysis 2.13. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 13 Adverse effects: 5. Glucose - change from baseline in mg/dl.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 13 Adverse effects: 5. Glucose - change from baseline in mg/dl
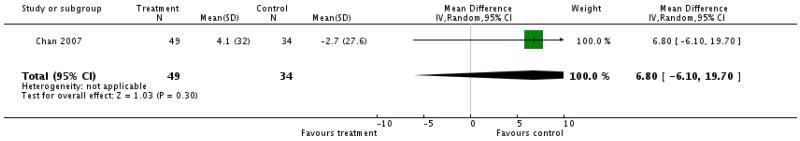 |
Analysis 2.14. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 14 Adverse effects: 6a. Prolactin associated side effects.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 14 Adverse effects: 6a. Prolactin associated side effects
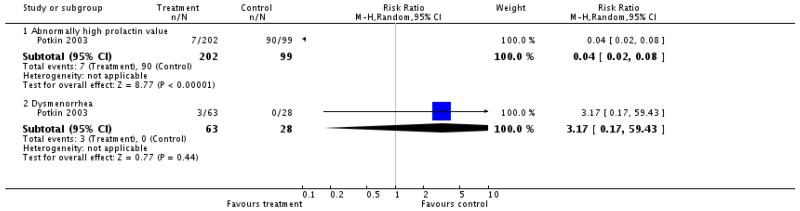 |
Analysis 2.15. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 15 Adverse effects: 6b. Prolactin - change from baseline in ng/ml.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 15 Adverse effects: 6b. Prolactin - change from baseline in ng/ml
 |
Analysis 2.16. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 16 Adverse effects: 7a. Weight gain of 7% or more of total body weight.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 16 Adverse effects: 7a. Weight gain of 7% or more of total body weight
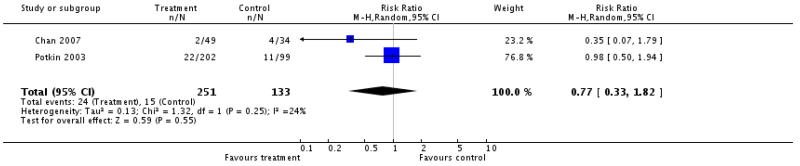 |
Analysis 2.17. Comparison 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE, Outcome 17 Adverse effects: 7b. Weight gain - change from baseline in kg.
Review: Aripiprazole versus other atypical antipsychotics of schizophrenia
Comparison: 2 COMPARISON 2. ARIPIPRAZOLE versus RISPERIDONE
Outcome: 17 Adverse effects: 7b. Weight gain - change from baseline in kg
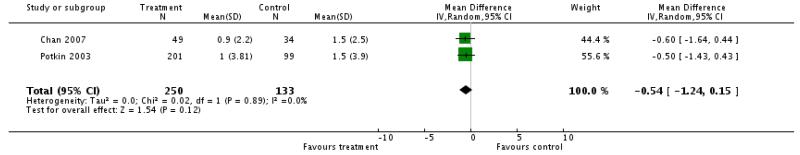 |
HISTORY
Protocol first published: Issue 3, 2007
Review first published: Issue 4, 2009
| Date | Event | Description |
|---|---|---|
| 4 September 2008 | Amended | Converted to new review format. |
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
The review was slightly adapted to new formatting and functions available in Review Manager 5, notably the risk of bias tables.
Appendix 1
We searched the Cochrane Schizophrenia Group Trials Register (August 2005) using the phrase:
[(aripiprazol* AND (amisulprid* OR clozapin* OR olanzapin* OR quetiapin* OR risperidon* OR sertindol* OR ziprasidon* OR zotepin*)) in title, abstract or index terms of REFERENCE].
Footnotes
DECLARATIONS OF INTEREST
Katja Komossa - none known.
Stefan Leucht - has received speaker/consultancy honoraria from SanofiAventis, BMS, EliLilly, Janssen, Lundbeck and Pfizer. He has received research support from SanofiAventis and EliLilly.
Werner Kissling - has received speaker/consultancy honoraria from SanofiAventis, BMS, Lilly, Janssen, Lundbeck, Bayer and Pfizer.
Christine Rummel - has received lecture honoraria and travel grants to attend scientific meetings from AstraZeneca, Janssen-Cilag, Eli Lilly and Pfizer.
Heike Hunger - none known.
Franziska Schmid - none known.
Sandra Schwarz - none known.
Hany George El-Sayeh - none known.
References to studies included in this review
- BMS CN 138003 2005 {published data only} .BMS A multicenter, double-blind, randomized, comparative study of aripiprazole and olanzapine in the treatment of patients with acute schizophrenia. Clinical Study Report. 2005:CN138003. [Google Scholar]; *
- Chan 2007 {published data only} .Chan HY, Lin WW, Lin SK, Hwang TJ, Su TP, Chiang SC, Hwu HG. Efficacy and safety of aripiprazole in the acute treatment of schizophrenia in chinese patients with risperidone as an active control: A randomized trial. Journal of Clinical Psychiatry. 2007;68(1):29–36. doi: 10.4088/jcp.v68n0104. [DOI] [PubMed] [Google Scholar]; *
- Hwang TJ, Chan HY, Lin WW, Lin SK, Hwu HG, Cheng MY, Forbes RA. Aripiprazole versus risperidone in the treatment of acutely relapsed patients with schizophrenia in Taiwan: a randomized controlled trial. Journal of the European College of Neuropsychopharmacology. 2005;14(Suppl 3):S497. [Google Scholar]
- McQuade 2004 {published data only} .McQuade RD, Stock E, Marcus R, Jody D, Gharbia NA, Vanveggel S, Carson WH. A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. Journal of Clinical Psychiatry. 2004;65(Suppl 18) [PubMed] [Google Scholar]
- Potkin 2003 {published data only} .Potkin SG, Kujawa M, Carson WH, Saha AR, Ali M, Ingenito G. Aripiprazole and risperidone versus placebo in schizophrenia and schizoaffective disorder. Schizophrenia Research. 2003;60:300. doi: 10.1001/archpsyc.60.7.681. [DOI] [PubMed] [Google Scholar]
- Potkin SG, Saha AR, Kujawa MJ, Carson WH, Ali M, Stock E, Stringfellow J, Ingenito G, Marder SR. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Archives of General Psychiatry. 2003;60(7):681–90. doi: 10.1001/archpsyc.60.7.681. [DOI] [PubMed] [Google Scholar]; *
References to studies excluded from this review
- Beuzen 2005 {published data only} .Beuzen JN, Pans M, Modell S, Hagens P, McQuade R, Iwamoto T, Carson W. Naturalistic study of aripiprazole treatment; Proceedings of the XIII World Congress of Psychiatry; Cairo, Egypt. Cairo: World Congress of Psychiatry. 2005 10-15th Sept; 2005. [Google Scholar]
- Blonde 2004 {published data only} .Blonde L, Ray S, Corey-Lisle PK, Cislo PR, L’Italien G. The risk of new-onset type 2 diabetes and coronary heart disease in chronic schizophrenic patients treated with aripiprazole and olanzapine. Journal of the European College of Neuropsychopharmacology. 2004;14(Suppl 3):S275. [Google Scholar]
- Casey 2003 {published data only} .Casey D, L’Italien G, Waldeck R, Cislo P, Carson W. Metabolic syndrome comparison between olanzapine, aripiprazole, and placebo; Proceedings of the 156th Annual Meeting of the American Psychiatric Association; San Francisco, California, USA. San Francisco: American Psychiatric Association. 2003 May 17-22; 2003. [Google Scholar]
- Chen 2005 {published data only} .Chen J-D, Zhao J-P, Li L-H, Guo X-F, Zhai J-G, Wang C-Y, Xie S-P, Gao C-G, Ding Y,, Chen Y-G. A multicentre, randomised and double-blind controlled trial of aripiprazole in treatment of schizophrenia. Chinese Journal of New Drugs and Clinical Remedies. 2005;11:845–8. [Google Scholar]
- Cornblatt 2002 {published data only} .Cornblatt B, Kern RS, Carson WH, Stock E, Ali M, Ingenito G, Green MF. Neurocognitive effects of aripiprazole versus olanzapine in patients with stable psychosis. Schizophrenia Research. 2002;53(3 Suppl 1):27. [Google Scholar]
- Dai 2005 {published data only} .Dai J-P, Zhao Z-H, Liu G-X. Comparison of efficacy and safety of aripiprazole and quetiapine in the treatment of schizophrenia. Chinese Journal of Behavioral Medical Science. 2005;14(8):712–4. [Google Scholar]
- Fan 2005 {published data only} .Fan W-l, Yu C-M,, Wen J-S. Efficacy analysis of aripiprazole and clozapine in the treatment of schizophrenia. Journal of North Sichuan Medical College. 2005;20(4):377–9. [Google Scholar]
- Han 2005 {published data only} .Han P, Zhang Y-H, Zhang Y-Q. A controlled study of schizophrenia treated with aripiprazole and clozapine. Clinical Journal of Rehabilitation in Theory and Practice. 2005;11(10):853–4. [Google Scholar]
- Kern 2006 {published data only} .Kern RS, Green MF, Cornblatt BA, Owen JR, McQuade RD, Carson WH, Ali M, Marcus R. The neurocognitive effects of aripiprazole: an open-label comparison with olanzapine. Psychopharmacology. 2006;187(3):312–20. doi: 10.1007/s00213-006-0428-x. [DOI] [PubMed] [Google Scholar]
- Mai 2005 {published data only} .Mai G, Cai G-H, Huang J-M. Comparative study on the effect of aripiprazole and risperidone on schizophrenia. Chinese Journal of Rehabilitation. 2005;20(3):184–5. [Google Scholar]
- McQuade 2003 {published data only} .McQuade R, Jody D, Kane J, Carson W, Kujawa M, Stringfellow J, Marcus R, Sanchez R, Meltzer HY. Efficacy and safety of aripiprazole versus perphenazine in treatment-resistant schizophrenia. Journal of the European College of Neuropsychopharmacology. 2003;13(4):S326. [Google Scholar]
- Newcomer 2006 {published data only} .Newcomer JW, L’Italien G, Vester-Blokland, McQuade RD, Carson WH, Marcus RN. Improvement of non-hdl cholesterol levels among patients randomized to aripiprazole versus olanzapine; Proceedings of the 159th Annual Meeting of the American Psychiatric Association; Toronto, Canada. Toronto: American Psychiatric Association. 2006 May 20-25; 2006. [Google Scholar]
- Ray 2004 {published data only} .Ray S, Corey-Lisle PK, Cislo PR, L’Italien G, Weiden P. An economic evaluation of aripiprazole compared to olanzapine based on metabolic side-effect profile. Journal of the European College of Neuropsychopharmacology. 2004;14(Suppl 3):S279. [Google Scholar]
- Sanchez 2006 {published data only} .Sanchez R, Kostic D, Stock E, Torbeyns AF, Kerselaers W, Nyilas M, McQuade R, Carson WH, Marcus RN. Aripiprazole vs olanzapine in patients with acutely relapsing or chronic, stable schizophrenia: a 52-week open-label extension study; Proceedings of the 13th Biennial Winter Workshop on Schizophrenia Research; Davos, Switzerland. 2006 Feb 4-10; 2006. [Google Scholar]
- Swanson 2006 {published data only} .Swanson JW, Swartz MS, Van Dorn RA. Effectiveness of atypical antipsychotics for substance abuse in schizophrenia patients; Proceedings of the 159th Annual Meeting of the American Psychiatric Association; Toronto, Canada. Toronto: American Psychiatric Association. 2006 May 20-25; 2006. [Google Scholar]
- Tandon 2006 {published data only} .Tandon R, Marcus RN, Stock EG, Riera LC, Kostic D, Pans M, McQuade RD, Nyilas M, Iwamoto T, Crandall DT. A prospective, multicenter, randomized, parallel-group, open-label study of aripiprazole in the management of patients with schizophrenia or schizoaffective disorder in general psychiatric practice: Broad Effectiveness Trial With Aripiprazole (BETA) Schizophrenia Research. 2006;84(1):77–89. doi: 10.1016/j.schres.2005.12.857. [DOI] [PubMed] [Google Scholar]
- Wang 2005 {published data only} .Wang R, Liu Y, Ning Z. A controlled study of aripiprazole vs clozapine in the treatment of first-episode schizophrenia. Journal of Clinical Psychosomatic. 2005;11(4):301–2. [Google Scholar]
- Wlodzimiers 2006 {published data only} .Chrzanowski WK, Marcus RN, Torbeyns A, Nyilas M, McQuade RD. Effectiveness of long-term aripiprazole therapy in patients with acutely relapsing or chronic, stable schizophrenia: a 52-week, open-label comparison with olanzapine. Psychopharmacology. 2006;189:259–266. doi: 10.1007/s00213-006-0564-3. [DOI] [PubMed] [Google Scholar]
- Ye 2005 {published data only} .Ye X-R, Xia X-l. A comparative study between aripiprazole and risperidone in treatment of first-onset schizophrenia. Wutaishan Hospital in Yangzhou City. 2005;6:616–8. [Google Scholar]
- Zhi 2005 {published data only} .Zhi S-L. Comparison study of aripiprazole and risperidone on schizophrenia. Modern Journal of Integrated Traditional Chinese and Western Medicine. 2005;14(21):2787–8. [Google Scholar]
- Zhu 2005 {published data only} .Zhu P-J, Cheng Z-E, Zhang J, Zhu P-L, Zhan X-M. Clinical study of therapeutic effects of aripiprazole in treatment of patients with schizophrenia. China. 2005;10:1194–6. [Google Scholar]
References to ongoing studies
- Eli Lilly 2003 {published data only} .Eli Lilly, Company . Study of olanzapine vs aripiprazole in the treatment of schizophrenia. Eli Lilly and Company Clinical Trial Registry; 2003. [Google Scholar]
- Eli Lilly 2004 {published data only} .Eli Lilly, Company . Olanzapine versus aripiprazole in the treatment of acutely ill patients with schizophrenia. Eli Lilly and Company Clinical Trial Registry; 2004. [Google Scholar]
Additional references
- Altman 1996 .Altman DG, Bland JM. Detecting skewness from summary information. BMJ. 1996;313:1200. doi: 10.1136/bmj.313.7066.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA 2004 .American Psychiatric Association . American Journal of Psychiatry. 2nd. American Psychiatric Publishing, Inc; 2004. Practice guidelines for the treatment of patients with schizophrenia; pp. 1–114. [Google Scholar]
- Arnt 1998 .Arnt J, Skarsfeldt T. Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology. 1998;18:63–101. doi: 10.1016/S0893-133X(97)00112-7. [DOI] [PubMed] [Google Scholar]
- Barnes 1989 .Barnes TR. A rating scale for drug-induced akathisia. British Journal of Psychiatry. 1989;154:672–6. doi: 10.1192/bjp.154.5.672. [DOI] [PubMed] [Google Scholar]
- Bland 1997 .Bland JM, Kerry SM. Statistics notes. Trials randomised in clusters. BMJ. 1997;315:600. doi: 10.1136/bmj.315.7108.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boissel 1999 .Boissel JP, Cucherat M, Li W, Chatellier G, Gueyffier F, Buyse M, Boutitie F, Nony P, Haugh M, Mignot G. The problem of therapeutic efficacy indices. 3. Comparison of the indices and their use. Therapie. 1999;54(4):405–11. [PubMed] [Google Scholar]
- Carpenter 1994 .Carpenter WT, Jr, Buchanan RW. Schizophrenia. New England Journal of Medicine. 1994;330:681–90. doi: 10.1056/NEJM199403103301006. [DOI] [PubMed] [Google Scholar]
- Deeks 2000 .Deeks J. Issues in the selection for meta-analyses of binary data; Proceeding of the 8th International Cochrane Colloquium; Cape Town, South Africa. Cape Town: Cochrane Collaboration. 2000 Oct 25-28th; 2000. [Google Scholar]
- Divine 1992 .Divine GW, Brown JT, Frazer LM. The unit of analysis error in studies about physicians’ patient care behavior. Journal of General Internal Medicine. 1992;7:623–9. doi: 10.1007/BF02599201. [DOI] [PubMed] [Google Scholar]
- Donner 2002 .Donner A, Klar N. Issues in the meta-analysis of cluster randomized trials. Statistics in Medicine. 2002;21:2971–80. doi: 10.1002/sim.1301. [DOI] [PubMed] [Google Scholar]
- Duggan 2005 .Duggan L, Dardennes R, El-Dosoky A, Fenton M, Indran S, Rathbone J. Olanzapine for schizophrenia. Cochrane Database of Systematic Reviews. 2005;(2) doi: 10.1002/14651858.CD001359.pub2. DOI: 10.1002/14651858.CD001359.pub2. [DOI] [PubMed] [Google Scholar]
- Egger 1997 .Egger M, Davey-Smith G, Schneider M, Minder CSO. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;13:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbourne 2002 .Elbourne D, Altman DG, Higgins JPT, Curtina F, Worthingtond HV, Vaile A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology. 2002;31(1):140–9. doi: 10.1093/ije/31.1.140. [DOI] [PubMed] [Google Scholar]
- FDA 2002 .U.S. Federal Drug Administration CDER [accessed 18 August 2006];Abilify (aripiprazole) tablets, medical review. 2002 www.fda.gov/cder/foi/nda/2002/21-436.Abilify.htm.
- Furukawa 2006 .Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology. 2006;59:7–10. doi: 10.1016/j.jclinepi.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Gaebel 2006 .Gaebel W, Falkai P, Weinmann S, Wobrock T. Treatment guidelines for schizophrenia [Behandlungsleitlinie Schizophrenie] Steinkopf: 2006. [Google Scholar]
- Gulliford 1999 .Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community-based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology. 1999;149:876–83. doi: 10.1093/oxfordjournals.aje.a009904. [DOI] [PubMed] [Google Scholar]
- Guy 1976 .Guy U. ECDEU assessment manual for psychopharmacology. National Institute of Mental Health; 1976. ECDEU assessment manual for psychopharmacology. [Google Scholar]
- Heres 2006 .Heres S, Davis J, Maino K, Jetzinger E, Kissling W, Leucht S. Why olanzapine beats risperidone, risperidone beats quetiapine, and quetiapine beats olanzapine. American Journal of Psychiatry. 2006;163:185–94. doi: 10.1176/appi.ajp.163.2.185. [DOI] [PubMed] [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions 5.0.1 [updated September 2008] The Cochrane Collaboration; John Wiley and Sons Ltd; Chichester, UK: 2008. [Google Scholar]
- Jones 2006 .Jones PB, Barnes TRE, Davies L, Dunn G, Lloyd H, Hayhurst KP, Murray RM, Markwick A, Lewis SW. Randomized controlled trial of the effect on quality of life. Archives of General Psychiatry. 2006;63:1079–6. doi: 10.1001/archpsyc.63.10.1079. [DOI] [PubMed] [Google Scholar]
- Kane 1988 .Kane JM, Honigfeld G, Singer J, Meltzer H, Clozaril Collaborative Study Group Clozapine for the treatment of treatment-resistant schizophrenia: a double-blind comparison with chlorpromazine. Archives of General Psychiatry. 1988;45:789–96. doi: 10.1001/archpsyc.1988.01800330013001. [DOI] [PubMed] [Google Scholar]
- Kane 1993 .Kane JM. Treatment programme and long term outcome in chronic schizophrenia. Acta Psychiatrica Scandinavica. 1993;46:585–93. doi: 10.1111/j.1600-0447.1990.tb05309.x. [DOI] [PubMed] [Google Scholar]
- Kay 1986 .Kay SR, Opler LA, Fiszbein A. Positive and negative syndrome scale (PANSS) manual. Multi-Health Systems; North Tonawanda (NY): 1986. [Google Scholar]
- Leucht 2005a .Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. Clinical implications of Brief Psychiatric Rating Scale Scores. British Journal of Psychiatry. 2005;187:366–71. doi: 10.1192/bjp.187.4.366. [DOI] [PubMed] [Google Scholar]
- Leucht 2005b .Leucht S, Kane JM, Kissling W, Hamann J, Etschel E, Engel R. What does the PANSS mean? Schizophrenia Research. 2005;79:231–8. doi: 10.1016/j.schres.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Leucht 2008 .Leucht S, Komossa K, Rummel-Kluge C, Corves C, Hunger H, Schmid F, Asenjo Lobos C, Schwarz S, Davis JM. A meta-analysis of head-to-head comparisons of second- generation antipsychotics in the treatment of schizophrenia. American Journal of Psychiatry. 2009;166(2):152–63. doi: 10.1176/appi.ajp.2008.08030368. DOI: 10.1176/appi.ajp.2008.08030368. [DOI] [PubMed] [Google Scholar]
- Lieberman 2005 .Liebermann JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Keefe RSE, Davis SM. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine. 2005;353:1209–23. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- Marshall 2000 .Marshall M, Lockwood A, Adams C, Bradley C, Joy C, Fenton M. Unpublished rating scales - a major source of bias in randomised controlled trials of treatments for schizophrenia? British Journal of Psychiatry. 2000;176:249–52. doi: 10.1192/bjp.176.3.249. [DOI] [PubMed] [Google Scholar]
- Marvaha 2004 .Marvaha S, Johnson S. Schizophrenia and employment - a review. Social Psychiatry and Psychiatric Epidemiology. 2004;39:337–49. doi: 10.1007/s00127-004-0762-4. [DOI] [PubMed] [Google Scholar]
- Moher 2001 .Moher D, Schulz KF, Altman D. The CONSORT Statement: Revised Recommendations for Improving the Quality of Reports of Parallel-Group Randomized Trials. JAMA. 2001;285:1987–1. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- Möller 2000 .Möller HJ. New assessment of atypical antipsychotics [Aktuelle Bewertung neuer/atypischer Neuroleptika] Nervenarzt. 2000;71:329–44. doi: 10.1007/s001150050567. [DOI] [PubMed] [Google Scholar]
- Overall 1962 .Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports. 1962;10:799–812. [Google Scholar]
- Rivas-Vasquez 2003 .Rivas-Vasquez RA. Aripiprazole: A novel antipsychotic with dopamine stabilising properties. Professional Psychology: Research and Practice. 2003;34(1):108–11. [Google Scholar]
- Rust 1989 .Rust J, Golombok S. Modern Psychometrics. Routledge; London: 1989. [Google Scholar]
- Simpson 1970 .Simpson EN, Angus JWF. A rating scale for extrapyramidal side-effects. Acta Psychiatrica Scandinavica Supplementum. 1970;212:11–9. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]
- Tandon 2008 .Tandon R, Keshavan MS, Nasralllah HA. Schizophrenia, “Just the Facts” What we know in 2008. 2. Epidemiology and etiology. Schizophrenia research. 2008;102:1–18. doi: 10.1016/j.schres.2008.04.011. [DOI] [PubMed] [Google Scholar]
- Tsuang 1978 .Tsuang MT. Suicide in schizophrenics, manics, depressives, and surgical controls: a comparison with general population suicide mortality. Archives of General Psychiatry. 1978;35:153–55. doi: 10.1001/archpsyc.1978.01770260031002. [DOI] [PubMed] [Google Scholar]
- Ukoumunne 1999 .Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review. Health Technology Assessment. 1999;3(5):iii–92. [PubMed] [Google Scholar]
- WHO 2001 .WHO . The World Health Report 2001 - Mental Health: New Understanding, New Hope. World Health Organisation; Geneva: 2001. [Google Scholar]
- Xia 2007 .Xia J, Adams CE, Bhagat N, Bhagat V, Bhoopathi P, El-Sayeh H, Pinfold V, Takriti Y. The Leeds Outcomes Stakeholders Survey (LOSS) Study; Proceedings of the 15th Cochrane Colloquium; Sao Paulo, 23-27 October 2007; 2007. [Google Scholar]
References to other published versions of this review
- El-Sayeh 2006 .El-Sayeh HG, Morganti C. Aripiprazole for schizophrenia. Cochrane Database of Systematic Reviews. 2006;(2) doi: 10.1002/14651858.CD004578.pub3. DOI: 10.1002/14651858.CD004578.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- * Indicates the major publication for the study