Abstract
Introduction
We sought to compare characteristics of emergency medical services-treated out-of-hospital cardiac arrests resulting from suspected drug overdose with non-overdose cases and test the relationship between suspected overdose and survival to hospital discharge.
Methods
Data from emergency medical services-treated, non-traumatic out-of-hospital cardiac arrests from 2006–2008 and late 2009–2011 were obtained from 4 EMS agencies in the Pittsburgh, Pennsylvania metropolitan area. Case definition for suspected drug overdose was naloxone administration, indication on the patient care report and/or indication by a review of hospital records. Resuscitation parameters included chest compression fraction, rate, and depth and the administration of resuscitation drugs. Demographic and outcome variables compared by suspected overdose status included age, sex, and survival to hospital discharge.
Results
From 2,342 treated out-of-hospital cardiac arrests, 180 were suspected overdose cases (7.7%) and were compared to 2,162 non-overdose cases. Suspected overdose cases were significantly younger (45 vs. 65, p < 0.001), less likely to be to be witnessed by a bystander (29% vs. 41%, p < 0.005), and had a higher rate of survival to hospital discharge (19% vs. 12%, p = 0.014) than non-overdoses. Suspected overdose cases had a higher overall chest compression fraction (0.69 vs. 0.67, p = 0.018) and higher probability of adrenaline, sodium bicarbonate, and atropine administration (p < 0.001). Suspected overdose status was predictive of survival to hospital discharge when controlling for other variables (p < 0.001).
Conclusion
Patients with suspected overdose-related out-of-hospital cardiac arrest were younger, received different resuscitative care, and survived more often than non-overdose cases.
Introduction
Out-of-hospital cardiac arrest (OHCA) from suspected drug overdose (OD) is a significant public health issue in the United States and abroad. Published incidence rates vary geographically between 2.7 and 29.4% of all non-traumatic, emergency medical services (EMS)-treated OHCA.1–5 In the developed world, the most common etiology of non-traumatic OHCA is cardiac, primarily myocardial infarction due to atherosclerosis and coronary artery disease.6 Suspected OD-OHCA then presents a unique subset of cardiac arrests that results from the misuse of a variety of illicit, legal, and/or prescribed agents. While the literature is limited on the topic, the most common agents implicated in suspected OD-OHCA are opioids, cocaine, and alcohol,3 with opioids accounting for 75.2% of all drug-related deaths in 2010 in the United States.7 Opioids are also the most often implicated substance in cases of polypharmaceutical overdose.7 Other agents commonly abused include antidepressants, antiepileptics, antihistamines, barbiturates, and benzodiazepines. 3, 7
Despite clear differences in the etiology of suspected OD and non-OD OHCA, the International Liaison Committee on Resuscitation guidelines published in 2010 do not specify different treatments for suspected OD-OHCA patients during resuscitation, and state that there is no evidence promoting the intra-arrest administration of the opioid antagonist naloxone.8 Data are required to determine if alternative management strategies might be beneficial for suspected OD-OHCA.
In the present study, we describe the characteristics of the subset of OHCA cases attributed to suspected OD in a distinct geographic area. Second, we compared patient and treatment characteristics between suspected OD-OHCA and non-OD OHCA cases. Lastly, we investigated the relationship between suspected OD status and survival to hospital discharge, adjusting for other characteristics.
Methods
We obtained approval from the Institutional Review Board of the University of Pittsburgh prior to commencing this retrospective study. Case data from EMS-treated OHCAs occurring from 2006 to late 2008 and late 2009 to 2011 were obtained from the Pittsburgh site of the Resuscitation Outcomes Consortium (ROC), a multicenter clinical research network with ten sites across the United States and Canada. The catchment area for this study included a population of approximately 940,000 people, with an annual incidence of OHCA estimated to be 105.1 per 100,000, as of 2008. This region encompassed the service areas of 4 EMS agencies, all of which provided advanced life support (ALS) care.9 We excluded cases identified as “dead on arrival” (DOA) by EMS, as well as cases from a period spanning late 2008 to late 2009, during the multisite ROC PRIMED clinical trial for which the data were embargoed.10
Available patient and treatment data sources included prehospital patient care reports (PCRs) written by paramedics, electronic ECG files from defibrillator monitors, and select data elements from hospital records. Cardiopulmonary resuscitation (CPR) process parameters including chest compression fraction (CCF), rate, and depth were abstracted from defibrillator downloads by data abstractors for up to the first 20 minutes of each resuscitation event. Frequency of shock delivery, as well as the administration of resuscitation drugs including adrenaline (epinephrine), sodium bicarbonate, lidocaine, atropine, and amiodarone were abstracted from PCRs and defibrillator downloads. Drug administration for ALS drugs was coded as “administered ever” for each drug.
We identified suspected OD cases by three criteria: 1) the administration of at least one dose of naloxone during prehospital resuscitation, and 2) paramedic indication of suspected overdose in the PCR. In the latter case, explicit mention of drugs intended for medicinal or recreational use, drug paraphernalia, or witness accounts of drug use leading to cardiac arrest were necessary for establishing suspected OD status. Pesticides and other environmental poisonings were not included in the suspected OD subset. Specific agents contributing to OHCA were not identifiable in all cases, however for consistency with existing research,1 we attempted to limit the study to illicit and prescription drugs and excluded cases that only mentioned alcohol. The third method of suspected OD identification utilized in-hospital confirmation of drug use provided by data abstractors using select data elements from hospital records. ROC data abstractors could indicate the “suspected cause of arrest” was drug overdose (prescribed or illicit) after review of in-hospital records, however, this data point was only available for OHCA patients who were admitted to the hospital; this did not yield any information pertaining to patients whose resuscitation was terminated in the out-of-hospital setting. Furthermore, demographic, condition and circumstantial variables included age, sex, EMS- and bystander-witnessed status, return of spontaneous circulation, survival to hospital admission, and survival to hospital discharge.
Clinical characteristics were compared between suspected OD and non-OD cases with two-tailed comparison of proportions and t-tests. The effect of suspected OD status and time on CCF was tested with a simple generalized estimating equations (GEE) model. To assess the independent relationship between suspected OD status and survival while adjusting for demographic and clinical covariates, a multivariable logistic regression model was constructed, and adjusted odds ratios (OR) were reported. Suspected OD status was forced into the logistic model as a key variable, and other variables were included in the model if they had significant univariate relationships with suspected OD status. All statistical calculations were conducted with Stata 11 (StataCorp, College Station, TX) using an alpha level of 0.05.
Results
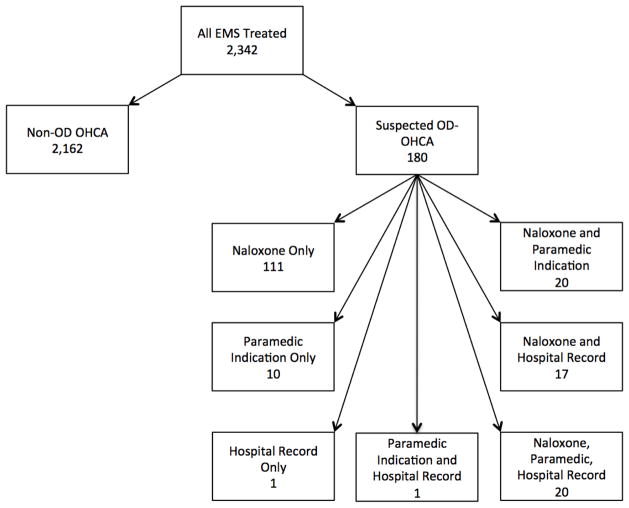
For the period between 2006 and 2011, a total of 2,342 OHCA cases were available for inclusion in this study. Of these, 180 cases (7.7%) were identified as suspected OD-OHCA, leaving 2,162 non-OD OHCA. Naloxone administration was the identifying factor for 168 (93.3%) cases. Fifty-one cases (28.3%) included in our suspected OD group had an indication of suspected OD by paramedics in the out-of-hospital setting; 39 (21.7%) were confirmed as an overdose in the hospital (see Figure 1). There was extremely limited data on DOA cases and we could not confidently compare such cases to those in our study cohort.
Figure 1.
Consort Diagram
Abbreviations:
EMS: Emergency Medical Services; Non-OD OHCA: Non-Overdose Out-of-Hospital Cardiac Arrest; OD-OHCA: Suspected Overdose Out-of-Hospital Cardiac Arrest
Table 1 summarizes characteristics and outcomes by suspected OD status. Suspected OD-OHCA cases were younger and less-often bystander witnessed than non-OD cases. Sex and EMS witnessed status did not differ by suspected OD status. Suspected OD cases were more likely than non-ODs to survive to hospital discharge (OR: 1.82, 95% CI: 1.12–2.94, p = 0.015).
Table 1.
Characteristics and Outcomes Stratified by OD Status
| Variable | Overall | OD | Non-OD | p-value |
|---|---|---|---|---|
| Age, y mean (SD) | 63.6 (19.6) | 44.8 (14.7) | 65.1 (19.1) | < 0.001 |
| Sex, % (SE) | 60.0 (1.0) | 65.4 (3.6) | 59.6 (1.1) | 0.130 |
| EMS Witnessed, % (SE) | 9.3 (0.7) | 6.7 (1.9) | 9.5 (0.7) | 0.207 |
| Bystander Witnessed, % (SE) | 51.3 (1.2) | 48.4 (4.4) | 51.5 (1.2) | 0.508 |
| Bystander Resuscitation, % (SE) | 51.3 (1.2) | 48.4 (4.4) | 51.5 (1.2) | 0.508 |
| Public Location, % (SE) | 14.1 (0.7) | 17.2 (2.8) | 13.8 (0.7) | 0.210 |
| VF/VT First OHCA ECG Rhythm, % (SE) | 13.1 (0.7) | 15.6 (2.7) | 12.9 (0.7) | 0.302 |
| ROSC, % (SE) | 26.3 (0.9) | 25.0 (3.2) | 26.4 (0.9) | 0.689 |
| Survival to Hospital Admission, % (SE) | 31.3 (1.3) | 34.2 (4.4) | 31.1 (1.3) | 0.486 |
| Survival to Hospital Discharge, % (SE) | 11.9 (0.8) | 18.9 (3.5) | 11.3 (0.8) | 0.014 |
Abbreviations:
ECG: Electrocardiogram; EMS: Emergency Medical Service; Non-OD: Non-Overdose Out-of-Hospital Cardiac Arrest; OD: Suspected Overdose Out-of-Hospital Cardiac Arrest; OHCA: Out-of-Hospital Cardiac Arrest; SD: Standard Deviation; SE: Standard Error; VF/VT: Ventricular Fibrillation/Ventricular Tachycardia
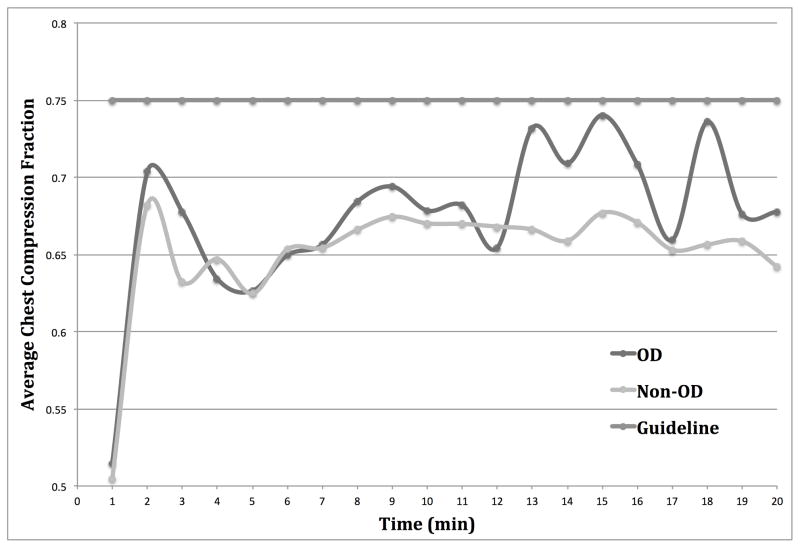
Table 2 summarizes CPR process parameters. Overall chest compression rate and depths did not differ between suspected OD and non-OD cases. Average CCF was higher in the suspected OD-OHCA group than the non-OD group across the entire available resuscitation period. However CCF did not differ between groups over the first 5 minutes of the resuscitation. The time course of CCF is shown in Figure 2. A GEE model of CCF containing time and suspected OD status yielded no significant relationship between suspected OD status and CCF across the available resuscitation period, but did show a significant relationship between time and CCF (p <0.001).
Table 2.
CPR Process Parameters Stratified by OD Status
| Process Measures | Overall | OD | Non-OD | p-value |
|---|---|---|---|---|
| Compression Rate, Case Average (SD) | 78.7 (29.8) | 80.7 (27.8) | 78.5 (30.1) | 0.402 |
| Compression Rate, First 5 min Average (SD) | 79.3 (35.3) | 80.5 (35.1) | 79.2 (35.3) | 0.661 |
| Compression Depth, Case Average (SD) | 37.4 (8.4) | 38.6 (7.6) | 37.3 (8,5) | 0.109 |
| Compression Depth, First 5 min Average (SD) | 37.9 (9.7) | 38.6 (8.5) | 37.8 (9.8) | 0.430 |
| Compression Fraction, Case Average (SD) | 67.1 (12.3) | 69.4 (10.6) | 66.9 (12.5) | 0.018 |
| Compression Fraction, First 5 min Average (SD) | 65.4 (14.1) | 65.8 (13.1) | 65.3 (14.2) | 0.666 |
Abbreviations:
Non-OD: Non-Overdose Out-of-Hospital Cardiac Arrest; OD: Suspected Overdose Out-of-Hospital Cardiac Arrest; SD: Standard Deviation
Figure 2.
Average Chest Compression Fraction of OD vs. Non-OD Cases
Abbreviations:
Non-OD: Non-Overdose Out-of-Hospital Cardiac Arrest; OD: Suspected Overdose Out-of-Hospital Cardiac Arrest
Table 3 summarizes the rates of key drug interventions, as well as rescue shocks, by suspected OD status. The proportion of cases shocked and average number of shocks delivered did not differ between groups. However, rates of administration of adrenaline, bicarbonate, and atropine were higher in suspected OD cases than non-ODs.
Table 3.
Prehospital Interventions Stratified by OD Status
| Intervention | Overall | OD | Non-OD | p-value |
|---|---|---|---|---|
| Shocked, % (SE) | 31.6 (1.0) | 33.9 (3.5) | 31.4 (1.0) | 0.483 |
| Shocks, mean (SD) | 3.1 (2.5) | 2.9 (2.6) | 3.1 (2.5) | 0.505 |
| Adrenaline, % (SE) | 75.4 (0.9) | 85.6 (2.6) | 74.3 (1.1) | <0.001 |
| Bicarbonate, % (SE) | 31.1 (1.1) | 52.2 (3.7) | 28.8 (1.1) | <0.001 |
| Amiodarone, % (SE) | 5.4 (0.5) | 5.6 (1.7) | 5.4 (0.5) | 0.925 |
| Atropine, % (SE) | 68.7 (1.1) | 78.9 (3.0) | 67.6 (1.1) | <0.005 |
Abbreviations:
Non-OD: Non-Overdose Out-of-Hospital Cardiac Arrest; OD: Suspected Overdose Out-of-Hospital Cardiac Arrest; SD: Standard Deviation; SE: Standard Error
A multivariable logistic regression model testing for an independent effect of suspected OD status on survival to hospital discharge is shown in Table 4. Suspected OD status and an initial VF/VT rhythm had independent direct associations with survival. Adrenaline and atropine administration had independent inverse associations with survival.
Table 4.
Multivariable Logistic Regression with Outcomes of Survival to Hospital Discharge
| Predictor | OR | 95% CI | p-value |
|---|---|---|---|
| OD Status | 3.89 | 1.91–7.92 | <0.001 |
| Age | 1.00 | 0.99–1.01 | 0.785 |
| Sex | 0.67 | 0.42–1.07 | 0.095 |
| Bystander Witnessed | 1.09 | 0.78–1.53 | 0.600 |
| VF/VT First OHCA ECG Rhythm | 6.87 | 4.10–11.49 | <0.001 |
| Adrenaline | 0.18 | 0.09–0.34 | <0.001 |
| Bicarbonate | 0.83 | 0.45–1.55 | 0.565 |
| Atropine | 0.19 | 0.10–0.36 | <0.001 |
Abbreviations:
95% CI: 95% Confidence Interval; ECG: Electrocardiogram; Non-OD: Non-Overdose Out-of-Hospital Cardiac Arrest; OD: Suspected Overdose Out-of-Hospital Cardiac Arrest; OHCA: Out-of-Hospital Cardiac Arrest; OR: Odds Ratio; VF/VT: Ventricular Fibrillation/Ventricular Tachycardia
Discussion
We found that the treatment and outcomes of suspected OD-OHCA differed from those of non-OD OHCA. Demographic features of non-OD and suspected OD cases also differed. We cannot determine whether these differences in treatment or demographic characteristics are related to differences in outcome. However, these data do support the idea that treatment might be tailored to the cause of cardiac arrest in an effort to improve outcomes.
We encountered difficulty in ascertainment of suspected OD as a cause of cardiac arrest. Autopsy is rare for OHCA, and only a fraction cases reach the hospital for further testing. We relied on either naloxone administration or clear description of circumstantial evidence in the PCR to identify a suspected OD. Clear descriptions are also rare, and most (93%) of the cases were identified by naloxone administration. Naloxone during cardiac arrest is not part of any regional protocol, and all of these administrations are deviations from recommended practice. There may be other cases in which paramedics suspected OD, but did not deviate from protocol to administer naloxone. Therefore, it is impossible to be certain whether the actual number of OD cases is larger or smaller than the reported number. However, the use of naloxone as a proxy indicator of suspected OD has been supported in the literature.11 It is likely that the current sample of 180 suspected OD-OHCA cases represent situations in which the treating paramedics at least considered opioid OD as a possible contributor to arrest.
Our study provides additional description of suspected OD-OHCA, a historically understudied phenomenon. A handful of previous studies provide characteristics of patients presenting with this general etiology of OHCA. When compared to the 2004 study by Paredes et al., our suspected OD-OHCA patients are similar in age, and relatively close in distribution of sexes (73% male versus 65%). Our suspected OD-OHCA cases had higher survival (19%), compared to both Paredes’s study (12.9%) and a 2007 study by Hess et al. (11.1%). Additionally, Paredes found a much lower rate of first EMS assessed OHCA ECG rhythm of VF/VT (6%),3 compared to our own estimate of 15.6%.
This study had several limitations. First, embargoed data resulting in exclusion of a large period of time from the middle of the study period limits a complete epidemiological estimate of the incidence of suspected OD-OHCA. However, there is no reason to suspect that cases differed during that period were not comparable to the cases captured during the period of our study. Second, when ascertaining suspected OD status, we relied on a combination of evidence of naloxone administration and PCR review for indication of direct or circumstantial evidence indicating suspected OD, which has the limitations discussed above. Moreover, we are unable to state with certainty which drugs were utilized in each arrest, as this information is difficult to obtain in the prehospital environment, and toxicology reports were not available for our review. Lastly, as this was a retrospective study utilizing records and a surveillance network that were conceived before our study, we were unable to capture several data points that might have clarified our findings, including toxicological screens of patients post-resuscitation or at autopsy.
Conclusion
Suspected OD-OHCA patients were treated differently than non-OD cases to a limited degree, particularly in drug administration and one parameter of CPR. Suspected OD-OHCAs were also more likely to be younger and to survive to hospital discharge than non-OD OHCAs.
Acknowledgments
This work was supported by significant research grants from the National Heart, Lung, and Blood Institute (5U01 HL077863 and 1R21HL104440-01A1) awarded to Dr. Callaway and Dr. Menegazzi, respectively. All analyses were performed in Pittsburgh, PA.
The authors would like to thank the Pittsburgh EMS and Mutual Aid Ambulance Service of the Pittsburgh area for their participation this study.
Footnotes
Presented as a poster at the American Heart Association’s Resuscitation Science Symposium in November 2012 in Los Angeles, California and at the National Association of EMS Physicians Annual Meeting in January 2013 in Bonita Springs, Florida.
Conflicts of Interest
The authors report no conflicts of interest regarding this work.
Conflict of Interest Statement:
The authors, Allison C. Koller, David D. Salcido, Clifton W. Callaway, and James J. Menegazzi, report no conflicts of interest regarding this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boyd JJ, Kuisma MJ, Alaspää AO, Vuori E, Repo JV, Randell TT. Outcome after heroin overdose and cardiopulmonary resuscitation. Acta Anaesthesiol Scand. 2006 Oct;50(9):1120–4. doi: 10.1111/j.1399-6576.2006.01142.x. [DOI] [PubMed] [Google Scholar]
- 2.Hess EP, Campbell RL, White RD. Epidemiology, trends, and outcome of out-of-hospital cardiac arrest of non-cardiac origin. Resuscitation. 2007 Feb;72(2):200–6. doi: 10.1016/j.resuscitation.2006.06.040. [DOI] [PubMed] [Google Scholar]
- 3.Paredes VL, Rea TD, Eisenberg MS, Cobb LA, Copass MK, Cagle A, Martin TG. Out-of-hospital care of critical drug overdoses involving cardiac arrest. Acad Emerg Med. 2004 Jan;11(1):71–4. doi: 10.1197/j.aem.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Deasy C, Bray JE, Smith K, Harriss LR, Bernard SA, Cameron P. Out-of-hospital cardiac arrests in young adults in Melbourne, Australia. Resuscitation. 2011 Jul;82(7):830–4. doi: 10.1016/j.resuscitation.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Safranek DJ, Eisenberg MS, Larsen MP. The epidemiology of cardiac arrest in young adults. Ann Emerg Med. 1992 Sep;21(9):1102–6. doi: 10.1016/s0196-0644(05)80651-1. [DOI] [PubMed] [Google Scholar]
- 6.Engdahl J, Holmberg M, Karlson BW, Luepker R, Herlitz J. The epidemiology of out-of-hospital ‘sudden’ cardiac arrest. Resuscitation. 2002 Mar;52(3):235–45. doi: 10.1016/s0300-9572(01)00464-6. [DOI] [PubMed] [Google Scholar]
- 7.Jones CM, Mack KA, Paulozzi LJ. Pharmaceutical overdose deaths, United States, 2010. JAMA. 2013 Feb 20;309(7):657–9. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 8.Soar J, Perkins GD, Abbas G, Alfonzo A, Barelli A, Bierens JJ, Brugger H, Deakin CD, Dunning J, Georgiou M, Handley AJ, Lockey DJ, Paal P, Sandroni C, Thies KC, Zideman DA, Nolan JP. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010 Oct;81(10):1400–33. doi: 10.1016/j.resuscitation.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, Rea T, Lowe R, Brown T, Dreyer J, Davis D, Idris A, Stiell I Resuscitation Outcomes Consortium Investigators. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008 Sep 24;300(12):1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aufderheide TP, Nichol G, Rea TD, Brown SP, Leroux BG, Pepe PE, Kudenchuk PJ, Christenson J, Daya MR, Dorian P, Callaway CW, Idris AH, Andrusiek D, Stephens SW, Hostler D, Davis DP, Dunford JV, Pirrallo RG, Stiell IG, Clement CM, Craig A, Van Ottingham L, Schmidt TA, Wang HE, Weisfeldt ML, Ornato JP, Sopko G Resuscitation Outcomes Consortium (ROC) Investigators. A trial of an impedance threshold device in out-of-hospital cardiac arrest. N Engl J Med. 2011 Sep 1;365(9):798–806. doi: 10.1056/NEJMoa1010821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Knowlton A, Weir BW, Hazzard F, Olsen Y, McWilliams J, Fields J, Gaasch W. EMS runs for suspected opioid overdose: implications for surveillance and prevention. Prehosp Emerg Care. 2013 Jul-Sep;17(3):317–29. doi: 10.3109/10903127.2013.792888. [DOI] [PMC free article] [PubMed] [Google Scholar]