Abstract
Objectives
To describe methodology used to diagnose delirium in research studies evaluating delirium detection tools.
Design
A survey addressing reference rater methodology for delirium diagnosis, including rater characteristics, sources of patient information and diagnostic process.
Setting
Survey completed via web or telephone interview according to respondent preference.
Participants
Authors of 39 studies included in 3 recent systematic reviews of delirium detection instruments in hospitalized patients.
Results
Authors from 85% (n=33) of the 39 eligible studies responded to the survey. The median (Interquartile Range [IQR]) number of raters per study was 2.5 (2–3); 79% were physicians. The raters’ median (IQR) duration of clinical experience with delirium diagnosis was 7 (4–10) years, with 5% having no prior clinical experience. Inter-rater reliability was evaluated in 70% of studies. Cognitive tests and delirium detection tools were used in the delirium reference rating process in 61% (n=21) and 45% (n=15) of studies, respectively, with 33% (n=11) using both and 27% (n=9) using neither. When patients were too drowsy or declined to participate in delirium evaluation, 70% (n=23) of studies used all available information for delirium diagnosis, while 15% excluded such patients.
Conclusions
Significant variability exists in reference standard methods for delirium diagnosis in published research. Increasing standardization by documenting inter-rater reliability, using standardized cognitive and delirium detection tools, incorporating diagnostic expert consensus panels and using all available information in patients declining or unable to participate with formal testing may help advance delirium research by increasing consistency of case detection and improving generalizability of research results.
Keywords: delirium, dementia, amnestic, cognitive disorders, reference standards, research design, data collection
Introduction
Delirium is a clinical syndrome characterized by an acute and fluctuating cognitive impairment, occurring over hours to days, primarily associated with inattention and other cognitive and behavioral changes.1 Delirium occurs very frequently throughout the healthcare system and is associated with substantial suffering and loss of dignity,2,3 longer hospital stays, 4–6 institutionalization at hospital discharge,7,8 increased healthcare expenditures, 9 increased 1-year mortality 10–13 and long-term cognitive impairment.14–17
Common to most diagnoses in the psychiatric literature, no pathognomonic test (e.g., laboratory, imaging, or biomarker) can identify delirium; therefore the diagnosis is predicated upon the careful clinical examination. In addition to a thorough patient history and physical examination, a delirium diagnosis requires: 1) history from collateral sources documenting an acute and fluctuating change in cognitive function and behavior from baseline, 2) examination of the patient’s mental state documenting decreased attention and other associated cognitive and behavioral impairments (e.g., disorientation, impaired short- and long-term memory, perceptual disturbances, hallucinations, delusions, motoric abnormalities and sleep disturbances), and 3) review of laboratory and other investigations (e.g. radiological testing) which may help detect underlying cause(s) of delirium.18
Reliable and valid delirium diagnoses, using a reference standard, are crucial for the advancement of clinical research in this field. To better understand its epidemiology, risk factors, phenomenology, etiology and prevention, accurate case detection is important. Given the fluctuating nature of its presentation, accurate and reproducible diagnoses are an especially challenging issue for delirium research of all types.19 One particular type of study that must, by design, regularly employ an independent reference rater evaluation to serve as the reference standard, is the development and evaluation of delirium detection tools. 20–22 Details of these reference rater methods are scant in most research publications. Although reference standards are important in all types of delirium research, understanding the reference rater methodology that underpins the development of detection instruments is arguably the most important standard to characterize, as it underlies the assumptions made in studies, where only the delirium detection instrument is used as evidence of the diagnosis. Hence, the objective of this inquiry is to characterize the methodology used as a reference standard in studies evaluating delirium detection tools in hospitalized patients, using a survey-based study design.
Methods
Study Sample
A sampling frame of 37 unique investigators representing 39 studies, published between 1990 and 2012, were obtained from 3 systematic reviews of the literature evaluating delirium detection tools against a reference standard for delirium diagnosis.20–22 Of these 39 studies, 16 (41%) were performed in ICU and 23 (59%) in non-ICU in-patient hospital settings (See Appendix).
Survey Design and Testing
The survey was designed by co-authors with expertise in the clinical diagnosis of delirium, the development and use of delirium detection tools and/or survey design methodology. The survey included questions about the following areas of reference rater methodology: 1) characteristics of delirium reference raters (number per study, professional background, training and experience), (2) sources of information used in determining the delirium diagnosis (including use of standardized cognitive testing and delirium detection tools), (3) the use of consensus panels in making a final delirium diagnosis, and (4) methodology for evaluating patients who did not answer questions due to decreased arousal or patient refusal. The survey was pilot-tested with two delirium researchers and revised based on their feedback. A web-based version of the survey was developed using “SurveyMonkey ” (www.surveymonkey.com) and pilot tested by two additional delirium researchers. As a token of appreciation, an electronically issued $US 50 gift card was offered to participants. This study was reviewed and approved by the Johns Hopkins University Institutional Review Board; all survey respondents provided informed consent.
Survey Distribution and Response
In September 2012, an email was sent to the corresponding author of each of the 39 studies eligible for this research, requesting completion of the web-based survey with respect to the reference rater methodology used in the specific eligible study. At least 2 additional emails inviting participation were resent to non-responders in October and November, 2012. The authors who did not respond to email invitations were contacted by phone and offered the option of completing the survey via a telephone interview (conducted by KJN). The last survey was completed in May 2013. Respondents included 31 of 37 (84%) authors, representing 33 of 39 (85%) studies; 29 authors responded to the web-based survey, and 4 completed the survey by phone. No response was received from 5 authors and 1 declined to participate.
Survey Analysis
Standard descriptive statistics were performed using Excel (version 2010). Median values and 25–75% interquartile ranges (IQR) were reported for data with non-normal distributions.
Results
Respondent and Reference Rater Characteristics
Respondents identified themselves as the principal investigator in 76% of the 33 studies, with 55% of respondents serving as a delirium reference rater in the study being evaluated. Of 82 reference raters participating in the 33 studies, 79% were physicians from the following specialties: 51% psychiatry, 29% geriatrics, 9% critical care, 9% neurology and 2% not described. The background of the physician reference raters (n=65) were described as: 51% attendings/consultants, 20% fellows/senior registrars and 14% house staff (i.e., interns, residents, and junior registrars), with 15% not reported. The remainder of the reference raters (n=17) were nurses (7%), psychologists (4%) and research assistants (1%), with 7% not reported. Reference raters’ median (IQR) duration of clinical experience with diagnosing delirium was 7 (4–10) years, with 5% having no clinical experience prior to conducting the eligible study.
Reference Rater Training Practices
The median number (IQR) of reference raters per study was 2.5 (2–3) with a range of 1 to 15; 18% (n=6) of studies used only one reference rater. Of the remaining 27 studies with more than one reference rater, inter-rater reliability was evaluated in 70% (n=19) of studies, not evaluated in 15% (n=4), and not reported in 15%. Based on the 23 studies acknowledging reference rater training approaches, a median (IQR) of 20 (11–100) patients per study were evaluated by the study’s reference raters prior to starting the study as part of standardization and training. However narrative descriptions by some of the respondents in the survey reporting the highest numbers of patients, suggest that this often included patients who had been seen in routine clinical practice by the reference rater previous to the start of the study, and not patients evaluated using the standardized procedures unique to the given study.
Reference Rater Examination Practices
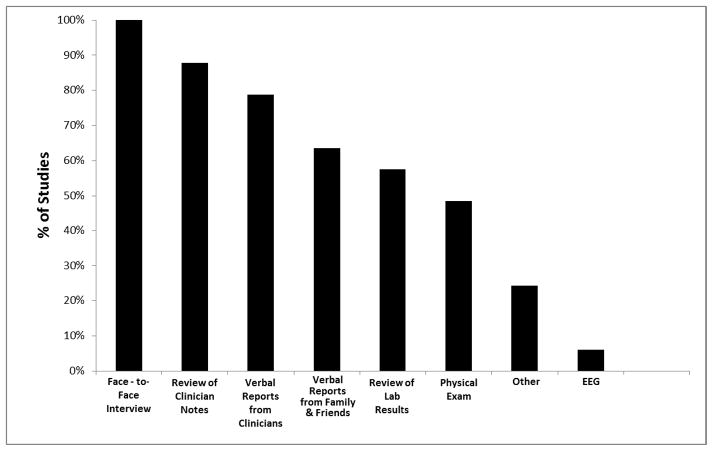
The sources of information used in the reference rater examination are outlined in Figure 1. The median (IQR) time spent with the patient, and time taken for the entire examination including medical record review were reported as 18 (15–30) and 30 (20–45) minutes, respectively. Respondents were asked about the use of formal cognitive tests and delirium detection tools in the reference standard diagnosis of delirium. At least one cognitive test was used in 20 studies (61%), at least one delirium detection tool was used in 15 studies (45%); 11 studies (33%) used both standardized cognitive testing and delirium detection tools, 13(39%) used one or the other, and 9 (27%) used neither. The types of cognitive and delirium detection tools used are outlined in the Table. The most frequently used cognitive tests were the Mini Mental State Examination (MMSE), Digit Span, and Testing for Orientation. The most frequently used delirium detection tools were the Confusion Assessment Method (CAM), the Memorial Delirium Assessment Scale (MDAS), and the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). (Place Table Here)
Figure 1.
Sources of Information for Reference Raters’ Delirium Evaluation (n=33 studies)
Table.
Frequency and Type of Standardized Cognitive and Delirium Detection Tool Used by Reference Rater as Part of Delirium Evaluation
| Cognitive Tests (Used in 20 (61%) of 33 studies)a | N | % of All Studies N=33 |
|---|---|---|
| Mini Mental Status Exam (MMSE) | 17 | 52% |
| Digit Span | 12 | 36% |
| Testing for Orientation (e.g. person, place, time) | 12 | 36% |
| Months of the Year Backwards | 7 | 21% |
| Days of the Week Backwards | 5 | 15% |
| Clinician’s Global Rating | 5 | 15% |
| Clock Drawing Test | 2 | 6% |
| Short Portable Mental Status Questionnaire (SPMSQ) | 2 | 6% |
| Comprehensive Geriatric Assessment | 2 | 6% |
| Clinical Dementia Rating (CDR) | 2 | 6% |
| Trail Making Test A | 2 | 6% |
| Trail Making Test B | 2 | 6% |
| Blessed Dementia Scale | 2 | 6% |
| Digit Cancellation Test | 1 | 3% |
| Vigilance “A” Test (VAT) | 1 | 3% |
| Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) | 1 | 3% |
| Delirium Detection Tools (Used in 13 (39%) of 33 studies)a | ||
| Confusion Assessment Method (CAM) | 7 | 21% |
| Memorial Delirium Assessment Scale (MDAS) | 4 | 12% |
| Confusion Assessment Method for the ICU (CAM-ICU) | 4 | 12% |
| Delirium Rating Scale- Revised 1998 (DRS-98R) | 3 | 9% |
| Intensive Care Delirium Screening Checklist (ICDSC) | 2 | 6% |
| Clinical Assessment of Confusion (CAC) | 1 | 3% |
| Nursing Delirium Screening Scale (Nu-DESC) | 1 | 3% |
| Cognitive Test for Delirium (CTD) | 1 | 3% |
| Delirium Index | 1 | 3% |
| Other (list) | 6 | 18% |
More than one cognitive test or delirium detection tool could be used in a given study.
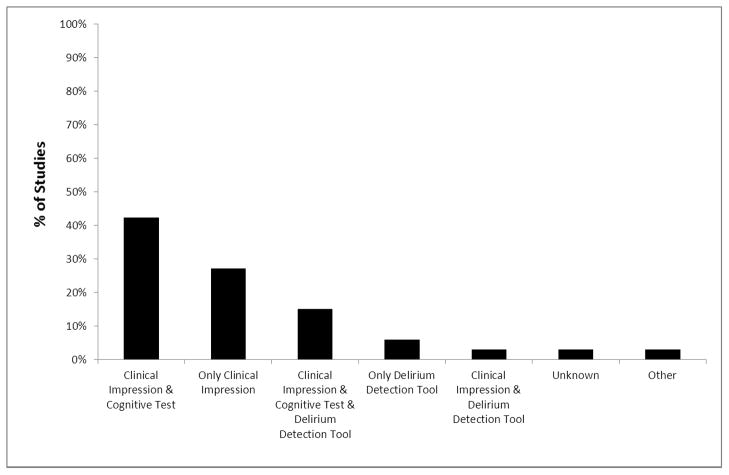
Delirium Diagnostic Assignment
The diagnostic classification systems used in the 33 studies were as follows: 58% DSM IV, 24% DSM III-R, 9% ICD 10, and 9% CAM algorithm. The incorporation of cognitive and delirium screening tool information and clinical impression in the diagnostic assignment is displayed in Figure 2. Respondents described the use of a consensus panel to review delirium diagnoses in 70% (n=23) of studies; 27% (n=9) did not use such a procedure and 3% (n=1) reported another procedure where only select patients were reviewed.
Figure 2.
Information Used in Reference Raters’ Delirium Diagnosis (n=33 studies)
Special Examination Considerations
Respondents reported procedures used when patients declined to answer the cognitive testing questions during the evaluation. Studies used all available information to decide on delirium diagnosis in this case in 70% (n=23), excluded the patient in 15% (n=5), and were not certain about the procedure in 15% (n=5). The procedure for evaluating patients with a decreased level of arousal that precluded formal cognitive testing revealed that 70% (n=23) of the studies used all available information to decide on delirium diagnosis, 15% (n=5) excluded the patient from the study, 6% (n=2) were uncertain about the procedure, and in 9% (n=3) another procedure was employed but the description was not included in the response to the survey.
Discussion
This is the first systematic evaluation of reference rater practices for the diagnosis of delirium in clinical research studies of hospitalized patients. The reference rater methods reported in the survey are quite variable. The majority of reference raters were physicians, from a number of different specialties, with wide-ranging clinical experience in diagnosing delirium. Almost without exception, the reference standard diagnosis was reported to be based on “clinical judgment”, and while diagnosis was reported to incorporate diverse sources of information, including the patient’s performance on a wide range of cognitive tests and delirium rating tools, a substantial proportion of reference raters based their diagnosis on clinical judgment in the absence of any standardized testing.
The literature suggests that delirium under-diagnosis by physicians in clinical practice is as high as 46–66% among non-critically ill, hospitalized patients. 23, 24 Findings in an ICU population reveal that physicians were able to identify delirium with 29% sensitivity when using clinical judgment alone without the aid of objective testing.25 While clinical judgment will be required in reference standard diagnosis, it needs to be informed by data gained from objective cognitive testing and collateral information gathered in a systematic examination.
There are no definitive objective diagnostic tests for delirium at this time; however this is true of many other psychiatric diseases as well. As is typically the case in most psychiatric research, clinical and research practice has typically relied on determining a categorical presence or absence of a given diagnosis, using clinical examination, with the clinician both eliciting and interpreting the significance of patients’ signs and symptom.26 This approach relies on the experience of the clinician for making accurate (or valid) diagnoses in this process and has often regarded the more experienced physician as the “gold standard”. 27 However there are potential shortcomings with this approach; for example, literature has demonstrated the fallibility of radiologic diagnosis, with as many as 30% of pulmonary lesions missed when using a single radiologist’s review.28 Since the potential for diagnostic error might be high in delirium given its fluctuating presentation, even a one-time assessment by an experienced physician cannot necessarily be regarded as a “gold standard”, with serial assessments and collateral information from sources such as family, care providers and validated chart review to detect fluctuations over time potentially being required for the most accurate diagnostic assessment.
The results from our survey suggest that only a minority of reference raters were non-physicians. Our survey does not determine the appropriateness of non-physicians in completing such assessments. There is some evidence that well-trained, non-clinical research personnel can use standardized tools to gather information relevant to delirium assessment with high reliability and validity when compared to physicians.29 Rigorous training, before and during studies, led by experienced clinicians expert in delirium diagnosis, accompanied by inter-rater reliability evaluation, is one method to improve reliability of delirium diagnoses.27 Quality control efforts, such as co-rating in-person, videotaped interviews or sequential evaluations of the same patient on the same day, should be used to assess inter-rater reliability throughout a study. Due to the heavy reliance on clinical impression by reference raters, a consensus panel of multiple experts reviewing all available data after a patient evaluation may also increase the validity of the delirium diagnostic process. 30 A majority of studies in this survey indicated convening a consensus panel.
Two thirds of survey respondents endorsed the use of either standardized cognitive testing and/or the use of delirium detection tools as part of their diagnostic assessment; one third did not use any such instruments, basing their diagnosis solely on clinical impression. The use of standardized tools might be an additional method for improving the reliability, and ultimately validity and generalizability of delirium diagnoses. The use of itemized dimensional symptom scales, such as the MDAS 31 or the Delirium Rating Scale-Revised 9832 allows for the calculation of delirium severity and further study of specific delirium phenomenology. Approaches to operationalize criteria in delirium diagnosis detailed in the literature, include the careful description by Gottlieb and colleagues.33 Each DSM III criteria is demonstrated clinically with specific cognitive testing and rating of behavioral symptoms. A similar approach is employed by other authors in the comparing delirium identification by different diagnostic systems including the DSM editions III, III-R, IV and the ICD10.34–36 Routinely reporting operationalization approaches used by reference raters in the describing study methodology would greatly enhance the ability to compare findings between studies of delirium.
Findings from this survey highlight variability in how studies incorporate patients who may be unable or unwilling to participate in cognitive testing. Patients who decline to answer questions, or are too drowsy to participate in cognitive testing may be more likely to have delirium than those who are willing and able. A previous study reported that 50% of patients refusing to answer attention testing questions were assessed as delirious by a second examiner using all available clinical information.37 Studies excluding patients who refuse to participate on a given day, or are too drowsy to comply with active testing may be subject to ascertainment bias, especially if not including information from collateral informants and medical record review. The exclusion of non-responders who represent patients with the hypoactive motoric subtype of delirium is a serious problem; previous research suggests that the hypoactive subtype is associated with worse clinical outcomes when compared to the hyperactive subtype.36
This is the first study to systematically describe the reference rater methodology used for delirium diagnosis in clinical research evaluating hospitalized patients, and to our knowledge, is a unique contribution to the delirium literature. Advancing reference rater methodology is critical because, in the absence of laboratory tests or biomarkers, clinical expert opinion will remain the standard to establish diagnostic criteria for the field moving forward. This study also has potential limitations. First, the survey does not include information from all possible studies in the field; however, it does include 33 (85%) of 39 studies from 3 independent systematic reviews of delirium screening tools, and as such it is likely representative of the main body of available literature. Moreover, our survey response rate is better than the 68% rate previously described for physicians 38 and 56% for academics in general.39 Second, our survey did not delineate exactly how each reference raters used data from the exam to operationalize the delirium criteria employed in the various diagnostic classification systems (e.g., DSM-IV) used in these studies. More detail in this regard would be helpful in understanding the generalizability of the diagnostic process and help develop research standards for diagnosis. This detail would be better elucidated via future qualitative interviews of reference raters. Finally, this study cannot offer guidelines for best diagnostic practices; however, until present the reference standard delirium diagnosis has remained a “black box” in much of the literature. This survey clearly describes the variability of practice and reveals areas where increased standardization of reference examinations may help advance the field.
Conclusion
This survey demonstrates significant variability in reference rater methods for delirium diagnosis in published research of hospitalized patients. Based on these findings, reference rater methods could be further improved in the following areas: 1) performing and reporting inter-rater reliability among multiple reference raters, 2) using standardized cognitive and validated delirium detection tools, 3) incorporating consensus panels for adjudication of diagnoses, and 4) using all available information in patients declining or unable to comply with formal testing. Such measures have the potential to advance delirium research by increasing consistency of case detection and improving generalizability of studies conducted in different settings.
Supplementary Material
Acknowledgments
Funding Sources for this Study Include
Internal Funding from the Department of Psychiatry and Behavioral Sciences, Johns Hopkins University School of Medicine
Dr. Inouye’s time is supported in part by Grants No. K07AG041835 and P01AG031720 from the National Institute on Aging and by the Milton and Shirley F. Levy Family Chair
Footnotes
Conflicts of Interest:
Dr. Neufeld receives funding from a grant by Ornim Medical Device manufacturers.
References
- 1.American Psychiatric Association, American Psychiatric Association. DSM-5 Task Force; Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, Va: American Psychiatric Association; 2013. [Google Scholar]
- 2.Marcantonio ER. In the clinic. Delirium. Ann Intern Med. 2011;154:ITC6-1–16. doi: 10.7326/0003-4819-154-11-201106070-01006. [DOI] [PubMed] [Google Scholar]
- 3.Leslie DL, Inouye SK. The importance of delirium: economic and societal costs. J Am Geriatr Soc. 2011;59 (Suppl 2):S241–3. doi: 10.1111/j.1532-5415.2011.03671.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rudolph JL, Marcantonio ER. Review articles: postoperative delirium: acute change with long-term implications. Anesth Analg. 2011;112:1202–1211. doi: 10.1213/ANE.0b013e3182147f6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomason JW, Shintani A, Peterson JF, et al. Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. 2005;9:R375–81. doi: 10.1186/cc3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pun BT, Ely EW. The importance of diagnosing and managing ICU delirium. Chest. 2007;132:624–636. doi: 10.1378/chest.06-1795. [DOI] [PubMed] [Google Scholar]
- 7.McAvay GJ, Van Ness PH, Bogardus ST, Jr, et al. Older adults discharged from the hospital with delirium: 1-year outcomes. J Am Geriatr Soc. 2006;54:1245–1250. doi: 10.1111/j.1532-5415.2006.00815.x. [DOI] [PubMed] [Google Scholar]
- 8.Neufeld KJ, Leoutsakos JM, Sieber FE, et al. Outcomes of Early Delirium Diagnosis After General Anesthesia in the Elderly. Anesth Analg. 2013;117:471–478. doi: 10.1213/ANE.0b013e3182973650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leslie DL, Marcantonio ER, Zhang Y, et al. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168:27–32. doi: 10.1001/archinternmed.2007.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Salluh JI, Soares M, Teles JM, et al. Delirium epidemiology in critical care (DECCA): an international study. Crit Care. 2010;14:R210. doi: 10.1186/cc9333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rabins PV, Folstein MF. Delirium and dementia: diagnostic criteria and fatality rates. Br J Psychiatry. 1982;140:149–153. doi: 10.1192/bjp.140.2.149. [DOI] [PubMed] [Google Scholar]
- 12.Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762. doi: 10.1001/jama.291.14.1753. [DOI] [PubMed] [Google Scholar]
- 13.Pisani MA, Kong SY, Kasl SV, et al. Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med. 2009;180:1092–1097. doi: 10.1164/rccm.200904-0537OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saczynski JS, Marcantonio ER, Quach L, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367:30–39. doi: 10.1056/NEJMoa1112923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davis DH, Muniz Terrera G, Keage H, et al. Delirium is a strong risk factor for dementia in the oldest-old: a population-based cohort study. Brain. 2012;135:2809–2816. doi: 10.1093/brain/aws190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Girard TD, Jackson JC, Pandharipande PP, et al. Delirium as a predictor of long-term cognitive impairment in survivors of critical illness. Crit Care Med. 2010;38:1513–1520. doi: 10.1097/CCM.0b013e3181e47be1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pandharipande PP, Girard TD, Jackson JC, et al. Longterm Cognitive Impairment after Critical Illness. N Engl J Med. 2013;369:1306–16. doi: 10.1056/NEJMoa1301372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lipowski ZJ. Delirium: acute confusional states. New York: Oxford University Press; 1990. [Google Scholar]
- 19.Davis DH, Kreisel SH, Terrera GM, et al. The epidemiology of delirium: challenges and opportunities for population studies. Am J Geriatr Psychiatry. 2013 Jul 30;:S1064–7481. 215–217. doi: 10.1016/j.jagp.2013.04.007. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gusmao-Flores D, Salluh JI, Chalhub RA, et al. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) and Intensive Care Delirium Screening Checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. 2012;16:R115. doi: 10.1186/cc11407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neto AS, Nassar AP, Jr, Cardoso SO, et al. Delirium screening in critically ill patients: a systematic review and meta-analysis. Crit Care Med. 2012;40:1946–1951. doi: 10.1097/CCM.0b013e31824e16c9. [DOI] [PubMed] [Google Scholar]
- 22.Wong CL, Holroyd-Leduc J, Simel DL, et al. Does this patient have delirium? : value of bedside instruments. JAMA. 2010;304:779–786. doi: 10.1001/jama.2010.1182. [DOI] [PubMed] [Google Scholar]
- 23.Armstrong SC, Cozza KL, Watanabe KS. The misdiagnosis of delirium. Psychosomatics. 1997;38:433–439. doi: 10.1016/S0033-3182(97)71420-8. [DOI] [PubMed] [Google Scholar]
- 24.Swigart SE, Kishe Y, Thurber S, et al. Misdiagnosed delirium in patient referrals to a university-based hospital psychiatry department. Psychosomatics. 2008;49:104–108. doi: 10.1176/appi.psy.49.2.104. [DOI] [PubMed] [Google Scholar]
- 25.van Eijk MM, van Marum RJ, Klijn IA, et al. Comparison of delirium assessment tools in a mixed intensive care unit. Crit Care Med. 2009;37:1881–1885. doi: 10.1097/CCM.0b013e3181a00118. [DOI] [PubMed] [Google Scholar]
- 26.Dohrenwend BP, Dohrenwend BS. Perspectives on the past and future of psychiatric epidemiology. The 1981 Rema Lapouse Lecture. Am J Public Health. 1982;72:1271–1279. doi: 10.2105/ajph.72.11.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. Oxford; New York: Oxford University Press; 2003. [Google Scholar]
- 28.Yerushalmy J. Reliability of chest radiography in the diagnosis of pulmonary lesions. Am J Surg. 1955;89:231–240. doi: 10.1016/0002-9610(55)90525-0. [DOI] [PubMed] [Google Scholar]
- 29.Simon SE, Bergmann MA, Jones RN, et al. Reliability of a structured assessment for nonclinicians to detect delirium among new admissions to postacute care. J Am Med Dir Assoc. 2006;7:412–415. doi: 10.1016/j.jamda.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 30.Zou Y, Cole MG, Primeau FJ, et al. Detection and diagnosis of delirium in the elderly: psychiatrist diagnosis, confusion assessment method, or consensus diagnosis? Int Psychogeriatr. 1998;10:303–308. doi: 10.1017/s1041610298005390. [DOI] [PubMed] [Google Scholar]
- 31.Breitbart W, Rosenfeld B, Roth A, et al. The Memorial Delirium Assessment Scale. J Pain Symptom Manage. 1997;13:128–137. doi: 10.1016/s0885-3924(96)00316-8. [DOI] [PubMed] [Google Scholar]
- 32.Trzepacz PT, Mittal D, Torres R, et al. Validation of the Delirium Rating Scale-revised-98: comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci. 2001;13:229–242. doi: 10.1176/jnp.13.2.229. [DOI] [PubMed] [Google Scholar]
- 33.Gottlieb GL, Johnson J, Wanich C, Sulllivan E. Delirium in the medically ill elderly: operationalizing the DSM-III criteria. Int Psychogeriatr. 1991;3:181–196. doi: 10.1017/s1041610291000650. [DOI] [PubMed] [Google Scholar]
- 34.Kazmierski J, Kowman M, Banach M, Fendler W, Okonski P, Banys A, Jaszewski R, Sobow T, Kloszewska I. Clinical utility and use of DSM-IV and ICD-10 criteria and the Memorial Delirium Assessment Scale in establishing a diagnosis of delirium after cardiac surgery. Psychosomatics. 2008;49:73–76. doi: 10.1176/appi.psy.49.1.73. [DOI] [PubMed] [Google Scholar]
- 35.Laurila JV, Pitkala KH, Strandberg TE, Tilvis RS. The impact of different diagnostic criteria on prevalence rates for delirium. Dement Geriatr Cogn Disord. 2003;16:156–162. doi: 10.1159/000071004. [DOI] [PubMed] [Google Scholar]
- 36.Meagher DJ, Leonard M, Donnelly S, Conroy M, Adamis D, Trzepacz PT. A longitudinal study of motor subtypes in delirium: relationship with other phenomenology, etiology, medication exposure and prognosis. J Psychosom Res. 2011;71:395–403. doi: 10.1016/j.jpsychores.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 37.Neufeld KJ, Hayat MJ, Coughlin JM, et al. Evaluation of two intensive care delirium screening tools for non-critically ill hospitalized patients. Psychosomatics. 2011;52:133–140. doi: 10.1016/j.psym.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 38.Ahlers-Schmidt CR, Chesser A, Hart T, et al. Assessing Physician Response Rate Using a Mixed-Mode Survey. KJM. 2010;3:1–6. [Google Scholar]
- 39.Baruch Y. Response rate in academic studies- a comparative analysis. Hum Relat. 1999;52:421–438. [Google Scholar]
- 40.Bergeron N, Dubois MJ, Dumont M, et al. Intensive Care Delirium Screening Checklist: evaluation of a new screening tool. Intensive Care Med. 2001;27:859–864. doi: 10.1007/s001340100909. [DOI] [PubMed] [Google Scholar]
- 41.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU) JAMA. 2001;286:2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 42.Ely EW, Margolin R, Francis J, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2001;29:1370–1379. doi: 10.1097/00003246-200107000-00012. [DOI] [PubMed] [Google Scholar]
- 43.George C, Nair JS, Ebenezer JA, et al. Validation of the Intensive Care Delirium Screening Checklist in nonintubated intensive care unit patients in a resource-poor medical intensive care setting in South India. J Crit Care. 2011;26:138–143. doi: 10.1016/j.jcrc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 44.Guenther U, Popp J, Koecher L, et al. Validity and reliability of the CAM-ICU Flowsheet to diagnose delirium in surgical ICU patients. J Crit Care. 2010;25:144–151. doi: 10.1016/j.jcrc.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 45.Gusmao-Flores D, Salluh JI, Dal-Pizzol F, et al. The validity and reliability of the Portuguese versions of three tools used to diagnose delirium in critically ill patients. Clinics (Sao Paulo) 2011;66:1917–1922. doi: 10.1590/S1807-59322011001100011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heo EY, Lee BJ, Hahm BJ, et al. Translation and validation of the Korean confusion assessment method for the intensive care unit. BMC Psychiatry. 2011;11:94. doi: 10.1186/1471-244X-11-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Immers HE, Schuurmans MJ, van de Bijl JJ. Recognition of delirium in ICU patients: a diagnostic study of the NEECHAM confusion scale in ICU patients. BMC Nurs. 2005;4:7. doi: 10.1186/1472-6955-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lin SM, Liu CY, Wang CH, et al. The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med. 2004;32:2254–2259. doi: 10.1097/01.ccm.0000145587.16421.bb. [DOI] [PubMed] [Google Scholar]
- 49.Luetz A, Heymann A, Radtke FM, et al. Different assessment tools for intensive care unit delirium: which score to use? Crit Care Med. 2010;38:409–418. doi: 10.1097/CCM.0b013e3181cabb42. [DOI] [PubMed] [Google Scholar]
- 50.Mitasova A, Kostalova M, Bednarik J, et al. Poststroke delirium incidence and outcomes: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) Crit Care Med. 2012;40:484–490. doi: 10.1097/CCM.0b013e318232da12. [DOI] [PubMed] [Google Scholar]
- 51.Radtke FM, Franck M, Oppermann S, et al. The Intensive Care Delirium Screening Checklist (ICDSC)--translation and validation of intensive care delirium checklist in accordance with guidelines. Anasthesiol Intensivmed Notfallmed Schmerzther. 2009;44:80–86. doi: 10.1055/s-0029-1202647. [DOI] [PubMed] [Google Scholar]
- 52.Tobar E, Romero C, Galleguillos T, et al. Confusion Assessment Method for diagnosing delirium in ICU patients (CAM-ICU): cultural adaptation and validation of the Spanish version. Med Intensiva. 2010;34:4–13. doi: 10.1016/j.medin.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 53.Toro AC, Escobar LM, Franco JG, et al. Spanish version of the CAM-ICU (Confusion Assessment Method for the Intensive Care Unit) Pilot study of validation Med Intensiva. 2010;34:14–21. doi: 10.1016/j.medin.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 54.van Eijk MM, van den Boogaard M, van Marum RJ, et al. Routine use of the confusion assessment method for the intensive care unit: a multicenter study. Am J Respir Crit Care Med. 2011;184:340–344. doi: 10.1164/rccm.201101-0065OC. [DOI] [PubMed] [Google Scholar]
- 55.de Negreiros DP, da Silva Meleiro AM, Furlanetto LM, et al. Portuguese version of the Delirium Rating Scale-Revised-98: reliability and validity. Int J Geriatr Psychiatry. 2008;23:472–477. doi: 10.1002/gps.1906. [DOI] [PubMed] [Google Scholar]
- 56.de Rooij SE, van Munster BC, Korevaar JC, et al. Delirium subtype identification and the validation of the Delirium Rating Scale--Revised-98 (Dutch version) in hospitalized elderly patients. Int J Geriatr Psychiatry. 2006;21:876–882. doi: 10.1002/gps.1577. [DOI] [PubMed] [Google Scholar]
- 57.Farrell KR, Ganzini L. Misdiagnosing delirium as depression in medically ill elderly patients. Arch Intern Med. 1995;155:2459–2464. [PubMed] [Google Scholar]
- 58.Gaudreau JD, Gagnon P, Harel F, et al. Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale. J Pain Symptom Manage. 2005;29:368–375. doi: 10.1016/j.jpainsymman.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 59.Gemert van LA, Schuurmans MJ. The Neecham Confusion Scale and the Delirium Observation Screening Scale: capacity to discriminate and ease of use in clinical practice. BMC Nurs. 2007;6:3. doi: 10.1186/1472-6955-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gonzalez M, de Pablo J, Fuente E, et al. Instrument for detection of delirium in general hospitals: adaptation of the confusion assessment method. Psychosomatics. 2004;45:426–431. doi: 10.1176/appi.psy.45.5.426. [DOI] [PubMed] [Google Scholar]
- 61.Grassi L, Caraceni A, Beltrami E, et al. Assessing delirium in cancer patients: the Italian versions of the Delirium Rating Scale and the Memorial Delirium Assessment Scale. J Pain Symptom Manage. 2001;21:59–68. doi: 10.1016/s0885-3924(00)00241-4. [DOI] [PubMed] [Google Scholar]
- 62.Hestermann U, Backenstrass M, Gekle I, et al. Validation of a German version of the Confusion Assessment Method for delirium detection in a sample of acute geriatric patients with a high prevalence of dementia. Psychopathology. 2009;42:270–276. doi: 10.1159/000224151. [DOI] [PubMed] [Google Scholar]
- 63.Inouye SK, van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941–948. doi: 10.7326/0003-4819-113-12-941. [DOI] [PubMed] [Google Scholar]
- 64.Leung JM, Leung VW, Leung CM, et al. Clinical utility and validation of two instruments (the Confusion Assessment Method Algorithm and the Chinese version of Nursing Delirium Screening Scale) to detect delirium in geriatric inpatients. Gen Hosp Psychiatry. 2008;30:171–176. doi: 10.1016/j.genhosppsych.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 65.Matsuoka Y, Miyake Y, Arakaki H, et al. Clinical utility and validation of the Japanese version of Memorial Delirium Assessment Scale in a psychogeriatric inpatient setting. Gen Hosp Psychiatry. 2001;23:36–40. doi: 10.1016/s0163-8343(00)00121-3. [DOI] [PubMed] [Google Scholar]
- 66.O’Keeffe ST, Gosney MA. Assessing attentiveness in older hospital patients: global assessment versus tests of attention. J Am Geriatr Soc. 1997;45:470–473. doi: 10.1111/j.1532-5415.1997.tb05173.x. [DOI] [PubMed] [Google Scholar]
- 67.Pompei P, Foreman M, Cassel CK, et al. Detecting delirium among hospitalized older patients. Arch Intern Med. 1995;155:301–307. [PubMed] [Google Scholar]
- 68.Rockwood K, Goodman J, Flynn M, et al. Cross-validation of the Delirium Rating Scale in older patients. J Am Geriatr Soc. 1996;44:839–842. doi: 10.1111/j.1532-5415.1996.tb03745.x. [DOI] [PubMed] [Google Scholar]
- 69.Rolfson DB, McElhaney JE, Jhangri GS, et al. Validity of the confusion assessment method in detecting postoperative delirium in the elderly. Int Psychogeriatr. 1999;11:431–438. doi: 10.1017/s1041610299006043. [DOI] [PubMed] [Google Scholar]
- 70.Rosen J, Sweet RA, Mulsant BH, et al. The Delirium Rating Scale in a psychogeriatric inpatient setting. J Neuropsychiatry Clin Neurosci. 1994;6:30–35. doi: 10.1176/jnp.6.1.30. [DOI] [PubMed] [Google Scholar]
- 71.Ryan K, Leonard M, Guerin S, et al. Validation of the confusion assessment method in the palliative care setting. Palliat Med. 2009;23:40–45. doi: 10.1177/0269216308099210. [DOI] [PubMed] [Google Scholar]
- 72.Schuurmans MJ, Shortridge-Baggett LM, Duursma SA. The Delirium Observation Screening Scale: a screening instrument for delirium. Res Theory Nurs Pract. 2003;17:31–50. doi: 10.1891/rtnp.17.1.31.53169. [DOI] [PubMed] [Google Scholar]
- 73.Trzepacz PT, Baker RW, Greenhouse J. A symptom rating scale for delirium. Psychiatry Res. 1988;23:89–97. doi: 10.1016/0165-1781(88)90037-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.