Abstract
Purpose
To describe the transition to digital imaging and assess any impact on ocular disease classification.
Methods
Film and digital images, acquired by certified photographers, were evaluated independently according to standard procedures for the following: image quality, presence of cytomegalovirus (CMV) retinitis lesions, their extent, and proximity from disc and macula. Inter-grader agreement within the digital medium was also assessed.
Results
Among the fifteen eyes with CMV retinitis, the mean difference between film and digital images for linear distance of lesion edge to disc was 0.02 disc diameters (DD), for distance to center of macula was −0.04 DD and area covered by CMV retinitis was 0.95 disc area (DA). There was no statistically significant difference in distance and area measurements between media. Inter grader agreement in measurements of digital images was excellent for distance and area estimated.
Conclusion
Our results suggest that digital grading of CMV retinitis in LSOCA is comparable to that from film with respect to disease classification, measurements, and reproducibility. These findings provide support for continuity of grading data, despite the necessary transition in imaging media.
Keywords: imaging, digital fundus photography, CMV retinitis, AIDS
Introduction
The Longitudinal Studies of the Ocular Complications of AIDS (LSOCA) is a prospective observational study of patients with Acquired Immune Deficiency Syndrome (AIDS) in the era of highly active anti-retroviral therapy (HAART). Since 1998, the study has been following patients with and without CMV retinitis, collecting data on medication use and co-morbidities, and performing detailed ophthalmologic evaluations, including wide-angle fundus photographs that document nearly the entire retina. These photograph sets consist of one central stereoscopic (posterior pole) and eight surrounding 50° or 60° views, extending nearly to the equator. These periodic retinal photographs are sent to a centralized fundus photograph reading center (RC) for evaluation of ocular complications, especially cytomegalovirus (CMV) retinitis.1
At study inception, the fundus photographs were taken on film as color slide transparencies, and were mounted in plastic sheets in the approximate anatomic position. However, advances in digital color fundus imaging systems, coupled with decreasing availability of traditional film and laboratory processing has led most clinical centers to convert from film to digital imaging.2
Differences between digital and color retinal images may change the appearance of retinal lesions and might thereby create spurious changes in disease classification or lesion measurement in patients followed longitudinally. Morphology evaluations from digital images ideally must have continuity with historical data sets for appropriate comparisons. Some studies have noted a disturbing loss of sensitivity of lesion detection in digital images of diabetic retinopathy.3 Digital camera chips handle tonal balance and illumination differently than film, and digital clinical trial photograph submissions tend to have greater variability in quality compared to film submissions.4 The sensitivity of digital image evaluation could be improved to approximate that of film grading in age-related macular degeneration assessment with post hoc image enhancement at a reading center.5
To analyze potential effects on the grading of CMV retinitis status and other ocular complications of AIDS over the film to digital transition, LSOCA conducted a comparative study evaluating grading from both film and digital images obtained in the same session using a previously published standardized photographic protocol.1
Methods
Sets of fundus images using both film and digital media were collected from 25 LSOCA study patients after obtaining informed consent. Patients were selected based on their willingness to undergo additional photography. The fundus photographs of nine fields in each eye were taken with a wide-angle (50 or 60 degree) fundus camera, i.e., stereoscopic photographs of the disc and macula surrounded by photographs of 8 peripheral fields.1 The RC certified clinic photographers and digital systems, based upon submission of sample images, prior to initiation of digital photography. Both sets of photographs were deidentified and sent to the LSOCA reading center at the University of Wisconsin for detailed evaluation according to the standardized procedures.6 For uniform handling at the RC, digital image from the various makes of fundus cameras were loaded into Topcon IMAGEnet (Topcon Medical Imaging Inc., Paramus, NJ) and compressed at the highest quality setting.
For film grading, sets of 9-field photographs were examined on a light box (fitted with fluorescent tubes with a color rating of approximately 6,200 degrees Kelvin) using a Donaldson 5X stereo viewer. The location and extent of CMV retinitis were assessed using standard grid templates. The grader worked across photographic field boundaries, combining information from two or more images, when evaluating CMV retinitis lesions. Superimposing grids printed on transparent plastic sheets allowed the grader to establish the proper spatial relationships between individual fields.
For construction of a digital montage of the fundus, images were exported to Photoshop CS3 (Adobe Systems Inc, San Jose, CA) so that the fields could be positioned in anatomic location, using landmarks to facilitate alignment. The posterior pole was positioned at the center of the workspace and other fields were aligned peripherally. To accomplish this, graders were able to move and rotate the images, and to make them partially transparent for alignment of features in overlapping areas. Once the mosaic was completed, a digital version of the LSOCA grid, which demarcates the retinal regions (Zones 1–3) further divided into eight peripheral sectors (corresponding to the eight peripheral photographic fields), was placed over the montage for evaluation.
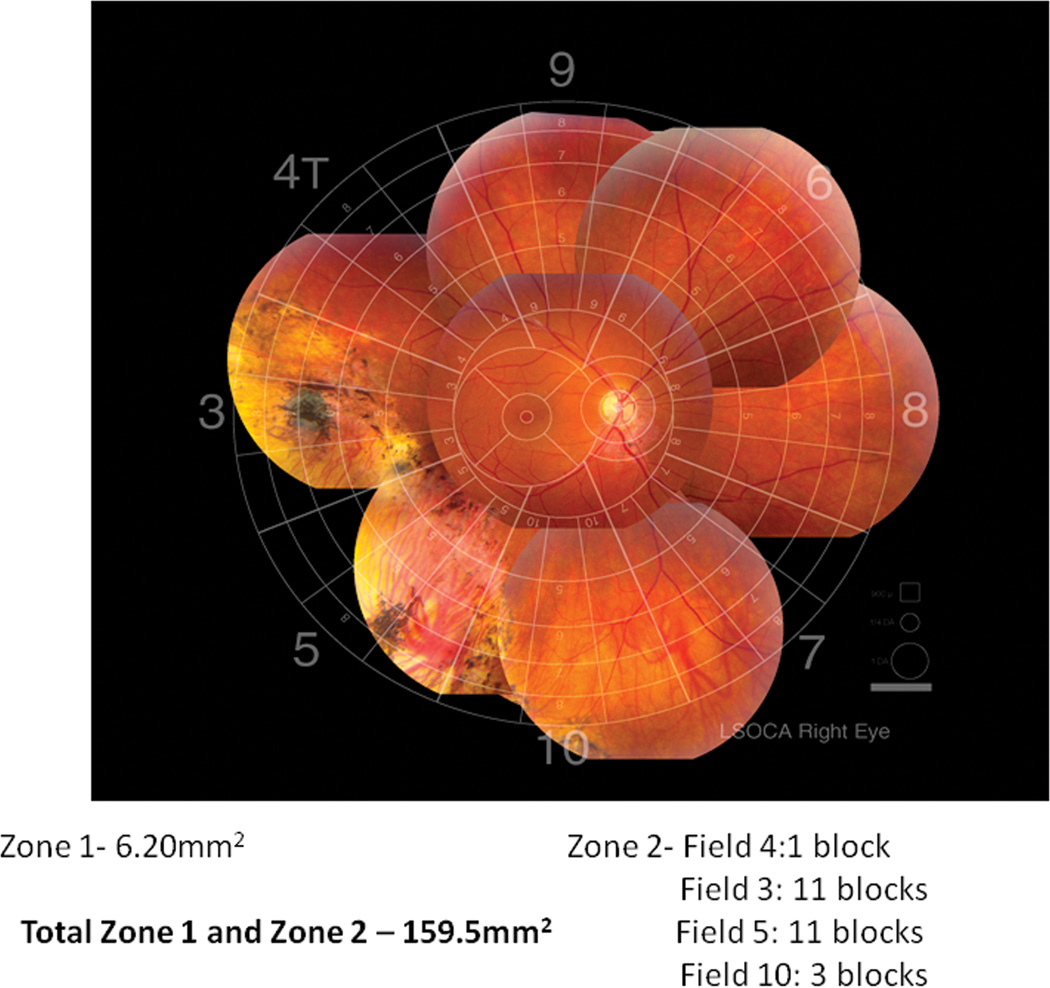
Extent of retinitis in each eye was evaluated according to the SOCA grading protocol.6 Proximity of CMV lesion to disc and macula were measured on film and digital images. On film, distance was measured using a stand magnifier incorporating a millimeter scale and then converted to standard DD (one DD equals 1.8 mm on the retina). Distances in digital images were measured using an electronic ruler and then converted to DD. Total area involved by CMV retinitis was estimated on film and digital images by counting the number of equal-area blocks demarcated by the LSOCA grid which are involved by CMV retinitis. The grader mentally combines partially-filled blocks to arrive at the total number of involved blocks in each sector or field, as shown in Figure 1.6 The area covered in each sector of the grid is summed to yield the total area of CMV retinitis in disc areas (DA) or as a percentage of the entire retina (1 DA equals 2.54 mm2). 7, 8This measurement is performed in the area extending to the ampullae of the vortex veins (Zones 1 and 2). Further peripheral involvement (Zone 3) is not measured but is noted on the grading form. Areas where the fundus cannot be visualized, due to poor photographic field definition, are also counted as “ungradable area”. For this study, the images were graded by 4 evaluators independantly, to assess the effect of grader variability with digital evaluations.
Figure 1.
Area of CMV retinitis measured by block counting method..
The principal difference between film and digital methods of display is that, in film, the images are mounted separately in the plastic sheet, so that a grader must superimpose the grid on each field in turn, whereas in digital the images are organized into an integrated mosaic so that the grid can be properly positioned on all images simultaneously. The objective assessment of digital image quality was assessed by using 3 color channel luminance histograms to analyze and manipulate separately each of the RGB channels. For each color channel, brightness is defined by the peak of the luminance curve and contrast as the span of the curve. The results were compared to previously published “optimal” brightness, contrast and color balance parameters.5
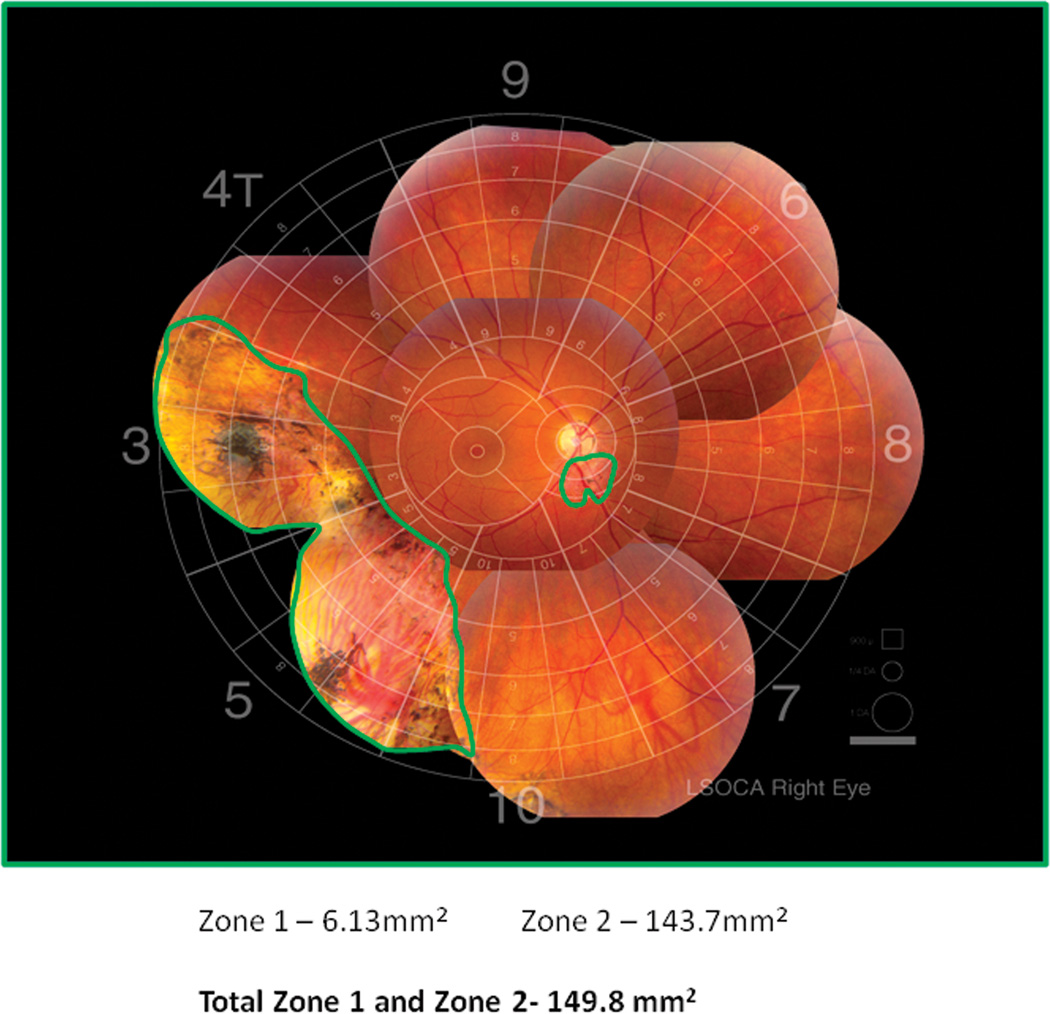
To explore the comparability of using computerized planimetry instead, twelve eyes (12 eyes) with CMV retinitis were evaluated independently for area of involvement using both the block counting method and planimetry. In order to include images that had varying amounts of CMV retinitis, another set of images with stratified area of CMV retinitis was analyzed. Rather than combining and then counting blocks, the grader simply outlines the entire retina (or sections thereof) with the planimetry tool (Figure 2). The computer program calculates the circumscribed area in square millimeters and converts it to disc areas (DA). Similarly, grid areas that are not adequately imaged or aligned are outlined via planimetry to determine the “ungradable area”.
Figure 2.
Area of CMV retinitis measured by computerized planimetry
For statistical analysis, Wilcoxon signed rank test was used to compare the differences between media and intraclass correlation coefficient was calculated to assess for grader variability. Mean absolute differences and mean differences were calculated. Analysis was performed using commercial software (SAS version 9.2 SAS Corporation, Cary, North Carolina).
Results
Comparison between film and digital media
Of the 48 film and digital images obtained, 33 eyes did not have any evidence of CMV retinitis and hence were not evaluated further. This is similar to the overall enrollment in the LSOCA trial, where one third of the AIDS patients present with CMV retinitis, and hence is representative of the LSOCA population. The film images were graded per regular procedure, while the digital images were graded independently by four different graders using standardized grading procedures.
Subjective assessment of image quality of the digital images was considered good to excellent. None of the digital images were ungradable due to poor photo quality. Evaluation of the luminance histograms of the 48 eyes showed red peak at 9/16 (span 7/16), green at 4/16 (span 5/16) and green red ratio was 0.44. There were no images with oversaturation of red, which could lead to washed out retinal features.
The AREDS model, based on luminance histograms of exemplar digital images of the fundus, showed red peak at 12/16 (span 8/16), green at 6/16 (span 8/16) and green- red ratio was 0.50.5 Although the LSOCA images were not optimal, they were in the safe range, where post hoc manipulation was not necessary for viewing the lesions of CMV retinitis.
There was no evidence of systematic difference between imaging media for determination of presence/absence of CMV retinitisamong the 15 eyes studied…
Distance measurement
Among the 15 eyes with CMV retinitis, the mean absolute difference for distance of lesion to outer edge of the optic disc was 0.16 DD (95 % CI 0.08–0.25), that for distance to center of macula was 0.17 DD (95% CI 0.04–0.30) (Table 1). There was no statistically significant difference between digital and film in measurement of retinitis proximity to disc and macula (p values for mean difference were 0.29 and 0.98 respectively).
Table 1.
Comparison of film vs. digital grading for variables of distance and area of CMV retinitis (N=48)
| Variables | N* | Digital images Mean(SD) |
Film images Mean (SD) |
Mean absolute difference (95% CI) |
Mean Difference (95% CI) |
p value |
|---|---|---|---|---|---|---|
| Distance to Disc (DD) | 14 | 2.89 (2.52) | 2.87 (2.62) | 0.16 (0.08, 0.25) | 0.02 (−0.11, 0.15) | 0.29 |
| Distance to macula (DD) | 14 | 3.70 (2.51) | 3.74 (2.68) | 0.17 (0.04, 0.30) | −0.04 (−0.21, 0.12) | 0.98 |
| Area of CMV retinitis (DA) | 15 | 44.08 (26.34) | 43.13 (26.04) | 1.77 (0.85, 2.68) | 0.95 (−0.30, 2.20) | 0.13 |
Includes images with gradable CMV retinitis only.
DD-disc diameter, DA- disc area, p value – Wilcoxon signed rank test
Area measurement
Mean retinal area involved by CMV retinitis was 44.08 DA for digital and 43.13 DA for film images. The mean absolute difference between film and digital images was 1.77 DA (95% CI 0.85–2.68). Area measurements were not significantly different between media. (p value for mean difference = 0.13) (Table 1).
In order to assess intergrader variability in the digital environment, distance and area measurements of each grader were compared to the senior evaluator. Intraclass correlations for proximity of CMV retinitis to the disc was 0.94 – 0.99, for proximity to the macula was 0.97–0.99, and for area of retinitis lesion was 0.88–0.91. (Table 2)
Table 2.
Inter-grader reproducibility of linear and area measurements on digital images (N=48)
| Variables | N* | Grader 1 ICC (95% CI) |
Grader 2 ICC (95% CI) |
Grader 3 ICC (95% CI) |
|---|---|---|---|---|
| Distance to Disc (DD) | 14 | 0.99 (0.96, 1) | 0.94 (0.84, 0.98) | 0.99 (0.98, 1) |
| Distance to macula (DD) | 14 | 0.99 (0.96, 1) | 0.97 (0.90, 0.99) | 0.99 (0.96, 1) |
| Area of CMV retinitis (DA) | 15 | 0.91 (0.77, 0.97) | 0.88 (0.68, 0.96) | 0.91 (0.77, 0.97) |
Includes images with gradable CMV retinitis only.
DD-disc diameter, DA- disc area
Comparison between block counting and computerized planimetry
Mean absolute difference for area of CMV retinitis between block estimation and planimetry (Figure 1), both performed on digital images, was 1.74 DA (95 % CI 0.67–2.81) and for ungradable area was 5.92 DA (95% CI 3.98–7.87). Although both measurements of area showed statistically significant differences between the block estimation and planimetry (p values of 0.03 and 0.001 respectively) (Table 3), the magnitude of the differences in area of CMV retinitis was not large enough to be clinically meaningful.
Table 3.
Block estimation vs. planimetry of area measured on digital mosaic images (N=12)
| Block Mean (SD) |
Planimetry Mean (SD) |
Mean absolute difference (95% CI) |
Mean Difference (95% CI) |
p value |
|
|---|---|---|---|---|---|
| CMV retinitis area (DA) | 48.51 (38.14) | 49.60 (39.35) | 1.74 (0.67, 2.81) | −1.09 (−2.49, 0.31) | 0.03 |
| Ungradable Area (DA) | 33.12 (24.22) | 38.94 (23.82) | 5.92 (3.98, 7.87) | −5.83 (−7.90, −3.76) | <0.01 |
DA- disc area, p value – Wilcoxon signed rank test
Discussion
LSOCA and the RC began to consider the possibility of transitioning to digital media in late 2005. Film used for study photos and good processing were becoming more difficult to find and clinics were acquiring digital cameras for general clinical photography. LSOCA was one of the first multicenter, longitudinal studies to investigate a switch to digital media mid study and hence a task force was assembled at the reading center, to evaluate the risk benefit ratio and analyze the climate for change in clinics. A questionnaire was sent to all participating clinics to assess the presence of, or possiblity of acquiring color digital systems. Initial problems seen in color digital images were poor photo quality due to low resolution capture devices and also a lack of knowledge of how to achieve optimal illumination and saturation of the color channels.
This initial phase took almost a year, during which time technology of digital fundus cameras was also rapidly progressing. Certification of digital systems and re-certification of photographers for digital images, helped standardize the resolution and tonal characteristics of images received for evaluation. There were a few hurdles experienced due to lack of motivation of some clinics, attributed in part, to the expenses involved with the upgrade to acceptable digital systems and in part related to the perceived lack of utility of such camera systems outside of clinical trials.
A number of published reports have reported the reliability, sensitivity and specificity of digital images to assess various ocular diseases with variable conclusions with respect to loss of sensitivity for lesion detection by digital imaging. 3, 9, 10Despite the many obvious advantages of digital photographs,11 image quality (specifically brightness, contrast, and color balance) of digital images can be more difficult to control than with film, thus possibly obscuring features of retinal disease.2 Color slides have a broader dynamic range than digital photos and exposure and color balance are much easier to control with film imaging. For detection of atrophic CMV retinitis, the presence of small spots and the border detection of larger ones, less than optimal image quality can be an issue.12, 13 Difficulties ensue from both underexposure, in which case the image may be too dark to differentiate lesion against normal retinal pigment epithelial (RPE) background, or from overexposure (typically involving over saturation of the red channel), in which case the subtle RPE abnormalities identifying atrophic lesions are washed out. The fundus photograph reading center attempts to correct for these variances by standardizing the equipment and technique of photography and also by tutoring the photographers to evaluate images for quality during the photo session. Another method to correct for color and contrast imbalances is by evaluating the color histogram of the photograph and modifying the color curves in order to maximize the visualization of ocular lesions.5
The results from this study suggest that evaluation of this small sample of digital images for assessment of CMV retinitis was equivalent to film, both in comparability of measurements and in grading reproducibility. The study is that is shows that as long as the images cover the required fields and have appropriate tonal and spatial characteristics, there is no meaningful difference in the data derived from film and digital images from a variety of camera makes and models. It also supports the use of planimetry to estimate area measurements. The efficiency of planimetry for measurements as opposed to grid block counting in individual slide frames offsets the time spent by the grader to create the photographic montage. As seen in Table 3, the area measurements for CMV retinitis as well as ungradable area are greater by planimetry. We think that this difference is due to the grading practice of not counting blocks until they are at least half filled with retinitis, which would tend to underestimate area. Similarly, ungradable areas are also calculated larger by planimetry, probably due to the same counting convention. In practice, we think planimetry should be the preferred mode of assessing longitudinal change in area, as the measurements will not be dependent on individual grid placement over separated fields. Figure 1 demonstrates the differences between grid block counting where area is calculated by counting the number of blocks filled with lesions, while planimetry assesses area by circumscribing the perimeter. In this example, measurements between both methods are fairly equivalent. Annotated images of measurements performed by planimetry can saved over the original image as an overlay and this can be used as a reference tool in clinical practice, to assist the evaluator or clinician in identifying change in lesion size over time. Planimetry can be easily learned and has proven reproducible in multiple studies at the reading center.
When the original SOCA procedure was written, 1DD was presumed to be 1500 µm, as described by Duke Elder - although with the caveat that the correct value was probably 1800–1900 µm. The diameter of the disc was thought to be a clinically useful unit, which led to its adoption as a standard measure. However, several large, carefully done epidemiological studies subsequently published data demonstrating that the more accurate dimensions of the average disc were in the 1.8–1.9 mm range.14 In this study, because the standard DD was based upon a sized overlay and the image magnification could be assumed to be uniform, the actual measurement of lesions using DD and DA was unaffected. In the current era, modern digital fundus cameras implement the assumption that 1 DD = 1800 µm and 1 DA = 2.54 mm2 on the retina. In LSOCA, DD and DA continue to be used to maintain continuity with historic data and reports.
Progression of CMVR is defined in SOCA as (1) extension of an existing CMV retinitis lesion by 1/2 DD over a front 1/2 DD wide or (2) onset of a new CMV retinitis lesion at least ¼ DA in area (a circle with diameter of 1/2 DD).15 When these distances and areas, are expressed in metric units, one must be careful to understand whether the underlying data (which are uniformly denominated) are being expressed with the assumption that ½ DD = 750µm by historical practice, or that ½ DD = 900µm by modern practice). An advantage of digital imaging over film for pan-retinal imaging is the ability to easily manipulate the nine fields of the photograph and to retinotopically align them for measurement by planimetry. Mosaic images often exhibit a radial distortion due to the curvature of the ocular fundus similar to the problem cartographers encounter when transferring the globe-shaped earth onto a two dimensional map. For accurate and reliable evaluation over time, it is very important to have consistent images of retinal morphology between visits. Automated mosaic with smoothing and blending functions may generate dissimilar retinal images at each visit owing to variable photographic qualities, which would increase grading noise. Therefore, we employed a mosaic method to allow a composite view of the retina without manipulating the photographic information, to be suitable for longitudinal clinical studies. The manual construction of a quasi-mosaic (through juxtaposition of the images handled as different layers) minimizes cartographic distortion.
Limitations of the study are the small cross-sectional dataset, absence of active CMV retinitis and the possible bias in selection of subjects. Subjects were selected based on their willingness to undergo two sets of photographs, and no other selection criteria was imposed. The sample is representative of the LSOCA cohort, with only a third of the patients presenting with CMV retinitis and very low rates of active CMV retinitis since the start of the HAART regimen.
Conclusion
Digital mosaic grading for LSOCA is comparable to film grading, ensuring continuity of grading data in the transition from film to digital photography. Availability of digital measuring tools enhances the efficiency and accuracy of grading. Using disc areas and disc diameters as the unit of measurement standardizes the differences between older data collected on film and newer digital photographic data.
Summary statement.
Transition to digital grading preserves continuity with historical data sets and allows ongoing longitudinal assessment of CMV retinitis. Efficiencies are gained in workflow and grading methodology due to the use of digital tools.
Acknowledgments
Financial support: Supported by cooperative agreements from the National Eye Institute, the National Institutes of Health, Bethesda, MD to the Mount Sinai School of Medicine, New York, NY (U10 EY08052); the Johns Hopkins University Bloomberg School of Public Health, Baltimore, MD (U10 EY08057); and the University of Wisconsin, Madison, Madison, WI (U10 EY08067).
Footnotes
Conflict of interest: None of the authors have any conflict of interest pertinent to this 16 manuscript.
References
- 1.Studies of ocular complications of AIDS Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial: 1. Rationale, design, and methods. AIDS Clinical Trials Group (ACTG) Control Clin Trials. 1992 Feb;13(1):22–39. doi: 10.1016/0197-2456(92)90027-w. [DOI] [PubMed] [Google Scholar]
- 2.Ferris FL, III, Hubbard LD. Digital Color Retinal Imagin. 2009 Spring;31:1–6. [Google Scholar]
- 3.Tennant MT, Greve MD, Rudnisky CJ, Hillson TR, Hinz BJ. Identification of diabetic retinopathy by stereoscopic digital imaging via teleophthalmology: a comparison to slide film. Can J Ophthalmol. 2001 Jun;36(4):187–196. doi: 10.1016/s0008-4182(01)80039-9. [DOI] [PubMed] [Google Scholar]
- 4.Tyler ME, Hubbard LD, Boydston K, Pugliese AJ. Characteristics of Digital Fundus Camera Systems Affecting Tonal Resolution in Color Retinal Images. 2009 Spring;31:1–9. [Google Scholar]
- 5.Hubbard LD, Danis RP, Neider MW, Thayer DW, Wabers HD, White JK, Pugliese AJ, Pugliese MF. Age-Related Eye Disease 2 Research Group. Brightness, contrast, and color balance of digital versus film retinal images in the age-related eye disease study 2. Invest Ophthalmol Vis Sci. 2008 Aug;49(8):3269–3282. doi: 10.1167/iovs.07-1267. [DOI] [PubMed] [Google Scholar]
- 6.Studies of the Ocular Complications of AIDS Research Group. SOCA cytomegalovirus retinitis grading protocol. 1997. Available from the National Technical Information Services, US Department of Commerce, 5285 Port Royal Road, Springfield, VA 22161L NTIS accession no. PB97-192082) [Google Scholar]
- 7.Holland GN, Buhles WC, Jr, Mastre B, Kaplan HJ. A controlled retrospective study of ganciclovir treatment for cytomegalovirus retinopathy. Use of a standardized system for the assessment of disease outcome. UCLA CMV Retinopathy. Study Group. Arch Ophthalmol. 1989 Dec;107(12):1759–1766. doi: 10.1001/archopht.1989.01070020841024. [DOI] [PubMed] [Google Scholar]
- 8.Curcio CA, Allen KA. Topography of ganglion cells in human retina. J Comp Neurol. 1990 Oct 1;300(1):5–25. doi: 10.1002/cne.903000103. [DOI] [PubMed] [Google Scholar]
- 9.Somani R, Tennant M, Rudnisky C, Weis E, Ting A, Eppler J, Greve M, Hinz B, de Leon A. Comparison of stereoscopic digital imaging and slide film photography in the identification of macular degeneration. Can J Ophthalmol. 2005 Jun;40(3):293–302. doi: 10.1016/S0008-4182(05)80072-9. [DOI] [PubMed] [Google Scholar]
- 10.Rudnisky CJ, Tennant MT, Weis E, Ting A, Hinz BJ, Greve MD. Web-based grading of compressed stereoscopic digital photography versus standard slide film photography for the diagnosis of diabetic retinopathy. Ophthalmology. 2007 Sep;114(9):1748–1754. doi: 10.1016/j.ophtha.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 11.Prasad S, Bannon P, Clearkin LG, Phillips RP. Digital fundus imaging: a quality and cost comparison with 35-mm film. Acta Ophthalmol Scand. 1999 Feb;77(1):79–82. doi: 10.1034/j.1600-0420.1999.770118.x. [DOI] [PubMed] [Google Scholar]
- 12.Flores-Aguilar M, Munguia D, Besen G, Gangan P, Arevalo JF, Freeman WR. Clinical versus fundus photographic evaluation of the status of cytomegalovirus retinitis in AIDS patients. Retina. 1996;16(5):363–372. doi: 10.1097/00006982-199616050-00001. [DOI] [PubMed] [Google Scholar]
- 13.Weinberg DV, Holbrook JT, Hubbard LD, Davis MD, Jabs DA, Holland GN. Studies of Ocular Complications of AIDS Research Group. Clinician versus reading center assessment of cytomegalovirus retinitis lesion size. Ophthalmology. 2005 Apr;112(4):559–566. doi: 10.1016/j.ophtha.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 14.Jonas JB, Gusek GC, Naumann GOH. Optic disc, cup and neuroretinal rim size, configuration, and correlations in normal eyes. Invest Ophthalmol Vis Sci. 1988;29:1151–1158. Correction: Invest Ophthalmol Vis Sci 1991. [PubMed] [Google Scholar]
- 15.Enger C, Jabs DA, Dunn JP, Forman MS, Bressler NM, Margolick JB, Charache P. Viral resistance and CMV retinitis: design and methods of a prospective study. CRVR Research Groups. Cytomegalovirus Retinitis Viral Resistance Research Group. Ophthalmic Epidemiol. 1997 Mar;4(1):41–48. doi: 10.3109/09286589709058060. [DOI] [PubMed] [Google Scholar]