Abstract
The US population of cancer survivors age ≥ 65 years will continue to grow rapidly over the next few decades. This growth will be driven largely by the aging of the national population. With the diffusion of earlier detection and more effective therapies, the majority of these individuals can expect to live long term after diagnosis. This often vulnerable group of survivors poses significant challenges for both researchers and clinicians with regard to how best to document and address its unique health care needs. In this article, we briefly review the long-term and late-occurring effects of cancer and its treatment in older survivors, review information on current patterns of post-treatment care and the evolving guidelines for this care, and discuss opportunities for future research.
INTRODUCTION
The next two decades will see an unprecedented increase in the number of older cancer survivors—individuals age ≥ 65 years diagnosed or living with a history of cancer. This expected rise in the prevalent population will be a function of the aging of the US (as well as global) population and the trend toward increasing lifespan, coupled with broader dissemination of advances in early detection of cancer and its treatment as well as improvements in supportive care. Although understanding better how to treat older adults with cancer is critical as the number of older survivors continues to grow, a rapidly emerging challenge is how best to care for these individuals after treatment ends. In this article, we provide information on the prevalence of older adult survivors in the United States, briefly outline some of the more common long-term and late psychosocial and health-related consequences they may face after cancer, review information on current patterns of post-treatment care and the evolving guidelines for this care, and discuss opportunities for future research.
Magnitude of the Challenge
Because cancer is a disease associated with aging, the aging of the US population has profound implications for the number of anticipated cancer survivors in the decades to come. As of January 2012, an estimated 8,016,226 cancer survivors—or 59% of the prevalent population of cancer survivors—was age ≥ 65 years. By 2030, it is estimated that 19.3% of the population will be age ≥ 65 years. Furthermore, it is expected that by 2050, 19 million people will be age ≥ 85 years (so-called oldest old), up from only 5.7 million in 2008.1 At the same time, length of survival from cancer is steadily increasing. In the most recently published figures, an estimated 64% of survivors had been diagnosed ≥ 5 years earlier, and roughly 15% represented survivors whose cancer was diagnosed ≥ 20 years earlier.2 The consequence of these two trends—the aging of the nation and longer expected cancer survival periods—is that by the year 2020, two thirds of all cancer survivors will be age ≥ 65 years1 (Fig 1). As illustrated in Figure 2, most of these older adults, men and women alike, will have survived ≥ 5 years beyond a cancer diagnosis. Thus, as articulated across the articles in the special issue of Journal of Clinical Oncology (JCO), developing a better understanding of and better managing the treatment and care of older adult survivors will present key challenges for oncology research and practice.
Fig 1.
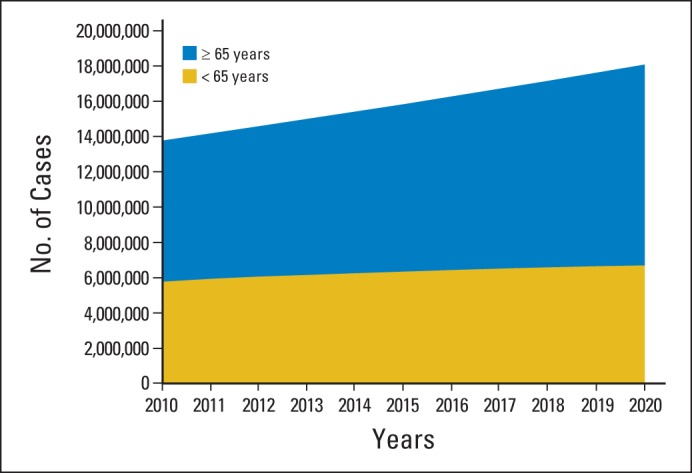
Estimated number of persons with history of cancer from 1971 to 2008, by age group, projected through the year 2030. Data adapted.1
Fig 2.
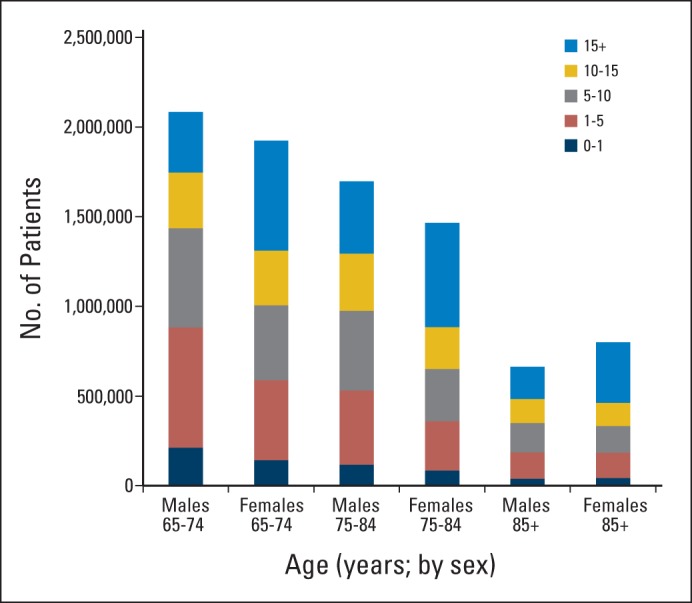
2014 prevalence by age, sex, and duration among cancer survivors age ≥ 65 years. Prevalence was projected for 2014 using SEER data and applying Prevalence Incidence Approach Model, a method that calculates prevalence from cancer incidence, cancer survival, and all-cause mortality.
Comparative studies suggest that older survivors manifest better psychosocial adaptation to cancer than younger survivors.3–5 This may be explained in part by a tendency for older adults to frame the cancer experience differently from younger persons. That is, aging in and of itself often presents a set of challenges to adults, and for some, cancer may be one of several competing health and life demands to which they must adapt and adjust. With aging, most people will experience and have to cope with illness or trauma of one kind or another. At the same time, however, older adults are at greater risk for physical limitations as a result of a higher likelihood of pre-existing, comorbid health conditions that may be exacerbated by or compromise cancer care.6–8 As many as 80% of older adults have one comorbid condition, and 50% have ≥ two.9,10 Older data suggest that when compared with their peers without a history of cancer, cancer survivors report more functional limitations, even when controlling for the number of comorbid conditions.11 More recent data identify some late physical health effects of cancer and its treatment that are clinically important in older adults, including cancer-related fatigue12; cognitive function decrements (described in greater detail by Mandelblatt et al13 in JCO); chemotherapy-induced peripheral neuropathy, which is particularly problematic for older patients with gait instability14; and bone-health issues such as those observed in postmenopausal women treated with aromatase inhibitors for breast cancer15 as well as in older men with prostate cancer exposed to androgen-suppression therapy.16 The interplay between cancer treatment–related health effects and normative age-related health issues presents significant challenges for survivorship care. Emerging evidence shows that exercise interventions in older adult survivors can be safe and beneficial for reducing risk or controlling functional decline, bone health, and cancer-related fatigue. Furthermore, observational studies suggest that physical activity may also prolong survival.17–21
Among the preexisting conditions that an older person may have is a prior history of cancer. An estimated 8% of the prevalent population has had > one cancer, and among all newly diagnosed patients with cancer, 16% have a history of cancer.22 This latter figure is lower in younger patients (< 1% in those diagnosed at age ≤ 19 years), because prevalence of multiple malignancies increases with age. By age 60 to 69 years, this figure is 7%; by age 70 to 79 years, it is 10%; and by age ≥ 80 years, it increases to 12.1%.23 To date, little research has been conducted on the segment of the population with multiple cancers.
Survivorship Care After Cancer
Several national reports are credited with promoting broader recognition of the unique needs that cancer survivors have after completing treatment. These include the President's Cancer Panel report, “Living Beyond Cancer,”24 and the Institute of Medicine (IOM) reports, “From Cancer Patient to Cancer Survivor: Lost in Transition”25 and “Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs.”26 Efforts by the clinical community to address the recommendations in each of these reports have led to several important initiatives. One of these was the creation of the Cancer Survivorship Committee within the American Society of Clinical Oncology (ASCO).27 The Cancer Survivorship Committee is working systematically to identify extant guidelines for addressing specific aspects of survivors' post-treatment care and to develop new guidelines as needed. To date, this includes recommendations for managing anxiety and depression, fatigue, and chemotherapy-induced peripheral neuropathy.28–30 Working in parallel, the National Comprehensive Cancer Network has released survivorship guidelines for selected cancers.31 It is important to note that none of these guidelines specifically addresses care of older survivors. Another larger effort, spurred mainly by the advocacy community, is a push to develop and deliver treatment summaries (TSs) and survivorship care plans (SCPs), documents meant to be shared with all survivors and primary care providers (PCPs) in making the transition from active patient to recovery.32 The components of these, originally detailed in the President's Cancer Panel report24 and later adapted for inclusion in the IOM's “Lost in Transition” report,25 are summarized in Tables 1 and 2.
Table 1.
Treatment Summary Elements
| Element |
|---|
| Diagnostic tests performed and results |
| Tumor characteristics (eg, site, stage and grade, hormone receptor status, marker information) |
| Dates of treatment initiation and completion |
| Surgery, chemotherapy, radiotherapy, transplantation, hormonal therapy, genetic therapy, or other therapies provided, including agents used, treatment regimens, total dosage, identifying No. and title of clinical trials (if any), indicators of treatment response, and toxicities experienced during treatment |
| Psychosocial, nutritional, and other supportive services provided |
| Full contact information for treating institutions and key individual providers |
NOTE. Data adapted.24
Table 2.
Survivorship Care Plan Key Domains
| Domain |
|---|
| Surveillance for recurrence or new cancer |
| Assessment and treatment or referral for persistent effects, including psychosocial and economic as well as physical (eg, pain, fatigue, sexual dysfunction, functional impairment, depression, employment issues) |
| Evaluation of risk for and prevention of late effects (eg, second cancers, cardiac problems, thyroid disorders, osteoporosis) and health promotion (lifestyle interventions: diet, weight control, physical activity, sunscreen use, alcohol control, smoking cessation) |
| Coordination of care (eg, frequency of visits, tests to be performed, who performs tests) |
NOTE. Data adapted.25
Intended to facilitate survivorship care planning, coordination, and communication, interest in using TSs and SCPs has grown. In 2008, ASCO added two elements—the development of and delivery of TS documents to patients and their providers—as part of its core Quality Oncology Practice Initiative quality measures. More recently, the American College of Surgeons Commission on Cancer mandated that by 2015, hospitals seeking Commission on Cancer accreditation must be able to show that they are using TSs and SCPs.33 This lofty goal notwithstanding, because of the fragmented way in which cancer care is delivered in the United States and the lack of integrated electronic databases, generating the information needed to populate a TS and SCP is challenging. Furthermore, almost no data exist to show that using these documents has an impact on either the care received or patient outcomes.34 Indeed, the one study published to date shows little benefit to patients in levels of distress, patient satisfaction, or general health status35; however, the study was conducted among breast cancer survivors of higher socioeconomic status in Canada, a country with universal health care, and did not assess adherence to follow-up care guidelines.
As outlined in Table 3, there is potential for TSs and SCPs to positively affect outcomes on many levels—from survivors' knowledge, function, and health to clinicians' knowledge and behaviors to system-level efficiencies and cost reduction. Critically important, although sometimes forgotten in the pressure to generate them, is recognizing that SCPs fundamentally are tools that must be part of a dynamic conversation between patients and their health care providers that may include education, motivation, and a mechanism for increasing adherence to the SCP. In this context, determining when best to have this dialogue and who should be responsible for initiating it (eg, oncologist, nurse, special survivorship navigator) are questions that remain to be answered.34,36 To address this knowledge gap, the National Cancer Institute (NCI) has two program announcements designed to solicit research on the impact of survivorship care planning on multilevel outcomes (PA-12-274 [R21s], PA-12-275 [R01s]). Applications from those caring for older adult survivors regarding how best to facilitate these care transitions would be particularly welcome.
Table 3.
Evaluating Impact of Survivorship Care Planning: Metrics for Success
| Metric |
|---|
| Survivor level |
| Improved (perceived) patient-physician communication |
| Improved understanding of needed follow-up tests, their purpose and timing, and who will conduct them |
| Better understanding of potential late effects of illness and what symptoms might be important to report |
| Better adherence to recommended follow-up activities; fewer requests for unnecessary tests |
| Improved ability to identify providers and resources to address persistent effects of cancer and its treatment |
| Decreased cancer-related morbidity |
| Improved health-related quality of life and function |
| Improved healthy lifestyle choices |
| Potentially improved overall survival |
| Clinician level |
| Improved (perceived) patient-physician communication |
| Improved physician-physician communication |
| Better ability to coordinate care |
| Improved knowledge about and ultimately standardization of follow-up care behaviors |
| Improved ability to monitor survivors' health and implement changes in care in response to new information about treatment exposures and follow-up needs |
| System level |
| Reduced duplication of services |
| Improved access to information necessary to guide follow-up care; less time spent searching for this |
| Enhanced quality of care delivery (eg, compliance with evolving quality standards) |
NOTE. Data adapted.36
In their study, Salz et al37 found that despite the favorable view of SCPs expressed by both providers and survivors, fewer than half (43%) of the 53 NCI-designated comprehensive cancer centers surveyed provided SCPs; of documents provided, none included all of the recommended IOM elements. Data from a large (N = 1,345) national survey of cancer survivors found similarly low rates of TS provision; even among those recently treated, only 38% reported TS receipt, although 58% reported receiving written instructions about follow-up care after cancer.38 The challenges at the community level (where most older survivors are treated) of delivering SCPs are well articulated by members of the NCI Community Cancer Centers Program sites.39 Table 4 lists some of these challenges and potential solutions.
Table 4.
Barriers to Survivorship Treatment Summary and Care Plan Implementation: Community-Based Perspective
| Barrier | Strategies to Overcome Barrier |
|---|---|
| Time constraints | |
| Time intensive to gather data and complete form | Use tumor registry data to populate form |
| Time span (lag) between patient completing therapy and tumor registry abstracting data | Purchase commercially available software product to electronically populate fields Implement RQRS in tumor registry to provide more timely data abstraction |
| Information technology | |
| Manually populated forms versus documents automatically populated from EHRs | Nurse navigators/nurse practitioners manually populate forms (many standard templates available online) |
| Lack of shared EHRs between cancer centers and private practice physician offices | Purchase software for shared EHRs between cancer centers and private practice physician offices |
| Poor access to private practice medical records | Use (expand upon) existing processes for communicating and requesting information from private practice staff |
| Establish agreements for access to private practice medical records | |
| Processes and responsibilities | |
| For which patients are treatment summaries appropriate? | Obtain feedback from multidisciplinary teams to identify survivor populations on which to focus for initial implementation |
| When additional treatment is received, how are updates made to the summary? | Establish survivorship clinics |
| Care plan recommendations | |
| Lack of standards for adult cancer survivorship surveillance | Collaborate with multidisciplinary team members to establish follow-up surveillance (and care) recommendations based on ASCO, NCCN, and other professional guidelines |
NOTE. Data adapted.39
Abbreviations: ASCO, American Society of Clinical Oncology; EHR, electronic health record; NCCN, National Comprehensive Cancer Network; RQRS, rapid quality reporting system.
It is important to note that to date, research on SCP adoption does not specifically target the use of these documents in an older population. It is expected that important modifications to this process might be needed when used with older cohorts of survivors and their families. First, consideration may need to be given to the format used in sharing information. Some studies are piloting the use of flash drives or Web-based platforms to share TSs and SCPs. For older adults with restricted computer savvy, this format may not be as acceptable or familiar. Furthermore, it is important to ensure that the type font used in any written document intended for older readers is large enough to be read easily. Although subsequent generations of older survivors will have higher educational attainment, being sensitive to the reading level of today's heterogeneous older survivors may also need to be considered in SCP development.
Second, assessment of persistent and coexisting health problems, an element of the SCP process (Table 2), may need to be tailored for older adults. Inclusion of the geriatric depression scale to assess affect should be considered, along with potential inclusion of a full geriatric assessment at the end of treatment. Also, older adults typically see numerous specialists in addition to their PCP, and it is essential that SCPs be given to all providers because of the complexity of the conditions that many older adults have.
Third, because family caregivers play an integral part in cancer survivors' care—particularly for older survivors who often have more health care–related needs to begin with—it is important to include them in the survivorship care planning process. Note, however, that this has inherent challenges. Older survivors often have older caregivers (generally spouses) who themselves may have health problems. Determining what a caregiver may or may not be able to do in support of a survivor's post-treatment care and identifying others who can help will be necessary.
Fourth, because the population of survivors, including older survivors, is expected to become more diverse over the next two decades,10 ensuring that staff are trained to provide education that is culturally relevant and to deliver survivorship care in a culturally sensitive fashion will be vital. To date, studies conducted among diverse populations of older cancer survivors are lacking. If we are to provide care that is tailored to a truly multicultural and heterogeneous population, it will be important to include diverse participants based on race, ethnicity, socioeconomic status, sexual orientation, geographic location, and disability in future research. Finally, and a corollary to the last point, care must be taken in identifying the appropriate individuals to deliver post-treatment medical as well as psychosocial care and monitoring in older populations. Assignment of responsibility for these roles continues to be a source of debate.40 The use of geriatric nurses and providers who generally have a more thorough and complete understanding of their patients' comorbid health profile, medication use, and support system might be most appropriate.
One of the current debates in oncology focuses on who should handle follow-up in the growing population of cancer survivors. The deepening shortage of medical oncologists and geriatricians places practical limits on most practitioners as to whom they have time to see in their respective practices.41,42 There are, however, other reasons to look elsewhere for this care. Research suggests that the current model, in which survivors are seen by treating oncologists, may result in missed opportunities to optimize their general health.43 Furthermore, most older adults have an identified PCP who already is familiar with their health status and function.44 Given that most older adult cancer survivors will likely die as a result of something other than their cancer45 and, as noted earlier, are at increased risk for other complicating chronic health conditions, a strong case can be made for trying to return these individuals to their PCP after treatment, with a care plan delineating what cancer-specific follow-up is most appropriate. Finally, the new focus on health span, not simply lifespan, is drawing greater attention to the role of disease prevention (eg, smoking cessation, weight management, use of vaccines and flu shots) and better management of chronic conditions (eg, optimal control of hypertension, arthritis, diabetes, chronic obstructive pulmonary disease) across the lifespan, both the purviews of primary and specialty care providers.46 Despite these compelling arguments and the pressing need to identify optimal post-treatment care pathways, no consensus about the preferred model of follow-up care is as yet apparent for any age group, much less older survivors. Moreover, given the health complexities of the aging population, it is clear that post-treatment care for older cancer survivors will require multidisciplinary teams.44
Studies conducted in the United Kingdom and Canada have demonstrated that PCPs can safely provide cancer follow-up care for early-stage breast cancer survivors.47,48 However, US breast cancer survivors are more doubtful. They worry that their PCP may be less knowledgeable about monitoring for a recurrence or treating persistent or late-occurring effects of cancer.49 Studies among physician groups indicate that medical oncologists share patients' concerns about PCPs' ability to manage cancer follow-up, and PCPs themselves are anxious about their own skills in this domain.50,51 Factors that contribute to PCPs being more comfortable with providing cancer-related follow-up care include more training in the long-term and late effects of cancer, higher volume of patients with cancer, and receipt of treatment summaries from oncologists.51 Some have proposed that a shared care model may work best.52,53 In the study by Klabunde et al,51 preference for a shared model of survivorship care was associated with comanagement of care by PCPs for both medical oncologists and PCPs. In the United Kingdom, a model is being tested in which cancer survivors are triaged to more intensive, oncology-based (v less intensive, PCP-based) care depending on the seriousness of the disease and associated complications of treatment.54
Future Challenges and Opportunities
The many unanswered questions about how best to deliver optimal post-treatment care to all cancer survivors, and to older cancer survivors in particular, pose a significant challenge for oncology. Indeed, how we will effectively manage the growing population of older adults with cancer is a theme that runs throughout the 2014 IOM report, “Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis.”55 At the same time, this situation presents unique opportunities to conduct novel research and have an impact on reducing the national burden of cancer.
National Investment in Cancer and Aging Research
Expanding our investment in research being conducted among older cancer survivors will be an important first step in addressing the gaps in our knowledge base. Although this includes (as highlighted elsewhere in the special JCO issue) increasing treatment trials for those age ≥ 65 years, it also means eliciting and supporting research to examine the health and functional outcomes of older adults living beyond cancer, along with those of their caregivers, and interventions to optimize these outcomes. Current estimates suggest that although 78% of NCI-funded research examining post-treatment outcomes among cancer survivors includes those age ≥ 65 years, fewer than 4% of these studies focus on this population specifically.56 It is not entirely clear why this is the case, given the prevalence of older survivors, and notwithstanding the fact that NCI has a dedicated Office of Cancer Survivorship and language in all of the parent funding mechanisms to invite applications that identify and address all survivors' needs (eg, PA-13-302 [R01], PA-13-146 [R21], PA-14-007[R03]). One factor may be less willingness among members of this group to engage in research, in some cases because of ill health.57,58 Additional barriers may be that these individuals are seen and treated more often in the community, whereas most funded survivorship studies include survivors treated at large cancer centers, where the average age of treated patients is younger. Furthermore, data collection tools may be poorly suited to older age groups because of their small font/print size, complex language, inclusion of questions that are not relevant to older adult concerns, and reliance on written versus in-person interview information capture.59 The large number of studies conducted among breast cancer survivors (which generally include samples with lower mean age) versus those with lung, colorectal, or prostate cancer likely also contributes to the relative lack of information about older adult survivorship experiences. Deliberate efforts to design data collection tools and strategies that efficiently and effectively capture relevant information and to recruit and retain samples of older adult survivors will be needed to rectify this situation. As argued elsewhere,59 increasing our investment in and attention to older adults with cancer should include not only a top-down approach (focusing on funding agencies) but also a bottom-up approach leveraging the voice of large health and aging-related organizations, including the American Association of Retired Persons. Engaging these organizations and working with their members may play a key and creative role in accruing this difficult-to-reach population.
The growing attention being paid to understanding the interface between cancer and chronic illness is expected to spur efforts in this regard.60 The creation in 2012 of a trans–National Institutes of Health (NIH) special interest group, the Geroscience Interest Group (GSIG), may help to address the issues that exist at the federal level with respect to consideration and funding of research that cuts across disease types. The goals of GSIG are four-fold: (1) to raise awareness, both within and outside the NIH, of the relevant role played by aging biology in the development of age-related chronic disease; (2) to promote the coordination of activities within NIH relating to the specific needs of the research community; (3) to develop public/private partnerships through interactions with scientific societies, industry, and other institutions with related interests; and (4) to develop trans-NIH initiatives to encourage research on the basic biology of aging and its relation to chronic diseases of the elderly. In the first summit sponsored by GSIG, researchers examined shared mechanisms and pathways that may underlie a host of chronic illnesses, including cancer.61 Insight into shared mechanisms may help us to better understand not only cancer onset and progression processes but also fundamental pathways to slow normal aging.
Cancer and Aging Interface
As highlighted earlier, cancer is commonly one of several competing health conditions with which older adults must contend. The extent to which health problems resulting from cancer and its treatment are a function of and/or exacerbated by coexisting medical conditions is unclear, nor is it clear what influence this interaction may have on subsequent rates of morbidity or mortality.62 Moreover, the extent to which cancer and its treatment influences post-treatment aging processes, including but not limited to cardiovascular performance and respiratory capacity and visual and hearing problems, has received little attention.63 Although initially illustrated in research conducted among younger cancer survivor cohorts64,65 and recently hinted at among young-adult survivors,66,67 it is not clear if this process or risk also affects those diagnosed later in life with cancer. To advance work at this interface, efforts will be needed to foster greater dialogue between oncology and geriatric specialists and to promote cross-training of clinical researchers in both of these fields, a challenge that could be met in part with greater use by investigators of various NCI training mechanisms.
Models of Care
In addition to the issues raised earlier, questions remain to be explored regarding optimal models of care for older adult survivors. These include determining what older survivors should (and can) manage with respect their post-treatment care if we are to adopt, as many propose, a chronic disease management model for survivorship care. A related question is what role caregivers might play in such a model. We know that cancer affects the whole family and not only the survivor.68,69 This is particularly true for older survivors, for whom family support may be vital, even before a diagnosis; this support becomes more so after treatment ends. Caregivers need information regarding what recovery will look like, how to carry out expected tasks (eg, help with medical appliances, administering medications, monitoring symptoms), juggle competing demands (children, work), and simultaneously address their own physical and emotional health issues.68 Too often, however, caregivers are left out of these transition conversations, or their concerns are not specifically addressed. Even if not included in the potential outcomes of successful care planning outlined in Table 3, caregivers could well benefit from active inclusion in the care-planning process. As with care recipients, thoughtful care planning that includes the key caregiver has the potential to improve the caregiver's knowledge of the long-term and late effects of cancer in his or her loved one; awareness of appropriate follow-up practices that he or she could support; recognition of the importance of a healthy lifestyle, an understanding that might affect his or her own behavior70; sense of competency or self-efficacy in helping a loved one make the transition to life after cancer; and overall quality of life by reducing the stress over how best to provide ongoing care. Testing different models of survivorship care for our oldest survivors (shared care, PCP only, survivorship clinics, more or less intensive follow-up regimens) will be critical if we are to contain the spiraling health care costs we face in the future.
On a final note, it is clear that advancing our capacity to care for the burgeoning population of older and, in increasing numbers, elderly cancer survivors will take a certain level of both personal and political will. In this vein, it should be remembered that counted among these survivors are the baby boomers, many of whom came of age during a period that encompassed the civil rights movement, women's liberation, war protests, AIDS advocacy, and strong consumerist activity. Some of these same—now older adult—individuals are already active constituents of large cancer advocacy groups: National Breast Cancer Coalition, Us TOO, Colon Cancer Alliance, Lung Cancer Alliance, and Bladder Cancer Action Network. It is not likely that given this legacy, this group will rest easy with things as they are, specifically with cancer care that continues to be poorly coordinated, is of inconsistent and at times questionable quality, and is increasingly expensive. Tolerance will also be limited for care that is not patient centered, taking into consideration each patient's hopes, values, and personal experience. With this in mind, clinicians and researchers should consider the powerful ally they have in survivors themselves in seeking the support and resources at all levels (ie, institutional, community, state, national) needed to advance quality survivorship care.
Acknowledgment
We thank Marcia Feinleib and Joanne Brodsky for their timely and efficient assistance in the production of this article. We also thank Angela Mariotto, PhD, from the Data Modeling Branch of the Surveillance Research Program at the National Cancer Institute.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the official position of the National Institutes of Health or the National Cancer Institute.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: All authors
Administrative support: Julia H. Rowland
Collection and assembly of data: Julia H. Rowland
Manuscript writing: All authors
Final approval of manuscript: All authors
REFERENCES
- 1.Parry C, Kent EE, Mariotto AB, et al. Cancer survivors: A booming population. Cancer Epidemiol Biomarkers Prev. 2011;20:1996–2005. doi: 10.1158/1055-9965.EPI-11-0729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Moor JS, Mariotto AB, Parry C, et al. Cancer survivors in the United States: Prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013;22:561–570. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bellizzi KM, Rowland JH. Role of comorbidity, symptoms and age in the health of older survivors following treatment for cancer. Aging Health. 2007;3:625–635. [Google Scholar]
- 4.Weaver KE, Forsythe LP, Reeve BB, et al. Mental and physical health-related quality of life among U.S. cancer survivors: Population estimates from the 2010 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2012;21:2108–2117. doi: 10.1158/1055-9965.EPI-12-0740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clough-Gorr KM, Ganz PA, Silliman RA. Older breast cancer survivors: Factors associated with change in emotional well-being. J Clin Oncol. 2007;25:1334–1340. doi: 10.1200/JCO.2006.09.8665. [DOI] [PubMed] [Google Scholar]
- 6.Keating NL, Nørredam M, Landrum MB, et al. Physical and mental health status of older long-term cancer survivors. J Am Geriatr Soc. 2005;53:2145–2152. doi: 10.1111/j.1532-5415.2005.00507.x. [DOI] [PubMed] [Google Scholar]
- 7.Koroukian SM, Murray P, Madigan E. Comorbidity, disability, and geriatric syndromes in elderly cancer patients receiving home health care. J Clin Oncol. 2006;24:2304–2310. doi: 10.1200/JCO.2005.03.1567. [DOI] [PubMed] [Google Scholar]
- 8.Mohile SG, Xian Y, Dale W, et al. Association of a cancer diagnosis with vulnerability and frailty in older Medicare beneficiaries. J Natl Cancer Inst. 2009;101:1206–1215. doi: 10.1093/jnci/djp239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Healthy Aging at a Glance, 2011. http://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/2011/healthy_aging_aag_508.pdf.
- 10.Centers for Disease Control and Prevention. The State of Aging and Health in America, 2013. http://www.cdc.gov/features/agingandhealth/state_of_aging_and_health_in_america_2013.pdf.
- 11.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: Age, health and disability. J Gerontol A Biol Sci Med Sci. 2003;58:82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 12.Diemling GT, Bowman KF, Wagner LJ. The effects of cancer-related pain and fatigue on functioning on older adult, long-term cancer survivors. Cancer Nurs. 2007;30:421–433. doi: 10.1097/01.NCC.0000300168.88089.2b. [DOI] [PubMed] [Google Scholar]
- 13.Mandelblatt JS, Jacobsen PB, Ahles T. Cognitive effects of cancer systemic therapy: Implications for the care of older patients and survivors. J Clin Oncol. 2014;32:2617–2626. doi: 10.1200/JCO.2014.55.1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stubblefield MD, Burnstein HJ, Burton AW, et al. NCCN task force report: Management of neuropathy in cancer. J Natl Compr Canc Netw. 2009;7(suppl 5):S1–S26. doi: 10.6004/jnccn.2009.0078. [DOI] [PubMed] [Google Scholar]
- 15.Choksi P, Williams M, Clark PM, et al. Skeletal manifestations of treatment of breast cancer. Curr Osteoporos Rep. 2013;11:319–328. doi: 10.1007/s11914-013-0179-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sountoulides P, Rountus T. Adverse effects of androgen deprivation therapy for prostate cancer: Prevention and management. ISRN Urol. 2013;2013:240108. doi: 10.1155/2013/240108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blair CK, Morey MC, Desmond RA, et al. Light-intensity activity attenuates functional decline in older cancer survivors. Med Sci Sports Exerc. 2014;46:1375–1383. doi: 10.1249/MSS.0000000000000241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Winters-Stone KM, Leo MC, Schwartz A. Exercise effects on hip bone mineral density in older, post-menopausal breast cancer survivors are age dependent. Arch Osteoporos. 2012;7:301–306. doi: 10.1007/s11657-012-0071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown JC, Huedo-Medina TB, Pescatello LS, et al. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: A meta-analysis. Cancer Epidemiol Biomarkers Prev. 2011;20:123–133. doi: 10.1158/1055-9965.EPI-10-0988. [DOI] [PubMed] [Google Scholar]
- 20.Lee IM, Wolin KY, Freeman SE, et al. Physical activity and survival after cancer diagnosis in men. J Phys Act Health. 2014;11:85–90. doi: 10.1123/jpah.2011-0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner JR, Livingston PM, Fraser SF. Effects of exercise on treatment-related adverse effects for patients with prostate cancer receiving androgen-deprivation therapy: A systematic review. J Clin Oncol. 2014;32:335–346. doi: 10.1200/JCO.2013.49.5523. [DOI] [PubMed] [Google Scholar]
- 22.Mariotto AB, Rowland JH, Ries LAG, et al. Multiple cancer prevalence: A growing challenge in long-term survivorship. Cancer Epidemiol Biomarkers Prev. 2007;16:566–571. doi: 10.1158/1055-9965.EPI-06-0782. [DOI] [PubMed] [Google Scholar]
- 23.Yancik R, Ganz PA, Varricchio CG, et al. Perspectives on comorbidity and cancer in older patients: Approaches to expand the knowledge base. J Clin Oncol. 2001;19:1147–1151. doi: 10.1200/JCO.2001.19.4.1147. [DOI] [PubMed] [Google Scholar]
- 24.President's Cancer Panel. Living Beyond Cancer: Finding a New Balance. http://deainfo.nci.nih.gov/advisory/pcp/annualReports/pcp03-04rpt/Survivorship.pdf.
- 25.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 26.Adler NE, Page AEK, editors. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 27.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: Achieving high quality cancer survivorship care. J Clin Oncol. 2013;31:631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Andersen BL, DeRubeis RJ, Berman BS, et al. Screening, assessment, and care of anxiety and depressive symptoms in adults with cancer: An American Society of Clinical Oncology practice guideline adaptation. J Clin Oncol. 2014;32:1605–1619. doi: 10.1200/JCO.2013.52.4611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bower JE, Bak K, Berger A, et al. Screening, assessment and management of fatigue in adult survivors of cancer: An American Society of Clinical Oncology practice guideline adaptation. J Clin Oncol. 2014;32:1840–1850. doi: 10.1200/JCO.2013.53.4495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hershman DL, Lacchetti C, Dworkin RH, et al. Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: An American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2014;32:1941–1967. doi: 10.1200/JCO.2013.54.0914. [DOI] [PubMed] [Google Scholar]
- 31.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Survivorship—Version 1.2013. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 32.Hewitt ME, Ganz PA. Implementing Cancer Survivorship Care Planning: Workshop Summary. Washington, DC: National Academies Press; 2007. (rapporteurs) [Google Scholar]
- 33.Stricker CT, O'Brien M. Implementing the Commission on Cancer standards for survivorship care plans. Clin J Oncol Nurs. 2014;18(suppl):15–22. doi: 10.1188/14.CJON.S1.15-22. [DOI] [PubMed] [Google Scholar]
- 34.Parry C, Kent EE, Forsythe LP, et al. Can't see the forest for the care plan: A call to revisit the context of care planning. J Clin Oncol. 2013;31:2651–2653. doi: 10.1200/JCO.2012.48.4618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: Results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29:4755–4762. doi: 10.1200/JCO.2011.36.8373. [DOI] [PubMed] [Google Scholar]
- 36.Rowland JH, Ganz PA. Cancer survivorship plans: A paradigm shift in the delivery of quality cancer care. In: Feuerstein M, Ganz PA, editors. Health Services for Cancer Survivors: Policy, Practice and Research. New York, NY: Springer; 2011. pp. 169–185. [Google Scholar]
- 37.Salz T, Oeffinger KC, McCabe MS, et al. Survivorship care plans in research and practice. CA Cancer J Clin. 2012;62:101–117. doi: 10.3322/caac.20142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sabatino SA, Thompson TD, Smith JL, et al. Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: Results of a national survey. J Cancer Surviv. 2012;7:32–43. doi: 10.1007/s11764-012-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blaseg K, Kile M, Salner A. A Comprehensive Approach to a Survivorship Care Plan. http://ncccp.cancer.gov/files/NCCCP_SurvPalliativeCare.pdf.
- 40.Forsythe LP, Alfano CA, Leach CR, et al. Who provides psychosocial follow-up care for post-treatment cancer survivors? A survey of medical oncologists and primary care physicians. J Clin Oncol. 2012;30:2897–2905. doi: 10.1200/JCO.2011.39.9832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin J, Donehower RC. Make quality cancer survivorship care possible in the era of workforce shortage. J Oncol Pract. 2010;6:52–53. doi: 10.1200/JOP.091056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Geriatrics Society, Association of Directors of Geriatric Academic Programs. A clinical imperative for an aging population, part I. Ann Longterm Care. 2005;13:18–22. [Google Scholar]
- 43.Earle CC, Burstein JH, Winer EP, et al. Quality of non-breast cancer health maintenance among elderly breast cancer survivors. J Clin Oncol. 2003;21:1447–1451. doi: 10.1200/JCO.2003.03.060. [DOI] [PubMed] [Google Scholar]
- 44.Unroe KT, Cohen HJ. Multidisciplinary models of care. In: Bellizzi KM, Gosney MA, editors. Cancer and Aging Handbook: Research and Practice. Hoboken, New Jersey: Wiley Blackwell; 2012. pp. 487–497. [Google Scholar]
- 45.Mariotto AB, Wang Z, Klabunde C, et al. Life tables adjusted for comorbidity more accurately estimate noncancer survival for recently diagnosed cancer patients. J Clin Epidemiol. 2013;66:1376–1385. doi: 10.1016/j.jclinepi.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salomon JA, Wang H, Freeman MK, et al. Healthy life expectancy for 187 countries, 1990-2010: A systematic analysis of the global burden of disease. Lancet. 2012;380:2144–2162. doi: 10.1016/S0140-6736(12)61690-0. [DOI] [PubMed] [Google Scholar]
- 47.Grunfeld E, Mant D, Yudkin P, et al. Routine follow up of breast cancer in primary care: Randomised trial. BMJ. 1996;313:665–669. doi: 10.1136/bmj.313.7058.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grunfeld E, Levine MN, Julian JA, et al. Randomized trial of long-term follow-up for early-stage breast cancer: A comparison of family physician versus specialist care. J Clin Oncol. 2006;24:848–855. doi: 10.1200/JCO.2005.03.2235. [DOI] [PubMed] [Google Scholar]
- 49.Mao JJ, Bowman MA, Stricker CT, et al. Delivery of survivorship care by primary care physicians: The perspective of breast cancer patients. J Clin Oncol. 2009;27:933–938. doi: 10.1200/JCO.2008.18.0679. [DOI] [PubMed] [Google Scholar]
- 50.Forsythe LP, Parry C, Alfano CM, et al. Use of survivorship care plans in the United States: Associations with survivorship care. J Natl Cancer Inst. 2013;105:1579–1587. doi: 10.1093/jnci/djt258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Klabunde CN, Han PKJ, Carle CC, et al. Physician roles in the cancer-related follow-up care of cancer survivors. Fam Med. 2013;45:463–474. [PMC free article] [PubMed] [Google Scholar]
- 52.Oeffinger KC, McCabe MS. Models for delivering survivorship care. J Clin Oncol. 2006;24:5117–5124. doi: 10.1200/JCO.2006.07.0474. [DOI] [PubMed] [Google Scholar]
- 53.Grunfield E, Earle CC. The interface between primary and oncology specialty care: Treatment through survivorship. J Natl Cancer Inst Monogr. 2010;40:25–30. doi: 10.1093/jncimonographs/lgq002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jefford M, Rowland J, Grunfeld E, et al. Implementing improved post-treatment care for cancer survivors in England, with reflections for Australia, Canada and the USA. Br J Cancer. 2013;108:14–20. doi: 10.1038/bjc.2012.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Institute of Medicine: Delivering High Quality Cancer Care. Charting a New Course for a System in Crisis, 2014. http://books.nap.edu/openbook.php?record_id=18359. [PubMed]
- 56.National Cancer Institute, Office of Cancer Survivorship. FY2012 NIH-wide cancer survivorship research portfolio analysis
- 57.Carter WB, Elward K, Malmgren J, et al. Participation of older adults in health programs and research: A critical review of the literature. Gerontologist. 1991;31:584–592. doi: 10.1093/geront/31.5.584. [DOI] [PubMed] [Google Scholar]
- 58.Ford JG, Howerton MM, Lai GY, et al. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2008;112:228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- 59.Bellizzi KM, Mustian KM, Palesh OG, et al. Cancer survivorship and aging: Moving the science forward. Cancer. 2009;113:3530–3539. doi: 10.1002/cncr.23942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Edwards BK, Noone AM, Mariotto AB, et al. Annual report to the nation on the status of cancer, 1975-2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120:1290–1314. doi: 10.1002/cncr.28509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Burch JB, Augustine AD, Frieden LA, et al. Advances in geroscience: Impact on healthspan and chronic disease. J Gerontol A Biol Sci Med Sci. 2014;69:S1–S3. doi: 10.1093/gerona/glu041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meyerhardt JA, Catalano PJ, Haller DG, et al. Impact of diabetes mellitus on outcomes in patients with colon cancer. J Clin Oncol. 2003;21:433–440. doi: 10.1200/JCO.2003.07.125. [DOI] [PubMed] [Google Scholar]
- 63.Schmitz KH, Cappola AR, Stricker CT, et al. The intersection of cancer and aging: Establishing the need for breast cancer rehabilitation. Cancer Epidemiol Biomarkers Prev. 2007;16:866–872. doi: 10.1158/1055-9965.EPI-06-0980. [DOI] [PubMed] [Google Scholar]
- 64.Oeffinger KC, Meertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–1582. doi: 10.1056/NEJMsa060185. [DOI] [PubMed] [Google Scholar]
- 65.Ness KK, Krull KR, Jones KE, et al. Physiologic frailty as a sign of accelerated aging among adult survivors of childhood cancer: A report from the St Jude Lifetime cohort study. J Clin Oncol. 2013;31:4496–4503. doi: 10.1200/JCO.2013.52.2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Weaver KE, Foraker RE, Alfano CM, et al. Cardiovascular risk factors among long-term survivors of breast, prostate, colorectal and gynecologic cancers: A gap in survivorship care? J Cancer Surviv. 2013;7:253–261. doi: 10.1007/s11764-013-0267-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Koelwyn GJ, Khouri M, Mackey JR, et al. Running on empty: Cardiovascular reserve capacity and late effects of therapy in cancer survivorship. J Clin Oncol. 2012;30:4458–4461. doi: 10.1200/JCO.2012.44.0891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.van Ryn M, Sanders S, Kahn K, et al. Objective burden, resources, and other stressors among informal cancer caregivers: A hidden quality issue? Psychooncology. 2011;20:44–52. doi: 10.1002/pon.1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Anderson LA, Edwards VJ, Pearson WS, et al. Adult caregivers in the United States: Characteristics and differences in well-being by caregiver age and caregiving status. Prev Chronic Dis. 2013;10:E135. doi: 10.5888/pcd10.130090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Weaver KE, Rowland JH, Augustson E, et al. Smoking concordance in lung and colorectal cancer patient-caregiver dyads and quality of life. Cancer Epidemiol Biomarkers Prev. 2011;20:239–248. doi: 10.1158/1055-9965.EPI-10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]


