Abstract
Background
Surgeon-dependent factors such as optimal implant alignment are thought to play a significant role in outcome following primary total knee arthroplasty (TKA). Exact definitions and references for optimal alignment are, however, still being debated. This overview of the literature describes different definitions of component alignment following primary TKA for (1) tibiofemoral alignment in the AP plane, (2) tibial and femoral component placement in the AP plane, (3) tibial and femoral component placement in the sagittal plane, and (4) rotational alignment of tibial and femoral components and their role in outcome and implant survival.
Methods
We performed a literature search for original and review articles on implant positioning following primary TKA. Definitions for coronal, sagittal, and rotational placement of femoral and tibial components were summarized and the influence of positioning on survival and functional outcome was considered.
Results
Many definitions exist when evaluating placement of femoral and tibial components. Implant alignment plays a role in both survival and functional outcome following primary TKA, as component malalignment can lead to increased failure rates, maltracking, and knee pain.
Interpretation
Based on currently available evidence, surgeons should aim for optimal alignment of tibial and femoral components when performing TKA.
Total knee arthroplasty (TKA) is one of the most frequently performed orthopedic procedures, with an estimated 700,000 primary TKAs performed annually in the USA alone (National Hospital Discharge Survey 2010). While survival of primary TKAs is excellent, as most registries report 10-year survival of close to 95% for most implants (Graves et al. 2013, NJR 2013), recent studies have indicated that patient satisfaction is substantially worse. Up to 20% of the patients are not satisfied with the outcome as assessed 1 year postoperatively (Bourne et al. 2010, Klit et al. 2014) and a recent review found that 10–34% of patients had pain 3 months to 5 years after TKA (Beswick et al. 2012). Although patient-related factors (such as age, preoperative OKS and EQ5D, comorbidities, general health, depression, anxiety, and ASA) have been found to influence patient-reported outcome the most, surgical factors such as implant brand, hospital type (Baker et al. 2012), and implant alignment are also important (Choong et al. 2009, Longstaff et al. 2009).
Implant malalignment following primary TKA has been reported to be the primary reason for revision in 7% of revised TKAs (Schroer et al. 2013) and it has been linked to both decreased implant survival (Ritter et al. 2011) and inferior patient-reported outcomes (Choong et al. 2009, Longstaff et al. 2009). However, optimal alignment still remains a matter of controversy, as several recent reports have found little or no correlation between postoperative tibiofemoral malalignment in the coronal plane and revision rates (Morgan et al. 2008, Parratte et al. 2010, Bonner et al. 2011). The emergence of computer navigation (Fu et al. 2012) and patient-specific cutting blocks (Lachiewicz and Henderson 2013)—with the proposed benefits of improved component positioning and fewer outliers—have further fueled this debate, as benefits in survival and patient related outcome are not apparent. Also, kinematic alignment (as opposed to mechanical alignment) in TKA has been debated in recent years as inherently, it does not adhere to traditional thinking concerning implant positioning and it is intended to improve postoperative outcome (Howell et al. 2013a).
We investigated whether the literature supports definitions of optimal alignment following primary TKA surgery and whether a correlation between malalignment and inferior outcome could be identified. The following parameters were investigated separately: (1) tibiofemoral alignment in the AP plane; (2) tibial and femoral component placement in the AP plane; (3) tibial and femoral component placement in the sagittal plane; and (4) rotational alignment of tibial and femoral components.
Methods
In January and February 2014, we conducted a systematic Medline-based literature search for articles that addressed alignment and the outcome of TKA (finalized February 22, 2014). First, a search using mesh terms including: “Arthroplasty”, “Total Knee Replacement” and “TKA” was performed to verify the general notion of the operative surgery technique and the correct spelling of it. Then we searched the Medline (PubMed) database with restriction to the English language and by using mainly a combination of keywords “Arthroplasty”, “Knee Replacement”, and “Alignment”. 1,135 articles were found. Titles were reviewed, abstracts were read, and relevant studies were selected for analysis. Only articles on primary TKA using conventional surgical techniques were included, as we did not include papers on revision arthroplasty or those describing the use of navigation or patient-specific guides/instruments. Based on the abstracts, 44 relevant papers were identified and included in this narrative overview. Additional papers were included based on references from the original 44 publications.
Results and discussion
Overall tibiofemoral alignment
Restoration of an overall mechanical neutral axis of the lower limb, also known as the hip-knee-ankle (HKA) axis, is traditionally considered one of the goals of TKA. HKA is commonly defined as the angle between the mechanical axis of the femur (center of the femoral head to center of the knee) and the mechanical axis of the tibia (center of the proximal tibial plateau to the center of talus) (Moreland et al. 1987, Cooke et al. 2007). When standing full-length lower-limb radiographs are not available, anatomical tibiofemoral axis (TFA) is determined on short films, and considered normal when between 7° and 9° of valgus (Ewald 1989, Fang et al. 2009). Intraoperatively, the alignment of the leg is primarily controlled by the distal femur as well as proximal tibial cuts, and most surgeons agree that the postoperative limb alignment should be corrected within 0° ± 3° of the mechanical axis (Parratte et al. 2010, Bonner et al. 2011). However, the latter viewpoint has been challenged recently, as Bellemans (2011) reported that up to 32% of adult men and 17% of adult women had constitutional varus knees, with a natural mechanical alignment of > 3° varus.
Recent studies by Ritter et al. (2011) and by Fang et al. (2009) examined 6,070 primary TKAs with a mean follow-up of 8 years and found increased failure rates in malaligned TKAs, with hazard ratios (HRs) of 2.3 and 3.1 for knees with postoperative varus malalignment (TFA < 2.5°) and valgus malalignment (TFA > 7.5°).
Similar results were reported by Kim et al. (2014) who investigated 3,048 TKAs with a mean follow-up of 16 years, and showed a failure rate of 2.3% in knees with postoperative varus malalignment (TFA < 3°) compared to a 0.6% failure rate in neutrally aligned knees (TFA 3–7.5°). However, they did not find a significant increase in failure rates for valgus malalignment (0.9%).
Different mechanisms of failure have been reported in malaligned TKAs. The study by Fang et al. (2009) showed that TKAs in overall varus malalignment mainly failed due to medial collapse, while TKAs in overall valgus malalignment mainly failed because of ligament instability. A study by Berend et al. (2004) investigated failure mechanisms in 41 revised tibial components out of a cohort of 3,152 TKAs and found that overall anatomical varus malalignment was associated with medial bone collapse.
It is important to note that neutral alignment should be achieved by optimal placement of both the femoral component and the tibial component, as Ritter et al. (2011) showed that correction of varus or valgus malalignment of the first component by placing the second component to attain neutral tibiofemoral alignment was associated with a failure rate of 3.2% for tibial component varus malalignment and 7.8% for femoral component valgus malalignment. Overall alignment has not only been linked to revision rates, but also to functional outcome—as shown in a study of 115 patients by Choong et al. (2009), who reported superior International Knee Society (KSS) and Short-Form 12 (SF12) scores in knees aligned within ± 3° of neutral mechanical axis.
Contradictory to the findings above, several authors have failed to find any correlation between overall alignment and outcome following primary TKA. Both the Bonners et al. (2011) study of 501 TKAs and the Parratte et al. (2010) study of 398 TKAs—both of which had 15 years of follow-up—failed to show increased revision rates for TKA with postoperative HKA outside neutral ± 3°. Similar results were reported by Morgan et al. (2008) in 197 patients with a mean follow-up of 9 years. They found similar revision rates in TKAs with neutral postoperative TFA (4–9° valgus) and TKAs with either varus or valgus malalignment. Magnussen et al. (2011) reported medium-term survival and KSS scores for patients with residual postoperative varus alignment (HKA > 3°, varus) following TKA compared to patients with neutral postoperative alignment (HKA 0° ± 3°). Similar results were obtained by Vanlommel et al. (2013) who reported significantly better KSS scores in patients with mild postoperative varus alignment (HKA 3–6°, varus) than in patients with postoperative neutral alignment (HKA 0° ± 3°) and severe varus (HKA > 6°, varus). Finally, Matziolis et al. (2010) investigated 218 TKAs with a minimum follow-up of 5 years, and found similar survival rates and functional outcome scores (WOMAC and SF36) for aligned TKAs (HKA 0° ± 3°) and malaligned TKAs.
In conclusion, there have been conflicting reports on the importance of overall alignment on survival and functional outcome after primary TKA. As some studies used HKA for evaluation of alignment and others used TFA, direct comparison is difficult. However, neutral coronal alignment is still the gold standard, and it should therefore be aimed for until there is conclusive evidence to suggest otherwise (Lombardi et al. 2011).
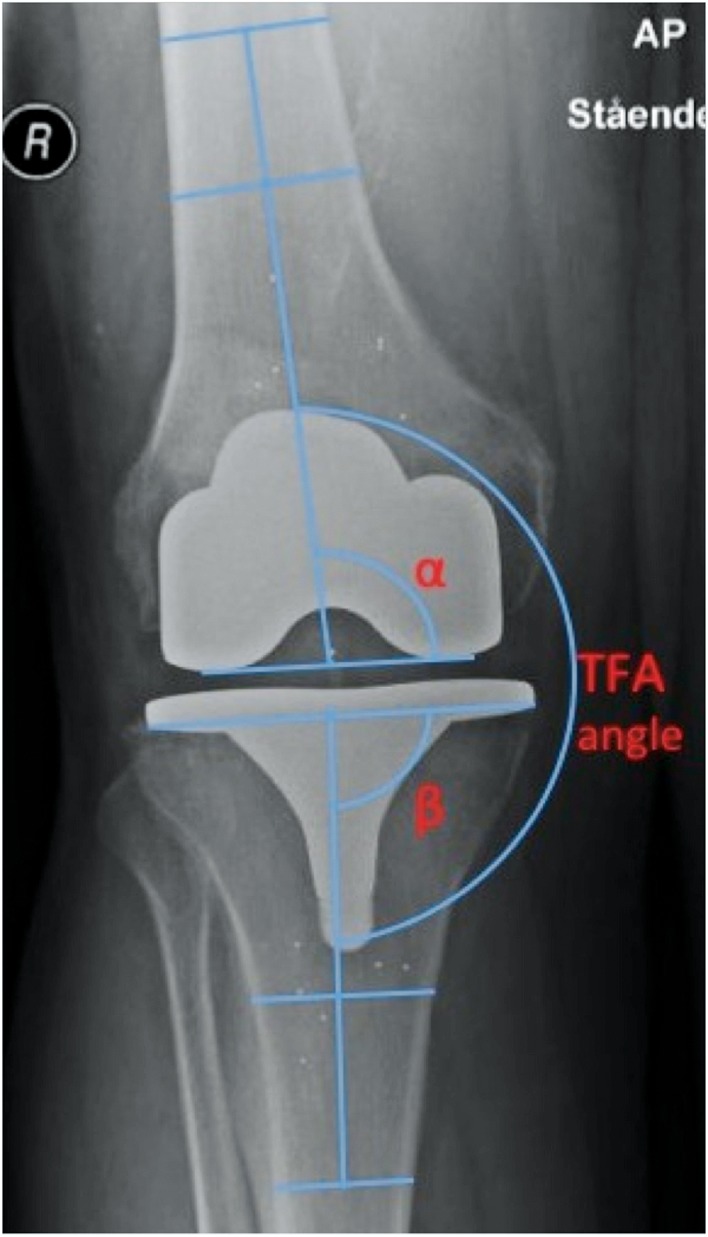
Coronal alignment of the femoral component (Figure 1)
Figure 1.
Example of measurements of femoral and tibial TKA component placement in the coronal plane with respect to the femoral and tibial anatomical axes, respectively, according to Petersen and Engh (1988) and as used by e.g. Ritter et al. (2011). Placement of the femoral component is measured using the angle (α) between the line across the bottom of the femoral condyles and femoral shaft axis. α = 90 corresponds to neutral placement, α > 90 corresponds to valgus placement of the femoral component, and α < 90 corresponds to varus placement of the femoral component. Placement of the tibial component is measured using the angle (β) between the line across the base of the tibial plate and the tibial shaft axis. β = 90 corresponds to neutral placement, β > 90 corresponds to valgus placement of the tibial component, and β < 90 corresponds to varus placement of the tibial component. TFA stands for tibiofemoral axis, measured at the angle between the tibial and femoral shaft axes (TFA angle). TFA angle = 180 corresponds to neutral alignment, TFA angle > 180 correponds to TFA in valgus, and TFA angle < 180 corresponds to TFA in varus.
The distal femoral cut is typically made 2–7°of valgus relative to the axis of the femoral shaft, in order to achieve neutral mechanical alignment (McPherson 2006). Thus, component position is either determined with respect to the femoral anatomical axis (FAA) or the mechanical axis (FMA).
Ritter et al. (2011) showed that a femoral component alignment of > 8°of valgus (with respect to the FAA) resulted in a 5 times higher rate of failure. Kim et al. (2014) reported a 1.7% failure rate in knees with femoral valgus alignment > 8° (with respect to the FAA) compared to a 0.7% failure rate in knees with neutrally aligned femurs (2–8° with respect to the FAA), while < 2° valgus led to an increased failure rate of 5%. Correct placement of the femoral component has also been shown to play a role in functional outcome, as Longstaff et al. (2009) reported that patients with neutral femoral alignment (± 2°on neutral FMA) had better KSS scores at 1-year follow-up.
In conclusion, the optimal distal femoral cut is typically 2–7°of valgus as neutral alignment seems to result in optimal functional outcome, while an alignment of > 8° and < 2° valgus with respect to the FMA has been shown to be an important contributor to implant failure.
Coronal alignment of the tibial component (Figure 1)
The goal of tibial component positioning is to maximize coverage to prevent settling (Lemaire et al. 1997), and to achieve a neutral tibial alignment. The latter is achieved by a proximal tibial cut 90º to the mechanical axis (Ritter et al. 1996).
Malalignment of the tibial component alters the distribution of tibial loading, which can lead to increased shear forces at the tibiofemoral interface, resulting in increased wear. Tibial malalignment of > 3° of varus has been reported to increase the risk of medial bone collapse (Berend et al. 2004). The study by Kim et al. (2014) showed an increased failure rate of 3.4% in TKAs with a tibial component alignment other than neutral, compared to 0% failure in neutrally aligned tibias, while Ritter et al. (2011) showed an 11-times higher rate of failure in TKAs with varus tibial malalignment (> 0°). Contradictory to these findings, Dossett et al. (2012) reported that on average kinematically aligned TKAs had a tibial component placed in 2.3° more varus and the femoral component placed in 2.4° more valgus than mechanically aligned TKAs, which resulted in improved patient-reported outcomes 6 months postoperatively. Long-term outcome of this technique and component placement are, however, unknown.
The role of tibial malalignment has also been extensively investigated by biomechanical ex vivo studies. D’Lima et al. (2001) demonstrated an almost 3-fold increase in wear in implants mounted with a 3° varus malalignment using a knee wear simulator, while a study by Werner et al. (2005) showed that a tibial malposition of > 3° can greatly alter the distribution of pressure and load between the medial and lateral compartments under static loading. A similar study determined that a 5° varus or valgus tilt increased contact stress by approximately 50% in 5 different knee implants (Matsuda et al. 1999).
In conclusion, tibial components should be placed in neutral alignment (90°).
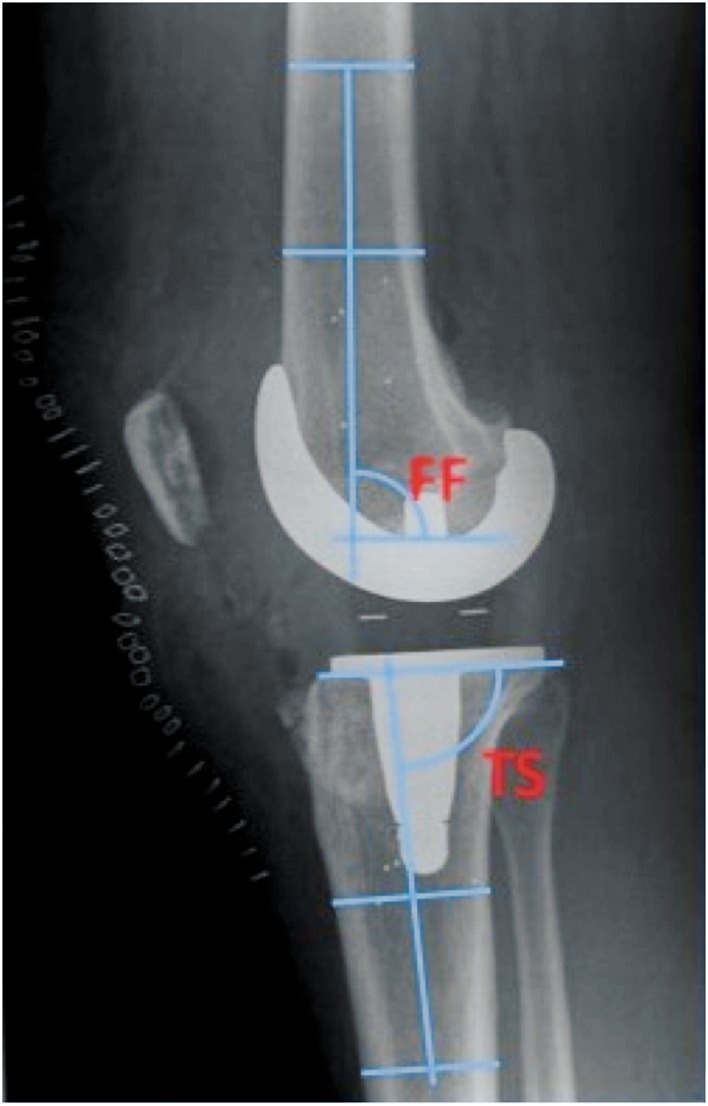
Sagittal alignment (Figure 2)
Figure 2.
Example of measurements of femoral and tibial TKA component placement in the sagittal plane with respect to the femoral and tibial anatomical axes, respectively, according to Petersen and Engh (1988) and as used by e.g. Ritter et al. (2011). Flexion of the femoral component is measured as the angle (FF) between the line across the bottom of the femoral implant and the femoral shaft axis. FF = 90 corresponds to neutral placement, FF > 90 corresponds to femoral component in extension, and FF < 90 corresponds to femoral component in flexion.
Tibial slope* is measured as the angle (TS) between the line across the bottom of the tibial plate and the tibial shaft axis. TS = 90 correponds to neutral placement, TS > 90 corresponds to anterior tibial slope*, and TS < 90 corresponds to posterior tibial slope*.
* Some component types have posterior slope built into the implant design.
Sagittal alignment of the femoral and tibial components is most commonly assessed in relation to femoral and tibial anatomical axes, respectively. With conventional techniques, sagittal prosthetic alignment is based on limited anatomical features that are palpable during surgery and determined intraoperatively with intramedullary or extramedullary rods. The proper alignment of a TKA in the sagittal plane and its clinical impact on function and outcome has been studied relatively little.
Most surgeons aim to place the femoral component in neutral alignment to the femoral axis in the sagittal plane, often using an intramedullary guide, while the sagittal tibial alignment is determined by posterior slope of the proximal tibial cut. The desired tibial sagittal alignment for most prosthesis types is a posterior slope between 0° and 7°, which can either be achieved by bony resection or if the posterior slope is built into the polyethylene.
The study by Lustig et al. (2012) of 95 patients showed that sagittal placement of the femoral component predicts flexion contracture, as posterior slope of > 3.5° from the mechanical axis increased the risk of mild flexion contracture at 1-year follow-up by 3 times—independently of other variables. These results contrast with those of Faris et al. (1988), who reviewed the sagittal plane orientation of cruciate retaining (CR) TKAs and found no correlation between implant position and knee range of motion.
A recent randomized control trial involving 40 knees by Murphy et al. (2014) showed that positioning of the femoral implant in 4° flexion in CR-TKA provided a difference in knee flexion compared to a neutral position. However, the improvement appeared to mainly occur at surgery, and was not associated with a clinical or functional benefit at 1 year; nor was it associated with increased patient satisfaction. Additionally, placing the femoral component in flexion can lead to painful patellar crepitus, as reported by Dennis et al. (2011).
Sagittal malpositioning of the femoral component has also been linked to inferior survival, as Kim et al. (2014) showed a 3.3% failure rate in knees with femoral implant flexed > 3°—compared to failure rates of 0% and 0.9% in neutrally aligned femoral components (0–3° flexion) and extended femoral components (> 1° extension), respectively. The same study also found that tibial malalignment in the sagittal plane (< 0° or > 7°) had a failure rate of 4.5%, as compared to a failure rate of 0.2% in the neutrally aligned group. The role of posterior slope in relation to functional outcome is debated, as cadaver studies have indicated that an increase in posterior slope may lead to increased flexion following TKR (Jojima et al. 2004, Bellemans et al. 2005), while a clinical study by Kansara and Markel (2006) failed to find any difference in postoperative flexion when increasing the posterior tibial slope by 5 degrees.
A study by In et al. (2009) showed that an insufficient tibial slope was an independent risk factor for flexion gap tightness. Further insight came from Singh et al. (2013), who suggested that re-creation of the anatomical tibial slope appears to improve maximum flexion in a study of 209 posterior-stabilized (PS) TKAs. Under no circumstances should the proximal tibia be cut with an anterior slope, as it would lead to impaired posterior flexion space and possible instability (Waelchli and Romero 2001).
In conclusion, few studies have investigated the role of sagittal component positioning in TKA surgery. It appears that to improve the survival rate and functional outcome following TKA, the surgeon should aim to place the femoral component in 0–3° of flexion. Posterior tibial slope should be 0–7°, as placement of the tibial component outside this range might be detrimental to implant survival and lead to instability (excessive posterior slope) or flexion gap tightness and reduced postoperative flexion (relative anterior slope). Correct posterior slope can be achieved by a proper proximal tibial cut, but can also be built into the polyethylene of the implant, depending on implant design.
Femoral component rotation
Optimal femoral component rotation has been debated for many years, and at least 4 distinct methods of determining proper femoral component rotation have been described: the trans-sulcus axis (TSA, better known as Whiteside’s line (Whiteside and Aruma 1995)), surgical transepicondylar axis (sTEA), anatomical transepicondylar axis (aTEA), and posterior condylar axis (PCA) and gap balancing (GB) (Scott 2013). sTEA is the line between medial femoral sulcus and the lateral femoral epicondyle, while aTEA is the line between medial and lateral femoral epicondyles. An angle of 3.2° ± 1° between aTEA and sTEA has been reported by Yoshino et al. (2001), with aTEA being more externally rotated. Most surgeons have personal preferences regarding surgical technique; however, studies have indicated that all methods yield similar results (Olcott and Scott 2000) with a possible advantage of using the TSA techniques in valgus knees (Aruma et al. 1995).
Cadaver studies have shown that optimal patella tracking is achieved when the femoral component is in a neutral position or externally rotated (Anouchi et al. 1993), and a study by Rhodes et al. (1990) showed that internal femoral rotation can result in abnormally high stresses on the patellar implant. These findings were confirmed by Matsuda et al. (2001) who showed a correlation between internal rotation of the femoral component between patellar tilt angle and clinical symptoms. Besides placing abnormal stress on the patella, internal rotation of the femoral component will displace the patella medially, thus increasing the Q angle, which can in turn lead to lateral patellar tilt, lateral patellar overhang, subluxation, and dislocation (Kelly 2001).
A study by Bell et al. (2014) on 56 TKA patients with unexplained knee pain showed that an internally rotated femoral component (> 0.3° internally rotated in relation to sTEA) was a significant factor in pain following TKA. Murakami et al. (2012) also reported a correlation between pain following TKA and internal rotation of the femoral component (> 0° internally rotated in relation to sTEA). External rotation of the femoral component in relation to PCA was also suggested by Akagi et al. (1999), who found a reduced need for lateral retinacular release and improved patellar tracking in the externally rotated group.
Excessive external rotation should also be avoided, as Miller et al. (2001) reported increasing tibiofemoral wear motion and worsening of patellar tracking in excessive femoral external rotation. Also, excessive external rotation (> 5°) may cause problems with tightness of the popliteus tendon complex, necessitating releases (Nagamine et al. 1995). Finally, an increased failure rate has been reported by Kim et al. (2014) in femoral components with < 2° of external rotation (6.7% failure) and also in femoral components with > 5° of external rotation (1.9% failure) when compared to components with 2–5° of external rotation (0% failure) in relation to sTEA, suggesting that 2–5° of external rotation is the optimal position.
Gap balancing technique relies on ligament balancing to establish symmetrical and rectangular flexion and also extension gap prior to definite bone resection and component placement (Scott 2013, Daines and Dennis 2014). Boldt et al. (2006) showed that this technique results in 90% of femoral components being placed within ± 3° in relation to sTEA, while Luyckx et al. (2012) reported similar femoral component rotation achieved by measured resection and gap balancing. Some authors have hypothesized that gap balancing provides better functional performance following primary TKA than TKAs performed using measured resection (Dennis et al. 2010, Daines and Dennis 2014).
In conclusion, many references exist for measuring femoral component rotation, with sTEA being the most commonly used, despite having the worst track record regarding intra- and inter-observer variability (Victor 2009). Internal rotation of the femoral component with respect to sTEA should be avoided, as 2–5° of external rotation in relation to sTEA seems to be the optimal range.
Tibial component rotation
3 distinct intraoperative methods of determining tibial component rotation have been described (Scott 2013): anatomical placement of an asymmetrical tibial tray on the cut surface, rotating the tibial tray relative to the tibial tubercle (usually using the junction of the medial and central thirds of the tubercle as an anatomical landmark), and finally the self-seeking method, where the tibial component is rotated into alignment following the femoral component during extension (Lee et al. 2008). An intraoperative study using rotating platforms by Huddleston et al. (2005) also investigated the self-seeking method and showed that using a fixed tibial anatomical landmark can lead to significant mismatch between tibial and femoral component rotation; they therefore recommended the use of a rotating platform to minimize the tibiofemoral mismatch. Postoperatively, projected femoral TEA, transverse axis of the tibia, tibial tubercle axis (TTA) (18° of internal tibial implant rotation in relation to the tibial tuberosity is considered neutral), anatomical tibial axis, and anteroposterior axis are used to determine tibial component position; however, no gold standard exists (Akagi et al. 2005, Cobb et al. 2008, Hutter et al. 2013). The sole use of any of these landmarks—and especially relying solely on the TTA—has been associated with erroneous positioning (Bonnin et al. 2011), so using a combination of landmarks may improve both positioning and outcome (Page et al. 2011).
Nicoll and Rowley (2010) compared painful and pain-free knees in 740 PS TKAs and found that internal rotation of the tibial component by > 9° (in relation to neutral TTA) was a major cause of pain and functional deficit following TKA. The same study did not find external rotational errors to be associated with pain. Barrack et al. (2001) investigated 102 TKAs with a minimum follow-up of 5 years and found significant differences in tibial component rotation between the 2 groups, with patients with anterior knee pain averaging 6° of internal rotation (in relation to neutral TTA) as compared to 0.4° of external rotation in the control group.
Bedard et al. (2011) investigated preoperative tibial and femoral component rotation in 34 TKAs revised for stiffness and found pathological tibial internal rotation in 33 cases, suggesting that excessive internal tibial rotation can lead to poor motion, patellar tracking complications, and anterior knee pain. Bell et al. (2014) found that an internally rotated tibial component (internally in relation to neutral TTA) was a substantial factor for pain following TKA. Finally, Kim et al. (2014) showed that rotational alignment of the tibial component by < 2° or > 5° of external rotation (in relation to posterior margins of the tibial plateau) increased component failure rates.
In conclusion, there is no gold standard for measurement of tibial component rotation. Excessive internal rotation when measured in relation to the tibial tubercle can lead to knee pain. Care must be taken when using fixed anatomical landmarks for positioning of a fixed bearing tibial component.
Combined tibial and femoral component rotation
Bell et al. (2014) found combined internal rotation of the femoral and tibial component (femoral with respect to TEA and tibial with respect to neutral TTA), and also rotational mismatch between the femoral and tibial component, to be associated with knee pain.
Berger et al. (1998) found that small amounts (1–4°) of combined femoral and tibial component internal rotation (femoral with respect to TEA and tibial with respect to neutral TTA) were associated with lateral tracking and tilting of the patella, whereas larger amounts of internal rotation (7–17°) were associated with early patellar dislocation and late patellar prosthesis failure. Patients with components that were aligned between 0° and 10° of external rotation did not present with patellar-femoral complications. The adverse effect of a combined internal rotation was confirmed by Barrack et al. (2001), who found a combined 4.7° of internal rotation in patients with anterior knee pain as compared to 2.6° external rotation in the control group. They showed that patients with a combined component internal rotation were more than 5 times as likely to experience anterior knee pain after TKA than patients with combined external rotation.
In conclusion, a combined internal rotation and rotational mismatch should be avoided as it can lead to pain following TKA.
Kinematic alignment
Implant alignment as discussed in this literature overview covers mechanically or anatomically aligned TKA that relies on restoring the patient’s HKA axis and placing the implants in relation to the body’s mechanical or anatomical axes.
Kinematic alignment was recently introduced as an alternative to conventional alignment techniques. In contrast to mechanical alignment, in kinematically aligned TKA the femoral and tibial components are positioned so that the angles and the levels of the distal and posterior femoral joint line and the tibial joint line are each restored to the patient’s natural alignment (Howell et al. 2013a), which is not necessarily mechanically neutral (Eckhoff et al. 2005). Kinematically aligned TKAs often use preoperative MRI templating and patient-specific instrumentation (Dossett et al. 2012); however, a technique for kinematic alignment with generic instruments has been described recently (Howell et al. 2013b). Few studies have compared the 2 alignment techniques (Dossett et al. 2012, Nogler et al. 2012), and currently no clear recommendations can be made regarding the optimal alignment strategy, as the study by Nogler et al. (2012) showed similar results for both techniques, and the study by Dosset et al. (2012), while showing improved patient-reported functional outcome in TKA performed with kinematic alignment, only had a 6-month follow-up, making conclusions about long-term outcome and survival difficult. More studies are therefore needed to investigate whether kinematic alignment can produce superior survivorship and functional outcome following primary TKA.
Soft tissue balance
Soft tissue balancing is considered to be an important factor influencing outcome following TKA, and some surgeons have emphasized that optimal outcome following primary TKA is more dependent on soft tissue management than on bone management (Peters 2006). Many techniques exist for achievement of optimal soft tissue balance (Mihalko et al. 2009), but an overview of the literature on this extensive subject is not within the scope of this paper.
Conclusion
Although primary TKA has shown its effectiveness by reducing knee pain and increasing knee function in activities of daily living, a general consensus about the optimal alignment of the femoral and tibial components is still lacking. In the present literature overview, we give the following recommendations for optimal TKA component placement:
Neutral overall coronal alignment is still currently the gold standard, and neutral HKA axis or 2–7° valgus TFA should be targeted until there is conclusive evidence to suggest otherwise (Fang et al. 2009, Lombardi et al. 2011, Ritter et al. 2011). The femoral component should be placed in 2–8° coronal valgus with respect to FAA and > 3 mm of overhang should be avoided (Mahoney and Kinsey 2010, Ritter et al. 2011, Kim et al. 2014). The tibial component should be placed in neutral coronal alignment (90°) with maximum bone coverage and minimal if any overhang (Berend et al. 2004, Bonner et al. 2011, Ritter et al. 2011, Kim et al. 2014). In the sagittal plane, the femoral component should be placed with 0–3° of flexion, and the tibial slope should be 0–7° (In et al. 2009, Lustig et al. 2012, Kim et al. 2014, Singh et al. 2013). Internal rotation of the femoral component with respect to sTEA should be avoided, as the femoral component should be placed in 2–5° of external rotation in relation to sTEA (Akagi et al. 1999, Matsuda et al. 2001, Kim et al. 2014, Bell et al. 2014). Excessive tibial rotation with respect to neutral TTA and also combined internal tibiofemoral rotation should also be avoided (Barrack et al. 2001, Nicoll and Rowley 2010, Bédard et al. 2011). There is a large variability in methodology when measuring component alignment following TKA, and further studies are required to investigate optimal component placement, not only with respect to implant survival but also to patient-reported outcomes following primary TKA.
Acknowledgments
KG, MG, HH, and AT designed the search strategy and the manuscript. KG and MK performed the literature search and selected the papers. KG wrote the initial draft of the paper, which was subsequently revised by MK, MG, HH, and AT. All authors approved the final manuscript.
No competing interests declared.
References
- Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, et al. Effect of rotational alignment on patellar tracking in total knee arthroplasty . Clin Orthop. 1999;366:155–63. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty . Clin Orthop. 2005;436:172–6. doi: 10.1097/01.blo.0000160027.52481.32. [DOI] [PubMed] [Google Scholar]
- Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens . Clin Orthop. 1993;287:170–7. [PubMed] [Google Scholar]
- Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note . J Bone Joint Surg (Am) 1995;77(9):1331–4. doi: 10.2106/00004623-199509000-00006. [DOI] [PubMed] [Google Scholar]
- Baker PN, Deehan DJ, Lees D, Jameson S, Avery PJ, Gregg PJ, et al. The effect of surgical factors on early patient-reported outcome measures (PROMS) following total knee replacement . J Bone Joint Surg (Br) 2012;94(8):1058–66. doi: 10.1302/0301-620X.94B8.28786. [DOI] [PubMed] [Google Scholar]
- Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty . Clin Orthop. 2001;392:46–55. doi: 10.1097/00003086-200111000-00006. [DOI] [PubMed] [Google Scholar]
- Bédard M, Vince KG, Redfern J, Collen SR. Internal rotation of the tibial component is frequent in stiff total knee arthroplasty . Clin Orthop. 2011;469(8):2346–55. doi: 10.1007/s11999-011-1889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, et al. Component rotational alignment in unexplained painful primary total knee arthroplasty . Knee. 2014;21(1):272–7. doi: 10.1016/j.knee.2012.09.011. [DOI] [PubMed] [Google Scholar]
- Bellemans J. Neutral mechanical alignment: a requirement for successful TKA: opposes . Orthopedics. 2011;34(9):507–9. doi: 10.3928/01477447-20110714-41. [DOI] [PubMed] [Google Scholar]
- Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H. The influence of tibial slope on maximal flexion after total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2005;13(3):193–6. doi: 10.1007/s00167-004-0557-x. [DOI] [PubMed] [Google Scholar]
- Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, et al. Tibial component failure mechanisms in total knee arthroplasty . Clin Orthop. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty . Clin Orthop. 1998;356:144–53. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- Beswick AD, Wylde V, Gooberman-Hill R, Blom A, Dieppe P. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients . BMJ Open. 2012;2(1):e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boldt JG, Stiehl JB, Munzinger U, Beverland D, Keblish PA. Femoral component rotation in mobile-bearing total knee arthroplasty . Knee. 2006;13(4):284–9. doi: 10.1016/j.knee.2006.01.007. [DOI] [PubMed] [Google Scholar]
- Bonner TJ, Eardley W GP, Patterson P, Gregg PJ. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years . J Bone Joint Surg (Br) 2011;93(9):1217–22. doi: 10.1302/0301-620X.93B9.26573. [DOI] [PubMed] [Google Scholar]
- Bonnin MP, Saffarini M, Mercier P-E, Laurent J-R, Carrillon Y. Is the anterior tibial tuberosity a reliable rotational landmark for the tibial component in total knee arthroplasty? . J Arthroplasty. 2011;26(2):260–7. e1–2. doi: 10.1016/j.arth.2010.03.015. [DOI] [PubMed] [Google Scholar]
- Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron K DJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? . Clin Orthop. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty . J Arthroplasty. 2009;24(4):560–9. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- Cobb JP, Dixon H, Dandachli W, Iranpour F. The anatomical tibial axis: reliable rotational orientation in knee replacement . J Bone Joint Surg (Br) 2008;90(8):1032–8. doi: 10.1302/0301-620X.90B8.19905. [DOI] [PubMed] [Google Scholar]
- Cooke T DV, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement . J Rheumatol. 2007;34(9):1796–801. [PubMed] [Google Scholar]
- Daines BK, Dennis DA. Gap balancing vs. measured resection technique in total knee arthroplasty . Clin Orthop Surg. 2014;6(1):1–8. doi: 10.4055/cios.2014.6.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis DA, Komistek RD, Kim RH, Sharma A. Gap balancing versus measured resection technique for total knee arthroplasty . Clin Orthop. 2010;468(1):102–7. doi: 10.1007/s11999-009-1112-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis DA, Kim RH, Johnson DR, Springer BD, Fehring TK, Sharma A. The John Insall Award: control-matched evaluation of painful patellar Crepitus after total knee arthroplasty . Clin Orthop. 2011;469(1):10–7. doi: 10.1007/s11999-010-1485-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Lima DD, Hermida JC, Chen PC, Colwell CW. Polyethylene wear and variations in knee kinematics . Clin Orthop. 2001;392:124–30. doi: 10.1097/00003086-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Dossett HG, Swartz GJ, Estrada NA, LeFevre GW, Kwasman BG. Kinematically versus mechanically aligned total knee arthroplasty . Orthopedics. 2012;35(2):e160–9. doi: 10.3928/01477447-20120123-04. [DOI] [PubMed] [Google Scholar]
- Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, et al. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality . J Bone Joint Surg (Am) (Suppl 2) 2005;87:71–80. doi: 10.2106/JBJS.E.00440. [DOI] [PubMed] [Google Scholar]
- Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system . Clin Orthop. 1989;248:9–12. [PubMed] [Google Scholar]
- Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty . J Arthroplasty. 2009;24(6):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- Faris PM, Ritter MA, Keating EM. Sagittal plane positioning of the femoral component in total knee arthroplasty . J Arthroplasty. 1988;3(4):355–8. doi: 10.1016/s0883-5403(88)80037-8. [DOI] [PubMed] [Google Scholar]
- Fu Y, Wang M, Liu Y, Fu Q. Alignment outcomes in navigated total knee arthroplasty: a meta-analysis . Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1075–82. doi: 10.1007/s00167-011-1695-6. [DOI] [PubMed] [Google Scholar]
- Graves S, Davidson D, de Steiger RN. Australian Orthopaedic Association National Joint Replacement Registry Annual Report. 2013.
- Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? . Clin Orthop. 2013a. 471. pp. 1000–7. [DOI] [PMC free article] [PubMed]
- Howell SM, Papadopoulos S, Kuznik KT, Hull ML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments . Knee Surg Sports Traumatol Arthrosc. 2013b;21(10):2271–80. doi: 10.1007/s00167-013-2621-x. [DOI] [PubMed] [Google Scholar]
- Huddleston JI, Scott RD, Wimberley DW. Determination of neutral tibial rotational alignment in rotating platform TKA . Clin Orthop. 2005;440:101–6. doi: 10.1097/01.blo.0000185448.43622.77. [DOI] [PubMed] [Google Scholar]
- Hutter EE, Granger JF, Beal MD, Siston RA. Is there a gold standard for TKA tibial component rotational alignment? Clin Orthop. 2013;471(5):1646–53. doi: 10.1007/s11999-013-2822-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- In Y, Kim J-M, Woo Y-K, Choi N-Y, Sohn J-M, Koh H-S. Factors affecting flexion gap tightness in cruciate-retaining total knee arthroplasty . J Arthroplasty. 2009;24(2):317–21. doi: 10.1016/j.arth.2007.10.022. [DOI] [PubMed] [Google Scholar]
- Jojima H, Whiteside LA, Ogata K. Effect of tibial slope or posterior cruciate ligament release on knee kinematics . Clin Orthop. 2004;426:194–8. doi: 10.1097/01.blo.0000138960.57680.60. [DOI] [PubMed] [Google Scholar]
- Kansara D, Markel DC. The effect of posterior tibial slope on range of motion after total knee arthroplasty . J Arthroplasty. 2006;21(6):809–13. doi: 10.1016/j.arth.2005.08.023. [DOI] [PubMed] [Google Scholar]
- Kelly MA. Patellofemoral complications following total knee arthroplasty . Instr Course Lect. 2001;50:403–7. [PubMed] [Google Scholar]
- Kim Y-H, Park J-W, Kim J-S, Park S-D. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis . Int Orthop. 2014;38(2):379–85. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klit J, Jacobsen S, Rosenlund S, Sonne-Holm S, Troelsen A. Total knee arthroplasty in younger patients evaluated by alternative outcome measures . J Arthroplasty. 2014;29(5):912–7. doi: 10.1016/j.arth.2013.09.035. [DOI] [PubMed] [Google Scholar]
- Lachiewicz PF, Henderson RA. Patient-specific instruments for total knee arthroplasty . J Am Acad Orthop Surg. 2013;21(9):513–8. doi: 10.5435/JAAOS-21-09-513. [DOI] [PubMed] [Google Scholar]
- Lee D-H, Seo J-G, Moon Y-W. Synchronisation of tibial rotational alignment with femoral component in total knee arthroplasty . Int Orthop. 2008;32(2):223–7. doi: 10.1007/s00264-006-0310-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemaire P, Pioletti DP, Meyer FM, Meuli R, Dörfl J, Leyvraz PF. Tibial component positioning in total knee arthroplasty: bone coverage and extensor apparatus alignment . Knee Surg Sports Traumatol Arthrosc. 1997;5(4):251–7. doi: 10.1007/s001670050059. [DOI] [PubMed] [Google Scholar]
- Lombardi AV, Berend KR, Ng VY. Neutral mechanical alignment: a requirement for successful TKA: affirms . Orthopedics. 2011;34(9):e504–6. doi: 10.3928/01477447-20110714-40. [DOI] [PubMed] [Google Scholar]
- Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function . J Arthroplasty. 2009;24(4):570–8. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Lustig S, Scholes CJ, Stegeman TJ, Oussedik S, Coolican M RJ, Parker DA. Sagittal placement of the femoral component in total knee arthroplasty predicts knee flexion contracture at one-year follow-up . Int Orthop. 2012;36(9):1835–9. doi: 10.1007/s00264-012-1580-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyckx T, Peeters T, Vandenneucker H, Victor J, Bellemans J. Is adapted measured resection superior to gap-balancing in determining femoral component rotation in total knee replacement? . J Bone Joint Surg (Br) 2012;94(9):1271–6. doi: 10.1302/0301-620X.94B9.28670. [DOI] [PubMed] [Google Scholar]
- Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus . Clin Orthop. 2011;469(12):3443–50. doi: 10.1007/s11999-011-1988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney OM, Kinsey T. Overhang of the femoral component in total knee arthroplasty: risk factors and clinical consequences . J Bone Joint Surg (Am) 2010;92(5):1115–21. doi: 10.2106/JBJS.H.00434. [DOI] [PubMed] [Google Scholar]
- Matsuda S, Whiteside LA, White SE. The effect of varus tilt on contact stresses in total knee arthroplasty: a biomechanical study . Orthopedics. 1999;22(3)(7):303. doi: 10.3928/0147-7447-19990301-06. [DOI] [PubMed] [Google Scholar]
- Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees . Am J Knee Surg. 2001;14(3):152–6. [PubMed] [Google Scholar]
- Matziolis G, Adam J, Perka C. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement . Arch Orthop Trauma Surg. 2010;130(12):1487–91. doi: 10.1007/s00402-010-1064-9. [DOI] [PubMed] [Google Scholar]
- McPherson EJ. Patellar tracking in primary total knee arthroplasty . Instr Course Lect. 2006;55:439–48. [PubMed] [Google Scholar]
- Mihalko WM, Saleh KJ, Krackow KA, Whiteside LA. Soft-tissue balancing during total knee arthroplasty in the varus knee . J Am Acad Orthop Surg. 2009;17(12):766–74. doi: 10.5435/00124635-200912000-00005. [DOI] [PubMed] [Google Scholar]
- Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty . Clin Orthop. 2001;392(38) doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity . J Bone Joint Surg (Am) 1987;69(5):745–9. [PubMed] [Google Scholar]
- Morgan SS, Bonshahi A, Pradhan N, Gregory A, Gambhir A, Porter ML. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty . Int Orthop. 2008;32(5):639–42. doi: 10.1007/s00264-007-0391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami AM, Hash TW, Hepinstall MS, Lyman S, Nestor BJ, Potter HG. MRI evaluation of rotational alignment and synovitis in patients with pain after total knee replacement . J Bone Joint Surg (Br) 2012;94(9):1209–15. doi: 10.1302/0301-620X.94B9.28489. [DOI] [PubMed] [Google Scholar]
- Murphy M, Journeaux S, Hides J, Russell T. Does flexion of the femoral implant in total knee arthroplasty increase knee flexion: A randomised controlled trial . Knee. 2014;21(1):257–63. doi: 10.1016/j.knee.2012.10.028. [DOI] [PubMed] [Google Scholar]
- Nagamine R, White SE, McCarthy DS, Whiteside LA. Effect of rotational malposition of the femoral component on knee stability kinematics after total knee arthroplasty . J Arthroplasty. 1995;10(3):265–70. doi: 10.1016/s0883-5403(05)80172-x. [DOI] [PubMed] [Google Scholar]
- National Hospital Discharge Survey: 2010
- National Joint Registry for England and Wales 10th Annual Report 2013.
- Nicoll D, Rowley DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement . J Bone Joint Surg (Br) 2010;92(9):1238–44. doi: 10.1302/0301-620X.92B9.23516. [DOI] [PubMed] [Google Scholar]
- Nogler M, Hozack W, Collopy D, Mayr E, Deirmengian G, Sekyra K. Alignment for total knee replacement: a comparison of kinematic axis versus mechanical axis techniques. A cadaver study . Int Orthop. 2012;36(11):2249–53. doi: 10.1007/s00264-012-1642-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olcott CW, Scott RD. A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty . J Arthroplasty. 2000;15(1):22–6. doi: 10.1016/s0883-5403(00)91051-9. [DOI] [PubMed] [Google Scholar]
- Page SR, Deakin AH, Payne AP, Picard F. Reliability of frames of reference used for tibial component rotation in total knee arthroplasty . Comput Aided Surg. 2011;16(2):86–92. doi: 10.3109/10929088.2011.552252. [DOI] [PubMed] [Google Scholar]
- Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements . J Bone Joint Surg (Am) 2010;92(12):2143–9. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- Peters CL. Soft-tissue balancing in primary total knee arthroplasty . Instr Course Lect. 2006;55(413) [PubMed] [Google Scholar]
- Petersen TL, Engh GA. Radiographic assessment of knee alignment after total knee arthroplasty . J Arthroplasty. 1988;3(1):67–72. doi: 10.1016/s0883-5403(88)80054-8. [DOI] [PubMed] [Google Scholar]
- Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB. Patellofemoral complications following total knee arthroplasty. Effect of a lateral release and sacrifice of the superior lateral geniculate artery . J Arthroplasty. 1996;11(4):368–72. doi: 10.1016/s0883-5403(96)80024-6. [DOI] [PubMed] [Google Scholar]
- Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA. The effect of alignment and BMI on failure of total knee replacement . J Bone Joint Surg (Am) 2011;93(17):1588–96. doi: 10.2106/JBJS.J.00772. [DOI] [PubMed] [Google Scholar]
- Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, et al. Why are total knees failing today? Etiology of total knee revision in 2010 . J Arthroplasty. 2013;28(8):116–9. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- Scott RD. Femoral and tibial component rotation in total knee arthroplasty: methods and consequences . Bone Joint J (Suppl A) 2013;95-B(11):140–3. doi: 10.1302/0301-620X.95B11.32765. [DOI] [PubMed] [Google Scholar]
- Singh G, Tan JH, Sng BY, Awiszus F, Lohmann CH, Nathan SS. Restoring the anatomical tibial slope and limb axis may maximise post-operative flexion in posterior-stabilised total knee replacements . Bone Joint J. 2013;95-B(10):1354–8. doi: 10.1302/0301-620X.95B10.31477. [DOI] [PubMed] [Google Scholar]
- Vanlommel L, Vanlommel J, Claes S, Bellemans J. Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees . Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2325–30. doi: 10.1007/s00167-013-2481-4. [DOI] [PubMed] [Google Scholar]
- Victor J. Rotational alignment of the distal femur: a literature review . Orthop Traumatol Surg Res. 2009;95(5):365–72. doi: 10.1016/j.otsr.2009.04.011. [DOI] [PubMed] [Google Scholar]
- Waelchli B, Romero J. Dislocation of the polyethylene inlay due to anterior tibial slope in revision total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc. 2001;9(5):296–8. doi: 10.1007/s001670100203. [DOI] [PubMed] [Google Scholar]
- Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements . J Biomech. 2005;38(2):349–55. doi: 10.1016/j.jbiomech.2004.02.024. [DOI] [PubMed] [Google Scholar]
- Yoshino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees . J Arthroplasty. 2001;16(4):493–7. doi: 10.1054/arth.2001.23621. [DOI] [PubMed] [Google Scholar]