Abstract
Background
It is estimated that more than 20% of pregnant women worldwide consume alcohol. Current research suggests that alcohol intake of seven or more standard drinks (one standard drink = 13.6 grams of absolute alcohol) per week during pregnancy places the baby at risk of serious, lifelong developmental and cognitive disabilities. Psychological and educational interventions may help women to reduce their alcohol intake during pregnancy.
Objectives
To determine the effectiveness of psychological and educational interventions to reduce alcohol consumption during pregnancy in pregnant women or women planning pregnancy.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register (August 2008), CENTRAL (The Cochrane Library 2007, Issue 4), MEDLINE (1966 to November 2007), EMBASE (1980 to November 2007), CINAHL (1982 to November 2007), Counsel.Lit (1980 to November 2007), PsycLIT (1974 to November 2007) and PsycINFO (1967 to November 2007) and checked cited references from retrieved articles.
Selection criteria
Randomized controlled trials examining the effectiveness of psychological and educational interventions for reducing consumption of alcohol among pregnant women, or women planning for pregnancy.
Data collection and analysis
At least two review authors independently extracted information from the results sections of the included studies.
Main results
Four studies met the inclusion criteria (715 pregnant women), and reported on at least one of the outcomes of interest. We performed no meta-analyses as the interventions and outcomes measured in the studies were not sufficiently similar. For most outcomes there were no significant differences between groups; and results relating to abstaining or reducing alcohol consumption were mixed. Results from individual studies suggest that interventions may encourage women to abstain from alcohol in pregnancy. There was very little information provided on the effects of interventions on the health of mothers and babies.
Authors’ conclusions
The evidence from the limited number of studies suggests that psychological and educational interventions may result in increased abstinence from alcohol, and a reduction in alcohol consumption among pregnant women. However, results were not consistent, and the paucity of studies, the number of total participants, the high risk of bias of some of the studies, and the complexity of interventions limits our ability to determine the type of intervention which would be most effective in increasing abstinence from, or reducing the consumption of, alcohol among pregnant women.
Medical Subject Headings (MeSH): Alcohol Drinking [adverse effects; *prevention & control], Counseling [*methods], Ethanol [*poisoning], Fetal Alcohol Spectrum Disorders [prevention & control], Preconception Care, Pregnancy Complications [prevention & control], Psychotherapy [*methods], Randomized Controlled Trials as Topic
MeSH check words: Female, Humans, Pregnancy
BACKGROUND
Introduction
It is estimated that more than 20% of pregnant women worldwide consume alcohol (Chang 2000). Current research suggests that alcohol intake of seven or more standard drinks (one standard drink = 13.6 grams of absolute alcohol) per week during pregnancy places the baby at risk from the negative effects of ethanol (Abel 1995; Chudley 2005; CPS Statement 2002; Ebrahim 1999; Roberts 2000). However, the effects of alcohol on the fetus are influenced not only by the absolute amount of alcohol consumed, but by the pattern of alcohol consumption (binge drinking versus daily consumption of alcohol), exposure-threshold amounts of alcohol in the blood, as well as the timing of exposure during pregnancy. Factors such as maternal age, health and nutritional status, fetal susceptibility and concurrent use of other psychoactive substances may also influence the outcome on the fetus (Abel 1995; Ebrahim 1999; Roberts 2000).
Drinking in pregnancy
Ascertaining the numbers of women drinking alcohol in pregnancy and any associated harm is not simple. Alcohol abuse, particularly in pregnancy, remains a socially stigmatized activity, and surveys of drinking behaviour in pregnancy may underestimate the extent of alcohol consumption (Clark 1999). Case control and other studies examining lifestyle behaviours in mothers who have given birth to children with abnormalities may be affected by recall bias (Czeizel 2004). Estimating the amount of alcohol women drink is also complicated and inexact. There is considerable variation in research studies in definitions of what constitutes heavy, moderate or light alcohol consumption. In different studies, alcohol has been measured in grams, other standard units, or in glasses (described as small or large). This is further complicated by the different strengths of different types of alcoholic drink. This leads to very imprecise definitions of light alcohol consumption, such as “a small glass of normal strength wine per day”. These variations in measurement mean that it is often difficult to interpret studies examining drinking prevalence, or outcomes associated with drinking varying amounts of alcohol in pregnancy (Clark 1999). Surveys in several countries have reported that approximately 15-20% of women continue to drink alcohol throughout pregnancy (Ebrahim 1999). However, figures may be much higher in the first trimester before pregnancy has been recognized. For example, a telephone survey in Canada reported that 80% of those interviewed said that they consumed alcohol before pregnancy, 50% in the early stages of pregnancy (before pregnancy recognition) and 18% throughout pregnancy (Tough 2006). Although many women are known to reduce their alcohol consumption during pregnancy, there remain a sizeable minority who continue to drink moderate amounts of alcohol, or indulge in binge drinking. In the Canadian study described, more than 11% of those interviewed reported binge drinking in the early stages of pregnancy.
There is general agreement that binge drinking (more than approximately five units of alcohol on one occasion) and moderate and heavy alcohol consumption during pregnancy are harmful; they increase the risk of miscarriage, preterm birth, low birth weight and may lead to serious disorders in children (Hannigan 2000;Jaddoe 2007; Mariscal 2006; Waterson 1990). There is more debate about the adverse effects associated with light consumption and whether women should be advised to abstain from alcohol altogether during pregnancy (Nathanson 2007; O’Brien 2007). A review of the effects of low consumption (defined as less than 12 grams of alcohol per day) concluded that there was only very limited evidence that this level of alcohol consumption was harmful. Risk of miscarriage was slightly higher in women who had consumed small amounts of alcohol, but there was little evidence that premature delivery, low birthweight, preterm delivery or fetal malformations were increased (Henderson 2007). However, the long-term effects of low alcohol consumption on other outcomes remain unknown and current knowledge has not defined a safe amount of alcohol that can be consumed in pregnancy.
In view of controversy surrounding the benefits of total abstinence, some government policies continue to support light drinking during pregnancy, but several countries have developed guidelines advocating total abstinence from alcohol because of the lack of clarity around threshold effects, and factors contributing to neonatal risks (ICAP 1999). Government policies advocating abstinence do acknowledge that the occasional drink of alcohol during pregnancy will likely result in no harm, but note that abstinence eliminates any possible risk (ICAP 1999).
The effects of alcohol in pregnancy
Studies in both animals and humans have shown the adverse effects associated with heavy alcohol consumption in pregnancy (Sokol 1981). There is some evidence of a dose-response effect (with greater consumption being associated with progressively worse outcomes) although, as we have noted, the findings are less clear with regard to the effects of more limited consumption (Armstrong 1992; Henderson 2007). A large cohort study in the Netherlands found that the adverse effects of alcohol were not confined to the early stages of pregnancy; alcohol consumption in late pregnancy was also associated with poor pregnancy outcomes, although the authors recognized that the confounding effects of unmeasured lifestyle and socio-economic factors may also have played a part (Jaddoe 2007).
There are various physiological mechanisms whereby alcohol causes harm to the developing baby, and many are not well understood (Goodlett 2005). Alcohol can cross the placental barrier and can directly affect important developmental processes by causing cell damage and disrupting cell functions. It can also have a less direct effect by causing damage to the placenta and other maternal tissues and organs essential to the wellbeing of the developing baby.
Since the early 1970s research has revealed that excessive maternal alcohol consumption (in excess of 80 grams or 8 units of alcohol per day) is associated with an increased risk of a spectrum of disorders in babies and children including serious developmental delay and physical disability (Baumann 2006; Hannigan 2000;Jaddoe 2007; Waterson 1990). As research has accumulated, the terms used to describe these alcohol-related adverse effects have changed several times, and remain inconsistent between countries and healthcare institutions. Specifically, fetal alcohol syndrome is used to describe a full-blown syndrome, characterized by prenatal or postnatal growth restriction or both, facial anomalies and central nervous system dysfunction. Other clinical manifestations of fetal alcohol syndrome may include cardiac anomalies, urogenital defects, skeletal abnormalities, and visual and hearing problems. Partial fetal alcohol syndrome is a term used to describe individuals with only some of the characteristic abnormalities. The term ’fetal alcohol effects’ has also been used to describe a partial expression of fetal alcohol syndrome. For example, the presentation may include neurodevelopmental changes and few or no facial anomalies or impaired growth, along with confirmed maternal drinking. Alcohol-related neurodevelopmental disorder (ARND) describes neurobehavioral pathology and structural central nervous system abnormalities due to in utero alcohol injury. The term alcohol-related birth defects (ARBD) is used to describe various malformations and, finally, fetal alcohol spectrum disorder acknowledges that the syndrome is a continuum, with differing degrees of malformations and dysfunction (AAP Statement 2000; Aase 1995;Astley 2000; Chudley 2005; CPS Statement 2002; Greenbaum 2002; Hoyme 2005).
The incidence of fetal alcohol syndrome and its milder variants are around nine per 1000 live births (Sampson 1997), and its effects are lifelong. It is one of the most important causes of serious developmental delay and disability in developed countries (Baumann 2006), and May 2007 has reported particularly high rates of fetal alcohol syndrome in South Africa.
Children with fetal alcohol syndrome often demonstrate poor impulse control, problems in social perception, deficits in higher level receptive and expressive language, poor capacity for abstraction, and problems in memory, attention and judgement (Coles 2002;Connor 2000; Johnson 1996; Loock 2005; Mattson 2001; Randall 2001; Sokol 2003; Streissguth 1996). Streissguth 1996). Other researchers have demonstrated that the long-term effects associated with gestational alcohol exposure may include a higher incidence of mental health problems, disruptive school experience, trouble with the law, substance abuse problems and an increased need for dependent living than the general population. Stade 2006 found that children with fetal alcohol syndrome experienced a significantly lower mean health-related quality of life score (0.47 versus 0.95) when compared with a reference group of children from the general population. The alcohol-affected children demonstrated severe dysfunction on the attributes of cognition and emotion, which reduced their overall quality of life scores. The total costs of caring for children affected by fetal alcohol syndrome in the United States have been estimated to be $74.6 million to $1.6 billion, based on an incidence of 0.33 and 1.99 cases per 1000 live births respectively (Abel 1991; Harwood 1985; Rice 1991).
Description of the intervention
Both pharmacological and psychological/educational strategies to reduce alcohol consumption have been described in the literature. Pharmacological interventions include disulfiram, natrexone and acamprosate (Harvard 2002). Disulfiram (Antabuse) is a drug used to deter drinking by preventing the liver from fully metabolizing alcohol. It blocks the oxidation of alcohol at the acetaldehyde stage and causes the toxic breakdown product acetaldehyde to accumulate. The combination of disulfiram use and alcohol consumption can lead to extremely unpleasant symptoms including nausea, flushing, headache, high blood pressure, and chest pain. Naltrexone, an opioid antagonist, reverses the effects of narcotics and reduces the activity of the body’s natural opioids, which are stimulated by alcohol as well as narcotics. Individuals who take naltrexone should get less pleasure out of drinking and not want to drink as much. Acamprosate is a calcium channel blocker. It is chemically related to glutamate, the brain’s chief excitatory neurotransmitter. When the brain is constantly exposed to alcohol (a sedative that tends to shut down cortical activity) nerve receptors for glutamate compensate by becoming hypersensitive. Acamposate seems to stimulate inhibitory GABA receptors and to antagonize excitatory amino acids, such as glutamate. This helps to prevent some of the pleasurable, reinforcing effects of alcohol use. The effectiveness of disulfiram, naltrexone, and acamprosate in the treatment of alcohol abuse has been well described (Chick 1992;Harvard 2002; Mason 2001; Streeton 2001). However, their safety in pregnancy has not been demonstrated, and disulfiram has been associated with limb reduction anomalies when used during pregnancy (Nora 1977; Reitnauer 1997).
Psychological and educational interventions for reducing alcohol use among heavy users have been described. They include educational sessions, motivational enhancement therapy, self-help groups, psychotherapeutic techniques and cognitive-behavioural interventions. Psychological interventions include cognitive-behavioural therapy (CBT), brief psychodynamic psychotherapy, interpersonal psychotherapy, and supportive counselling or therapy (Churchill 2003). Specifically, CBT incorporates core elements of both behavioural and cognitive models. CBT focuses on diminishing the patient’s negative automatic thoughts and dysfunctional underlying beliefs that evoke unwanted symptoms, through collaborative ’hypothesis-testing’, behavioural tasks and skills training (Ellis 1962). Brief psychodynamic psychotherapy is grounded in psychoanalytic principles and uses the therapeutic relationship to explore and resolve unconscious conflict. The therapeutic goals are development of insight and circumscribed change (Malan 1963). Interpersonal psychotherapy uses the connection between mood and current interpersonal experiences to focus on four problem areas of grief, role dispute, role transition and interpersonal deficits (Klerman 1984). Supportive counselling is sometimes described as Rogerian person-centred therapy. Rooted in a non-mechanistic philosophy, person-centred therapy is non-manualized and experiential, and core conditions of empathy, acceptance and genuineness are utilized by the therapist within the therapeutic relationship to facilitate the client towards self-awareness and self-determination (Rogers 1961).
Educational interventions are generally based on social learning theory. Bandura and his colleagues (Bandura 1986) have shown that the application of consequences is not necessary for learning to take place. Learning can therefore occur through the simple processes of observing someone else’s activity. This work provided the foundation for Bandura’s later work in social cognition. Bandura formulated his findings in a four-step pattern: (1) attention: the individual notices something in the environment; (2) retention: the individual remembers what was noticed; (3) reproduction: the individual copies the action that was noticed; (4) motivation: the environment delivers a consequence that changes the probability that the behavior will be performed again (reinforcement and punishment) (Bandura 1986; Price 1995). Educational interventions are less well defined than psychological interventions but include brief educational counselling sessions, structured long-term educational programs with motivational enhancement interventions (greater than five sessions), individual-focused educational strategies, family-focused programs, professional group education interventions and self-help group educational interventions (Manwell 2000; Schorling 1993).
Why it is important to do this review
Several randomized controlled trials (RCTs) have described the effectiveness of psychological and educational interventions to reduce alcohol intake when used in combination with pharmacological interventions or alone (Ait-Daoud 2001; Brown 2001;Connors 2001; Fleming 2002; McIntosh 1997; Walters 2000). As pharmacological interventions are contraindicated during pregnancy, psychological and educational interventions have been advocated for reducing alcohol intake among pregnant women or women planning pregnancy. However, their effectiveness has not been systematically reviewed. This systematic review aims to examine all trials including pregnant women or women planning for pregnancy which compare psychological and/or educational interventions versus no intervention (or usual care) for reducing the consumption of alcohol during pregnancy.
OBJECTIVES
The primary objective of this review is to determine the effectiveness of either psychological or educational interventions, or both, for reducing prenatal consumption of alcohol among pregnant women, or women planning for pregnancy.
The secondary objectives are to describe any adverse effects on the mother or the fetus when psychological and/or educational interventions are used to reduce prenatal alcohol consumption.
METHODS
Criteria for considering studies for this review
Types of studies
RCTs that compare the effectiveness of psychological and/or educational interventions for reducing prenatal consumption of alcohol among pregnant women, or women planning for pregnancy. This includes studies where educational and/or psychological interventions have been compared with no intervention; where interventions were compared with ’routine care’ (where possible providing details of what such care involved); or, where different educational and/or psychological interventions have been compared (again, including details of care provided to women in different arms of trials).
Types of participants
Pregnant women or women planning pregnancy who consume alcohol, and who are participating in studies examining psychological or educational interventions to reduce alcohol use. Alcohol consumption would be demonstrated by women’s self-report or by urine or blood screening for alcohol. (This review does not focus on pregnant women participating in treatment programmes for alcohol abuse or dependence; this group is included in a related Cochrane Review (Lui 2008)).
Types of interventions
Psychological and/or educational interventions during pregnancy or 12 months before conception for women planning pregnancy. Psychological interventions include cognitive-behavioural therapy, brief psychodynamic psychotherapy, interpersonal psychotherapy and supportive counselling/therapy. Educational interventions include brief educational counselling sessions, structured long-term educational programs with motivational enhancement interventions (greater than five sessions), individual-focused educational strategies, family-focused programs, professional group education interventions and self-help group educational interventions.
Types of outcome measures
Primary outcomes
Abstinence from alcohol during pregnancy;
reduction of alcohol consumption during pregnancy to less than seven standard drinks a week.
Secondary outcomes
Maternal
Duration of abstinence or reduced intake during pregnancy, and postnatally;
adverse effects in the mother such as delirium tremors, depression, anxiety, withdrawal from prenatal care;
benefits to the mother such as reduction in psychological distress, depression, anxiety, improvement in quality of life.
Neonatal
Diagnosis of fetal alcohol syndrome, partial fetal alcohol syndrome, alcohol-related neurodevelopmental disorder (ARND);
admission to neonatal intensive care unit/special care nurseries, pediatric hospital unit;
weight, length (height) and head circumference;
signs of neurological sequelae such as poor suck, irritability, increased muscle tone;
birth defects associated with prenatal exposure to alcohol with or without a diagnosis of fetal alcohol syndrome such as cardiac anomalies, urogenital defects, skeletal abnormalities, absence or partial absence of the corpus callosum;
placement in foster or adoptive care.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co-ordinator (August 2008).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co-ordinator and contains trials identified from:
quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE;
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL and MEDLINE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co-ordinator searches the register for each review using the topic list rather than keywords.
In addition, we searched CENTRAL (The Cochrane Library 2007, Issue 4), MEDLINE (1966 to November 2007), EMBASE (1980 to November 2007), CINAHL (1982 to November 2007), Counsel.Lit (1980 to November 2007), PsycLIT (1974 to November 2007) and PsycINFO (1967 to November 2007). See Appendix 1 for the search strategy used. A qualified librarian assisted the authors in searching these databases.
Searching other resources
We searched cited references from retrieved articles and reviewed abstracts and letters to the editor to identify unpublished RCTs. We contacted the primary investigator when further data were required.
We did not apply any language restrictions.
Data collection and analysis
Six review authors undertook this review, five of whom are content experts. Four authors conducted the additional literature search. Five of the authors screened the studies that were found as a result of this search, discarding the studies that were clearly ineligible but aiming to be overly inclusive rather than risk losing relevant studies. Then two authors independently abstracted information from the results sections of the included studies. We resolved discrepancies by discussion. One author checked and entered the data, all data in tables were then independently rechecked. Where possible, we sought missing data from the authors.
We evaluated studies for methodological quality using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
(1) Sequence generation (checking for possible selection bias)
We have described for each included study the methods used to generate the allocation sequence.
We assessed the methods as:
adequate (any truly random process, e.g. random number table; computer random-number generator);
inadequate (any non-random process, e.g. odd or even date of birth; hospital or clinic record number); or
unclear.
(2) Allocation concealment (checking for possible selection bias)
We have described for each included study the method used to conceal the allocation sequence and determine whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We have assessed the methods as:
adequate (e.g. telephone or central randomization; consecutively numbered sealed opaque envelopes);
inadequate (open random allocation; unsealed or non-opaque envelopes, alternation; date of birth);
unclear.
(3) Blinding (checking for possible performance bias)
We have described for each included study all the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. With educational and psychological interventions blinding of care providers and participants is generally not feasible, but we have noted where there has been partial blinding for some outcomes or classes of outcomes. We have assessed the methods as:
adequate, inadequate or unclear for participants;
adequate, inadequate or unclear for personnel;
adequate, inadequate or unclear for outcome assessors.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We have described for each included study the completeness of data including attrition and exclusions from the analysis. We state whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomized participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups. Again, methods used to take account of missing data have been assessed as adequate, inadequate or unclear; we have assessed attrition above 20% as inadequate even where loss was balanced across groups.
(5) Selective reporting bias
We have described for each included study how the possibility of selective outcome reporting bias was examined by us and what we found.
We have assessed the methods as:
adequate (where it is clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported);
inadequate (where not all the study’s pre-specified outcomes have been reported; one or more reported primary outcomes were not pre-specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear.
(6) Other sources of bias
We have described for each included study any important concerns we have about other possible sources of bias.
(7) Overall risk of bias
We have made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). With reference to (1) to (6) above, we have assessed the likely magnitude and direction of the bias and in the results section we have discussed how the methodological quality of studies may impact on the findings.
Measures of treatment effect
We carried out statistical analysis using Review Manager Software (RevMan 2008). Because it was not clear that interventions or outcomes measured in studies were the same or very similar, we have presented the results from individual studies separately. We performed statistical analyses for dichotomous data using risk ratio, with 95% confidence intervals. For continuous data we have analyzed results using the mean difference. In updates of the review, if studies measure the same outcome but using different methods (for example, using different visual analogue scales) we will use the standardized mean difference if data are combined in meta-analysis.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification.
We identified a total of 22 studies for possible inclusion in the review.
Four studies, including 715 pregnant women, met the inclusion criteria and reported on at least one of the outcomes of interest for this systematic review (Chang 1999; Handmaker 1999a;O’Connor 2007; Reynolds 1995). These studies were all conducted in the United States of America. We have set out details of the participants and descriptions of the interventions and the comparison conditions in the table Characteristics of included studies. All included studies combined educational and psychological approaches. We contacted authors of three of the included studies for additional information, and all provided some unpublished data which we have used in the review (Chang 1999; Handmaker 1999a; O’Connor 2007).
We have provided details of the 17 excluded studies in the table Characteristics of excluded studies.
We excluded six studies as they lacked randomization (Eisen 2000;Eustace 2000; Grant 2005; Larsson 1983; Meberg 1986; Rosett 1983); seven did not meet the inclusion criteria relating to participants (Aalto 2000; Floyd 2007; Handmaker 1999b; Hankin 2002; Manwell 2000; Palinkas 1996; Scott 1990) (in these studies either pregnant women were explicitly excluded or it was not clear that participants were pregnant or planning pregnancy); in three studies there was no educational or psychological intervention to reduce alcohol consumption (Belizan 1995; Fox 1987; Reading 1982); last, one study, which may otherwise have been eligible, did not collect data on outcomes relevant to the review (Calabro 1996). One study (awaiting classification) which was eligible for inclusion did not present outcome data in a way that we could use in the review, and we have contacted the authors for more information (Chang 2005).
Risk of bias in included studies
Methodological quality of included studies
We have presented the assessments of the methodological quality and risk of bias for individual studies in the risk of bias tables attached to the table Characteristics of included studies.
The risk of bias of included studies was mixed, with none of the studies providing full information about the methods used. We assessed the method of sequence generation as adequate in only one of the four studies (Chang 1999); the remaining studies did not provide information on this. It was not clear in any of the studies how randomization was achieved and whether there was adequate allocation concealment. Blinding participants and care providers to group allocation for educational and psychological interventions is generally not feasible. Two of the studies report that outcome assessors were not aware of group allocation (Chang 1999; Handmaker 1999a). The lack of blinding may introduce bias and this should be kept in mind when interpreting results. Levels of attrition were low (less than 10%) in two of the included studies (Chang 1999; Reynolds 1995) but were high in the studies by Handmaker 1999a (19% lost to follow up) and O’Connor 2007 (26% attrition, and those lost to follow up were reported as being different in several respects from those remaining in the study). A problem with all of the included studies was that the description of the intervention and comparison conditions and the methods of assessment were not sufficient to allow for study replication; and for all four studies results were not simple to interpret. For this reason, many of the results are reported narratively rather than by analyses.
Effects of interventions
Four studies met the inclusion criteria. These included a total of 715 pregnant women, and reported on at least one of the outcomes of interest for this systematic review.
A variety of approaches and comparison groups were used in the four included studies, and different outcomes were measured in different ways at different follow-up points. For these reasons studies have not been combined in meta-analysis; rather, we have presented results separately for each included study.
All four studies included advice on alcohol reduction, but in all cases data on alcohol use were based on self-report rather than being biochemically validated; this is likely to be a source of bias in these studies and should be kept in mind in when interpreting the results.
All four studies recruited women who had either consumed alcohol during the last month or were described as being “at risk” of consuming alcohol during pregnancy based on their responses to an alcohol screening tool.
In the Chang 1999 study, the intervention consisted of a 45-minute counselling session and women were provided with a self-help manual. The comparison group received no active intervention, but both groups underwent a comprehensive assessment of alcohol related behaviour. In the Handmaker 1999a study, similarly, women in both the intervention and control groups underwent a comprehensive assessment. In addition, the intervention group took part in a one-hour motivational interview while the control group received a letter describing risks and were referred to their usual care providers. In both the O’Connor 2007 and Reynolds 1995 studies, women in the intervention group had shorter interventions (approximately 15 minutes) with follow-up activities or reinforcement, and in both studies control groups received advice to abstain from drinking alcohol as part of their routine antenatal care.
Abstinence from alcohol during pregnancy
All four studies reported some measure of abstinence from alcohol following the intervention. Chang 1999 reported that, following the intervention, 69% of the intervention group versus 62% of the control group were abstinent; the difference between groups was not significant (unpublished data) (risk ratio (RR) 1.11, 95% confidence interval (CI) 0.93 to 1.33). Chang 1999 also provides figures for abstinence for those women in the intervention and control groups who were abstinent at the initial assessment. Results for this subset of the sample suggest that the intervention had a positive effect in terms of maintaining levels of abstinence (RR 1.20, 95% CI 1.01 to 1.42). Levels of post-intervention abstinence in the Handmaker 1999a and O’Connor 2007 trials are set out in Table 1 and Table 2 respectively (the latter was a cluster-randomized trial and figures were adjusted for unit of randomization). Both of these studies report a positive intervention effect. Similarly, in the Reynolds 1995, study more women abstained from alcohol after the intervention, although the evidence of a difference between groups was not statistically significant (RR 1.25, 95% CI 0.97 to 1.61).
Table 1.
The effects of motivational interviews compared to brief written information
| Handmaker 1999a | Intervention group (n = 16) | Control group (n = 18) |
| mean (SD) | mean (SD) | |
| Total standard units of alcohol pre-intervention | 26.5 (41.3) | 38.9 (95.8) |
| Total standard units of alcohol post-intervention | 9.7 (31.0) | 11.1 (19.5) |
| Days abstinent pre-intervention | 49.6 (12.7) | 53.2 (10) |
| Days abstinent post-intervention | 57.5 (6.2) | 55.1 (8.3) |
Table 2.
Brief intervention versus routine care (Cluster trial: figures adjusted for co-variates)
| O’Connor 2007 | Intervention group (brief intervention) n = 117 |
Control group (assessment only) n = 138 |
|---|---|---|
| 1. Abstinence | ||
| Abstinent (3rd trimester) | 115 | 126 |
| Still drinking | 2 | 12 |
| (Adjusted odds ratio (OR) 5.39, 95% CI 1.59 to 18. 25) | ||
| 2. Alcohol reduction | Adjusted mean (SD) | Adjusted mean (SD) |
| Initial drinking score | 2.10 (3.35) | 1.73 (1.73) |
| 3rd trimester score | 0.01 (0.06) | 0.18 (0.05) (Difference reported as statistically significant P < 0. 01) |
Reduction of alcohol consumption during pregnancy
All four studies included some measure of alcohol reduction in pregnancy, although each trial used a different measure and follow up occurred at different times. (In both the Chang 1999 and theReynolds 1995 studies, mean scores were reported but standard deviations (SDs) were not provided; the values for SDs used in the analysis for these outcomes have been calculated from P values set out in the papers.) Chang 1999 reported the mean number of drinking episodes during pregnancy; the difference between groups was not statistically significant (mean difference (MD) -0.30, 95% CI -0.68 to 0.08). Reynolds 1995 reported the average number of alcoholic drinks per month consumed following the intervention; again, the evidence for a difference between groups was not significant (MD -0.78, 95% CI -1.58 to 0.02). The difference in the number of alcoholic drinks (standard units) at baseline and post intervention for intervention and control groups was not significantly different in the Handmaker 1999a study (Table 1). O’Connor 2007 suggests that a brief intervention was associated with a greater reduction in alcohol consumption in the third trimester compared with the control group (assessment only), although scores were very low in both groups in late pregnancy and there were high levels of attrition in this study (Table 2).
Other outcomes
Only limited information was provided on the effects of the interventions on the health and wellbeing of mothers and babies.O’Connor 2007 reported that, after adjustment, the intervention was associated with slightly higher birthweights for babies whose mothers were heavier consumers of alcohol at the initial assessment, but this pattern was reversed for women who initially consumed low amounts of alcohol; for low initial alcohol consumers, babies in the control group were slightly heavier at birth. There was a similar pattern of results for birth length. This study also reported on miscarriages and stillbirth rates in the two groups; there was one miscarriage in the intervention group and two miscarriages and two stillbirths in the control group (these results relate only to those women available at follow up in a study with high rates of attrition). Chang 1999 reported that there were no significant differences between groups in terms of birthweights or one- and five-minute Apgar scores.
Subgroup and sensitivity analysis
We were not able to examine interventions aimed at women planning pregnancy, as none of the included studies focused on such women. We had planned to carry out sensitivity analysis examining the impact of risk of bias on results; however, none of the included studies provided information on allocation concealment and all had other study design characteristics (for example, lack of blinding or high attrition rates) which meant that, overall, all of the included studies were at high risk of bias.
DISCUSSION
This review focused on the efficacy of interventions for reducing alcohol consumption and did not include other types of substance use, The review includes only randomized control trials; and ensured that the time frame of the search strategy was not limited, but rather extended over 30 years.
To date this systematic review includes only four studies and 715 women and all of the included studies had methodological weaknesses that meant that they were at risk of bias.
The studies included in the review suggest that educational and counselling interventions may encourage women to abstain from alcohol during pregnancy. However, for outcomes relating to alcohol consumption, the evidence of a difference between groups was in some cases weak and results were not consistent. Overall, the included studies provided only very limited information on the effects of interventions on the health of women and babies.
The evidence on reductions in consumption and abstinence in the included studies was all based on self-reported drinking levels (although in one study there was an attempt to corroborate accounts by questioning (with the woman’s permission) significant others (Handmaker 1999a). As we acknowledged in the introduction, consuming alcohol in pregnancy is a socially stigmatized activity in many cultures, and results based on self-reported behaviour may exaggerate the positive effects of interventions. Evidence from smoking cessation trials has demonstrated that biochemically validated quit rates following interventions tend to be lower than those based on self-report (Lumley 2004).
Drawing conclusions on the overall effects of interventions was difficult, as the interventions included were different (ranging from 10 minutes through to a structured hour-long interview with reinforcement at subsequent visits). It was also difficult to assess the impact of interventions within the individual trials, as it was not always clear what the comparison groups received. In the Chang 1999 study, it was reported that women in the control group received no active intervention, but it was not clear whether women received any advice as part of routine care. In the remaining three studies, women in the control groups received some advice encouraging them to reduce their alcohol intake, and in all four studies women in both groups underwent lengthy assessments of their alcohol consumption behaviour, which itself may have had some effect.
The included studies all recruited women who reported that they had consumed some alcohol since the beginning of pregnancy or who were screened as being “at risk” of consuming alcohol in pregnancy by their positive responses to an alcohol screening tool. However, many of the women included had already stopped drinking by the time they were recruited to the studies (although they may well have drunk alcohol before pregnancy confirmation). Of those that continued to drink, although the groups may have included some moderate and heavy drinkers, the average levels of alcohol consumption tended to be relatively low (less than approximately one drink each day). Further, as pregnancy progressed, drinking levels tended to decrease in both the intervention and control groups. This pattern reflects that described in observational studies of lifestyle behaviour changes in pregnancy; with reductions in drinking once pregnancy has been recognized. It is also possible that the screening interviews diluted the intervention effect as it may also have had an impact on behaviour in both the intervention and control groups. Under these circumstances, where baseline drinking levels are relatively low and where many women reduce their alcohol consumption during pregnancy irrespective of any specific intervention, large studies are needed to identify meaningful differences in drinking behaviour between groups.
The main conclusion of this review is that overall there is very little evidence about the effects of educational and psychological interventions aiming to reduce alcohol consumption in pregnancy, and in particular, on the effect of such interventions on the health of women and babies. The lack of evidence from trials in this area is very surprising to us, given that heavy alcohol consumption increases risk of serious harm (fetal alcohol syndrome being an important cause of severe developmental delay). While this subject has received so little research attention, modification of other lifestyle factors in pregnancy has been the focus of a great deal of research. The Cochrane review of interventions to reduce smoking includes 64 trials carried out in different settings and countries, and using a variety of strategies (Lumley 2004). The four studies included in this review were all carried out in the USA, which raises the question of their generalizability to other settings. There is an urgent need for more research on this topic.
AUTHORS’ CONCLUSIONS
Implications for practice
Individual studies suggest that psychological and educational interventions may result in increased abstinence from alcohol among pregnant women. However, the paucity of studies and number of total participants does not allow us to determine the overall effectiveness of psychological and/or educational interventions for reducing prenatal consumption of alcohol among pregnant women, or women planning pregnancy. While some benefits to babies were reported, overall there was very little information provided on health outcomes for mothers and babies.
Implications for research
The results of the current systematic review highlight the need for further research. A large multi-centred double-blinded randomized trial measuring relevant outcomes (including reduction of alcohol consumption during pregnancy to less than seven standard drinks a week; abstinence from alcohol during pregnancy, adverse effects and/or benefits to the mother and neonatal outcomes) must be conducted. The trial must overcome the methodological limitations of past trials.
PLAIN LANGUAGE SUMMARY.
Psychological and educational interventions to reduce alcohol consumption by pregnant women
Many women continue to consume alcohol when they are pregnant. Drinking seven or more standard drinks per week may be harmful, and can cause growth restrictions in babies; binge drinking and heavy alcohol consumption can lead to learning difficulties, behaviour problems and physical disabilities in children. Government policies acknowledge that the occasional drink is not likely to cause harm but that abstinence from alcohol in pregnancy eliminates any possible risks. Psychological and educational interventions (such as supportive counselling sessions and brief educational sessions) may help women to reduce their alcohol intake during pregnancy.
Four randomized controlled studies were included in the review; individual studies suggest that educational and counselling interventions may encourage women to abstain from alcohol or reduce the amount of alcohol they drink in pregnancy. The studies involved women who were less than 28 weeks pregnant who were consuming some alcohol. All were carried out in the USA. The interventions ranged from a 10-minute education session and provision of a self-help manual through to an hour-long motivational interview with reinforcement at each prenatal visit. Women in the control groups generally received routine care, which may have included advice on reducing alcohol intake. Outcomes were measured in different ways, and so results have been presented separately for each study. The studies provided very limited information on the effects of interventions on the health of women and their babies.
There was very little information provided in these studies on the effects of interventions on the health of mothers and babies. There is an urgent need for more information in this area.
ACKNOWLEDGEMENTS
Rebecca Zakoor, Health Sciences Library, St Michael’s Hospital.
Audrey Hughes, Library Assistant, Health Sciences Library, St Michael’s Hospital.
As part of the pre-publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group’s international panel of consumers and the Group’s Statistical Adviser.
SOURCES OF SUPPORT
Internal sources
Department of Pediatrics, St Michael’s Hospital, Toronto, Canada.
External sources
National Institute for Health Research, UK.
NIHR NHS Cochrane Collaboration Programme Grant Scheme award for NHS-prioritised centrally-managed, pregnancy and childbirth systematic reviews: CPGS02
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
The background section has been extended and the methods section has now been updated.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | RCT (individual randomization). | |
| Participants | Setting: women attending for prenatal care at a Boston, USA hospital. Women were screened at their first antenatal appointment 250 pregnant women meeting inclusion criteria randomized. Inclusion criteria: women identified as being at risk for prenatal risk drinking. All had consumed some alcohol in the 6 months before recruitment and scored 2 or more on an alcohol screening tool T-ACE (none of the women had current diagnoses of alcohol or drug abuse dependence). More than half of the women included reported that they were abstaining from alcohol at the time of recruitment Exclusion criteria: gestational age > 28 weeks, no alcohol consumed in the previous 6 months, miscarriage, planned to attend elsewhere for care, planned abortion, non-English speaking, participation in substance abuse programme Baseline characteristics of experimental and comparison group participantswere reported as being similar. Mean gestation at recruitment = 16 weeks |
|
| Interventions | Experimental group: comprehensive alcohol assessment and 45-minute educational counselling intervention including identifying the woman’s drinking goal, motivation, risk situation for drinking and alternatives to alcohol. Women were provided with a manual on how to prevent alcohol-related problems at end of counselling Comparison group: comprehensive alcohol assessment but no active intervention Both groups received $50 for completing the assessment and $75 for the postpartum follow-up interview |
|
| Outcomes | Antepartum alcohol consumption; reductions in and abstinence from alcohol; birth weights; Apgar scores at 1 and 5 minutes | |
| Notes | Authors contacted formore information on study design and results and kindly provided some additional information | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random assignment. |
| Allocation concealment? | Unclear | No information. |
| Blinding? Participants |
No | Educational intervention by physician. |
| Blinding? Care providers |
No | |
| Blinding? Outcome assessors |
Unclear | Postpartum outcome assessor reported to be blind to results of initial assessment |
| Incomplete outcome data addressed? All outcomes |
Yes | Few women lost to follow up. (Participants were paid to complete assessments.) |
| Free of selective reporting? | Unclear | Few direct comparisons between experimental and comparison groups |
| Free of other bias? | Unclear | Results difficult to interpret. Experimental and comparison groups were not compared for many outcomes |
| Methods | Stratified RCT (stratified by level of alcohol consumption). | |
| Participants | 42 pregnant women who had consumed at least 1 alcoholic drink in the previous month (but were not seeking help for drug or alcohol problems) were recruited. Women were attending for care at a New Mexico hospital It was not clear at what gestational age women were recruited to this study |
|
| Interventions | 1-hour drinking assessments were completed by all participants before randomization Intervention: the women received a 1-hour motivational interview to raise awareness of the risks to the baby of consuming alcohol and support and encouragement to reduce consumption Comparsion group: letter informing them of risks and referring them to their usualhealthcare providers |
|
| Outcomes | Abstinence from alcohol, reduction in alcohol consumption. | |
| Notes | Partners or significant others were asked to corroborate accounts. Women paid $20 for baseline assessment and $10 for follow-up assessment The study author kindly provided additional unpublished data for inclusion in the review |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Stratified to achieve equal distribution of heavy and light drinkers in each group |
| Allocation concealment? | Unclear | Described as: “interviewer privately opened a prepared envelope” |
| Blinding? Participants |
No | Educational intervention. |
| Blinding? Care providers |
No | |
| Blinding? Outcome assessors |
Unclear | Reported that assessors were not aware of group allocation but information was collected at interviews |
| Incomplete outcome data addressed? All outcomes |
Unclear | 19% attrition (34 of 42 recruited followed up). |
| Free of other bias? | Unclear | Results difficult to interpret. Control group had higher levels of alcohol consumption at baseline |
| Methods | Cluster randomized trial (12 clinics randomized to 2 conditions) | |
| Participants | 345 women consuming alcohol during pregnancy. 245 women were followed to third trimester Inclusion criteria: Pregnant women attending a special supplemental nutrition program for women, infants and children were screened and those described as “current drinkers” (any alcohol since pregnancy recognition) were included Exclusion criteria: 24 women were referred to alcohol treatment programs, most exclusions were women who had not consumed alcohol since conception (3112) or had not consumed any alcohol since pregnancy recognition (603) Women were recruited at an average of 18 weeks’ gestation. |
|
| Interventions | Both groups had a comprehensive assessment of alcohol consumption at baseline Experimental group: brief 10- to 15-minute intervention by a nutritionist using a script to encourage reduction in alcohol consumption. Reinforcement at each prenatal visit. Comparison group: women were assessed for alcohol use and advised to stop drinking during pregnancy |
|
| Outcomes | Newborn outcomes including birthweight, length and condition at birth. Maternal abstinence from alcohol in pregnancy | |
| Notes | Analysis by logistic regression which took account of cluster randomization and other factors such as gestational age at booking. Results difficult to interpret The study author kindly provided further unpublished data for inclusion in the review |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Not described. |
| Allocation concealment? | Unclear | 12 clinics randomized to 2 conditions, it was not clear how randomization was achieved |
| Blinding? Participants |
No | Educational intervention. |
| Blinding? Care providers |
No | |
| Incomplete outcome data addressed? All outcomes |
No | High risk of bias. Attrition 24.6% in the control group and 27.8% in the experimental group. Those lost to follow up were different in terms of race and education compared to those remaining part of the sample |
| Free of selective reporting? | Unclear | Pre-specified outcomes reported but results difficult to interpret |
| Methods | RCT. | |
| Participants | Intervention aimed at low-income pregnant women attending public health clinics in urban settings in the USA Inclusion criteria: 78 women who reported that they had consumed alcohol in the past month. Women were recruited at approximately 12 weeks’ gestation Exclusion criteria: women who were > 25 weeks pregnant or who had not consumed any alcohol in the previous month |
|
| Interventions | Intervention group: usual care plus a cognitive-behavioural self-help intervention based on a pilot study, including a 10-minute educational session with a self-help manual to be completed by women over 9 days Comparison group: usual care. Information on the effects of alcohol in pregnancy was routinely provided by clinic staff and a video on prenatal care included alcohol advice |
|
| Outcomes | Quantitiy and frequency of alcohol consumption. | |
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as “randomly assigned”. |
| Allocation concealment? | Unclear | No information on how randomization was carried out. “Educators were blinded to randomization status until prior to the intervention” |
| Blinding? Participants |
No | Educational intervention. Not feasible. |
| Blinding? Care providers |
No | |
| Blinding? Outcome assessors |
No | |
| Incomplete outcome data addressed? All outcomes |
Yes | Less than 10% attrition (72/78 followed up). |
| Free of selective reporting? | Unclear | Difficult to interpret results. Denominators for some outcomes not provided |
| Free of other bias? | Unclear | Some differences at baseline between intervention and control groups. Used a “bogus” breathalyzer device to pretend to test alcohol levels |
RCT: randomized controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aalto 2000 | Controlled study of 118 female heavy drinkers (n = 118) evaluated the effectiveness of long-lasting brief alcohol intervention counselling for women in a routine general practice setting. The study did not meet criteria for inclusion as it did not include women that were pregnant or who were planning pregnancy |
| Belizan 1995 | Controlled study of 2235 pregnant women evaluated the impact of health education during pregnancy on behaviour and utilization of health resources. The study did not meet criteria as it did not meet criteria for types of intervention. Knowledge about the effects of alcohol use was only one component of a broad intervention which included reinforcement of social support network, knowledge about pregnancy and delivery and reinforcement of adequate health services utilization |
| Calabro 1996 | This study focused on pregnant women attending public health clinics in southwestern USA. The aim of the study was to compare the effectiveness of educational materials written at different reading levels (for 3rd or 10th grade reading ages). Post-tests were carried out immediately after the intervention. Outcomes included recall, knowledge and attitudes but no information on outcomes relevant to the review was collected |
| Eisen 2000 | The impact on drug prevention, education and treatment projects versus an alternative or no intervention for pregnant and postpartum women (n = 658) was evaluated. The study did not meet criteria as it used a quasiexperimental design |
| Eustace 2000 | This study was not randomized. Women were allocated to groups by day of clinic attendance |
| Floyd 2007 | Study in 6 community-based settings (jail, alcohol treatment centres, primary care and hospital gynecology clinics). Aimed at women aged 18-44 but explicitly excluded pregnant women or women planning pregnancy in the next 9 months |
| Fox 1987 | In this study the intervention was specifically promoting smoking cessation. Although data on alcohol use and other health behaviours in pregnancy were collected, the intervention did not included any advice on alcohol consumption |
| Grant 2005 | This study examined a home visitation intervention for alcohol and drug abusing women. The sample included both pregnant women and postpartum women. The study was not a RCT. Recruitment in different centres was carried out in different ways, in one centre there was quasi-randomized recruitment, whereas in 2 other centres all women recruited were allocated to the intervention condition |
| Handmaker 1999b | In this study the intervention was directed at healthcare practitioners and not at pregnant women |
| Hankin 2002 | The intervention in this study was carried out in the postnatal period |
| Larsson 1983 | The purpose of this study was to develop earlier detection of maternal alcohol abuse and treatment including support and counselling for those with excessive alcohol use. Outcomes of the mothers and infants were included. The study did meet inclusion criteria as it was not a RCT |
| Manwell 2000 | RCT of women in their childbearing years (n = 205) examined the impact of a brief intervention on alcohol use reduction. The study did not meet criteria for inclusion in this review as it excluded pregnant women |
| Meberg 1986 | This controlled study examined reduction of alcohol in two groups of pregnant women: an intervention group (n = 58) and a control group (n = 74). In the intervention group, structured interviews including counselling on reduction of alcohol consumption and potential benefits to the fetus, and interview. The control group received an interview after delivery. The study lacked randomization and thus was not included in the review |
| Palinkas 1996 | Study focusing on high-risk adolescent women at risk of drug use or pregnancy. The intervention was not specifically aimed at pregnant women or women planning pregnancy. A small number of participants were pregnant (approximately a third were either pregnant or had young children). Alcohol consumption during pregnancy and other pregnancy-related outcomes were not measured |
| Reading 1982 | In this study the intervention was a routine ultrasound examination at the first antenatal visit with verbal feedback. The control group received the ultrasound examination without feedback. Women in the feedback group were shown the fetal size, shape and movement. The intervention did not include any education or recommendations regarding alcohol use in pregnancy |
| Rosett 1983 | The researchers prospectively examined the drinking patterns among pregnant women at Boston City Hospital between 1974 and 1979. Of 49 pregnant problem drinkers identified who participated in at least 3 counselling sessions, 33 (67%) reduced alcohol consumption before the third trimester. Benefits to the offspring were noted. The study failed to meet inclusion criteria as it was not a RCT |
| Scott 1990 | RCT of 72 women. Women in the treatment group received 10 minutes of advice from their general practitioner to reduce alcohol consumption. Women in the control group received no advice, unless on request. The study was excluded as there was no indication that the women were pregnant or planning pregnancy. Mean age was 44.4 and 47.2 in the treatment and control group respectively |
RCT: randomized controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | RCT. |
| Participants | 304 women attending a Boston (USA) hospital who were assessed at being at risk of consuming alcohol in pregnancy |
| Interventions | Brief intervention (lasting approximately 25 minutes) for women and their partners encouraging abstinence from alcohol. The intervention involved goal setting and strategies for behaviour modification. The control group were assessed but received no active intervention |
| Outcomes | Abstinence from alcohol in pregnancy. Reduction in alcohol consumption |
| Notes | Author contacted for more information on trial results August 2008 |
RCT: randomized controlled trial
DATA AND ANALYSES
Comparison 1.
Brief alcohol reduction intervention versus alcohol assessment only
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Women who were abstinent following the intervention | 1 | 250 | Risk Ratio (M-H, Fixed, 95% CI) | 1.11 [0.93, 1.33] |
| 2 Women who remained abstinent throughout the study | 1 | 142 | Risk Ratio (M-H, Fixed, 95% CI) | 1.20 [1.01, 1.42] |
| 3 Number of antenatal alcohol drinking episodes | 1 | 250 | Mean Difference (IV, Fixed, 95% CI) | −0.30 [−0.68, 0.08] |
Comparison 2.
Brief cognitive behavioural intervention versus usual advice
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number abstaining from alcohol at follow up | 1 | 72 | Risk Ratio (M-H, Fixed, 95% CI) | 1.25 [0.97, 1.61] |
| 2 Average drinks per month (post-intervention) | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | −0.78 [−1.58, 0.02] |
Analysis 1.1. Comparison 1 Brief alcohol reduction intervention versus alcohol assessment only, Outcome 1 Women who were abstinent following the intervention
Review: Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy
Comparison: 1 Brief alcohol reduction intervention versus alcohol assessment only
Outcome: 1 Women who were abstinent following the intervention
 |
Analysis 1.2. Comparison 1 Brief alcohol reduction intervention versus alcohol assessment only, Outcome 2 Women who remained abstinent throughout the study
Review: Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy
Comparison: 1 Brief alcohol reduction intervention versus alcohol assessment only
Outcome: 2 Women who remained abstinent throughout the study
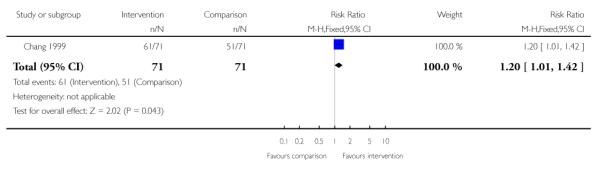 |
Analysis 1.3. Comparison 1 Brief alcohol reduction intervention versus alcohol assessment only, Outcome 3 Number of antenatal alcohol drinking episodes
Review: Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy
Comparison: 1 Brief alcohol reduction intervention versus alcohol assessment only
Outcome: 3 Number of antenatal alcohol drinking episodes
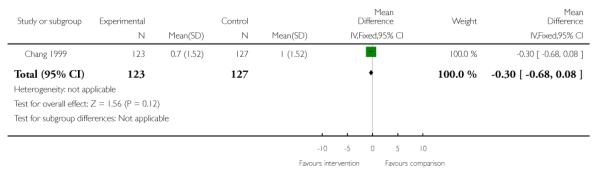 |
Analysis 2.1. Comparison 2 Brief cognitive behavioural intervention versus usual advice, Outcome 1 Number abstaining from alcohol at follow up
Review: Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy
Comparison: 2 Brief cognitive behavioural intervention versus usual advice
Outcome: 1 Number abstaining from alcohol at follow up
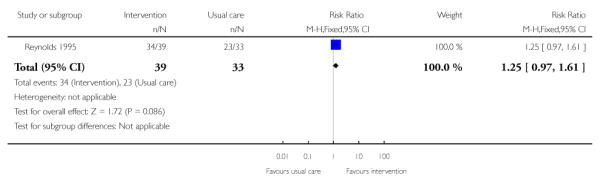 |
Analysis 2.2. Comparison 2 Brief cognitive behavioural intervention versus usual advice, Outcome 2 Average drinks per month (post-intervention)
Review: Psychological and/or educational interventions for reducing alcohol consumption in pregnant women and women planning pregnancy
Comparison: 2 Brief cognitive behavioural intervention versus usual advice
Outcome: 2 Average drinks per month (post-intervention)
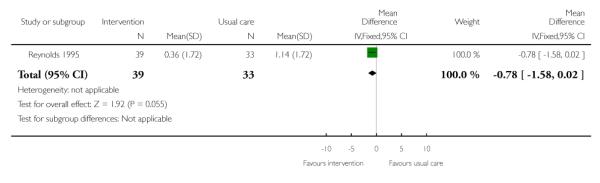 |
HISTORY
Protocol first published: Issue 2, 2003
Review first published: Issue 2, 2009
| Date | Event | Description |
|---|---|---|
| 8 May 2008 | Amended | Converted to new review format. |
Appendix 1. Search strategies
CENTRAL (The Cochrane Library)
A qualified librarian assisted the authors in searching the databases.
MeSH and keywords: (alcohol OR alcohol affected OR prenatal alcohol exposure OR prenatally alcohol exposed OR fetal alcohol syndrome OR fetal alcohol) AND (pregnancy OR alcohol cessation OR psychological interventions OR educational interventions OR cognitive interventions OR behavioural interventions OR brief interventions).
We adapted this search strategy for MEDLINE (1966 to November 2007), EMBASE (1980 to November 2007), CINAHL (1982 to November 2007), Counsel.Lit (1980 to November 2007), PsycLIT (1974 to November 2007) and PsycINFO (1967 to November 2007) by selecting MeSH and keywords from their respective thesauri.
Footnotes
DECLARATIONS OF INTEREST None known.
References to studies included in this review
* Indicates the major publication for the study
- Chang 1999 {published and unpublished data} .Chang G. Personal communication. Email communication received. Aug, 2008. ; Chang G, Goetz MA, Wilkins-Haug L, Berman S. A brief intervention for prenatal alcohol use: an in-depth look. Journal of Substance Abuse Treatment. 2000;18:365–9. doi: 10.1016/s0740-5472(99)00105-1. [DOI] [PubMed] [Google Scholar]; *; Chang G, Wilkins-Haug L, Berman S, Goetz MA. Brief intervention for alcohol use in pregnancy: randomized trial. Addiction. 1999;94(10):1499–508. doi: 10.1046/j.1360-0443.1999.941014996.x. [DOI] [PubMed] [Google Scholar]
- Handmaker 1999a {published data only} .Handmaker N, Miller W, Manicke M. Findings of a pilot study of motivational interviewing with pregnant drinkers. Journal of Studies on Alcohol. 1999;60:285–7. doi: 10.15288/jsa.1999.60.285. [DOI] [PubMed] [Google Scholar]
- O’Connor 2007 {published and unpublished data} .O’Connor M, Whaley S. Brief intervention for alcohol use by pregnant women. American Journal of Public Health. 97(2):252–8. doi: 10.2105/AJPH.2005.077222. 200. [DOI] [PMC free article] [PubMed] [Google Scholar]; O’Connor MJ. Personal communication. Email communication received. Jul, 2008.
- Reynolds 1995 {published data only} .Reynolds KD, Coombs DW, Lowe JB, Peterson PL, Gayoso E. Evaluation of a self-help program to reduce alcohol consumption among pregnant women. International Journal of the Addictions. 1995;30(4):427–43. doi: 10.3109/10826089509048735. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Aalto 2000 {published data only} .Aalto M, Saksanen R, Laine P, Forsstrom R, Ralkaa M, Kiviluoto M, et al. Brief intervention for female heavy drinkers in routine general practice: a 3-year randomized, controlled study. Alcoholism, Clinical and Experimental Research. 2000;24(11):1680–6. [PubMed] [Google Scholar]
- Belizan 1995 {published data only} .Belizan JM, Barros F, Langer A, Farnot U, Victora C, Villar J. Impact of health education during pregnancy on behavior and utilization of health resources. American Journal of Obstetrics and Gynecology. 1995;173(3):894–9. doi: 10.1016/0002-9378(95)90362-3. [DOI] [PubMed] [Google Scholar]
- Calabro 1996 {published data only} .Calabro K, Taylor WC, Kapadia A. Pregnancy, alcohol use and the effectiveness of written health education materials. Patient Education & Counseling. 1996;29(3):301–9. doi: 10.1016/s0738-3991(96)00944-5. [DOI] [PubMed] [Google Scholar]
- Eisen 2000 {published data only} .Eisen M, Keyser-Smith J, Dampeer J, Sambrano S. Evaluation of substance use outcomes in demonstration projects for pregnant and postpartum women and their infants: findings from a quasi-experiment. Addictive Behaviors. 2000;25(1):123–9. doi: 10.1016/s0306-4603(98)00116-6. [DOI] [PubMed] [Google Scholar]
- Eustace 2000 {published data only} .Eustace LW. Fetal alcohol syndrome prevention: affecting maternal alcohol consumption behavior through nurse supportive-educative intervention [thesis] University of Alabama, at Birmingham; Birmingham: 2000. [Google Scholar]
- Floyd 2007 {published data only} .Floyd RL, Sobell M, Velasquez MM, Ingersoll K, Nettleman M, Sobell L, et al. Preventing alcohol-exposed pregnancies: a randomized controlled trial. American Journal of Preventive Medicine. 2007;32(1):1–10. doi: 10.1016/j.amepre.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox 1987 {published data only} .Fox NL, Sexton MJ, Hebel JR. Alcohol consumption among pregnant smokers: effects of a smoking cessation intervention program. American Journal of Public Health. 1987;77:211–3. doi: 10.2105/ajph.77.2.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant 2005 {published data only} .Grant TM, Ernst CC, Streissguth A, Stark K. Preventing alcohol and drug exposed births in Washington state: intervention findings from three parent-child assistance program sites. American Journal of Drug and Alcohol Abuse. 2005;31(3):471–90. doi: 10.1081/ada-200056813. [DOI] [PubMed] [Google Scholar]
- Handmaker 1999b {published data only} .Handmaker NS, Hester RK, Delaney HD. Videotaped training in alcohol counseling for obstetric care practitioners: a randomized controlled trial. Obstetrics & Gynecology. 1999;93(2):213–8. doi: 10.1016/s0029-7844(98)00377-9. [DOI] [PubMed] [Google Scholar]
- Hankin 2002 {published data only} .Hankin J, Sokol R. Improved neurobehavioral outcomes in alcohol exposed infants following brief intervention [abstract] American Journal of Obstetrics and Gynecology. 2002;187(6 Pt 2):S94. [Google Scholar]
- Larsson 1983 {published data only} .Larsson G. Prevention of fetal alcohol effects. An antenatal program for early detection of pregnancies at risk. Acta Obstetricia et Gynecologica Scandinavica. 1983;62(2):171–8. doi: 10.3109/00016348309155786. [DOI] [PubMed] [Google Scholar]
- Manwell 2000 {published data only} .Manwell LB, Fleming M, Mundt M, Stauffacher EA, Barry KL. Treatment of problem alcohol use in women of childbearing age: results of a brief intervention trial. Alcoholism, Clinical and Experimental Research. 2000;24(10):1517–24. [PubMed] [Google Scholar]
- Meberg 1986 {published data only} .Meberg A, Halvorsen B, Holter B, Ek IJ, Askeland A, Gaaserud W, et al. Moderate alcohol consumpton - need for intervention programs in pregnancy? Acta Obstetricia et Gynecologica Scandinavica. 1986;65(8):861–4. doi: 10.3109/00016348609157039. [DOI] [PubMed] [Google Scholar]
- Palinkas 1996 {published data only} .Palinkas LA, Atkins CJ, Miller C, Ferreira D. Social skills training for drug prevention in high-risk female adolescents. Preventive Medicine. 1996;25(6):692–701. doi: 10.1006/pmed.1996.0108. [DOI] [PubMed] [Google Scholar]
- Reading 1982 {published data only} .Reading AE, Campbell S, Cox DN, Sledmere CM. Health beliefs and health care behaviour in pregnancy. Psychological Medicine. 1982;12:379–83. doi: 10.1017/s0033291700046717. [DOI] [PubMed] [Google Scholar]
- Rosett 1983 {published data only} .Rosett HL, Weiner L, Edelin K. Treatment experience with pregnant problem drinkers. JAMA. 1983;249(15):2029–33. [PubMed] [Google Scholar]
- Scott 1990 {published data only} .Scott E, Anderson P. Randomized controlled trial of general practitioner intervention in women with excessive alcohol consumption. Drug and Alcohol Review. 1990;10:313–21. doi: 10.1080/09595239100185371. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
- Chang 2005 {published data only} .Chang G, McNamara TK, Orav EJ, Koby D, Lavigne A, Ludman B, et al. A brief intervention for prenatal alcohol use: results from a randomized trial of 304 couples [abstract]. 15th Annual Meeting of American Academy of Addiction Research.2004. p. 26. [Google Scholar]; Chang G, McNamara TK, Orav EJ, Wilkins-Haug L. Brief intervention for prenatal alcohol use: the role of drinking goal selection. Journal of Substance Abuse Treatment. 2006;31(4):419–24. doi: 10.1016/j.jsat.2006.05.016. [DOI] [PubMed] [Google Scholar]; Chang G, McNamara TK, Orav J, Koby D, Lavigne A, Ludman B, et al. Brief intervention for prenatal alcohol use: a randomized trial. Obstetrics & Gynecology. 2005;105(5 Pt 1):991–8. doi: 10.1097/01.AOG.0000157109.05453.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
- AAP Statement 2000 .American Academy of Pediatrics Fetal alcohol syndrome and alcohol related neurodevelopmental disorders. Pediatrics. 2000;106:358–61. [PubMed] [Google Scholar]
- Aase 1995 .Aase JM, Jones KL, Clarren SK. Do we need the term “FAE”? Pediatrics. 1995;95:428–30. [PubMed] [Google Scholar]
- Abel 1991 .Abel EL, Sokol RJ. A revised conservative estimate of the incidence of FAS and its economic impact. Alcoholism, Clinical and Experimental Research. 1991;15:514–24. doi: 10.1111/j.1530-0277.1991.tb00553.x. [DOI] [PubMed] [Google Scholar]
- Abel 1995 .Abel EL, Hannigan JH. Maternal risk factors in fetal alcohol syndrome: provocative and permissive influences. Neurotoxicology and Teratology. 1995;17:445–62. doi: 10.1016/0892-0362(95)98055-6. [DOI] [PubMed] [Google Scholar]
- Ait-Daoud 2001 .Ait-Daoud N, Johnson BA, Prihoda TJ, Hargita ID. Combining ondansetron and naltrexone reduces craving among biologically predisposed alcoholics: preliminary clinical evidence. Psychopharmacology. 2001;154:23–7. doi: 10.1007/s002130000607. [DOI] [PubMed] [Google Scholar]
- Armstrong 1992 .Armstrong BG, McDonald AD, Sloan M. Cigarette, alcohol, and coffee consumption and spontaneous abortion. American Journal of Public Health. 1992;82(1):85–7. doi: 10.2105/ajph.82.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astley 2000 .Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: introducing the 4-digit diagnostic code. Alcohol and Alcoholism. 2000;35:400–10. doi: 10.1093/alcalc/35.4.400. [DOI] [PubMed] [Google Scholar]
- Bandura 1986 .Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Baumann 2006 .Baumann P, Schild C, Hume RF, Sokol RJ. Alcohol abuse--a persistent preventable risk for congenital anomalies. International Journal of Gynecology & Obstetrics. 2006;95(1):66–72. doi: 10.1016/j.ijgo.2006.05.033. [DOI] [PubMed] [Google Scholar]
- Brown 2001 .Brown SA, D’Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from adolescent alcohol and drug treatment. Journal of Studies on Alcohol. 2001;62:381–8. doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Chang 2000 .Chang G, Goetz MA, Wilkins-Haug L, Berman S. A brief intervention for prenatal alcohol use: an in-depth look. Journal of Substance Abuse Treatment. 2000;18:365–9. doi: 10.1016/s0740-5472(99)00105-1. [DOI] [PubMed] [Google Scholar]
- Chick 1992 .Chick J, Gough K, Falkowski W, Kershaw P, Hore B, Mehta B. Disulfiram treatment of alcoholism. British Journal of Psychiatry. 1992;161:84–9. doi: 10.1192/bjp.161.1.84. [DOI] [PubMed] [Google Scholar]
- Chudley 2005 .Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N, et al. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Canadian Medical Association Journal. 2005;172:S1–S21. doi: 10.1503/cmaj.1040302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchill 2003 .Churchill R, Hunot V, Corney R, Knapp M, McGuire H, Tylee A, et al. Brief psychological therapies versus treatment as usual for depression. Cochrane Database of Systematic Reviews. 2003;(Issue 1) [DOI: 10.1002/ 14651858.CD001763.pub2] [Google Scholar]
- Clark 1999 .Clark KA, Dawson S, Martin SL. The effect of implementing a more comprehensive screening for substance use among pregnant women in North Carolina. Maternal & Child Health Journal. 1999;3(3):161–6. doi: 10.1023/a:1022397906325. [DOI] [PubMed] [Google Scholar]
- Coles 2002 .Coles CD. Fetal alcohol exposure and attention: moving beyond ADHD. Alcohol Research and Health. 2001;25:199–203. [PMC free article] [PubMed] [Google Scholar]
- Connor 2000 .Connor PD, Sampson PD, Bookstein FL, Barr HM, Streissguth AP. Direct and indirect effects of prenatal alcohol damage on executive function. Developmental Neuropsychology. 2000;18:331–54. doi: 10.1207/S1532694204Connor. [DOI] [PubMed] [Google Scholar]
- Connors 2001 .Connors GJ, Walitzer KS. Reducing alcohol consumption among heavy drinking women: evaluating the contributions of life-skills training and booster sessions. Journal of Consulting and Clinical Psychology. 2001;69:447–56. doi: 10.1037//0022-006x.69.3.447. [DOI] [PubMed] [Google Scholar]
- CPS Statement 2002 .Canadian Pediatric Society Fetal alcohol syndrome. Pediatric Child Health. 2002;7:161–74. [Google Scholar]
- Czeizel 2004 .Czeizel AE, Petik D, Puho E. Smoking and alcohol drinking during pregnancy. The reliability of retrospective maternal self-reported information. Central European Journal of Public Health. 2004;12(4):179–83. [PubMed] [Google Scholar]
- Ebrahim 1999 .Ebrahim SH, Diekman ST, Floyd RL, Decoufle P. Comparison of binge drinking among pregnant and nonpregnant women, United States, 1991-1995. American Journal of Obstetrics and Gynecology. 1999;180(1 Pt 1):1–7. doi: 10.1016/s0002-9378(99)70139-0. [DOI] [PubMed] [Google Scholar]
- Ellis 1962 .Ellis A. Reason and emotion in psychotherapy. Lyle Stuart; New York: 1962. [Google Scholar]
- Fleming 2002 .Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcoholism, Clinical and Expermental Research. 2002;26:36–43. [PubMed] [Google Scholar]
- Goodlett 2005 .Goodlett CR, Horn KH, Zhou FC, Goodlett Charles R, Horn Kristin H, Zhou Feng C. Alcohol teratogenesis: mechanisms of damage and strategies for intervention. Experimental Biology & Medicine. 2005;230(6):394–406. doi: 10.1177/15353702-0323006-07. [DOI] [PubMed] [Google Scholar]
- Greenbaum 2002 .Greenbaum R, Koren G. Fetal alcohol spectrum disorder-new diagnostics initiatives. Pediatrics and Child Health. 2002;7:139–41. doi: 10.1093/pch/7.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannigan 2000 .Hannigan JH, Armant DR. Alcohol in pregnancy and neonatal outcome. Seminars in Neonatology. 2000;5(3):243–54. doi: 10.1053/siny.2000.0027. [DOI] [PubMed] [Google Scholar]
- Harvard 2002 .Anonymous Drug treatments for alcoholism. Harvard Mental Health Letter. 2002;18:4–7. [PubMed] [Google Scholar]
- Harwood 1985 .Harwood HJ, Napolitano DM. Economic implications of the fetal alcohol syndrome. Alcohol Health and Research World. 1985;10:38–43. [Google Scholar]
- Henderson 2007 .Henderson J, Gray R, Brocklehurst P. Systematic review of the effects of low-moderate prenatal alcohol exposure on pregnancy outcome. BJOG: an international journal of obstetrics and gynaecology. 2007;114(3):243–52. doi: 10.1111/j.1471-0528.2006.01163.x. [DOI] [PubMed] [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.0.0. [updated February 2008]. Available from www.cochrane-handbook.org. [Google Scholar]
- Hoyme 2005 .Hoyme HE, May PA, Kalberg WO, Kodituwakku P, Gossage JP, Trujillo PM, et al. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: clarification of the 1996 institute of medicine criteria. Pediatrics. 2005;115(1):39–47. doi: 10.1542/peds.2004-0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ICAP 1999 .International Center for Alcohol Policies . ICAP Reports. Vol. 6. International Center for Alcohol Policies; Washington DC: 1999. Government policies on alcohol and pregnancy; pp. 1–7. [Google Scholar]
- Jaddoe 2007 .Jaddoe VW, Bakker R, Hofman A, Mackenbach JP, Moll HA, Steegers EA, et al. Moderate alcohol consumption during pregnancy and the risk of low birth weight and preterm birth. The generation R study. Annals of Epidemiology. 2007;17(10):834–40. doi: 10.1016/j.annepidem.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Johnson 1996 .Johnson V, Swayze V, Sato Y, Andreasen N. Fetal alcohol syndrome: craniofacial and central nervous system manifestations. American Journal of Medical Genetics. 1996;61:329–39. doi: 10.1002/(SICI)1096-8628(19960202)61:4<329::AID-AJMG6>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Klerman 1984 .Klerman G, Weissman M, Rounsaville B, Chevron E. Interpersonal psychotherapy of depression. Basic Books; New York: 1984. [Google Scholar]
- Loock 2005 .Loock C, Conry J, Cook JL, Chudley AE, Rosales T. Identifying fetal alcohol spectrum disorder in primary care. Canadian Medical Association Journal. 2005;172(5):628–30. doi: 10.1503/cmaj.050135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lui 2008 .Lui S, Terplan M, Smith EJ. Psychosocial interventions for women enrolled in alcohol treatment during pregnancy. Cochrane Database of Systematic Reviews. 2008;(Issue 3) doi: 10.1002/14651858.CD006753.pub2. [DOI: 10.1002/14651858.CD006753.pub2] [DOI] [PubMed] [Google Scholar]
- Lumley 2004 .Lumley J, Oliver SS, Chamberlain C, Oakley L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews. 2004;(Issue 3) doi: 10.1002/14651858.CD001055.pub2. [DOI: 10.1002/14651858. CD001055.pub2] [DOI] [PubMed] [Google Scholar]
- Malan 1963 .Malan D. A study of brief psychotherapy. Plenum; London: 1963. [Google Scholar]
- Mariscal 2006 .Mariscal M, Palma S, Llorca J, Perez-Iglesias R, Pardo-Crespo R, Delgado-Rodriguez M, et al. Pattern of alcohol consumption during pregnancy and risk for low birth weight. Annals of Epidemiology. 2006;16(6):432–8. doi: 10.1016/j.annepidem.2005.07.058. [DOI] [PubMed] [Google Scholar]
- Mason 2001 .Mason BJ. Treatment of alcohol-dependent outpatients with acamposate: a clinical review. Journal of Clinical Psychiatry. 2001;62:42–8. [PubMed] [Google Scholar]
- Mattson 2001 .Mattson SN, Schoenfeld AM, Riley EP. Teratogenic effects of alcohol on brain and behavior. Alcohol Research and Health. 2001;25:185–91. [PMC free article] [PubMed] [Google Scholar]
- May 2007 .May PA, Gossage JP, Marais AS, Adnams CM, Hoyme HE, Jones KL, et al. The epidemiology of fetal alcohol syndrome and partial FAS in a South African community. Drug & Alcohol Dependence. 2007;88(2-3):259–71. doi: 10.1016/j.drugalcdep.2006.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntosh 1997 .McIntosh MC, Leigh G, Baldwin NJ, Marmulak J. Reducing alcohol consumption. Comparing brief methods in family practice. Canadian Family Physician. 1997;43:1959–62. 1965–7. [PMC free article] [PubMed] [Google Scholar]
- Nathanson 2007 .Nathanson V, Jayesinghe N, Roycroft G. Is it all right for women to drink small amounts of alcohol in pregnancy? No. BMJ. 2007;335(7625):857. doi: 10.1136/bmj.39356.489340.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nora 1977 .Nora AH, Nora JJ, Blu J. Limb-reduction anomalies in infants born to disulfiram-treated alcoholic mothers. Lancet. 1977;2:664. doi: 10.1016/s0140-6736(77)92534-x. [DOI] [PubMed] [Google Scholar]
- O’Brien 2007 .O’Brien P. Is it all right for women to drink small amounts of alcohol in pregnancy? Yes. BMJ. 2007;335(7625):856. doi: 10.1136/bmj.39371.381308.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price 1995 .Price V, Archbold J. Development and application of social learning theory. British Journal of Nursing. 1995;4:1263–8. doi: 10.12968/bjon.1995.4.21.1263. [DOI] [PubMed] [Google Scholar]
- Randall 2001 .Randall CL. Alcohol and pregnancy: highlights from three decades of research. Journal of Studies on Alcohol. 2001;62:554–61. doi: 10.15288/jsa.2001.62.554. [DOI] [PubMed] [Google Scholar]
- Reitnauer 1997 .Reitnauer PJ, Callanan NP, Farber RA, Aylsworth AS. Prenatal exposure to disulfiram implicated in the cause of malformations in discordant monozygotic twins. Teratology. 1997;56:358–62. doi: 10.1002/(SICI)1096-9926(199712)56:6<358::AID-TERA3>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- RevMan 2008 .The Cochrane Collaboration . Review Manager (RevMan). 5.0. The Nordic Cochrane Centre: The Cochrane Collaboration; Copenhagen: 2008. [Google Scholar]
- Rice 1991 .Rice D, Kelman S, Miller L. The economic cost of alcohol abuse. Public Health Reports. 1991;106:307–16. [PMC free article] [PubMed] [Google Scholar]
- Roberts 2000 .Roberts G, Nanson J. Canada’s Drug Strategy Division. Health Canada; 2000. Best practices: fetal alcohol syndrome/ fetal alcohol effects and the effects of other substance use during pregnancy. [Google Scholar]
- Rogers 1961 .Rogers C. On becoming a person. Houghon Mifflin; Boston: 1961. [Google Scholar]
- Sampson 1997 .Sampson P, Streissguth A, Bookstein F, Little R, Clarren S, Dehaene P. Incidence of fetal-alcohol syndrome and prevalence of alcohol-related neurodevelopmental disorder. Teratology. 1997;56:317–26. doi: 10.1002/(SICI)1096-9926(199711)56:5<317::AID-TERA5>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Schorling 1993 .Schorling JB. The prevention of prenatal alcohol use: a critical analysis of intervention studies. Journal of Studies on Alcohol. 1993;54:261–7. doi: 10.15288/jsa.1993.54.261. [DOI] [PubMed] [Google Scholar]
- Sokol 1981 .Sokol RJ. Alcohol and abnormal outcomes of pregnancy. Canadian Medical Association Journal. 1981;125(2):143–8. [PMC free article] [PubMed] [Google Scholar]
- Sokol 2003 .Sokol RJ, Delaney-Black V, Nordstrom B. Fetal alcohol spectrum disorder. JAMA. 2003;10(22):2996–9. doi: 10.1001/jama.290.22.2996. [DOI] [PubMed] [Google Scholar]
- Stade 2006 .Stade B, Stevens B, Ungar W, Beyene J, Koren G. Burden of prenatal exposure to alcohol: measurement of quality of life and cost. Health and Quality of Life Outcomes. 2006;3(81):1–10. doi: 10.1186/1477-7525-4-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streeton 2001 .Streeton C, Whelan G. Naltrexone, a relapse prevention maintenance treatment of alcohol dependence: a meta-analysis of randomized controlled trials. Alcohol and Alcoholism. 2001;36:544–62. doi: 10.1093/alcalc/36.6.544. [DOI] [PubMed] [Google Scholar]
- Streissguth 1996 .Streissguth AP, Barr HM, Kogan J, Bookstein FL. Understanding the occurrence of secondary disabilities in clients with fetal alcohol syndrome (FAS) and fetal alcohol effects (FAE) Final Reports, Centers for Disease Control and Prevention Grant No. R04/CCR888515. 1996.
- Tough 2006 .Tough S, Tofflemire K, Clarke M, Newburn-Cook C, Tough Suzanne, Tofflemire Karen, et al. Do women change their drinking behaviors while trying to conceive? An opportunity for preconception counseling. Clinical Medicine & Research. 2006;4(2):97–105. doi: 10.3121/cmr.4.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters 2000 .Walters ST, Bennett ME, Miller JH. Reducing alcohol use in college students: a controlled trial of two brief interventions. Journal of Drug Education. 2000;30:361–72. doi: 10.2190/JHML-0JPD-YE7L-14CT. [DOI] [PubMed] [Google Scholar]
- Waterson 1990 .Waterson EJ, Murray-Lyon IM. Preventing alcohol related birth damage: a review. Social Science & Medicine. 1990;30(3):349–64. doi: 10.1016/0277-9536(90)90190-4. [DOI] [PubMed] [Google Scholar]


