Abstract
Background
The health benefits of physical activity and exercise are well documented and these effects could help people with schizophrenia.
Objectives
To determine the mental health effects of exercise/physical activity programmes for people with schizophrenia or schizophrenia-like illnesses.
Search methods
We searched the Cochrane Schizophrenia Group Trials Register (December 2008) which is based on regular searches of CINAHL, EMBASE, MEDLINE and PsycINFO. We also inspected references within relevant papers.
Selection criteria
We included all randomised controlled trials comparing any intervention where physical activity or exercise was considered to be the main or active ingredient with standard care or other treatments for people with schizophrenia or schizophrenia-like illnesses.
Data collection and analysis
We independently inspected citations and abstracts, ordered papers, quality assessed and data extracted. For binary outcomes we calculated a fixed-effect risk ratio (RR) and its 95% confidence interval (CI). Where possible, the weighted number needed to treat/ harm statistic (NNT/H) and its 95% confidence interval (CI), was also calculated. For continuous outcomes, endpoint data were preferred to change data. We synthesised non-skewed data from valid scales using a weighted mean difference (WMD).
Main results
Three randomised controlled trials met the inclusion criteria. Trials assessed the effects of exercise on physical and mental health. Overall numbers leaving the trials were similar. Two trials compared exercise to standard care and both found exercise to significantly improve negative symptoms of mental state (Mental Health Inventory Depression:1RCT, n=10, MD 17.50 CI 6.70 to 28.30, PANSS negative: 1RCT, n=10, MD -8.50 CI -11.11 to -5.89). No absolute effects were found for positive symptoms of mental state. Physical health improved significantly in the exercise group compared to those in standard care (1RCT, n=13, MD 79.50 CI 33.82 to 125.18), but no effect on peoples’ weight/BMI was apparent. One trial compared exercise with yoga and found that yoga had a better outcome for mental state (PANSS total: 1RCT, n=41, MD 14.95 CI 2.60 to 27.30). The same trial also found those in the yoga group had significantly better quality of life scores (WHOQOL Physical: 1RCT, n=41, MD -9.22 CI -18.86 to 0.42). Adverse effects (AIMS total scores) were, however, similar.
Authors’ conclusions
Results of this Cochrane review are similar to existing reviews that have examined the health benefits of exercise in this population. Although studies included in this review are small and used various measures of physical and mental health, results indicated that regular exercise programmes are possible in this population, and that they can have healthful effects on both the physical and mental health and well-being of individuals with schizophrenia. Larger randomised studies are required before any definitive conclusions can be drawn.
Medical Subject Headings (MeSH): Exercise [*psychology], Randomized Controlled Trials as Topic, Schizophrenia [*rehabilitation], Schizophrenic Psychology, Yoga [psychology]
MeSH check words: Humans
BACKGROUND
For people with mental health disorders such as schizophrenia, improvement in quality of life tends to enhance the individual’s ability to cope with and manage their disorder. As such, physical activity has the potential to improve quality of life for people with mental health disorders through two routes: physical and psychological (Faulkner 2006). In terms of physical health, individuals with mental health disorders have the same physical health needs as the general population. Individuals with serious mental illness are more likely to be sedentary than the general population (Brown 1999; Chamove 1986; Davidson 2001) and are consequently at high risk for chronic medical conditions associated with inactivity. For example, much of the increase in chronic medical illness among individuals with serious mental illness may be attributed to the increased prevalence of obesity in this population (Goff 2005) and physical inactivity likely contributes to this increased prevalence. In terms of mental health, positive psychological effects from physical activity in clinical populations have been reported even among those individuals who experience no objective diagnostic improvement. Improved quality of life is particularly important for individuals with severe and enduring mental health problems when complete remission may be unrealistic (Faulkner 1999). For example, there is a potential role for exercise in the treatment of schizophrenia, Faulkner 2005 concludes that exercise may alleviate secondary symptoms of schizophrenia such as depression, low self-esteem and social withdrawal.
Description of the condition
Schizophrenia is a serious mental illness that is characterised by (1) psychotic positive symptoms such as hallucinations, delusions, disorganised speech and thinking, (2) behavioural negative symptoms such as avolition, alogia, blunted or flattened affect and (3) serious neurocognitive and social cognitive deficits (DSM-IV 1994). Individuals who live with schizophrenia experience distortions of reality, changes in thinking and perceptions, difficulties in social situations, and problems with daily functions. Based on current estimates from epidemiological studies, approximately 15.2 in 100,000 individuals develop schizophrenia annually with a lifetime prevalence of 4 in 1,000 individuals (McGrath 2008).
Description of the intervention
Physical activity is a term that describes any bodily movement that is produced by skeletal muscles that requires energy expenditure above rest (Caspersen 1985). Exercise is a form of physical activity that is “planned, structured, repetitive, and purposive in the sense that improvement or maintenance of one or more components of physical fitness is an objective.” (Caspersen 1985, p.128).
How the intervention might work
In terms of physical activity, no single mechanism has yet been found to adequately explain the diverse range of mental health effects possible through physical activity participation. At present, the plausible mechanisms for psychological change through physical activity and exercise fall into one of three broad perspectives: (1) biochemical changes such as increased levels of neurotransmitters (e.g. endorphins or serotonin), (2) physiological changes such as improved cardiovascular and muscle function, thermogenesis and, (3) psychological changes such as social support, sense of autonomy, improved perceptions of competence, enhanced body image, self-efficacy and distraction (Mutrie 2003).
Why it is important to do this review
There is a growing recognition that physical activity can enhance mental health (Faulkner 2005b). With regard to the effects of exercise on schizophrenia, there is limited evidence to suggest that such benefits are also reported in populations characterised by serious mental illness such as schizophrenia. Studies tend to consist mostly of case reports but some group studies do exist (Faulkner 2005). Based on this evidence, there is some tentative support that participating in exercise is associated with an alleviation of negative symptoms associated with schizophrenia, such as depression, low self esteem and social withdrawal. There is less evidence that exercise may be a useful coping strategy for dealing with positive symptoms, such as auditory hallucinations (Faulkner 2005). These conclusions are drawn primarily from studies of pre-experimental design. The purpose of this review is to focus specifically on methodologically rigorous trials in updating current consensus concerning the potential role of exercise in improving the mental health of individuals with schizophrenia.
OBJECTIVES
To determine the mental health effects of exercise/physical activity programmes for people with schizophrenia or schizophrenia-like illnesses.
METHODS
Criteria for considering studies for this review
Types of studies
All relevant randomised controlled trials. We excluded quasi-randomised studies, such as those allocating by using alternate days of the week. We also did not include cross-over studies where participants receive different treatments sequentially, because of potential carry-over effects from all treatments.
Types of participants
People diagnosed with schizophrenia or schizophrenia-like illnesses using any criteria, with any length of illness and in any treatment setting. We included trials where it was implied that the majority of the participants had a severe mental illness which was likely to be schizophrenia. We did not exclude trials due to age, nationality or gender of participants.
Types of interventions
Physical activity or exercise: any intervention, used alone or in conjunction with others, where physical activity or exercise was considered to be the main or active element. Interventions which included exercise in a multiple component weight management programme were excluded since the specific effects of exercise on mental health could not be addressed.
Standard care: we defined standard care as care that a person would normally receive had they not been included in the research trial. This would include interventions such as medication, hospitalisation, community psychiatric nursing input and day hospital.
Other treatments: including any other treatment (biological, psychological or social) such as medication, problem solving therapy, psycho-education, social skills training, cognitive-behavioural therapy, family therapy or psychodynamic psychotherapy.
For a study to be included, the experimental and comparison interventions had to have had a similar duration.
Types of outcome measures
Outcomes were groups according to assessments of mental and physical health, and health care utilisation and cost. Outcome measures were not grouped by different time periods.
Primary outcomes
1. Mental state (with particular reference to the positive and negative symptoms of schizophrenia)
1.1 No clinically important change in general mental state
1.2 Average endpoint general mental state score
1.3 Average change in general mental state scores
1.4 No clinically important change in specific symptoms (positive symptom of schizophrenia, negative symptoms of schizophrenia, depression, mania)
1.5 Average endpoint specific symptom score
1.6 Average change in specific symptom scores
2. General functioning
2.1 No clinically important change in general functioning
2.2 Average endpoint general functioning score
2.4 Average change in general functioning scores
2.5 No clinically important change in specific aspects of functioning, such as social or life skills
2.6 Average endpoint specific aspects of functioning, such as social or life skills
2.7 Average change in specific aspects of functioning, such as social or life skills
Secondary outcomes
1. Global state
1.1 Relapse
1.2 No clinically important change in global state (as defined by individual studies)
1.3 Average endpoint global state score
1.4 Average change in global state scores
2. Behaviour
2.1 No clinically important change in general behaviour
2.2 Average endpoint general behaviour score
2.3 Average change in general behaviour scores
2.4 No clinically important change in specific aspects of behaviour
2.5 Average endpoint specific aspects of behaviour
2.6 Average change in specific aspects of behaviour
3. Adverse effects
3.1 Suicide and all causes of mortality
3.2 Clinically important general adverse effects
3.3 Average endpoint general adverse effect score
3.4 Average change in general adverse effect scores
3.5 Clinically important specific adverse effects
3.6 Average endpoint specific adverse effects
3.7 Average change in specific adverse effects
4. Physical fitness
4.1 No clinically important change in physical fitness
4.2 Average endpoint physical fitness score
4.3 Average change in physical fitness scores
4.4 No clinically important change in specific aspects of physical fitness
4.5 Average endpoint specific aspects of physical fitness
4.6 Average change in specific aspects of physical fitness
5. Weight
5.1 No clinically important change in weight measures
5.2 Average endpoint weight measures
5.3 Average change in weight measures
6. Service outcomes
6.1 Hospital admission
6.2 Time to admission
7. Satisfaction with treatment
7.1 Leaving the studies early
7.2 Recipient of care not satisfied with treatment
7.3 Recipient of care average satisfaction score
7.4 Recipient of care average change in satisfaction scores
7.5 Carer not satisfied with treatment
7.6 Carer average satisfaction score
7.7 Carer average change in satisfaction scores
8. Quality of life
8.1 No clinically important change in quality of life
8.2 Average endpoint quality of life score
8.3 Average change in quality of life scores
8.4 No clinically important change in specific aspects of quality of life
8.5 Average endpoint specific aspects of quality of life
8.6 Average change in specific aspects of quality of life
9. Economic outcomes
9.1 Direct costs
9.2 Indirect costs
Search methods for identification of studies
No language restriction was applied within the limitations of the search.
Electronic searches
We searched the Cochrane Schizophrenia Group Trials Register (December 2008) using the phrase:
[(physical* and (therap* or intervention)) within the same field of title, abstract or index term fields) or ((fitness* or sport* or gym* or exercis* or * danc*) in title, abstract and index fields in REFERENCE) OR (*exercise* or danc* or physical act* in interventions field in STUDY)]
This register is compiled by systematic searches of major databases, hand searches and conference proceedings (see Group Module). For previous search strategy see Appendix 1
Searching other resources
We inspected the reference list of all identified studies for more relevant citations.
Data collection and analysis
Selection of studies
PG and GF independently assessed the abstracts of the studies returned by the searches for relevance. Where disagreements occurred or the abstract was unclear, we acquired the full report and repeated the assessment process. If a dispute still existed this was resolved by discussion and if there remained insufficient information to assess relevance we contacted the first author of the study.
Data extraction and management
1. Data Extraction
PG and GF extracted data from each study independently with disagreements resolved by documented discussion. Where disagreements were not resolved, we listed the study under the awaiting assessment section. Data did not need to be published to be included in this review.
2. Management
Data were extracted onto standard forms. Where relevant, data were entered into RevMan by the PG.
3. Scale-derived data
3.1 Valid Scales
Continuous data from scales were only included if the instrument had been described in a peer reviewed journal and had been found to be both reliable and valid given that unpublished scales have been shown to be subject to bias when used in trials that examine treatment in schizophrenia (Marshall 2000).
Assessment of risk of bias in included studies
PG and GF independently assessed the methodological quality of all relevant studies. Criteria in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008) was used to evaluate the quality of each trial on the following items:
sequence generation;
allocation concealment;
blinding;
incomplete outcome data;
selective reporting of the results;
any other biases identified.
Each item was rated on level of bias. A ‘YES’ rating identified that there was a low risk of bias while a ‘NO’ rating meant there was a high risk of bias. Where a risk of bias could not be determined, the item was given a rating of ‘UNCLEAR.’ Due to the small number of identified trials, all studies that were identified as randomised were included in the review, regardless of how many total biases they possessed.
Measures of treatment effect
1. Binary data
For binary outcomes we calculated a standard estimation of the fixed-effect risk ratio (RR) and its 95% confidence interval (CI). For statistically significant results we calculated the number needed to treat/harm statistic (NNT/H), and its 95% confidence interval (CI) using Visual Rx taking account of the event rate in the control group. It has been shown that RR is more intuitive (Boissel 1999) than odds ratios and that odds ratios tend to be interpreted as RR by clinicians (Deeks 2000). This misinterpretation then leads to an overestimate of the impression of the effect.
1.2 Binary outcomes from scale data
Continuous outcome measures were not converted to binary data by identifying specific cut-off points on rating scales. Binary data were only used if they were clearly identified as dichotomous outcomes.
2. Continuous data
Continuous data on outcomes in mental health trials are often not normally distributed. To avoid the pitfall of applying parametric tests to non-parametric data we applied the following standards to all endpoint data derived from continuous measures. The criteria were used before inclusion: (a) standard deviations and means had to be obtainable; and, for finite scores, such as endpoint measures on rating scales, (b) the standard deviation (SD), when multiplied by 2 had to be less than the mean (as otherwise the mean was unlikely to be an appropriate measure of the centre of the distribution) (Altman 1996). If a scale starts from a positive value (such as PANSS, which can have values from 30 to 210) the calculation described above in (b) should be modified to take the scale starting point into account. In these cases skewness is present if 2SD>(SSmin), where S is the mean score and Smin is the minimum score. Skewed endpoint data from studies with less the 200 participants were not shown graphically, but were added to ‘Other data’ tables and briefly commented on in the text. However, skewed endpoint data from larger studies (=/>200 participants) pose less of a problem and we entered the data for analysis.
For continuous mean change data (endpoint minus baseline) the situation is even more problematic. In the absence of individual patient data it is impossible to know if change data are skewed. The RevMan meta-analyses of continuous data are based on the assumption that the data are, at least to a reasonable degree, normally distributed. Therefore we included such data, unless endpoint data were also reported from the same scale.
2.1 Intention-to-treat analysis
For dichotomous data a ‘once-randomised-always-analyse’ approach was taken and it was assumed that all those lost to follow-up had relapsed. For continuous data a ‘last-observation-carried-forward’ (LOCF) approach, which maintains the sample size, was used in this review.
2.2 Summary statistics
In the case of continuous outcome measurement, a weighted mean difference (WMD) between groups was estimated. Again if evidence of heterogeneity was found a random effects model was used.
2.3 Scale derived data
Data obtained using a scale were only included if its psychometric properties (i.e. concerning reliability and validity) were reported in a peer reviewed journal (Marshall 2000). Furthermore these data were only included if the scale was either self-report or completed by an independent rater or a relative and not the therapist or provider of the intervention.
Unit of analysis issues
1. Cluster trials
Studies increasingly employ cluster randomisation (such as randomisation by clinician or practice) but analysis and pooling of clustered data poses problems. Firstly, authors often fail to account for intraclass correlation in clustered studies, leading to a ‘unit of analysis’ error (Divine 1992) whereby p values are spuriouslylow, confidence intervals unduly narrow and statistical significance overestimated. This can cause Type I errors (Bland 1997, Gulliford 1999).
Where clustering was not accounted for in primary studies, we presented the data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. In subsequent versions of this review we will seek to contact first authors of studies to obtain intraclass correlation coefficients of their clustered data and to adjust for this using accepted methods (Gulliford 1999). Where clustering has been incorporated into the analysis of primary studies, we will also present these data as if from a non-cluster randomised study, but adjusted for the clustering effect.
We have sought statistical advice and have been advised that the binary data as presented in a report should be divided by a design effect. This is calculated using the mean number of participants per cluster (m) and the intraclass correlation coefficient (ICC) [Design effect=1+(m-1)*ICC] (Donner 2002). If the ICC was not reported it was assumed to be 0.1 (Ukoumunne 1999). If cluster studies had been appropriately analysed taking into account intraclass correlation coefficients and relevant data documented in the report, we synthesised these with other studies using the generic inverse variance technique.
2. Cross-over trials
A major concern of cross-over trials is the carry-over effect. It occurs if an effect (e.g. pharmacological, physiological or psychological) of the treatment in the first phase is carried over to the second phase. As a consequence on entry to the second phase the participants can differ systematically from their initial state despite a wash-out phase. For the same reason cross-over trials are not appropriate if the condition of interest is unstable (Elbourne 2002). As both effects are very likely in schizophrenia, we will only use data of the first phase of cross-over studies.
3. Studies with multiple treatment groups
Where a study involved more than two treatment arms, if relevant, the additional treatment arms were presented in comparisons. Where the additional treatment arms were not relevant, these data were not reproduced.
Dealing with missing data
1. Overall loss of credibility
At some degree of loss to follow up data must lose credibility (Xia 2007). Since there is no evidence as to the degree of attrition which makes a reasonable analysis of the data possible, we included all trials in the main analysis. If, for a given outcome, more than 50% of the total numbers randomised were not accounted for we did not present results as such data will be impossible to interpret with authority.
2. Binary
Where attrition for a binary outcome is between 0 and 50%, and outcomes of these individuals are described, we included these data in our analysis.
3. Continuous
Where attrition for a continuous outcome is between 0 and 50%, and outcomes of these individuals are described, we included these data in our analysis.
Assessment of heterogeneity
1. Clinical heterogeneity
We considered all included studies without any comparison to judge clinical heterogeneity.
2. Statistical
2.1 Visual inspection
We visually inspected graphs to investigate the possibility of statistical heterogeneity.
2.2 Employing the I-squared statistic
This provided an estimate of the percentage of inconsistency thought to be due to chance. I-squared estimate greater than or equal to 50% was interpreted as evidence of high levels of heterogeneity (Higgins 2003). If heterogeneity was found, the data were re-analysed using a random effects model to see if this made a substantial difference. If it did, the studies responsible for heterogeneity were not added to the main body of homogeneous trials, but summated and presented separately and reasons for heterogeneity investigated.
Assessment of reporting biases
Reporting biases arise when the dissemination of research findings is influenced by the nature and direction of results (Egger 1997). Although funnel plots may be useful in investigating bias, they have a limited ability to detect small-study effects. Given the small number of studies examined in this review, we did not use funnel plots to asses reporting biases.
Data synthesis
Where possible we employed a fixed-effect model for analyses. We understand that there is no closed argument for preference for use of fixed or random-effects models. The random-effects method incorporates an assumption that the different studies are estimating different, yet related, intervention effects. This does seem true to us, however, random-effects does put added weight onto the smaller of the studies - those trials that are most vulnerable to bias. For this reason we favour using the fixed-effect model.
Subgroup analysis and investigation of heterogeneity
1. Subgroup analysis
No subgroup analyses were undertaken in this review.
2. Investigation of heterogeneity
If data were clearly heterogeneous we checked that the data were correctly extracted and entered and that we made no unit-of-analysis errors. If heterogeneity was found, the data were re-analysed using a random-effects model to see if this made a substantial difference. If it did, the studies responsible for heterogeneity were not added to the main body of homogeneous trials, but summated and presented separately and reasons for heterogeneity investigated.
Sensitivity analysis
No sensitivity analyses were conducted.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification; Characteristics of ongoing studies.
For substantive descriptions of studies please see Characteristics of included studies; Characteristics of excluded studies; Characteristics of studies awaiting classification;Characteristics of ongoing studies.
Results of the search
We inspected 442 electronic reports and of these, 421 studies were excluded on the basis of their abstracts. We included three randomised controlled trials (Beebe 2005; Duraiswamy 2007;Marzaloni 2008) and excluded ten trials (Acil 2008; Adams 2001;Apter 1978;Hu 2004; Li 2005;Liu 2006; Skrinar 2005;Su 1999;Wu 2008 Wu 2007). Additionally, we are waiting for more information from seven studies (Lin 2006; NCT00286299; Ning 2003; Scheidhacker 1991; Wu 2007b; Xie 2006; Zhang 2006). Lastly, one trial is still ongoing (NCT00338832) and further information has been sought from the authors.
Included studies
We included three randomised controlled trials (Beebe 2005;Duraiswamy 2007; Marzaloni 2008). All studies have been published since 2005 which possibly illustrates growing attention to the role of exercise as a form of adjunctive therapy for schizophrenia. One study investigated the effects of an exercise programme that included both aerobic and strength training components (Marzaloni 2008). This programme was 12 weeks in length, included a warm up session, 30-60 minutes of aerobic fitness, 15-20 minutes of strength training, and 5-10 minutes of cool down. Participants in this trial met twice a week. The other two studies evaluated the effects of a walking programme (Beebe 2005) and a light exercise programme (Duraiswamy 2007). In the Beebe 2005 study, researchers evaluated the effects of a 16 week walking programme where participants met for 10-30 minutes three times per week. In the Duraiswamy 2007 study, researchers evaluated the effects of a 16 week light exercise programme that consisted of light walking, jogging, stretching, and relaxation techniques. Participants in the Duraiswamy 2007 study met for one hour five times per week.
1. Methods
All trials were randomised and two were single-blind (Beebe 2005;Duraiswamy 2007). The duration of the trials ranged between 12 weeks (Marzaloni 2008) and 16 weeks (Beebe 2005; Duraiswamy 2007).
2. Participants
All trials included people diagnosed with schizophrenia using DSM-IV criteria (Beebe 2005; Duraiswamy 2007; Marzaloni 2008). Two studies included both in- and outpatients (Duraiswamy 2007; Marzaloni 2008), while one concentrated solely on outpatients (Beebe 2005). Approximately 96 participants were initially recruited into the studies and there were more male than female participants included. Participants ranged in age from 18 to 63 years with a mean age of 32.4 years.
3. Setting
Two studies were conducted in hospital settings that offered inand outpatient services (Beebe 2005; Duraiswamy 2007). One study was conducted in a community centre (Marzaloni 2008).
4. Study size
All studies utilised small samples and ranged in size from from 12 (Beebe 2005) to 61 participants (Duraiswamy 2007). One study used 13 participants (Marzaloni 2008).
5. Interventions
5.1 Exercise
The experimental conditions identified in each of the included studies differed in exercise duration and intensity. The exercise programme in the Beebe 2005 study included 3 exercise sessions per week that consisted of a 10 minute warm-up and walking on a treadmill. Over the course of the study, participants increased their walking time from 5 minutes on the first day to 30 minutes.
In the Duraiswamy 2007 study, the programme consisted of brisk walking, jogging, exercises in standing and sitting postures and relaxation. Participants underwent three weeks of training and then continued with the programme for the remaining three months. Participants met for 1 hour a day, 5 days a week.
In the Marzaloni 2008 study, the programme consisted of a 10 minute warm-up, 20 minutes of resistance weight training, 60 minutes of aerobic training, and a 5 minute cool-down. Participants met twice a week for 12 weeks. Each session was 90 minutes in length. Participants were encouraged to exercise one additional time per week independently.
All exercise programmes were in addition to participants usual care.
5.2. Control interventions
5.2.1 Standard care
In the Beebe 2005 study, participants continued with their usual treatment but told they were on a waiting list for the exercise therapy. At the conclusion of this study, those in the standard care group were given the opportunity to take part in the experimental treatment. Participants in the control group of the Marzaloni 2008 study continued with treatment as usual.
5.2.2 Other treatment
Participants in Duraiswamy 2007 study took part in yoga classes five times per week that lasted one hour in length. Again participation in yoga classes was in addition to usual care.
6. Outcomes
6.1 Outcome scales
Details of the only scales that provided usable data are shown below. Reasons for exclusion of data are given under ‘Outcomes’ in the ‘Characteristics of included studies’ section.
6.1.1 Mental state (with particular reference to the positive and negative symptoms of schizophrenia)
6.1.1.1 Positive and Negative Syndrome Scale - PANSS (Kay 1986)
This schizophrenia scale has 30 items, each of which can be defined on a seven-point scoring system varying from 1 - absent to 7 - extreme. This scale can be divided into three sub-scales for measuring the severity of general psychopathology, positive symptoms (PANSS-P), and negative symptoms (PANSS-N). A lower score indicates lesser severity. Two studies reported data using this scale (Beebe 2005; Duraiswamy 2007).
6.1.1.2 Mental Health Inventory (MHI) (Veit 1983; Ware 1998)
This self-report scale has 18 items that measure anxiety, depression, behavioural control, and positive affect. It offers a total mental health score as well as sub scores for each of the subscales. Each item on the scale has six response options, with higher values indicating better mental health. The Marzaloni 2008 study reversed the presentation and subsequent analysis of the depression sub-scale for easier comprehension of results. One study reported data using this scale (Marzaloni 2008).
6.1.2 General functioning
6.1.2.1 Social and Occupational Functioning Scale - SOFS (Saraswat 2006)
This scale has 14 items, each of which can be defined on a 5-point scale where 1= no impairment and 5 = extreme impairment. This scale examines bathing and grooming, dressing, eating, neatness, conversational skills, social appropriateness, social engagement, money management, orientation/mobility, social skills, recreation, work relationships, respect for property and independence. Higher scores on the SOFS indicate greater social impairment. One study reported data using this scale (Duraiswamy 2007).
6.1.3 Adverse effects
6.1.3.1 Simpson Angus Scale - SAS (Simpson 1970)
This 10-item scale, with a scoring system of 0-4 for each item, measures drug-induced parkinsonism, a short-term drug-induced movement disorder. A low score indicates low levels of parkinson ism. One study reported data using this scale (Duraiswamy 2007). 6.1.3.2 Abnormal Involuntary Movements Scale - AIMS (Munetz 1988)
AIMS is a 12-item instrument assessing abnormal involuntary movements associated with antipsychotic drugs, such as tardive dystonia and chronic akathisia, as well as ‘spontaneous’ motor disturbance related to the illness itself. Scoring the AIMS consists of rating the severity of movement in three main anatomic areas (facial/oral, extremities, and trunk), based on a five-point scale (0=none, 4=severe). One study reported data using this scale (Duraiswamy 2007).
6.1.4 Quality of life
6.1.4.1 World Health Organization Quality of Life BREF Version, WHOQOL-BREF (Skevington 2004)
This scale is a 26-item version of the WHOQOL-100 assessment. The scale assesses physical health, psychological, social relations and the environment on a five-point scale where 1 = poor QofL and 5 = good QofL. One study reported data using this scale (Duraiswamy 2007).
6.2 Other outcomes
6.2.1 Physical fitness
6.2.1.1 Six Minute Walk Test (Enright 1998)
This test measures level of aerobic fitness. Participants are requested to walk for 6 minutes and distance travelled is measured to the nearest foot. Two studies reported data using this test (Beebe 2005; Marzaloni 2008).
6.2.1.2 Maximal Strength
Maximal strength was measured by one repetition maximum test on the bicep curl exercise. One study reported data using this test (Marzaloni 2008).
6.2.2 Cardiovascular measures
One study reported data on resting blood pressure (Marzaloni 2008).
6.2.3 Weight
6.2.3.1 Body Mass Index
Height and weight were captured using calibrated and standardized measurements (e.g., stadiometer, balance-beam scale). BMI = weight in kg/height in meters squared. Two studies reported pre and post measures of BMI of their participants (Beebe 2005;Marzaloni 2008).
6.2.3.2 Percentage Body Fat
Participants’ percentage body fat was obtained through skinfold callipers. A three site method was used to measure the triceps, abdominal, and suprailiac skin folds (American College of Sports Medicine, 1995). One study reported data on percentage body fat (Beebe 2005).
6.2.3.3 Waist and hip circumference
Waist circumference was measured at the level of the umbilicus and hip circumference was measured at the largest circumference of the hips. One study reported waist circumference (Marzaloni 2008).
6.2.4 Leaving the study early
Two studies reported a loss of participants (Beebe 2005;Duraiswamy 2007), but all three studies reported detailed information on the number of participants throughout their studies.
Excluded studies
We excluded ten studies from the review and reasons for this are presented in the ‘Characteristics of excluded studies’ table (Acil 2008; Adams 2001;Apter 1978;; Li 2005; Liu 2006; Skrinar 2005;Su 1999; Wu 2008 Wu 2007).
Awaiting assessment
Seven studies await assessment and these are generally registered clinical trials ( Lin 2006; NCT00286299; Ning 2003;Scheidhacker 1991; Wu 2007b; Xie 2006; Zhang 2006). Further information has been sought from these authors.
Ongoing studies
One trial is classified as ongoing (NCT00338832). Further information has been sought from authors.
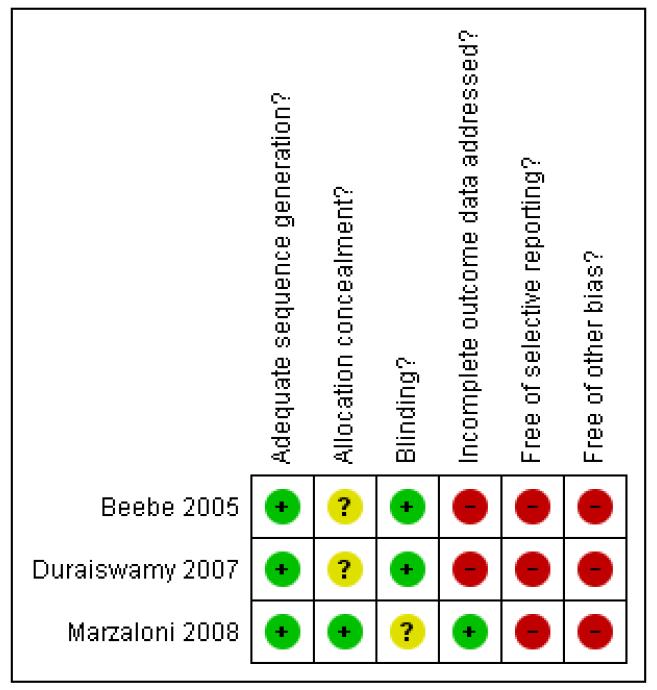
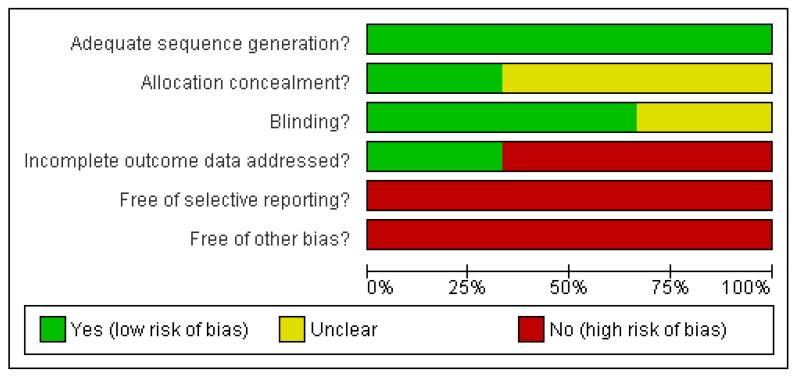
Risk of bias in included studies
Judgement of risks are illustrated in Figure 1 and Figure 2.
Figure 1.
Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Figure 2.
Methodological quality graph: review authors’ judgements about each methodological quality item presented as percentages across all included studies.
Allocation
All included studies were reported as randomised; however, most of the included studies did not explicitly describe the methods used. Two trials explained their randomisation processes (Beebe 2005; Duraiswamy 2007). Beebe 2005 utilised a randomisation schedule designed by a statistician and Duraiswamy 2007 used a computer generated allocation schedule. Concealment of allocation has repeatedly been shown to be of key importance in excluding selection biases (Jüni 2001). No studies reported using concealment of allocation. Analyses based on methodological quality were not conducted.
Blinding
None of the studies were double-blinded. The reported results may exaggerate estimates of treatment effect (Boutron 2004). None of the studies reported any test of blinding.
Incomplete outcome data
Two of the three trials experienced a loss of participants and reported results on the individuals that remained in the trials (Beebe 2005; Duraiswamy 2007). In the Beebe 2005 study, two participants left before they began their first exercise session. In theDuraiswamy 2007 trial, 10 participants left from each study arm because of disinterest or long distance from hospital for outpatients.
Selective reporting
Only the included studies reported both means and standard deviations, although not for all variables of interest. Many studies awaiting classification failed to provide standard deviations when reporting mean changes. We are seeking further data from the first authors of relevant trials.
Other potential sources of bias
No other potential biases were found.
Effects of interventions
The included studies varied considerably in the designs of their respective exercise programmes and what variables they measured. Two of the included studies examined aspects of both physical and mental health (Beebe 2005;Marzaloni 2008), and one study only looked at improvements in mental health (Duraiswamy 2007). In general, all included studies showed positive mental and physical health effects associated with exercise participation.
1. COMPARISON 1. EXERCISE versus STANDARD CARE
Although two studies compared exercise to standard care, results could only be pooled for one outcome, leaving the study early.
1.1 Mental State
1.1.1 Mental Health Inventory (MHI)
During the 12 week Marzaloni 2008 trial scale ratings of mental health increased from a baseline M=56.3(SD 10.5) to endpoint M=65.5 (SD 9.0) (p< .03) in the exercise group, but these scores were not significantly different to those found in the standard care group (n=10, MD 7.40 CI -2.46 to 17.26). There were significantdifferences observed between groups for depression (n=10, MD 17.50 CI 6.70 to 28.30) and anxiety scores (n=10, MD 8.00 CI 0.80 to 15.20). No significant differences were observed for positive affect (n=10, MD 3.30 CI -23.66 to 30.26) and behavioural scores (n=10, MD -5.40 CI -21.28 to 10.48).
1.1.2 PANSS scores
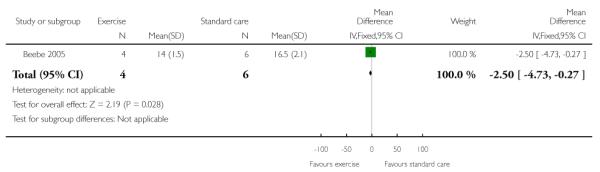
Beebe 2005 found those in the exercise group had significantly better PANSS negative scores than those in standard care (n=10, MD -8.5 CI -11.11 to -5.89). A similar favourable effect for exercise was found for positive scores, this result was just significant (n=10, MD -2.5 CI -4.73 to -0.27).
1.2 Physical fitness
1.2.1 Six Minute Walking Distance
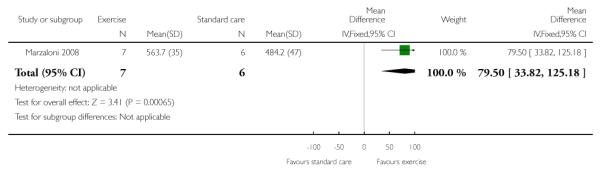
Two studies examined the distance participants could walk in six minutes (Beebe 2005; Marzaloni 2008). Data from Beebe 2005 could not be used in the analysis as no SD were provided. Although both studies observed increases in the distance covered by their respective exercise groups, only participants in the Marzaloni 2008 increased their distance travelled significantly (n=13, MD 79.50 CI 33.82 to 125.18).
1.2.2 Maximal Strength
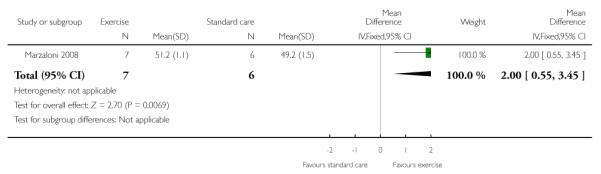
One study reported on maximal strength (Marzaloni 2008). Participants in the exercise group reported a significant increase in strength (n=13, MD 2.00 CI 0.55 to 3.45).
1.2.3 Cardiovascular measures
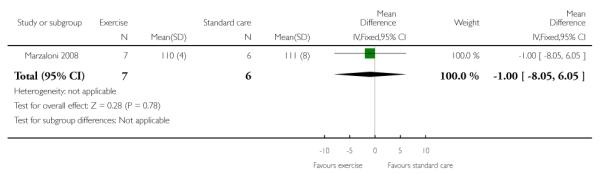
One study reported on cardiovascular measures. The Marzaloni 2008 study reported on data on resting blood pressure and revealed no significant improvements (n=13, MD -1.00 CI -8.05 to 6.05).
1.3 Weight
1.3.1 BMI
Two studies examined changes in BMI (Beebe 2005; Marzaloni 2008) but only Marzaloni 2008 provided useable data, no effect was found (n=13, MD -1.20 CI -2.92 to 0.52). Again, standard deviations were not provided for the Beebe 2005 study and the authors have been contacted.
1.3.2 Percentage Body Fat
One study examined changes in percentage body fat (Beebe 2005). Participants in the exercise group reduced their body fat by 3.7% which was significantly larger than the 0.02% reduction experienced by those in the control group (p< .03), however, standard deviations were not provided for the Beebe 2005 study and so data are not analysed in this review, the authors have been contacted.
1.3.3 Waist and hip circumference
One study reported data on waist and hip circumferences and noted no effect (Marzaloni 2008) (n=13, MD 0.01 CI -0.02 to 0.04).
1.3.4 Final Weight
One study reported data on final weight and noted no effect (n= 13, MD 1.30 CI -3.64 to 6.24) (Marzaloni 2008).
1.4 Leaving the study early
No differences in numbers leaving the study early were found between exercise and standard care groups (2RCTs, n=25, RR 5.00 CI 0.29 to 86.43).
2. COMPARISON 2. EXERCISE versus OTHER TREATMENT
One study (n=61) provided data for this comparison Duraiswamy 2007. The other treatment for this trial were regular sessions of yoga.
2.1 Mental State
2.1.1 PANSS Total
Participants in the yoga group reported a significantly lower overall Total PANSS score than those in the exercise group (n=41, MD 14.95 CI 2.60 to 27.30).
2.1.1.1 PANSS Depression
When reporting PANSS Depression score, those in the yoga group had more favourable scores, the difference between groups was just significant (n=41, MD 2.89 CI 0.86 to 4.92).
2.1.1.2 PANSS Anergia
Those practising yoga reported a just significantly lower PANSS Anergia score than those in the exercise group (n=41, MD 2.40 CI 0.47 to 4.33).
2.1.1.3 PANSS Positive
Participants who were in the exercise group did not have significantly lower scores on the PANSS Positive score than those in the yoga control group (n=41, MD 2.41, CI -1.20 to 6.02).
2.1.1.4 PANSS Negative
Participants who were in the exercise group had significantly higher scores on the PANSS Negative score than those in the yoga control group (n=41, MD 5.56, CI 1.69 to 9.43).
2.2 General Functioning
2.2.1 Social and Occupational Functioning Scale - SOFS
Although ratings of the social and occupational functioning were reduced, there were no significant differences in social and occupation functioning between the yoga and exercise therapy groups (n=41, MD 4.35 CI -1.18 to 9.88).
2.3 Adverse effects
2.3.1 Simpson Angus Scale - SAS
No significant differences in adverse side effects were found between the yoga and exercise groups (n=41, MD 0.50 CI -0.44 to 1.44).
2.3.2 Abnormal Involuntary Movements Scale - AIMS
No significant differences in abnormal involuntary movements were observed for either the yoga or exercise group (n=41, MD 0.20 CI -1.18 to 1.58).
2.4 Quality of Life
2.4.1 World Health Organization Quality of Life BREF Version, WHOQOL-BREF
Quality of life scores as measured by the WHOQOL all showed a favourable effect for those in the yoga group:
2.4.1.1 Physical
(n=41, MD -9.22 CI -18.86 to 0.42).
2.4.1.2 Psychosocial
(n=41, MD -17.70 CI -28.90 to -6.50).
2.4.1.3 Social
(n=41, MD -20.75 CI -34.08 to -7.42).
2.4.1.4 Environmental
(n=41, MD -18.09 CI -28.52 to -7.66).
2.5 Leaving the study early
Numbers leaving early from each group were fairly high (ten from the yoga group and eleven from the exercise group), but similar (n=61, RR 0.94 CI 0.47 to 1.88).
DISCUSSION
The Searches
Electronic searching produced 442 electronic reports, 21 of which were selected for further examination. Overall, three studies were included given they met the eligibility criteria for this review.
Summary of main results
Three studies were included in this review. Overall, these studies showed that exercise therapy can have an impact on mental health outcomes like mental state and general functioning with no adverse effects and a limited effect on physical health outcomes such as weight. The included studies illustrate that randomised controlled trials that examine the mental health effects of physical activity are possible to conduct with individuals with schizophrenia although they are characterised by their short-term nature and small samples. Importantly, attrition rates were similar in the trials with no significant differences between groups. All of the included studies have been conducted within the last four years which suggests that researchers have responded to calls for greater methodological rigour (Faulkner 2005). Although these studies have been conducted recently and are more methodologically rigorous than those conducted in the past, it was not possible to combine their findings to calculate weighted mean difference or risk ratios. Results have been stratified below according to mental health and physical health outcomes.
1. Mental Health
Overall, findings show that exercise improves mental health measures, specifically negative symptoms, compared to standard care, but when exercise is compared to other types of exercise, such as yoga, the benefits of exercise are not as profound. Findings should be viewed with caution as results are based on a limited number of trials that had small sample sizes.
2. Physical Health
Several physical health measures were examined in this review. Although participants in the exercise arm of Marzaloni 2008 study improved their physical fitness, overall, studies did not find significant changes in physical health outcomes that measured BMI, waist to hip ratio, final weight, or resting blood pressure. This may reflect the relatively short nature of the described intervention studies, or a lack of adherence to the exercise intervention. Given that individuals with schizophrenia live with various co-morbidities which often stem from overweight or obesity (Lambert 2003;Meyer 2003), this review reinforces the need for further research examining how to get this population physically active in order to receive physical health benefit.
Overall completeness and applicability of evidence
Overall, several results from the three included studies show that mental health and physical fitness improves with exercise; however, given the small number of included studies, and the use of various instruments used to measure different aspects of mental and physical health, these findings must be viewed with caution. Furthermore, a wide variety of physical health outcomes such as BMI, waist to hip ratio, final weight, and resting blood pressure, did not improve significantly.
Quality of the evidence
In the included studies data reporting was inconsistent. All future studies should respect standards of measuring outcomes and of reporting data in order to enhance the comparability of study results (Begg 1996; Moher 2001).
In order to strengthen the quality of future randomised controlled trials, researchers should attempt to limit the number of study biases. These biases include selection, performance, detection, attrition, and reporting. In this Cochrane review, selection biases were observed in all three included studies. Only two studies utilised methods of generating a sequence of allocation (Beebe 2005; Duraiswamy 2007) and none of the studies concealed their group allocations. Failure to conceal group allocations may indicate an inability to adhere to the randomly generated results of group allocation. Future studies should utilise some form of sequence generation such as a random number generator or a randomisation schedule and conceal their randomisation results by placing them in sequentially-numbered, opaque, sealed envelopes (Schulz 2001).
Although researchers may not blind participants to behavioural interventions to remove threats of performance biases, every attempt should be made to collect study data in a blind manner. In this review, only two of the included studies were single blind (Beebe 2005; Duraiswamy 2007). Researchers conducting future studies should at least blind study personnel to group allocation in order to guard against detection biases in order to minimise any exaggeration of treatment effect (Boutron 2004).
Lastly, adherence is a great concern for researchers that conduct studies that include individuals with schizophrenia. Future research should address issues of programme adherence and researchers should pay careful attention to barriers that prevent regular exercise.
Potential biases in the review process
Although a thorough and extensive search and review was undertaken, potential biases may still exist. Throughout this review process, we found very few randomised controlled trials that met our inclusion criteria. Publication bias may exist and may threaten the results given that all research studies do not get published in major journals that may be identified through CINAHL, EMBASE, MEDLINE and PsycINFO. Additionally, language may present an additional challenge as a great deal of research is not being published in English. Several steps are being taken to translate numerous studies, evaluate them, and determine if they should be included in the next stage of this review.
Agreements and disagreements with other studies or reviews
Two other reviews have identified and reviewed existing research studies that used exercise as a form of adjunct therapy for schizophrenia (Ellis 2007;Faulkner 2005). These reviews examined various forms of research methods including qualitative, quantitative, and mixed methods. Their results are in line with this review. Both reviews indicated that exercise can improve physical and psychological health and social well-being in this population. Additionally, both reviews stressed the need for more methodologically rigorous research to be conducted given that most studies had used pre-experimental designs. This review suggests such calls are starting to be addressed.
AUTHORS’ CONCLUSIONS
Implications for practice
1. For people with schizophrenia
The results of this review indicate that there are various benefits to exercise. Individuals with schizophrenia can improve components of mental health by participating in regular exercise. However, clear guidance regarding what dose of exercise works best for improving mental health is limited by the small number of studies and the variability of the interventions themselves as well as their intensity and duration. People with schizophrenia should ask their clinician for support and advice regarding getting more physically active. Current guidelines for lifestyle activity and exercise appear just as acceptable to individuals with schizophrenia in terms of potential mental health benefit. That is, accumulating 30 minutes of moderate physical activity on most or all days of the week remains a good guideline. In terms of short term goals, sedentary individuals could be encouraged to participate in two thirty-minute sessions of moderate activity a week.
2. For clinicians
Given the physical, mental, and social benefits of regular exercise, clinicians should ensure their clients are becoming and staying active. Although research shows that the physical health of clients may be neglected by health care practitioners and systems (Meyer 2003), multidisciplinary approaches need to be taken to provide clients with information about and opportunities to take part in regular exercise. Both psychiatrists and general physicians need to take responsibility for both the physical and mental well-being of their clients. Additionally, all physicians should take into consideration the negative symptoms of schizophrenia when prescribing any exercise programme. Although exercise has been shown to improve negative symptoms (Beebe 2005; Duraiswamy 2007), clients may at first be too unmotivated to begin an exercise programme. Not only do the health and social benefits of exercise need to be emphasised, but careful attention needs to be paid to various barriers that prevent clients from exercise. Before recommending any exercise programme, clinicians could pay specific attention to and address mental illness symptoms, medication side effects, safety concerns, stigma, and structural barriers (e.g., transportation, social economic status). In addition to addressing barriers to exercise, clinicians should structure programmes to be informative, flexible, allow clients to progress at their own pace, and offer motivational leadership.
3. For policy makers
Individuals with schizophrenia have an increased chance of having one or more morbidity (Lambert 2003). Clinicians need to carefully screen clients for both physical and mental health conditions and pay attention to the health needs of clients (Lykouras 2008). Research has shown that multidisciplinary approaches to health care can have a profound positive impact on the health and well-being of clients and address issues such as helping clients maintain regular appointments and assisting them with communication difficulties (Lambert 2003; Meyer 2003). Also research has shown that through multidisciplinary approaches, clinicians spend more time with clients and address more of their health needs. Through these types of treatment approaches, clinicians may be able to offer more information to clients about the importance of exercise as an adjunct treatment for schizophrenia and be able to address specific barriers clients may have that prevent them from participating and adhering to regular exercise. Policy makers should consider the implementation of such multidisciplinary programmes within their respective treatment facilities.
Implications for research
1. General
All future studies should respect standards of measuring outcomes and of reporting data in order to enhance the comparability of study results (Begg 1996; Moher 2001). In the included studies data reporting was inconsistent.
2. Specific
In future research, the exact nature of the exercise programme must be clearly defined with the duration, frequency, and intensity of exercise reported. Adherence must also be clearly reported. Changes in fitness levels should also be documented as well as the incorporation of follow-up measures in research designs. The participants should be clearly described in terms of their age, sex, diagnosis, duration of illness, and medication regimen. Outcome measures should include measures relevant to schizophrenia-related symptomatology, particularly the negative symptoms, and consider broader clinical outcomes such as use of health services, medication compliance, and rate of relapse.
Although the included studies in this Cochrane review described their exercise programmes in detail, all the studies neglected to disclose specific behavioural theories and aspects of exercise intensity, duration, and frequency. In order to examine the full physical and mental health effects of exercise, researchers should consider proposing specific theories and defining and measuring specific aspects of the exercise conducted by participants. Specifically, we need to know how best to get this population engaged in exercise programmes and continuing participation. All of the identified studies did not describe the theoretical basis for how behaviour change was being facilitated. Comparison of lifestyle and structured interventions to increase physical activity should also be conducted as we do not know whether less structured interventions can work with this population. Their flexibility, lower cost, and easy integration into daily schedules might be particularly appealing to individuals with schizophrenia.
PLAIN LANGUAGE SUMMARY.
Exercise Therapy for Schizophrenia
Regular exercise and physical activity is thought to improve both physical and mental health. Although only three studies are included in this review, the overall results show that regular exercise can help some individuals with schizophrenia improve their physical and mental health and well-being. Future studies should address how best to help individuals with schizophrenia begin, and continue to exercise.
ACKNOWLEDGEMENTS
Ontario Mental Health Foundation (OMHF).
The Cochrane Schizophrenia Group Editorial Base in Nottingham produces and maintains standard text for use in the Methods sections of their reviews. We have used this text as the basis of what appears here and adapted it as required.
SOURCES OF SUPPORT
Internal sources
Faculty of Physical Education and Health, University of Toronto, Canada.
External sources
Ontario Mental Health Foundation, Canada.
Centre for Urban Health Initiatives, Canada.
Appendix 1. Previous search strategy
We previously searched the Cochrane Schizophrenia Group’s Trials register (May 2003) using the phrase:
[(*physical* and *fitness*) or (*exercise*) in title or (*physical* and *fitness*) or (*exercise*) in abstract, index or title terms of REFERENCE] or [Exercise Therapy* in interventions of STUDY]
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | Allocation: randomised. Blinding: single. Duration: 16 weeks. Setting: Veterans Affairs Hospital, USA. |
|
| Participants | Diagnosis: schizophrenia (DSM-IV). N=12. Age: mean ~ 52 years. Sex: 8M, 2F. |
|
| Interventions |
|
|
| Outcomes | Mental state: PANSS positive, negative score. Leaving study early. Unable to use - Mental state: PANSS total score (SDs not reported). Physical fitness: Six Minute Walk Test (SDs not reported). Weight: BMI, Percentage body fat (SDs not reported - some data for percentage body fat presented as other data) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Allocation schedule designed by statistician. |
| Allocation concealment? | Unclear risk | No details given. |
| Blinding? All outcomes |
Low risk | Single, researcher blinded to group status, untested. |
| Incomplete outcome data addressed? All outcomes |
High risk | 83.3% of participants in the analysis (10/12). Two participants in the exercise arm did not attend first session. These participants were excluded from the results |
| Free of selective reporting? | High risk | Several SDs were not reported for PANSS, BMI, and Percentage Body Fat |
| Free of other bias? | High risk | Small sample size. |
| Methods | Allocation: randomised. Blinding: single. Duration: 15 weeks. Setting: National Institute of Mental Health and Neuro Sciences, Bangalore, India |
|
| Participants | Diagnosis: schizophrenia, any subtype, DSM-IV. N=61. Age: mean ~ 31 years. Sex: 42M, 19F. |
|
| Interventions |
|
|
| Outcomes | Mental State: PANSS positive, negative, depression, anergia, total score. General Functioning: SOFS score. Adverse effects: SAS, AIMS total score. Qualty of Life: World Health Organization Quality of LIfe BREF version - psychological, physical, social and environmental QofL Unable to use - Qualty of Life: World Health Organization Quality of LIfe BREF version - total Qofl (score not reported) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Computer generated. |
| Allocation concealment? | Unclear risk | No details given. |
| Blinding? All outcomes |
Low risk | Single, researcher blinded to group status, untested. |
| Incomplete outcome data addressed? All outcomes |
High risk | 67.2% of participants in the analysis (41/61). Then participants in each study arm left early because of disinterest and long distance from hospital. These participants were excluded from the results |
| Free of selective reporting? | High risk | Quality of life total data not reported. |
| Free of other bias? | High risk | No true control group used. Exercise compared with yoga. Same therapist delivered both conditions |
| Methods | Allocation: randomised. Blinding: unknown. Duration: 12 weeks. Setting: community centre, Toronto, Canada. |
|
| Participants | Diagnosis: schizophrenia, any subtype, DSM-IV. N=13. Age: mean ~ 45 years. Sex: 8M, 5F. |
|
| Interventions |
|
|
| Outcomes | Mental state: Mental Health Inventory (MHI) - total, depression, positive affect, behavioral, anxiety scores. Physical fitness: Six Minute Walk Test, maximum strength. Satisfaction with treatment: Satisfaction and Feedback survey. Leaving study early. Unable to use - Weight: BMI, resting blood, waist and hip circumferences (data not reported) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors’ judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Two options for group assignments were identified on an equal number of identical cards and blindly chosen from a selection box |
| Allocation concealment? | Low risk | Random draw by an independent observer uninvolved in the study. |
| Blinding? All outcomes |
Unclear risk | Single, researcher blinded to group status, untested. |
| Incomplete outcome data addressed? All outcomes |
Low risk | 100% of participants in the analysis (13/13). |
| Free of selective reporting? | High risk | Not all anthropometric measurements were reported. |
| Free of other bias? | High risk | Small sample size. |
Characteristics of excluded studies [author-defined order]
| Study | Reason for exclusion |
|---|---|
| Acil 2008 | Allocation: quasi-experimental design. |
| Adams 2001 | Allocation: unclear. |
| Apter 1978 | Allocation: randomised. Participants: uncertain how many individuals were diagnosed with schizophrenia |
| Hu 2004 | Allocation: randomised. Participants: schizophrenia. Intervention: included both music and sports therapy. |
| Li 2005 | Allocation: randomised. Participants: schizophrenia. Intervention: included both music and sports therapy. |
| Liu 2006 | Allocation: randomised. Participants: schizophrenia. Intervention: Drug trial, no exercise or physical activity. |
| Skrinar 2005 | Allocation: randomised. Participants: less than 50% of the participants had a diagnosis of schizophrenia |
| Su 1999 | Allocation: randomised. Participants:schizophrenia. Intervention: included both music and sports therapy. |
| Wu 2008 | Allocation: randomised. Participants: schizophrenia. Intervention: lifestyle components included physical activity and diet modification. Not possible to clearly link physical activity to mental health outcomes |
| Wu 2007 | Allocation: randomised Participants: schizophrenia. Intervention: lifestyle component included physical activity and diet modification. Not possible to clearly link physical activity to mental health outcomes |
Characteristics of studies awaiting assessment [ordered by study ID]
| Methods | Allocation: randomised. Blinding: unclear, no details provided. Duration: Unclear, no details provided. Setting: China. |
| Participants | Diagnosis: schizophrenia. N=60. Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Exercise Therapy Group: unclear, no details provided. N=30. Standard Care Group: unclear, no details provided. N=30. |
| Outcomes | Unclear, no details provided. |
| Notes | Paper needs to be translated. |
| Methods | Allocation: randomised. Blinding: unclear, no details provided. Duration: unclear, no details provided. Setting: unclear, no details provided. |
| Participants | Diagnosis: schizophrenia (ICD 10, F20). N=40. Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Physical activity Group: unclear, no details provided. Control Group: unclear, no details provided. |
| Outcomes | Mental State. PANSS. General Functioning. Short-form Health Survey-36. |
| Notes | Details being sought from author. |
| Methods | Allocation: randomised. Blinding: unclear, no details provided. Duration: unclear, no details provided. Setting: China. |
| Participants | Diagnosis: schizophrenia. N=80. Age: unclear, no details provided. Sex: 80F. |
| Interventions | Jianshen Gymnastics Group: Jianshen gymnastics and common treatment. Control Group: Common treatment. |
| Outcomes | Mental state. PANSS, SANS. Behaviour. NOSIE. |
| Notes | Paper needs to be translated. |
| Methods | Allocation: randomised. Blinding: unclear, no details provided. Duration: Unclear, no details provided. Setting: Germany. |
| Participants | Diagnosis: schizophrenia. N = unclear, no details provided. Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Horse Riding Group: Unclear, no details provided. Control Group: Unclear, no details provided. |
| Outcomes | Unclear, no details provided. |
| Notes | Paper needs to be translated. |
| Methods | Allocation: randomised. Blinding: unclear. Duration: unclear, no details provided. Setting: China. |
| Participants | Diagnosis: Schizophrenia. N=128. Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Exercise Therapy: unclear, no details provided. Standard Care: unclear, no details provided. |
| Outcomes | Mental State. PANSS. General Functioning. IPROS. Behaviour. NOSIE. Leaving study early. |
| Notes | Paper needs to be translated to obtain further details. |
| Methods | Allocation: randomised. Blinding: unclear, no details provided. Duration: unclear, no details provided. Setting: working and Entertainment Treatment Room, Mental Health Centre of Shantou University, Shantou, China |
| Participants | Diagnosis: schizophrenia. N=80. Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Yoga Group: yoga exercises for 8 weeks in addition to antipsychotic treatment. N=38. Control Group: N=42. |
| Outcomes | Quality of Life. |
| Notes | Paper needs to be translated to obtain further details. |
| Methods | Allocation: randomised. Blinding: unclear. Duration: unclear, no details provided. Setting: China. |
| Participants | Diagnosis: schizophrenia. N=58. Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Exercise Therapy: unclear, no details provided. Standard Care: unclear, no details provided. |
| Outcomes | Nurses’ observation scale for inpatient evaluation (NOSIE). |
| Notes | Paper needs to be translated to obtain further details. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Effectiveness of a lifestyle intervention for increasing physical activity in adults with schizophrenia |
| Methods | Allocation: randomised. Blinding: single. Duration: unclear, no details provided. Setting: San Diego, CA. |
| Participants | Diagnosis: schizophrenia. N = 86 (expected enrolment). Age: unclear, no details provided. Sex: unclear, no details provided. |
| Interventions | Physical activity and leisure Group: 90minute sessions conducted weekly for the first 16 weeks, then biweekly for the following 8 weeks. Sessions will focus on short and long term goals, learning about physical activity, and playing leisure activities (e.g., board games). Participants will also have opportunities to socialise with each other Control Group: unclear, no details provided. |
| Outcomes | Physical Fitness. Cardiovascular Measures. Weight. BMI. Qualifty of Life. |
| Starting date | June 2006. |
| Contact information | Laurie Lindamer UC San Diego 858 552 8585 x3870 llindamer@ucsd.edu |
| Notes |
DATA AND ANALYSES
Comparison 1.
COMPARISON 1: EXERCISE versus STANDARD CARE
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mental state 1a: Mental Health Inventory Total - Endpoint score: high score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 7.40 [−2.46, 17.26] |
| 2 Mental State 1b: Mental Health Inventory Depression - Endpoint: high score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 17.5 [6.70, 28.30] |
| 3 Mental state 1c: Mental Health Inventory Positive Affect - Endpoint: high score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 3.30 [−23.66, 30.26] |
| 4 Mental state 1d: Mental Health Inventory Behavioural - Endpoint: high score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | −5.40 [−21.28, 10.48] |
| 5 Mental state 1e: Mental Health Inventory Anxiety - Endpoint: high score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [0.80, 15.20] |
| 6 Mental state 2a: PANSS Negative - Endpoint: low score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | −8.5 [−11.11, −5.89] |
| 7 Mental state 2b: PANSS Positive - Endpoint: low score good | 1 | 10 | Mean Difference (IV, Fixed, 95% CI) | −2.5 [−4.73, −0.27] |
| 8 Physical fitness 1: Six minute walking test - Endpoint: High score good | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 79.50 [33.82, 125.18] |
| 9 Physical fitness 2: Maximal strength - Endpoint: High score good | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [0.55, 3.45] |
| 10 Physical Fitness 3: Cardiovascular measures 1: Blood pressure | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | −1.0 [−8.05, 6.05] |
| 11 Weight 1: BMI | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | −1.20 [−2.92, 0.52] |
| 12 Weight 2: Percentage body fat | Other data | No numeric data | ||
| 13 Weight 3: Waist and Hip Ratio | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [−0.02, 0.04] |
| 14 Weight 4: Final Weight | 1 | 13 | Mean Difference (IV, Fixed, 95% CI) | 1.30 [−3.64, 6.24] |
| 15 Leaving the study early | 2 | 25 | Risk Ratio (M-H, Fixed, 95% CI) | 5.0 [0.29, 86.43 |
Comparison 2.
COMPARISON 2: EXERCISE versus OTHER TREATMENT
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mental state 1a: PANSS Total - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 14.95 [2.60, 27.30] |
| 2 Mental state 1b: PANSS Depression - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 2.89 [0.86, 4.92] |
| 3 Mental state 1c: PANSS Anergia - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 2.40 [0.47, 4.33] |
| 4 Mental state 1d: PANSS Positive - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 2.41 [−1.20, 6.02] |
| 5 Mental state 1d: PANSS Negative - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 5.56 [1.69, 9.43] |
| 6 General functioning 1: SOFS - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 4.35 [−1.18, 9.88] |
| 7 Adverse effects 1: SAS - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [−0.44, 1.44] |
| 8 Adverse effects 2: AIMS - Endpoint: low score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [−1.18, 1.58] |
| 9 Quality of life 1a: WHOQOL-100 Physical - Endpoint: High score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | −9.22 [−18.86, 0.42] |
| 10 Quality of life 1b: WHOQOL-100 Psychological - Endpoint: High score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | −17.70 [−28.90, −6.50] |
| 11 Quality of life 1c: WHOQOL-100 Social - Endpoint: High score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | −20.75 [−34.08, −7.42] |
| 12 Quality of life 1d: WHOQOL-100 Environmental - Endpoint: High score good | 1 | 41 | Mean Difference (IV, Fixed, 95% CI) | −18.09 [−28.52, −7.66] |
| 13 Leaving the study early | 1 | 61 | Risk Ratio (M-H, Fixed, 95% CI) | 0.94 [0.47, 1.88 |
Analysis 1.1. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 1 Mental state 1a: Mental Health Inventory Total - Endpoint score: high score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 1 Mental state 1a: Mental Health Inventory Total - Endpoint score: high score good
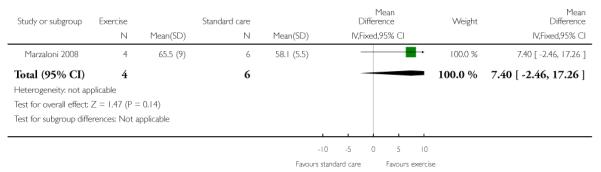 |
Analysis 1.2. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 2 Mental State 1b: Mental Health Inventory Depression - Endpoint: high score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 2 Mental State 1b: Mental Health Inventory Depression - Endpoint: high score good
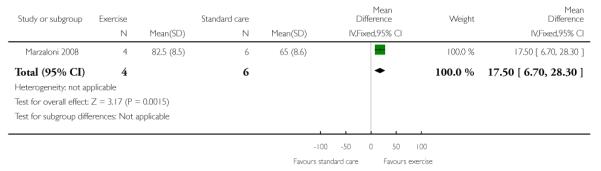 |
Analysis 1.3. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 3 Mental state 1c: Mental Health Inventory Positive Affect - Endpoint: high score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 3 Mental state 1c: Mental Health Inventory Positive Affect - Endpoint: high score good
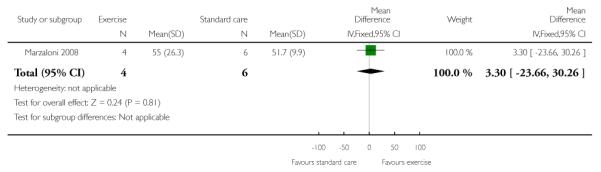 |
Analysis 1.4. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 4 Mental state 1d: Mental Health Inventory Behavioural - Endpoint: high score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 4 Mental state 1d: Mental Health Inventory Behavioural - Endpoint: high score good
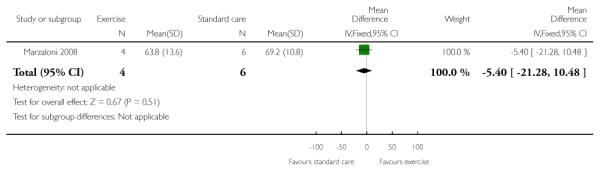 |
Analysis 1.5. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 5 Mental state 1e: Mental Health Inventory Anxiety - Endpoint: high score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 5 Mental state 1e: Mental Health Inventory Anxiety - Endpoint: high score good
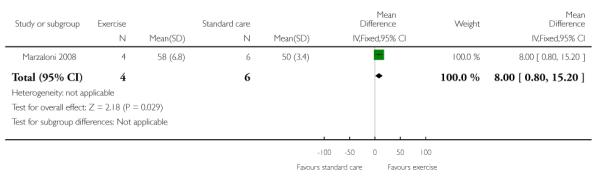 |
Analysis 1.6. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 6 Mental state 2a: PANSS Negative - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 6 Mental state 2a: PANSS Negative - Endpoint: low score good
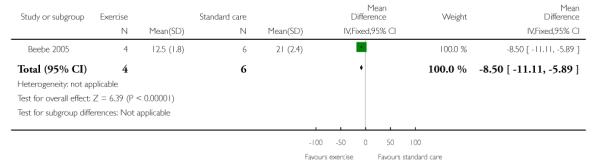 |
Analysis 1.7. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 7 Mental state 2b: PANSS Positive - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 7 Mental state 2b: PANSS Positive - Endpoint: low score good
 |
Analysis 1.8. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 8 Physical fitness 1: Six minute walking test - Endpoint: High score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 8 Physical fitness 1: Six minute walking test - Endpoint: High score good
 |
Analysis 1.9. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 9 Physical fitness 2: Maximal strength - Endpoint: High score good
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 9 Physical fitness 2: Maximal strength - Endpoint: High score good
 |
Analysis 1.10. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 10 Physical Fitness 3: Cardiovascular measures 1: Blood pressure
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 10 Physical Fitness 3: Cardiovascular measures 1: Blood pressure
 |
Analysis 1.11. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 11 Weight 1: BMI
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 11 Weight 1: BMI
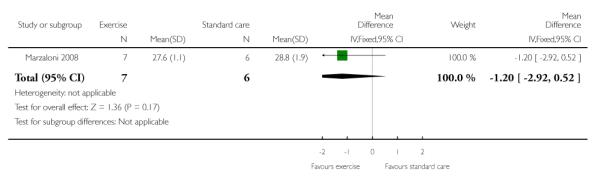 |
Analysis 1.12. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 12 Weight 2: Percentage body fat
Weight 2: Percentage body fat
| Study | Exercise Group | Standard care Group |
|---|---|---|
| Beebe 2005 | reduced body fat by 3.7% | reduced body fat by 0.02% |
Analysis 1.13. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 13 Weight 3: Waist and Hip Ratio
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 13 Weight 3: Waist and Hip Ratio
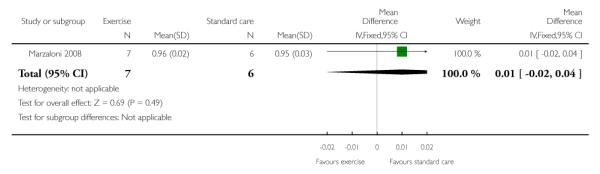 |
Analysis 1.14. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 14 Weight 4: Final Weight
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 14 Weight 4: Final Weight
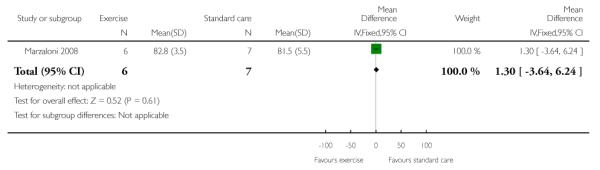 |
Analysis 1.15. Comparison 1 COMPARISON 1: EXERCISE versus STANDARD CARE, Outcome 15 Leaving the study early
Review: Exercise therapy for schizophrenia
Comparison: 1 COMPARISON 1: EXERCISE versus STANDARD CARE
Outcome: 15 Leaving the study early
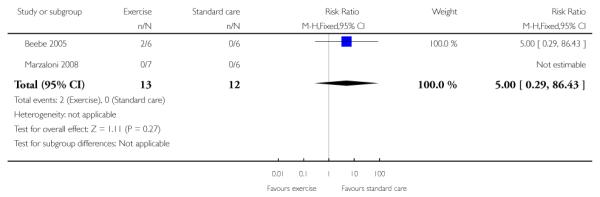 |
Analysis 2.1. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 1 Mental state 1a: PANSS Total - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 1 Mental state 1a: PANSS Total - Endpoint: low score good
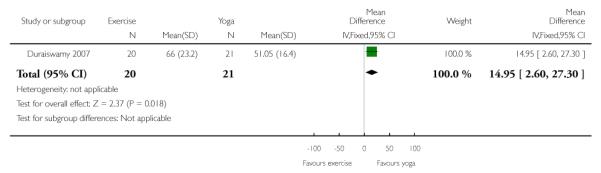 |
Analysis 2.2. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 2 Mental state 1b: PANSS Depression - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 2 Mental state 1b: PANSS Depression - Endpoint: low score good
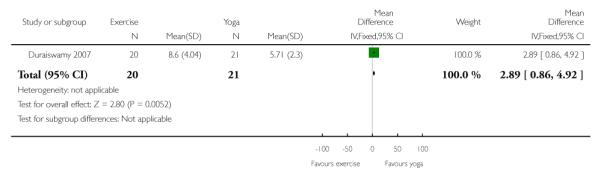 |
Analysis 2.3. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 3 Mental state 1c: PANSS Anergia - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 3 Mental state 1c: PANSS Anergia - Endpoint: low score good
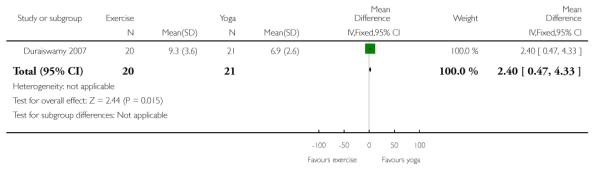 |
Analysis 2.4. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 4 Mental state 1d: PANSS Positive - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 4 Mental state 1d: PANSS Positive - Endpoint: low score good
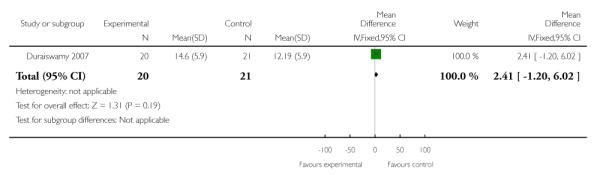 |
Analysis 2.5. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 5 Mental state 1d: PANSS Negative - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 5 Mental state 1d: PANSS Negative - Endpoint: low score good
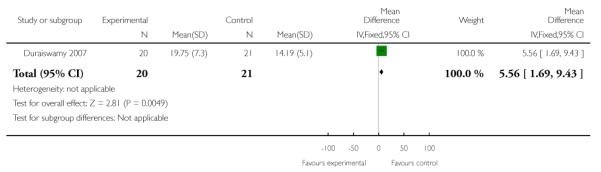 |
Analysis 2.6. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 6 General functioning 1: SOFS - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 6 General functioning 1: SOFS - Endpoint: low score good
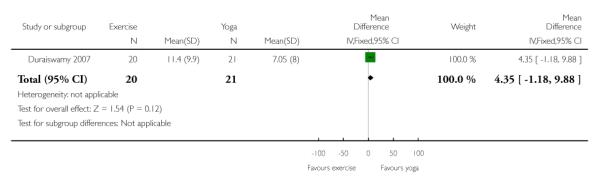 |
Analysis 2.7. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 7 Adverse effects 1: SAS - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 7 Adverse effects 1: SAS - Endpoint: low score good
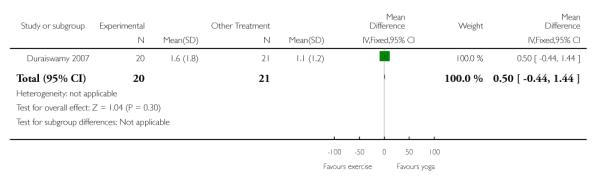 |
Analysis 2.8. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 8 Adverse effects 2: AIMS - Endpoint: low score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 8 Adverse effects 2: AIMS - Endpoint: low score good
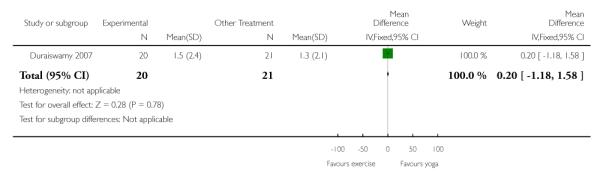 |
Analysis 2.9. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 9 Quality of life 1a: WHOQOL-100 Physical - Endpoint: High score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 9 Quality of life 1a: WHOQOL-100 Physical - Endpoint: High score good
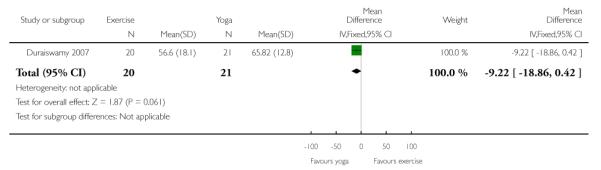 |
Analysis 2.10. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 10 Quality of life 1b: WHOQOL-100 Psychological - Endpoint: High score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 10 Quality of life 1b: WHOQOL-100 Psychological - Endpoint: High score good
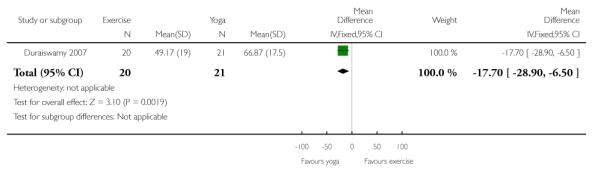 |
Analysis 2.11. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 11 Quality of life 1c: WHOQOL-100 Social - Endpoint: High score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 11 Quality of life 1c: WHOQOL-100 Social - Endpoint: High score good
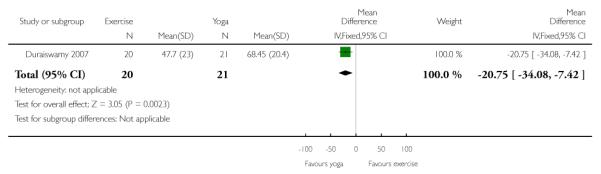 |
Analysis 2.12. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 12 Quality of life 1d: WHOQOL-100 Environmental - Endpoint: High score good
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 12 Quality of life 1d: WHOQOL-100 Environmental - Endpoint: High score good
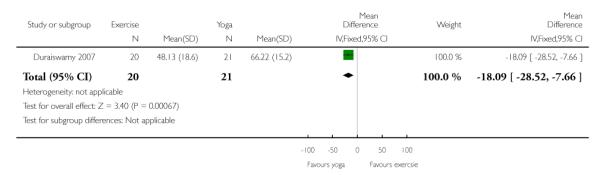 |
Analysis 2.13. Comparison 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT, Outcome 13 Leaving the study early
Review: Exercise therapy for schizophrenia
Comparison: 2 COMPARISON 2: EXERCISE versus OTHER TREATMENT
Outcome: 13 Leaving the study early
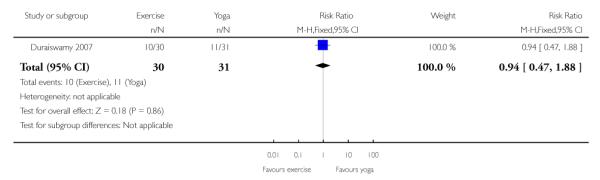 |
HISTORY
Protocol first published: Issue 4, 2003
Review first published: Issue 5, 2010
| Date | Event | Description |
|---|---|---|
| 12 May 2010 | Amended | PANNS changed to PANSS |
| 24 July 2008 | Amended | Converted to new review format. |
WHAT’S NEW
Last assessed as up-to-date: 9 June 2009.
| Date | Event | Description |
|---|---|---|
| 11 May 2011 | Amended | Contact details updated. |
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
This review’s main focus was to examine the mental health outcomes (e.g. mental states, general function) of physical activity and exercise. A secondary focus to address physical health outcomes (e.g. physical fitness, weight) was added in a recent revision. This secondary focus was added to examine the data for any potential intervention effects that may have a dual role and address both mental and physical health indicators.
Footnotes
DECLARATIONS OF INTEREST None known.
References to studies included in this review
- Beebe 2005 {published data only} .Beebe LH, Tian L, Morris N, Goodwin A, Allen SS, Kuldau J. Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues in Mental Health Nursing. 2005;26(6):661–76. doi: 10.1080/01612840590959551. [PUBMED: 16020076] [DOI] [PubMed] [Google Scholar]
- Duraiswamy 2007 {published data only} .Duraiswamy G, Thirthalli J, Nagendra HR, Gangadhar BN. Yoga therapy as an add-on treatment in the management of patients with schizophrenia - a randomized controlled trial. Acta Psychiatrica Scandinavica. 2007;116(3):226–32. doi: 10.1111/j.1600-0447.2007.01032.x. [PUBMED: 17655565] [DOI] [PubMed] [Google Scholar]
- Marzaloni 2008 {published data only} .Marzaloni S, Jensen B, Melville P. Feasibility and effects of a group-based resistance and aerobic exercise program for individuals with schizophrenia: a multidisciplinary approach. Mental Health and Physical Activity. 2009;2(1):29–36. [Google Scholar]
References to studies excluded from this review
- Acil 2008 {published data only} .Acil AA, Dogan S, Dogan O. The effects of physical exercises to mental state and quality of life in patients with schizophrenia. Journal of Psychiatric and Mental Health Nursing. 2008;15:808–15. doi: 10.1111/j.1365-2850.2008.01317.x. [DOI] [PubMed] [Google Scholar]
- Adams 2001 {published data only} .Adams L. Randomized control trial of the effects of an exercise intervention programme on the symptomatology of people with schizophrenia. The pilot study.. National Research Register. 2001 [Google Scholar]
- Apter 1978 {published data only} .Apter A, Sharir I, Tyano S, Wijsenbeek H. Movement therapy with psychotic adolescents. British Journal of Medical Psychology. 1978;51:155–59. doi: 10.1111/j.2044-8341.1978.tb02460.x. [DOI] [PubMed] [Google Scholar]
- Hu 2004 {published data only} .Hu Q-L, Xue L-H, Gao X-H. Effect of music-sport therapy on the insight and behavioral disturbance in patients with schizophrenia. Zhongguo Linchuang Kangfu. 2004;8(9):1626–27. [Google Scholar]
- Li 2005 {published data only} .Li M, Wang H, Li X. Effect of music and sport therapy as assistant treatment for schizophrenia. Heilongjiang Nursing Journal. 2005;11(20):1677–78. [Google Scholar]
- Liu 2006 {published data only} .Liu L-F, Yang T, Xiao Z-B. Comparative study between brisking and risperidone in treatment of schizophrenia. Medical Journal of Chinese Civil Administration. 2006;18(9):716–18. [Google Scholar]
- Skrinar 2005 {published data only} .Skrinar GS, Huxley NA, Hutchinson DS, Menninger E, Glew P. The role of a fitness intervention on people with serious psychiatric disabilities. Psychiatric Rehabilitation Journal. 2005;29(2):122–27. doi: 10.2975/29.2005.122.127. [DOI] [PubMed] [Google Scholar]
- Su 1999 {published data only} .Su L, Fan Z, Qu Y. The effect of dance therapy for chronic schizophrenia patient. Chinese Journal of Psychiatry. 1999;32(3):167–69. [Google Scholar]
- Wu 2007 {published data only} .Wu M-K, Wang C-K, Bai Y-M, Huang C-Y, Lee S-D. Outcomes of obese, clozapine-treated inpatients with schizophrenia placed on a six-month diet and physical activity program. Psychiatric Services. 2007;58(4):544–50. doi: 10.1176/ps.2007.58.4.544. [DOI] [PubMed] [Google Scholar]
- Wu 2008 {published data only} .Wu R-R, Zhao J-P, Jin H, Shao P, Fang M-S, Guo X-F, He Y-Q, Liu Y-J, Chen J-D, Li L-H. Lifestyle intervention and metformin for treatment of antipsychotic-induced weight gain: A randomized controlled trial. JAMA. 2008;299(2):185–93. doi: 10.1001/jama.2007.56-b. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
- Lin 2006 {published data only} .Lin MR. The effect of ’sit ups’ on constipation in patients with schizophrenia. International Journal of Nursing. 2006;25(1):58–9. [Google Scholar]
- NCT00286299 {published data only} .Nilsberg G. Aerobic endurance training and effect on symptoms of schizophrenia. 2006 http://www.clinicaltrials.gov
- Ning 2003 {published data only} .Ning XH, Chen YX, Lu F. The effect of jianshen gymnastics on the negative symptoms of schizophrenia. Chinese journal of Behavioral Medical Science. 2003;7478(3):329. [Google Scholar]
- Scheidhacker 1991 {published data only} .Scheidhacker M, Bender W, Vaitl P. The efficacy of horse-riding in the treatment of chronic schizophrenic patients [Die wirksamkeit des therapeutischen reitens bei behandlung chronisch schizophrener patienten: experimentelle ergebnisse und klinische erfahrungen] Nervenarzt. 1991;62:283–7. [PubMed] [Google Scholar]
- Wu 2007b {published data only} .Wu J. The role of exercise rehabilitation in chronic schizophrenic patients. Medical Journal of Chinese People’s Health. 2007;19(17):799, 801. [Google Scholar]
- Xie 2006 {published data only} .Xie J, Lin Y-H, Guo C-R, Chen F. Study on influences of yoga on quality of life of schizophrenic inpatients. Nanfang Journal of Nursing. 2006;13(1):9–10. [Google Scholar]
- Zhang 2006 {published data only} .Zhang Q. The role of physical therapy in rehabilitation of patients with chronic schizophrenia. Medical Journal of Chinese People’s Health. 2006;18(23):1066. [Google Scholar]
References to ongoing studies
- NCT00338832 {published data only} .Lindamer L, Delapena J. Adapting a physical activity intervention for schizophrenia. 2006 http://www.clinicaltrials.gov [Google Scholar]
Additional references
- Altman 1996 .Altman DG, Bland JM. Detecting skewness from summary information. BMJ. 1996;313:1200. doi: 10.1136/bmj.313.7066.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg 1996 .Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, Pitkin R, Rennie D, Schulz KF, Simel D, Stroup DF. Improving the quality of randomized controlled trials: The CONSORT statement. JAMA. 1996;276:637–9. doi: 10.1001/jama.276.8.637. [DOI] [PubMed] [Google Scholar]
- Bland 1997 .Bland JM, Kerry SM. Statistics notes. Trials randomised in clusters. BMJ. 1997;315:600. doi: 10.1136/bmj.315.7108.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boissel 1999 .Boissel JP, Cucherat M, Li W, Chatellier G, Gueyffier F, Buyse M, Boutitie F, Nony P, Haugh M, Mignot G. The problem of therapeutic efficacy indices. 3. Comparison of the indices and their use. Therapie. 1999;54(4):405–11. [PubMed] [Google Scholar]
- Boutron 2004 .Boutron I, Tubach F, Giraudeau B, Ravaud P. Blinding was judged more difficult to achieve and maintain in nonpharmacologic than pharmacologic trials. Journal of Clinical Epidemiology. 2004;57:543–50. doi: 10.1016/j.jclinepi.2003.12.010. [DOI] [PubMed] [Google Scholar]
- Brown 1999 .Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychological Medicine. 1999;29(3):697–701. doi: 10.1017/s0033291798008186. [DOI] [PubMed] [Google Scholar]
- Caspersen 1985 .Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise,and physical fitness:Definitions and distinctions for health-related research. Public Health Reports. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- Chamove 1986 .Chamove AS. Positive short-effects of activity on behavior in chronic-schizophrenic patients. British Journal of Clinical Psychology. 1986;25(2):125–33. doi: 10.1111/j.2044-8260.1986.tb00681.x. [DOI] [PubMed] [Google Scholar]
- Davidson 2001 .Davidson S, Judd F, Jolley D, Hocking B, Thompson S, Hyland B. Cardiovascular risk factors for people with mental illness. The Australian and New Zealand Journal of Psychiatry. 2001;35:196–202. doi: 10.1046/j.1440-1614.2001.00877.x. [DOI] [PubMed] [Google Scholar]
- Deeks 2000 .Deeks J. Issues in the selection for meta-analyses of binary data. Proceedings of the 8th International Cochrane Colloquium; Cape Town. 2000 Oct 25-28; Cape Town: Cochrane Collaboration; 2000. [Google Scholar]
- Divine 1992 .Divine GW, Brown JT, Frazer LM. The unit of analysis error in studies about physicians’ patient care behavior. Journal of General Internal Medicine. 1992;7:623–29. doi: 10.1007/BF02599201. [DOI] [PubMed] [Google Scholar]
- Donner 2002 .Donner A, Klar N. Issues in the meta-analysis of cluster randomized trials. Statistics in Medicine. 2002;21:2971–80. doi: 10.1002/sim.1301. [DOI] [PubMed] [Google Scholar]
- DSM-IV 1994 .American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Vol. 4. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Egger 1997 .Egger M, Davey-Smith G, Schneider M, Minder CSO. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal. 1997;13:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis 2007 .Ellis N, Crone D, Davey R, Groga S. Exercise interventions as an adjunct therapy for psychosis: A critical review. British Journal of Clinical Psychology. 2007;46(1):95–111. doi: 10.1348/014466506x122995. [DOI] [PubMed] [Google Scholar]
- Enright 1998 .Enright PL, Sherrill DL. Reference equations for the 6-minute walk in healthy adults. American Journal of Respiratory and Critical Care Medicine. 1998;158:1384–87. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- Faulkner 1999 .Faulkner G, Sparkes A. Exercise as therapy for schizophrenia: An ethnographic study. Journal of Sport and Exercise Psychology. 1999;21:52–69. [Google Scholar]
- Faulkner 2005 .Faulkner G. Exercise as an adjunct treatment for schizophrenia. In: Faulkner G, Taylor A, editors. Exercise, Health, and Mental Health: Emerging Relationships. Routledge; London, UK: 2005. pp. 27–47. [Google Scholar]
- Faulkner 2005b .Faulkner G, Taylor AH. Exercise, Health and Mental Health: Emerging relationships between physical activity and psychological well-being. 1st Edition Routledge; London: 2005. [Google Scholar]
- Faulkner 2006 .Faulkner G, Carless D. Physical activity and the process of psychiatric rehabilitation: Theoretical and methodological issues. Psychiatric Rehabilitation Journal. 2006;29:258–66. doi: 10.2975/29.2006.258.266. [DOI] [PubMed] [Google Scholar]
- Goff 2005 .Goff DC, Sullivan LM, McEvoy JP, Meyer JM, Nasrallah HA, Daumit GL, Lamberti S, D’Agostino RB, Stroup TS, Davis S, Lieberman JA. A comparison of ten-year cardiac risk estimates in schizophrenia patients from the CATIE study and matched controls. Schizophrenia Research. 2005;80:45–53. doi: 10.1016/j.schres.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Gulliford 1999 .Gulliford MC, Ukoumunne OC, Chinn S. Components of variance and intraclass correlations for the design of community-based surveys and intervention studies: data from the Health Survey for England 1994. American Journal of Epidemiology. 1999;149:876–83. doi: 10.1093/oxfordjournals.aje.a009904. [DOI] [PubMed] [Google Scholar]
- Higgins 2003 .Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins 2008 .Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0.1. The Cochrane Collaboration; [updated September 2008]. 2008. Available from www.cochrane-handbook.org. The Cochrane Collaboration. [Google Scholar]
- Jüni 2001 .Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ. 2001;323:42–46. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay 1986 .Kay SR. Positive and negative symptom (PANSS) scale manual. Schizophrenia Bulletin. 1986;13:261–78. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Lambert 2003 .Lambert TJR, Velakoulis D, Pantelis C. Medical comorbidity in schizophrenia. Medical Journal of Australia. 2003;178(Suppl 9):S67–S70. doi: 10.5694/j.1326-5377.2003.tb05311.x. [DOI] [PubMed] [Google Scholar]
- Lykouras 2008 .Lykouras L, Douzenis A. Do psychiatric departments in general hospitals have an impact on the physical health of mental patients? Current Opinion in Psychiatry. 2008;21(4):398–402. doi: 10.1097/YCO.0b013e32830079d0. [DOI] [PubMed] [Google Scholar]
- Marshall 2000 .Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry. 2000;176:249–52. doi: 10.1192/bjp.176.3.249. [DOI] [PubMed] [Google Scholar]
- McGrath 2008 .McGrath J, Saha S, Chant D, Welham J. Schizophrenia: A concise overview of incidence, prevalence, and mortality. Epidemiologic Reviews. 2008;30(1):67–76. doi: 10.1093/epirev/mxn001. [DOI] [PubMed] [Google Scholar]
- Meyer 2003 .Meyer JM, Nasrallah HA. Medical Illness and Schizophrenia. Vol. 1. American Psychiatric Press, Inc; Washington, D.C: 2003. [Google Scholar]
- Moher 2001 .Moher D, Schulz KF, Altman D, CONSORT Group The CONSORT statement: Revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–91. doi: 10.1001/jama.285.15.1987. [DOI] [PubMed] [Google Scholar]
- Munetz 1988 .Munetz MR, Benjamin S. How to examine patients using the Abnormal Involuntary Movement Scale. Hospital and Community Psychiatry. 1988;39:1172–7. doi: 10.1176/ps.39.11.1172. [DOI] [PubMed] [Google Scholar]
- Mutrie 2003 .Mutrie N, Faulkner G. Physical activity and mental health. In: Everett T, Donaghy M, Fever S, editors. Physiotherapy and Occupational Therapy in Mental Health: An evidence based approach. Routledge; London: 2003. pp. 82–97. [Google Scholar]
- Saraswat 2006 .Saraswat N, Rao K, Subbakrishna DK, Gangadhar BN. The Social Occupational Functioning Scale (SOFS): a brief measure of functional status in persons with schizophrenia. Schizophrenia Research. 2006;81:301–9. doi: 10.1016/j.schres.2005.09.008. [DOI] [PubMed] [Google Scholar]
- Schulz 2001 .Schulz KF. Assessing allocation concealment and blinding in randomised controlled trials: why bother? Evidence Based Nursing. 2001;4(1):4–6. doi: 10.1136/ebn.4.1.4. [DOI] [PubMed] [Google Scholar]
- Simpson 1970 .Simpson GM, Angus JWS. A rating scale for extrapyramidal side-effects. Acta Psychiatrica Scandinavica Supplementum. 1970;212:11–9. doi: 10.1111/j.1600-0447.1970.tb02066.x. [DOI] [PubMed] [Google Scholar]
- Skevington 2004 .Skevington SM, Lotfy M, O’Connell KA. The World Health Organization’s Whoqol-Bref quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL group. Quality of Life Research. 2004;13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00. [DOI] [PubMed] [Google Scholar]
- Ukoumunne 1999 .Ukoumunne OC, Gulliford MC, Chinn S, Sterne JAC, Burney PGJ. Methods for evaluating area-wide and organistation-based intervention in health and health care: a systematic review. Health Technology Assessment. 1999;3(5):1–75. [PubMed] [Google Scholar]
- Veit 1983 .Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology. 1983;51:730–42. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- Ware 1998 .Ware JE, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. Journal of Clinical Epidemiology. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- Xia 2007 .Xia J, Adams CE, Bhagat N, Bhoopathi P, El-Sayeh H, Pinfold V. Takriti Y. The Leeds Outcomes Stakeholders Survey (LOSS) study. Proceedings of the 15th Cochrane Cologquium; Sao Paulo. 2007 Oct 23-27; Cochrane Collaboration; 2007. [Google Scholar]
- * Indicates the major publication for the study