Abstract
Background & objectives:
Evidence has suggested that parenting styles have peculiar characteristics in families with drug-related issues. This study was undertaken to investigate the perception of crack (smoke cocaine) users and non-users about parental bonding quality regarding care and control in Brazil.
Methods:
A total of 198 hospitalized crack users and 104 users of any non-illicit drug were assessed using the Parental Bonding Instrument (PBI), the sixth version of the Addiction Severity Index (ASI) and Mini International Neuropsychiatric Interview (MINI).
Results:
Adjusted logistic regression analysis showed that crack users were more likely (ORadj = 9.68; 95% CI: 2.82, 33.20) to perceive neglectful mothers, as well as more likely (ORadj = 4.71, 95% CI: 2.17, 10.22) to perceive controlling and affectionless fathers in comparison with non-illicit drug users who were more likely to perceive optimal parenting.
Interpretation & conclusions:
Our findings indicate that the perception of neglectful mothers and affectionless controlling fathers may be associated with the tendency of the children to be less resilient when facing stressful events, leading them to a greater risk to use crack.
Keywords: Crack, dependency, drug abuse and exposure, family functioning, parenting style
Studies have suggested that aspects linked to drug users’ families, specifically in terms of environment and parental care related to affection, protection, control, and authoritative parenting, are predictors of development and maintenance of drug dependence1,2. Conversely, parental practices such as protection, monitoring, and involvement in the children's activities are considered protective factors against the initiation of drug use, especially in adolescence3. Since the harms caused by crack (freebase cocaine, namely, smokable cocaine) to the psychological, familial, and social aspects have been demonstrated in various countries, it is important to investigate the quality of crack users’ parental bonds3,4,5,6. This approach will make it possible to investigate specific factors related to maternal and paternal care, serving as the basis for the implementation of new therapeutic approaches in terms of psychoeducation and prevention. This study was, therefore aimed to investigate the perception of crack users and non-users about parental bonding quality regarding care and control.
Material & Methods
This study was conducted by the Drugs and Alcohol Research Center at the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, Brazil from August 2011 to February 2012. Data were collected in the cities of Canoas and Porto Algre, Brazil. All participants provided the written informed consent. This study protocol was approved by the Ethics Committee at the Hospital de clinicas de Porto Algre under protocol 10-0269. A total of 126 free base cocaine users were enrolled from the Hospital Psiquiátrico São Pedro -Unit specialized for Addiction Treatment- in city of Porto Alegre, South of Brazil and 72 subjects from the São Jose Clinic, specializing in treating chemical dependency, in city of Porto Alegre, South of Brazil. The method of convenience sampling was used. Only male crack users were selected according to the predefined inclusion criteria.
Measures: The perceptions of maternal and paternal care were collected using the Parental Bonding Instrument (PBI), originally developed by Parker7 and validated for the Brazilian population8. The PBI consists of 25 Likert type questions (0 to 3) on children's perception of maternal and paternal care (parental care). Each subject answers 25 questions related to their perception of maternal care and 25 questions on their perception of paternal care relevant to the first 16 years of his life. The PBI measures two constructs: the first one termed care (affection, emotional warmth, empathy, and closeness vs. emotional coldness, indifference, and neglect) and the second one termed control or overprotection (control, intrusion vs. encouragement of autonomy). Although the literature offers several different ways (models) of analysing PBI results in different populations, in this study the data were analyzed according to the Parker's model7. The analysis using this model results in four styles of parenting: optimal parenting (OP) - high care/low control; affectionate control (AC) - high care/high control; affectionless control (AlC) - low care/high control and neglect parenting (NP) - low care/low control. This instrument provides data that make it possible to measure the parental models in relation to care and control7.
The Brazilian version of the Mini International Neuropsychiatric Interview-MINI was administered by research assistants trained to confirm the clinical diagnosis of cocaine-related disorder according to the Diagnositc and Statistical Mannual of Mental Disorders (DSM IV-TR)9. The Kappa coefficient was 0.93 for the interviewers during the pilot study.
Addiction severity index (ASI-6): It consists of a scale of dependence severity that evaluates in detail the following problem areas: medical, employment, legal, family/social, alcohol, drug, psychiatric10. It is a semi-structured interview, which is completed in approximately 45 to 60 min. Such interview estimates the number, the extent, and the duration of problem-symptoms throughout the interviewee's whole life and, specifically, in the 30 days preceding the assessment based on the subjective report of the patient, estimating the severity of the current problem and the need for intervention in each area. This scale was recently adapted and validated for use in Brazil. In this study, only the socio-demographic data collected by ASI-6 was analyzed11.
Procedure: The group of crack users who completed the Parental Bonding Instrument (PBI)-mother scale included male users admitted for treatment at the following types of health care facilities: public psychiatric hospital (n = 126), and a rehab clinic offering mostly private care (n = 72), reaching a total of 198 cases. Of these 198 cases, 178 crack users also completed the PBI-father. All users met the diagnostic criteria for drug dependence according to the DSM IV-TR9. Individuals between 14 and 40 years of age who reported that crack was the major drug related to their drug dependence and the main reason for seeking treatment were included in the study. Crack users with mental retardation, dementia, or another organic brain syndrome, as well as those who, during the interview, showed psychotic symptoms were excluded from the study. The Kappa coefficient was 0.93 for the interviewers during the pilot study.
For the control group, 104 male users of any non-illicit drug e.g. alcohol and tobacco were volunteers, recruited from the records of Posto de Saúde Igara health center specializing in primary care (general practice family medicine), paediatrics and gynaecologist) in Canoas, South of Brazil, according to the neighborhood or geographical area of residence of crack users. They were matched by age, ethnicity and schooling. The initial control sample of non-drug users was 120. From these 16 subjects were excluded for reporting the use of illegal drugs. The sample of non-drug users who completed the PBI-mother included 104 males who denied the use of cocaine/crack, heroin, marijuana and any other illicit drug. Of these subjects, only 98 completed the PBI-father (many reported not having a father/father substitute until they were 16 years old). All non-crack/cocaine and any other illicit drug users were evaluated through the Mini International Neuropsychiatric Interview (MINI) and those subjects were excluded who met the diagnostic criteria for abuse of any psychoactive substance according to the DSM IV-TR and who had severe psychiatric disorders and psychosis, severe depression, among others.
Chi-square test was used to compare the proportions of diagnoses: of alcohol abuse, major depressive episode, social phobia, post traumatic stress disorder, maniac episode, generalized anxiety disorder, antisocial personality disorder and lifetime mood disorder, differed from crack users and non-drug users. Controls were excluded if cocaine use was reported in the last year or if they tested positive for cocaine in a urine screening test. For final modelling, the following variables: age, ethnicity, and educational level were adjusted.
Data analysis: All data were analyzed using the PASW (Predictive Analytics Software) Statistics for Version 18, Chicago, USA. The chi-square test was used to investigate the association of the qualitative variables with the groups (users and non-users). Student's t test for independent samples was used to compare the means between the groups. To create models for the perceptions of parental care, linking users to non-users, adjusted logistic regression was used for the variables age, educational level, and odds ratios (OR) and 95% confidence interval (95%CI) were estimated based on this analysis. In logistic regression, the dependent variable was used for being a crack user or not being a crack user. The independent variables were age, race, education and PBI.
Results
The crack users showed higher rates of psychiatric disorders compared to non-users. Descriptions of positive psychiatric diagnoses were: alcohol abuse (crack users: 11.7%, non-drug users: 0%; P=0.001), major depressive episode (crack users: 28.8%, non-drug users: 5.8%; P<0.001), social phobia (crack users: 14.1%, non-drug users: 4.7%; P=0.041), Post Traumatic Stress Disorder (crack users: 12.1%, non-drug users: 0%; P=0.002), maniac episode (crack users: 23.7%, non-drug users: 7%; P=0.002), generalized anxiety disorder (crack users: 24.6%, non-drug users: 3.8%; P<0.001), antisocial personality disorder before the age of 15 (crack users: 51.7%, non-drug users: 9.4%; P<0.001) and antisocial personality disorder after the age of 18 yr (crack users: 37.8%, non-drug users: 3.5%; P<0.001). The diagnostic of lifetime mood disorder was the only one that was not significant, with results of 62.5 per cent of users and 42.9 per cent of non-drug users (P=0.592).
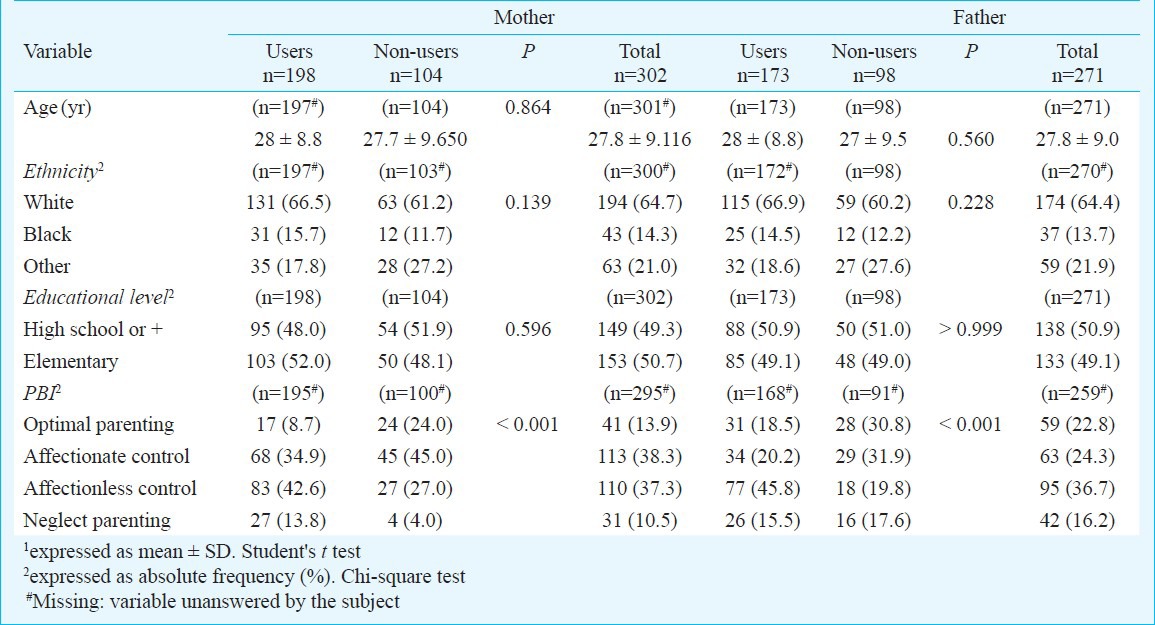
Considering the evident association between optimal parenting (high care/low control) and mental health in the literature and its higher occurrence in the group of non-drug users in our study, optimal style was used as a reference for comparison between users and non-users for maternal and paternal styles. Using Parker's two-factor model, the PBI-mother and father scores were significantly different between crack users and non-drug users (P<0.001) (Table I).
Table I.
Demographic comparison and descriptive analysis of the Parental Bonding Instrument-PBI (mother and father) parenting styles of crack users and non-users
In the univariate analysis (Table II), crack users had more than twice the odds to perceive maternal affectionate constraint (high care/high control) in comparison with subjects who had a perception of paternal optimal parenting. Crack users were much more likely to perceive maternal neglectful style (low care/low control) when compared with the perception of optimal parenting. Crack users had more than four times the odds to perceive maternal affectionless control (low care/high control) when compared with the perception of optimal parenting. In the adjusted logistic regression model (Table II) regarding the perception of maternal care, when adjusted for age, ethnicity, and education level, these odds increased.
Table II.
Univariate and multivariate logistic regression analysis – Parental Bonding Instrument-PBI (Mother and Father)
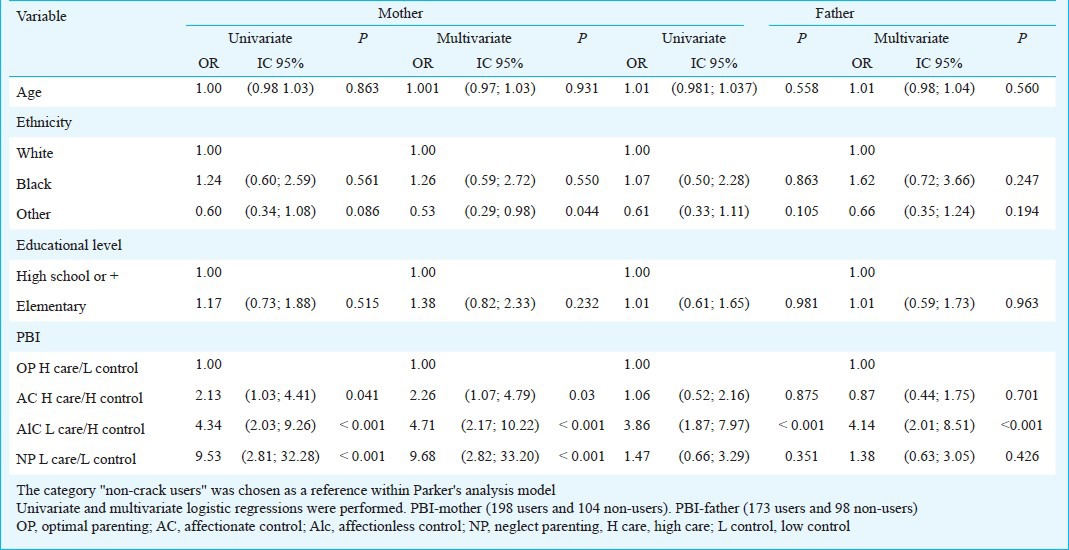
In the univariate analysis, crack users were almost four times more likely to perceive paternal affectionless control when compared with the subjects who perceived optimal parenting. In the adjusted logistic regression model, after adjusting for age, ethnicity, and educational level, these odds were even greater (Table II).
Discussion
Our findings showed that crack users had a perception of neglectful mothering, showing a significant difference from the group of non-users, who reported a predominant perception of maternal optimal parenting. This is similar with other studies about the influence of the family on the process of addiction1,12,13. Epidemiological studies indicate that drug abuse is a public health issue and there is a need for planning of longitudinal studies in order to continue investigating this population14. The major substantive contribution of our study was presenting quantitative data on an important topic for emotional development.
The strength of our study was that we used a community control sample with demographic characteristics similar to those of the clinical sample. Controls lived in poor areas, marked by high violence rates and probably submitted to similar life stressors, except crack use. Conversely, the study had some limitations. It was based on clinical sample with a non-randomized selection. We evaluated only male patients who sought treatment, limiting the generalization of our findings on females and other profiles of crack users. The study also did not assess the participants’ mothers and fathers directly. Finally, the cross-sectional design of our study prevented the conclusions of causality between the main results obtained.
These findings may be useful in planning strategies that involve crack users’ family members, with the purpose of reducing family risk factors, and to contribute to the implementation of public policies aimed at this population, bringing benefits to cases of drug addiction and preventing new cases by means of psychoeducation.
References
- 1.Choquet M, Hassler C, Morin D, Falissard B, Chau N. Perceived parenting styles and tobacco, alcohol and cannabis use among French adolescents: gender and family structure differentials. Alcohol Alcohol. 2008;43:73–80. doi: 10.1093/alcalc/agm060. [DOI] [PubMed] [Google Scholar]
- 2.Brajević-Gizdić I, Mulić R, Pletikosa M, Kljajić Z. Self-perception of drug abusers and addicts and investigators’ perception of etiological factors of psychoactive drug addiction. Coll Antropol. 2009;33:225–31. [PubMed] [Google Scholar]
- 3.Fang L, Schinke SP, Cole KC. Preventing substance use among early Asian-American adolescent girls: initial evaluation of a web-based, mother-daughter program. J Adolesc Health. 2010;47:529–32. doi: 10.1016/j.jadohealth.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dunlap E, Golub A, Johnson BD. The severely-distressed African American family in the Crack Era: Empowerment is not enough. J Social Soc Welf. 2006;33:115–39. [PMC free article] [PubMed] [Google Scholar]
- 5.Kopak AM, Chen AC, Haas SA, Gillmore MR. The importance of family factors to protect against substance use related problems among Mexican heritage and White youth. Drug Alcohol Depend. 2012;124:34–41. doi: 10.1016/j.drugalcdep.2011.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–30. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parker G. The parental bonding instrument: psychometric properties reviewed. Psychiatr Dev. 1989;7:317–35. [PubMed] [Google Scholar]
- 8.Hauck S, Schestatsky S, Terra L, Knijnik L, Sanchez P, Ceitlin LH. Psychometric properties of the sixth version of the Addiction Severity Index (ASI-6) in Brazil. Rev Psiquiatr RS. 2006;28:61–8. doi: 10.1590/s1516-44462012000100006. [DOI] [PubMed] [Google Scholar]
- 9.Amorim P. Mini international neuropsychiatric interview (MINI): validation of a short structured diagnostic psychiatric interview. Rev Bras Psiquiatr. 2000;22:106–15. [PubMed] [Google Scholar]
- 10.McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The addiction severity index at 25: origins, contributions and transitions. Am J Addict. 2006;15:113–24. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- 11.Kessler FH, Cacciola J, Faller S, Formigoni M, Cruz M, Brasiliano S, et al. Psychometric properties of the sixth version of the addiction severity index (ASI-6) in Brazil. Rev psiquiatr Rio Gd Sul. 2007;29:335–6. doi: 10.1590/s1516-44462012000100006. [DOI] [PubMed] [Google Scholar]
- 12.Rudolph AE, Jones KC, Latkin C, Crawford ND, Fuller CM. The association between parental risk behaviors during childhood and having high risk networks in adulthood. Drug Alcohol Depend. 2011;118:437–43. doi: 10.1016/j.drugalcdep.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stanton MD, Todd TC, Heard DB, Kirschner S, Kleiman JI, Mowatt DT, et al. Heroin addiction as a family phenomenon: a new conceptual model. Am J Drug Alcohol Abuse. 1978;5:125–50. doi: 10.3109/00952997809027993. [DOI] [PubMed] [Google Scholar]
- 14.Basu D, Mattoo SK. Epidemiology of substance abuse in India: methodological issues and future perspectives. Indian J Psychiatry. 1999;41:145–53. [PMC free article] [PubMed] [Google Scholar]


