Abstract
Background & objectives:
Newly diagnosed HIV patients may be asymptomatic or present with a wide range of symptoms related to opportunistic infections, acute seroconversion illness or other medical illnesses. This study was designed to evaluate the socio-demographic parameters, spectrum of the presenting clinical conditions and concurrent immunological status of newly diagnosed HIV patients and document the WHO clinical stages at the time of HIV diagnosis.
Methods:
This cross-sectional, observational study was undertaken over a 12 month period at a tertiary referral hospital in eastern India. Three hundred sixty consecutive newly diagnosed HIV patients were selected for the study from the HIV clinic and medicine wards of this hospital. Demographic and clinical data and relevant laboratory investigations of the patients were recorded and analyzed.
Results:
Mean age of patients was 36.38 ± 10.62 yr, while 63.89 per cent were males. The main mode of transmission of HIV for males and females were unprotected exposure to commercial sex (139, 60.44%) and intercourse with HIV seropositive spouses (89, 68.46%), respectively. Fever (104, 28.89%), weight loss (103, 28.61%) and generalized weakness (80, 22.22%) were the predominant symptoms. Overall mean CD4 count was 176.04 ± 163.49 cells/μl (males 142.19 ± 139.33 cells/μl; females 235.92 ± 185.11 cells/μl). Overall, 224 opportunistic infections were documented in 160 patients, opportunistic diarrhoea (44, 12.22%) and pulmonary tuberculosis (39, 10.83%) being the commonest. There were 83 and 133 patients in WHO clinical stages 3 and 4, respectively; 291 (80.83%) patients were eligible for initiation of first-line antiretrovirals at presentation.
Interpretation & conclusions:
Advanced immunodeficiency and burden of opportunistic infections characterize newly diagnosed HIV patients in eastern India. The physicians should keep in mind that these patients may have more than one clinical condition at presentation.
Keywords: Human immunodeficiency virus (HIV), immunological profile, newly diagnosed, WHO clinical staging
Newly diagnosed human immunodeficiency virus (HIV) infected patients may be asymptomatic1, or they may present with a wide range of symptoms, including emergency conditions2. These may be related to opportunistic infections, acute seroconversion illness or other medical illnesses not specifically related to HIV. HIV-related causes account for many hospitalizations when patients are first diagnosed with HIV. Many of these HIV-related hospitalizations could have been prevented if patients were diagnosed early and linked to medical care.
More than a quarter of patients with HIV in the United States are diagnosed in hospital settings most often with advanced HIV related conditions3. In a large multicentric prospective study on the national HIV database in France4, nearly 20 per cent of the study population had an acquired immune deficiency syndrome (AIDS) defining illness at presentation, the most common of which was Pneumocystis jiroveci pneumonia (23.5%) followed by tuberculosis (17.7%). India bears a large burden of newly infected patients in a single country5. However, there are only a few studies documenting the socio-demographic, clinical, immunological and opportunistic infection-related profile of newly diagnosed HIV patients in India1. A prevalence study conducted amongst the serving members of the Indian Armed Forces in 2002 confirmed that pulmonary tuberculosis was the most prominent (67%) of all opportunistic infections present in people newly diagnosed with HIV1.
The National AIDS Control Organization (NACO), India factsheet of 2012 reports that while the national prevalence of HIV infection stands at 0.31 per cent, the annual death rate among all HIV-infected persons in the country is still 7.2 per cent6. To counter the inordinately high HIV-associated mortality rate, early diagnosis of HIV and early linkage to HIV-care have assumed a significant role. In this scenario, the present study was designed to study the socio-demographic parameters, the spectrum of the presenting clinical conditions and concurrent immunological status of newly diagnosed HIV patients in eastern part of India and document the WHO clinical stages at the time of HIV diagnosis.
Material & Methods
This cross-sectional, observational study was undertaken over a 12 month period from August 2011 to July 2012 at Medical College and Hospital, Kolkata, West Bengal, a tertiary referral hospital in Eastern India. The institutional ethical committee approved the protocol of this study. All newly diagnosed HIV patients attending the HIV clinic of this hospital and patients being diagnosed HIV positive after admission to the medicine department during the study period were selected for this study, subject to their fulfilling the definition of newly diagnosed HIV patient and the inclusion and exclusion criteria.
Individuals with a serologically proved diagnosis of HIV infection which prompted the current hospital attendance, or documented during the current hospital stay, were considered newly diagnosed HIV patients. Patients on highly active antiretroviral therapy (HAART), on prophylaxis for opportunistic infections, or treated for opportunistic infections at any point, after HIV detection, and those with concurrent diseases/therapies, unrelated to HIV/AIDS, which might alter the presentation of HIV-related illness were excluded.
A total of 2929 HIV positive patients were evaluated during the 12-month study period, of whom, 360 patients fulfilling the inclusion criteria were enrolled in this study (Fig. 1). These patients were interviewed at the HIV clinic or at the bedside in the Medicine inpatient wards after informed written consent was obtained from each of them. Using a pre-designed field tested questionnaire-cum-case record form, the socio-demographic parameters like age, gender, religion, place of residence, level of education, occupation, annual income, sexual orientation, marital status, spouse HIV status, offspring HIV status and mode of transmission of HIV were recorded, as were the presenting symptom(s) and anthropometric measurements like body weight, height and body mass index (BMI). For recording of mode of transmission of HIV, the patients were informed about the known routes of HIV transmission and were asked to identify which was the most probable route of HIV acquisition in them. In case a patient was unsure of his/her possible route of HIV acquisition, or refused to reveal sexual exposure history, or refused to reveal prior intravenous (iv) drug use, or refused to impart or could not recollect past medical, surgical or blood transfusion history, then that particular patient was designated as “Unknown” in possible mode of transmission (MOT). Medical records in the form of HIV clinic registers, outpatient department tickets and referral documents from antenatal clinics and private practitioners were also consulted. Relevant laboratory investigations were performed in accordance with the National AIDS Control Organization (NACO) guidelines7. The final diagnosis and organ system/s involved were recorded. CD4 cell count and absolute lymphocyte count (ALC) were recorded to evaluate immunological status of the patient. CD4 count was done using FACSCOUNT (Becton Dickson Biosciences, USA) machine using the peripheral venous blood sample. Clinical stage was determined according to the WHO guidelines on clinical staging of HIV/AIDS for adults and adolescents8.
Fig. 1.
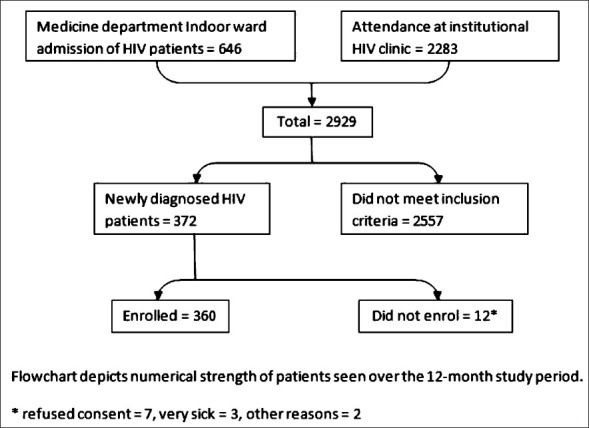
Flowchart depicting enrolment of patients in study.
Statistical analysis: Individual patient-wise information and records were transferred from the questionnaire-cum-case record forms to a predesigned Microsoft Office Excel worksheet. The data sheet was subjected to analysis by statistical software Epi Info 7 (Centre for Disease Control, Atlanta, USA). Descriptive statistical methods like percentage, ratio and proportion were used for categorical variables, and mean, median, standard deviation and percentiles were used for quantitative analysis. SPSS version 16 software (SPSS Inc., USA) was used to draw receiver operating characteristic (ROC) curve for ALC and CD4 counts, considering CD4 count < 200 cells. The optimal cut-off value for the ROC curve was estimated based on sensitivity and specificity and was calculated based on minimal distance (d) from coordinate (0,1) and any point on the ROC curve. The distance was calculated as d= √[(1-sensitivity2 +(1-specificity2. Scatter diagram was drawn and Pearson's correlation coefficient with 2-sided P value was calculated to depict the relationship between CD4 count and ALC.
Results
Three hundred and sixty (360) newly diagnosed HIV patients who fulfilled the inclusion criteria were included in this study. Of these, 146 patients (40.6%) were included from the HIV clinic during their first visit following HIV detection which did not prompt admission. The remaining 214 (59.4%) were enrolled from the Medicine wards, either admitted following their first visit to the HIV clinic or diagnosed as HIV positive following their admission.
The mean age of the patients was 36.38 ± 10.62 yr, while males comprised 63.89 per cent of the study population. The majority (229, 63.61%) of the patients were in the age group of 20-40 yr while 31.11 per cent were above 40 yr of age. Urban residents (219, 60.83%) and Hindus (287, 79.72%) dominated our study group. With regards to educational status, 85 (23.61%) were illiterate, 90 (25.00%) and 129 (35.83%) patients had attained primary and secondary level of education, respectively in contrast to the 56 who had attended high school.
Occupational data of the study subjects were classified in accordance with the International Standard Classification of Occupation (ISCO-08) published by the International Labour Organization9. The majority (144, 40.00%) were employed in elementary occupations like domestic, hotel and office cleaners and helpers, vehicle, window, laundry and other hand cleaning workers etc., followed by service workers, shop and market sales workers (71, 19.72%) and craft and related workers (64, 17.78%). More than 70 per cent of the newly diagnosed HIV patients had never migrated to other cities or regions for occupational, educational or other reasons; 40 (11.11%) patients had been migrants in the past, while 54 (15.00%) migrants.
The majority of the patients were heterosexual in their sexual preference; only six admitted to have homosexual preferences and practices. The marital status of the patients included in the study, as well as the spousal seroconcordance and discordance rates among the married sub-group and the prevalence of HIV infection in progeny were analysed (Table I).
Table I.
Marital status of patient population and HIV status of spouse and progeny
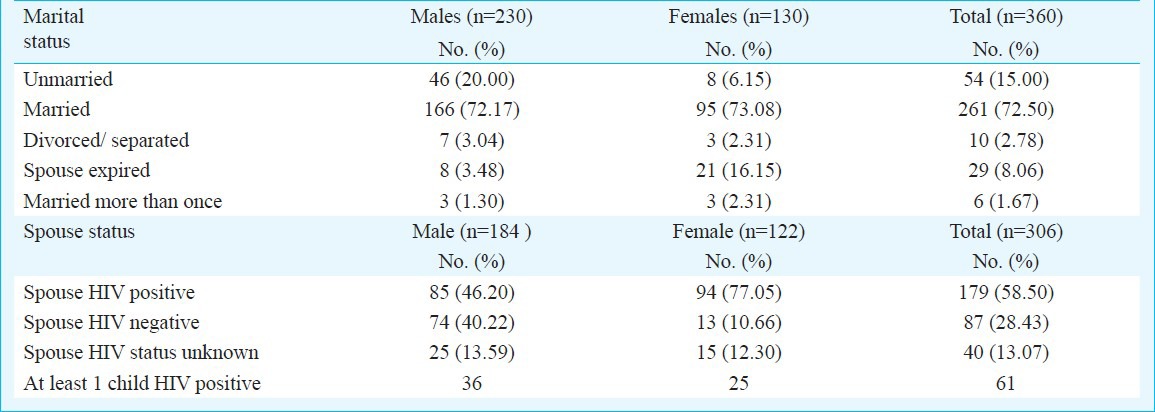
The predominant mode of transmission of HIV for both males and females was unprotected sexual intercourse [172/230 (74.78%) and 109/130, 83.85%, respectively]. Further analysis of the sexual route as a mode of transmission revealed that for males, unprotected exposure to commercial sex (139, 60.44%) was the commonest modality while female patients acquired their infection mostly from sexual intercourse with their HIV seropositive husbands (89, 68.46%); further details of the various modes of transmission and the mean CD4 counts associated with each route are shown in Table II.
Table II.
Possible modes of transmission (MOT) of HIV in study cohort (n= 360)
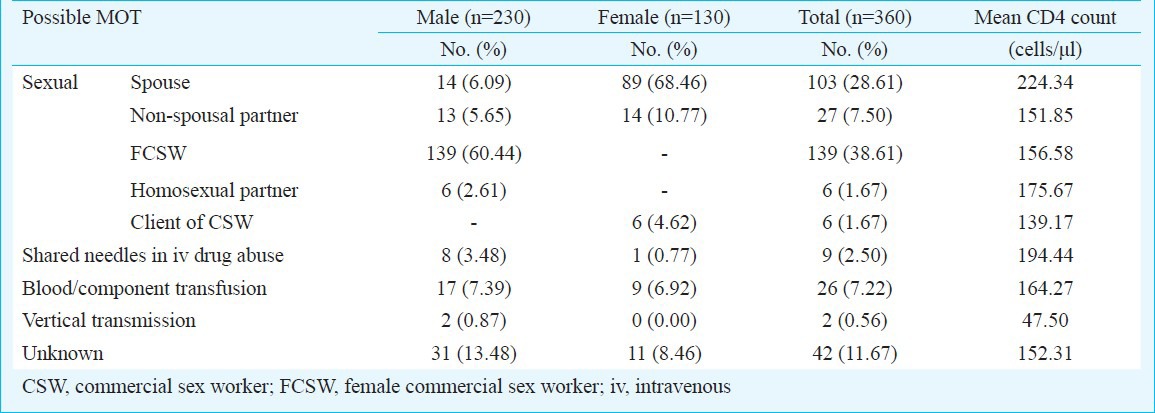
Clinical and immunological status: Fifty (13.89%) patients (males 25/230, 10.87%; females 25/130, 19.23%) were asymptomatic and had attended the HIV clinic after being diagnosed as HIV positive. HIV testing was conducted in these patients either voluntarily or as part of spouse counselling and testing under National AIDS Control Programme. In addition, 18 pregnant women were referred from various antenatal clinics after HIV diagnosis but did not have any symptoms of HIV related illnesses.
The presenting symptoms of the newly diagnosed HIV patients were analyzed on the basis of probable systemic involvement (Table III). Fever was the commonest (104, 28.89%) systemic, and overall symptom, followed closely by weight loss (103,28.61%), generalized weakness (80, 22.22%), diarrhoea (54, 15.00%) and cough (52, 14.44%).
Table III.
Organ system wise distribution of presenting symptoms of study population
Mean body weights were similar in both males and females (48.70 ± 9.08 vs. 49.28 ± 9.68 kg). Likewise, mean BMI was comparable across gender differences (17.90 ± 3.44 kg/ m2 for males vs. 19.71 ± 4.17 kg/m2 for females).
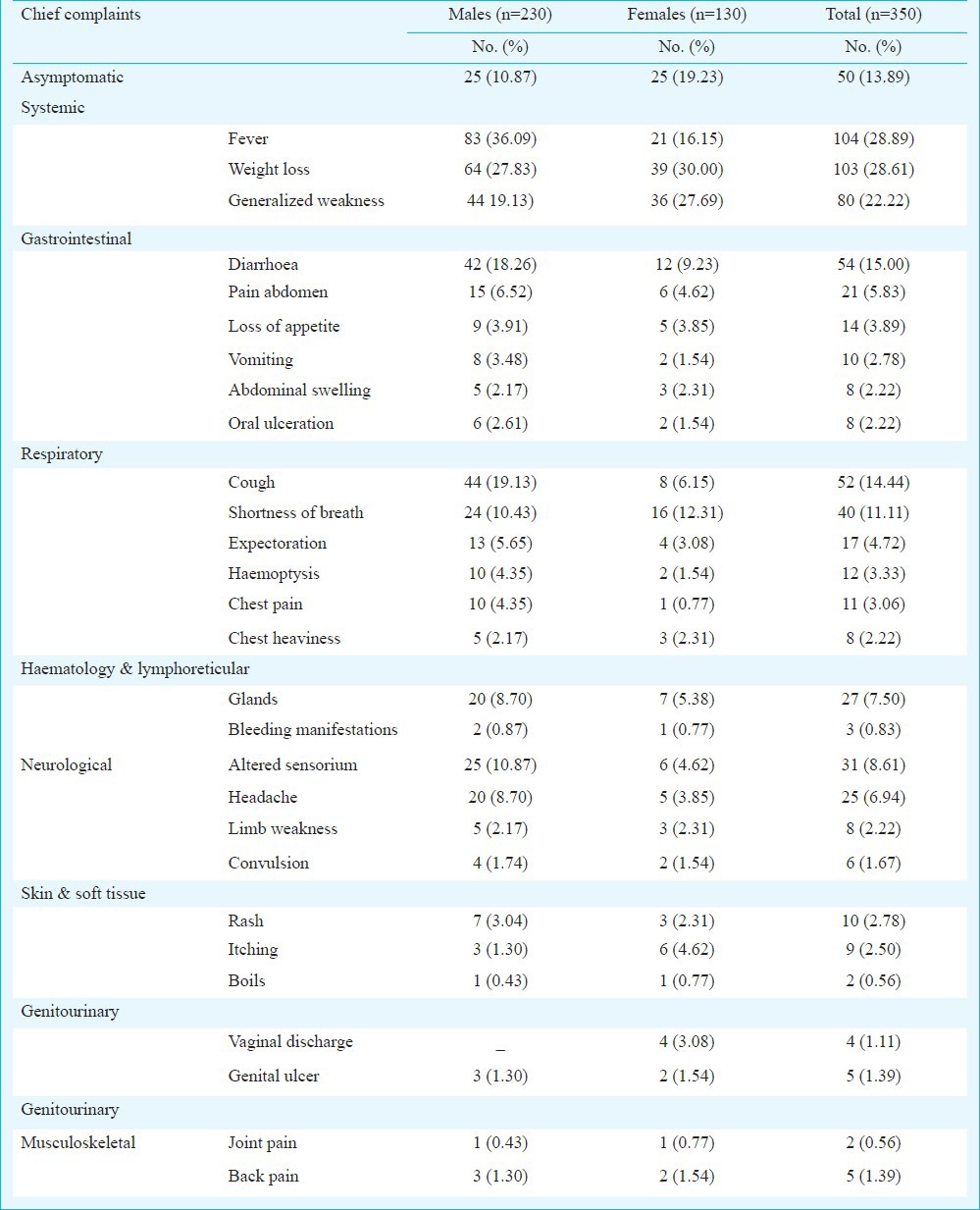
Among the immunological parameters studied, mean CD4 counts were significantly less in males (142.19 ± 139.33 cells/μl) than in females (235.92 ± 185.11 cells/μl) while the overall mean CD4 count was 176.04 ± 163.49 cells/μl). Absolute lymphocyte count (ALC) in males and females were 1485.27 ± 943.42 and 1953.58 ± 1224.23 cells/μl, respectively. Correlation analysis of ALC values with CD4 counts showed a Pearson's coefficient of 0.32, with a 2-sided P<0.05. Further analysis of CD4 counts after stratification revealed that a majority of patients (168, 46.67%) had CD4 counts less than 100 cells/μl at presentation, while only 23 (6.39%) presented at the opposite end of the spectrum with CD4 counts greater than 500 cells/ μl (Table IV). The ROC curve (Fig. 2) was plotted to determine the sensitivities and specificities of various ALC cut-off values to detect a CD4 count < 200 cells/ μl. As revealed from area under the curve of 0.31, ALC was not found well suited as a surrogate marker for CD4 count in the present setting.
Table IV.
Distribution of patient population across ranges of CD4 counts and immunodeficiency. Stratification of immunodeficiency according to revised WHO guidelines for clinical staging and immunological classification of HIV, 200614
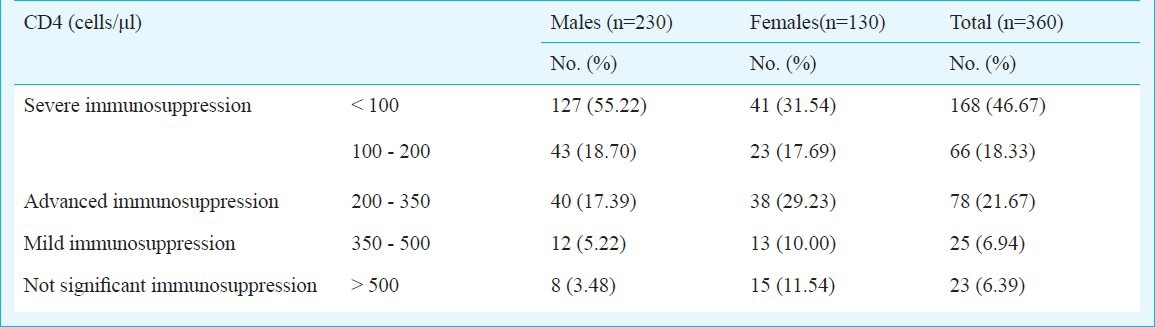
Fig. 2.
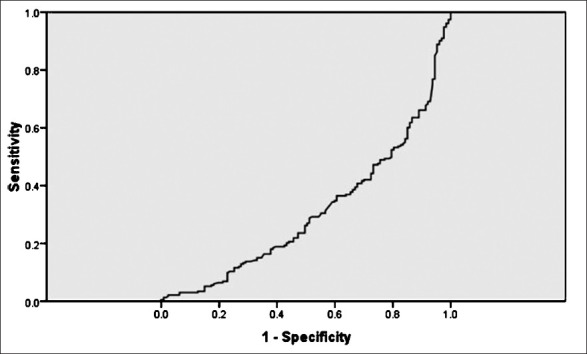
ROC curve depicting the sensitivities and specificities of various ALC cut-off values to detect a CD4 count < 200 cells/μl.
Analysis of clinical diagnoses was performed on the basis of organ system involvement. The various diagnoses reached in newly diagnosed HIV patients are shown in Table V, along with the mean CD4 count for each diagnosis. Overall, 224 opportunistic infections were documented in 160 patients in the study, 64 patients having dual opportunistic infection.
Table V.
List of major diagnoses reached in newly diagnosed HIV patients (n=360), and their frequencies and mean CD4 counts
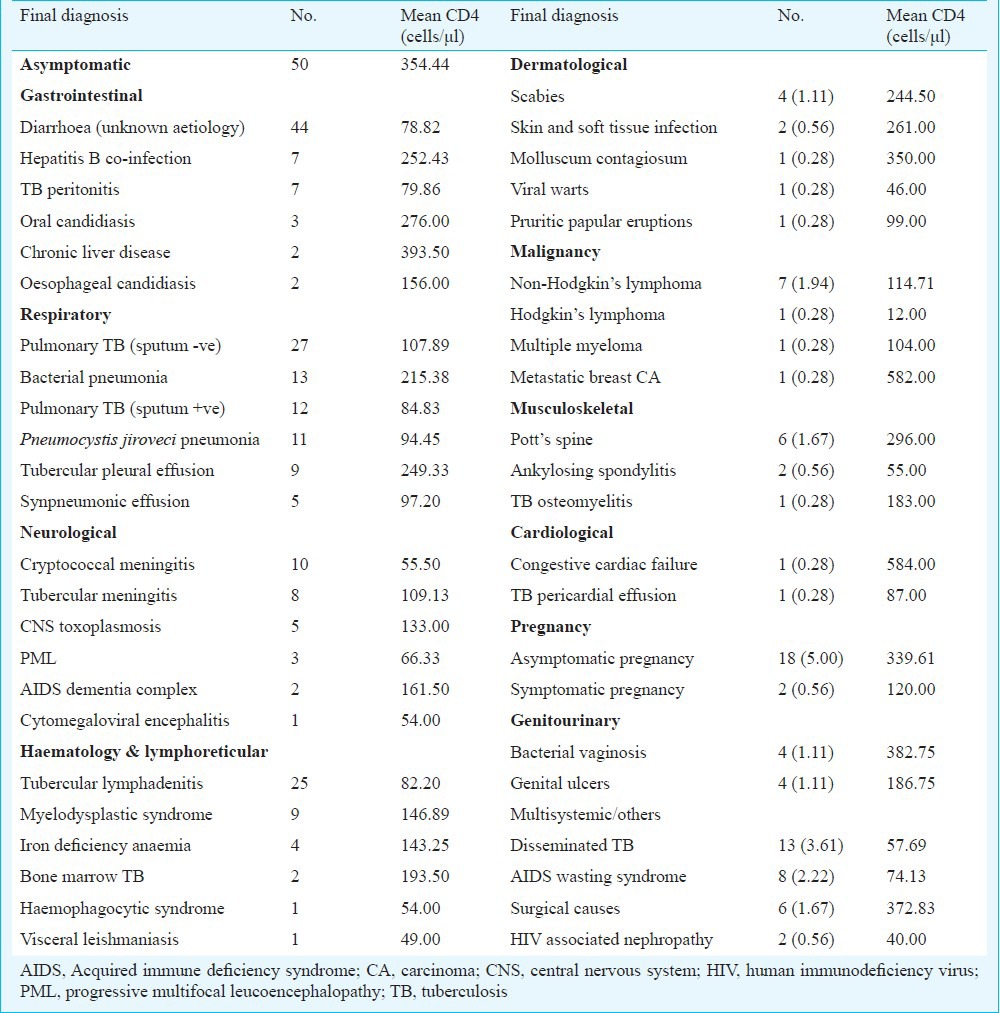
WHO clinical staging and need for HAART initiation: Maximum number of patients (133, 36.94%) were in WHO clinical stage 4 while 83, 47 and 78 patients were in stages 3, 2 and 1, respectively. Nineteen (5.28%) patients could not be stratified according to the existing classification and were grouped as “Unclassified”. Predictably, mean CD4 counts showed a decline across the WHO clinical stages; patients in WHO stage 4 had a mean CD4 of 106.25 ± 102.69 cells/μl while those in stage 1 had mean CD4 of 338.83 ± 182.34 cells/μl.
Two hundred and ninety one (80.83%) patients were eligible for initiation of first-line antiretroviral therapy in accordance with their clinical staging and CD4 counts at the time of diagnosis. Sixteen (32.00%) of the 50 asymptomatic patients who qualified for HAART in accordance with NACO guidelines7 had a mean CD4 count of 194.06 ± 72.60 cells/μl compared to the remaining 34 asymptomatic patients who had a mean CD4 of 416.68 ± 138.85 cells/μl.
Pregnant patients, co-infection with HBV or HCV, HIV associated malignancies: Of the 20 pregnant women who had been diagnosed HIV positive during routine antenatal testing, 18 (90.00%) were asymptomatic. Eleven were in their 2nd trimester of pregnancy while seven were diagnosed early in their 1st trimester. Eleven cases of HIV- HBV co-infection were detected, along with five patients coinfected with hepatitis C virus. Of these 16 patients, two presented with decompensated cirrhosis of liver (1 each with HIV- HBV and HIV- HCV co-infection). Seven patients presented with HIV associated non-Hodgkin's lymphoma, which is an AIDS-defining diagnosis; the mean CD4 count at presentation for these patients was 114.71 cells/μl.
Discussion
Most studies conducted on newly diagnosed HIV patients have been based on national HIV databases or nation-wide network of HIV clinics, typically including 1000 to 6000 patients4,10. However, this present study was conducted at a single tertiary care hospital and enrolled only 360 newly diagnosed HIV patients.
In a large multicentric analysis carried out in France, a majority of the subjects (67.8%) were below the age of 40 years compared to a similar 68.89 per cent in our study3. Data from a 2003 nationwide case review in United Kingdom and Ireland have shown a male: female ratio of 1.24 : 1 while the National Family Health Survey- 3 (NFHS-3) from India reports that only 3 per cent of all Indian women have ever been tested for HIV10,11. It is reflected in the higher male: female ratio of 1.78 : 1 in our study.
Only 11.39 per cen of our patients had received high-school education vis-a-vis 27 per cent of study population in a prospective observational cohort study from Texas, USA3. In a South African study, the rates of HIV seroconcordance and serodiscordance among sex partners were 31.37 and 68.73 per cent, respectively12. Our study showed 58.5 per cent seroconcordance and 28.43 per cent serodiscordance among married couples. NFHS-3 attributes this to late diagnosis of HIV, reluctance to use condoms and non-disclosure of HIV status to spouse, and indicates the need for more comprehensive and family oriented HIV testing11.
Earlier studies from the United Kingdom and France revealed homosexual practices in 29-33 per cent of study subjects, in contrast to 1.67 per cent in our study4,10. Delpierre and co-workers4 reported an estimated 47 per cent of patients having acquired HIV through heterosexual transmission whereas in our study 76.39 per cent of HIV transmission was found to be due to unprotected heterosexual intercourse. This is in agreement with the 2011-2012 report from the National AIDS Control Organization, India, where 88.2 per cent of HIV positive persons had heterosexual route of transmission13.
In a prospective audit of HIV status of children of HIV positive mothers living in UK, only 6.92 per cent children studied were HIV positive14. In contrast, nearly 20 per cent of the married patients in our study had at least HIV positive one child, underscoring the need for country-wide adoption of more stringent policies to prevent parent-to-child-transmission.
The predominant diagnosis (52.0 to 96.7% patients) in a few Indian studies on newly diagnosed HIV patients has been pulmonary or extra-pulmonary tuberculosis1,15. Tuberculosis was also the predominant opportunistic condition in our study, accounting for 31.39 per cent cases. Diarrhoeal diseases and Pneumocystis carinii pneumonia were not reported to be important in other similar studies4,10.
CD4 counts have long been deemed as a marker of cell mediated immune function16. In a 6-year long study on the CD4 counts of newly diagnosed HIV patients in England and Wales, Gupta and colleagues17 documented more than 50 per cent of patients having CD4 counts less than 350 cells/μl17. Our data revealed that 86.67 per cent of patients had CD4 counts less than 350 cells/μl, while a further 65 per cent had an initial CD4 count less than 200 cells/μl. According to WHO guidelines for immunological classification of HIV,7 this translates into the fact that a majority of the HIV patients in the present setting have advanced or severe immunosuppression at the time of diagnosis.
Absolute lymphocyte counts in HIV patients have been shown to correlate strongly with their CD4 counts in various studies18,19. It has also been suggested that ALC can be used as a surrogate marker of CD4 count in resource restricted settings20. In the present study, ROC curve was drawn considering CD4 count of 200/μl as the cut-off. The area under the curve was 0.31 and ALC values were not found to be a suitable marker for immunodeficiency in the present setting. Optimal cut-off value was estimated based on sensitivity and specificity and other criteria like cost of investigation, cost of consequences of test results were not considered.
CDC guidelines define AIDS as stage 3 HIV infection, with CD4 < 200 cells/μl or documentation of an AIDS defining condition21. Analysis of European data reveals only 14.7-15 per cent of patients having AIDS at the time of diagnosis while in our study, this figure was 71.94 per cent. The British study9 also reported 59.1 per cent of their patients to be asymptomatic at the time of diagnosis, whereas in our experience, only 21.67 per cent patients were asymptomatic at presentation.
Out study had certain or limitations. Being a single centre study from a referral centre, the data from this study might not accurately reflect data from across the nation or region. Further, HIV viral loads were not estimated in newly detected HIV patients in keeping with national protocols.
In conclusion, our results show that lower educational levels, unemployment and unsafe sexual practices are the major risk factors for the acquisition of HIV in India. Majority of the initial presentations of HIV were common symptoms that require specific awareness on the part of the physicians to suspect HIV disease. On the other hand, a significant fraction of patients presented with advanced immunodeficiency, and the compounding burden of opportunistic infections should be of concern to health care planners and providers. Physicians in India should remember that more than one clinical condition may often coexist in newly diagnosed HIV cases in order to provide comprehensive HIV care.
References
- 1.Sawhney MP, Sharma YK, Sayal SK. Mode of detection of HIV infection - A retrospective study of 612 cases. Med J Armed Forces India. 2005;61:220–3. doi: 10.1016/S0377-1237(05)80157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rewari BB, Tanwar S. Emergencies in HIV medicine. J Indian Med Assoc. 2009;107:317–22. [PubMed] [Google Scholar]
- 3.Shahani L, Hartman C, Troisi C, Kapadia A, Giordano TP. Causes of hospitalization and percieved access to care among persons newly diagnosed with HIV infection: Implications for HIV testing programs. AIDS Patient Care STDs. 2012;26:81–6. doi: 10.1089/apc.2011.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delpierre C, Lauwers-Cances V, Pugliese P, Poizot-Martin I, Billand E, Duviver C, et al. Characteristics trends, mortality and morbidity in persons newly diagnosed HIV positive during the last decade: the profile of new HIVdiagnosed people. Eur J Public Health. 2008;18:345–7. doi: 10.1093/eurpub/ckm117. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. New Delhi: World Health Organization, Regional Office for South-East Asia; 2012. HIV/AIDS in the South-East Asia Region Progress Report, 2011. [Google Scholar]
- 6.National AIDS Control Organization (NACO) New Delhi: NACO; 2007. Antiretroviral therapy guidelines for HIV-infected adults and adolescents including post-exposure prophylaxis. [Google Scholar]
- 7.World Health Organization. Geneva: WHO; 2006. Revised WHO clinical staging and immunological classification of HIV and case definition of HIV for surveillance. [Google Scholar]
- 8.International Labour Organization. I. Geneva: International Labour office; 2012. International standard classification of occupations 2008 (ISCO-08): Structure, group definitions and correspondence tables. [Google Scholar]
- 9.Sullivan AK, Curtis H, Sabin CA, Johnson MA. Newly diagnosed HIV infections: review in UK and Ireland. BMJ. 2005;330:1301–2. doi: 10.1136/bmj.38398.590602.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Family Health Survey (NFHS-3), 2005-06: India. I. Mumbai: IIPS; 2007. International Institute for Population Science (IIPS) and Macro International. [Google Scholar]
- 11.Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett GP, Sweat MD, et al. Who infects whom? HIV-1 concordance and discordance among migrant and non-migrant couples in South Africa. AIDS. 2003;17:2245–52. doi: 10.1097/00002030-200310170-00013. [DOI] [PubMed] [Google Scholar]
- 12.National AIDS Control Organization. New Delhi: NACO; 2012. Annual report 2011-12. [Google Scholar]
- 13.Eisenhut M, Sharma V, Kawsar M, Balachandran T. Knowledge of their children's HIV status in HIV-positive mothers attending a genitourinary medicine clinic in the UK. HIV Med. 2008;9:257–9. doi: 10.1111/j.1468-1293.2008.00556.x. [DOI] [PubMed] [Google Scholar]
- 14.Jain MK, John TJ, Keusch GT. A review of human immunodeficiency virus infection in India. J Acquir Immune Defic Syndr. 1994;7:1185–94. [PubMed] [Google Scholar]
- 15.Tsunemi S, Iwasaki T, Imado T, Higasa S, Kakishita E, Shirasaka T, et al. Relationship of CD4+ CD25+ regulatory T cells to immune status in HIV-infected patients. AIDS. 2005;19:879–86. doi: 10.1097/01.aids.0000171401.23243.56. [DOI] [PubMed] [Google Scholar]
- 16.Gupta SB, Gilbert RL, Brady AR, Livingstone SJ, Evans BG. CD4 cell counts in adults with newly diagnosed HIV infection: results of surveillance in England and Wales, 1990-1998. CD4 Surveillance Scheme Advisory Group. AIDS. 2000;14:853–61. doi: 10.1097/00002030-200005050-00012. [DOI] [PubMed] [Google Scholar]
- 17.Anastos K, Shi Q, French AL, Levine AL, Greenblatt RM, Williams C, et al. Total lymphocyte count, hemoglobin, and delayed-type hypersensitivity as predictors of death and AIDS illness in HIV-1-infected women receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2004;35:383–92. doi: 10.1097/00126334-200404010-00008. [DOI] [PubMed] [Google Scholar]
- 18.Bedell R, Heath KV, Hogg RS, Wood E, Press N, Yip B, et al. Total lymphocyte count as a possible surrogate of CD4 cell count to prioritize eligibility for antiretroviral therapy among HIV-infected individuals in resource-limited settings. Antivir Ther. 2003;8:379–84. [PubMed] [Google Scholar]
- 19.Jacobson MA, Liu L, Khayam-Bashi H, Deeks SG, Hecht FM, Kahn J. Absolute or total lymphocyte count as a marker for the CD4 T lymphocyte criterion for initiating antiretroviral therapy. AIDS. 2003;17:917–9. doi: 10.1097/00002030-200304110-00019. [DOI] [PubMed] [Google Scholar]
- 20.Schneider E, Whitmore S, Glynn KM, Dominguez K, Mitsch A, McKenna MT. Centers for Disease Control and Prevention (CDC). Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years - United States, 2008. MMWR Morb Mortal Wkly Rep. 2008;57:1–8. [PubMed] [Google Scholar]


