Abstract
Introduction:
Tuberculosis is an infectious disease caused by Mycobacterium Tuberculosis complex. It is one of the most common infectious diseases largely resulting from the patient's lifestyle. The purpose of the present study is to investigate factors related with adopting health behaviors by patients with tuberculosis based on the health belief model.
Materials and Methods:
The present cross-sectional study was performed on 196 patients with tuberculosis. Data was collected using a 47-item, self-designed, questionnaire. Cronbach's alpha was calculated as 73.9. The Pearson test was used to study the correlation between independent variables and adopting a healthy behavior.
Results:
The mean score for adopting healthy behaviors by patients was 87.52 ± 13.8. The Pearson correlation test indicated a statistically significant relation between adopting healthy behaviors and scores of knowledge (P < 0.001, r = 0.536), perceived susceptibility (P < 0.001, r = 0.36), perceived benefits (P < 0.001, r = 0.347), and perceived barriers (P = 0.046, r = 0.143).
Conclusion:
Direct relationship was found between adoptinga healthy behavior and scores of knowledge, perceived susceptibility, and perceived benefit. Although the results of this study can be the basis of educational interventions, any generalizations should be performed cautiously.
Keywords: Healthy behavior, health belief model, tuberculosis patients
INTRODUCTION
Tuberculosis is a chronic infectious disease which is still a global health problem. In humans it is caused by the Mycobacterium Tuberculosis complex and in most cases is caused by Mycobacterium Tuberculosis.[1,2] Tuberculosis attacks the lungs, and in one-third of the cases, other organs of the body are involved.[3] Approximately one-third of the population of the world is infected with Mycobacterium Tuberculosis.[4] Tuberculosis is the leading cause of mortality in the world, with two million death reports in developing countries.[5,6] The geographical location of Iran and its neighborhood, with some countries having a high prevalence of tuberculosis, require our considerable attention to this disease.[7] Epidemiological data, in 2010, showed that about 13.7 million people in the world were infected with tuberculosis, of whom more than 80% belonged to 22 developing countries. Each year, about 1.8 million people die of tuberculosis.[8,9] The above-mentioned report stated that the number of people infected with tuberculosis in 2009, in Iran, was 10099. Tuberculosis is the deadliest infectious disease among women of reproductive age. As most affected women in the reproductive age are almost always young, the highest number of orphans resulting from a disease is associated with tuberculosis. Tuberculosis, more than any other disease, leads to loss of income and disruption of family.[10] In terms of frequency of the global burden of disease and the rank among diseases, tuberculosis ranks 10, and it is predicted that in 2020, it will reach rank 7 of the global burden of disease, based on Disability Adjusted Life Years (DALY). This occurs when most of the infectious diseases decrease to lower ranks in this frequency and priority.[9,11] The increase of acquired immune deficiency syndrome (AIDS) and tuberculosis, resistant to treatment, has increased the occurrence of tuberculosis disease in recent years, in different countries. Due to this fact, in 1993, tuberculosis was introduced by the World Health Organization (WHO) as a global emergency disease.[12] Directly Observed Treatment Short-course (DOTS) is the strategy recommended by the WHO for controlling tuberculosis.[13] Although this strategy reduces the mortality rate of tuberculosis, this disease is the reason for deaths that can be prevented.[14] Successful performance of DOTS in fighting against tuberculosis requires the collaboration of all sections giving health-clinical services including clinical health networks, hospitals, university centers, and private physicians.[15] The lack of compliance in using drugs by patients is one of the problems and its investigation in some diseases such as tuberculosis is of great importance, due to its contagious nature.[16] Tuberculosis can be treated, but as it requires long treatment despite other infectious diseases, completion of the treatment period by the patient is of great importance.[17] The studies showed that the behavior condition of tuberculosis patients is one of the most important factors in controlling tuberculosis. For example, Taqizadeh et al., in their study on the status and attitude of patients with pulmonary tuberculosis to treatment, susceptibility, and perceived benefits, in a group that did not follow the treatment were low.[18] In a study conducted by Rahbar et al., in the Taleqani Hospital of Orumieh city, it was defined that diet was directly associated with the education level, self-confidence, living in the city, and receiving previous education.[17] The study conducted by Janakan et al. on smear- positive patients, in Sri Lanka, indicated that susceptibility and benefit scores in the group that did not observe the treatment, were low.[19] Generally, the researches, including Jahani et al., Pishkar et al., and Clark et al., emphasized on the relationship between an individual attitude to treatment and adherence to treatment.[20,21,22]
Behavior change is a complex process.[23] As human behavior is a reflection of different factors, recognizing this causative network is important to influence the effective factors of behavior; for many years, behavior specialists have been pursuing it. Thus, true identification of the factors related to tuberculosis, based on the theory, can be useful in improving the conditions for treatment of patients with tuberculosis. Various approaches and theories are considered to investigate this phenomenon and one of these approaches is the health belief model. This model is one of the social psychological models that are used to understand health behavior. The health belief model is the first behavior change model and is accepted widely in empirical applications.[24]
MATERIALS AND METHODS
The present cross-sectional study was performed on 196 patients with pulmonary tuberculosis in Isfahan, for a period of six months. Data was collected using a 47-item and nine-section, self-designed questionnaire, which included personal data, knowledge (six items) (e.g. drug use duration in patients with tuberculosis), perceived susceptibility (four items) (e.g., Family members of patients with tuberculosis are susceptible to the disease), perceived severity (five items) (e.g. in case of lack of a good treatment, tuberculosis can kill a person), perceived benefits (six items) (e.g. Free drugs in clinical centers), perceived barriers (four items) (e.g., yellow color of the eyes due to drug use), self-efficacy (four items) (e.g. assurance by the patient of doing experiments inthe second, fourth, and sixth month), guidance of action (three items) (e.g. Getting information from health staff), and functional questions (nine items) (e.g., using drugs regularly). Scoring in knowledge questions were marked thus: In case of a correct response, they got one point, and in case of incorrect answers a zero was given to them. Responding to perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and guidance for action questions, which were in multi-choice form, was by some choices, such as, completely agree (score 3), agree (score 2), disagree (score 1), and strongly disagree (zero score). The subjects would select one of the choices that was close to their personal idea. The score that the patients received for perceived susceptibility, perceived barriers, and self-efficacy questions was between 0 and 12. The received score of perceived severity was (0-15), perceived benefits (0-18), and guidance for actions questions score (0-9). Responding function questions were Yes (score 1) and No (score 0) and the received score for this part was (0-9). The reliability of the questionnaire in a 30-person sample was 73.9, with Cronbach's alpha of 62.7 for guidance of action and 80.4 for perceived benefit structure. For easy comparison, the structure scores were calculated out of 100. After data collection, the data were entered in an SPSS 18 software and were analyzed by statistical tests.
RESULTS
In this study, 196 patients with pulmonary tuberculosis, under the supervision of the Clinical Health Centers of Isfahan, were investigated. The patients were with an age average of 52.23 (SD of 23.62), 48% of the patients were women and 52% of the patients were men; 19.9% of the patients were under the supervision of the clinical rural centers of Isfahan province and 80.1% of the patients were under the supervision of the clinical urban centers of the Isfahan province [Table 1].
Table 1.
Frequency distribution of patients with pulmonary tuberculosis based on nationality and clinical center under the supervision of Isfahan province
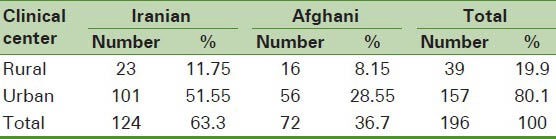
The findings of Table 1 show that 11.75% of the Iranian patients are under the supervision of health-clinical centers of the village and 51.55% are under the supervision of health-clinical centers of the city. Among Afghani people, 11.75% were under the supervision of the health-clinical center of the village and 8.15% were under the supervision of the urban clinical-health centers.
The average score received by the patients of the health belief model variables is shown in Table 2.
Table 2.
Average and standard deviation scores of patients with pulmonary tuberculosis based on predictive and outcome variables-Isfahan province
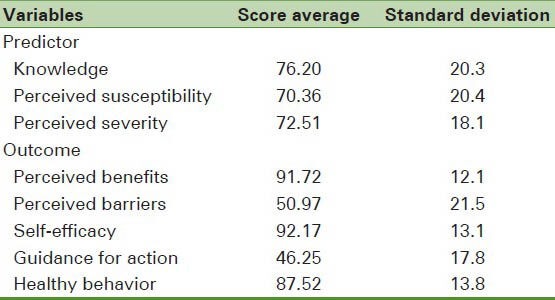
As shown in Table 2, the outcome variable in the current study is adopting a healthy behavior, and perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy, and guidance for action are predictive variables to take behavior.
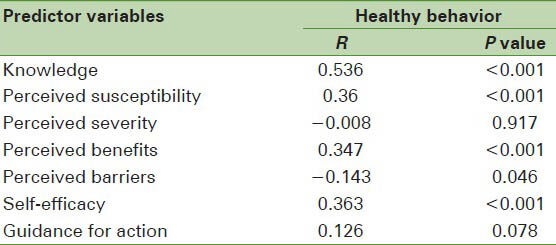
The results of the Pearson test in Table 3 show that there is a significant association between all variables of the health belief model, except perceived severity and guidance for action, with adopting healthy behaviors. The results of the analysis show that the highest direct relation between knowledge and adopting healthy behaviors, with the correlation coefficient of 0.536, and the lowest relation, is between the perceived benefits and adopting healthy behaviors with a correlation coefficient of 0.347.
Table 3.
Correlation scores between predictor variables and considering healthy behavior
DISCUSSION
The problems in tuberculosis management are protecting patients during the treatment cycle and completion of the treatment period. Negative outcomes of not adhering to the treatment are extensive. Thus, recognizing the factors related to the treatment-adherence behavior of the patients is an important issue in the reduction of some outcomes, such as, drug resistance and reduction of re-treatment costs.
The purpose of the current study was to determine the factors related to adopting healthy behaviors by tuberculosis patients, based on the health belief model (healthy behavior in this study is patient adherence to treatment for a period of six months). It is with reference to the knowledge of the patient to tuberculosis and illness treatment, and according to the current study findings, the average and standard deviation of the score of the patients’ knowledge was 76.20 ± 20.3. In the current study, most of the patients had a low knowledge of the disease symptoms. Also, the results of the study showed that there was a significant difference between the knowledge score that patients attained and healthy behavior (r = 0.536, P < 0.001), and the above results were expected. Niknami et al. stated that the patients’ education and their knowledge of the nature of disease and tuberculosis treatment increased their understanding and intake of their treatment diet.[15] The study conducted by Tornee et al., in Bangkok, proved the results of the current study; in their study, there was a significant association between knowledge and screening test, as healthy behavior in tuberculosis patients was less than 1/1000.[25] Also, another study that was carried out by Jankan et al., in Sri Lanka, found a direct significant association between knowledge and treatment adherence in the patients.[19] In a study conducted by Clark et al., in Turkey, and in the study conducted by Jahani et al., in Ahvaz city, the patients with a better knowledge or adequate education about the disease and treatment, showed better adherence.[20,21] However, the study conducted by Mweemba et al., did not show any significant association between knowledge and treatment adherence.[26]
Perceived susceptibility is a structure that is called mental perception of the patient, with regard to the danger that is caused in case of not completing the six-month treatment. The average and standard deviation of the received score of the patients was 74.36 ± 20.4, which had direct correlation with the adopting healthy behavior outcome, at a level less than 1/1000, which was in line with the results of Tornee et al.'s study.[25] However, the study of Jankan et al., in Sri Lanka, did not show a significant association between the perceived susceptibility and healthy behavior (19). Also, the study conducted by Taqizadeh et al., was not in line with the results of our study.[18] The perceived severity variable included some feelings that were about considering the seriousness of the outcomes in case of not completing the treatment by the patient, which includedevaluation of the medical and clinical outcomes. The mean and standard deviation of the perceived severity was 72.51 ± 81. The results of the test didnot report a significant association between the perceived severity score and healthy behavior (r = −0.008). The result was not in line with the assumptions of the study.
Probably it was due to the immediate outcome of the treatment that the patients-felt better and the symptoms were reduced considerably after a short time of treatment. The results of the other studies were not in line with the results of the current study. As per the study conducted by Taqhizadeh et al., it reported the above-mentioned relationship as being significant.[18] Also, the studies carried out by Tornee et al. and Jankan et al. reported an association between the perceived severity variable and adopting healthy behavior.[19,25] The observed differences in the results of the studies could be due to the type of study (that is based on cross-section results) and the data collection method.
The exact determination of the prediction of perceived severity of objective behavior requires long-term studies. The perceived benefits variable refers to the reality that human beings are inclined to carry outsome behaviors that have the maximum benefits for them. In the current study, the mentioned benefits are mostly emphasizing on receiving free drugs and experiments, and the mean and standard deviation of the score of patients of perceived benefits variable was 91.72 ± 12.1. Correlation analysis results showed that there was a significant association between the perceived benefits of the patients and adopting healthy behaviors (r = 0.347, P < 0.001) and the above-mentioned results were in line with the results of Taqizadeh et al. studies.[18] Also, Jankan et al. and Tornee et al. reported similar results.[19,25] The study of McDonnell et al. found the usefulness of the treatment with adherence to the drug diet.[27] The above-mentioned studies introduced that a good relationship of the health staff with the patients and easy access to good clinical facilities helps to improve the treatment adherence level.[19,25,27] In these behaviors, if no condition is provided, there is no barrier for the behavior, despite the shortage of facilities; a person is less inclined to use the behavior. In the current study, the barriers of treatment adherence were evaluated by perceived barriers, questions and mostly drug side effects and long treatment duration were mentioned, and the studied sample achieved a mean and standard deviation score of 50.97 ± 21.5 for perceived barriers, and the results showed that there was a reverse relationship between the perceived barriers variable and adopting healthy behaviors (r = −0.143, P = 0.046). The studies conducted by Tornee et al. proved the result of the study.[23] However, Taqizadeh et al. reported different results.[18] The studies of Jankan et al., did not state a significant relationship between the perceived barriers and healthy behavior.[19] The probable reason for this contradiction with the results of the research can be heterogeneity of the research population, such that, in our study the investigated samples were urban and rural patients. In the study conducted by Taqizadeh et al., only urban patients were investigated. In the study of Jankan et al., the cultural and social differences were effective on a different perception of patients’ barriers.
Guidance for action were factors that prepared for active behavior change. In the current study, the mean and standard deviation for guidance of action of the patients was 46.25 ± 17.8 and did not have significant relationship with healthy behavior (r = 0.126, P = 0.078). Other studies were in line with our study. The study of Tornee et al. did not report this relationship.[19]
The general result of the current study, based on the health belief model, showed that attitude factors could determine the healthy behavior of the patients well, such that, by increasing the positive attitude, healthy behaviors in patients showed positive changes and this result was expected. The study conducted by Jahani et al. reported a significant relationship between patients’ attitude and adherence to orders quality.[21] The results of the studies by Mweemba et al. and Clark et al. showed similar results.[24,26] The study conducted by Pishkar et al. reported that the relationship between the attitude of patients and compliancewas significant. Patients who observed many things in using the drugs and eliminating mucus had the highest performance, they also had high attitude scores.[22] The structures related to healthy behaviors were highly associated with knowledge, perceived susceptibility, and perceived benefits. The perceived barrier structure was inversely related to healthy behavior, and perceived severity structures and guidance for action were not related to healthy behavior.
Recommendations
The results are related to the investigating sample and generalizing these results to other populations requires conducting other studies. The current study can be the basis of future educational interventions. This study has taken into consideration self-efficacy as a variable determining healthy behavior, which is not considered in other similar studies. In this study, to evaluate healthy behavior, self-reporting was used. Thus, the limitations of such a method should be considered. One of the proposed methods for the reduction of self-report limitations is a long-term study, which allows the observation of the outcome behavior possible for the researcher.
The current study is based on an approved thesis from the Medical Sciences of Isfahan University.
ACKNOWLEDGMENT
The authors’ gratitude goes to the kind collaboration of the staff of the Disease Control Units of the Health Networks of the Isfahan Province and the tuberculosis patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Mirhaghani L, Nasehi M. Tehran: Seda; 2002. The guideline of tuberculosis prevention. [Google Scholar]
- 2.Sofian M, Zarinfar N, Mirzaee M, Moosavinejad A. Epidemiology of tuberculosis in Arak, Iran. Koomesh. J Semnan Univ Med Sci. 2009;10:261–6. [Google Scholar]
- 3.James ST. Philadelphia: Versa Press; 2000. Expert guide to infectious disease. [Google Scholar]
- 4.Asgari M, Davoodian P, Dadvand H. Prisoners knowledge about clinical signs and the way of pulmonary tuberculosis transferring in the central jail of Hormozgan province. Presented at the 17 th National congress of Tuberculosis. 2003 [Google Scholar]
- 5.Seraj SR, Ghafarpassand F, Afshari A, Ekrahi M. persented at the 16th Iranian Congress on Infectious Disease and Tropical medicine. Tehran: 2007. Study of chest radiogeraphy in active tuberculosis patients admitted in Shiraz educational hospital. [Google Scholar]
- 6.Salehi H. Frequency of mycobacterium tuberculosis infection in weaving workers in Isfahan. J Isfahan Med Univ. 2006;95:24–6. [Google Scholar]
- 7.Tuberculosis. bulletin of the national TB day. Center for Diseases Control (CDC), Iranian Ministry of Health and Medical Education. 2004 [Google Scholar]
- 8.Young DB, Perkins MD, Duncan K, Barry CE., III confornting the Scientific obstacles to global control of tuberculosis. J Clin Invest. 2008;118:1255–65. doi: 10.1172/JCI34614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.A report of status of tuberculos is in the world and Iran. 2010. Available from: http://www.cdc.hbi.ir .
- 10.WHO; 2003. WHO report on TB epidemic. [Google Scholar]
- 11.Crofton J, Horne N, Miller F. London: Macmillan; 2001. Clinical tuberculosis. [Google Scholar]
- 12.Azizi F, Janghorbani M, Hatami H. Epidemiology and control of common disorders in Iran. 2009 [Google Scholar]
- 13.WHO. An expanded DOTS framework for effective tuberculosis control. WHO/CDS/TB/2002297. 2002. Available from: http://whqlibdoc.who.int/hq/2002/WHO_CDS_TB_2002297.pdf . [PubMed]
- 14.WHO. TB/HIV: Aclinicalmanual. 2004. Available from: http://whqlibdoc.who.int/publications/2004/9241546344.pdf .
- 15.Education needs of patients with pulmonary tuberculosis admitted to Taleghani Hospital in Urmia to comply with treatment regimen. 19th National Congress of Tuberculosis. 2008 [Google Scholar]
- 16.Sterling TR, Lehmann HP, Frieden TR. Impact of DOTS compared with DOTS-plus on multidrug resistant tuberculosis deaths: Decision analysis. BMJ. 2003;326:574. doi: 10.1136/bmj.326.7389.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niknami SH, Taheri Aziz M, Mohraz M. Effectiveness of designed health education package on healthy behaviors of patients with tuberculosis at Pasteur Institute of Iran. J Zanjan Univ Med Sci Health Serv. 2009;17:13–20. [Google Scholar]
- 18.Taghizadeh R, Eshrati B, Kamali M, Masjedi M. Comply status of patients with pulmonary tuberculosis treated with directly observed in the urban area of Tehran with the Health Belief Model. 19th National Congress of Tuberculosis. 2008 [Google Scholar]
- 19.Janakan N, Seneviratne R. Factors contributing to medication noncompliance of newly diagnosed smear- positive pulmonary of Colombo Sri Lanka. Asia Pac J Public Health. 2008;20:214–23. doi: 10.1177/1010539508316974. [DOI] [PubMed] [Google Scholar]
- 20.Clark PM, Karagoz T, Apikoglu-Rabus S, Izzettin FV. Effect of pharmacist-led patient education on adherence to tuberculosis treatment. Am J Health Syst Pharm. 2007;64:497–505. doi: 10.2146/ajhp050543. [DOI] [PubMed] [Google Scholar]
- 21.Jahani S, Elahi N, Shahinzade A, Hakim A, Latifi SM. Relation of knowledge and attitude with control ofmedication in tuberculosis patients in Ahvaz, Iran. J Gorgan Univ Med Sci. 2011;12:80–4. [Google Scholar]
- 22.Pishkar Mofrad Z, Sabzavari S, Mohammad Alizadeh S. A survey of knowledge and attitude in medication controls of Tuberculosis patients referring to Zahedan anti TB centers in 1999. J Kerman Univ Med Sci. 2001;8:153–60. [Google Scholar]
- 23.Dean W, Graham R. How effective are health programs resistance, reactance, rationality and risk? recommendation for effective practice. Int J of Nurs Studies. 2004;41:163–72. doi: 10.1016/s0020-7489(03)00117-2. [DOI] [PubMed] [Google Scholar]
- 24.Heydariniya A. Tehran: Zamani Nasser; 2003. In theprocessof health educationtopics. [Google Scholar]
- 25.Tornee S, Kaewkungwal J, Fungladda W, Silachamroon U, Akarasewi P, Sunakorn P. Factors associated with the household contact screening adherence of tuberculosis of patients. Southeast Asian J Trop Med Public Health. 2005;36:331–40. [PubMed] [Google Scholar]
- 26.Mweemba P, Haruzivishe C, Siziya S, Chipimo PJ, Cristenson K, Johansson E. Knowledge, attitude and compliance with tuberculosis treatment, Lusaka, Zambia. Med J Zambia. 2008;35:121–8. [Google Scholar]
- 27.McDonnell M, Turner J, Weaver MT. Antecedents of adherence to anti tuberculosis therapy. Public Health Nurs. 2001;18:392–400. doi: 10.1046/j.1525-1446.2001.00392.x. [DOI] [PubMed] [Google Scholar]


