Abstract
Background
Legally mandated minimum hospital caseload requirements for certain invasive procedures, including pancreatectomy, esophagectomy, and some types of organ transplantation, have been in effect in Germany since 2004. The goal of such requirements is to improve patient care by ensuring that patients undergo certain procedures only in hospitals that have met the corresponding minimum caseload requirement. We used the case numbers published in legally mandated hospital quality control reports to determine whether the hospitals actually met the stipulated requirements.
Methods
We performed a secondary analysis of data supplied by hospitals in their quality control reports for the years 2004, 2006, 2008, and 2010 with respect to six procedures that have a minimum caseload requirement: complex interventions on the esophagus and pancreas, total knee replacement, and hepatic, renal, and stem-cell transplantation.
Results
The total case numbers for these six different procedures rose from 22 064 (0.1% of all procedures) in 2004 to 170 801 (0.9% of all procedures) in 2010. From 2006 onward, procedures to which minimum caseload requirements apply have been carried out in half of all hospitals studied. These procedures account for 0.9% of all inpatient cases in Germany. The percentage of hospitals that continue to perform certain procedures despite not having met the minimum caseload requirement ranged from 5% to 45%, depending on the type of procedure, and the percentage of cases carried out in such hospitals ranged from 1% to 15%. These values remained nearly constant for each of the six minimum caseload requirements over the 4 reporting years for which data were examined.
Conclusion
The establishment of minimum caseload requirements in Germany in 2004 did not lessen the number of cases performed in violation of these requirements over the period 2004 to 2010.
Minimum caseloads are widely held to be an effective way of ensuring and improving the quality of medical interventions. However, the empirical evidence for this beneficial effect is inconsistent. Difficulties in interpreting the empirical evidence are caused particularly by inhomogeneity of the methods used for data acquisition and calculation (1–4). Debate focuses on the following aspects:
The type of data used (5)
The use of valid indicators to measure outcome quality (6, 7)
Comprehensive adjustment procedures to compare the patient populations treated (8–11)
The statistical relevance of rare events (12)
Moreover, numerous studies have investigated what structural and process-related factors lie behind the proxy indicator “case volume of facility” (16–23).
Nonetheless, the Federal Joint Committee (G-BA) acceded to the demands of German legislators and implemented, with due consideration of the current state of knowledge, “a catalog of planable interventions […] for which the quality of treatment outcome depends strongly on the volume of interventions performed […] as well as minimum caseloads per physician or hospital and exceptional circumstances” (§ 137 German Social Code V). Minimum caseloads were established for five inpatient surgical interventions in 2004, for a sixth operation in 2006, and for two further interventions in 2010. No minimum volumes have yet been defined for heart surgery (24). The classes of intervention and the prescribed volumes are shown in Table 1.
Table 1. Minimum caseload requirements 2004 to 2012: minimum volumes per hospital by report year.
| Intervention class | 2004 | 2006 | 2008 | 2010 | 2012 |
|---|---|---|---|---|---|
| Complex interventions on the esophagus organ system | 5 | 10 | 10 | 10 | 10 |
| Complex interventions on the pancreas organ system | 5 | 10 | 10 | 10 | 10 |
| Kidney transplantation | 20 | 25 | 25 | 25 | 25 |
| Liver transplantation | 10 | 20 | 20 | 20 | 20 |
| Stem cell transplantation | 12 | 25 | 25 | 25 | 25 |
| Total knee replacement | – | 50 | 50 | 50 | 50* |
| Heart surgery | – | – | – | – | – |
| Prematures and neonates with birthweight <1250g | – | – | – | 14 | 14 |
*Suspended for 2012
We set out to investigate the six areas of surgery for which minimum caseload requirements were introduced in 2004 or 2006. The minimum volume for treatment of neonates, introduced in 2010, was excluded—although currently much debated (25, 26) —because only data for the year 2010 were available.
On implementation of the minimum caseloads, hospitals in Germany became obliged to publish a biennial structured quality control report showing the number of patients treated with each of the interventions for which minimum caseloads are required. This report also has to explain any exceptional circumstances leading to failure to meet minimum caseload requirements. The quality control reports are freely available on the internet and can be obtained in electronic form from the G-BA. The data from the quality control reports permit conclusions to be drawn with regard to hospitals, case numbers, and exceptional circumstances. In this article we describe the implementation of six minimum caseload requirements in the period 2004 to 2010.
Methods
The investigation was designed as a retrospective, cross-sectional, observational study with the quality control report data from the years 2004, 2006, 2008, and 2010 as secondary source data. The XML files were exported to Excel and SPSS for evaluation. The analysis was purely descriptive. The data for each year were analyzed separately. For liver transplantation, the only data analyzed were those from the institutions defined as liver transplantation centers by the German Organ Transplantation Foundation, as previously described in detail in an evaluation of the data for the year 2004 (27); data from hospitals where other hepatic interventions were performed were not considered. All hospital caseload data for minimum caseload procedures was checked for plausibility. In one year, one hospital was excluded from analysis owing to an implausible six-digit number of interventions. Redundant quality control reports from 12 hospitals were removed from the data set, as were quality control reports from 76 hospitals organized into 34 hospital groups in which the case numbers per minimum volume intervention could not be assigned to the individual hospitals. For these reasons, 2.2% of all hospitals with minimum caseload data and 2 815 (0.6%) interventions involving minimum volume procedures were not included in our analysis.
Results
Hospitals and cases analyzed
Of the 1983 hospitals that published a quality control report for the year 2004, 481 (24%) had carried out at least one class of minimum volume intervention. Following the addition of minimum caseload requirements for total knee replacement (TKR), the proportion of hospitals reporting relevant interventions rose to 52% in 2006, 54% in 2008, and 56% in 2010. After the inclusion of TKR the total number of minimum volume interventions rose sharply from 22 064 in 2004 to 143 058 in 2006; further increases in 2008 and 2010 took the total to 170 850 at the end of the study period. The minimum volume interventions represented 0.1% of all inpatient cases in German hospitals in 2004, rising to 0.9% in 2010 (Table 2). According to the Federal Statistical Office, the total number of inpatient cases increased by 7% between 2004 and 2010 (28).
Table 2. Number of hospitals issuing quality control reports and number of hospitals performing at least one of the six classes of intervention with minimum caseload requirements in the period 2004 to 2010.
| 2004 | 2006 | 2008 | 2010 | |
|---|---|---|---|---|
| Hospitals with quality control report | 1983 | 1940 | 1922 | 1871 |
| Hospitals with at least one MV class, uncorrected | 485 | 1018 | 1047 | 1071 |
| Hospitals with at least one MV class, corrected (% of all hospitals with quality control reports) | 481 (24%) | 1007 (52%) | 1032 (54%) | 1055 (56%) |
| Inpatient admissions in Germany | 16 801 649 | 16 832 883 | 17 519 579 | 18 026 451 |
| Case numbers of the six MV intervention classes according to quality control reports (% of all cases) | 22 064 (0.1%) | 143 012 (0.8%) | 166 361 (0.9%) | 170 801 (0.9%) |
MV, minimum volumes
Number of hospitals and case numbers per minimum volume intervention and report year
The number of hospitals that reported carrying out the individual minimum volume interventions fluctuated hardly at all between 2004 and 2010 (Table 3). The numbers performing complex operations on the esophagus and the pancreas went down from 2004 to 2006 but increased again thereafter. The fluctuation was even smaller for liver, kidney, and stem cell transplantations.
Table 3. Number of hospitals performing minimum volume interventions and case numbers per minimum volume and report year.
| Year | MV threshold | Hospitals with MV data | Hospitals under MV threshold | Hospitals under MV threshold without exceptional circumstances | Number of cases*1 | Number of cases in hospitals under MV threshold | |
|---|---|---|---|---|---|---|---|
| Complex interventions on esophagus | 2004 | 5 | 297 | 86 (29%) | – | 3302 | 179 (5%) |
| 2006 | 10 | 279 | 119 (43%) | 47 (39%) | 3450 | 515 (15%) | |
| 2008 | 10 | 283 | 134 (47%) | 23 (17%) | 3459 | 573 (17%) | |
| 2010 | 10 | 289 | 128 (44%) | 34 (27%) | 3610 (+9%) | 534 (15%) | |
| Complex interventions on pancreas | 2004 | 5 | 456 | 84 (18%) | – | 8417 | 200 (2%) |
| 2006 | 10 | 453 | 163 (36%) | 56 (34%) | 8643 | 741 (9%) | |
| 2008 | 10 | 457 | 139 (30%) | 28 (20%) | 9161 | 631 (7%) | |
| 2010 | 10 | 471 | 136 (29%) | 29 (21%) | 9440 (+12%) | 626 (7%) | |
| Kidney transplantation | 2004 | 20 | 43 | 4 (9%) | – | 2528 | 39 (2%) |
| 2006 | 25 | 40 | 2 (5%) | 0 (0%) | 2784 | 15 (1%) | |
| 2008 | 25 | 40 | 4 (10%) | 0 (0%) | 2784 | 63 (2%) | |
| 2010 | 25 | 37 | 2 (5%) | 0 (0%) | 2856 (+13%) | 32 (1%) | |
| Liver transplantation*2 | 2004 | 10 | 24 | 0 (0%) | – | 2639 | 0 (0%) |
| 2006 | 20 | 23 | 1 (4%) | 0 (0%) | 1381 | 16 (1%) | |
| 2008 | 20 | 23 | 3 (13%) | 0 (0%) | 1386 | 37 (3%) | |
| 2010 | 20 | 23 | 1 (4%) | 0 (0%) | 1464 (+6%) | 17 (1%) | |
| Stem cell transplantation | 2004 | 12 | 82 | 13 (16%) | – | 5178 | 77 (1%) |
| 2006 | 25 | 82 | 18 (22%) | 7 (39%) | 6206 | 254 (4%) | |
| 2008 | 25 | 74 | 19 (26%) | 4 (21%) | 5564 | 274 (5%) | |
| 2010 | 25 | 84 | 22 (26%) | 6 (27%) | 6320 (+22%) | 290 (5%) | |
| Total knee replacement | 2006 | 50 | 900 | 118 (13%) | 45 (38%) | 120548 | 2705 (2%) |
| 2008 | 50 | 936 | 76 (8%) | 19 (25%) | 144007 | 1842 (1%) | |
| 2010 | 50 | 969 | 81 (8%) | 19 (23%) | 147111 (+22%) | 2048 (1%) |
*1 In parentheses, percent increase during observation period; *2data from liver transplantation centers; MV, minimum volume
The number of hospitals carrying out TKR between 2006 and 2010 increased by around 30 with each new report. The number of cases increased for all minimum caseload interventions between 2004 and 2010. Compared with the 7% increase in total inpatient cases in the same period, the changes in case numbers were slightly lower for liver transplantation (+6%) but somewhat higher for complex interventions on the esophagus (+9%). The changes for complex interventions on the pancreas (+12%) and kidney transplantation (+13%) were much more pronounced. The case numbers for stem cell transplantation and TKR rose even more sharply (+22%).
Number of hospitals below the minimum caseload requirement
The number of hospitals that did not meet the minimum caseload requirements varied among the interventions, but remained broadly constant for each individual intervention.
With the minimum volume thresholds for esophageal and pancreatic interventions doubling from 5 in 2004 to 10 in 2006, the number of hospitals failing to fulfill the requirements increased sharply. From 2006 onwards, the rate was around 45% for esophageal operations and 30% for pancreatic surgery. For kidney transplantation the rate varied between 5% and 10%, for liver transplantation between 0% and 13%. The number of hospitals that did not achieve the minimum caseload requirement for stem cell transplantation increased when the threshold was raised from 12 to 25 interventions per year; since then the rate has been around 25%. For TKR the proportion of hospitals that did not meet the minimum caseload requirement fell from 13% to 8%.
The case numbers in the hospitals with too few interventions varied widely among the classes of intervention, but remained fairly constant over time for each individual intervention class. The lowest case numbers were for liver and kidney transplantations, at 1 to 3% and 15 to 63 cases, followed by stem cell transplantation with 5% and 250 to 290 cases. The proportion was also low for TKR in the two most recent report years, at 1%, but this represented approximately 2000 patients each time. The percentages were much higher for complex interventions on the pancreas (7 to 9%, 626 to 741 cases) and the esophagus (15 to 17%, over 500 cases).
Under the minimum caseload regulations, hospitals that do not achieve the caseload thresholds are obliged to itemize any exceptional circumstances. Since 2010, these comprise:
Emergency interventions
Extension of services offered
Staff restructuration
Decisions taken by the federal state authorities (responsible for hospital planning) to ensure state-wide provision of care.
Two circumstances previously classed as exceptional, “intervention started with curative intent but finished palliatively or exploratively” and “surgeon training,” no longer count.
For each class of intervention, between 20 and 40% of hospitals that lay under the minimum volume thresholds reported no exceptional circumstances at any time during the period 2006 to 2010 (Table 3). No equivalent statement can be made for the year 2004 because of differences in the reporting format.
Average numbers of interventions per hospital
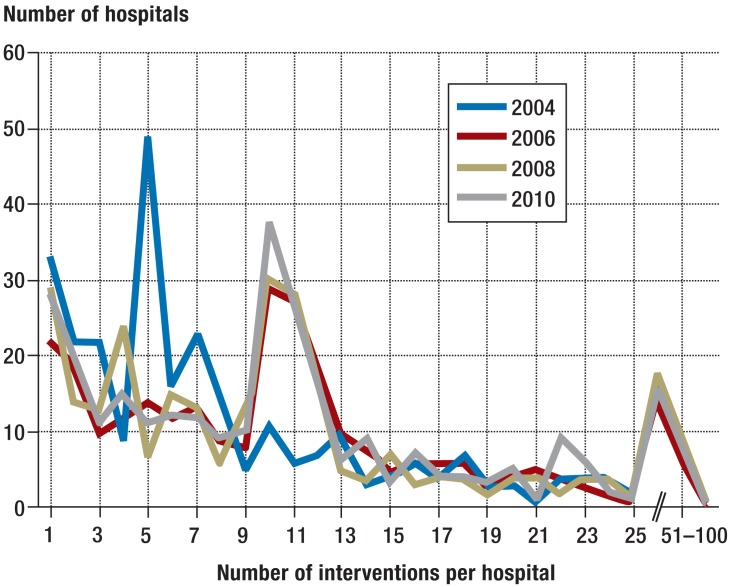
The average numbers of minimum volume interventions per hospital and year are listed in Table 4, together with the statistical measures of central tendency. Inspection of the number of operations per class of intervention in each individual hospital reveals that the number of interventions per hospital peaked at exactly the minimum volume threshold, as illustrated for complex interventions on the esophagus in the Figure.
Table 4. Average number of interventions per hospital by minimum volume and report year.
| Year | Minimum | Maximum | Median | Mean | Standard deviation | |
|---|---|---|---|---|---|---|
| Complex interventions on esophagus | 2004 | 1 | 236 | 6 | 11.1 | 17.8 |
| 2006 | 1 | 150 | 10 | 12.3 | 13.8 | |
| 2008 | 1 | 124 | 10 | 12.2 | 14.0 | |
| 2010 | 1 | 112 | 10 | 12.5 | 14.1 | |
| Complex interventions on pancreas | 2004 | 1 | 362 | 10 | 18.5 | 28.8 |
| 2006 | 1 | 384 | 11 | 19.1 | 31.7 | |
| 2008 | 1 | 395 | 13 | 20.1 | 29.8 | |
| 2010 | 1 | 427 | 13 | 20.0 | 29.8 | |
| Kidney transplantation | 2004 | 1 | 192 | 48 | 58.8 | 36.9 |
| 2006 | 4 | 251 | 57.5 | 69.6 | 48.4 | |
| 2008 | 9 | 255 | 60.5 | 69.9 | 48.7 | |
| 2010 | 12 | 264 | 69 | 77.2 | 51.7 | |
| Liver transplantation* | 2004 | – | – | – | – | – |
| 2006 | 16 | 143 | 51 | 60.0 | 36.7 | |
| 2008 | 11 | 146 | 47 | 60.3 | 37.9 | |
| 2010 | 17 | 160 | 60 | 63.7 | 35.7 | |
| Stem cell transplantation | 2004 | 1 | 370 | 37 | 64.0 | 69.9 |
| 2006 | 1 | 349 | 39 | 75.7 | 78.6 | |
| 2008 | 1 | 306 | 39 | 75.2 | 74.7 | |
| 2010 | 1 | 320 | 38.5 | 75.2 | 77.5 | |
| Total knee replacement | 2006 | 1 | 979 | 93 | 134.3 | 126.0 |
| 2008 | 1 | 1329 | 109 | 153.9 | 143.3 | |
| 2010 | 1 | 1367 | 108 | 151.8 | 140.2 |
*Data from liver transplantation centers
Figure.
Complex esophageal interventions: number of cases per year and hospital over the study period. The minimum volume threshold was five cases in 2004, ten cases from 2006 onwards
In 2004 there were nine hospitals with four esophageal interventions and 49 hospitals (5.4 times as many) with five operations on the esophagus. From 2006 onwards, after the threshold was raised from 5 to 10 interventions per year, the number of hospitals with 10 operations on the esophagus was 2.3 to 3.8 times higher than that with nine interventions. Comparable differences precisely at the threshold value in all report years were found for TKR (3.3- to 5.0-fold), while the differences were somewhat less pronounced for complex interventions on the pancreas (2.4- to 3.2-fold) and stem cell transplantation (2.0- to 4.0-fold). No such increase was found for liver or kidney transplantation.
Discussion
The caseload requirements for the six minimum volume interventions we investigated, which involve more than half of all hospitals in Germany—although they comprise scarcely 1% of inpatient cases—are not always fulfilled. The goal of the minimum caseload requirements, namely to carry out the defined interventions exclusively in hospitals that achieve the minimum volumes, is therefore not being achieved.
The number of hospitals that performed such interventions without reaching the threshold remained constant throughout the study period, as did the proportion of patients treated in such hospitals. This was not affected by the fact that for most of the defined classes of intervention the percentage rise in the number of cases exceeded the increase for surgery in Germany overall. There has therefore been no increase in centralization for the minimum volume interventions. The existing extent of centralization can be described as the proportion of interventions carried out in hospitals that do not meet the minimum caseload requirements. By this yardstick liver transplantation, kidney transplantation, and TKR, with 1 to 2% of interventions in such hospitals, have achieved a high degree of centralization. The corresponding proportions of cases are much higher for pancreatic and esophageal interventions, at 7% and 15% respectively, while stem cell transplantation occupies an intermediate position with 5%.
How do these figures compare with other countries? Esophageal and pancreatic interventions are of particular interest, and comparable studies have been published. In the USA, where minimum volumes have been promoted in various ways since the 1990s, Learn and Bach (29) found tendencies towards centralization for many different interventions in a nationwide sample. For instance, the proportion of pancreatectomies carried out in hospitals with fewer than 10 cases per year fell from 67% in the three-year period 1997 to 1999 to only 51% in 2004 to 2006. Over the same time span, the proportion of esophagectomies performed in hospitals with fewer than six cases per year sank from 69% to 53%. This degree of centralization is nowhere near that achieved in Germany. In the Netherlands, however, the situation is comparable with that in Germany: a minimum volume threshold of 10 interventions was introduced for pancreatectomy in 2006, and the proportion of interventions carried out in hospitals with fewer than 10 interventions per year decreased from 47.2% in 2004 to 9% in 2009 (30).
It remains to be seen how the proportion of cases in hospitals that do not meet the minimum caseload requirements will develop. Three fourths of these hospitals mentioned exceptional circumstances. “Emergency interventions” will continue to be cited as a reason, and “extension of services” and “staff restructuration” are signs of evolution in the hospital sector. To date, “ensuring state-wide provision of care” is practically irrelevant in this regard. As for the hospitals that cited no exceptional circumstances as reasons for failing to achieve minimum caseloads, the potential for and barriers to regional cooperation with regard to low-volume interventions should be investigated.
The impact of the German minimum caseload regulations on the quality of care is outside the scope of this study. Nevertheless, the fact that no substantial trend towards centralization has yet occurred makes such an effect seem unlikely. It remains difficult to furnish concrete proof of shifts in the quality of treatments in Germany, as early evaluations have shown (28, 31). However, this may change. Since 2006, hospitals have been obliged to document some of the quality indicator outcomes of external quality assurance in their quality control reports, e.g., for TKR and for liver and kidney transplantations. One crucial factor in assessing evolution over time will be consistency in definition of the indicators. However, because hospitals are obliged to respect patients' privacy and quality indicators are reported only from five cases upward, quality assessment remains restricted for the particularly interesting low case numbers.
Limitations
With regard to the method, the data quality of hospitals' reports of their own activities has to be questioned. It is astounding, for example, how many hospitals precisely fulfilled the minimum caseload requirements for the non-transplantation interventions. This may point to distortion by falsification of the data in the quality control reports or to dubious extension of indications for the interventions concerned. Clarification of the reason would require separate empirical investigation of these two factors. The hospitals themselves state that they use their quality control reports not only for internal quality management and comparison with other hospitals, but also for purposes of external presentation (32). In this regard, a public statement of whether or not a minimum caseload requirement was met could well be important, although patients practically never use information of this kind (33).The quality control reports are also addressed to health insurance funds; however, an analysis published in 2008 yielded no indication that these bodies made systematic use of the information on minimum volumes in budget negotiations (34). It should be investigated whether health insurance funds have since changed their behavior in this respect.
Prospects
Further research should link the individual hospitals' quality control reports over the years to allow longitudinal analyses to establish how consistently hospitals adhere to minimum caseload requirements. Moreover, geographical analyses could examine questions of regional availability from the patients' perspective (35- 39). Furthermore, the results could prompt comparison of the relevance and impact of the minimum volumes regulation with other structure-related quality initiatives, such as that for the development of breast centers in North Rhine–Westphalia (40).
Summary
The overall conclusion is that health services research should continue to evaluate the politically heavily favored requirements for minimum caseloads with the aim of identifying not only the possible positive effects of these regulations but also any negative consequences. The impact of the minimum caseload requirements on patients' health outcomes should also be investigated in comparison with other measures that are actually implemented and may exert a more sustained influence on the quality of care.
Key Messages.
Minimum volume thresholds were introduced for five classes of interventions (complex esophageal and pancreatic surgery, transplantation of liver, kidney, and stem cells) in German hospitals in 2004; total knee replacement was added in 2006, neonatal interventions in 2010. Hospitals are obliged to disclose how many of these interventions were performed in their quality control reports.
The minimum caseload requirements introduced in 2004 and 2006 affect half of the hospitals in Germany, but involve only 0.9% of all inpatient cases.
Depending on the class of intervention, 5 to 45% of reporting hospitals fail to achieve the minimum volume threshold.
The proportion of patients treated in hospitals that do not fulfill the minimum caseload requirements varies among the different interventions from 1% to 15%, but remains broadly constant over time for each intervention.
The strikingly high numbers of hospitals that precisely attain the minimum volume thresholds for the non-transplantation interventions prompts questions regarding data quality and/or indication quality, at least for this case number segment.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Prof. Geraedts has received payment from the German Medical Association for acting as a consultant on minimum caseloads. He has received honoraria for lectures on minimum caseloads and reimbursement of travel costs from the Federal Joint Committee (G-BA). His research on minimum volumes has been supported by the Federal Ministry of Health.
The other two authors declare that no conflict of interest exists.
References
- 1.Kozower BD, Stukenborg GJ. Lung cancer resection volume: is procedure volume really an indicator of quality? Semin Thorac Cardiovasc Surg. 2012;24:93–98. doi: 10.1053/j.semtcvs.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Hogan AM, Winter DC. Does practice make perfect? Ann Surg Oncol. 2008;15:1267–1270. doi: 10.1245/s10434-007-9804-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Geraedts M. Spärliche Evidenz für explizite Mindestmengen. Dtsch Arztebl. 2004;101:A1402–A1405. [Google Scholar]
- 4.Geraedts M, de Cruppé W. Kontroverse Studienergebnisse zur Mindestmengenproblematik. ZaeFQ. 2006;100:87–91. [PubMed] [Google Scholar]
- 5.Khuri SF, Henderson WG. The case against volume as a measure of quality of surgical care. World J Surg. 2005;29:1222–1229. doi: 10.1007/s00268-005-7987-6. [DOI] [PubMed] [Google Scholar]
- 6.Wouters MWJM, Boot H, Tollenaar RAEM, van Sandick JW Courrech Staal EFW. Quality-of-care indicators for oesophageal cancer surgery: A review. Eur J Surg Oncol. 2010;36:1035–1043. doi: 10.1016/j.ejso.2010.08.131. [DOI] [PubMed] [Google Scholar]
- 7.Tanvetyanon T. Quality-of-care indicators for non-small cell lung cancer. Cancer Control. 2009;16:335–341. doi: 10.1177/107327480901600408. [DOI] [PubMed] [Google Scholar]
- 8.Gruen RL, Pitt V, Green S, Parkhill A, Campbell D, Jolley D. The effect of provider case volume on cancer mortality: systematic review and meta-analysis. CA Cancer J Clin. 2009;59:192–211. doi: 10.3322/caac.20018. [DOI] [PubMed] [Google Scholar]
- 9.Rogers SO., Jr The holy grail of surgical quality improvement: process measures or risk-adjusted outcomes? Am Surg. 2006;72:1046–1050. discussion 1061-9, 1133-48. [PubMed] [Google Scholar]
- 10.Christian CK, Gustafson ML, Betensky RA, Daley J, Zinner MJ. The volume-outcome relationship: don't believe everything you see. World J Surg. 2005;29:1241–1244. doi: 10.1007/s00268-005-7993-8. [DOI] [PubMed] [Google Scholar]
- 11.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Annals of Internal Medicine. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 12.Thomas JW, Hofer TP. Accuracy of risk-adjusted mortality rate as a measure of hospital quality of care. Med Care. 1999;37:83–92. doi: 10.1097/00005650-199901000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Grouven U, Küchenhoff H, Schräder P, Bender R. Flexible regression models are useful tools to calculate and assess threshold values in the context of minimum provider volumes. J Clin Epidemiol. 2008;61:1125–1131. doi: 10.1016/j.jclinepi.2007.11.020. [DOI] [PubMed] [Google Scholar]
- 14.Bender R, Grouven U. Möglichkeiten und Grenzen statistischer Regressionsmodelle zurBerechnung von Schwellenwertenfür Mindestmengen. [Possibilities and limitations of statistical regression models for the calculation of threshold values for minimum provider volumes] Z Arztl Fortbild Qualitatssich. 2006;100:93–98. [PubMed] [Google Scholar]
- 15.Gandjour A, Bannenberg A, Lauterbach KW. Threshold volumes associated with higher survival in health care. Medical Care. 2003:10–1141. doi: 10.1097/01.MLR.0000088301.06323.CA. [DOI] [PubMed] [Google Scholar]
- 16.Brand CA, Barker AL, Morello RT, Vitale MR, Evans SM, Scott IA. A review of hospital characteristics associated with improved performance. Int J Qual Health Care. 2012;24:483–494. doi: 10.1093/intqhc/mzs044. [DOI] [PubMed] [Google Scholar]
- 17.Cornish JA, Tekkis PP, Tan E, Tilney HS, Thompson MR, Smith JJ. The national bowel cancer audit project: the impact of organisational structure on outcome in operative bowel cancer within the United Kingdom. Surg Oncol. 2011;20:e72–e77. doi: 10.1016/j.suronc.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Du Bois A, Rochon J , Pfisterer J, Hoskins WJ. Variations in institutional infrastructure, physician specialization and experience, and outcome in ovarian cancer: a systematic review. Gynecol Oncol. 2009;112:422–436. doi: 10.1016/j.ygyno.2008.09.036. [DOI] [PubMed] [Google Scholar]
- 19.Bilimoria KY, Phillips JD, Rock CE, Hayman A, Prystowsky JB, Bentrem DJ. Effect of surgeon training, specialization, and experience on outcomes for cancer surgery: a systematic review of the literature. Ann Surg Oncol. 2009;16:1799–1808. doi: 10.1245/s10434-009-0467-8. [DOI] [PubMed] [Google Scholar]
- 20.Chowdhury MM, Dagash H, Pierro A. A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg. 2007;94:145–161. doi: 10.1002/bjs.5714. [DOI] [PubMed] [Google Scholar]
- 21.Kraus TW, Büchler MW, Herfarth C. Relationships between volume, efficiency, and quality in surgery-a delicate balance from managerial perspectives. World J Surg. 2005;29:1234–1240. doi: 10.1007/s00268-005-7988-5. [DOI] [PubMed] [Google Scholar]
- 22.Urbach DR, Baxter NN. Does it matter what a hospital is „high volume“ for? Specificity of hospital volume-outcome associations for surgical procedures: analysis of administrative data. BMJ. 2004;328 doi: 10.1136/bmj.38030.642963.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klimm B, Brillant C, Skoetz N, Muller H, Engert A, Borchmann P. The effect of specialized cancer treatment centers on treatment efficacy in Hodgkin's lymphoma. Dtsch Arztebl Int. 2012;109:893–899. doi: 10.3238/arztebl.2012.0893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gemeinsamer Bundesausschuss. Regelungen des Gemeinsamen Bundesausschusses gemäß §137 Abs 3 Satz 1 Nr. 2 SGB V für nach § 108 SGB V zugelassene Krankenhäuser. (Mindestmengenreglungen, Mm-R). Bundeanzeiger (BAnz AT 29.11.2012 B2) https://www.g-ba.de/informationen/richtlinien/5/ (last accessed on 25 March 2014)
- 25.Kutschmann M, Bungard S, Kotting J, Trumner A, Fusch C, Veit C. The care of preterm infants with birth weight below 1250 g. Dtsch Arztebl Int. 2012;109:519–526. doi: 10.3238/arztebl.2012.0519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zimmer KP. Neonatology departments under economic pressure. Dtsch Arztebl Int. 2012;109:517–518. doi: 10.3238/arztebl.2012.0517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gemeinsamer Bundesausschuss. Ergebnisse der Begleitforschung zur Einführung von Mindestmengen in Deutschland. http://www.g-ba.de/informationen/richtlinien/5/ (last accessed on 25 March 2014)
- 28.Statistisches Bundesamt. Destatis Fachserie 12 Reihe 61.1. Gesundheit, Grunddaten der Krankenhäuser 2012. Stand 20.3.2014. Wiesbaden: Statistisches Bundesamt 2013. https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Krankenhaeuser/GrunddatenKrankenhaeuser.html;jsessionid=D8295A0266E4B90272BB2975AFDD8B1B.cae4. (last accessed on 25 March 2014)
- 29.Learn PA, Bach PB. A decade of mortality reductions in major oncologic surgery: the impact of centralization and quality improvement. Med Care. 2010;48:1041–1049. doi: 10.1097/MLR.0b013e3181f37d5f. [DOI] [PubMed] [Google Scholar]
- 30.de Wilde RF, Besselink MGH, van der Tweel I, de Hingh IHJT, van Eijck CHJ, Dejong CHC. Impact of nationwide centralization of pancreaticoduodenectomy on hospital mortality. Br J Surg. 2012;99:404–410. doi: 10.1002/bjs.8664. [DOI] [PubMed] [Google Scholar]
- 31.Geraedts M, de Cruppé W, Blum K, Ohmann C. Implementation and effects of Germany's minimum volume regulations: results of the accompanying research. Dtsch Arztebl Int 2008. 105:890–896. doi: 10.3238/arztebl.2008.0890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Auras S, de Cruppé W, Blum K, Geraedts M. Mandatory quality reports in Germany from the hospitals' point of view: a cross-sectional observational study. BMC Health Services Research. 2012;12 doi: 10.1186/1472-6963-12-378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Cruppé W, Geraedts M. Wie wählen Patienten ein Krankenhaus für elektive operative Eingriffe? [How do patients choose a hospital for elective surgery?] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2011;54:951–957. doi: 10.1007/s00103-011-1320-3. [DOI] [PubMed] [Google Scholar]
- 34.Geraedts M, Kühnen C, de Cruppé W, Blum K, Ohmann C. Unterschreitungen der Mindestmengen 2004: Begründungen und Konsequenzen. Gesundheitswesen. 2008;70:63–67. doi: 10.1055/s-2007-1022522. [DOI] [PubMed] [Google Scholar]
- 35.de Cruppé W, Ohmann C, Blum K, Geraedts M. Evaluating compulsory minimum volume standards in Germany: how many hospitals were compliant in 2004? BMC Health Serv Res. 2007;7 doi: 10.1186/1472-6963-7-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Cruppé W, Ohmann C, Blum K. Geraedts M: Auswirkung der Mindestmengenvereinbarung auf die stationäre Versorgungsstruktur (Influence of minimum volumes on the structure of inpatient care) Gesundheitswesen. 2008;70:9–17. doi: 10.1055/s-2007-985888. [DOI] [PubMed] [Google Scholar]
- 37.Geraedts M, de Cruppé W, Blum K, Ohmann C. Distanzen zu Krankenhäusern mit Mindestmengen-relevanten Eingriffen 2004 bis 2006. Das Gesundheitswesen. 2009;72:271–278. doi: 10.1055/s-0029-1225653. [DOI] [PubMed] [Google Scholar]
- 38.Simoes E, Bauer S, Jaeckel R, Schwoerer P, Schmahl FW. Effekte von Mindestmengenregelungen auf die stationäre Versorgungslandschaft. Arbeitsmed Sozialmed Umweltmed. 2004;39:410–417. [Google Scholar]
- 39.Birkmeyer JD, Siewers AE, Marth NJ, Goodman DC. Regionalization of high-risk surgery and implications for patient travel times. JAMA. 2003;290:2703–2708. doi: 10.1001/jama.290.20.2703. [DOI] [PubMed] [Google Scholar]
- 40.Geraedts M, Malik M, Jung O, de Cruppé W. Brustkrebszentren in Nordrhein-Westfalen – Fallzahlenentwicklung 2004–2010 [Breast cancer centres in North Rhine-Westphalia—case volume trends 2004–2010] Gesundheitswesen. 2013;75:424–429. doi: 10.1055/s-0032-1323701. [DOI] [PubMed] [Google Scholar]