Abstract
Introduction
The implementation of enhanced recovery programmes (ERPs) in colorectal surgery has seen improvements in the length of inpatient stay with no increase in complications. We investigated the role of ERP in radical cystectomy at our institution.
Methods
Prospective data were collected from 26 consecutive patients prior to the introduction of the ERP and 51 patients who underwent open radical cystectomy within an ERP. Individuals in the ERP cohort did not receive bowel preparation or nasogastric drainage but received preoperative carbohydrate drinks, perioperative epidural analgesia and immediate mobilisation on day 1. Primary outcome measures included duration of intensive care unit (ICU) stay and length of hospital stay. Secondary outcome measures included the time to the passage of flatus and faeces, and time to mobilisation. Other measures that were analysed included operation time and complications.
Results
Baseline characteristics for both groups were similar. The median length of hospital stay fell from 11.5 days to 10.4 days and the mean ICU stay dropped from 2.4 days to 1.0 days (p=0.01). Time to removal of nasogastric tube, and time to passage of flatus and faeces were significantly shorter in the ERP group, as was the time to full oral diet. Clavien complication rates and 30-day mortality rates were similar in both groups. There were no readmissions.
Conclusions
ERP in radical cystectomy is safe and not associated with any increase in complications or readmissions. It is associated with reductions in ICU stay, and could also reduce length of hospital stay and duration of postoperative ileus.
Keywords: Enhanced recovery programme, Cystectomy, Stoma, Length of stay
Bladder cancer is a major cause of morbidity and mortality worldwide, with almost 9,000 new cases diagnosed in England and Wales in 2010 and over 4,000 deaths occurring from the disease. 1,2 The overwhelming majority of bladder carcinomas (>90%) are urothelial carcinomas and almost 80% of this group are non-muscle invasive. About 20% will present with muscle invasive disease, and require radical treatments such as cystectomy and reconstruction.
Patients who undergo such a radical intervention are often starved preoperatively, prescribed purgatives and admitted for long hospital stays. In fact, the UK mean inpatient stay for radical cystectomy is 15.6 days. 3 During this period of time, the reintroduction of fluids and diet is delayed. This is often dependent on the clinical detection of bowel sounds together with the passage of flatus and faeces. The rationale for this regime was the concern that early dietary input would increase the risk of anastomotic dehiscence as well as bowel distension and bowel obstruction.
Despite this established practice, recent papers have demonstrated that the introduction of enhanced recovery programmes (ERPs) for patients undergoing colorectal surgery has been associated with a significant reduction in hospital stay with no increase in readmissions, complications or mortality. 4,5 ERPs are made up of a number of different elements, all of which have a good evidence base. The elements of an ERP include the omission of a number of practices (oral bowel purgative preparation, preanaesthetic anxiolytic or analgesic medication and the limitation of antimicrobial prophylaxis), the alteration of some techniques (perioperative fluid management, ileus prophylaxis) and the introduction of novel methods (preadmission information and counselling, fluid and carbohydrate loading, and early mobilisation). 6
A key feature of the ERPs is that patients are allowed to drink clear fluids up to two hours prior to surgery. 7 While solid foods must be avoided for six hours, specially designed polymeric carbohydrate beverages can be given safely up to two hours prior to surgery. These drinks are absorbed rapidly in the upper gastrointestinal tract and are therefore unlikely to affect the field used in urological surgery (ie proximal ileum). 8,9
The initial work on ERPs excluded patients with stomas but recent work has demonstrated that stoma formation need not prolong hospital stay after open anterior resection. 10,11 The impact of an ERP in urological surgery has also been assessed previously by Arumainayagam et al, who conducted a retrospective analysis of the case notes of 112 patients who had undergone a radical cystectomy. 12 Fifty-six of these patients had done so in the context of a newly introduced ERP while the remainder had received their surgery without this programme. This former group was associated with a significantly reduced hospital stay from 15 days (range: 13–21 days) in the non-ERP group to 12 days (range: 10–15 days) in the ERP group (p=0.001).
We sought to implement an ERP at our institution to improve our inpatient hospital stay while ensuring clinical safety. This was conducted on the background of an ERP already introduced by the colorectal department in our hospital. (Data not published.) We collected data prospectively from all individuals undergoing a radical cystectomy and reconstruction from October 2007, and compared these outcomes with those of patients undergoing a radical cystectomy and reconstruction following the implementation of the ERP.
Methods
The implementation of the ERP at our institution followed the principles as suggested by Kehlet and Faiz et al (Table 1). 10,13 An ERP had already been introduced by the colorectal department in our hospital for all patients undergoing major colorectal surgery, enhancing our understanding of the issues central to its use. Given this, there were no specific inclusion or exclusion criteria for this change to clinical practice although patient consent for the use of ERP was sought prior to its introduction. All consultant surgeons who completed radical cystectomy at our institution participated in the production of the ERP and its subsequent implementation. The involvement of nursing colleagues and anaesthetists was also central to the ERP. Formal ethical approval was not sought for these changes to clinical practice but the principles of the Helsinki Declaration were followed.
Table 1.
Principles important in enhanced recovery programmes
| Preoperative education of all patients | Short-acting anaesthesia |
|---|---|
| Preoperative nutrition | Intraoperative warming |
| No oral bowel preparation | Avoidance of fluid/sodium overload |
| Carbohydrate loading | Routine postoperative mobilisation |
| No premedication | Prevention of nausea and vomiting |
| Short incisions | Early feeding |
| Avoidance of nasogastric tubes and drains | Non-opiate oral analgesia |
| Midthoracic epidural analgesia | Early removal of urinary catheters |
Data were collected prospectively from all individuals undergoing radical cystectomy and reconstruction at our institution from October 2007 onwards. This enabled direct comparison of outcomes between patients undergoing radical cystectomy and reconstruction prior to the implementation of the ERP (26 patients: October 2007– June 2009) with 59 patients who had undergone the procedure following its implementation (July 2009 – April 2012). Randomisation was not conducted as benefits had already been documented in the literature in the context of colorectal surgery, cystectomy and also in our institution with patients undergoing colorectal procedures (unpublished). 6,10,11
The ERP for radical cystectomy was instituted on 30 June 2009 with the processes of our department reconfigured from the beginning of the patient journey. Patients were informed actively of the ERP when seen in clinic and again at the preoperative assessment. Nursing staff gave patients preoperative energy drinks to be taken two hours prior to surgery. Intraoperatively, care was taken to avoid large incisions, nasogastric tubes and also unnecessary drains. Intraoperative fluid management, positioning of epidural catheters and mode of intra and postoperative epidural analgesia remained at the discretion of the anaesthetist. At the time of placement, morphine and bupivacaine was used but in the postoperative period, bupivacaine was used alone. (Data as to the exact siting of catheters etc were not available and were dependent on the anaesthetist. This was not analysed.)
Patients were discharged when they met specific criteria to prevent inappropriate early discharge. These followed the principles set out by Fearon et al. 6 Following discharge, community nursing staff were trained to take final steps in removing ureteric stents and for practical stoma education if necessary. Finally, the ward staff, both medical and nursing, were available in case of any postoperative concerns. Routine telephone follow-up was completed in the first week following discharge.
Data collection and statistical analysis
As part of a prospective database, data on all patients undergoing a cystectomy were collected. These data included patient demographics (age, body mass index, co-morbidities), the procedure undertaken (open versus robotic assisted cystectomy and type of urinary diversion), perioperative outcomes (blood loss, intraoperative fluid administration, blood transfusion and operative time) and postoperative outcomes (time to nasogastric removal, time to mobilisation, time to bowel activity and total length of hospital stay).
Our primary outcome measures included duration of intensive care unit (ICU) stay and length of hospital stay. Secondary outcome measures included time to the passage of flatus and faeces, and time to mobilisation. Other measures included operation time and complications.
Data on mobilisation, passage of flatus and faeces were collected prospectively from both patients and nursing staff, and were entered into a database on the day in question. Nursing staff and patients were not made aware that data would be used subsequently in an analysis determining differences between cohorts in order to prevent bias.
Time to mobilisation was defined as the number of days after surgery until the patient was out of bed for more than six hours per day and at the same level of independence with respect to daily living as before surgery. Total hospital stay was defined as the number of nights spent in hospital after surgery, including nights after readmission within 30 days of surgery. Data on morbidity and mortality were determined from a combination of inpatient clinical stay records and review at subsequent outpatient visits. Data analysis was performed using Prism® (GraphPad Software, La Jolla, CA, US).
Baseline characteristics
Fifty-one consecutive patients (39 male, 12 female) underwent a cystectomy at our institution with the ERP. They were compared with 26 consecutive patients (21 male, 5 female) in the standard non-ERP group. The patient demographics of both cohorts are detailed in Table 2. Data were analysed with the unpaired t-test.
Table 2.
Baseline characteristics
| Non-ERP group (n=26) | ERP group (n=51) | p-value | |
|---|---|---|---|
| Age | |||
| Median (range) | 71.5 (49–85) | 68.0 (52–81) | |
| Mean (SD) | 69.8 (8.3) | 67.7 (7.8) | 0.48 |
| Male-to-female ratio | 21:5 | 39:12 | 0.54 |
| Body mass index | |||
| Mean | 26.5kg/m 2 | 27.5kg/m 2 | 0.849 |
| <18.5 (underweight) | 0 | 0 | – |
| 18.5–24.9 (normal) | 9 (35%) | 15 (29%) | 0.67 |
| 25–30 (overweight) | 13 (50%) | 25 (49%) | 0.79 |
| >30 (obese) | 4 (15%) | 11 (22%) | 0.28 |
| ASA grade 2 | 8 | 16 | 0.78 |
| ASA grade 3 | 18 | 35 | 0.83 |
| Preoperative grade | |||
| Grade 1 | 0 | 1 | 0.63 |
| Grade 2 | 1 | 4 | 0.12 |
| Grade 3* | 23 | 41 | 0.79 |
| Carcinoma in situ alone | 1 | 2 | 0.87 |
| Preoperative stage | |||
| <T2 | 12 | 17 | 0.79 |
| ≥T2 | 13 | 32 | |
| Previous open pelvic surgery | 1 | 0 | 0.68 |
| Open cystectomy | 26 | 51 | 0.78 |
| Ileal conduit | 24 | 48 | 0.47 |
| Neobladder | 2 | 3 | 0.32 |
ERP = enhanced recovery programme; SD = standard deviation; ASA = American Society of Anesthesiologists
One patient in the non-ERP group and two patients in the ERP group had a cystectomy for significant lower urinary tract symptoms and haematuria. One patient in the ERP group had a cystectomy for extensive adenocarcinoma of the bladder.
Almost 65% of patients in the non-ERP group were overweight or obese compared with 71% of patients in the ERP group. In addition, 60% of patients in the ERP group and 69% of non-ERP patients were categorised as ASA (American Society of Anesthesiologists) grade 3 due to the level of co-morbidities.
All patients in the non-ERP group underwent an open radical cystectomy as did all 51 patients in the ERP group. The main mode of urinary diversion was with an ileal conduit although a neobladder was the chosen form of diversion for two patients in the non-ERP group and three cases in the ERP group.
Results
Impact of the enhanced recovery programme
The introduction of the ERP at our institution produced significant improvements in several outcome measures (Table 3). These included the mean length of stay in the ICU (2.4 ±0.9 days vs 1.0 ±0.1 days, p=0.01), mean time to passage of flatus (6.2 ±0.4 days vs 4.6 ±0.2 days, p=0.0003) and faeces (7.4 ±0.5 days vs 6.1 ±0.3 days, p=0.013). Time to full oral diet and time to removal of nasogastric tube also improved significantly (p<0.05). Improvements in the duration of inpatient stay were also observed with the median stay falling from 11.5 days to 10.4 days although this was not statistically significant.
Table 3.
Comparison of outcome measures between patients with/without enhanced recovery programme (ERP)
| Non-ERP group (n=26) | ERP group (n=51) | p-value | |
|---|---|---|---|
| Total theatre time | 315 ±10 mins | 335 ±10 mins | 0.10 |
| Intraoperative transfusion | 1.6 ±0.6 units | 1.2 ±0.2 units | 0.46 |
| Total transfusion | 2.5 ±0.8 units | 1.8 ±0.2 units | 0.36 |
| Length of intensive care unit stay | 2.4 ±0.9 days | 1.0 ±0.1 days | 0.01 |
| Time to removal of nasogastric tube | 5.1 ±1.2 days | 2.0 ±0.3 days | 0.001 |
| Time to removal of intravenous fluids | 4.9 ±0.5 days | 3.6 ±0.3 days | 0.021 |
| Time to passage of flatus | 6.2 ±0.4 days | 4.6 ±0.2 days | 0.003 |
| Time to passage of faeces | 7.4 ±0.5 days | 6.1 ±0.3 days | 0.013 |
| Time to full oral diet | 5.9 ±0.3 days | 4.6 ±0.2 days | 0.002 |
| Median length of stay (range) | 11.5 days (7–24) | 10.4 days (6–62) | 0.66 |
| Mean length of stay (modified without outlier) | 12.9 days | 11.5 days | 0.32 |
Elements of the operation that were not dependent on the ERP did not differ significantly. These included fluid loss, intraoperative time and total transfusion volume.
Complications and readmission rates
Complications were recorded according to the Clavien– Dindo classification system, 14 and were similar in frequency and incidence. A breakdown of the complications is given in Table 4. Three individuals died following their cystectomy. All three patients had very high co-morbidity preoperatively. One individual was found to have bowel infarction away from the site of surgery and this was also in the context of significant co-morbidities. A significant proportion of complications were limited to requiring medical interventions such as antiemetics, analgesics or antibiotics. There were no readmissions in either group of patients.
Table 4.
Breakdown of Clavien complications for patients with/without enhanced recovery programme (ERP)
| Grade | Non-ERP group | ERP group |
|---|---|---|
| I |
n=3
3 – leakage from around wound |
n=4
2 – leakage from around wound 2 – high drain (nasogastric) output |
| II |
n=6
2 – myocardial infarction 1 – atrial fibrillation 1 – lower respiratory tract infection 1 – C difficile 1 – sepsis |
n=12
2 – atrial fibrillation 2 – ileus 2 – late pyrexia, given antibiotics 1 – postoperative chest pain 1 – pulmonary embolism 1 – elevated troponin I 1 – urinary tract infection 1 – vomiting 1 – ileus, C difficile, diarrhoea |
| IIIa |
n=1
1 – collection drained under local anaesthesia |
|
| IIIb |
n=1
1 – defunctioning colostomy |
n=1
1 – wound dehiscence |
| IVa |
n=1
1 – intensive care unit (bleeding due to excess anticoagulation) |
|
| IVb | ||
| V |
n=1
1 – respiratory sepsis |
n=1
1 – bilateral lower limb ischaemia |
Figures 1–4 show Kaplan–Meier plots demonstrating the relationships between the ERP and improvements in time to: removal of nasogastric tube (p=0.001), return of full bowel function (p=0.013), length of stay (p=0.66) and the length of stay following removal of one outlier (p=0.32).
Figure 1.
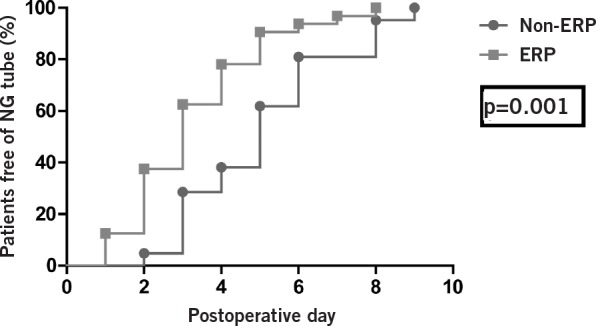
Kaplan–Meier plot demonstrating the relationship between the enhanced recovery programme (ERP) and improvements in time to removal of nasogastric (NG) tube
Figure 2.
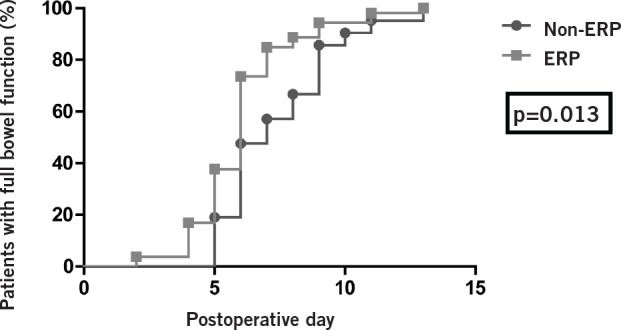
Kaplan–Meier plot demonstrating the relationship between the enhanced recovery programme (ERP) and improvements in time to return of full bowel function
Figure 3.
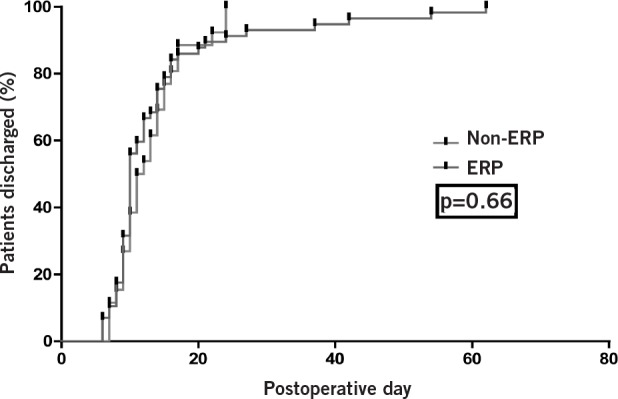
Kaplan–Meier plot demonstrating the relationship between the enhanced recovery programme (ERP) and improvements in length of stay
Figure 4.
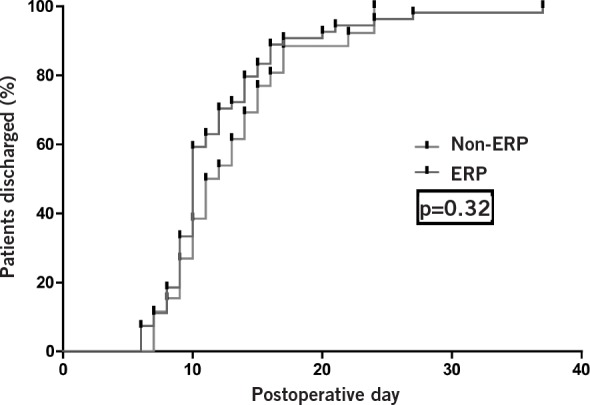
Kaplan–Meier plot demonstrating the relationship between the enhanced recovery programme (ERP) and improvements in length of stay following removal of one outlier
Discussion
The results from our study demonstrate the ability to introduce an evidence-based ERP successfully in a previously ‘orthodox’ urology unit, in the context of both open and robotic radical cystectomy. This study has demonstrated improvements in the length of ICU stay, time to passage of flatus and faeces, and time to return to full diet with the application of an ERP. The ERP cohort was also associated with an earlier discharge (albeit non-significant) from hospital with no increase in the complications or readmission rates. These key findings demonstrate that an ERP can be implemented successfully and safely, with potentially lower inpatient stays but with no increase in complications or readmissions.
ERPs involve the use of a multimodality approach to improve recovery after major surgical procedures. These are intended to reduce the surgical stress response and organ dysfunction, and therefore shorten the time to full recovery. The key features of the authors’ ERP emphasised the avoidance of nasogastric tubes and drains, early mobilisation and carbohydrate loading. However, what is the rationale for these steps?
Carbohydrate loading can be given safely up to two hours prior to surgery and is absorbed rapidly in the upper gastrointestinal tract. 8,9 This is thought to reduce intestinal dysfunction and, in turn, ileus. Meanwhile, the routine use of nasogastric tubes may increase the incidence of pneumonia and delay enteral feeding according to a large metaanalysis while the use of drains has also shown little advantage. 10,15,16 Early mobilisation is also key to patient recovery: bed rest increases muscle loss, impairs lung function and predisposes to thromboembolic disease. Moreover, as most surgeons are aware, immobility reduces bowel activity. Thus, the use of ERPs has gained increasing acceptance in colorectal surgery. Despite this, there is a paucity of literature in the role of ERPs in the context of radical cystectomy.
Hospital Episode Statistics show that the mean inpatient stay for radical cystectomy is 15.6 days, with a median of 12 days. 3 Moreover, Arumainayagam et al recorded a baseline median inpatient stay of 17 days, which improved to 13 days with an ERP in radical cystectomy. 12 Our study demonstrates further improvements can be achieved through the application of an ERP.
Our key outcome measure, the median length of stay, demonstrated an improvement from 11.5 days to 10.4 days in our study. However, this was not associated with improvements in the mean length of stay, primarily because of the presence of two outlying patients. While these patients were appropriate for discharge earlier in the course of their hospital stay, they had also experienced mishaps in their home environments (flood and fire), making them dependent on social services placement.
Although we have demonstrated significant benefits with this ERP in terms of reduction of ICU stay, improvements in time to return to full oral diet and bowel function, further improvements can be achieved by extending this programme. A logical next step would be to further reduce the use of opiate analgesics (in the form of patient controlled analgesia) in more than a fifth of the ERP cohort. Opiate analgesics are known to reduce bowel motility and are also known to have detrimental effects on the cough impulse and respiratory drive. Bowel motility can significantly affect gut activity while cough impulse and respiratory drive can increase the risk of respiratory complications.
Further improvements may also be seen with the introduction of rectus sheath catheters for analgesia but due to varying anaesthetic availability, this was not performed routinely. Nevertheless, as the relative advantages and disadvantages of this technique become known in comparison with epidurals, we may seek to integrate this mode of analgesia into our ERP.
A crude assessment of compliance with the ERP revealed that 39 of 51 patients followed the ERP in full. (Data not given.) Those patients where adherence was patchy were associated with the absence of the dedicated enhanced recovery nurse and also the introduction of a new team of junior medical staff. This could account for the absence of significant results for the ERP group. Further improvements through the introduction of an ERP nurse and the dissemination of knowledge of the ERP to junior team members of staff can help to produce greater improvements in length of stay. Maessen et al reported that familiarity with and acceptance of enhanced recovery, organisation and previous exposure to fast track concepts most strongly promoted reduced length of stay. 17 Poor postoperative compliance with the ERP was evidenced by the fact that almost a third of patients were not mobilised on day 1.
Moreover, decision making regarding the use of intraoperative fluid administration, opioid use and epidural anaesthesia was the domain of the anaesthetist. This agrees with previous studies that suggest that the degree of implementation of ERPs (and therefore their results) may be affected in relation to the size and complexity of the host institution. Changes in an organisational strategy require the cooperation of other healthcare professionals. This is all the more the case in the setting of a teaching institution, where more rigid structures are encountered as well as a greater number of professionals, making change more difficult to achieve. 18,19 This is seen most prominently during intraoperative and postoperative care; ERPs actively involve more disciplines, allied health professionals and junior medical staff. Therefore, action to improve protocol adherence may involve altering structures in surgical units, particularly with regard to the organisation and education of registrars and nurses. 17,20
Another reason for the lack of a significant change in length of stay could relate to the presence of a stoma as this is thought to have a variable effect on length of stay. King et al suggested that the presence of a stoma prolonged length of stay by 3–4 days while other work maintains that an ileostomy should not affect this outcome following open surgery. 21 Finally, the length of stay also reflects a multifactorial outcome: patient health and mobility, appropriate social support and confidence are all important factors prior to discharge. An absence of or a lack of certainty in any one of these parameters can prevent prompt discharge and so it is key that this is addressed appropriately.
Conclusions
This study further highlights the need for rigorous adherence to ERPs in the postoperative phase in order to improve recovery rates. Methods to improve postoperative ileus, motivation and mobility are central in improving outcomes, especially length of stay. Moreover, a greater understanding of the ERPs by all grades of the multidisciplinary team is likely to yield more efficacious results. Further analysis will undoubtedly reveal that ERPs will yield significant improvements in peri and postoperative urological outcomes.
References
- 1.Cancer Statistics Registrations, England, Series MB1 No. 41, 2010. Office for National Statistics. http://ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-262496 (cited January2013).
- 2.Mortality Statistics: Deaths Registered in England and Wales (Series DR), 2010. Office for National Statistics. http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-230730 (cited January2013).
- 3.Main procedures and interventions: 3 character 2011–12. Hospital Episode Statistics. http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=205 (cited January2013).
- 4.Andersen J, Hjort-Jakobsen D, Christiansen PS, Kehlet H. Readmission rates after a planned hospital stay of 2 versus 3 days in fast-track colonic surgery. Br J Surg 2007; 94: 890–893. [DOI] [PubMed] [Google Scholar]
- 5.Gouvas N, Tan E, Windsor Aet al Fast-track vs standard care in colorectal surgery: a meta-analysis update. Int J Colorectal Dis 2009; 24: 1,119–1,131. [DOI] [PubMed] [Google Scholar]
- 6.Fearon KC, Ljungqvist O, Von Meyenfeldt Met al Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr 2005; 24: 466–477. [DOI] [PubMed] [Google Scholar]
- 7.Ljungqvist O, Søreide E. Preoperative fasting. Br J Surg 2003; 90: 400–406. [DOI] [PubMed] [Google Scholar]
- 8.Nygren J, Thorell A, Jacobsson Het al Preoperative gastric emptying. Ann Surg 1995; 222: 728–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brunetto AL, Pearson AD, Gibson Ret al The effect of pharmacological modification of gastric emptying and mouth-to-caecum transit time on the absorption of sugar probe marker molecules of intestinal permeability in normal man. Eur J Clin Invest 1990; 20: 279–284. [DOI] [PubMed] [Google Scholar]
- 10.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997; 78: 606–617. [DOI] [PubMed] [Google Scholar]
- 11.Hignett S, Parmar CD, Lewis Wet al Ileostomy formation does not prolong hospital length of stay after open anterior resection when performed within an enhanced recovery programme. Colorectal Dis 2011; 13: 1,180–1,183. [DOI] [PubMed] [Google Scholar]
- 12.Arumainayagam N, McGrath J, Jefferson KP, Gillatt DA. Introduction of an enhanced recovery protocol for radical cystectomy. BJU Int 2008; 101: 698–701. [DOI] [PubMed] [Google Scholar]
- 13.Faiz O, Brown T, Colucci G, Kennedy RH. A cohort study of results following elective colonic and rectal resection within an enhanced recovery programme. Colorectal Dis 2009; 11: 366–372. [DOI] [PubMed] [Google Scholar]
- 14.Clavien PA, Barkun J, de Oliveira MLet al The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187–196. [DOI] [PubMed] [Google Scholar]
- 15.Cheatham ML, Chapman WC, Key SP, Sawyers JL. A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Ann Surg 1995; 221: 469–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kehlet H. Acute pain control and accelerated postoperative surgical recovery. Surg Clin North Am 1999; 79: 431–443. [DOI] [PubMed] [Google Scholar]
- 17.Maessen J, Dejong CH, Hausel Jet al A protocol is not enough to implement an enhanced recovery programme for colorectal resection. Br J Surg 2007; 94: 224–231. [DOI] [PubMed] [Google Scholar]
- 18.Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet 2003; 362: 1,225–1,230. [DOI] [PubMed] [Google Scholar]
- 19.Schwarzbach M, Hasenberg T, Linke Met al Perioperative quality of care is modulated by process management with clinical pathways for fast-track surgery of the colon. Int J Colorectal Dis 2011; 26: 1,567–1,575. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell RE, Lee BT, Cookson MSet al Immediate surgical outcomes for radical prostatectomy in the University HealthSystem Consortium Clinical Data Base: the impact of hospital case volume, hospital size and geographical region on 48,000 patients. BJU Int 2009; 104: 1,442–1,445. [DOI] [PubMed] [Google Scholar]
- 21.King PM, Blazeby JM, Ewings Pet al Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg 2006; 93: 300–308. [DOI] [PubMed] [Google Scholar]


