Abstract
Purpose
The objective of the present investigation was to test the feasibility and clinical utility of a real-time internet based protocol for remote, telefluoroscopic evaluation of oropharyngeal swallowing.
Method
This prospective cohort study evaluated 32 patients with a primary diagnosis of stroke or head/neck cancer. All patients participated in two separate fluoroscopic swallowing evaluations, one traditional on-site, and one telefluoroscopic off-site through the use of a telemedicine system. Agreement between sites was tested for three categories of variables: a) overall severity of swallowing difficulty b) presence and extent of laryngeal penetration and aspiration as rated by the eight-point Aspiration-Penetration scale and c) treatment recommendations.
Results
Results showed overall good agreement in subjective severity ratings (kappa = 0.636) and in Penetration-Aspiration Scale ratings (mean absolute difference 1.1 points) between the on-site and the off-site clinicians. Agreement in treatment recommendations was moderate to high ranging from 69.3% to 100%.
Conclusions
The present study supports the feasibility and clinical utility of a telemedicine system for evaluating oropharyngeal swallowing. Given the difficulty and expertise needed to complete such evaluations, this study offers promising clinical avenues for patients in rural, remote and under-served communities and countries where expert swallowing specialists are not available.
Keywords: deglutition, telemedicine, videofluoroscopy, dysphagia, swallowing
Introduction
Oropharyngeal dysphagia (OPD) results from a variety of medical conditions and can occur at any age (Logemann, 2007). OPD can result in respiratory complications, malnutrition, or even death (Bartlett, Gorbach, & Finegold, 1974; Johanson & Harris, 1980; Kirsch & Sanders, 1988; Mion, McDowell, & Heaney, 1994; Veldee & Peth, 1992). In addition to physical health and life threatening consequences, OPD can also limit an individual's ability to participate in the social interactions of everyday life, potentially leading to serious emotional consequences.
Due to these complications, it is important that all patients who are at risk for dysphagia receive an appropriate and comprehensive examination of swallowing function. Such an examination typically begins with a non-instrumental clinical evaluation (Perlman, Langmore, Milianti, Miller, Mills, & Zenner, 1991), i.e. a comprehensive head and neck physical and cranial nerve examination evaluating the structures and the physiology of all muscles and sensory areas involved in swallowing (Logemann, 1997; Palmer, Drennan, & Baba, 2000), as well as a screening for speech, language, or cognitive/awareness dysfunctions (Perlman, 1996). Following the non-instrumental clinical examination, when OPD is considered to be likely, patients generally receive a videofluoroscopic assessment of their swallowing function. Although other forms of assessment may be considered, the videofluoroscopic examination provides the most depth and breadth of information on the physiology of swallowing (Logemann, Rademaker, Pauloski, Ohmae, & Kahrilas, 1998) and is widely used (Palmer et al., 2000).
Despite the recognized value of this diagnostic method in the diagnosis of OPD, interjudge reliability of videofluoroscopic findings has not been high and there has been considerable variability across investigations (Becker, McLeroy, & Carpenter, 2005; Ekberg, Nylander, Fork, Sjöberg, Birch-Iensen, & Hillarp, 1988; Hind et al., 2009; Kuhlemeier, Yates, and Palmer, 1998; McCullough, Wertz, Rosenbek, Mills, Webb, & Ross, 2001; Scott, Perry, & Bench, 1998; Stoeckli, Huisman, Seifert, & Martin-Harris, 2003). Most studies have reported highest reliability for limited observations, such as the presence of aspiration and /or penetration (Becker et al., 2005; Ekberg et al., 1988; Hind et al., 2009; Kuhlemeier, Yates, and Palmer, 1998; Stoeckli et al. 2003;), Zenker's diverticulum (Ekberg et al., 1988), pharyngeal residue and cricopharyngeal opening (Kuhlemeier, Yates, and Palmer, 1998; McCullough et al., 2001). When raters are pretrained to criterion, interjudge reliability on videfluoroscopic observations does improve (Hind et al., 2009; Perlman, Booth, & Grayhack, 1994; Scott et al., 1998). Despite these variable reliability reports, videofluoroscopy is still considered by many as “the gold standard” in OPD evaluation (Logemann, 2007; Palmer et al., 2000).
Many geographic areas in the U.S. and around the world do not have adequately trained professionals to make this assessment technique available to all patients. This is particularly evident for many under-served communities where speech language pathologists (SLPs) with expertise in assessment of swallowing disorders are not available. In such cases, patients often travel long distances experiencing added discomfort and expense to obtain quality care (Pierrakeas, Georgopoulos, & Malandraki, 2005) or they do not receive appropriate evaluation and treatment.
In order to cover the needs of such patients, an internet system that permits real-time, remote, and interactive evaluation of oropharyngeal swallowing function was created (Perlman & Witthawaskul, 2002). This system, called the Teledynamic Evaluation Software System, (TESS) a detailed description of which is offered in Perlman and Witthawaskul (2002), has already been tested. In the present investigation this system was successfully used to collect data from a hospital in the state of Arkansas while directing the procedure from the University of Illinois at Urbana-Champaign (UIUC).
The objective of the present study was to test the feasibility and clinical utility of this internet based protocol. The overriding hypothesis stated that oropharyngeal swallowing function evaluated by an SLP using TESS would have an acceptable level of agreement with the evaluations performed by an SLP who is present in the fluoroscopy suite and using the traditional videofluoroscopic methodology. Based on the findings of previous research on reliability of videofluoroscopic assessments, validation of this overriding hypothesis was determined by the following secondary hypotheses: agreement for a) subjective ratings of severity, b) Penetration-Aspiration Scale scoring (Rosenbek, Robbins, Roecker, Coyle, & Wood, 1996), and c) treatment recommendation selection between the off-site (UIUC) clinician and the on-site (hospital) clinician will be compatible with that achieved in other reported investigations (moderate to high).
Methods
Patients
A total of 32 patients were recruited from the University of Arkansas for Medical Sciences (UAMS) Medical Center over a period of two years. Analysis for severity ratings included 30 subjects due to data entry errors for two subjects, however analysis for Penetration/Aspiration scale ratings and recommendations included all 32 participants. Patients had a primary diagnosis of either stroke or head/neck cancer and were between 50 and 75 years of age. All individuals with a history of neurodevelopmental or congenital anatomical disorders, moderate or advanced stage dementia, Type I diabetes, progressive neurological disease, or traumatic brain injury were excluded. All recruited subjects gave written consent to participate. This investigation was approved by the UIUC Institutional Review Board and the UAMS Institutional Review Board.
System Configuration
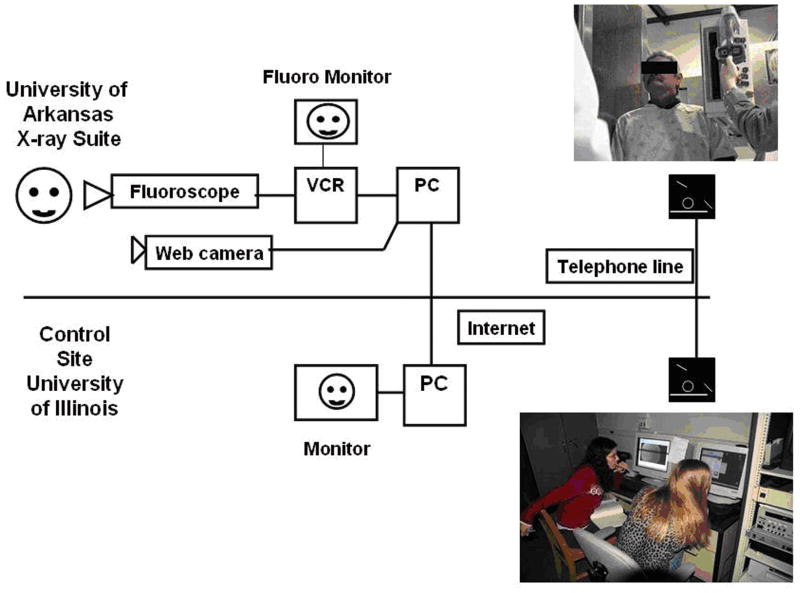
TESS has been described in detail (Perlman and Witthawaskul, 2002). In short, the system consists of two main components (Figure 1). A Dell PC-server located in the UAMS hospital fluoroscopy suite is connected to the fluoroscope output and is termed the ‘VIC’, videofluroscopic computer. The video signals can be captured onto the VIC and simultaneously transmitted in lossy format over the network in real time. Full-resolution video images are stored on the VIC. A second computer, termed CAC (control and analysis computer), which is located at the UIUC Swallowing Research Laboratory, has capabilities of managing the video capture process while the examination is occurring at the remote hospital, directing the transmission of the stored images at the end of the videofluoroscopic examination and analyzing the examination data after data transmission is completed. The VIC and CAC communicate through a broadband internet connection. No personal identifying information is transmitted through this medium.
Figure 1.
System configuration.
A web camera placed in the hospital x-ray suite allows for viewing of a patient by the off-site clinician. This allows the offsite clinician to remotely observe the patient's method of ambulation, posture, and level of alertness. With use of a speaker telephone, the remote clinician also hears samples of the patient's speech, voice, and language and allows for communication with the patient, the radiologist, and the onsite SLP—thus conforming to the Health Insurance Portability and Accountability Act (HIPAA) regulations.
Clinicians-Raters
Two experienced SLPs, certified by the American Speech-Language-Hearing Association (ASHA), at UAMS and one SLP doctoral candidate at UIUC served as the clinicians-evaluators. Clinicians 1 and 2 (C1 and C2) from UAMS directed and evaluated the on-site traditional videofluoroscopic assessments in Arkansas. Clinicians 1 and 2 had multiple years of clinical experience in evaluating patients with swallowing disorders (Clinician 1: 12 years of dysphagia evaluation and treatment experience; Clinician 2: 10 years of dysphagia evaluation and treatment experience). Clinician 3 (C3) from UIUC directed and evaluated all of the off-site telefluoroscopic evaluations. Clinician 3 (first author) was a doctoral student at the time and received rigorous training by the PI (last author) who is an expert in swallowing disorders, because she did not have as much clinical experience as the first two clinicians at that time. Before she could actively participate in this research, given her reduced level of training, she had to reach high level of agreement (>90%) in rating videofluoroscopic findings with the PI. Also, C1 and C2 from UAMS had reached a high level of agreement (>90%) in rating videofuoroscopic findings before the study initiation. Additionally, all raters had received a one-time (half day) training session for evaluation using the PA scale, and participated in monthly telephone conferences where issues and questions that arose by the clinicians were discussed.
Procedure
After a patient signed all consent forms, the assigned on-site clinician (C1 or C2) completed a detailed non-instrumental clinical examination (Perlman et al, 1991). Both case history information and results of the clinical examination were either transmitted via fax or telephone, to the off-site clinician (C3) depending upon time constraints. HIPAA regulations were followed throughout all aspects of data transmission and examination.
Patients consented to participate in two separate fluoroscopic evaluations of swallowing function, one traditional and one telefluoroscopic. The traditional videofluoroscopic evaluation was performed at the request of each patient's physician because of a concern for the presence of dysphagia. The traditional examination was directed and evaluated by an on-site clinician (either C1 or C2). The telefluoroscopic examination was performed by the UIUC clinician (C3). During the telefluoroscopic evaluation, another hospital clinician, not C1 or C2, was present. The responsibility of that clinician was to administer the boluses to the patient. This improved efficiency and helped ensure patient safety—as this clinician was allowed to interrupt the study methodology and ask the patient to cough if he/she deemed necessary.
Both evaluations were performed in the presence of a radiologist with no more than a 30 minute lapse between studies. In most instances, order of evaluation, traditional or telefluoroscopic, was randomized; however, on occasion, this randomization was broken based on patient health status, hospital staffing constraints, and other time constraints imposed by normal clinical care. The onsite clinicians recorded their examinations onto SVHS videotape. Lossless images were transferred to the UIUC laboratory for analysis of the digital recordings by C3. C1 and C2 evaluated the examination that he/she had directed on site. C1 rated 25 evaluations and C2 rated the remaining 7 evaluations. This difference was based on the availability of the clinicians. Despite this difference, C1 and C2 had very high reliability ratings (>90% across all measurement categories) prior to study initiation. Clinician 3 (the remote clinician) rated all the evaluations she directed (all 32). A set videofluoroscopic protocol was not used for this research study, because it would limit the applicability of the study, however, all comparisons on observations, and PA scale ratings were made only across the same consistencies of presented materials for each patient.
Variables Examined
Evaluation and recommendation forms were completed by both the on-site and off-site clinicians for each patient. Because there were two different studies performed for each patient, direct reliability between diagnostic observations would not be meaningful. In the present study, the primary goal was to investigate whether evaluations will remain effective when a telemedicine system is used in lieu of the traditional videofluoroscopic examination. That is why the design of obtaining two separate examinations, one of each type, was used. This paradigm of performing two separate assessments, also, was required for NIH approval for two reasons. First, according to the NIH, if the same clinician directed and analyzed both data sets, the results could have been biased because the clinician is likely to be influenced in the second evaluation by what they learn from the same patient during the first examination. Secondly, according to NIH, the direction/instruction of the videofluoroscopic evaluation can influence reliability itself. Thus, each clinician had to direct and evaluate the examinations they completed. Otherwise the non-directing reviewer would be influenced by the one directing the study.
Agreement was tested for three variable categories: a) overall subjective severity of swallowing difficulty, rated on a four point scale ranging from normal to severe (1=Normal, 2=Mild, 3=Moderate, 4=Severe); overall severity was rated twice by each clinician, once without taking into consideration interventions tested during the swallow examination, and once after considering whether and how the patient's condition changed when interventions were applied; b) presence and extent of laryngeal penetration and aspiration as rated by the eight-point Aspiration-Penetration scale (Rosenbek, Robbins, Roecker, Coyle, & Wood, 1996); and c) clinician treatment recommendations. Table 1 displays grouped and individual recommendation options.
Table 1.
Individual and group recommendations.
| Groups of Recommendations (N=9) | Individual Recommendations (N=29) |
|---|---|
|
| |
| Reducing or Eliminating Oral Intake | Diet NPO |
| Diet NPO except for treatment with SLP | |
| Diet PPO | |
|
| |
| Altering meal habits | Control bolus size |
| Control rate | |
| Follow solids w/ liquids | |
| Multiple swallows | |
|
| |
| Medication administration method | Alter medication administration method |
|
| |
| Control bolus viscosity (dietary changes) | Thickened liquids |
| Softer solid diets | |
|
| |
| Postural adjustments | Chin tuck |
| Head turn right | |
| Head turn left | |
| Head tilt right | |
| Head tilt left | |
|
| |
| Laryngeal closure maneuvers and exercises | Supraglottic swallow (safe swallow) |
| Glottal closure exercises | |
|
| |
| Strengthening Maneuvers and Exercises and Range-Of-Motion Exercises | Effortful swallow |
| Masako maneuver | |
| Mendelsohn maneuver | |
| Shaker exercise | |
| Oral strengthening | |
| ROM exercises | |
|
| |
| Sensory enhancement | Thermal-tactile application |
|
| |
| Referrals | Referral to GI |
| Referral to ENT | |
| Referral to pulmonary | |
| Referral to dental | |
| Referral to neurology | |
Note. NPO = nothing by mouth; SLP = speech-language pathologist; PPO = partially by mouth; ROM = range of motion; GI = gastrointestinal specialist; ENT = ear–nose–throat specialist.
Clinicians rated their recommendations as Class 1 or Class 2; 1 referring to primary recommendations that the patient should start following immediately after the swallow examination was completed and 2 referring to recommendations that could also be considered but were not their first choices. Only recommendations that were rated as Class 1 were analyzed in this study. Any recommendation that was not chosen as a Class 1 recommendation had the potential of being a Class 2. Thus, all recommendations potentially could be rated as Class 1 or Class 2. The great majority of Class 2 recommendations, however, were recommendations of the “Altering Meal Habits” category—that is, recommendations such as follow solids with liquids, control rate, control bolus size, and multiple swallows.
Results
Overall Severity Ratings Agreement
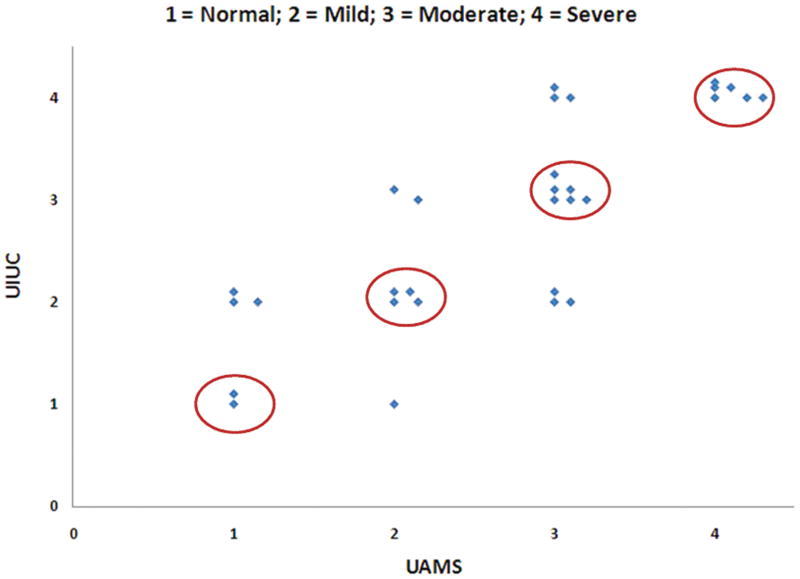
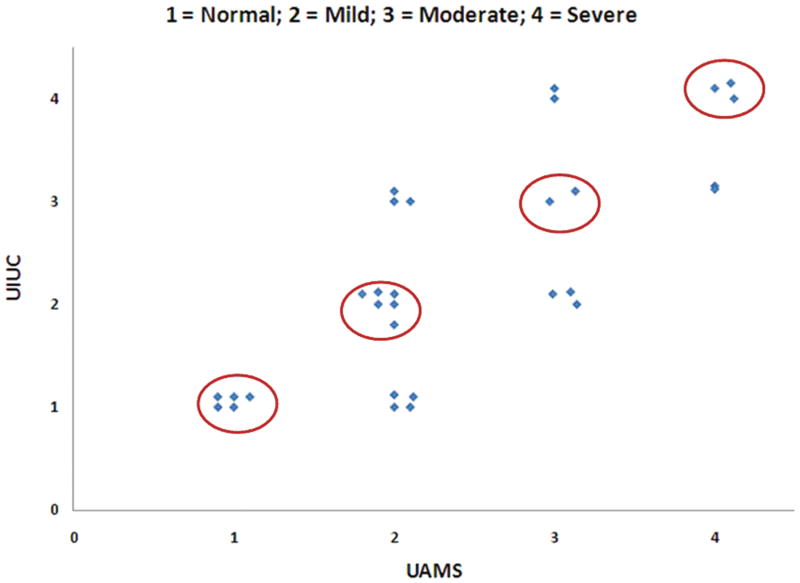
We hypothesized that agreement of the subjective rating of severity between the off-site (UIUC) clinician and the on-site (hospital) clinician would be moderate to high. Contingency results of overall severity ratings between the two sites without and with interventions taken into consideration are reported in Figures 2 and 3 respectively. When interventions were not taken into consideration, exact agreement between the UIUC clinician (C3) and the AR clinicians (C1 or C2) was achieved in 18/30 subjects (60%, weighted kappa= 0.636, good agreement). When interventions were taken into consideration, exact agreement was achieved in 16/30 subjects (53%, weighted kappa = 0.553, moderate agreement). In both conditions, disagreement was always within 1-point in the 4-point scale. The disagreements were evenly distributed between the off-site and on-site raters.
Figure 2.
Contingency results of severity ratings WITHOUT interventions between University of Arkansas for Medical Sciences (UAMS) and University of Illinois at Urbana-Champaign (UIUC). Circled ratings designate exact agreement.
Figure 3.
Contingency results of severity ratings WITH interventions between UAMS and UIUC. Circled ratings designate exact agreement.
Penetration-Aspiration (PA) Scale Scores Agreement
We also hypothesized that Penetration/Aspiration (PA) Scale score agreement between the off-site and the on-site clinicians would be moderate to high. On this 8-point scale, clinicians rated the most severe score for each consistency presented to the patients. Across all subjects the mean absolute difference in PA ratings between the two sites was 1.1 points (SD 1.4 points). Exact agreement was achieved in 10/32 subjects’ PA ratings. The difference was more than 2 points for only four subjects. It must be noted that for these four subjects the PA scores were consistently higher (worse) during the second evaluation, indicating a possible fatigue effect.
To further examine whether a fatigue factor was present in the overall study and could explain differences seen in severity ratings, a two-way Analysis of Variance (ANOVA) was used to estimate the effects of the order of examinations, and the site/clinician effect (UAMS vs. UIUC). After adjusting for the site/clinician effect, the second examination had a PA Scale score that was only slightly higher than the first examination (a difference of 0.12 points) and was not statistically significant.
Recommendations Agreement
We also hypothesized that agreement in treatment recommendations between the off-site and the on-site clinicians would be moderate to high. There were a total of 29 possible recommendations that clinicians could potentially select for each subject. These were grouped into 9 recommendation categories (Table 1). Table 2 displays the number of discrepancies/disagreements, the percent agreement, and the 95% confidence intervals (CI) for the percent agreement in each group category. To examine whether these levels of agreement were comparable to levels of agreement achieved on recommendation ratings by two clinicians rating the same examination of the same patient, C2 analyzed the videofluoroscopic swallow examinations of four randomly selected subjects who were also evaluated and analyzed by C1. In those four subjects the overall disagreement portion across the 29 possible recommendations was approximately 15%. The overall disagreement rate is 14.23% (see Table 2). Thus, this overall rate is essentially the same as the one achieved by two clinicians evaluating the same assessments without the use of telemedicine.
Table 2.
Recommendation groups, number of discrepancies/disagreements, percentage of agreement and 95% CIs for the percentage of agreement.
| Recommendation group | Number of Discrepancies/Disagreements | % Agreement | 95% CI for the percentage of agreement | |
|---|---|---|---|---|
| Upper bound | Lower bound | |||
| Reducing or eliminating oral intake | 7/32 | 78.1 | 0.89 | 0.61 |
| Altering meal habits | 10/32 | 68.8 | 0.82 | 0.51 |
| Medication administration method | 1/32 | 96.9 | 1.00 | 0.84 |
| Control bolus viscosity | 6/32 | 81.2 | 0.91 | 0.65 |
| Postural adjustments | 5 /32 | 84.4 | 0.93 | 0.68 |
| Laryngeal closure maneuvers and exercises | 4/32 | 87.5 | 0.95 | 0.72 |
| Strengthening and ROM exercises and maneuvers | 2 /32 | 93.7 | 0.98 | 0.80 |
| Sensory enhancement | 0/32 | 100 | 1.00 | 0.89 |
| Referral to physicians | 6/32 | 81.2 | 0.91 | 0.65 |
Discussion
The aim of the present investigation was to test the feasibility and clinical utility of an internet based protocol for real-time, remote, telefluoroscopic evaluation of oropharyngeal swallowing function. Specifically, it was hypothesized that oropharyngeal swallowing function evaluated by an SLP using TESS would have an acceptable level of agreement with evaluations performed by an SLP present in the fluoroscopy suite using traditional videofluoroscopic methodology. The overall results of the present investigation support the hypothesis of this study.
Results showed that agreement between subjective severity ratings was exact for 60% of the patients evaluated and within 1-point of disagreement (in a 4-point scale) for all other subjects. Additionally, the mean absolute difference in the 8-point PA scale scores provided for all subjects was only 1.1. These levels are comparable to, if not better than, levels of agreement other studies have found when two or more clinicians evaluate the same videofluoroscopic swallow evaluations (Becker et al., 2005; Kuhlemeier et al., 1998; McCullough et al., 2001; Stoeckli et al., 2003).
Pre-training to criterion has shown improvement in reliability scores in previous studies (Hind et al., 2009; Perlman et al., 1994; Scott et al., 1998). In the present investigation, raters had received a one-time (half day) training session for evaluating with the PA scale but no training for severity ratings and recommendations. Pre-training may have contributed to the high reliability with PA ratings.
The PA scale score discrepancy of more than 2 points—observed for four out of the 32 patients—may be explained by several factors. First, clinicians were evaluating two different studies for each patient. Thus, different swallows are being assessed by each clinician. Additionally, these four patients had consistently higher PA ratings in their second swallowing evaluation. The effect of the order of examination was not statistically significant across all subjects; nonetheless, this clinical observation for these four patients with more than two points difference may indicate that they exhibited a more severe clinical picture during their second evaluation. This possible “fatigue” effect might be of clinical interest—as it may indicate how fatigue can impact a patient's meal time swallowing function within a time frame of less than an hour. Kays and colleagues identified tongue strength and endurance as significantly reduced at the end of a small meal in both young and older healthy adults (Kays, Hind, Gangnon, & Robbins, 2010). Further investigation is warranted to identify if such an effect can have significant implications for treatment planning and recommendations. Additional factors that may explain this discrepancy include randomness and individual variability as seen in other studies even within the same videofluoroscopic swallow examination, (Robbins, Coyle, Rosenbek, Roecker, & Wood, 1999), slight differences that may have occurred in the clinician's instructions from one study to the next; and minimal differences in study protocol.
For most of the patients, however, the results show moderate to high agreement. This finding is important, not only because it shows clinical agreement, but also indicates patient stability (for most subjects). If patients were so variable in two short videofluoroscopic studies that occurred within short time frames on the same day, then the functionality and utility of these examinations in general would be at stake. Overall, our results suggest that patients can be rated by different clinicians, in different studies performed on the same day and still exhibit similar symptoms. This suggests both clinical agreement and patient stability.
The present investigation was one of the few that has examined agreement levels in the recommendations and interventions provided to patients by two clinicians performing two studies. Agreement within recommendation category was moderate to high, however if one were to evaluate by specific recommendation, certain discrepancies would be noted. Most are attributable to clinician's training, clinical opinion and experiences. For example, the on-site clinicians tended to recommend the head turn postural adjustment for people with unilateral pharyngeal paresis or paralysis, and the off-site clinician tended to recommend the head tilt. Both interventions target similar underlying pathologies. Thus, discrepancies in specific recommendations can be explained as differences in clinician's clinical training, experiences, opinion or knowledge of patient history.
Telemedicine Technical Challenges for Evaluation of Swallowing Function
Evaluating swallowing function is one of the more challenging and important responsibilities of a hospital-based SLP. The addition of a telemedicine option may add a few challenges. Technical difficulties faced by the investigators, as well as solutions that were developed, are listed below.
With the current software, a 1-2 second delay occurred during the online transmission. Given that the duration of the pharyngeal stage of a normal swallow is less than 1 second, this delay, although minimal, could impact interpretation and potentially, swallowing safety. To overcome this issue, another SLP (not C1 or C2) was always on site during a telefluoroscopic evaluation. This SLP was responsible for completing the orders given by the off-site clinician and for securing safety of the patient. Specifically, they were not allowed to overrule the off-site clinician's orders in any way, except in one condition: if the patient aspirated and did not cough, and the offsite clinician did not ask them to cough in sufficient time. At that point, the onsite clinician could intervene and instruct the patient to cough. In a real life situation, an SLP would typically not be on site during a telefluoroscopic evaluation; thus, prior training of the radiologist and/or radiology technician would be most advisable.
Another limitation of the present investigation was that the remote examiner had access to basic medical history information that was transmitted to them through fax, but they did not have access to the entire medical record. This was not possible, due to hospital regulations at the time of study completion. This should definitely be addressed in future studies and access to full medical record of the patients should be allowed for optimal assessments to be completed.
Quality of the images during online transmission was often reduced, making it difficult for the off-site clinician to perform the online evaluation at the desirable level of image precision. Possible reasons for this phenomenon could be internet connectivity difficulties, overload of internet transmissions at high use times, or radiologic and/or computer equipment failures. During a videofluoroscopic swallowing assessment, the clinician has to make decisions quickly and efficiently. Decisions about next steps are mainly dictated by what was just observed. Thus, quality of images is essential for correct decisions to be made rapidly. To avoid image quality online transmission issues, clinicians were trying to complete their examinations during times of the day that internet connection was not overloaded (e.g. early in the morning).
A few human errors/equipment failures also occurred and usually required small interventions, such as re-starting of equipment, replacement of backup batteries, or securing complete connection of cables. All of these problems can be addressed and improved as internet transmission and overall technology continues to improve.
Clinical Implications and Conclusions
The present investigation showed overall good agreement for both evaluation and recommendation ratings performed by two clinicians, one on-site with the patient and one off-site performing the evaluation via an internet based protocol. This is the first study to document the feasibility, applicability and clinical utility of a telemedicine system for evaluating oropharyngeal swallowing function. Given the difficulty, education and expertise needed to complete oropharyngeal swallowing evaluations, our findings offer promising clinical avenues for patients in rural, small, remote and under-served communities and countries where expert speech pathologists and swallowing specialists are not available.
Appropriate and timely evaluation of oropharyngeal dysphagia is critical for high quality management of a potentially life-threatening condition. The protocol presented and tested in this study can offer a useful means for remotely evaluating swallowing function in cases that expert specialists are not available on-site. Further testing of this system between clinicians in different countries and through the use of different modalities (e.g. Fiberoptic Endoscopic Evaluation of Swallowing, FEES) will provide broader clinical application and will improve diagnostic management of dysphagia globally. Future studies examining the short- and long-term outcomes of patients evaluated through TESS would provide important information on the therapeutic effects and life long outcomes and would expand the utility of this system.
Acknowledgments
This work was supported by the RO1 DC005603-01A2 awarded to the last author by the National Institute of Deafness and Communication Disorders of the National Institutes of Health.
The authors wish to thank Wee Witthawaskul, Juan Shen and Jaime Olson, for their great help in data acquisition and analysis.
References
- Agresti A, Coull BA. Approximate is better than “exact” for interval estimation of binomial proportions. American Statistician. 1998;52:119–126. [Google Scholar]
- Bartlett JG, Gorbach SL, Finegold SM. The bacteriology of aspiration pneumonia. American Journal of Medicine. 1974;56(2):202–207. doi: 10.1016/0002-9343(74)90598-1. [DOI] [PubMed] [Google Scholar]
- Becker S, McLeroy KE, Carpenter MA. Reliability of observations from modified barium swallow studies. Journal of Medical Speech and Language Pathology. 2005;13(2):97–108. [Google Scholar]
- Ekberg O, Nylander G, Fork FT, Sjöberg S, Birch-Iensen M, Hillarp B. Interobserver variability in cineradiographic assessment of pharyngeal function during swallow. Dysphagia. 1988;3(1):46–48. doi: 10.1007/BF02406279. [DOI] [PubMed] [Google Scholar]
- Hind JA, Gensler G, Brandt DK, Gardner PJ, Blumenthal L, Gramigna GD, Kosek S, Lundy D, McGarvey-Toler S, Rockafellow S, Sullivan PA, Villa M, Gill GD, Lindblad AS, Logemann JA, Robbins J. Comparison of trained clinician ratings with expert ratings of aspiration on videofluoroscopic images from a randomized clinical trial. Dysphagia. 2009;24(2):211–217. doi: 10.1007/s00455-008-9196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johanson WG, Jr, Harris GD. Aspiration pneumonia, anaerobic infections, and lung abscess. Medical Clinics of North America. 1980;64(3):385–394. doi: 10.1016/s0025-7125(16)31599-1. [DOI] [PubMed] [Google Scholar]
- Kays S, Hind J, Gangnon R, Robbins J. Effects of dining on tongue endurance and swallowing-related outcomes. Journal of Speech, Hearing and Language Research. 2010 doi: 10.1044/1092-4388(2009/09-0048). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirsch CM, Sanders A. Aspiration pneumonia. Medical management. Otolaryngology Clinics of North America. 1988;21(4):677–689. [PubMed] [Google Scholar]
- Kuhlemeier KV, Yates P, Palmer JB. Intra- and interrater variation in the evaluation of videofluorographic swallowing studies. Dysphagia. 1998;13(3):142–147. doi: 10.1007/PL00009564. [DOI] [PubMed] [Google Scholar]
- Logemann JA. Oropharyngeal dysphagia and nutritional management. Current Opinion in Clinical Nutrition and Metabolic Care. 2007;10(5):611–614. doi: 10.1097/MCO.0b013e328285d872. [DOI] [PubMed] [Google Scholar]
- Logemann JA, Rademaker AW, Pauloski BR, Ohmae Y, Kahrilas PJ. Normal swallowing physiology as viewed by videofluoroscopy and videoendoscopy. Folia Phoniatrica Logopedica. 1998;50(6):311–319. doi: 10.1159/000021473. [DOI] [PubMed] [Google Scholar]
- McCullough GH, Wertz RT, Rosenbek JC, Mills RH, Webb WG, Ross KB. Inter- and intrajudge reliability for videofluoroscopic swallowing evaluation measures. Dysphagia. 2001;16(2):110–118. doi: 10.1007/PL00021291. [DOI] [PubMed] [Google Scholar]
- Mion LC, McDowell JA, Heaney LK. Nutritional assessment of the elderly in the ambulatory care setting. Nurse Practitioner Forum. 1994;5(1):46–51. [PubMed] [Google Scholar]
- Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. American Family Physician. 2000;61(8):2453–2462. [PubMed] [Google Scholar]
- Perlman A, Langmore SE, Milianti FJ, Miller RM, Mills RH, Zenner PM. Comprehensive clinical examination of swallowing function. Seminars in Speech and Language. 1991;12(3):246–254. [Google Scholar]
- Perlman AL. Dysphagia in stroke patients. Seminars in Neurology. 1996;16(4):341–8. doi: 10.1055/s-2008-1040992. [DOI] [PubMed] [Google Scholar]
- Perlman AL, Witthawaskul W. Real-time remote telefluoroscopic assessment of patients with dysphagia. Dysphagia. 2002;17(2):162–167. doi: 10.1007/s00455-001-0116-2. [DOI] [PubMed] [Google Scholar]
- Pierrakeas C, Georgopoulos V, Malandraki G. Online collaboration environments in telemedicine applications of speech therapy. Conference Proceedings IEEE Engineering in Medicine and Biology Society. 2005;2:2183–2186. doi: 10.1109/IEMBS.2005.1616895. [DOI] [PubMed] [Google Scholar]
- Robbins JA, Coyle JL, Rosenbek JC, Roecker EB, Wood JL. Differentiation of normal and abnormal airway protection during swallowing using the penetration-aspiration scale. Dysphagia. 1999;14:228–232. doi: 10.1007/PL00009610. [DOI] [PubMed] [Google Scholar]
- Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–98. doi: 10.1007/BF00417897. [DOI] [PubMed] [Google Scholar]
- Scott A, Perry A, Bench J. A study of interrater reliability when using videofluoroscopy as an assessment of swallowing. Dysphagia. 1998;13(4):223–227. doi: 10.1007/PL00009576. [DOI] [PubMed] [Google Scholar]
- Stoeckli SJ, Huisman TA, Seifert B, Martin-Harris BJ. Interrater reliability of videofluoroscopic swallow evaluation. Dysphagia. 2003;18(1):53–57. doi: 10.1007/s00455-002-0085-0. [DOI] [PubMed] [Google Scholar]
- Veldee MS, Peth LD. Can protein-calorie malnutrition cause dysphagia? Dysphagia. 1992;7(2):86–101. doi: 10.1007/BF02493439. [DOI] [PubMed] [Google Scholar]