Abstract
Objective. The latest European guidelines for the management of hemorrhagic shock suggest the use of vasopressors (norepinephrine) in order to restore an adequate mean arterial pressure when fluid resuscitation therapy fails to restore blood pressure. The administration of arginine vasopressin (AVP), or its analogue terlipressin, has been proposed as an alternative treatment in the early stages of hypovolemic shock. Design. A meta-analysis of randomized controlled animal trials. Participants. A total of 433 animals from 15 studies were included. Interventions. The ability of AVP and terlipressin to reduce mortality when compared with fluid resuscitation therapy, other vasopressors (norepinephrine or epinephrine), or placebo was investigated. Measurements and Main Results. Pooled estimates showed that AVP and terlipressin consistently and significantly improve survival in hemorrhagic shock (mortality: 26/174 (15%) in the AVP group versus 164/259 (63%) in the control arms; OR = 0.09; 95% CI 0.05 to 0.15; P for effect < 0.001; P for heterogeneity = 0.30; I 2 = 14%). Conclusions. Results suggest that AVP and terlipressin improve survival in the early phases of animal models of hemorrhagic shock. Vasopressin seems to be more effective than all other treatments, including other vasopressor drugs. These results need to be confirmed by human clinical trials.
1. Introduction
Trauma is the principal cause of death for people under 35 years of age, with more than 5 million injury-related deaths every year in the world. Approximately 30% of these deaths can be attributed to hemorrhagic shock [1, 2]. Untreated prehospital hemorrhagic shock is one of the leading causes of cardiac arrest [3, 4]. Appropriate management and treatment are necessary to prevent adverse events and outcomes [5–7]. The early phase of hemorrhagic shock is characterized by a vasoconstrictive response and if the shock is left untreated it can lead to vasodilation that does not respond to conventional resuscitation strategies [8, 9]. Prehospital hemorrhagic shock treatment should be focused on maintaining adequate mean arterial pressure (MAP) along with organ perfusion up until arrival at the hospital [10, 11].
Small volume resuscitation with colloids or hyperoncotic fluids may be useful during early phases of uncontrolled bleeding [12–14]. Recent international guidelines suggest that vasopressors may also be required to maintain tissue perfusion where fluid resuscitation itself does not achieve the expected goal [15].
Arginine vasopressin (AVP) is an endogenous neurohypophysial hormone with an antidiuretic function. The most important AVP release stimulus is the plasma osmolality variation followed by blood pressure variations [16–18]. AVP also suppresses nitric oxide (NO) production [19]. The AVP release may also be suppressed by increased levels of norepinephrine and the increased release of NO from vascular endothelium of the posterior pituitary gland [20, 21]. Terlipressin is a long-acting synthetic analogue of AVP, proposed in the septic shock management as a rescue therapy, when adequate MAP values are difficult to reach with standard therapy. It is characterized by a longer duration of action and a higher selectivity on the V1 receptors that limits the edemigenous effect mediated by the V2 receptors differently from what its native counterpart does [22]. AVP and terlipressin can be both used with the aim of reaching the desired MAP target or reducing the norepinephrine dosage [23, 24].
In animal models in which severe uncontrolled blood loss has been induced, the administration of AVP has shown improvement in survival, neurologic outcome, and enhanced hemodynamic performance [25–27]. During the irreversible phase of hemorrhagic shock, unresponsive to fluids and catecholamines administration, AVP can mediate peripheral vasoconstriction through V1 receptors [13, 28, 29]. AVP works primarily on arterioles in extracerebral tissues, with less constriction action on coronary and renal vessels with potential vasodilatory effect on cerebral and pulmonary flow [30]. Recent animal studies have shown that AVP treatment can achieve hemodynamic optimization during prehospital hemorrhagic shock, while fluids and catecholamines showed neither improvement of hemodynamic parameters nor survival [1, 31, 32].
AVP use is associated with some adverse effects such as ischemic complications especially in cardiac, splanchnic, and skin circulation [33]. The decreased gut perfusion may determine tissue necrosis with subsequent translocation of bacteria that promotes the development of sepsis in the postresuscitation phase [34]. The increased expression of the V1 receptor subtype in trauma brain injury might promote the development of cerebral edema [8, 35].
To evaluate the impact on survival of V1 receptor agonists in hypovolemic refractory shock, we conducted a systematic review and meta-analysis of data pooled from existing trials comparing AVP or terlipressin and conventional shock management in mammals.
2. Materials and Methods
2.1. Search Strategy
All randomized animal trials using AVP or terlipressin in hypovolemic shock were identified. Relevant studies were independently searched by two trained investigators in Google Scholar and PubMed (updated November 4, 2013). The full PubMed search strategy, including keywords AVP, arginine vasopressin, terlipressin, and hemorrhagic and hypovolemic shock, was developed according to Biondi-Zoccai et al. and is available in the Appendix [36].
2.2. Study Selection
References obtained from databases and literature searches were first examined independently at the title/abstract level by two investigators, with divergences resolved by consensus and then, if potentially pertinent, retrieved as a complete article.
Inclusion criteria for potentially relevant studies were random allocation to treatment; animal experimental design; comparison of AVP or terlipressin (with or without fluid administration) versus placebo or fluids or catecholamines or both fluids plus catecholamines. Exclusion criteria were duplicate publications, human trials, and studies with no data on survival. Two investigators selected studies for the final analysis by independently assessing compliance to the selection criteria. Divergences from the selection criteria were resolved by consensus.
2.3. Data Abstraction and Study Characteristics
Two investigators independently extracted data on the study design, experimental setting, dosages of AVP or terlipressin, and experimental duration, with divergences resolved by consensus. If the required data could not be retrieved from the published report, at least two separate attempts to contact the original authors were made.
The primary end-point was mortality at the longest available follow-up. In addition, we performed further subanalysis comparing animals treated with AVP (or terlipressin) with those treated, respectively, with placebo, fluid resuscitation, and other vasoconstrictive drugs.
2.4. Data Analysis and Synthesis
Computations were performed with RevMan 4.2 [35]. Binary outcomes from individual studies were analyzed to compute individual odds ratios (ORs) with pertinent 95% confidence intervals (CIs), and a pooled summary effect estimate was calculated by means of the Mantel-Haenszel method and the fixed effect model in case of low statistical inconsistency (I 2 < 25%) or the random-effect model in case of moderate or high statistical inconsistency (I 2 > 25%) [37]. Statistical heterogeneity and inconsistency were measured using Cochran Q tests and I 2 (by Higgins and Thompson), respectively [38]. Statistical significance was set at 2-tailed 0.05 for hypothesis testing and at 0.10 for heterogeneity testing. According to Higgins et al., the I 2 values around 25%, 50%, and 75% were considered to represent, respectively, low, moderate, and severe statistical inconsistency [38].
The risk of publication bias was assessed by visual inspection of the funnel plot for mortality. Sensitivity analyses were performed by sequentially removing each study and reanalysing the remaining dataset (producing a new analysis for each study removed) and by analysing only data from studies with low risk of bias.
3. Results
3.1. Study Characteristics
Database searches, backwards snowballing, and contacts with experts yielded a total of 246 citations. After excluding nonpertinent titles or abstracts, 22 studies were retrieved in complete form and assessed according to the selection criteria (Figure 1). Seven studies were further excluded for the absence of survival data. Fifteen eligible trials were included in the final analysis.
Figure 1.
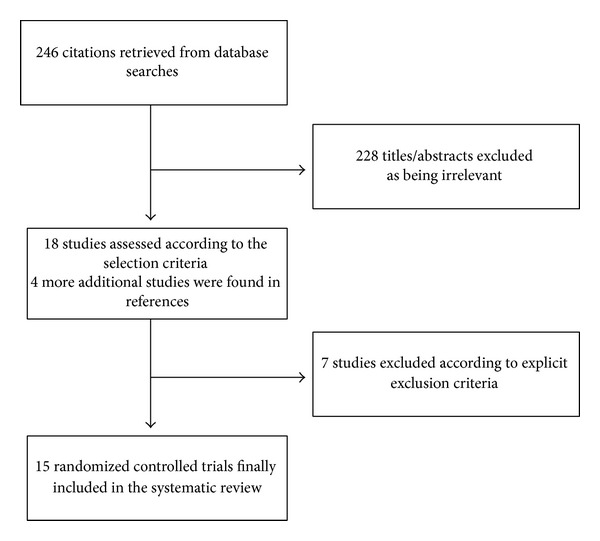
Flow diagram of the systematic review process.
The 15 included studies randomized 433 animals, 174 to AVP (14 trials) or terlipressin (one trial) and 259 to control (placebo, vasopressors, or fluid resuscitation). The included trials were conducted on pigs (12 studies) and on rats (three studies). All manuscripts were published in indexed journals. Detailed study characteristics are summarized in Table 1.
Table 1.
Studies included in the meta-analysis.
| 1st author | Journal | Year | Number of AVP (V) or terlipressin (T) | Number of Controls | Control | Animal |
|---|---|---|---|---|---|---|
| Bayram [3] | Am J Emerg Med | 2012 | 7 (T) | 14 | Placebo (7); Ringer lactate (7) |
Rats |
|
| ||||||
| Cavus [31] | Resuscitation | 2009 | 8 (V) | 8 | Fluid resuscitation (8) | Pigs |
|
| ||||||
| Cavus [55] | Resuscitation | 2010 | 8 (V) | 16 | Fluid resuscitation (8); noradrenaline + HS (8) |
Pigs |
|
| ||||||
| Dudkiewicz [56] | Crit Care Med | 2008 | 10 (V) | 10 | Phenylephrine (10) | Pigs |
|
| ||||||
| Feinstein [8] | J Am Coll Surg | 2005 | 14 (V) | 23 | Crystalloid (9); phenylephrine (5); crystalloid + phenylephrine (9) |
Pigs |
|
| ||||||
| Feinstein [32] | J Trauma | 2005 | 8 (V) | 9 | NS (9) | Pigs |
|
| ||||||
| Li [11] | J Surg Res | 2011 | 30 (V) | 40 | Placebo (10); Ringer lactate (10); whole blood (10); NE (10) | Rats |
|
| ||||||
| Liu [39] | Shock | 2013 | 32 (V) | 48 | Hypotensive resuscitation (16); Ringer lactate (16); NE (16) |
Rats |
|
| ||||||
| Meybohm [13] | J Trauma | 2007 | 7 (V) | 7 | HHS + NE (7) | Pigs |
|
| ||||||
| Meybohm [57] | Resuscitation | 2008 | 10 (V) | 20 | Fluid (10); HHS + NS (10) | Pigs |
|
| ||||||
| Raedler [10] | Anesth Analg | 2004 | 7 (V) | 14 | Saline placebo (7); fluid resuscitation (7) |
Pigs |
|
| ||||||
| Sanui [21] | Crit Care Med | 2006 | 5 (V) | 5 | Placebo (5) | Pigs |
|
| ||||||
| Stadlbauer [30] | Anesthesiology | 2003 | 9 (V) | 14 | Saline placebo (7); fluid resuscitation (7) |
Pigs |
|
| ||||||
| Stadlbauer [40] | Crit Care | 2007 | 7 (V) | 12 | Saline placebo (5); fluid resuscitation (7) |
Pigs |
|
| ||||||
| Voelckel [1] | Crit Care Med | 2003 | 7 (V) | 14 | Epinephrine (7); saline placebo (7) |
Pigs |
3.2. Quantitative Data Synthesis
The overall analysis showed that AVP/terlipressin were associated with a reduction in animal mortality (26/174 (15%) in the AVP/terlipressin group versus 164/259 (63%) in the control arms; OR = 0.09 (95% CI 0.05–0.15); P for effect < 0.001; P for heterogeneity = 0.30; I 2 = 14%) (Figure 2). When studies were grouped to either fluid resuscitation, placebo, norepinephrine, or other vasoconstrictive drugs as a comparator, administration of AVP/terlipressin was still associated with a reduction in mortality. (see Supplementary Figures 6(b)–6(e) available online at http://dx.doi.org/10.1155/2014/421291).
Figure 2.
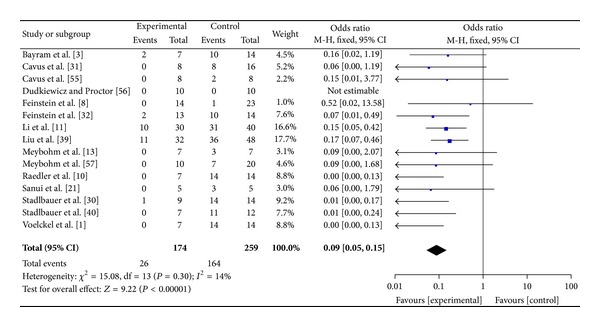
AVP or terlipressin versus all other strategies (fluid resuscitation, vasoconstrictors, and placebo).
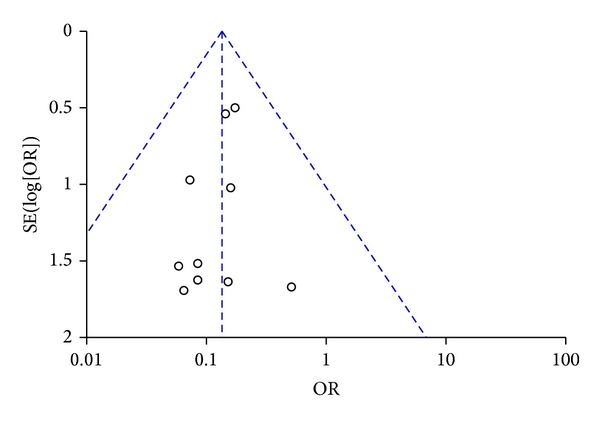
Visual inspection of funnel plot identified an asymmetrical shape, suggesting the presence of publication bias (Figure 3). Sensitivity analyses performed by sequentially removing each study and reanalysing the remaining dataset (producing a new analysis for each study removed) did not lead to major changes in direction or magnitude of statistical findings. Sensitivity analyses carried out with studies with low risk of bias (eliminating the studies responsible for the asymmetry of the funnel plot) confirmed the overall results of our work showing a reduction in mortality in AVP/terlipressin animals versus controls (OR = 0.13 (95% CI 0.08–0.24); P for effect < 0.001, P for heterogeneity 0.99, I 2 = 0% with 10 studies and 329 animals included) (Figures 4 and 5). Data of mortality are summarized in Table 2.
Figure 3.
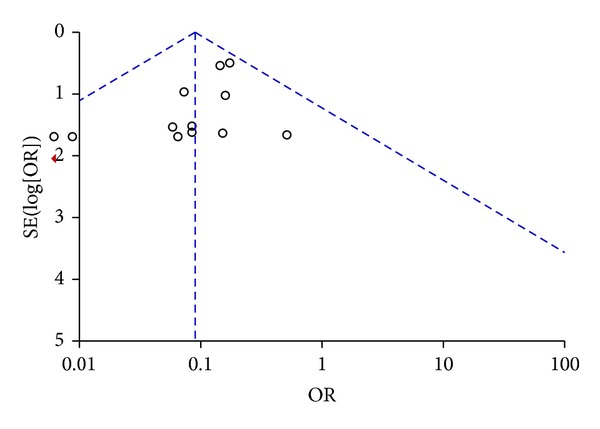
Funnel plot of comparison of AVP or terlipressin versus all other strategies (fluid resuscitation, vasoconstrictors, and placebo).
Figure 4.
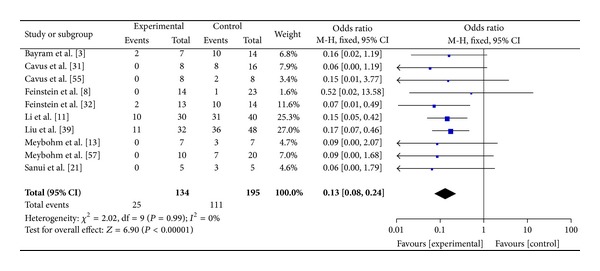
Forest plot of comparison of AVP or terlipressin versus all other strategies including studies with low risk of bias.
Figure 5.
Funnel plot of comparison of AVP or terlipressin versus all other strategies including studies with low risk of bias.
Table 2.
Results for mortality.
| Outcome | Number of included trials |
AVP/terlipressin animals |
Control animals |
OR | 95% CI | P for effect | P for heterogeneity | I 2 (%) |
|---|---|---|---|---|---|---|---|---|
| Overall trials | 15 | 174 | 259 | 0.09 | 0.05–0.15 | <0.001 | 0.30 | 14 |
| Mortality | 15% | 63% | ||||||
|
| ||||||||
| Placebo as comparator drug | 7 | 72 | 48 | 0.03 | 0.01–0.09 | <0.001 | 0.57 | 0 |
| Mortality | 18% | 92% | ||||||
|
| ||||||||
| Fluid resuscitation as comparator drug | 11 | 114 | 117 | 0.08 | 0.04–0.15 | <0.001 | 0.75 | 0 |
| Mortality | 18% | 67% | ||||||
|
| ||||||||
| Vasopressors (NE or epinephrine) as comparator drug | 7 | 88 | 87 | 0.18 | 0.08–0.44 | <0.001 | 0.96 | 0 |
| Mortality | 18% | 39% | ||||||
|
| ||||||||
| NE as comparator drug | 4 | 54 | 53 | 0.16 | 0.06–0.45 | <0.001 | 0.97 | 0 |
| Mortality | 20% | 47% | ||||||
|
| ||||||||
| Sensitivity analysis (including only low risk of bias studies) | 10 | 134 | 195 | 0.13 | 0.08–0.24 | <0.001 | 0.99 | 0 |
| Mortality | 18% | 57% | ||||||
In the majority of the studies included in this meta-analysis, AVP has been administered with an initial bolus followed by continuous infusion. Bolus doses ranged from 0.1 U/kg to 0.4 U/kg while continuous infusion dosages ranged from 0.04 U/kg/min to 0.08 U/kg/min. Other studies report AVP infusion dosages in U/kg/h that range from 0.1 [21] to 2 U/kg/h [39, 40]. In the study of Bayram et al., terlipressin was administered at the dose of 50 mcg/kg [3].
4. Discussion
The most important finding of this meta-analysis is that the use of AVP in the hypovolemic shock increases survival in animal studies. All studies included were randomized (AVP or terlipressin versus placebo, other vasopressors or fluid administration), were conducted on animal models (pig and rats), and were published in peer-reviewed journals.
The use of vasopressors in hypovolemic shock might contradict the conventional knowledge of how to treat this condition. Nevertheless their use in late phases of hemorrhagic shock is a common practice. Vasopressors have recently been suggested in the European guidelines for the management of hemorrhagic shock in order to maintain an adequate mean arterial pressure when fluid therapy gives no positive results [15, 41]. Guidelines recommend the use of norepinephrine as the vasopressor of choice, whilst the use of terlipressin or AVP is not mentioned.
The use of AVP and its synthetic analog terlipressin has received significant attention in clinical practice, especially in septic shock and cardiac arrest [43–46]. AVP was discovered in 1895 from the extract of the posterior pituitary gland and named after its vasoconstrictive properties [16, 42].
Landry et al. reported, for the first time, the successful administration of exogenous AVP in patients with septic shock [43]. Russell et al. compared the use of AVP versus norepinephrine in patients with septic shock in the “Vasopressin and Septic Shock Trial.”
In 779 patients the adverse effects were similar in both groups, with no differences in 28-day mortality and major organ dysfunction [44]. Another potential use of AVP is in the pharmacological treatment of cardiac arrest [45, 46]. AVP followed by epinephrine may be more effective than epinephrine alone in the treatment of refractory cardiac arrest, especially in patients with asystole [29].
In recent years, several animal studies have shown that the administration of AVP in patients with uncontrolled hemorrhagic shock is a promising treatment [10]. Our systematic analysis of literature has evaluated several clinical studies on animals. Morales et al. were the first ones to study the effects of the administration of different doses of AVP (from 1 to 4 mU/kg) in seven dogs undergoing prolonged hemorrhagic shock and concluded that AVP is an effective agent in the irreversible phase of hemorrhagic shock unresponsive to volume replacement and catecholamines [28].
For a long time the use of vasopressors in hemorrhagic shock was considered a debatable topic. During the early phases of hemorrhagic shock arterial pressure is maintained as adequate through the activation of compensatory vasoconstrictive mechanisms guaranteed by the sympathetic system that produces a venous and arterial compensatory vasoconstriction [41].
When blood loss is abundant and this mechanism is no longer efficient to maintain an adequate organ perfusion, the sympathetic system becomes inhibited with subsequent reduction of peripheral resistance and bradycardia. Hemorrhagic shock is also responsible for an abnormal vascular bed reaction mediated by nitric oxide that reduces the response to endogenous and exogenous norephineprine [47]. The trauma and organ damage developing from the shock-induced hypoperfusion bring about the activation of the inflammatory cascade with subsequent vasoplegia [48, 49].
The use of vasopressors may be helpful in these cases. In their retrospective study Plurad et al. determined that an early vasopressor exposure after a critical injury is independently associated with an increased mortality rate and this is not related to the volemic status where hypovolemic patients are those with values of central venous pressure ≤ 8 mmHg. In this retrospective study, vasopressor exposure was associated with death independent of injury severity. Vasopressor-treated patients had lower arterial pressure, required more fluids and transfusions, and had a higher serum creatine [50].
However the update of the European guidelines has recently considered the use of norepinephrine for irreversible hemorrhagic shock. There are several human case reports that have supported the use of AVP as an optimizing measure capable of supporting arterial pressure during the triage of trauma victims [27, 51].
At present, a multicenter, randomized controlled trial (Vasopressin in Traumatic Hemorrhagic Shock—VITRIS study) is being organized in Europe to evaluate the effects of AVP in prehospital management of hemorrhagic shock [52]. Unfortunately, as of now, we only have the results of retrospective studies on humans. Collier et al. conducted a retrospective cohort analysis of trauma patients requiring vasopressors within 72 hours of admission. They observed higher mortality (51% versus 41%) in patients treated with AVP concluding that its administration is associated with increased mortality in trauma patients with refractory hypotension [53]. However patients treated with AVP in this study have higher values of Trauma-Injury Severity Score (TRISS) and initial lactate levels. Arterial blood pressure values of these two groups are not reported. Grmec et al. performed a prehospital prospective cohort study to assess the influence of treatment with AVP and hydroxyethyl starch solution (HHS) on outcome in resuscitated blunt trauma patients with pulseless electrical activity (PEA) cardiac arrest. Thirty-one patients were studied concluding that victims of severe blunt trauma with PEA should be initially treated with AVP in combination with HHS for volume resuscitation followed by standard resuscitation therapy and other procedures when needed [54].
Studies conducted on animals have several limitations. Survival times measured in the experiments are different. The median value is 15.5 hours and the median is 1.5 hours. Few studies keep observing animals after six hours [11, 30]. Those studies are performed with different protocols in settings varying from head trauma [55, 56], thoracic trauma, and abdominal trauma [40] or after severe hepatic lesions [57].
Dosages used in animal trials are higher than dosages used in human studies. Humans have been successfully treated with AVP infusion of 2–4 U/h in vasodilatory shock [58, 59] and 10–20 UI boluses in patients with upper intestinal bleeding [60]. Most of the studies favorably estimate the impact of AVP to handle hemodynamic and improve survival. However it is recommended not to underestimate the possible adverse effects that might derive from the use of AVP since its use is only indicated in irreversible shock no longer treatable with fluid resuscitation alone. Vasopressin could be considered as a possible pharmacologic adjunct in patients with shock refractory to the administration of fluids and catecholamines but the use of AVP alone cannot replace the use of fluids [61]. The AVP, as well as other vasopressors, seems to be beneficial only when administered in association with fluids [62, 63].
5. Conclusions
Data acquired from our meta-analysis suggest strong scientific evidence for the efficacy of AVP for the early treatment of hemorrhagic shock in animal models. AVP has shown to be more effective than all other treatments, including other vasopressors drugs. We are awaiting the results of the VITRIS [50] study to confirm in humans the results obtained in animal studies.
6. Methodological Limitations
The purposes, designs, and conduct are different between systematic review and meta-analysis of preclinical and clinical studies. Clinical reviews are intrinsically confirmatory and the aim of a Cochrane review is to provide evidence to allow practitioners and patients to make informed decisions about the delivery of health-care. Animal studies are meant to be exploratory and do not lead to definitive conclusions directly applicable to humans [64].
The results shown should be interpreted with caution. Animal studies are inherently heterogeneous, more than the typical clinical trials. Successfully translating findings to human diseases depends largely upon understanding the sources of heterogeneity and their impact on effect size [64]. The study is conducted without randomized controlled trials in humans, and our findings should only be considered as a hypothetical suggestion for further research, awaiting the results of randomized controlled human trials.
Supplementary Material
In the supplemental materials we confronted AVP/terlipressin with different comparators singularly: fluid resuscitation (fig. 6a), placebo (6b), other vasoconstrictive drugs(6C) and norepineprhine(6d). In all the analysis we conducted AVP/terlipressin was associated to a reduction of the death rate. We also did a meta-analysis on survival considering separately the studies conducted on rats (fig. 7a) and on pigs (fig.7b). In fig.8 we considered only the studies where hemorrhagic shock was due to a splancnic bleeding. We then did a meta-analysis excluding those trials with zero mortality (fig. 9) and selecting the studies that had mortality as the primary end-point. In table 3 are reported the dosages of AVP, terlipressin, vasopressors and the total amount of fluids included in the studies in the meta-analysis. In table 4 are reported the primary end-points and the setting of the included studies.
Acknowledgment
The authors are indebted to Toby Schwartzbarth for the revision of the paper.
Appendix
(“Vasopressin”[MeSH Terms] OR terlipressin[Text Word] OR “arginine vasopressin”[Text Word]) AND (“hemorrhagic shock” OR trauma) AND ((randomized controlled trial[pt] OR controlled clinical trial[pt] OR randomized controlled trials[mh] OR random allocation[mh] OR double-blind method[mh] OR single-blind method[mh] OR clinical trial[pt] OR clinical trials[mh] OR (“clinical trial”[tw] OR ((singl∗[tw] OR doubl∗[tw] OR trebl∗[tw] OR tripl∗[tw]) AND (mask∗[tw] OR blind[tw])) OR (“latin square”[tw]) OR placebos[mh] OR placebo∗[tw] OR random∗[tw] OR research design[mh:noexp] OR comparative study[mh] OR evaluation studies[mh] OR follow-up studies[mh] OR prospective studies[mh] OR crossover studies[mh] OR control∗[tw] OR prospective∗[tw] OR volunteer∗[tw]) OR (animal[mh] OR human[mh]) NOT (comment[pt] OR editorial[pt] OR (meta-analysis[pt] NOT clinical trial[pt]) OR practice-guideline[pt] OR review[pt]))).
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Voelckel WG, Raedler C, Wenzel V, et al. Arginine vasopressin, but not epinephrine, improves survival in uncontrolled hemorrhagic shock after liver trauma in pigs. Critical Care Medicine. 2003;31(4):1286–1287. doi: 10.1097/01.CCM.0000060014.75282.69. [DOI] [PubMed] [Google Scholar]
- 2.Shoemaker WC, Peitzman AB, Bellamy R, et al. Resuscitation from severe hemorrhage. Critical Care Medicine. 1996;24(2):S12–S23. [PubMed] [Google Scholar]
- 3.Bayram B, Hocaoglu N, Atilla R, Kalkan S. Effects of terlipressin in a rat model of severe uncontrolled hemorrhage via liver injury. The American Journal of Emergency Medicine. 2012;30(7):1176–1182. doi: 10.1016/j.ajem.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Santry HP, Alam HB. Fluid resuscitation: past, present, and the future. Shock. 2010;33(3):229–241. doi: 10.1097/SHK.0b013e3181c30f0c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheung ATW, To PL, Chan DM, et al. Comparison of treatment modalities for hemorrhagic shock. Artificial Cells, Blood Substitutes, and Biotechnology. 2007;35(2):173–190. doi: 10.1080/10731190601188257. [DOI] [PubMed] [Google Scholar]
- 6.Stadlbauer KH, Wagner-Berger HG, Wenzel V, et al. Survival with full neurologic recovery after prolonged cardiopulmonary resuscitation with a combination of vasopressin and epinephrine in pigs. Anesthesia and Analgesia. 2003;96(6):1743–1749. doi: 10.1213/01.ANE.0000066017.66951.7F. [DOI] [PubMed] [Google Scholar]
- 7.Bonanno FG. Hemorrhagic shock: the “physiology approach”. Journal of Emergencies, Trauma and Shock. 2012;5(4):285–295. doi: 10.4103/0974-2700.102357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feinstein AJ, Patel MB, Sanui M, Cohn SM, Majetschak M, Proctor KG. Resuscitation with pressors after traumatic brain injury. Journal of the American College of Surgeons. 2005;201(4):536–545. doi: 10.1016/j.jamcollsurg.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 9.Fang Y, Li T, Fan X, Zhu Y, Liu L. Beneficial effects of activation of PKC on hemorrhagic shock in rats. The Journal of Trauma, Injury, Infection and Critical Care. 2010;68(4):865–873. doi: 10.1097/TA.0b013e3181bba209. [DOI] [PubMed] [Google Scholar]
- 10.Raedler C, Voelckel WG, Wenzel V, et al. Treatment of uncontrolled hemorrhagic shock after liver trauma: fatal effects of fluid resuscitation versus improved outcome after vasopressin. Anesthesia and Analgesia. 2004;98(6):1759–1766. doi: 10.1213/01.ANE.0000117150.29361.5A. [DOI] [PubMed] [Google Scholar]
- 11.Li T, Fang Y, Zhu Y, et al. A small dose of arginine vasopressin in combination with norepinephrine is a good early treatment for uncontrolled hemorrhagic shock after hemostasis. Journal of Surgical Research. 2011;169(1):76–84. doi: 10.1016/j.jss.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Bickell WH, Wall MJ, Jr., Pepe PE, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. The New England Journal of Medicine. 1994;331(17):1105–1109. doi: 10.1056/NEJM199410273311701. [DOI] [PubMed] [Google Scholar]
- 13.Meybohm P, Cavus E, Bein B, et al. Small volume resuscitation: arandomized controlled trial with either norepinephrine or vasopressin during severe hemorrhage. Journal of Trauma: Injury Infection & Critical Care. 2007;62(3):640–646. doi: 10.1097/01.ta.0000240962.62319.c8. [DOI] [PubMed] [Google Scholar]
- 14.Voelckel WG, Convertino VA, Lurie KG, et al. Vasopressin for hemorrhagic shock management: Revisiting the potential value in civilian and combat casualty care. Journal of Trauma. 2010;69(1):S69–S74. doi: 10.1097/TA.0b013e3181e44937. [DOI] [PubMed] [Google Scholar]
- 15.Spahn DR, Bouillon B, Cerny V, et al. Management of bleeding and coagulopathy following major trauma: an updated European guideline. Critical Care. 2013;17(2, article R76) doi: 10.1186/cc12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holt NF, Haspel KL. Vasopressin: a Review of Therapeutic Applications. Journal of Cardiothoracic and Vascular Anesthesia. 2010;24(2):330–347. doi: 10.1053/j.jvca.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 17.Bankir L. Antidiuretic action of vasopressin: quantitative aspects and interaction between V1a and V2 receptor-mediated effects. Cardiovascular Research. 2001;51(3):372–390. doi: 10.1016/s0008-6363(01)00328-5. [DOI] [PubMed] [Google Scholar]
- 18.Vincent J-L, Su F. Physiology and pathophysiology of the vasopressinergic system. Best Practice and Research: Clinical Anaesthesiology. 2008;22(2):243–252. doi: 10.1016/j.bpa.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 19.Moreau R, Barrière E, Tazi KA, et al. Terlipressin inhibits in vivo aortic iNOS expression induced by lipopolysaccharide in rats with biliary cirrhosis. Hepatology. 2002;36(5):1070–1078. doi: 10.1053/jhep.2002.36501. [DOI] [PubMed] [Google Scholar]
- 20.Wenzel V, Lindner KH. Employing vasopressin during cardiopulmonary resuscitation and vasodilatory shock as a lifesaving vasopressor. Cardiovascular Research. 2001;51(3):529–541. doi: 10.1016/s0008-6363(01)00262-0. [DOI] [PubMed] [Google Scholar]
- 21.Sanui M, King DR, Feinstein AJ, Varon AJ, Conn SM, Proctor KG. Effects of arginine vasopressin during resuscitation from hemorrhagic hypotension after traumatic brain injury. Critical Care Medicine. 2006;34(2):433–438. doi: 10.1097/01.ccm.0000196206.83534.39. [DOI] [PubMed] [Google Scholar]
- 22.Rehberg S, Ertmer C, Lange M, et al. Role of selective V2-receptor-antagonism in septic shock: a randomized, controlled, experimental study. Critical Care. 2010;14(6, article R200) doi: 10.1186/cc9320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. 2013;41(2):580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 24.Delmas A, Leone M, Rousseau S, Albanèse J, Martin C. Clinical review: vasopressin and terlipressin in septic shock patients. Critical Care. 2005;9(2):212–222. doi: 10.1186/cc2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson KB, Pearce FJ, Jeffreys N, McJames SW, Cluff M. Impact of Vasopressin on Hemodynamic and Metabolic Function in the Decompensatory Phase of Hemorrhagic Shock. Journal of Cardiothoracic and Vascular Anesthesia. 2006;20(2):167–172. doi: 10.1053/j.jvca.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 26.Voelckel WG, Lurie KG, Lindner KH, et al. Vasopressin improves survival after cardiac arrest in hypovolemic shock. Anesthesia and Analgesia. 2000;91(3):627–634. doi: 10.1097/00000539-200009000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Haas T, Voelckel WG, Wiedermann F, Wenzel V, Lindner KH. Successful resuscitation of a traumatic cardiac arrest victim in hemorrhagic shock with vasopressin: a case report and brief review of the literature. The Journal of Trauma. 2004;57(1):177–179. doi: 10.1097/01.ta.0000044357.25191.1b. [DOI] [PubMed] [Google Scholar]
- 28.Morales D, Madigan J, Cullinane S, et al. Reversal by vasopressin of intractable hypotension in the late phase of hemorrhagic shock. Circulation. 1999;100(3):226–229. doi: 10.1161/01.cir.100.3.226. [DOI] [PubMed] [Google Scholar]
- 29.Wenzel V, Krismer AC, Arntz HR, Sitter H, Stadlbauer KH, Lindner KH. A comparison of vasopressin and epinephrine for out-of-hospital cardiopulmonary resuscitation. The New England Journal of Medicine. 2004;350(2):105–113. doi: 10.1056/NEJMoa025431. [DOI] [PubMed] [Google Scholar]
- 30.Stadlbauer KH, Wagner-Berger HG, Raedler C, et al. Vasopressin, but not fluid resuscitation, enhances survival in a liver trauma model with uncontrolled and otherwise lethal hemorrhagic shock in pigs. Anesthesiology. 2003;98(3):699–704. doi: 10.1097/00000542-200303000-00018. [DOI] [PubMed] [Google Scholar]
- 31.Cavus E, Meybohm P, Doerges V, et al. Cerebral effects of three resuscitation protocols in uncontrolled haemorrhagic shock: a randomised controlled experimental study. Resuscitation. 2009;80(5):567–572. doi: 10.1016/j.resuscitation.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 32.Feinstein AJ, Cohn SM, King DR, et al. Early vasopressin improves short-term survival after pulmonary contusion. Journal of Trauma-Injury, Infection and Critical Care. 2005;59(4):876–883. doi: 10.1097/01.ta.0000187654.24146.22. [DOI] [PubMed] [Google Scholar]
- 33.Dünser MW, Mayr AJ, Tür A, et al. Ischemic skin lesions as a complication of continuous vasopressin infusion in catecholamine-resistant vasodilatory shock: Incidence and risk factors. Critical Care Medicine. 2003;31(5):1394–1398. doi: 10.1097/01.CCM.0000059722.94182.79. [DOI] [PubMed] [Google Scholar]
- 34.Prengel AW, Lindner KH, Wenzel V, Tugtekin I, Anhäupl T. Splanchnic and renal blood flow after cardiopulmonary resuscitation with epinephrine and vasopressin in pigs. Resuscitation. 1998;38(1):19–24. doi: 10.1016/s0300-9572(98)00078-1. [DOI] [PubMed] [Google Scholar]
- 35.Szmydynger-Chodobska J, Chung I, Koźniewska E, et al. Increased expression of vasopressin V1a receptors after traumatic brain injury. Journal of Neurotrauma. 2004;21(8):1090–1102. doi: 10.1089/0897715041651033. [DOI] [PubMed] [Google Scholar]
- 36.Biondi-Zoccai GGL, Agostoni P, Abbate A, Testa L, Burzotta F, Robinson KA. A simple hint to improve Robinson and Dickersin’s highly sensitive PubMed search strategy for controlled clinical trials. International Journal of Epidemiology. 2005;34(1):224–225. doi: 10.1093/ije/dyh311. [DOI] [PubMed] [Google Scholar]
- 37.Zangrillo A, Biondi-Zoccai GGL, Frati E, et al. Fenoldopam and acute renal failure in cardiac surgery: a meta-analysis of randomized placebo-controlled trials. Journal of Cardiothoracic and Vascular Anesthesia. 2012;26(3):407–413. doi: 10.1053/j.jvca.2012.01.038. [DOI] [PubMed] [Google Scholar]
- 38.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. The British Medical Journal. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu L, Tian K, Xue M, et al. Small doses of arginine vasopressin in combination with norepinephrine “buy” time for definitive treatment for uncontrolled hemorrhagic shock in rats. Shock. 2013;40(5):398–406. doi: 10.1097/SHK.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 40.Stadlbauer KH, Wagner-Berger HG, Krismer AC, et al. Vasopressin improves survival in a porcine model of abdominal vascular injury. Critical Care. 2007;11, article R81 doi: 10.1186/cc5977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beloncle F, Meziani F, Lerolle N, Radermacher P, Asfar P. Does vasopressor therapy have an indication in hemorrhagic shock? Annals of Intensive Care. 2013;3(1):1–6. doi: 10.1186/2110-5820-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oliver G, Schaefer E. On the physiological action of extract of pituitary body and certain other glandular organs. Journal of Physiology. 1895;18:277–279. doi: 10.1113/jphysiol.1895.sp000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Landry DW, Levin HR, Gallant EM, et al. Vasopressin pressor hypersensitivity in vasodilatory septic shock. Critical Care Medicine. 1997;25(8):1279–1282. doi: 10.1097/00003246-199708000-00012. [DOI] [PubMed] [Google Scholar]
- 44.Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. The New England Journal of Medicine. 2008;358(9):877–887. doi: 10.1056/NEJMoa067373. [DOI] [PubMed] [Google Scholar]
- 45.Lindner KH, Haak T, Keller A, Bothner U, Lurie KG. Release of endogenous vasopressors during and after cardiopulmonary resuscitation. Heart. 1996;75(2):145–150. doi: 10.1136/hrt.75.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lindner KH, Strohmenger HU, Ensinger H, Hetzel WD, Ahnefeld FW, Georgieff M. Stress hormone response during and after cardiopulmonary resuscitation. Anesthesiology. 1992;77(4):662–668. doi: 10.1097/00000542-199210000-00008. [DOI] [PubMed] [Google Scholar]
- 47.Thiemermann C, Szabó C, Mitchell JA, Vane JR. Vascular hyporeactivity to vasoconstrictor agents and hemodynamic decompensation in hemorrhagic shock is mediated by nitric oxide. Proceedings of the National Academy of Sciences of the United States of America. 1993;90(1):267–271. doi: 10.1073/pnas.90.1.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Eltzschig HK, Carmeliet P. Hypoxia and inflammation. The New England Journal of Medicine. 2011;364(7):656–665. doi: 10.1056/NEJMra0910283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smaïl N, Descorps Declère A, Duranteau J, Vigué B, Samii K. Left ventricular function after severe trauma. Intensive Care Medicine. 1996;22(5):439–442. doi: 10.1007/BF01712161. [DOI] [PubMed] [Google Scholar]
- 50.Plurad DS, Talving P, Lam L, Inaba K, Green D, Demetriades D. Early vasopressor use in critical injury is associated with mortality independent from volume status. Journal of Trauma-Injury, Infection and Critical Care. 2011;71(3):565–572. doi: 10.1097/TA.0b013e3182213d52. [DOI] [PubMed] [Google Scholar]
- 51.Sharma RM, Setlur R. Vasopressin in hemorrhagic shock. Anesthesia and Analgesia. 2005;101(3):833–834. doi: 10.1213/01.ANE.0000175209.61051.7F. [DOI] [PubMed] [Google Scholar]
- 52.Lienhart HG, Wenzel V, Braun J, et al. Vasopressin for therapy of persistent traumatic hemorrhagic shock: the VITRIS study. Anaesthesist. 2007;56(2):145–150. doi: 10.1007/s00101-006-1114-4. [DOI] [PubMed] [Google Scholar]
- 53.Collier B, Dossett L, Mann M, et al. Vasopressin use is associated with death in acute trauma patients with shock. Journal of Critical Care. 2010;25(1):173.e9–173.e14. doi: 10.1016/j.jcrc.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 54.Grmec S, Strnad M, Cander D, Mally S. A treatment protocol including vasopressin and hydroxyethyl starch solution is associated with increased rate of return of spontaneous circulation in blunt trauma patients with pulseless electrical activity. International Journal of Emergency Medicine. 2008;1(4):311–316. doi: 10.1007/s12245-008-0073-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cavus E, Meybohm P, Doerges V, et al. Effects of cerebral hypoperfusion on bispectral index: a randomised, controlled animal experiment during haemorrhagic shock. Resuscitation. 2010;81(9):1183–1189. doi: 10.1016/j.resuscitation.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 56.Dudkiewicz M, Proctor KG. Tissue oxygenation during management of cerebral perfusion pressure with phenylephrine or vasopressin. Critical Care Medicine. 2008;36(9):2641–2650. doi: 10.1097/CCM.0b013e3181847af3. [DOI] [PubMed] [Google Scholar]
- 57.Meybohm P, Cavus E, Dörges V, et al. Release of protein S100B in haemorrhagic shock: effects of small volume resuscitation combined with arginine vasopressin. Resuscitation. 2008;76(3):449–456. doi: 10.1016/j.resuscitation.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 58.Lienhart HG, Lindner KH, Wenzel V. Developing alternative strategies for the treatment of traumatic haemorrhagic shock. Current Opinion in Critical Care. 2008;14(3):247–253. doi: 10.1097/MCC.0b013e3282fce62a. [DOI] [PubMed] [Google Scholar]
- 59.Dünser MW, Mayr AJ, Ulmer H, et al. The effects of vasopressin on systemic hemodynamics in catecholamine-resistant septic and postcardiotomy shock: a retrospective analysis. Anesthesia and Analgesia. 2001;93(1):7–13. doi: 10.1097/00000539-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 60.Dünser MW, Wenzel V, Mayr AJ, Hasibeder WR. Management of vasodilatory shock: defining the role of arginine vasopressin. Drugs. 2003;63(3):237–256. doi: 10.2165/00003495-200363030-00001. [DOI] [PubMed] [Google Scholar]
- 61.Sperry JL, Minei JP, Frankel HL, et al. Early use of vasopressors after injury: caution before constriction. Journal of Trauma. 2008;64(1):9–14. doi: 10.1097/TA.0b013e31815dd029. [DOI] [PubMed] [Google Scholar]
- 62.Beloncle F, Meziani F, Lerolle N, Radermacher P, Asfar P. Does vasopressor therapy have an indication in hemorrhagic shock? Annals of Intensive Care. 2013;3, article 13 doi: 10.1186/2110-5820-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rajani RR, Ball CG, Feliciano DV, Vercruysse GA. Vasopressin in hemorrhagic shock: review article. American Surgeon. 2009;75(12):1207–1212. [PubMed] [Google Scholar]
- 64.Vesterinen HM, Sena ES, Egan KJ, et al. Meta-analysis of data from animal studies: a practical guide. Journal of Neuroscience Methods. 2014;221(15):92–102. doi: 10.1016/j.jneumeth.2013.09.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In the supplemental materials we confronted AVP/terlipressin with different comparators singularly: fluid resuscitation (fig. 6a), placebo (6b), other vasoconstrictive drugs(6C) and norepineprhine(6d). In all the analysis we conducted AVP/terlipressin was associated to a reduction of the death rate. We also did a meta-analysis on survival considering separately the studies conducted on rats (fig. 7a) and on pigs (fig.7b). In fig.8 we considered only the studies where hemorrhagic shock was due to a splancnic bleeding. We then did a meta-analysis excluding those trials with zero mortality (fig. 9) and selecting the studies that had mortality as the primary end-point. In table 3 are reported the dosages of AVP, terlipressin, vasopressors and the total amount of fluids included in the studies in the meta-analysis. In table 4 are reported the primary end-points and the setting of the included studies.


