Abstract
Background and Purpose: During the last two decades, clinical reports have begun to place increasing emphasis on the possible neurological complications related to dengue. However, reports of cases with myelitis post dengue are rare. This study describes an unprecedented cluster of transverse myelitis following a dengue virus infection.
Methods: 51 possible cases of neurological complications related to dengue were identified by the epidemiological surveillance of the State of Rondônia, Brazil and submitted to serial neurological examination, electromyography, vertebral MR and laboratory investigation to confirm the dengue diagnosis and rule out other arboviruses.
Results: The diagnosis of acute transverse myelitis post-dengue was established in 26 patients, the majority were women, young and white. Antibodies against virus IgM were present in all cases and DEN 3 virus was isolated by PCR in one patient. Treatment with IV steroids was useful.
Conclusions: The cluster of transverse myelitis post-dengue with favorable clinical outcome here reported suggests an immune mediated mechanism for the spinal cord involvement. Whereas dengue epidemics are frequent in tropical and subtropical countries, the dengue fever should be part in the differential diagnosis of the infectious and post-infectious myelitis.
Keywords: Dengue, Transverse Myelitis, Brazil
Introduction
Dengue is a viral infection the etiologic agent of which is an arbovirus of the Flavivirus genus and Flaviridae family. This is the arbovirus that most seriously affects humans. Outbreaks frequently occur in tropical and subtropical countries and present a grave public health problem [1, 2].
The classical form of dengue induces fever, myalgia, retro-ocular pain, headache, nausea, vomiting, diarrhea, arthralgia, rash and pruritus lasting two to seven days. Dengue hemorrhagic fever is a severe form of the disease presentation that can potentially progress to severe hemorrhagic manifestations, hypovolemic shock and death. Until now, four serotypes have been isolated (DENV1-4), and the polymerase chain reaction (PCR) technique is the method of choice to the detection of the viral genome. However, the ELISA method for detection of IgM antibodies for the dengue virus is the most widely used for epidemiological purposes. During the last two decades, clinical reports have begun to place increasing emphasis on the possible neurological complications related to dengue, although not without controversies [3–5].
The number of studies reveals the scarcity of scientific research on the rare relationship between the dengue virus and transverse myelitis, but the fact that late post-infectious myelitis may lead to possible under reporting should not be ignored. Dengue epidemics are frequent in tropical and subtropical countries, and dengue fever should always be part of the differential diagnosis for infectious and post-infectious myelitis [3–8].
Here we report, an unusual and unprecedented cluster of transverse myelitis (TM) following dengue virus infection in the Amazon region of Brazil.
Methods
Patients and study design
This retrospective study is based on a survery of medical records from November 2004 to March 2005. In December 2004, eight patients of neurological symptoms possibly related to dengue were reported to epidemiological surveillance personnel during an outbreak of the virus in the State of Rondonia (Brazil).
As a methodological strategy the epidemiological team from the Ministry of Health adopted an active search in the municipalities in order to identify the newly suspected cases (Fig. 1).
Fig. 1.
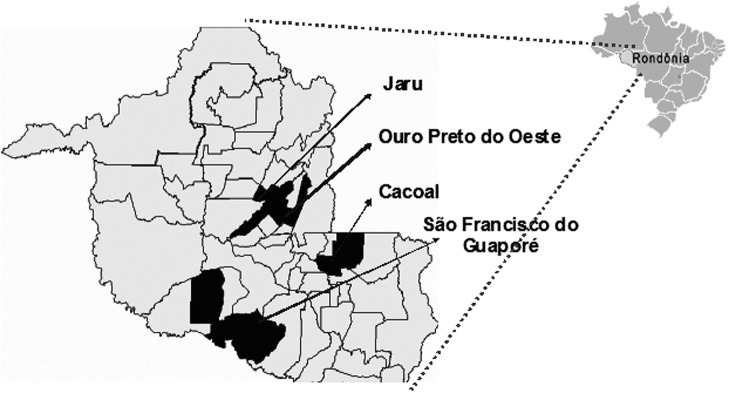
Map of the municipalities of Rondônia where cases were reported (Ministry of Health, Brazil).
As a result, 51 patients with a clinical diagnosis of dengue fever and neurological symptoms requiring clarification were referred to the Center of Neurology and Rehabilitation of Rondonia in Porto Velho (State Capital) to undergo examination and the neurological protocol proposed by one of the study authors (AMS) (Technique note from the Brazilian Ministry of Healthy http://chicomeloescreve.blogspot.com/2013/03/nota-tecnica.html).
Patients with a confirmed diagnostic of dengue infection who developed transverse myelitis (TM) were selected for this study. Only cases with six months of follow up and complete clinical and laboratorial data in medical records were included in the study. Patients with previous or concomitant systemic autoimmune diseases, other central nervous system (CNS) infections, idiopathic inflammatory demyelinating disorders and compressive myelopathy were excluded.
The study was approved by the Ethic Research Committee of the School of Medical Sciences and Health (Faculdade de Ciências Médicas e da Saúde) of Juiz de Fora (Brazil).
Definition of cases
The clinical diagnosis of dengue was defined according to classic symptoms. The main symptoms identified were acute febrile syndrome, severe headache, retro-orbital pain, myalgia and arthralgia. The laboratory criteria were the demonstration of IgM antibody to dengue virus antigens in paired serum samples.
Transverse myelitis (TM) was identified by the combination of varying degrees of motor syndrome, sensory and/or autonomic dysfunction with acute onset. The identification of upper sensitive thoracic level and pyramidal signs on neurological examination were required for the diagnosis of the spinal cord syndrome.
Data collection
The following data were collected directly from the medical charts: gender (male/female), age (years), race (Caucasian or African descent), age at onset of the disease (years), total number of TM per patient, time between the end of fever and onset of neurological symptoms, neurological manifestations and treatment with methylprednisolone EV for 5 days.
Complementary investigations
General laboratory tests: results of stool, blood, serum and cerebrospinal fluid (CSF) were analyzed by the laboratory service providers of the SUS (Brazilian Public National Health Service) in the localities involved in the epidemic, the Center for Research in Tropical Medicine, Porto Velho/Rondonia (CEPEM) and the Institute Evandro Chagas, Belém/Pará (IEC).
Specialized tests: results of magnetic resonance imaging (MRI) of the brain, spinal cord (cervical and thoracic segments) carried out in a radiology clinic contracted by the SUS. The spinal cord MRI data were analyzed with respect to inflammatory lesions. Brain MRI was analyzed and, in the case of inflammatory lesions, were classified as suggestive of TM or not. Electromyography (EMG) was performed at the Center of Neurology and Rehabilitation of Rondonia to exclude acute idiopathic inflammatory polyradiculoneuropathy and Guillain-Barré Syndrome (GBS).
Virology tests: results of specific tests for dengue in blood and CSF samples that were performed in IEC and CEPEM. Serum and CSF samples were tested for dengue IgM (ELISA) and West Nile Virus. The serum was also tested for inhibition hemagglutination (IH) for total antibodies against other arboviruses common in the Amazon region: alphavirus (Mayaro, Mucambo), bunyavirus (Guaroa, Maguari, Tacaiuma, Oropoche, Catu) and flavivirus (Ilheus, Rocio, Saint Louis, DEN 1, 2, 3, 4 and yellow fever) and other viruses such ashuman T cell lymphotropic virus type-1 (HTLV-1, cytomegalovirus [CMV]), human immunodeficiency virus (HIV), Epstein-Barr virus (HB) and herpes simplex virus (HS).
Neurological impairment
A spinal cord dysfunction scale [9] was applied in three phases of the disease: at nadirand at the time of two follow-up assessments (at 3 and 6 months). Severe spinal cord dysfunction was scored by motor (≥ 4), sensorial (≥ 3) and sphincter (≥ 2) scores.
Statistical analysis
The results from the analysis of categorical variables are presented as percentages and those relating to continuous variables as medians, accompanied by the minimum and maximum values. The percentage figures reflect valid values resulting from the exclusion of unknown values. The data were analyzed with the aid of SPSS for Windows (SPSS Inc., version;14, 1999).
Results
There were 26 patients with confirmed diagnostic of dengue infection and TM. Patients with a history of vaccination in the past two months (n = 2), neurological disease prior to infection (n = 2), negative serology for dengue (n = 6) or positive serology for dengue with incomplete laboratorial and clinical neurological investigation (n = 15) were excluded.
Most of the patients included were of low social and economic background (92.3%) and lived in Rondonia the during dengue epidemic, although 73.1% were born in other regions of Brazil. The demographic and clinical characteristics of the group are presented in Table 1. Most of the cases were women (57.7%), Caucasian (80.8%) and young adults with a mean age of 33.7 SD. 11.17 years. The onset of neurological symptoms occurred between 1 to 17 days after the end of the fever (median 3.0, IQR 2.0–9.0).
Table 1.
Demographics of transverse myelitis patients (n = 26)
| Characteristic | % |
|---|---|
| Gender | |
| Male | 42.3 |
| Female | 57.7 |
| Age at Onset of Illness (Decades) | |
| First decade (0–10 years) | 0 |
| Second decade (11–20 years) | 19.3 |
| Third decade (21–30 years) | 11.6 |
| Fourth decade (31–40 years) | 50.0 |
| Fifth decade (41–50 years) | 15.3 |
| Sixth decade (51–60 years) | 0 |
| Seventh decade (61–70 years) | 3.8 |
| Skin Color | |
| white | 80.8 |
| Afro Brazilians | 19.2 |
| black | 0 |
| Birth Origin | |
| Brazil (State of Rondônia) | 26.9 |
| Brazil (Other states) | 73.1 |
| Residence (Municipalities in Rondônia) | |
| Cacoal | 42.3 |
| OuroPreto | 7.7 |
| Jarú | 46.2 |
| São Francisco do Guaporé | 3.8 |
| Socioeconomic Background | |
| A (highest income bracket) | 7.7 |
| B | 0 |
| C | 0 |
| D | 80.8 |
| E (lowest income bracket) | 11.5 |
Table 2 presents the scores of motor, sensory and sphincter dysfunction in the three stages of the disease: at nadir and at the time of two subsequent neurological assessments. The more serious symptoms reported in the early stages of the disease were plegia in the lower limbs (30.8%), associated with a moderate decrease in sensitivity in the lower limbs (65.4%) and bladder or bowel incontinence (61.5%). In the first neurological assessment performed three months after the onset of symptoms, the majority of the patients had mild weakness in the lower limbs (80.8%) associated with pyramidal signs; 61.5% had decreased in sensitivity in the lower limbs and abdomen with a higher level in the thoracic region and 7.7% had a lack of sphincter control. In the last follow up, after six months, only one patient had objective neurological impairment characterized by moderate weakness in the lower limbs.
Table 2.
Evolution of transverse myelitis syndrome at three different timepoints (n = 26)
| Spinal Cord Dysfunction Scale | At Nadir % | Follow Up (Three Months) % | Follow Up (Six Months) % |
|---|---|---|---|
| Motor Dysfunction | |||
| Normal | 0 | 0 | 96.2 |
| Abnormal signs (pyramidal) without weakness | 0 | 0 | 0 |
| Mild weakness (grade 4 + or –5) | 0 | 80.8 | 0 |
| Moderate weakness (grade 3 or 4) | 26.9 | 15.4 | 3.8 |
| Severe weakness (grade 2) | 38.5 | 0 | 0 |
| Some plegic muscle (grade 0 or 1) | 3.8 | 3.8 | 0 |
| Plegia for all muscles | 30.8 | 0 | 0 |
| Sensory Dysfunction | |||
| Normal | 0 | 34.6 | 100 |
| Slight decrease in vibratory sensitivity | 0 | 0 | 0 |
| Slight decrease in pain, temperature or proprioception | 0 | 61.5 | 0 |
| Moderate abnormality of sensitivity | 65.4 | 0 | 0 |
| Loss of all types of sensitivity | 34.6 | 3.8 | 0 |
| Sphincter Dysfunction | |||
| Normal | 15.4 | 92.3 | 100 |
| Slight hesitation or urinary urgency | 0 | 0 | 0 |
| Moderate | 0 | 0 | 0 |
| Frequent urinary incontinence or retention requiring intermittent catheterization | 61.5 | 0 | 0 |
| Urinary catheterization with indwelling catheter or lack of sphincter control | 23.1 | 7.7 | 0 |
Five patients with neurological impairment received treatment with methylprednisolone 1 g/day for 5 days following the first neurological evaluation and showed a remission of the neurological symptoms.
Discussion
TM is a rare disease affecting one to four people per million [10]. The viruses associated with acute viral myelitis are herpes zoster, herpes simplex, cytomegalovirus, Epstein-Barr virus and HIV [10, 11], butin most cases the specific viral cause is never determined [12].
The association of TM with dengue virus is exceptional and suggests an acute infectious myelopathy or an immune-mediated process where the virus acts as a “trigger” of the inflammatory process targeting the myelin sheath cells. In these cases, the spinal cord involvement could represent a partial phenotypic manifestation of acute disseminated encephalomyelitis post viral (ADEM), which is an idiopathic inflammatory demyelinating disease related to infections or vaccinations [6–8, 13–15].
All of the cases described here could be classified as post-dengue myelitis, affecting mainly white women with a low socioeconomic background, living in the State of Rondonia in the Brazilian Amazon.
The spinal cord syndrome was characterized by acute and severe motor pyramidal impairment with sensorial deficit affecting mainly the lower limbs with a marked upper thoracic level and sphincter dysfunction following dengue fever. Inflammatory spinal cord MRI lesions were identified in one-third of the patients, reasonable percentage considering that the studies were conducted at different stages of the disease and that the absence of structural damage did not invalidate the clinical diagnosis of transverse spinal cord syndrome [11]. Leão et al. and Seet et al. described two cases of MT after dengue with normal MRI [13, 14].
Acute idiopathic inflammatory polyradiculoneuropathy or Guillain-Barré Syndrome (GBS) was not found in our series of patients. The diagnosis was excluded by clinical and complementary tests as CSF and EMG. This syndrome is the main differential diagnosis of patients with acute paralysis [16].
In a review of ADEM Garg did not include the dengue virus among the various viruses recognized as trigger immune-mediated central processes [17], but reports of recent cases reinforce the association between dengue and ADEM [6–8]. A strong argument for the hypothesis of immune-mediated myelitis is the delay between the end of the fever and the onset of neurological symptoms (mean 4.2 days, 1-day minimum and a maximum of 17 days) and the fact that no patient complained of neurological manifestations at the acute phase of dengue infection. Another important point is the reversibility of motor, sensory and sphincter dysfunctions, either spontaneously or after IV corticosteroid injection, which is less common in infectious myelitis than in immune-mediated myelitis [6, 7, 11]. At the last follow-up conducted six months later, a complete remission of the neurological dysfunction was observed in 95% of the cases. As for the diagnosis, post-infectious myelitis, unlike infectious myelitis, may be associated with a higher frequency of normal CSF [6, 10, 11, 15]. In our series, CSF did not show any significant or changes in cellularity or chemistry, reinforcing the hypothesis of an immunomediated mechanism. The presence of antibodies against dengue in the CSF may also indicate the breakdown of the blood-brain barrier [18].
Some studies have associated the neurological manifestations with dengue hemorrhagic fever [8, 19]. However, other studies show no such relationship [6, 7, 16, 18]. In our series, there were no cases of dengue hemorrhagic fever.
In the studies reviewed in the literature, there is a predominance of viruses DEN 2 and DEN 3 involved in large epidemics, but no correlation was observed between serotype and neurological complications [4, 5, 16]. The isolated DEN 3 virus was compatible with the dengue virus circulating in the epidemic.
Spinal cord tropism was demonstrated in our study, since all patients had only acute transverse myelitis as a complication of dengue. So far, there is no record in the medical literature of so many cases of TM reported in the same epidemic. The isolated natureand low incidence of myelitis in neurological complications of dengue fever corroborate this rarity. In a series of 21 patients with neurological manifestations of dengue, Solomon and colleagues described only two cases of transverse myelitis [20].
In a series of 41 patients with various complications related to dengue cases, Ferreira et al. [21] describe two ATM cases, and Sohler et al. [18] describe two cases of TM in a series of 13 patients. None of the studies provided a clinical prognosis on the treatment of a cluster of dengue-related myelitis.
In the acute phase, five of our 26 patients showed severe motor, sensory and sphincter dysfunction but an excellent response to intravenous corticosteroids, a finding already demonstrated in the literature [7, 11]. Sousa et al. demonstrated the efficacy of early use of intravenous corticosteroid in a young patient with post-dengueoptical neuromyelitis [6]. The early treatment of post-dengue myelitis is considered essential for clinical recovery [6, 11]. Yamamoto et al. described a case of post-dengue acute disseminated encephalomyelitis with optical and spinal cord involvement, in which intravenous steroids were administered 40 days after the onset of symptoms and resulted in only apartial improvement of symptoms [7].
The literature review shows that neurological manifestations related to the dengue virus infection are infrequent and that they were identified mainly during outbreaks where there is an increase in reported cases [22–25].
The cluster of post-dengue transverse myelitis with favorable clinical outcome reported here suggests an immune mediated mechanism for the spinal cord involvement. Whereas dengue epidemics are frequent in tropical and subtropical countries, and dengue fever should be included in the differential diagnosis of the infectious and post-infectious myelitis. This unexpected and unprecedented occurrence indicates the possible under reporting of such events. It is important that physicians be aware of the neurological manifestations after episodes of dengue fever to ensure early diagnosis and treatment.
References
- 1.Péres JGR, Clark GC, Gubler DJ, et al. . Dengue and Dengue hemorrhagic fever. Lancet 1998; 352: 971–977 [DOI] [PubMed] [Google Scholar]
- 2.Guzmán GM, Kouri G. Dengue: an update. Lancet Infect Dis 2002; 2: 33–42 [DOI] [PubMed] [Google Scholar]
- 3.Carod-Artal FJ, Wichmann O, Farrar J, et al. . Neurological complications of dengue virus infection. Lancet Neurol 2013; 12: 906–919 [DOI] [PubMed] [Google Scholar]
- 4.Hommel D, Talarmin A, Delbel V, et al. . Dengue encephalitis in French Guiana. Res Virol 1998; 149: 235–238 [DOI] [PubMed] [Google Scholar]
- 5.Palma-da Cunha-Matta A, Soares-Moreno SA, Cardoso-de Almeida A, et al. . Complicaciones neurológicas de la infección por el vírus del dengue. Rev Neurol 2004; 39: 233–237 [PubMed] [Google Scholar]
- 6.Miranda de Sousa A, Puccioni-Sohler M, Dias Borges A, et al. . Post-Dengue neuromyelitis optica: case report of a Japanese Brazilian Child. J Infect Chemother 2006; 12: 396–398 [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto Y, Tokasaki T, Yamada K, et al. . Acute disseminated encephalomyelitis following dengue fever. J Infect Chemother 2002; 8: 175–177 [DOI] [PubMed] [Google Scholar]
- 8.Sundaram C, Uppin SG, Dakshinamurthy KV, et al. . Acute disseminated encephalomyelitis following dengue hemorrhagic fever. Neurol India 2010; 58: 599–601 [DOI] [PubMed] [Google Scholar]
- 9.Wingerchuk DM, Hogancap WF, O’Brien PC, et al. . Clinical course of Neuromyelitis optica: (Devic Syndrome). Neurology 1999; 53: 1107–1114 [DOI] [PubMed] [Google Scholar]
- 10.Tranverse Myelitis Consortion Working Group Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology 2002; 59: 499–505 [DOI] [PubMed] [Google Scholar]
- 11.Krishnan C, Kaplin AL, Deshpande DM, et al. . Transverse Myelitis: pathogenesis, diagnosis and treatment. Front Biosci 2004; 9: 1483–1499 [DOI] [PubMed] [Google Scholar]
- 12.Kincaid O, Limpton HL. Viral myelitis: an update. Curr Neurol Neurosci Rep 2006; 6: 469–474 [DOI] [PubMed] [Google Scholar]
- 13.Leão RNQ, Oikawa T, Rosa EST, et al. . Isolation of dengue 2 virus from a patient with central nervous system involvement (tranverse myelitis). Rev Soc Bras Med Trop 2002; 35: 401–404 [DOI] [PubMed] [Google Scholar]
- 14.Seet RC, Lim EC, Wilder-Smith EP. Acute transverse myelitis following dengue vírus infection. J Clin Virol 2006; 35: 310–312 [DOI] [PubMed] [Google Scholar]
- 15.Jakob A, Weinshenker BG. An approach to the diagnosis of acute transverse myelitis. Semin Neurol 2008; 28: 105–120 [DOI] [PubMed] [Google Scholar]
- 16.Kumar S, Prabhakar S. Guillain Barré syndrome occurring in the course of dengue fever. Neurol India 2005; 53: 250–251 [DOI] [PubMed] [Google Scholar]
- 17.Garg RK Acute disseminated encephalomyelitis. Postgrad Med J 2003; 79: 11–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Puccioni-Sohler M, Soares CN, Papaiz-Alvarenga R, et al. . Neurologic dengue manifestations associated with intratecal especific immune response. Neurology 2009; 73: 1413–1417 [DOI] [PubMed] [Google Scholar]
- 19.Can BV, Fonsmark L, Hue NB, et al. . Prospective Case-Control Study of encephaloppathy in children with dengue hemorrhagic fever. Am J Trop Med Hyg 2001; 65: 848–851 [DOI] [PubMed] [Google Scholar]
- 20.Salomon T, Dung NM, Vaughn DW, et al. . Neurologic manisfestation of dengue infection. Lancet 2000; 355: 1053–1059 [DOI] [PubMed] [Google Scholar]
- 21.Ferreira MLB, Cavalcanti CG, Coelho CA, et al. . Manifestações neurológicas de dengue estudo de 41 casos. Arq Neuropsiquiatr 2005; 63: 488–493 [DOI] [PubMed] [Google Scholar]
- 22.Angibaud G, Lauate J, Laille M, et al. . Brain involvement in dengue fever. J Clin Neurosci 2001; 8: 63–65 [DOI] [PubMed] [Google Scholar]
- 23.Pancharoen C, Thisyakorn U. Neurological manifestations in dengue patients. South East Asian J Trop Med Public Health 2001; 32: 341–345 [PubMed] [Google Scholar]
- 24.Patey O, Ollivaud L, Breuil J, et al. . Usual neurologic manisfestations occurring during dengue fever infection. Am J Trop Med Hyg 1993; 48: 793–802 [DOI] [PubMed] [Google Scholar]
- 25.Kankirawatana P, Chokephaibulkit K, Puthavathana P, et al. . Dengue Infection Presenting With Central Nervous System Manifestation. J Child Neurol 2000; 15: 544–547 [DOI] [PubMed] [Google Scholar]


