Abstract
Although long-lasting insecticide-treated bednets (LLINs) have been widely used for malaria control, little is known about how the condition of LLINs affects the risk of malaria infection. The objective of this cross-sectional study was to examine the association between the use of LLINs with holes and caregiver-reported malaria diagnosed in children under five years of age (U5). Data were collected in Boboye health district, Niger, in 2010. Surveyors conducted interviews and bednet inspections in 1,034 households. If a household had a U5 child, the surveyor asked the caregiver whether the child had experienced a fever episode in the past two weeks that entailed standard treatment for uncomplicated malaria at a healthcare facility. The authors analyzed the association between the use of LLINs with holes and caregiver-reported malaria episodes in U5 children using logistic regression, adjusted for possible confounders. Of the 1,165 children included in the analysis, approximately half (53.3%) used an intact LLIN while far fewer (10.6%) used a LLIN with holes. Compared to children using an intact LLIN, children using a LLIN with holes were significantly more likely to have a caregiver-reported malaria episode (8.7% vs. 17.1%; odds ratio: 2.23; 95% confidence interval: 1.24–4.01). In this study site, LLINs with holes were less protective than intact LLINs.
Keywords: insecticide-treated bednets, mosquito control, malaria, Niger
Introduction
Malaria is one of the leading causes of death among children under five years of age (U5) in sub-Saharan Africa [1]. Long-lasting insecticide-treated bednets (LLINs), that is, factory-treated mosquito nets made with insecticide-treated fiber, have played a key role in malaria vector control. This type of bednet can protect people by repelling or killing mosquitoes that approach or come in contact with the net and thus are highly effective in reducing childhood mortality and morbidity from malaria [2]. Without any insecticide retreatment, LLINs are effective for at least three years [3]. In response to World Health Organization (WHO) recommendations, campaigns for the mass distribution of LLINs have been conducted to increase LLIN coverage in sub-Saharan African countries [1].
In Niger, which has one of the highest malaria burdens in sub-Saharan Africa, a nationwide mass distribution campaign took place in 2005 [4]. In the course of routine distribution, public healthcare facilities distribute LLINs to pregnant women and caregivers of U5s through immunization/antenatal clinics. In Boboye health district in particular, the Malaria Control Project, which was conducted by the Niger government, local health authorities and the Japan International Cooperation Agency, also distributed LLINs to requesting households through strengthened community health committees. As a result, household ownership of LLINs reached 82.5% in the project site in 2010 [5].
A number of studies have reported that LLINs sometimes become physically damaged and develop holes before reaching their expected lifespan [6, 7]. An experimental trial showed that, whether treated or untreated, the protective effects of insecticide-treated bednets diminished with increasing number of holes [8]. A study conducted in Equatorial Guinea and Malawi suggested that malaria infection was significantly more likely in children sleeping under LLINs with large holes than those sleeping under intact LLINs [9]. Although the protective effects of damaged LLINs may differ according to epidemiological setting, there are few reports on the protective effect of LLINs with holes in the field. Hence, we examined the association between usage of LLINs with holes and caregiver-reported diagnosed malaria episodes among U5 children in Boboye health district, Niger. In the present study, caregiver-reported diagnosed malaria is defined as cases in which the caregiver reported that, in the two weeks preceding the survey, his or her child had experienced a fever episode, visited a healthcare facility and received artemisinin-based combination therapy (Coartem®).
Methods
Study area
The Boboye health district is located in western Niger, approximately 110 km from Niamey, the nation’s capital. The district covers an area of 4,794 km2 and has a population of about 330,000 people. The district’s healthcare facilities are comprised of one district hospital, 23 health centers and 60 health posts. According to the national malaria control policy, health workers in these facilities use Paracheck Pf® (Orchid Biomedical System, Goa, India), a rapid diagnostic test kit, to diagnose malaria [10]. Coartem® (Norvartis, Basel, Switzerland), an artemisinin-based combination therapy, is used to treat uncomplicated malaria. Falciparum malaria is the leading cause of morbidity and mortality in the district, accounting for 45.7% (30,933/67,714) of reported outpatient visits to the district hospital [11].
Data collection
This study used selected data collected for the evaluation of the Malaria Control Project. The data collection strategies are described elsewhere [5]. Briefly, three villages were randomly selected from the catchment area of each of 10 health centers, with probability proportional to their estimated population size (Fig. 1). Then, 35 target households and some extra households, which were used to replace a target household in the event that it was unavailable, were randomly selected from each village.
Fig. 1.
Map of Boboye Health District showing the study villages and health centers.
The map inserted in the top right of the figure is the country of Niger; Boboye Health District is highlighted. Circles and squares indicate the locations of the study villages and health centers, respectively.
Surveyors visited the target households and conducted interviews with household members in January and February 2010. During the interviews, the surveyors collected demographic information; socio-economic information including the possession of assets and house type; and bednet-related information, including the place and time that bednets were obtained and individual respondents’ use of bednets prior to the survey. If a household had a U5 child, the surveyor asked the caregiver whether the child had a fever episode in the two weeks preceding the survey that entailed a healthcare facility visit and also whether the child had been given Coartem® at the facility (caregivers were shown a picture of the medicine). The surveyors also inspected bednets to determine their type and condition. Bednet information included whether it was LLIN or non-LLIN; its brand; and the presence/absence of holes. The surveyors also determined whether LLINs were those distributed by the project by confirming the mark that the project put on its nets before distribution.
The survey protocol was approved by the National Malaria Control Programme, Ministry of Health, Niger. Verbal consent was obtained from each household respondent before the survey was conducted.
Data analysis
Principal component analysis was used to assess the extent of household assets and to build a wealth index [12, 13]. Table 1 shows the scoring factors of the variables that went into the index. The caregiver-reported diagnosed malaria episode of U5 children was the primary outcome in this study. The caregiver-reported fever episode of U5 children was the secondary outcome. The odds ratios (OR) and 95% confidence intervals (95%CI) related to outcomes on the condition of the nets used by U5 children were estimated by logistic regression analysis. Bivariate and multivariate analyses were conducted. For the multivariate analysis, we adjusted for possible confounders such as the age and gender of U5 children, house type and wealth index of the household. Statistical analyses were performed using Stata 12 (StataCorp LP, Texas, USA). Village and household clustering was controlled using the “svy” command because a cluster sampling design, with village and household as sampling units, was adopted in this study.
Table 1.
Scoring factors for wealth index variables
| Variables | Scoring factors |
|---|---|
| Wall materials | |
| Mud | −0.216 |
| Straw | −0.200 |
| Cement | 0.394 |
| Brick | 0.176 |
| Household possessions | |
| Television | 0.697 |
| Radio | 0.451 |
| Mobile phone | 0.558 |
| CD/VCD/DVD player | 0.627 |
| Watch | 0.375 |
| Motorbike | 0.390 |
| Car/truck | 0.412 |
| Bicycle | 0.419 |
| Animal drawn-cart | 0.471 |
| Cow | 0.324 |
| Goat | 0.156 |
| Camel | 0.168 |
| Donkey | 0.138 |
| Sheep | 0.331 |
Results
No households refused to participate in the survey. However, due to the absence of adult household members, the total number of surveyed households did not reach the intended number of 35 in two of the villages. The survey covered 1,034 households with 5,788 household members and included 1,229 U5 children.
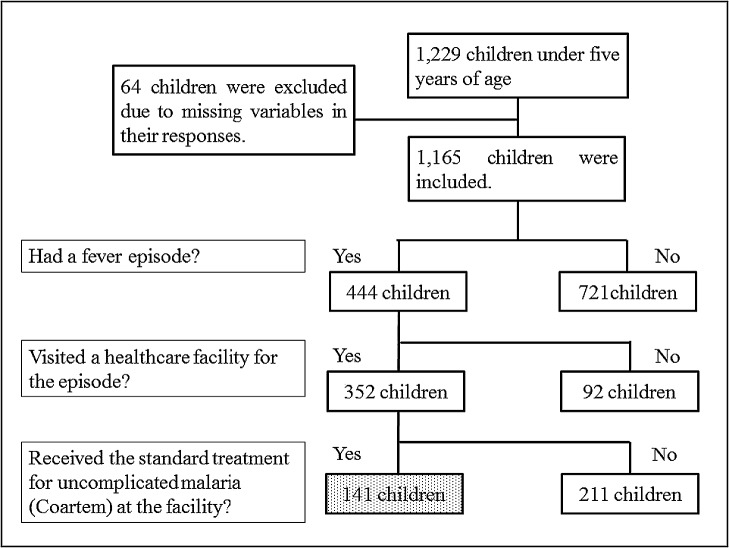
From the 1,229 U5 children, 64 were excluded due to missing variables in their responses, leaving data for 1,165 children (Fig. 2). According to caregivers’ reports, 444 (38.1%) had a fever episode and were defined as children with the secondary outcome (caregiver-reported fever episode). Of these, 352 (30.2%) subsequently visited a healthcare facility. Among those who visited a facility, 141 (12.1%) received Coartem® at the facility and were defined as children with the primary outcome (caregiver-reported diagnosed malaria episode).
Fig. 2.
Caregiver-reported diagnosed malaria episode definition
Table 2 shows the characteristics of the 1,165 U5 children and their households. The median age was two years, and nearly a half (48.5%) of the children were male. Most of them (77.3%, 900/1,165) used a bednet (of any type) on the night before the survey. Approximately half (53.3%, 621/1,165) used an intact LLIN. Far fewer (10.6%, 123/1,165) used a LLIN with holes on the night before the survey. Straw huts were the most common type of houses (42.6%), followed by cement/brick wall houses (31.3%).
Table 2.
Characteristics of children and their households
| Characteristics | Total (n = 1,165) | Children with diagnosed malaria episode (n = 141) | Children with fever episode (n = 444) |
|---|---|---|---|
| Age (years): median (inter-quartile) | 2 (1–3) | 2 (1–3) | 2 (1–3) |
| Gender (male): n (%) | 565 (48.5) | 70 (49.6) | 223 (50.2) |
| Use of bednet: n (%) | |||
| LLIN (intact) | 621 (53.3) | 54 (38.3) | 198 (44.6) |
| LLIN (holed) | 123 (10.6) | 21 (14.9) | 61 (13.7) |
| Untreated net (intact) | 88 (7.6) | 6 (4.3) | 33 (7.4) |
| Untreated net (holed) | 68 (5.8) | 8 (5.7) | 25 (5.6) |
| Not using bednet | 265 (22.7) | 52 (36.9) | 127 (28.6) |
| House type: n (%) | |||
| Straw hut | 496 (42.6) | 53 (37.6) | 176 (39.6) |
| Cement/brick wall house | 365 (31.3) | 60 (42.6) | 149 (33.6) |
| Mud wall house | 304 (26.1) | 28 (19.9) | 119 (26.8) |
LLIN: long-lasting insecticide-treated bednet
Table 3 shows the characteristics of the 744 LLINs that children used. Most of the LLINs (83.2%) were OlysetNet (Sumika Life-Tech Co., Osaka, Japan) bednets. The remainder (16.8%) were PermaNet (Vestergaard, Lausanne, Switzerland) bednets. Almost all of the LLINs (96.0%) were reported to have been obtained less than two years before the survey. A total of 196 LLINs (26.3%) bore the mark that the project had put on its bednets before distribution, indicating that they had been obtained less than two years earlier. All of the nets, including non-LLINs that children used the night before the survey, were left hanging in the sleeping places, which suggested their constant use.
Table 3.
Characteristics of long-lasting insecticide-treated bednets used by children
| Characteristics | n (n = 744) | % | |
|---|---|---|---|
| Brand | OlysetNet | 619 | 83.2 |
| PermaNet | 125 | 16.8 | |
| Condition | Intact | 621 | 83.5 |
| Holed | 123 | 16.5 | |
| Time the bednet was obtained | Within two years | 714 | 96.0 |
| More than two years ago | 30 | 4.0 |
For the primary outcome, bivariate logistic regression analysis shows that children who used a LLIN with holes were significantly more likely to have a caregiver-reported diagnosed malaria episode compared to those using an intact LLIN (17.1% vs. 8.7%, OR: 2.16, 95%CI: 1.21–3.87) (Table 4). In the multivariate analysis, the association remained statistically significant (OR: 2.23; 95%CI: 1.24–4.01). For the secondary outcome, bivariate logistic regression analysis showed that children who used a LLIN with holes were significantly more likely to have a caregiver-reported fever episode compared to those using an intact LLIN (49.6% vs. 31.9%; OR: 2.10; 95%CI: 1.30–3.40) (Table 5). In the multivariate analysis, the association remained statistically significant (OR: 2.13; 95%CI: 1.32–3.43).
Table 4.
Associations between caregiver-reported diagnosed malaria episodes and conditions of their bednets
| Variables | Percentage of children with diagnosed malaria episode | Bivariate analysis |
Multivariate analysis1 |
|||
|---|---|---|---|---|---|---|
| Odds ratio | 95% confidence interval | Odds ratio | 95% confidence interval | |||
| Conditions of bednets | ||||||
| LLIN (intact) | 8.7 | 1.00 | Reference | 1.00 | Reference | |
| LLIN (holed) | 17.1 | 2.16 | 1.21–3.87 | 2.23 | 1.24–4.01 | |
| Untreated bednet (intact) | 6.8 | 0.77 | 0.24–2.47 | 0.85 | 0.26–2.81 | |
| Untreated bednet (holed) | 11.8 | 1.40 | 0.58–3.36 | 1.57 | 0.66–3.75 | |
| Not using bednet | 19.6 | 2.56 | 1.47–4.46 | 2.50 | 1.41–4.42 | |
| Age | — | 1.13 | 0.99–1.29 | 1.12 | 0.97–1.28 | |
| Gender | — | 0.95 | 0.65–1.39 | 0.95 | 0.65–1.40 | |
| House type | — | 1.43 | 1.03–1.98 | 1.39 | 0.04–1.02 | |
| Wealth index | — | 0.99 | 0.81–1.21 | 1.03 | 0.84–1.25 | |
1 Adjusted for age, gender, house type, and wealth index
LLIN: long-lasting insecticide-treated bednet
Table 5.
Associations between caregiver-reported fever episodes and conditions of their bednets
| Variables | Percentage of children with fever episode | Bivariate analysis |
Multivariate analysis1 |
|||
|---|---|---|---|---|---|---|
| Odds ratio | 95% confidence interval | Odds ratio | 95% confidence interval | |||
| Conditions of bednets | ||||||
| LLIN (intact) | 31.9 | 1.00 | Reference | 1.00 | Reference | |
| LLIN (holed) | 49.6 | 2.10 | 1.30–3.40 | 2.13 | 1.32–3.43 | |
| Untreated bednet (intact) | 37.5 | 1.28 | 0.83–1.97 | 1.30 | 0.83–2.02 | |
| Untreated bednet (holed) | 36.8 | 1.24 | 0.59–2.62 | 1.25 | 0.60–2.59 | |
| Not using bednet | 47.9 | 1.97 | 1.29–3.00 | 2.01 | 1.35–2.99 | |
| Age | — | 0.98 | 0.88–1.08 | 0.96 | 0.87–1.06 | |
| Gender | — | 0.89 | 0.70–1.13 | 0.91 | 0.72–1.15 | |
| House type | — | 1.04 | 0.84–1.29 | 1.04 | 0.84–1.28 | |
| Wealth index | — | 1.02 | 0.87–1.19 | 1.05 | 0.89–1.23 | |
1 Adjusted for age, gender, house type, and wealth index
LLIN: long-lasting insecticide-treated bednet
Discussion
The present study demonstrated that U5 children sleeping under LLINs with holes were more likely to suffer fever and to receive a diagnosis of malaria than those sleeping under intact LLINs. This finding is consistent with the findings of Rehman et al., who reported the impaired effectiveness of LLINs with big holes [9]. It is likely that the holes allowed mosquitoes to penetrate the LLINs and to come in contact with the children.
There is a possibility that failure to use the nets on a daily basis is more of a determinant of malaria infections than holes. Iwashita et al. reported that net use was affected by sleeping arrangement and the availability of suitable locations for hanging nets, as well as net availability [14]. Although we did not inspect the determinants of net usage reported by Iwashita et al., our surveyors observed in the daytime that all the nets that children used the night before the survey, including non-LLINs, remained hanging. Therefore, the nets with holes children used in our study are likely to have been used on a daily basis.
Our study has several limitations. First, we did not record the size, number and location of the holes observed on the nets. As the protective effects of nets can depend on their physical condition [8], the results of our study would change if we classified LLINs with holes by the size, number and location of the holes. Second, as we did not examine the blood of study participants, we might have included some children who did not have malaria and excluded some of those who did. However, according to the Niger national malaria control policy, Coartem® is prescribed by health workers when patients test malaria-positive and are able to swallow oral medication. Although we did not confirm whether health workers actually used rapid diagnostic tests, we believe that most of the children who were included on the basis of our definition had malaria. Finally, as we included only febrile children with or without diagnosed malaria determined by a rapid diagnostic test, the results could have changed if we included the children who had no symptoms but possibly had malaria and those who were tested negative but possibly had malaria. However, as shown in the results, fever episodes alone were also associated with the use of holed LLIN; we thus believe that the association between the use of LLIN with holes and diagnosed malaria episodes is robust.
In this study site, the caregiver’s reports indicate that almost all of the LLINs used by children were obtained within the two-year period preceding the survey. However, as shown in Table 3, 16.5% of the LLINs used by children had already developed a hole. If we focus on the 196 LLINs confirmed to have been obtained within the two-year period preceding the survey, 9.2% had already developed a hole. These percentages could be higher if we included LLINs used by people other than U5 children and LLINs that were not in use, because better bednets tend to be assigned to young children in many countries [15, 16]. A number of studies on LLIN material durability have also reported that a substantial proportion of distributed LLINs became poor or very poor in condition (by developing a hole) before the expected lifespan of at least three years [17–20]. Therefore, more attention needs to be paid to the maintenance of the current generation of LLINs even before they reach the end of their lifespan.
In conclusion, children using LLINs with holes were significantly more likely to have been diagnosed with malaria in comparison to children using intact LLINs. Repairing holes on LLINs may enhance their protective effects.
Acknowledgements
The authors sincerely thank the study participants, field surveyors, and officers of the Japan International Cooperation Agency. This work was partly supported by the Grant for National Center for Global Health and Medicine (25-2).
References
- 1.World Health Organization. The World Malaria Report 2012. Geneva: World Health Organization; 2012.
- 2.Lengeler C Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev 2004; 2: CD000363. [DOI] [PubMed]
- 3.World Health Organization Guidelines for Laboratory and field testing of long-lasting insecticidal mosquito nets [Internet]. Geneva: World Health Organization; 2005 [cited 2014 Mar 14]. Available: http://whqlibdoc.who.int/hq/2005/WHO_CDs_WHOPES_GCDPP_2005.11.pdf
- 4.Centers for Disease Control and Prevention (CDC) Distribution of insecticide-treated bednets during a polio immunization campaign—Niger, 2005. MMWR Morb Mortal Wkly Rep 2006; 55: 913–916 [PubMed] [Google Scholar]
- 5.Nonaka D, Maazou A, Yamagata S, et al. . Distribution of subsidized insecticide-treated bed nets through a community health committee in Boboye Health District, Niger. Trop Med Health 2012; 40: 125–131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kilian A, Byamukama W, Pigeon O, et al. . Long-term field performance of a polyester-based long-lasting insecticidal mosquito net in rural Uganda. Malar J 2008; 7: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azondekon R, Gnanguenon V, Oke-Agbo F, et al. . A tracking tool for long-lasting insecticidal (mosquito) net intervention following a 2011 national distribution in Benin. Parasit Vectors 2014; 7: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irish S, N’guessan R, Boko P, et al. . Loss of protection with insecticide-treated nets against pyrethroid-resistant Culex quinquefasciatus mosquitoes once nets become holed: an experimental hut study. Parasit Vectors 2008; 1: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rehman AM, Coleman M, Schwabe C, et al. . How much does malaria vector control quality matter: the epidemiological impact of holed nets and inadequate indoor residual spraying. PLoS One 2011; 6: e19205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ministere de la Sante Publique, Republique du Niger Politique nationale de lutte contre le paludisme. Niamey: Ministere de la Sante Publique, Republique du Niger; 2008
- 11.Japan International Cooperation Agency Human Development Department Report of preliminary survey for Malaria Control Project, Republic of Niger [Internet]. Tokyo, Japan: Japan International Cooperation Agency; 2010 [cited 2014 Mar 14]. Available: http://libopac.jica.go.jp/images/report/P1000000207.html (in Japanese)
- 12.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 2001; 38: 115–132 [DOI] [PubMed] [Google Scholar]
- 13.Vyas S, Kumaranayake L. Constructing socio-economic status indices: how to use principal components analysis. Health Policy Plan 2006; 21: 459–468 [DOI] [PubMed] [Google Scholar]
- 14.Iwashita H, Dida G, Futami K, et al. . Sleeping arrangement and house structure affect bed net use in villages along Lake Victoria. Malar J 2010; 9: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsuang A, Lines J, Hanson K. Which family members use the best nets? An analysis of the condition of mosquito nets and their distribution within households in Tanzania. Malar J 2010; 9: 211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Githinji S, Herbst S, Kistemann T, et al. . Mosquito nets in a rural area of Western Kenya: ownership, use and quality. Malar J 2010; 9: 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allan R, O’Reilly L, Gilbos V, et al. . An observational study of material durability of three World Health Organization-recommended long-lasting insecticidal nets in eastern Chad. Am J Trop Med Hyg 2012; 87: 407–411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shirayama Y, Phompida S, Kuroiwa C, et al. . Maintenance behaviour and long-lasting insecticide-treated nets (LLITNs) previously introduced into Bourapar district, Khammouane province, Lao PDR. Public Health 2007; 121: 122–129 [DOI] [PubMed] [Google Scholar]
- 19.Mutuku FM, Khambira M, Bisanzio D, et al. . Physical condition and maintenance of mosquito bed nets in Kwale County, coastal Kenya. Malar J 2013; 12: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhatt RM, Sharma SN, Uragayala S, et al. . Effectiveness and durability of Interceptor® long-lasting insecticidal nets in a malaria endemic area of central India. Malar J 2012; 11: 189. [DOI] [PMC free article] [PubMed] [Google Scholar]