Abstract
Background
Fitzpatrick skin phototype (FSPT) is the most common method used to assess sunburn risk and is an independent predictor of skin cancer risk. Due to a conventional assumption that FSPT is predictable based on pigmentary phenotypes, physicians frequently estimate FSPT based on patient appearance.
Objective
To determine the degree to which self-reported race and pigmentary phenotypes are predictive of FSPT in a large, ethnically diverse population.
Methods
A cross-sectional survey collected responses from 3386 individuals regarding self-reported FSPT, pigmentary phenotypes, race, age and sex. Univariate and multivariate logistic regression analyses were performed to determine variables that significantly predict FSPT.
Results
Race, sex, skin color, eye color and hair color are significant but weak independent predictors of FSPT (P<0.0001). A multivariate model constructed using all independent predictors of FSPT only accurately predicted FSPT to within one point on the Fitzpatrick scale with 92% accuracy (weighted kappa statistic=0.53).
Limitations
Our study enriched for responses from ethnic minorities and does not fully represent the demographics of the U.S. population.
Conclusions
Patient self-reported race and pigmentary phenotypes are inaccurate predictors of sun sensitivity as defined by Fitzpatrick skin phototype. There are limitations to using patient-reported race and appearance in predicting individual sunburn risk.
Keywords: Fitzpatrick skin phototype, Fitzpatrick skin type, sunburn risk, skin cancer risk, suntan, race, pigmentary phenotype, predictor, hair color, eye color, skin color
Introduction
The incidence of non-melanoma and melanoma skin cancer continues to rise in the United States (U.S.) and exposure to UV radiation from sunlight is one of the strongest risk factors for developing these cancers 1. The Fitzpatrick skin phototype (FSPT) classification system is the most commonly used method to assess sunburn and suntan risk by evaluating patient-reported sun sensitivity. In 1975, Fitzpatrick first described sun reactive skin types I through IV to classify persons of white skin, and later modified it to include types V and VI for persons of brown and black skin 2. Over time, this system has evolved to classify an individual’s self-reported tendency to burn or tan after moderate sun exposure based on a scale of six skin types (Table I) 2, 3. A lower Fitzpatrick skin phototype corresponds to skin that burns easily and tans poorly, and a higher skin phototype indicates skin that burns rarely and tans profusely. Clinically, Fitzpatrick skin phototype is commonly used to predict skin cancer risk, guide sun protection advice, and estimate the initial minimal erythema dose (MED) for Ultraviolet B (UVB), Psoralen with Ultraviolet A (PUVA) and laser treatments 4–10. Evidence shows that FSPT is a significant and stronger predictor of skin cancer risk than pigmentary phenotypes such as hair, eye and skin color 9–11
Table I.
Determination of Fitzpatrick skin phototype (FSPT).
| Fitzpatrick Skin Phototype | Sunburn Tendency | Suntan Tendency |
|---|---|---|
| I | Always Burns Easily | Never Tan |
| II | Always Burns Easily | Tans Slightly |
| III | Burns Moderately | Tans Gradually |
| IV | Burns Minimally | Tans Moderately |
| V | Rarely Burns | Tans Profusely |
| VI | Never Burns | Tans Profusely |
FSPT is strictly defined as the patient self-report of their sun reactivity after moderate UV exposure 2, 3. However, physicians commonly predict FSPT based on race and pigmentary phenotypes, leading to the increasing trend for physicians to estimate sunburn and skin cancer risk based on visual inspection of patient appearance, a method known as physician-diagnosed skin phototype (PSPT). Given that FSPT is independently associated with skin cancer risk and the common assumption that race and pigmentary phenotypes predict FSPT, it is clinically important to investigate this relationship in an ethnically diverse population. We hypothesize that there is a phenotypically unmeasurable component of race that influences FSPT beyond its relationship with pigmentary phenotypes. Ultimately, the goal is to improve our understanding about the determination of skin cancer risk in non-Caucasian ethnic minorities.
Materials and Methods
Questionnaire Design and Study Population
A 6-month cross-sectional survey study collected internet and paper responses from 3386 individuals regarding age, sex, self-reported Fitzpatrick skin phototype, eye color, hair color, constitutive skin color determined from the inside of the wrist, and race/ethnicity. FSPT was determined based on each participant's self-reported response to the question "How does your skin react if you go outside without sunscreen for half an hour?" (Table I). There was no physician assessment of skin phototype for study participants. Constitutive skin color was measured by showing participants a color schematic and asking them to select the color that matched closest to the color on their inside wrist (Figure 1).
Figure 1.
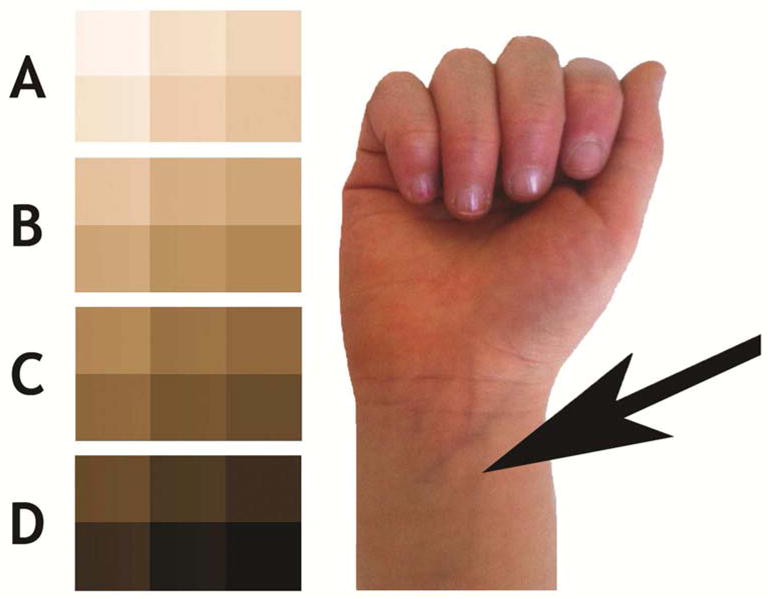
Determination of constitutive skin color. Participants were asked to select the color on the inside of their wrist as depicted by the arrow that matched closest to the displayed color schematic.
A. Light
B. Fair
C. Medium
D. Dark
An electronic link to the survey was distributed using social media sites (Facebook, Twitter) and was open to response from all over the U.S. In order to enrich for non-Caucasian participants, we targeted minority group pages on these social media websites. Chain-referral sampling (recruitment by participants amongst their acquaintances) was employed to further maximize participant responses. In addition, English and Spanish paper versions of the survey were distributed during community events, including church gatherings, community lectures and seminars at UCSF Medical Center. We initially categorized Hispanic/Latino as an ethnicity rather than a race. However, in our pilot study, Latinos frequently selected “Other” in response to the race question. Therefore, we included Latino as an answer option under race. Individuals under the age of 18 were excluded from the study. Study data were collected and managed using Research Electronic Data Capture (REDCap) tools at UCSF, a secure web-based application designed to support data capture for research studies. This study did not collect any protected health information, was performed in accordance with the Declaration of Helsinki and was self-certified in accordance with the UCSF Committee on Human Research.
Statistical Analysis
Descriptive statistics were used to summarize overall characteristics of the study population. We employed univariate analysis to identify significant single predictor variables of FSPT. The predictor variables assessed include age, sex, race, eye color, hair color, and skin color. Ordered logistic regression analysis was applied to identify variables that were significant univariate predictors of FSPT. We subsequently constructed a multivariate model by backward step-wise approach using those predictor variables with P-value <0.05 in univariate analysis. The Wald linear test for trend was used to assess multiple-level, ordinal categorical variables. Pigmentary phenotype categorical variables were ordered from lightest to darkest. We included all observations in the multivariate model and utilized a 10-fold cross-validation approach to assess the ability of the model to predict FSPT. In each iteration of validation, 90% of observations were used to construct the model and 10% were assigned predicted probabilities for each FSPT category. The model-predicted FSPT was based on the category with the highest probability and was compared to actual participant-reported FSPT data. The mean absolute error (MAE) and weighted kappa statistic were calculated to assess the effectiveness of the constructed model. The MAE measures the average magnitude of error and was expressed in the units of the variable of interest, FSPT. This validation was repeated for ten cycles and the MAE was averaged over all cycles. Sensitivity analysis with generalized ordinal logistic regression was completed to verify that the ordinal logistic model did not violate the proportional odds assumption 12. Likelihood ratio testing was performed to compare goodness of fit between multivariate models constructed with and without race. All statistical significance parameters were set at p<0.05. Statistical analysis was performed using STATA v11.2 (STATA Corporation, College Station, TX).
Results
A total of 3386 participant responses were collected from an ethnically diverse general population, of which 69% (2351) were female and 31% (1024) were male (Table II). Overall, the mean (SD) participant age was 37.0 (14.8). The racial distribution included 1021 White, 576 Asian, 556 Black, 245 Native American, 342 Latino and 564 multiracial individuals. Amongst individuals who reported multiple races, the predominant groups were 153 White/Native American, 52 White/Asian, 49 White/Black and 43 White/Black/Latino. In the collective study population, FSPT distribution was approximately 4.6% type I, 11.1% type II, 18.1% type III, 22.2% type IV, 25.0% type V, and 18.8% type VI. While 64.6% (2180) of all respondents had brown eyes and 90.4% (3061) had brown or black hair, only 3.4% (115) people reported to have skin color D, the darkest skin phenotype. The majority of the respondents (77.5%) reported skin color A or B, the two lightest phenotypes (Figure 1).
Table II.
Descriptive characteristics of study participants.
| Variable | FSPT I | FSPT II | FSPT III | FSPT IV | FSPT V | FSPT VI | N (Total=3386) | % | P-Value |
|---|---|---|---|---|---|---|---|---|---|
| Sex | |||||||||
| Male | 36 (3.5) | 92 (8.9) | 187 (18.3) | 215 (21.0) | 257 (25.1) | 237 (23.1) | 1024 | 30.2 | <0.0001 |
| Female | 119 (5.1) | 283 (12.0) | 426 (18.1) | 537 (22.8) | 589 (25.1) | 397 (16.9) | 2351 | 69.4 | |
| Age | |||||||||
| <25 | 34 (3.8) | 69 (7.5) | 138 (14.9) | 172 (18.6) | 282 (30.5) | 229 (24.7) | 925 | 27.3 | <0.0001 |
| 25–44 | 75 (5.2) | 181 (12.7) | 261 (18.3) | 312 (22) | 343 (24) | 248 (17.5) | 1421 | 42.0 | |
| >45 | 46 (4.5) | 126 (12.2) | 212 (20.5) | 268 (25.9) | 221 (21.4) | 156 (15.1) | 1031 | 30.4 | |
| Race | |||||||||
| White | 97 (9.5) | 222 ( 21.7) | 301 (29.5) | 219 (21.4) | 126 (12.3) | 56 (5.5) | 1021 | 30.2 | <0.0001 |
| Asian | 8 (1.3) | 34 (5.9) | 75 (13.0) | 151 (26.2) | 193 (33.5) | 115 (19.9) | 576 | 17.0 | |
| Black | 8 (1.4) | 17 (3.0) | 36 (6.5) | 64 (11.5) | 162 (29.1) | 269 (48.4) | 556 | 16.4 | |
| Native American | 3 (1.2) | 19 (7.8) | 20 (8.2) | 67 (27.3) | 88 (35.9) | 48 (19.6) | 245 | 7.2 | |
| Latino | 27 (7.9) | 37 (10.8) | 64 (18.7) | 95 (27.8) | 77 (22.5) | 40 (11.7) | 342 | 10.1 | |
| Multiracial | 11 (1.9) | 42 (7.4) | 104 (18.4) | 129 (22.9) | 184 (32.6) | 94 (16.7) | 564 | 16.7 | |
| Other | 0 (0.0) | 3 (5.5) | 9 16.7) | 22 (40.7) | 10 (18.5) | 10 (18.5) | 54 | 1.6 | |
| Missing/Prefer Not to Respond | 1 (4.7) | 2 (9.5) | 4 (19.0) | 5 (23.8) | 6 (28.6) | 3 (14.3) | 21 | 0.6 | |
| Skin Color | |||||||||
| Light (A) | 121 (10.5) | 228 (19.8) | 328 (28.4) | 212 (18.4) | 127 (11.0) | 77 (6.7) | 1153 | 34.1 | <0.0001 |
| Fair (B) | 21 (1.4) | 62 (4.2) | 244 (16.6) | 433 (29.5) | 462 (31.5) | 243 (16.6) | 1467 | 43.3 | |
| Medium (C) | 9 (1.5) | 20 (3.3) | 30 (4.9) | 93 (15.1) | 217 (35.3) | 245 (39.9) | 614 | 18.1 | |
| Dark (D) | 2 (1.7) | 4 (3.5) | 5 (4.3) | 9 (7.8) | 30 (26.0) | 65 (56.5) | 115 | 3.4 | |
| Hair Color | |||||||||
| Red | 24 (40.0) | 21 (35.0) | 6 (10.0) | 3 (5.0) | 3 (5.0) | 3 (5.0) | 60 | 1.8 | <0.0001 |
| Blonde | 31 (12.1) | 65 (25.3) | 82 (31.9) | 49 (19.1) | 20 (7.8) | 10 (3.9) | 257 | 7.6 | |
| Brown | 70 (3.8) | 229 (12.4) | 391 (21.1) | 456 (24.7) | 433 (23.5) | 265 (14.4) | 1846 | 54.5 | |
| Black | 30 (2.5) | 61 (5.2) | 134 (11.0) | 243 2(0.0) | 390 (32.1) | 357 (29.4) | 1215 | 35.9 | |
| Eye Color | |||||||||
| Blue, Gray | 57 (12.5) | 107 (23.5) | 136 (29.9) | 80 (17.6) | 47 (10.3) | 28 (6.2) | 455 | 13.4 | <0.0001 |
| Green | 18 (11.8) | 26 (17.1) | 38 (25.0) | 36 (23.7) | 21 (13.8) | 13 (8.6) | 152 | 4.5 | |
| Hazel-Green | 18 (6.5) | 53 (19.3) | 75 (27.2) | 72 (26.2) | 42 (15.3) | 15 (5.5) | 275 | 8.1 | |
| Hazel-Brown | 17 (5.4) | 51 (16.3) | 66 (21.1) | 80 (25.6) | 65 (20.8) | 32 (10.2) | 313 | 9.2 | |
| Brown | 45 (2.1) | 139 (6.4) | 298 (13.7) | 482 (22.1) | 670 (30.7) | 546 (25.0) | 2180 | 64.4 | |
Data presented as n (%), p-values obtained using chi-squared statistical testing. Sum of categories may not total to 3386 due to missing data points. Abbreviations: FSPT, Fitzpatrick skin phototype.
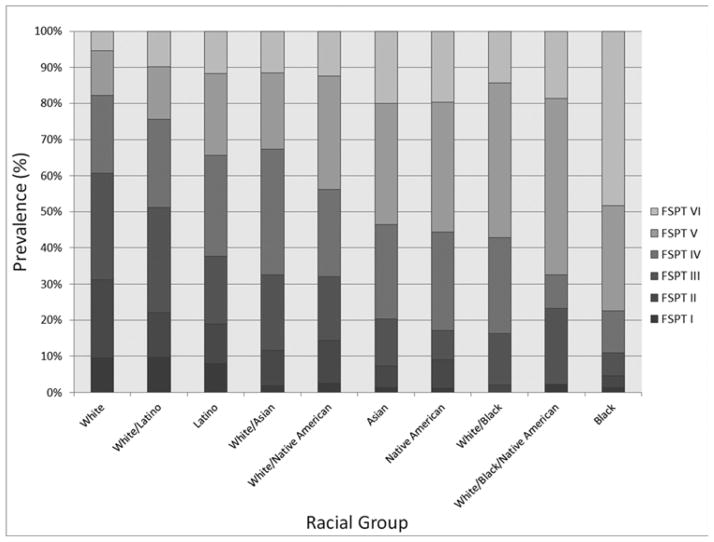
Although there were significant differences in FSPT amongst different racial groups (P<0.0001), the entire range of FSPT (I–VI) was observed in each racial group and in individuals reporting any range from light to dark pigmentary phenotypes. Our data showed that 17.7% (204) individuals reporting the lightest pigmentary phenotypes self-identified as skin phototype V or VI. The predominant FSPT for each racial group were as follows: White—type III, Latino—type IV, Asian—type V, Native American—type V, and Black—type VI (Figure 2). Whites and Latinos were the only two groups that reported a considerable number of type I FSPT (10%), while all racial groups reported a substantial number of type VI skin phototypes (range 5–45%). Non-Caucasian racial groups were more likely to tan than Caucasians, where >50% of Asians and Native Americans and >80% of Blacks reported tanning profusely with minimal or no burning after sun exposure. However, 61 Blacks (11%) also reported burning moderately or very easily (FSPT I, II, III) and 401 Caucasians (39%) reported tanning moderately or profusely (FSPT IV, V, VI). Multiracial individuals reported FSPT that was influenced by a mixture of their ethnic backgrounds (Figure 2).
Figure 2.
Comparison of FSPT distribution in subjects across different racial groups.
Univariate analysis indicated that sex, age, race, hair color, eye color and skin color were all significant predictors of FSPT (p<0.0001, Table II). Multivariate analysis revealed that after controlling for covariates, sex, hair color, eye color, skin color and race were significant, independent predictors of FSPT (p<0.0001, Table III). The final model did not violate the proportional odds/parallel lines assumption and there were no qualitative differences between the ordinal and generalized ordinal models in terms of the results. Men were significantly more likely to tan than women despite controlling for all covariates (OR 1.28, 95% CI 1.11–1.47, P<0.0001). Individuals with dark skin color were more likely to have a higher FSPT than those with light skin color (OR 7.48, 95% CI 4.83–11.57, p<0.0001). Similarly, those reporting black hair were 8-fold more likely to have a higher FSPT than those with red hair (OR 8.16, 95% CI 4.81–13.84, p<0.0001). In contrast, eye color was a weaker predictor of FSPT than skin and hair color (OR 1.97, 95% CI 1.56–2.48, p<0.0001). Race was an independent predictor of FSPT. After controlling for other covariates, Blacks were more likely than Caucasians to report FSPT VI (OR 3.56, 95% CI 2.74–4.63, p<0.0001).
Table III.
Multivariate logistic regression examining patient-reported predictors of higher FSPT.
| Variable | Odds Ratio | 95% Confidence Interval | P-Value |
|---|---|---|---|
| Sex | <0.0001 | ||
| Female | 1.00 | ||
| Male | 1.28 | 1.11–1.47 | |
| Age | 0.0879 | ||
| <25 | 1.00 | ||
| 25–45 | 0.77 | 0.65–0.90 | |
| >45 | 0.86 | 0.72–1.02 | |
| Race | <0.0001 | ||
| White | 1.00 | ||
| Asian | 1.56 | 1.22–2.01 | |
| Black | 3.56 | 2.74–4.63 | |
| Native American | 2.01 | 1.54–2.65 | |
| Latino | 0.96 | 0.75–1.22 | |
| Multiracial | 1.78 | 1.45–2.19 | |
| Hair Color | <0.0001 | ||
| Red | 1.00 | ||
| Blonde | 4.50 | 2.63–7.68 | |
| Brown | 6.21 | 3.75–10.27 | |
| Black | 8.16 | 4.81–13.84 | |
| Eye Color | <0.0001 | ||
| Blue | 1.00 | ||
| Green | 1.29 | 0.91–1.82 | |
| Hazel-Green | 1.17 | 0.89–1.54 | |
| Hazel-Brown | 1.23 | 0.93–1.63 | |
| Brown | 1.97 | 1.56–2.48 | |
| Skin Color | <0.0001 | ||
| Light (A) | 1.00 | ||
| Fair (B) | 3.34 | 2.84–3.93 | |
| Medium (C) | 6.51 | 5.19–8.17 | |
| Dark (D) | 7.48 | 4.83–11.57 |
P-values were generated using linear test for trend for multiple-level, ordinal categorical variables, significance is set at P<0.05. Odds ratios were determined by comparing each parameter to the following baseline variables, respectively—red hair, blue eyes, skin color A or Caucasian race. Odds Ratio>1.0 indicates a greater likelihood to report a higher FSPT.
A multivariate logistic regression model was constructed using the variables age, sex, pigmentary phenotypes and either with or without race to quantify the ability of these variables to collectively predict individual FSPT (Table III). Following cross-validation, comparison of model-predicted FSPT results to actual participant-reported FSPT in a model constructed without race resulted in a weighted kappa statistic of 0.52 (p<0.0001) and MAE of 0.93. The incorporation of race significantly improved the multivariate model (likelihood-ratio test p< 0.0001), although only minimally improving the weighted kappa statistic to 0.53 (p<0.0001) and MAE to 0.92. Together, the predicted FSPT values generated from this model deviated from actual individual FSPT by plus-minus one point on the Fitzpatrick scale, on average.
Discussion
Together, we report that self-reported race and pigmentary phenotypes are significant but weak predictors of FSPT and sunburn risk. Construction of a multivariate predictive model using the strongest, clinically-assessable phenotypic variables that are known to predict FSPT resulted in a kappa of 0.52, which is usually characterized as only moderate agreement. We also found a mean absolute error of 0.92, which indicates that model-predicted FSPT estimates were off by plus-minus one point (on average), and spanned three levels on the six point Fitzpatrick scale compared to participant self-reported FSPT. It is thus clear that self-reported appearance and race are only contributing a limited portion to individually reported sunburn risk, and that important unmeasured covariates impact tanning and burning more profoundly than conventionally anticipated. These results further highlight the fact that Fitzpatrick skin phototype is a classification intended to reflect individual sun sensitivity and not race or phenotypic features; these elements are clearly not the same. Given that FSPT is widely used clinically to predict skin cancer risk, inaccurate FSPT evaluation may lead to unreliable skin cancer risk stratification.
A number of studies have suggested a strong correlation between pigmentary phenotypes and FSPT in Caucasians 13–15, but studies in Korea, Thailand and Colombia 16–19 did not find such correlation. These data suggest that pigmentary phenotypes may be predictive of FSPT in Caucasians, but not in non-Caucasian minorities, rendering PSPT a less effective method of assessing skin cancer risk in an ethnically diverse population like the U.S. Physicians frequently overestimate sunburn risk for Caucasians based on patient appearance and underestimate sunburn risk for racial minorities 20. Several studies also discovered that physicians predominantly assign non-Caucasian, ethnic minorities to FSPT IV, V or VI based on their skin color or ethnic background and that this method has proven to be unreliable 21–23. The 2010 U.S. census estimates that non-Caucasian minorities made up 36.3% of the U.S. population, including 16.3% Hispanics or Latinos, 12.6% African Americans or Blacks, and 4.8% Asians 24. With this evolving ethnic diversity in the U.S., understanding the relationship between race, clinical pigmentary phenotypes and FSPT will impact our assessment of sunburn and skin cancer risk in ethnic minority patients.
We discovered that self-reported race is a weak independent predictor of FSPT even when controlling for pigmentary phenotypes, age, and sex. Although skin pigmentation is primarily responsible for differences in UV-induced DNA damage across different racial groups 25, race and genetics have also been proposed to contribute to the complex nature of skin response to UV damage and differences in individual sunburn risk. Our results lead us to believe that in addition to race and pigmentary phenotypes, there are unmeasured covariates that influence FSPT beyond physical appearance, perhaps through differential expression of genes that regulate the rate of melanization and distribution, or regulatory mechanisms for UV-induced DNA damage repair. Studies have reported that the redistribution rate of existing melanin towards the skin surface following sun exposure differs across different racial groups 26. Genetic polymorphisms affecting the differential infiltration of neutrophils to UV-damaged skin and the subsequent production of inflammatory cytokines (e.g. IL-10) and matrix metalloproteinases (e.g. MMP-1, MMP-9) have also been proposed as a potential mechanism that lead to differences in UV-associated skin damage in black versus white skin 25.
This is the largest study assessing the predictability of FSPT using self-reported race and pigmentary phenotypes in an ethnically diverse, heterogeneous population. One potential limitation of this study is that the sample population is not representative of the demographics of the United States. However, our goal was to investigate whether race and pigmentary features are predictive of FSPT in an ethnically diverse, multiracial population; therefore we enriched for non-Caucasian responses. The implemented survey was not validated for reliability, and we have not investigated the direct correlation between physician-diagnosed skin phototype and self-reported FSPT in this study. Thus, we cannot comment on the accuracy of physician assessment of FSPT in the clinical setting.
In summary, our study demonstrates that self-reported race and pigmentary phenotypes are not predictive of individual sunburn risk, as measured by the Fitzpatrick skin phototype scale. We present this data to highlight the potential limitations of a patient’s self-reported race and physical appearance in predicting individual sun sensitivity, and by extension, self-reported skin cancer risk. The results from our study expand on previous data demonstrating that self-reported FSPT correlates poorly with race 20. Currently, FSPT as defined by patient self-report remains to be the gold standard for describing sensitivity to UV exposure, and by extension UV-related outcomes such as skin cancer risk 8–10, 27. However, studies supporting this belief have been mainly conducted in ethnically homogeneous Caucasian populations 9. We recently reported that the risk of squamous cell carcinoma increased with each incremental decrease in FSPT in an ethnically diverse population of American organ transplant recipients, providing evidence that FSPT is an independent predictor of skin cancer risk in this population 11. Future studies will examine the effectiveness of FSPT in predicting skin cancer risk in a large, ethnically diverse general population.
Capsule Summary.
Fitzpatrick skin phototype (FSPT) is a patient-reported measure of sunburn risk and is a significant predictor of skin cancer risk.
Self-reported race and pigmentary phenotypes are inaccurate predictors of FSPT.
There are limitations to using self-reported race and appearance in predicting sunburn risk, as measured by the original Fitzpatrick system.
Acknowledgments
S.Y.H. is supported by the American Dermatological Association, Medical Student Research Fellowship.
S.T.A. is supported by the NIH/NCATS UCSF-CTSI grant number KL2 TR000143.
M.M.C. is supported by the NIH/NIAMSD grant number K24 AR052667.
E.L. is supported by the NCRR grant number KL2 RR024130 and Career Development Award from the American Skin Association and Dermatology Foundation.
Abbreviations
- FSPT
Fitzpatrick skin phototype
- MAE
Mean absolute error
- MED
Minimal erythema dose
- PSPT
Physician-diagnosed skin phototype
- PUVA
Psoralen with ultraviolet A
- REDCap
Research Electronic Data Capture
- UCSF
University of California, San Francisco
- U.S
United States
- UV
Ultraviolet
- UVB
Ultraviolet B
Footnotes
The authors have no conflict of interest to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Archives of dermatology. 2010;146:283–7. doi: 10.1001/archdermatol.2010.19. [DOI] [PubMed] [Google Scholar]
- 2.Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Archives of dermatology. 1988;124:869–71. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- 3.Fitzpatrick T. Soleil et peau. J Med Esthet. 1975;2:33–4. [Google Scholar]
- 4.Sachdeva S. Fitzpatrick skin typing: applications in dermatology. Indian journal of dermatology, venereology and leprology. 2009;75:93–6. doi: 10.4103/0378-6323.45238. [DOI] [PubMed] [Google Scholar]
- 5.Andreassi L, Simoni S, Fiorini P, Fimiani M. Phenotypic characters related to skin type and minimal erythemal dose. Photo-dermatology. 1987;4:43–6. [PubMed] [Google Scholar]
- 6.Sayre RM, Desrochers DL, Wilson CJ, Marlowe E. Skin type, minimal erythema dose (MED), and sunlight acclimatization. Journal of the American Academy of Dermatology. 1981;5:439–43. doi: 10.1016/s0190-9622(81)70106-3. [DOI] [PubMed] [Google Scholar]
- 7.Pershing LK, Tirumala VP, Nelson JL, Corlett JL, Lin AG, Meyer LJ, et al. Reflectance spectrophotometer: the dermatologists' sphygmomanometer for skin phototyping? The Journal of investigative dermatology. 2008;128:1633–40. doi: 10.1038/sj.jid.5701238. [DOI] [PubMed] [Google Scholar]
- 8.Xu LY, Koo J. Predictive value of phenotypic variables for skin cancer: risk assessment beyond skin typing. International journal of dermatology. 2006;45:1275–83. doi: 10.1111/j.1365-4632.2006.02999.x. [DOI] [PubMed] [Google Scholar]
- 9.Stern RS, Momtaz K. Skin typing for assessment of skin cancer risk and acute response to UV-B and oral methoxsalen photochemotherapy. Archives of dermatology. 1984;120:869–73. [PubMed] [Google Scholar]
- 10.Nicholas JS, Swearingen CJ, Kilmer JB. Predictors of skin cancer in commercial airline pilots. Occup Med (Lond) 2009;59:434–6. doi: 10.1093/occmed/kqp058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gogia RBM, Hirose R, Boscardin J, Chren MM, Arron ST. Fitzpatrick skin phototype is an independent predictor of squamous cell carcinoma risk after solid organ transplantation. Journal of American Academy of Dermatology. 2012 doi: 10.1016/j.jaad.2012.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams R. Generalized Ordered Logit/Partial Proportional Odds Models for Ordinal Dependent Variables. Stata Journal. 2006;6:58–82. [Google Scholar]
- 13.Azizi E, Lusky A, Kushelevsky AP, Schewach-Millet M. Skin type, hair color, and freckles are predictors of decreased minimal erythema ultraviolet radiation dose. Journal of the American Academy of Dermatology. 1988;19:32–8. doi: 10.1016/s0190-9622(88)70148-6. [DOI] [PubMed] [Google Scholar]
- 14.Guinot C, Malvy DJ, Latreille J, Ezzedine K, Galan P, Tenenhaus M, et al. Sun-reactive Skin Type in 4912 French adults participating in the SU.VI. MAX study. Photochemistry and photobiology. 2005;81:934–40. doi: 10.1562/2004-08-04-RA-260. [DOI] [PubMed] [Google Scholar]
- 15.Rubegni P, Cevenini G, Barbini P, Flori ML, Fimiani M, Andreassi L. Quantitative characterization and study of the relationship between constitutive-facultative skin color and phototype in Caucasians. Photochemistry and photobiology. 1999;70:303–7. [PubMed] [Google Scholar]
- 16.Lee JHTK. Relationship between constitutive skin color and ultraviolet light sensitivity in Koreans. Photodermatology, photoimmunology & photomedicine. 1999;15:231–5. doi: 10.1111/j.1600-0781.1999.tb00095.x. [DOI] [PubMed] [Google Scholar]
- 17.Leenutaphong V. Relationship between skin color and cutaneous response to ultraviolet radiation in Thai. Photodermatology, photoimmunology & photomedicine. 1996;11:198–203. doi: 10.1111/j.1600-0781.1995.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 18.Park SB, Suh DH, Youn JI. Reliability of self-assessment in determining skin phototype for Korean brown skin. Photodermatology, photoimmunology & photomedicine. 1998;14:160–3. doi: 10.1111/j.1600-0781.1998.tb00035.x. [DOI] [PubMed] [Google Scholar]
- 19.Sanclemente G, Zapata JF, Garcia JJ, Gaviria A, Gomez LF, Barrera M. Lack of correlation between minimal erythema dose and skin phototype in a Colombian scholar population. Skin Res Technol. 2008;14:403–9. doi: 10.1111/j.1600-0846.2008.00306.x. [DOI] [PubMed] [Google Scholar]
- 20.Chan JL, Ehrlich A, Lawrence RC, Moshell AN, Turner ML, Kimball AB. Assessing the role of race in quantitative measures of skin pigmentation and clinical assessments of photosensitivity. Journal of the American Academy of Dermatology. 2005;52:609–15. doi: 10.1016/j.jaad.2004.03.051. [DOI] [PubMed] [Google Scholar]
- 21.Taylor SC. Skin of color: biology, structure, function, and implications for dermatologic disease. Journal of the American Academy of Dermatology. 2002;46:S41–62. doi: 10.1067/mjd.2002.120790. [DOI] [PubMed] [Google Scholar]
- 22.Halder RM, Nootheti PK. Ethnic skin disorders overview. Journal of the American Academy of Dermatology. 2003;48:S143–8. doi: 10.1067/mjd.2003.274. [DOI] [PubMed] [Google Scholar]
- 23.Taylor SC. Morphology and physiology of skin color: defining differences in skin types I–III and IV–VI. Cosmetic Dermatol. 2003;16:5–8. [Google Scholar]
- 24.Bureau. UC. 2010 [Google Scholar]
- 25.Rijken F, Bruijnzeel PL, van Weelden H, Kiekens RC. Responses of black and white skin to solar-simulating radiation: differences in DNA photodamage, infiltrating neutrophils, proteolytic enzymes induced, keratinocyte activation, and IL-10 expression. The Journal of investigative dermatology. 2004;122:1448–55. doi: 10.1111/j.0022-202X.2004.22609.x. [DOI] [PubMed] [Google Scholar]
- 26.Tadokoro T, Yamaguchi Y, Batzer J, Coelho SG, Zmudzka BZ, Miller SA, et al. Mechanisms of skin tanning in different racial/ethnic groups in response to ultraviolet radiation. The Journal of investigative dermatology. 2005;124:1326–32. doi: 10.1111/j.0022-202X.2005.23760.x. [DOI] [PubMed] [Google Scholar]
- 27.Weinstock MA. Assessment of sun sensitivity by questionnaire: validity of items and formulation of a prediction rule. Journal of clinical epidemiology. 1992;45:547–52. doi: 10.1016/0895-4356(92)90104-u. [DOI] [PubMed] [Google Scholar]