Abstract
Sleep was examined as a process variable in relations between verbal and physical parent-child conflict and change in children’s internalizing and externalizing symptoms over time. Participants were 282 children at T1 (M age = 9.44 years; 48% girls), 280 children at T2 (M age = 10.41 years), and 275 children at T3 (M age = 11.35 years). Children reported on parent-child conflict, sleep was assessed with actigraphy, and parents reported on children’s internalizing and externalizing symptoms. Autoregressive effects for sleep and internalizing and externalizing symptoms were controlled to examine change over time. Supportive of intervening processes, physical parent-child conflict at T1 and increased change in internalizing and externalizing symptoms at T3 were indirectly related through their shared association with reduced sleep continuity (efficiency, long wake episodes) at T2. Findings build on a small but growing literature and highlight the importance of considering the role of sleep among relations between family conflict and child development.
Keywords: sleep, parent-child conflict, adjustment, actigraphy
Many studies have demonstrated that parent-child conflict (PCC) occurs frequently and is a robust predictor of children’s adjustment problems (Deardorff et al., 2013; Gershoff, 2002; Low & Stocker, 2005). Building on the established direct effects, scholars have considered mediating mechanisms to address why PCC may predict child maladjustment. Contemporary developmental perspectives contend that disruptions in bioregulatory systems including sleep may mediate relations between exposure to social stressors and children’s adaptation (El-Sheikh, 2011). Along this line and addressing recent calls in the literature (Erath & Tu, 2011), we examined whether sleep mediated relations between PCC and children’s internalizing and externalizing symptoms over 3 years using a community sample of school-aged children.
The term PCC refers to coercive acts and negative emotional expressions that parents direct toward children (Chang, Schwartz, Dodge, & McBride-Chang, 2003; Straus, Hamby, Finkelhor, Moore, & Runyan, 1998). For a more thorough assessment of PCC, we considered both verbal and physical conflict. Verbal conflict includes yelling, name calling, and making threats whereas physical conflict includes assault on the child’s body, including slapping or hitting with a closed fist. About 80% of children experience at least one form of verbal conflict and ~60% experience physical conflict each year (Straus et al., 1998). Further, verbal and physical PCC are well-established correlates of children’s internalizing (Deardorff et al., 2013; Low & Stocker, 2005) and externalizing symptoms (Deardorff et al., 2013; Gershoff, 2002). Although many mediators (e.g., emotion regulation, insecure parent-child relationship) have been established in relations between PCC and children’s adjustment, we are not aware of any studies that have considered the role of sleep as a potential mediator.
Sleep problems among otherwise typically developing school-aged children are common with estimates ranging from 20% to 40% (Mindell & Owens, 2010). Our reference to sleep problems refers to those in the non-clinical range including fewer sleep minutes and two indicators of sleep continuity, namely sleep efficiency (percentage of minutes spent asleep between sleep onset and morning wake time) and long wake episodes (number of wake episodes that exceed 5 minutes). A growing number of studies have found that sleep quantity and continuity may not uniformly impact children’s health and development (e.g., Michels et al., 2013) and recommendations have been made to examine various sleep parameters independently (Dewald, Meijer, Oort, Kerkhof, & Bögels, 2010). Accordingly, and because sleep quantity and continuity represent different constructs, we examined these sleep parameters separately. Further, sleep efficiency and long wake episodes were considered independently (rather than through a composite). Some children might wake often (resulting in reduced sleep efficiency) yet experience few long wake episodes because of their ability to fall back asleep quickly. Consequently, the examination of each allows for a more thorough assessment of sleep continuity. Sleep was measured with actigraphy, a wristwatch like device that provides an objective assessment of various sleep parameters (Sadeh, 2011b).
A growing literature has been focusing on sleep within the family context (El-Sheikh, 2011; El-Sheikh & Dahl, 2007) and findings indicate that family conflict is not conducive for children’s sleep. Dahl (1996) proposed that sleep and vigilance are antithetical such that a reduction in awareness is needed for adequate sleep. Thus, an optimal sleeping environment should be free from external threat. Prominent developmental theorists contend that children’s sense of safety is based largely on the family context (Bowlby, 1982; Cummings & Davies, 2010) and repeated exposure to such conflict may result in increased vigilance to detect threat, thereby disrupting sleep (El-Sheikh & Kelly, 2011). Attention has been given to the marital relationship with studies demonstrating that parental inter-partner conflict is a precursor of shorter sleep duration and poorer sleep continuity among children (Kelly & El-Sheikh, 2011, 2013a; Mannering et al., 2011; Rhoades et al., 2012). However, fewer studies have considered the extent that other familial stressors, including verbal and physical PCC have on children’s sleep.
Among clinical samples, abused children have poor sleep, including reduced sleep continuity (Glod, 2011; Glod, Teicher, Hartman, & Harakal, 1997; Sadeh et al., 1995). In community samples, there is some evidence supportive of relations between facets of the parent-child relationship, including PCC, and children’s sleep. A parenting style marked by blame and physical punishment was concurrently related to greater parent-reported child sleep problems (a general measure of sleep; Liu et al., 2000). A mother-child relationship characterized by less closeness and greater conflict in third grade predicted greater mother-reported child sleep problems (a general measure of sleep) 3 years later (Bell & Belsky, 2008). In a study using the first wave of the current investigation, greater verbal and physical PCC were related to poorer actigraphy-based sleep continuity and more self-reported sleep/wake problems in children (El-Sheikh, Kelly, Bagley, & Wetter, 2012). Further, greater inter-partner conflict at 9 months of age predicted increases in parent-reported child sleep problems at 4.5 years through the indirect effect of verbal and physical father-child conflict at 27 months of age (Rhoades et al., 2012). Collectively, these findings provide support for relations between PCC and children’s sleep, although there is a continued need to use objective measures of sleep (e.g., actigraphy) and multi-informant approaches. Further, exposure to family conflict is related to increased vigilance for extended periods (McCrory et al., 2011) thereby potentially compromising sleep over time (Kelly & El-Sheikh, 2013a). Consequently, the use of multi-wave designs is important to gain greater understanding of the long-term influence that PCC has on children’s sleep and adjustment.
Sleep plays a pivotal role in children’s adjustment. In community samples, sleep problems are related to internalizing (e.g., Alfano, Zakem, Costa, Taylor, & Weems, 2009) and externalizing symptoms (e.g., Quach, Hiscock, Canterford, & Wake, 2009). Reduced sleep duration, as measured by actigraphy, was concurrently related to greater parent-reported externalizing symptoms in children (Holley, Hill, & Stevenson, 2011). In a three-wave study that spanned 3 years, and with an independent sample from the one used in the current investigation, El-Sheikh, Bub, Kelly, and Buckhalt (2013) found that initial levels and increases in self-reported sleep wake problems over time predicted increases in greater internalizing and externalizing symptoms in the final wave when children were 10.
Despite evidence of relations between PCC and children’s sleep as well as between sleep and adjustment, no study to our knowledge has examined whether sleep mediates relations between PCC and children’s adjustment. However, sleep has been considered among relations between other environmental stressors and children’s development. Both exposure to community violence and peer victimization were related to children’s poorer academic performance through their shared relations with greater self-reported sleep/wake problems (Lepore & Kliewer, 2013). Further, verbal and physical inter-partner conflict were related to children’s internalizing and externalizing symptoms through both higher levels of emotional insecurity about the marital relationship and actigraphy measured sleep problems (El-Sheikh, Buckhalt, Cummings, & Keller, 2007). Building on these studies, it seems plausible that sleep might mediate relations between other environmental and familial stressors, including PCC, and children’s adjustment.
The Current Study
Using a diverse, community-based sample and three waves of data (T1 = age 9; T2 = age 10; T3 = age 11), we examined children’s sleep at T2 as a mediator between verbal and physical PCC at T1 and internalizing and externalizing symptoms at T3. Because parental inter-partner conflict and PCC often co-occur (Cox, Paley, & Harter, 2001), we controlled for verbal and physical inter-partner conflict in an attempt to isolate the unique influence of PCC. To reduce same reporter bias, children reported on PCC, actigraphy was used to measure sleep, and parents reported on children’s adjustment. Following recommendations and because of the comorbid nature of relations between these adjustment domains (Coulombe, Reid, Boyle, & Racine, 2011), we controlled for children’s internalizing symptoms while examining externalizing symptoms and vice versa. This approach allows for the assessment of whether PCC and sleep uniquely influence certain facets of adjustment. Similarly, both verbal and physical PCC were considered simultaneously as were each of the sleep parameters. We hypothesized that greater PCC at T1 and increased internalizing and externalizing symptoms at T3 would be indirectly related through their shared associations with fewer sleep minutes and poorer sleep continuity (reduced sleep efficiency, greater long wake episodes) at T2
Method
Participants
The current investigation consisted of three waves of data spanning 3 years and is part of a larger study examining biopsychosocial influences on a range of developmental outcomes (Auburn University Sleep Study). To recruit families at T1, over 2,700 letters inviting participation were distributed to children at public schools in the Southeastern United States. Interested families were asked to call our research laboratory. Of the 314 families who contacted our lab at T1 and met inclusion criteria (child not having a diagnosed sleep disorder or a learning disability based on mother report), 282 participated (90%). Exclusion criteria were implemented to reduce potential confounds in the larger study yet were not overly conservative.
Of the 282 children at T1 (data collected in 2009–2010), 48% were girls and 52% were boys (M age = 9.44 years, SD = 8.55 months); 65% were European American (EA) and 35% were African American (AA). Socioeconomic status (SES) was measured by the income-to-needs-ratio, which is computed using family size, family income, and the federal cutoff (< 1 indicates below the poverty line; U.S. Department of Commerce; www.commerce.gov). The mean income-to-needs ratio was 1.71 (SD = 1.04) indicating that on average, families lived 170% above the poverty threshold (Range = .27 to 4.10). Further, 32% of families lived below the poverty line. Mothers’ reports on the Puberty Development Scale (1 = prepubertal, 2 = early pubertal, 3 = midpubertal, 4 = late pubertal, 5 = postpubertal; Petersen, Crockett, Richards, & Boxer, 1988) indicated that on average both boys (M = 1.44, SD =.30) and girls (M = 1.71, SD = .44) were prepubertal. Most children lived with their biological mother (n = 252); of these children, 58% (n = 146) also lived with their biological father, 21% (n = 52) lived with their mothers’ partner (e.g., stepfather, boyfriend), and 21% (n = 54) lived with a single mother. Sixteen children lived with either a single father (n = 1), father and step-mother (n = 11), or adoptive parents (n = 4). The remaining 14 children lived with extended family members (e.g., grandparents; aunts/uncles). For simplicity, we refer to the child’s primary caregivers as parents. In analyses, single-mother status and family composition were considered as control variables.
Approximately one year later (M days between T1 and T2 = 350, SD = 28 days), 79% of the original sample (224 families) returned for T2 (collected in 2010–2011). To enhance power associated with attrition, we also recruited 56 additional families at T2. In longitudinal studies, it is not atypical to include new participants after the first wave (Graham, Taylor, & Cumsille, 2001; Mistler & Enders, 2012). In total, 280 families participated at T2 (45% girls; M age = 10.41, SD = 8.06); 63% EA and 37% AA. Average pubertal status at T2 was 1.53 (SD = .37) for boys and 1.96 (SD = .62) for girls, which corresponds to a prepubertal status for boys and nearly an early pubertal status for girls (Petersen et al., 1988). Of the 56 children who began participation at T2, the majority lived with their biological mother (n = 49); of these children, 47% (n = 23) also lived with their biological father, 16% (n = 8) lived with their mothers’ partner, and 37% (n = 18) lived with a single mother. The seven remaining children lived with adoptive parents (n = 2) or other family members (n = 5). Nine mothers who were in a relationship at T1 were single at T2; three who were single at T1 were in a relationship at T2.
Nearly one year following T2 (M days between T2 and T3 = 336, SD = 34 days), 275 families returned for T3 (98% of families who participated at T2; 47% girls; M age = 11.35 years, SD = 8.12 months); 63% EA and 37% AA. Data were collected during 2011–2012. Average pubertal status at T3 was 1.80 (SD = .55) for boys and 2.35 (SD = .62) for girls, which indicates a prepubertal status for boys and early pubertal status for girls (Petersen et al., 1988).
Independent-samples t tests and χ2 analyses were used to determine whether retained and attrited families (from T1 to T2 and from T2 to T3) differed on control and focal study variables. No differences were found. We also assessed whether families who began participation at T2 differed on study variables from families who began participation at T1. Children who began participation at T2 came from lower SES homes t(231) = −2.78, p < .01, and had fewer sleep minutes t(278) = −2.17, p < .05. No other differences were found. Note that full information maximum likelihood estimation was used to handle missing data (Acock, 2005) and primary study analyses were also conducted with the exclusion of the 56 families who began participation at T2; results were identical in nature to those reported with the inclusion of the 56 families. Similarly, we conducted analyses that did not include children from one-parent households and the results were very similar to analyses based on the full sample.
Procedure
Families visited our research laboratory during each study wave. Children completed questionnaires with a trained interviewer while parents completed measures in a neighboring room. At T1 and T2, children were instructed to wear an actigraph on their non-dominant wrist for 7 consecutive nights. Parents completed sleep diaries to cross validate actigraphy-based sleep and wake times. Actigraphy assessments typically occurred shortly before the lab visit (M at T1 = 3.47 days, SD = 8.73; M at T2 = 4.80 days, SD = 12.31) and during the regular school-year, excluding holidays and vacations. Only data from medication-free nights were used. Approval from the institution’s internal review board was obtained and participants gave informed consent and assent. Families were compensated monetarily for participation. Based on child reports of PCC, two families were reported to the Department of Human Resources for suspected child abuse at T2; neither family withdrew from the study.
Measures
Parent-child conflict
At T1, children reported on the frequency of PCC in the past year using the Parent-Child Conflict Tactics Scale (CTSPC; Straus, 1999). The Verbal Aggression (e.g., “Your father shouted, yelled, or screamed at you”) and Physical Aggression (e.g., “Your mother hit you with a fist or kicked you hard”) scales were examined. Children completed the CTSPC twice, once for mother- and once for father-child conflict. Likert-type response choices for each item ranged from 0 (this has not happened) to 6 (it has happened more than 20 times). Children’s reports of mothers’ and fathers’ verbal PCC and physical PCC were correlated (r = .72 for verbal conflict and .76 for physical conflict), and thus overall mean averages were created for verbal and physical PCC. Cronbach’s alpha = .76 for verbal PCC and .82 for physical PCC. For children with single mothers (n = 54), the PCC composite was based on mother-child conflict (single parent status was controlled in all analyses). Analyses comparing PCC for children with and without fathers did not yield significant differences.
Sleep
Actigraphic assessments occurred at T1 and T2. The actigraphs were Octagonal Basic Motionloggers (Ambulatory Monitoring Inc., Ardsley, NY) and data were analyzed using ActionW2 software. Motion was measured in 1-min epochs using zero crossing mode and Sadeh’s scoring algorithm (Sadeh, Sharkey, & Carskadon, 1994). Actigraphy data that showed poor correspondence with parent reports were excluded; 3% of nights were excluded at T1 and 4% of nights were excluded at T2. The actigraphs and software packages have demonstrated reliability and validity based on comparisons with polysomnography (Sadeh et al., 1994).
The inclusion of multiple sleep parameters is recommended (Sadeh, Raviv, & Gruber, 2000). We assessed: (a) Sleep Minutes - number of minutes scored as sleep between sleep onset and morning wake time; (b) Sleep Efficiency - % of epochs scored as sleep between sleep onset and waking; and (c) Long Wake Episodes - number of wake episodes ≥ 5 minutes.1 At T1, 57% of children had 7 nights of valid data, 18% had 6 nights, 12% had 5 nights, 6% had either 3 or 4 nights, and 7% did not have any actigraphy data (M = 5.89 nights, SD = 1.89 nights). At T2, 42% of children had 7 nights of valid data, 26% had 6 nights, 19% had 5 nights, 10% had 3 or 4 nights, 2% had 1 or 2 nights, and 1% did not have any data (M = 5.84 nights, SD = 1.40 nights). These rates of valid actigraphy data are considered very good (Acebo et al., 1999). Medication known to influence sleep (e.g., Benadryl, cough syrup), not wearing the actigraph and technical problems accounted for missing nights. Researchers have recommended that actigraphy assessments include at least 5 nights (Acebo et al., 1999; Sadeh, 2011a). Secondary analyses excluding cases that had fewer than 5 nights yielded an identical pattern of study results and thus, all cases were retained to enhance statistical power. Using the maximum number of nights with valid actigraphy data, alphas were as follows: sleep minutes (α = .85 at T1 and .78 at T2), sleep efficiency (α = .90 at T1 and .89 at T2), and long wake episodes (α = .77 at T1 and .80 at T2). Thus, sleep parameters were stable across the week and each variable was composited for analyses (i.e., across all available nights).
Internalizing and externalizing symptoms
At T2 and T3, parents completed the 280-item Personality Inventory for Children (PIC; Wirt, Lachar, Klinedinst, & Seat, 1990). The Internalizing and Externalizing scales were pertinent to the current investigation and have been used frequently in the child development literature (e.g., Kelly & El-Sheikh, 2013b; Leve, Winebarger, Fagot, Reid, & Goldsmith, 1998). The Internalizing scale assessed symptoms of depression, anxiety, worry, fear, and psychosomatic problems whereas the Externalizing scale assessed symptoms of impulsivity, noncompliance, disruptive behavior, delinquent behavior, and aggression. Six items pertaining to sleep were removed from the Internalizing scale prior to analyses. Mothers’ and fathers’ reports of internalizing (r = .56 at T2 and .70 at T3, ps < .001) and externalizing symptoms (r = .72 at T2 and .71 at T3, ps < .001) were correlated and thus were averaged at T2 and T3; mothers’ scores were used when fathers’ scores were not available. Cronbach’s alphas for the internalizing and externalizing scales were .75 and .86 at T2 and .84 and .92 at T3, respectively. Because the PIC T scores are age and gender corrected, raw scores were used for longitudinal analyses. The clinical cutoff T scores for internalizing and externalizing is ≥ 60 (Lachar & Gruber, 1995): 30 children at T2 and 27 children at T3 surpassed the clinical cutoff for internalizing symptoms. For externalizing symptoms, 26 children at T2 and 23 children at T3 surpassed the clinical cutoff.
Inter-partner conflict
At T2, children from two-parent families reported on the frequency of their parents’ inter-partner conflict in the last year using the Revised Conflict Tactics Scale (CTS2; Straus, 1995). The Psychological/Verbal (8 items; e.g., “My mother called my father fat or ugly”) and Physical Aggression scales (9 items; “My father twisted my mother’s arm or hair”) were used. Children’s reports of mothers’ and fathers’ verbal (r = .77, p<.001) and physical conflict (r = .86, p<.001) were correlated, and thus an overall mean average was created for inter-partner verbal and physical conflict. Cronbach’s alpha = .80 for verbal and .87 for physical inter-partner conflict. Verbal and physical inter-partner conflict were included as covariates. Data were treated as missing for children from one-parent homes.
Results
Plan of Analysis
A path model was fit to examine sleep (sleep minutes, sleep efficiency, and long wake episodes) as a mediator of relations between verbal and physical PCC and children’s internalizing and externalizing symptoms over three waves of data spanning 3 years. For more conservative estimates, both verbal and physical PCC were assessed in the same model. Similarly, all three sleep parameters and internalizing and externalizing symptoms were examined simultaneously. Autoregressive effects were included in the model for sleep and adjustment, which allows for the assessment of change in the predicted variable and helps reduce bias in parameter estimates (Cole & Maxwell, 2003). Thus, PCC at T1 was examined as a predictor of change in sleep at T2 and adjustment at T3, and sleep at T2 was examined as a predictor of change in adjustment at T3.
As will be explicated in the main results section, mediation effects were not supported. Thus, while retaining our main study objectives, we considered sleep at T2 as an intervening variable (vs. mediator) among relations between PCC at T1 and children’s adjustment at T3. It is not uncommon for researchers to consider a variable as both a mediator and intervening process (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In both a mediation model and intervening model, the independent variable (i.e., PCC) is significantly related to the process variable (i.e., sleep), which in turn is related to the outcome variable (i.e., internalizing and externalizing symptoms). In a mediation model but not an intervening variable model, the relation between the independent variable and outcome variable is significant prior to the inclusion of the process variable. Models supportive of intervening processes suggest that the development and change in the intervening mechanism over time is required to observe the indirect effect between the independent and dependent variables (MacKinnon et al., 2002).
Monte Carlo simulation was used to assess indirect effects (for mediation and intervening processes; Preacher & Selig, 2012). This bootstrapping method produces confidence intervals of the hypothesized indirect effects utilizing 20,000 iterations, resampling from the distributions of each direct effect. Selig and Preacher’s (2008) interactive tool was used for creating confidence intervals to test indirect effects, with an indirect effect being demonstrated when the confidence intervals do not contain zero.
Data points that surpassed 4 SDs were recoded as the highest observed value below 4 SDs (Cousineau & Chartier, 2010). Specifically, seven values were recoded for the PCC variables, 13 for the sleep variables, and nine for the adjustment variables. Verbal PCC at T1, physical PCC at T1, and sleep efficiency at T1 and T2 were skewed and log transformed.
We used Δχ2 tests to consider controlling for many known correlates of primary study variables. Child sex and ethnicity each significantly influenced model fit and were included. These variables were treated as time invariant and were allowed to covary with each other as well as with verbal and physical PCC at T1 and to predict sleep at T2 and adjustment at T3. SES at T1, T2, and T3 were each considered but only SES at T2 was influential; it was allowed to predict sleep at T2 and to covary with child sex and ethnicity. Single mother status at T1 was controlled and was allowed to covary with child sex, ethnicity, as well as with verbal and physical PCC at T1; single mother status at T2 and T3 were not influential. Finally, verbal and physical inter-partner conflict at T2 were retained as covariates and were allowed to covary with each other and to predict sleep at T2 and adjustment at T3. Pubertal status at all three waves and chronic illness were also considered but neither was retained.
Analyses were conducted using Amos 21 (Arbuckle, 2012). In the final model, verbal and physical PCC were allowed to covary. In addition, the residual variances among the sleep variables at T2 were allowed to correlate as were the residual variances among internalizing and externalizing symptoms at T3. Acceptable model fit included satisfying at least two of the following three criteria: χ2/df < 3, CFI > .90, and RMSEA ≤ .08 (Browne & Cudeck, 1993); the model satisfied these criteria.
Preliminary Analyses
Means, standard deviations, and bivariate correlations among study variables are presented in Table 1. Based on child-reported PCC, 61% of mothers and 60% of fathers used at least one form of verbal conflict within the last year. Similarly, 61% of mothers and 64% of fathers used at least one form of physical conflict against the child. Based on actigraphy, children slept on average 7 hours and 36 minutes a night at T1 and 7 hours and 24 minutes at T2.
Table 1.
Correlations among Study Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parent- child verbal conflict T1 | - | |||||||||||
| 2. Parent- child physical conflict T1 | .64*** | - | ||||||||||
| 3. Sleep minutes T1 | −.07 | .01 | - | |||||||||
| 4. Sleep efficiency T1 | −.02 | −.02 | .69*** | - | ||||||||
| 5. Long wake episodes T1 | .05 | −.05 | −.62*** | −.88*** | - | |||||||
| 6. Sleep minutes T2 | .06 | .01 | .35*** | .26*** | −.28*** | - | ||||||
| 7. Sleep efficiency T2 | −.04 | .05 | .24*** | .39*** | −.40*** | .60*** | - | |||||
| 8. Long wake episodes T2 | −.08 | .01 | −.23*** | −.38*** | .43*** | −.64*** | −.90*** | - | ||||
| 9. Internalizing symptoms T2 | .01 | −.01 | −.18** | −.15* | .16* | −.14* | −.15* | .07 | - | |||
| 10. Externalizing symptoms T2 | .14* | .14* | −.14* | −.21** | .20** | −.04 | −.04 | .05 | .56*** | - | ||
| 11. Internalizing symptoms T3 | .02 | −.03 | −.16* | −.18* | .25*** | −.06 | −.15* | .15* | .73*** | .51*** | - | |
| 12. Externalizing symptoms T3 | .02 | .03 | −.04 | −.19* | .18* | −.01 | .05 | .16 * | .43*** | .79*** | .61*** | - |
|
| ||||||||||||
| M | 3.13 | 3.47 | 456 min | 88.27 | 3.58 | 444 min | 88.38 | 3.47 | 4.42 | 5.08 | 4.04 | 4.53 |
| SD | 3.78 | 4.61 | 58 min | 7.60 | 2.13 | 48 min | 7.29 | 2.29 | 3.88 | 4.39 | 3.74 | 4.12 |
Note. T1 = data collected at Time 1; T2 = data collected at Time 2; T3 = data collected at Time 3. For average sleep minutes at T1, 456 min translates into 7 hrs and 36 min. Similarly, for sleep minutes at T2, 444 min translates into 7 hrs and 24 min.
p < .05;
p < .01;
p < .001
Parent-Child Conflict and Children’s Adjustment: The Intervening Role of Sleep
To consider sleep as a mediator of associations between PCC and children’s adjustment, the direct relations between verbal and physical PCC at T1 and change in internalizing and externalizing symptoms from T2 to T3 were first examined. No such statistically significant effects were discovered, which concluded the assessment of sleep as a mediator of effects. Next, the sleep parameters were entered into the model (see Figure 1) to assess their roles as intervening variables. The model was a good fit to the data, χ2(82) = 166.85, p < .001; χ2/df = 2.03; CFI = .96; RMSEA = .06ns, 95% CI [.04 to .07]. From T1 to T2, the autoregressive effects (not shown in the Figure for clarity) were significant for sleep minutes (B = .24, β = .29, p < .001), sleep efficiency (B = .25, β = .28, p < .001), and long wake episodes (B = .30, β = .31, p < .001). Similarly, the autoregressive effects were significant for children’s internalizing (B = .69, β = .73, p < .001) and externalizing symptoms (B = .72, β = .78, p < .001) from T2 to T3. In total, the model explained 17% of the variance in sleep minutes, 18% in sleep efficiency, 18% in long wake episodes, 57% in internalizing symptoms, and 64% in externalizing symptoms.
Figure 1.
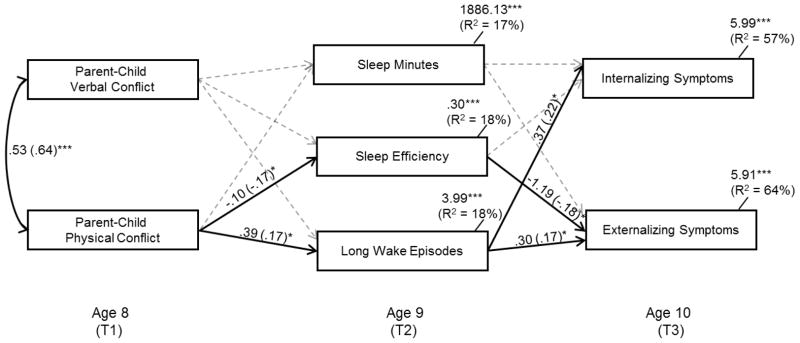
Examination of children’s sleep at T2 as an intervening process in the association between parent-child conflict at T1 and children’s internalizing and externalizing symptoms at T3. Model Fit: χ2(82) = 166.85, p < .001; χ2/df = 2.03; CFI = .96; RMSEA = .06ns, 95% CI [.04 to .07]. Residual variances among the sleep variables were allowed to correlate as were the residual variances among internalizing and externalizing symptoms. For ease of interpretation, statistically significant lines are solid and non-significant lines are dotted. For autoregressive effects, sleep minutes, sleep efficiency, and long wake episodes at T1 were controlled as were internalizing and externalizing symptoms at T2. Additional covariates were child sex, ethnicity, SES at T2, single mother status at T1 and verbal and physical inter-partner conflict at T2.
*p < .05; **p < .01; ***p < .001
Many control variables shared significant associations with the primary study variables (not shown in Figure). Child male status was related to reduced sleep efficiency (B =−.19, β = −.15, p = .01) and greater long wake episodes at T2 (B =.59, β = .13, p = .03). African American status was associated with greater sleep efficiency at T2 (B =.12, β = .17, p = .01) and fewer long wake episodes (B = −.74, β = −.16, p = .02). A higher SES was related to more sleep minutes at T2 (B = 6.32, β = .13, p = .05). Lastly, greater verbal inter-partner conflict at T2 was related to more internalizing symptoms at T3 (B = .12, β = .13, p = .03)
Greater physical PCC at T1 predicted a decrease in sleep efficiency (ΔR2 = 4%) and an increase in long wake episodes at T2(ΔR2 = 4%; Figure 1). Reduced sleep efficiency at T2 predicted greater externalizing symptoms at T3(ΔR2 = 3%) and more frequent long wake episodes at T2 predicted increased levels of internalizing (ΔR2 = 5%) and externalizing symptoms at T3 (ΔR2 = 4%).
Tests of Indirect Effects
Given that neither verbal nor physical PCC at T1 were directly related to changes in children’s adjustment from T2 to T3, all significant indirect effects support an intervening rather than a mediating process. Based on Monte Carlo simulation techniques, the indirect effect for children’s reduced sleep efficiency at T2 in the relation between greater parent-child physical conflict at T1 and increased externalizing symptoms at T3 was significant (95% CI [−.36 to −.01]). Similarly, the indirect effects for greater long wake episodes at T2 in the association between higher levels of parent-child physical conflict at T1 and increased internalizing (95% CI [.01 to .38]) and externalizing symptoms (95% CI [.001 to .40]) over time were significant.2,3
Discussion
To gain a nuanced understanding of associations between family functioning and children’s adjustment, we examined children’s sleep as a mediator of relations between PCC and internalizing and externalizing symptoms over 3 years. For more conservative model testing, autoregressive effects were controlled as were many influential covariates including verbal and physical inter-partner conflict. Shared method variance was reduced by using children’s reports of PCC, actigraphic assessments of sleep, and parent reports of children’s adjustment. Supportive of an intervening rather than a mediating process, physical PCC predicted poorer sleep continuity, which in turn predicted an increase in adjustment problems over time. Findings build on the literature and explicate some mechanisms of risk.
There is growing support for relations between inter-partner conflict and children’s sleep (e.g., Kelly & El-Sheikh, 2011, 2013a; Mannering et al., 2011; Rhoades et al., 2012). With an independent sample from the one used in the present study, cross-sectional evidence indicates that shorter sleep duration and poorer sleep continuity/quality served as intervening processes in relations between inter-partner conflict and children’s adjustment problems (El-Sheikh et al., 2007). Findings from the current study advance this relatively young literature by demonstrating that even after controlling for the effects of exposure to parental inter-partner conflict, sleep continuity/quality functioned as an intervening variable linking physical PCC and children’s externalizing and internalizing symptoms. Specifically, physical PCC predicted reduced sleep efficiency and greater long wake episodes (but not sleep minutes) 1 year later. In turn, reduced sleep efficiency predicted increased levels of externalizing symptoms over time and greater long wake episodes predicted increases in both internalizing and externalizing symptoms. Collectively, across studies, a clear picture is emerging: family stress including PCC may lead to children’s adjustment problems through its shared relation with disruptions in sleep.
Findings build on an expanding literature of relations between parent-child relationship processes and children’s sleep (Bell & Belsky, 2008; Liu et al., 2000; Rhoades et al., 2012). Feelings of safety facilitate reduction in vigilance and better sleep (Dahl, 1996). Children who experience physical PCC may feel unsafe and maintain environmental awareness, even during the night, leading to poor sleep continuity, as seen in our study. Further, based on the longitudinal design, physical PCC forecasted poorer sleep continuity 1 year later. Sustained exposure to conflict may result in a recalibration of neural networks and physiological systems to maintain vigilance and increased hypersensitivity for extended periods (Graham, Fisher, & Pfeifer, 2013; McCrory et al., 2011). Although such enhanced reactivity may be adaptive in the short term (e.g., the night of the aggressive incident), there may be adverse effects over time. For instance, children may continue to maintain heightened vigilance despite the absence of threat. It is also plausible that higher conflict families may differ from lower conflict families in many ways including more family chaos, less parental monitoring, and greater conflict among family members (Krishnakumar, Buehler, & Barber, 2003), all of which could spillover and influence sleep. Overall, we offer these explanations as tentative pending further examination.
Physical but not verbal PCC predicted change in children’s sleep. Much attention has been given to disentangling the effects that verbal and physical PCC have on children’s development and findings have been complex. In some studies, physical PCC had a more detrimental influence on children’s development (Berlin et al., 2009); others found more support for verbal PCC (Evans, Simons, & Simons, 2012) or no differences between PCC domains (McKee et al., 2007). In one of the few studies to include sleep (El-Sheikh et al., 2012), verbal and physical PCC were related to children’s sleep (using the first wave of the current study). However, the study was cross-sectional, thus suggesting that verbal and physical PCC were related concurrently to sleep. In the current study, PCC was examined as a predictor of change in sleep over 1 year (T1 to T2). Physical PCC may have both an immediate and long term influence on children’s sleep. Children often perceive physical PCC as more aggressive, threatening, and intrusive (McKee et al., 2007), which may lead to extended periods of vigilance and night awakenings. Our findings are also consistent with results from the clinical literature in which physical abuse had the most marked influence on children’s sleep (Glod, 2011).
Physical PCC predicted change in sleep efficiency and long wake episodes but not sleep minutes. This is consistent with past research that found a general measure of family stress (Sadeh et al., 2000) and PCC (El-Sheikh et al., 2012) to be correlates of sleep quality but not quantity. Following sleep loss, an intrinsic compensatory mechanism may extend the sleep period so that sleep minutes are not diminished (Sadeh, Gruber, & Raviv, 2003). Thus, children who are exposed to PCC and experience poorer sleep continuity may extend the sleep period to compensate for sleep debt.
Findings add to a growing literature supportive of relations between poorer sleep continuity and increased change in children’s adjustment problems (e.g., Quach et al., 2009). Reduced sleep continuity may disrupt processes mediated by the prefrontal cortex, which plays an important role with the executive functioning needed for emotion regulation and adjustment (Dahl, 1996; Jones & Harrison, 2001; Muzur, Pace-Schott, & Hobson, 2002). For example, poor sleep continuity may disrupt emotional memory coding. Individuals who do not receive adequate sleep often recall negative memories rather than neutral or positively themed memories, which may impact adjustment (Walker & van der Helm, 2009). Finally, inadequate sleep may disrupt facets of emotional intelligence and constructive thinking skills including reduced empathy toward others, poor impulse control, stress management, behavioral coping skills, and decreased positive thinking, all of which may overlap with adjustment problems (Killgore et al., 2008).
Inconsistent with expectations, PCC at age 8 did not predict children’s adjustment at age 10. It is not evident why direct relations were not observed. The conservative nature of assessments including controlling for autoregressive effects as well as many influential covariates and the extended time lag between assessments (i.e., 2 years) may have contributed to the null effects. Findings provide support for an intervening rather than mediating process, which is not uncommon in the literature (MacKinnon et al., 2002; MacKinnon, Krull, & Lockwood, 2000). Specifically, PCC at age 8 and change in adjustment at age 10 were indirectly related through their shared relations with changes in sleep at age 9. The intervening rather than mediation effect suggests that the development and change in sleep continuity from ages 8 to 9 is required to observe the indirect effect between physical PCC at age 8 and children’s adjustment at age 10 (MacKinnon et al., 2002). Further, the demonstration of a direct association between PCC at age 8 and children’s adjustment at age 10 is not a necessary criteria for our conceptual model, which hypothesizes that PCC ultimately influences children’s adjustment by setting in motion disruptions in bioregulatory systems in the child. PCC is no less a predictor in an intervening model because in its absence, the development of the unfolding series of sleep and adjustment problems would not have occurred (Emery, Fincham, & Cummings, 1992).
Children in the sample may not have received adequate sleep. Although there is no consensus about the amount of needed sleep (Lumeng, 2010), average sleep minutes per night (M = 7 hrs and 36 min at T1; 7 hrs and 24 min at T2 based on actigraphy) was far under the National Sleep Foundation’s (2009) recommendation of 10 to 11 hours for sleep duration (i.e., time spent in bed [actigraphy based sleep duration in our sample was 8 hrs and 37 min at T1 and 8 hrs and 23 min at T2]). Further, compared to other studies, children in our sample received less sleep. Among 7- to 13-year-old Israeli children, mean sleep minutes ranged from 7 hrs and 37 min to 8 hrs and 40 min across age and sex (Sadeh et al., 2000). Paavonen, Fjällberg, Steenari, and Aronen (2002) found that 7- to 13-year-old children slept on average 7 hrs and 56 min. Many children in our sample faced economic disadvantage (34% below the poverty line), which is a risk factor for reduced sleep (Buckhalt, El-Sheikh, Keller, & Kelly, 2009). Also, many children lived in rural communities and had extended commute times to school.
Findings have several clinical implications. Practitioners who treat children’s sleep problems may want to consider the home environment and facets of the parent-child relationship. Even non-clinical sleep problems (e.g., night wakings) can have an adverse influence on children’s development and should not be overlooked (Sadeh et al., 2003). Further, of relevance to policy makers, results highlight the critical role of sleep for children’s adjustment.
This study is not without limitations. The recruitment strategy of sending letters home with children from school resulted in a low, albeit common initial response rate of ~12% (MacGregor & McNamara, 1995). Comparisons between study participants and 2010 U.S. Census data indicated that our sample was somewhat similar to the population of the county from which it was drawn in terms of ethnicity (23% AA [35% were AA in our sample]), percent living below the poverty line (22% [32% in our sample]), and percent in single parent households (34% [21% in our sample]). Because of their underrepresentation in the literature, the inclusion of many African American children and those exposed to economic adversity is a study strength.
Regarding additional limitations, the use of a community sample confines inferences about clinical populations. Given that PCC predicted sleep using a community sample, findings are likely more robust in more violent circumstances. Further, although actigraphy is useful, other sleep assessments hold promise for advancing the sleep and family literature. Polysomnography would help understand how PCC impacts sleep stages. There is also a need to consider other facets of the parent-child relationship (e.g., parental warmth) that may moderate relations. Lastly, sleep was measured during the regular school year when children tend to have a more structured schedule; this may have resulted in null effects for both variability in sleep onset time and sleep onset latency as neither was related to PCC or adjustment. Despite limitations, findings support the important role of sleep in the connecting exposure to parent-child aggression with children’s adjustment.
Acknowledgments
The project described was supported by Grant Number R01HL093246 from the National Heart, Lung, and Blood Institute awarded to Mona El-Sheikh. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We wish to thank our lab staff, most notably Bridget Wingo and Lori Elmore-Staton, for data collection and preparation, and the school personnel and participating families.
Footnotes
Sleep onset latency (total minutes between bed time and sleep onset time) and variability in sleep onset time across the week of actigraphy were also considered. However, neither was related to PCC or children’s adjustment and thus, these sleep parameters were excluded.
Models were also fit while examining each sleep and adjustment variable separately (as opposed to including all variables in the same model). No differences were found.
Gender, ethnicity, and SES were examined as moderators of relations between PCC, sleep, and adjustment (moderated mediation). No significant interaction effects emerged.
Work was performed at Auburn University
Contributor Information
Ryan J. Kelly, University of New Mexico
Brian T. Marks, Auburn University
Mona El-Sheikh, Auburn University.
References
- Acebo C, Sadeh A, Seifer R, Tzischinsky O, Wolfson A, Hafer A, Carskadon M. Estimating sleep patterns with activity monitoring in children and adolescents: How many nights are necessary for reliable measures? Sleep. 1999;22:95–103. doi: 10.1093/sleep/22.1.95. [DOI] [PubMed] [Google Scholar]
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67:1012–1028. doi: 10.1111/j.1741-3737.2005.00191.x. [DOI] [Google Scholar]
- Alfano CA, Zakem AH, Costa NM, Taylor LK, Weems CF. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depression and Anxiety. 2009;26:503–512. doi: 10.1002/da.20443. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. IBM SPSS Amos 21.0 user’s guide. Chicago: Small Waters Corporation; 2012. [Google Scholar]
- Bell BG, Belsky J. Parents, parenting, and children’s sleep problems: Exploring reciprocal effects. British Journal of Developmental Psychology. 2008;26:579–593. doi: 10.1348/026151008x285651. [DOI] [Google Scholar]
- Berlin LJ, Ispa JM, Fine MA, Malone PS, Brooks-Gunn J, Brady-Smith C, Bai Y. Correlates and consequences of spanking and verbal punishment for low-income White, African American, and Mexican American toddlers. Child Development. 2009;80:1403–1420. doi: 10.1111/j.1467-8624.2009.01341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Retrospect and prospect. American Journal of Orthopsychiatry. 1982;52:664–678. doi: 10.1111/j.1939-0025.1982.tb01456.x. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Buckhalt JA, El-Sheikh M, Keller PS, Kelly RJ. Concurrent and longitudinal relations between children’s sleep and cognitive functioning: The moderating role of parent education. Child Development. 2009;80:875–892. doi: 10.1111/j.1467-8624.2009.01303.x. [DOI] [PubMed] [Google Scholar]
- Chang L, Schwartz D, Dodge KA, McBride-Chang C. Harsh parenting in relation to child emotion regulation and aggression. Journal of Family Psychology. 2003;17:598–606. doi: 10.1037/0893-3200.17.4.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112:558. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Coulombe JA, Reid GJ, Boyle MH, Racine Y. Sleep problems, tiredness, and psychological symptoms among healthy adolescents. Journal of Pediatric Psychology. 2011;36:25–35. doi: 10.1093/jpepsy/jsq028. [DOI] [PubMed] [Google Scholar]
- Cousineau D, Chartier S. Outliers detection and treatment: A review. International Journal of Psychological Research. 2010;3:58–67. [Google Scholar]
- Cox MJ, Paley B, Harter K. Interparental conflict and parent–child relationships. In: Grych JH, Fincham FD, editors. Interparental conflict and child development: Theory, research, and applications. New York, NY: Cambridge University Press; 2001. pp. 249–272. [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. New York, NY: Guilford Press; 2010. [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology. 1996;8:3–27. doi: 10.1017/s0954579400006945. [DOI] [Google Scholar]
- Deardorff J, Cham H, Gonzales NA, White RMB, Tein JY, Wong JJ, Roosa MW. Pubertal timing and Mexican-origin girls’ internalizing and externalizing symptoms: The influence of harsh parenting. Developmental Psychology. 2013;49:1790–1804. doi: 10.1037/a0031016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewald JF, Meijer AM, Oort FJ, Kerkhof GA, Bögels SM. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Medicine Reviews. 2010;14:179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011. [Google Scholar]
- El-Sheikh M, Bub KL, Kelly RJ, Buckhalt JA. Children’s sleep and adjustment: A residualized change analysis. Developmental Psychology. 2013;49:1591–1601. doi: 10.1037/a0030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA, Cummings EM, Keller P. Sleep disruptions and emotional insecurity are pathways of risk for children. Journal of Child Psychology and Psychiatry. 2007;48:88–96. doi: 10.1111/j.1469-7610.2006.01604.x. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Dahl R. Special issue: Carpe noctem: Sleep and family processes. Journal of Family Psychology. 2007;21:1–3. doi: 10.1037/0893-3200.21.1.1. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Kelly RJ. Sleep in children: Links with marital conflict and child development. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011. pp. 3–28. [Google Scholar]
- El-Sheikh M, Kelly RJ, Bagley EJ, Wetter EK. Parental depressive symptoms and children’s sleep: The role of family conflict. Journal of Child Psychology and Psychiatry. 2012;53:806–814. doi: 10.1111/j.1469-7610.2012.02530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emery RE, Cummings EM, Fincham FD. Parenting in context: Systemic thinking about parental conflict and its influence on children. Journal of Consulting and Clinical Psychology. 1992;60:909–912. doi: 10.1037//0022-006x.60.6.909. [DOI] [PubMed] [Google Scholar]
- Erath SA, Tu KM. The parenting context of children’s sleep. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011. pp. 29–47. [Google Scholar]
- Evans SZ, Simons LG, Simons RL. The effect of corporal punishment and verbal abuse on delinquency: Mediating mechanisms. Journal of Youth and Adolescence. 2012;41:1095–1110. doi: 10.1007/s10964-012-9755-x. [DOI] [PubMed] [Google Scholar]
- Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: A meta-analytic and theoretical review. Psychological Bulletin. 2002;128:539–579. doi: 10.1037/0033-2909.128.4.539. [DOI] [PubMed] [Google Scholar]
- Glod CA. Effects of trauma on children’s sleep. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011. pp. 99–111. [Google Scholar]
- Glod CA, Teicher MH, Hartman CR, Harakal T. Increased nocturnal activity and impaired sleep maintenance in abused children. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:1236–1243. doi: 10.1097/00004583-199709000-00016. [DOI] [PubMed] [Google Scholar]
- Graham AM, Fisher PA, Pfeifer JH. What sleeping babies hear: A functional MRI study of interparental conflict and infants’ emotion processing. Psychological Science. 2013;24:782–789. doi: 10.1177/0956797612458803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham JW, Taylor BJ, Cumsille PE. Planned missing-data designs in analysis of change. In: Collins LM, Sayer AG, editors. New methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 335–353. [Google Scholar]
- Holley S, Hill CM, Stevenson J. An hour less sleep is a risk factor for childhood conduct problems. Child: Care, Health and Development. 2011;37:563–570. doi: 10.1111/j.1365-2214.2010.01203.x. [DOI] [PubMed] [Google Scholar]
- Jones K, Harrison Y. Frontal lobe function, sleep loss and fragmented sleep. Sleep Medicine Reviews. 2001;5:463–475. doi: 10.1053/smrv.2001.0203. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, El-Sheikh M. Marital conflict and children’s sleep: Reciprocal relations and socioeconomic effects. Journal of Family Psychology. 2011;25:412–422. doi: 10.1037/a0023789. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, El-Sheikh M. Longitudinal relations between marital aggression and children’s sleep: The role of emotional insecurity. Journal of Family Psychology. 2013a;27:282–292. doi: 10.1037/a0031896. [DOI] [PubMed] [Google Scholar]
- Kelly RJ, El-Sheikh M. Reciprocal relations between children’s sleep and their adjustment over time. Developmental Psychology. 2013b doi: 10.1037/a0034501. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Killgore WDS, Kahn-Greene ET, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Medicine. 2008;9:517–526. doi: 10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Krishnakumar A, Buehler C, Barber BK. Youth perceptions of interpersonal conflict, ineffective parenting, and youth problem behaviors in European-American and African-American families. Journal of Social and Personal Relationships. 2003;20:239–260. doi: 10.1177/0265407503020002007. [DOI] [Google Scholar]
- Lachar D, Gruber CP. Personality Inventory for Youth (PIY) Los Angeles: Western Psychological Services; 1995. [Google Scholar]
- Lepore SJ, Kliewer W. Violence exposure, sleep disturbance, and poor academic performance in middle school. Journal of Abnormal Child Psychology. 2013;41 doi: 10.1007/s10802-013-9709-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Winebarger AA, Fagot BI, Reid JB, Goldsmith HH. Environmental and genetic variance in children’s observed and reported maladaptive behavior. Child Development. 1998;69:1286–1298. doi: 10.2307/1132266. [DOI] [PubMed] [Google Scholar]
- Liu X, Sun Z, Uchiyama M, Shibui K, Kim K, Okawa M. Prevalence and correlates of sleep problems in Chinese schoolchildren. Sleep. 2000;23:1053–1062. [PubMed] [Google Scholar]
- Low SM, Stocker C. Family functioning and children’s adjustment: Associations among parents’ depressed mood, marital hostility, parent-child hostility, and children’s adjustment. Journal of Family Psychology. 2005;19:394–403. doi: 10.1037/0893-3200.19.3.394. [DOI] [PubMed] [Google Scholar]
- Lumeng JC. Future directions for research on sleep durations in pediatric populations. Sleep: Journal of Sleep and Sleep Disorders Research. 2010;33:1281–1282. doi: 10.1093/sleep/33.10.1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacGregor E, McNamara JR. Comparison of return procedures involving mailed versus student-delivered parental consent forms. Psychological Reports. 1995;77:1113–1114. doi: 10.2466/pr0.1995.77.3f.1113. [DOI] [Google Scholar]
- MacKinnnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding, and suppression effect. Prevention Science. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannering AM, Harold GT, Leve LD, Shelton KH, Shaw DS, Conger RD, Reiss D. Longitudinal associations between marital instability and child sleep problems across infancy and toddlerhood in adoptive families. Child Development. 2011;82:1252–1266. doi: 10.1111/j.1467-8624.2011.01594.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, Viding E. Heightened neural reactivity to threat in child victims of family violence. Current Biology. 2011;21:R947–R948. doi: 10.1016/j.cub.2011.10.015. http://dx.doi.org/10.1016/j.cub.2011.10.015. [DOI] [PubMed] [Google Scholar]
- McKee L, Roland E, Coffelt N, Olson AL, Forehand R, Massari C, Zens MS. Harsh discipline and child problem behaviors: The roles of positive parenting and gender. Journal of Family Violence. 2007;22:187–196. doi: 10.1007/s10896-007-9070-6. [DOI] [Google Scholar]
- Michels N, Clays E, De Buyzere M, Vanaelst B, De Henauw S, Sioen I. Children’s sleep and autonomic function: Low sleep quality has an impact on heart rate variability. Sleep. 2013;36:1939–1946. doi: 10.5665/sleep.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mindell J, Owens J. Evaluation of pediatric sleep disorders. A Clinical Guide to Pediatric Sleep. Diagnosis and Management of Sleep Problems. 2010:42–54. [Google Scholar]
- Mistler SA, Enders CK. Planned missing data designs for developmental research. In: Laursen B, Little TD, Card NA, editors. Handbook of developmental research methods. New York, NY: Guilford Press; 2012. pp. 742–754. [Google Scholar]
- Muzur A, Pace-Schott EF, Hobson JA. The prefrontal cortex in sleep. Trends in Cognitive Sciences. 2002;6:475–481. doi: 10.1016/s1364-6613(02)01992-7. [DOI] [PubMed] [Google Scholar]
- National Sleep Foundation. How much sleep do we really need? 2011 from http://www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need.
- Paavonen EJ, Fjällberg M, Steenari MR, Aronen ET. Actigraph placement and sleep estimation in children. Sleep. 2002;25:235–237. doi: 10.1093/sleep/25.2.235. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17:117–133. doi: 10.1007/bf01537962. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Selig JP. Advantages of Monte Carlo confidence intervals for indirect effects. Communication Methods and Measures. 2012;6:77–98. doi: 10.1080/19312458.2012.679848. [DOI] [Google Scholar]
- Quach J, Hiscock H, Canterford L, Wake M. Outcomes of child sleep problems over the school-transition period: Australian population longitudinal study. Pediatrics. 2009;123:1287–1292. doi: 10.1542/peds.2008-1860. [DOI] [PubMed] [Google Scholar]
- Rhoades KA, Leve LD, Harold GT, Mannering AM, Neiderhiser JM, Shaw DS, Reiss D. Marital hostility and child sleep problems: Direct and indirect associations via hostile parenting. Journal of Family Psychology. 2012;26:488–498. doi: 10.1037/a0029164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews. 2011a;15:259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Sadeh A. Sleep assessment methods. In: El-Sheikh M, editor. Sleep and development: Familial and socio-cultural considerations. New York, NY: Oxford University Press; 2011b. pp. 355–371. [Google Scholar]
- Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: What a difference an hour makes. Child Development. 2003;74:444–455. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- Sadeh A, McGuire JPD, Sachs H, Seifer R, Tremblay A, Civita R, Hayden RM. Sleep and psychological characteristics of children on a psychiatric inpatient unit. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:813–819. doi: 10.1097/00004583-199506000-00023. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Developmental Psychology. 2000;36:291–301. doi: 10.1037/0012-1649.36.3.291. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep—wake identification: An empirical test of methodological issues. Sleep. 1994;17:201–207. doi: 10.1093/sleep/17.3.201. [DOI] [PubMed] [Google Scholar]
- Selig J, Preacher K. Monte Carlo method for assessing mediation: An interactive tool for creating confidence intervals for indirect effects [Computer software] 2008 quantpsy.org.
- Straus MA. Manual for the Conflict Tactics Scale. Durham, NH: Family Research Laboratory, University of New Hampshire; 1995. [Google Scholar]
- Straus MA. Unpublished manuscript. Durham, NH: University of New Hampshire; 1999. Child-report, adult-recall, and sibling version of the Revised Conflict Tactics Scales. [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent–Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Walker MP, van der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychological Bulletin. 2009;135:731–748. doi: 10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wirt RD, Lachar D, Klinedinst JK, Seat PS. Personality Inventory for Children - Revised. Los Angeles: Western Psychological Services; 1990. [Google Scholar]


