Abstract
Background: Menarche, a milestone in the reproductive life span of a woman, is influenced by several genetics and environmental factors. There is no consensus regarding the impact of body mass index (BMI) and lipid profiles on the age of menarche, as the results of various studies demonstrate.
Objective: To investigate the correlation between age of menarche and BMI/lipoprotein profile in a community sample of Iranian girls.
Materials and Methods: In the study, 370 girls, aged 10-16 years, who began their menarche within six months prior to the study, were recruited from the Tehran Lipid and Glucose Study (TLGS) population. Information was documented regarding their body composition, including height, weight, BMI, waist and hip circumference were collected and their lipid profiles were assessed after a 12-hour fast.
Results: In this study, the mean±SD of age of menarche and BMI were 12.6±1.1 years and 21.7±3.9 kg/m2, respectively. There were statistically significant relationships between age of menarche and height, BMI, waist circumference, and the maternal educational level. The relationship between age of menarche and the weight and lipid profiles of subjects was not statistically significant.
Conclusion: Age at menarche is not influenced by lipid profiles but it is influenced by BMI.
Key Words: Age of menarche, Body Mass Index, Serum lipid profile
Introduction
Puberty marks an especially important stage of life with significant physical, mental and emotional changes. The onset of puberty reflects numerous health aspects of a population including the timing of sexual maturation, growth and nutritional status and environmental conditions, in well-nourished, healthy girls and menarche is largely dependent on genetics, as confirmed by studies on the menarcheal age of twins, sisters and mother-and-daughter pairs (1-9).
The impacts of anthropometric parameters, central obesity indexes and body fat have been investigated by several studies but have yielded different results (9-11). In a study by Garcia et al, there was no correlation between age at menarche and BMI (10), while other studies report contradictory findings i.e. the age at menarche among girls with higher BMI was less than those girls with lower BMI (12-16). Various endocrine factors affect the rate of puberty and the gathering of body fat (17, 18).
There are limited studies in literature on the correlation between lipid profiles and age at menarche. We aimed to assess the correlation between age at menarche and anthropometric parameters and lipid profiles among a community based sample of girls whose menarcheal onset had occurred during the six months prior to the study.
Materials and methods
Our cases were recruited from the Lipid and Glucose study (TLGS) cohort, an ongoing prospective study, initiated in 1998, with the aim of determining the prevalence of non-communicable disease risk factors. The TLGS includes 15,005 people, ≥3 years selected from a geographically defined population using multistage cluster sampling. In this study the subjects were selected from the TLGS second phase between 2002-2005 years. Inclusion criteria were: 1) Age range 10-16 years. 2) Beginning of menarche within the six months prior to the study. And those with any history of chronic disorders (such as: diabetic mellitus, chronic heart disease) were excluded. Demographic and lifestyle variables were collected through face-to-face interviews by trained interviewers.
The follow-up included a general physical examination, height and weight measurements, their blood samples were taken after 12-hours over night fasting and lipid profile analyses were done at the TLGS research laboratory on the day of blood collection. The onset of menarche was asked and the date of the first cycle was recorded. The mother’s educational level was categorized to less than high school diploma, high school diploma and more than high school diploma. Weight was measured to the nearest 0.1 kg on a calibrated beam scale. Height and waist circumference (WC) were measured to the nearest 0.5 cm with a measuring tape, WC was measured midway between the lower rib margin and the iliac-crest at the end of a gentle expiration. Body mass index was calculated as weight in kilograms divided by the height in meters squared (kg/m2) (20).
BMI was categorized, according to WHO guidelines, into four groups. Those with BMI <15th percentile for age and gender standards were considered as “underweight”, those between the 15th percentile to less than <85th percentile as “normal weight”, between the 85th percentile to less than <95th percentile as “overweight”, and equal to or greater than ≥95 was considered as “obese” (21). To determine these cut off points, we used the data on anthropometric parameters of all participants of TLGS, aged10-16 years.
Lipid measurements including Total Cholesterol (TC), Triglycerides (TG) and High Density. Lipoprotein Cholesterol (HDL-C) were determined by commercial assay kits (Pars Azmoon Inc., Tehran, Iran), TC and TG were assayed using enzymatic colorimetric tests with cholesterol esterase and cholesterol oxidase, and glycerol phosphate oxidase, respectively. HDL-C was measured after precipitation of the apolipoprotein B containing lipoproteins with phosphotungistic acid. All samples were analyzed when internal quality control met the acceptable criteria. In all the biochemical analyses, the intra- and inter-assay coefficients of variation (CV) were less than 2.5% and 3.2%, respectively. Study participants were categorized according to their serum LDL-C values into three groups: 1) <110 mg/dl; 2) between 110-129 mg/dl and 3) >129 mg/dl. Based on their serum cholesterol study participants were placed in three groups: 1) <170 mg/dl, 2) between 170-199 mg/dl and 3) >199 mg/dl (20, 22, 23).
Statistical analysis
Continuous variables, checked for normality, using the one-sample Kolmogorov-Smirnoff test, are expressed as mean±SD deviation. Logarithmic transformation was applied to not normally distributed variables. Categorical variables are expressed as percentages.
The association between age at menarche with anthropometric parameters and lipid profiles with normal distribution was assessed using the Pearson correlation coefficient. Distributions of age at menarche between BMI, LDL-C and cholesterol groups were compared, using analysis of variance. Data analysis was performed using the SPSS 15.0 PC package (SPSS Inc., Chicago, IL). P≤0.05 were considered as significant.
Results
Of 727 girls, aged 10-16 years, 370 met our inclusion criteria. The mean±SD for age of menarche, weight, height, waist circumference and body mass index were 12.6±1.1 years, 53.7±10.5 kg, 157.3±5.5 cm, 72.5±9.8 cm and 21.7±3.9 kg/m2, respectively.
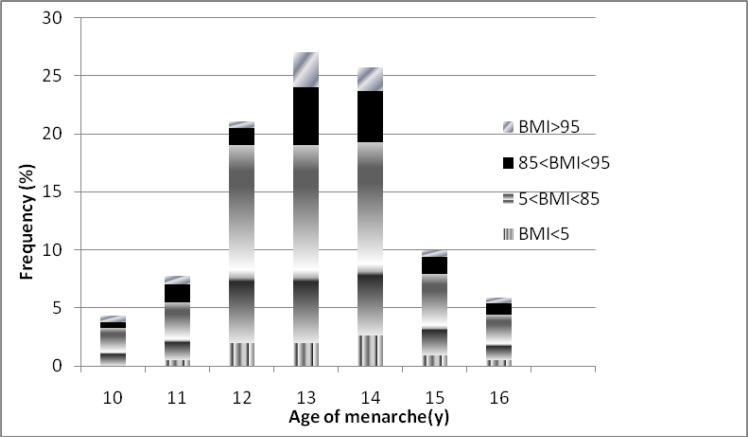
The menarche age range of 11-13 years constitutes 80.5% of distribution. General characteristics, anthropometrics and lipids parameters of study participants are demonstrated in table I. Prevalences of under, normal and overweight girls were 4.3%, 72.4% and 11.9%, respectively. Of our study participants, 11.4% were obese. Menarcheal age distribution of the study subjects, according to the BMI categories is shown in figure 1. There was a negative correlation between BMI and age at menarche using regression linear analysis (p=0.004, R-square=0.02).
Table I.
The basic and biochemical characteristics of study subjects
| Variables | Value |
|---|---|
| Age of menarche (years) | 12.6±1.1 |
| Weight (Kg) | 53.7±10.5 |
| Height (cm) | 157.3±5.5 |
| BMI (Kg/m2) | 21.7±3.9 |
| Waist circumference (cm) | 72.5±9.8 |
| Waist hip ratio | 0.2±0.01 |
| Total cholesterol (mg/dl) | 151±24.9 |
| Triglycerides* (mg/dl) | 4.5±0.4 |
| High-density lipoprotein (mg/dl) | 39±9.1 |
| Low-density lipoprotein (mg/dl) | 92±22.7 |
Value (means±SD).
SD of log-transformed.
Figure 1.
Distribution of age at menarche according to BMI groups
Although, age at menarche had a statistically significant positive correlation with height (R-square=0.04, p<0.005), it had a statistically significant negative correlation with waist circumference (R-square=0.01, p=0.04). No statistically significant relationship was found between menarcheal age and weight, waist hip ratio (WHR) and lipids parameters (R-square=0.00, p=0.9) (Table II).
Table II.
The relationship between age of menarche and anthropometric indexes and serum lipoproteins
| Variables | β | p-value |
|---|---|---|
| Weight | -0.07 | 0.18 |
| Height | 0.21 | 0.00* |
| BMI | -0.16 | 0.004* |
| WC | -0.1 | 0.04* |
| WHR | -0.001 | 0.9 |
| Total cholesterol | 0.07 | 0.2 |
| Triglycerides ** | 0.008 | 0.8 |
| High-density lipoprotein | 0.00 | 0.9 |
| Low-density lipoprotein | 0.07 | 0.22 |
β=Regression coefficient.
p<0.05.
No significant correlation was seen between LDL groups and menarcheal age after adjustment for BMI, height, weight, waist circumference, HDL cholesterol and total cholesterol. The influences of various independent variables, including mother’s educational status, anthropometric parameters and lipids profiles on age at menarche were explored using the multiple regression analysis (stepwise method).
There was a statistically significant parameters correlation between age at menarche and the mother’s educational status, with increasing mother’s education, age of menarche decreased (β=-0.112, CI=-0.22, -0.003, p=0.04), age of menarche increased as BMI decreased (β=-0.110, CI=-0.181, -0.04, p=0.005).
Discussion
Our study demonstrated no significant relationship between age of menarche and lipid parameters after adjustment for other anthropometrics and socio-economic variables. We did however find a negative association between age at menarche and body mass index. The mean menarcheal age of our study cohort was 12.6±1.1 years and the onset of menarche in majority of our subjects (80.5%) was between 11-13 years of age, similar to that reported by Khabazan et al in Tehran (24). The mean ages of menarche among Iranian girls reported in two other studies (1990, 1999) were 13.86 and 13.65 years respectively (25).
The mean±SD height of girls in this study was 157.3±5.5 cm. There was a significant positive correlation between the menarcheal age of our study subjects and their height, results similar to those demonstrated by Elizando (26) and Kabir et al (27). Various studies have documented contradictory results regarding the effect of weight on menarcheal age. In our study, there was no significant statistical relationship between weight and age of menarche, results similar to those reported in another study (24). Our results were in contrast with those of Meyer et al (28) and the Kim et al study (29) that found a positive relationship between weight and menarcheal age. In a study from Peru, an inverse relationship was observed between weight and body mass index and menarche age (30).
The impact of BMI on age at menarche is not clear yet. Merzenich et al reported that reaching a critical weight of 47.8 kg is a requisite for occurrence of menarche in girls (31); however studies have reported various associations between ages at menarche with BMI. In the present study, similar to other studies (32, 33), menarcheal age reduced with increasing body mass index. Other studies however found no significant association between BMI and average age of menarche (10). Kapiro et al found a linear association between BMI and menarche age in twin girls (9), whereas Demerath et al reported that onset of menarche and changes in body mass index were independent (34). There are studies that report a relationship between menarche and adiposity; the age at menarche of those girls with higher body mass index being less than others (18, 35-37).
There is limited data or associations between lipid profiles and menarcheal age (38-40). According to a study conducted in Spain on 272 girls aged 9-15 years, no significant association was found between the menarche age and blood lipids or waist circumference (39), very similar to results reported by Tell et al (40). Also, Kim et al study showed that there is a positive association between age at menarche and waist to hip ratio and waist circumference (29). Our study demonstrated no significant relationship between age of menarche and lipid parameters after adjustment for other anthropometric and socio-economic variables. Maternal educational level had a significant effect on menarcheal age in our study, which is in agreement with those reported by Kurdzielewicz in a study of 111 girls in Netherland (19).
There are several explanations for the various factors that affect age at menarche; these include the socio-economic and nutritional status and environmental conditions as well as genetic determinants. (2-10, 37, 41-43). Furthermore the recruitment of study subjects and the type of study have a great impact of the age at menarche and its other influencing factors (1, 17, 44-46). Our study has the advantage of examining this issue in a population-based cohort of Iranian girls with a specific age range. Furthermore, the amount of intra-assay variability in our data is likely to be minimal, because all the laboratory measurements were evaluated in the same laboratory by the same person.
Of our few limitations, the most significant was that we did not use a standard method for identification of the fat mass. Also we did not evaluate the effect of other important variables such as physical activity or nutritional status on menarcheal age. It needs to be mentioned that the current analyses were based on data from a single community in Tehran as a result it may not be possible to generalize these results to other communities in the Islamic Republic of Iran. In conclusion it seems that age at menarche is not influenced by lipid profiles.
Acknowledgements
We praise the substantial time and effort that each of the study participants contributed to this study. Acknowledgements are also due to research staff at the Tehran Lipid and Glucose Study Unit and staff in Research Endocrine Laboratory. My special thanks to Mrs. N. Shiva for editing the manuscript. We thank the National Council of Scientific Research of the Islamic Republic of Iran for approval of this project and its funding as a national research project.
References
- 1.Tehrani FR, Mirmiran P, Zahedi-Asl S, Nakhoda K, Azizi F. Menarcheal age of mothers and daughters: Tehran Lipid and Glucose Study. East Mediterr Health J. 2010;16:391–395. [PubMed] [Google Scholar]
- 2.Cameron N, Nagdee I. Menarcheal age in two generations of South Africa Indians. Ann Hum Biol. 1996;23:113–119. doi: 10.1080/03014469600004332. [DOI] [PubMed] [Google Scholar]
- 3.Chompootaweep S, Tankeyoon M, Poomsuwan P, Yamarat K, Dusitsin N. Age at menarche in Thai girls. Ann Hum Biol. 1997;24:427–433. doi: 10.1080/03014469700005192. [DOI] [PubMed] [Google Scholar]
- 4.Ayatollahi SM, Dwlatabadi E, Ayatollahi SA. Age at menarche in Iran. Ann Hum Biol. 2002;22:355–362. doi: 10.1080/03014460110086817. [DOI] [PubMed] [Google Scholar]
- 5.Danker-Hopfe H, Delibalta K. Menarcheal age of Turkish girls in Bemen. Anthropol Anz. 1990;48:1–14. [PubMed] [Google Scholar]
- 6.Amin alroaya A, Mirmiran P, Hamedi P, Azizi F. Assessment of puberty stages in girls (Eastern of Tehran) Pejouhesh Dar Pezeshki. 1996;20:1–11. [Google Scholar]
- 7.National Cholesterol Education Program (NCEP) Highlights of the Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. NCEP Expert Panel on blood cholesterol levels in Children and Adolescents. Pediatrics. 1992;89:495–501. [PubMed] [Google Scholar]
- 8.Anderson SE, Dallal GE, Must A. Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart. Pediatrics. 2003;111:844–850. doi: 10.1542/peds.111.4.844. [DOI] [PubMed] [Google Scholar]
- 9.Kaprio J, Rimpelä A, Winter T, Viken RJ, Rimpelä M, Rose RJ. Commen genetic influences on BMI and age at menarche. Hum Biol. 1995;67:739–753. [PubMed] [Google Scholar]
- 10.García Cuartero B, Gónzalez Vergaz A, Frías García E, Arana Cañete C, Díaz Martínez E, Tolmo MD. Assessment of the secular trend in puberty in boys and girls. An Pediatr (Barc) 2010;73:320–326. doi: 10.1016/j.anpedi.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Celi F, Bini V, De Giorgi G, Molinari D, Faraoni F, Di Stefano G, et al. Epidemiology of overweight and obesity among school children and adolescents in 3 provinces of central Ialy 1993-2001: study of potential influencing variables. Eur J Clin Nutr. 2003;57:1045–1051. doi: 10.1038/sj.ejcn.1601640. [DOI] [PubMed] [Google Scholar]
- 12.Ramachandran A, Snehalatha C, Vinitha R, Thayyil M, Kumar CK, Sheeba L, et al. Prevalance of overweight in urban Indian adolescent schoolchildren. Dabetes Res Clin Pract. 2002;57:185–190. doi: 10.1016/s0168-8227(02)00056-6. [DOI] [PubMed] [Google Scholar]
- 13.Feng Y, Hong X, Wilker E, Li Z, Zhang W, Jin D, et al. Effects of age at menarche, reproductive years, and menopause on metabolic risk factors for cardiovascular diseases. Atherosclerosis. 2008;196:590–597. doi: 10.1016/j.atherosclerosis.2007.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kivimäki M, Lawlor DA, Smith GD, Elovainio M, Jokela M, Keltikangas-Järvinen L, et al. Association of age at menarche with cardiovascular risk factors, vascular structure, and function in adulthood: the Cardiovascular Risk in Young Finns study. Am J Clin Nutr. 2008;87:1876–1882. doi: 10.1093/ajcn/87.6.1876. [DOI] [PubMed] [Google Scholar]
- 15.Heys M, Schooling CM, Jiang C, Cowling BJ, Lao X, Zhang W, et al. Age of menarche and the metabolic syndrome in China. Epidemiology. 2007;18:740–746. doi: 10.1097/EDE.0b013e3181567faf. [DOI] [PubMed] [Google Scholar]
- 16.Frontini MG, Srininvasan SR, Berenson GS. Longitudinal changes in risk variables underlying metabolic Syndrome X from childhood to young adulthood in female subjects with a history of early menarche: The Bogulasa Heart Study. Int J Obes Relat Metab Disord. 2003;27:1398–1404. doi: 10.1038/sj.ijo.0802422. [DOI] [PubMed] [Google Scholar]
- 17.Van Lenthe FJ, Kemper CG, van Mechelen W. Rapid maturation in adolescence results in greater obesity in adulthood: the Amsterdam Growth and Health Study. Am J Clin Nutr. 1996;64:18–24. doi: 10.1093/ajcn/64.1.18. [DOI] [PubMed] [Google Scholar]
- 18.Remsberg KE, Demerath Ew, Schbert CM, Chumlea WC, Sun SS, Siervogel RM. Early menarche and the development of cardiovascular disease risk factors in adolescent girls: the Fels Longitudinal Study. J Clin Endocrinol Metab. 2005;90:2718–2724. doi: 10.1210/jc.2004-1991. [DOI] [PubMed] [Google Scholar]
- 19.Kurdzielewicz M. Analysis of selected enviromental and biophysical parameters during menarche. Ann Acad Med Stetin. 2001;47:125–143. [PubMed] [Google Scholar]
- 20.Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in Iranian urban population: Tehran Lipid and Glucose Study (Phase1) Soz Praventivmed. 2002;47:408–426. doi: 10.1007/s000380200008. [DOI] [PubMed] [Google Scholar]
- 21.Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. Geneva: World Health Organization; 1995. WHO Technical Report Series, No. 854. [PubMed] [Google Scholar]
- 22.Hadaegh F, Zabetian A, Sarbakhsh P, Khalili D, James WPT, Azizi F. Appropriate cutoff values of anthropometric variables to predict cardiovascular outcomes: 7.6 years follow-up in an Iranian population. Int J Obes (lond) 2009;33:1437–1445. doi: 10.1038/ijo.2009.180. [DOI] [PubMed] [Google Scholar]
- 23.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 24.Khakbazan Z, Niroomanesh Sh, Mehran A, Magidi Ahie A. Age at menarche and its relationship with body mass index. Hayat. 2005;11:55–62. [Google Scholar]
- 25.Mohammad K, Zeraati H, Majdzadeh R, Karimloo M. Evaluating the trend of change in the mean onset age of menarche in Iranian girls. J Reprod Infertil. 2006;7:523–530. [Google Scholar]
- 26.Elizando S. Age at menarche: its relation to line and ponderal growth. Ann Hum Biol. 1992;19:197–199. doi: 10.1080/03014469200002072. [DOI] [PubMed] [Google Scholar]
- 27.Kabir A, Torkan F, Hakemi L. Evaluation age and relevant factors in Iranian female participants of the 1381 student olympic games. Iran J Endocrinol metab. 2007;8:383–391. [Google Scholar]
- 28.Meyer F, Moisan J, Marcoux D, Buchard D. Dietry and physical determinates of menarch. Epidemiology. 1990;1:377–381. doi: 10.1097/00001648-199009000-00007. [DOI] [PubMed] [Google Scholar]
- 29.Kim JY, Oh IH, Lee EY, Oh CM, Choi KS, Choe BK, et al. The relation of menarcheal age to anthropometric profiles in Korean girls. J Korean Med Sci. 2010;25:1405–1410. doi: 10.3346/jkms.2010.25.10.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gonzales GF, Villena A. BMI and age at menarche in Puvian children living at high altitude and at sea level. Hum Biol. 1996;68:265–275. [PubMed] [Google Scholar]
- 31.Merzenich H, Boeing H, Wahrendorf J. Dietary fat and sports activity as determinanats for age at menarche. Ann J Epidemiol. 1993;138:217–224. doi: 10.1093/oxfordjournals.aje.a116850. [DOI] [PubMed] [Google Scholar]
- 32.Pierce MB, Kuh D, Hardy R. Role of lifetime body mass index in the association between age at puberty and adult lipids: findings from men and women in a British birth cohort. Ann Epidemiol. 2010;20:676–682. doi: 10.1016/j.annepidem.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Batubara JR, Soesanti F, van de Waal HD. Age at menarche in indonesian girls: a national survey. Acta Med Indones. 2010;42:78–81. [PubMed] [Google Scholar]
- 34.Demerath EW, Towne B, Chumlea WC, Sun SS, Czerwinski SA, Remsberg KE, et al. Recent decline in age at menarche: the Fels Longitudinal Study. Am J Hum Biol. 2004;16:453–457. doi: 10.1002/ajhb.20039. [DOI] [PubMed] [Google Scholar]
- 35.Fuji K, Demura S. Rlationship between change in BMI with age and delayed menarche in female athletes. J Physiol Anthropol Appl HumanSci. 2003;22:97–104. doi: 10.2114/jpa.22.97. [DOI] [PubMed] [Google Scholar]
- 36.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of menarcheal age to obesity in childhood and adulthood: the Bogalusa heart study. BMC Pediatr. 2003;30:3. doi: 10.1186/1471-2431-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaplowitz PB, Slora EJ, Wasserman RC, Pedlow SE, Herman-Giddens ME. Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics. 2001;108:347–353. doi: 10.1542/peds.108.2.347. [DOI] [PubMed] [Google Scholar]
- 38.Cobbaert C, Deprost L, Mulder P, Rombaut K, Gijsels G, Kesteloot H. Pubertal serum lipoprotein (a) and its correlates in Belgian schoolchildren. Int J Epidemiol. 1995;24:78–87. doi: 10.1093/ije/24.1.78. [DOI] [PubMed] [Google Scholar]
- 39.Ruiz JR, Ortega FB, Tresaco B, Warnberg J, Mesa JL, Gonzalez-Gross M, et al. Serum Lipids, Body Mass Index and Waist Circumference during Pubertal Development in Spanish Adolescents: The AVENA Study. Horm Metab Res. 2006;38:832–837. doi: 10.1055/s-2006-956503. [DOI] [PubMed] [Google Scholar]
- 40.Tell GS, Mittelmark MB, Vellar OD. Cholesterol, high density lipoprotein cholesterol and triglycerides during puberty: The Oslo Youth Study. Am J Epidemiol. 1985;122:750–761. doi: 10.1093/oxfordjournals.aje.a114158. [DOI] [PubMed] [Google Scholar]
- 41.Liestol K, Rosenberg M. Height, weight and age of menarche of schoolgirls in Oslo An update. Ann Hum Biol. 1995;22:199–205. doi: 10.1080/03014469500003862. [DOI] [PubMed] [Google Scholar]
- 42.Kulin HE, Bwibo N, Mulie D, Santner SJ. The effect of chronic chile hood malnutrition on pubertal growth and development. AM J Clin Nutr. 1992;6:527–536. doi: 10.1093/ajcn/36.3.527. [DOI] [PubMed] [Google Scholar]
- 43.Adair LS, Gordon-Larsen P. Maturational timing and overweight prevalence in US adolescent girls. Am J Public Health. 2001;91:642–644. doi: 10.2105/ajph.91.4.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoffman WH, Barbeau P, Litaker MS, Johnson MH, Howe CA, Gutin B. Tanner staging of secondary sexual characteristics and body composition , blood pressure, and insulin in black girls. Obes Res. 2005;13:2195–2201. doi: 10.1038/oby.2005.272. [DOI] [PubMed] [Google Scholar]
- 45.Slyper AH. The pubertal timing controversy in the USA, and a review of possible causative factors for the advance in timing of onset of puberty. Clin Endocrinol (Oxf) 2006;65:1–8. doi: 10.1111/j.1365-2265.2006.02539.x. [DOI] [PubMed] [Google Scholar]
- 46.Wang Y. Is obesity associated with early sexual maturation? A comparison of the association in American boys versus girls. Pediatrics. 2002;110:903–910. doi: 10.1542/peds.110.5.903. [DOI] [PubMed] [Google Scholar]