Abstract
The objective of this study was to describe the 3-year outcomes (2011–2013) from the healthy lunchbox challenge (HLC) delivered in the US-based summer day camps (SDC) (8–10 hours day−1, 10–11 weeks summer−1, SDC) to increase children and staff bringing fruit, vegetables and water (FVW) each day. A single group pre- with multiple post-test design was used in four large-scale SDCs serving more than 550 children day−1 (6–12 years). The percentage of foods/beverages brought by children/staff, staff promotion of healthy eating and children’s consumption of FVW was assessed via direct observation over 98 days across three summers. For children (3308 observations), fruit and vegetables (>11–16%) increased; no changes were observed for FVW for staff (398 observations). Reductions in unhealthy foods/beverages (e.g. soda/pop and chips) were observed for both children and staff (minus −10% to 38%). Staff role modeling unhealthy eating/drinking initially decreased but increased by 2013. The majority of children who brought fruit/vegetables consumed them. The HLC can influence the foods/beverages brought to SDCs. Enhancements are required to further increase FVW brought and consumed.
Introduction
Summer is a time when children erase physical fitness gains made during the school year [1, 2] and gain excess body weight [3–5]. Summer day camps (SDCs) represent a potential setting for the extension of health and wellness efforts targeting children during the school year. Across the United States, SDCs serve >14.3 million youth [6] (<12 years) annually and are the single largest organized setting, outside of the school year, where children can engage in health promoting behaviors. SDCs last 8–10 hours day−1, span the entire summer (10–11 weeks) and include a wide assortment of activities each day (i.e. they do not focus on a single activity, as do sports/music camps). This represents a substantial amount of contact time in which SDCs can influence health behaviors, specifically healthy eating, of children during the program.
In a 2011 national study of emerging issues faced by SDC leaders, the American Camp Association [7] reported that SDC staff identified ‘healthy eating and physical activity of the children attending’ as the third most important issue facing SDCs, behind ‘financial security of the camp’ and ‘communication to parents’. In 2011, the National Afterschool Association (NAA) released childhood obesity policies referred to as the Healthy Eating and Physical Activity (HEPA) standards, which call upon SDCs to ensure the children enrolled are offered a serving of fruit and vegetables and water daily [8].
Many SDCs do not provide foods to the children attending, which places the responsibility of packing lunches and snacks on their parents. This scenario necessitates innovative strategies to ensure that what children bring for snacks and lunch meet the HEPA standards. The purpose of this study was to develop and evaluate an innovative healthy eating intervention, called the healthy lunchbox challenge (HLC), designed to increase the amount of FVW children and staff bring to SDC and to align staff behaviors with those called for in the NAA HEPA standards.
Methods
Participants and setting
Four large-scale community-based SDCs in central South Carolina participated in the study during the summer 2011 (baseline) and summers 2012 and 2013 (intervention). Parents were informed of study procedures through orientation packets, newsletters and information posted at each SDC location. Due to the observational nature of this study, participants provided passive consent for the recording of foods/beverages. All procedures were approved by the University’s Institutional Review Board for the Protection of Human Subjects. Approval by the IRB included not having any child assent or parental consent because of the direct observation protocol.
The SDCs each served ∼130 children per day (∼550 total across all SDCs) and employed around 12–15 staff each day at each SDC across the three measurement periods. The average age of children attending the SDCs was 7.8 years (range 4–12 years), with 53% boys and 46% White non-Hispanic. Based on 2012 Census Data, the percentage of the population in poverty for the SDCs ranged from 5.6% to 14.7%. The SDCs participating were structured programs that provided a variety of activities (e.g. snack/lunch, enrichment and physical activity) daily throughout the summer [9, 10]. Parents of children attending paid to participate in the SDCs, with a sliding fee scale based on SDC designated parental financial status. Each day, time was allotted for a morning and afternoon snack, and lunch. Each SDC employed a site leader and staff members. Site leaders created daily schedules, managed staff, interacted with parents and generally oversaw program operations. Staff’s main responsibility was to manage children as they moved through the planned activities each day. Scheduled activities at the SDCs were held from 9.00 a.m. to 4:30 p.m. Participant SDCs operated on an 11-week schedule throughout the summer with parents enrolling their children in camp for 1 week (Monday–Friday) at a time. The camps maintained a 1:10 to 15 staff-to-child ratio and grouped children by grade level (e.g. K–first, second–third). For example, there could be four groups of fourth–fifth graders each with 10–15 children. Most of the children were under 12 years of age and were enrolled in the program for 8 weeks during the summer. Enrolled children attended the program on average 4 days week−1 for 8 hours day−1. Based on SDC enrollment information, ∼65% of children re-enroll in the SDC each summer.
Healthy lunchbox challenge
The HLC was grounded in behavioral choice theory (BCT) [11] and goal-setting theory [12]. Studies employing BCT principles indicate that behavior change may be more likely when messages target increases in healthy behaviors (i.e. packing FVW) rather than messages restricting unhealthy behaviors (e.g. do not pack sugar-sweetened beverages, chips or candy) [13, 14]. Weekly incentives, such as movie tickets, extra swim time and holding the ‘spirit stick’, served as motivational reinforcers, with group-based goals focused on children, within their age-/grade-level groups (groups based on grade levels within the SDCs, e.g. 3 groups of 10 second graders), vying to attain the highest amount of HLC points (see below) by Friday of each week based on the number of times they brought FVW for lunch and snack daily. These approaches were the theoretical foundation upon which the HLC was created.
Weekly meetings with SDC leaders from March–May 2012 identified strategies to influence parental and staff decisions regarding foods/beverages brought to SDC. From these meetings, two intervention components were developed: (i) parent and staff knowledge and skills and (ii) child and staff incentive program. Healthy eating education materials included a description of the HLC mission and procedures, a ‘Building a Better Lunchbox’ guide to choosing healthy foods and beverages, a double-sided visual guide of what constitutes a healthy lunchbox, and tips on making healthy purchases at lower cost. The second component of the HLC was designed to influence parental decisions of foods/beverages purchased for SDC through child incentives; with the assumption that incentives would motivate children’s request for FVW to be packed daily [15, 16]. The primary targets of the HLC were FVW. This was based on the recommendations from the HEPA standards, the ability develops a rewards system using easily identifiable food/beverage items, as well as, the BCT which indicates that behavior change may be more effective when the focus is on promoting more healthful foods, rather than penalizing children for bringing less healthful foods/beverages. Parents were provided printed copies of the HLC materials upon enrollment of their child in the SDCs. Additionally, emails were sent to parents each week of the SDC that include electronic copies of the HLC materials, in addition to the regular SDC parent info provided by the SDCs each week.
Children were informed about the HLC during daily morning assembly and by their group counselors. A point system was developed where children could earn up to three points per day for bringing FVW. Points were tallied by SDC staff, within pre-determined groups (i.e. K–first, second–third) prior to morning snack to ensure all possible points were given before food/beverage consumption. To record points, staff asked children to show any FVW they had brought for the day. To account for varying group sizes, group points were tallied as total percentage for each category. A maximum of three points (i.e. one for fruits, one for vegetables and one for water) were awarded regardless of the total number of items brought in any given category. Group points were displayed on a HLC board (4′ x 3′ marker board) located where parents dropped-off and picked-up their children. Prizes were awarded to groups with the highest points at the end of each week. The Healthy Eating Standards emphasize the role staff play in nutrition promotion and modeling [8]; therefore, staff were also encouraged to participate in the HLC. The HLC was initiated immediately following the trainings, which took place prior to the start of SDC. Outcome observations took place during weeks 6–11 of the SDC program.
Process evaluation measures
Trained research staff conducted one training at the beginning of each intervention summer (∼45 min) for SDC directors and staff where they were shown how to record, input, calculate and display points daily. Training also included healthy eating promotion components such as role modeling, promoting healthy eating and using healthy eating resources for nutrition education. Technical support consisted of weekly communications and site visits where field notes were recorded to identify and resolve implementation errors. Electronic recording forms provided to SDC directors enabled them to calculate the percentage of children in each group who brought FVW. Recording forms were evaluated weekly by trained research staff for accuracy and to troubleshoot instances of missing data. To quantify reach, parents were asked during daily pick-up or drop-off times throughout the study to the extent of their knowledge about the HLC. Staff were provided with written evaluation forms on the HLC (including discrete- and open-ended questions) following program completion.
Food and beverages brought to the SDC
Groups of children were randomly selected for observation using a stratified sampling procedure, based on grouping or grade level. Two groups of trained data collectors observed four age groups across two SDC sites daily for 16 days each summer. Trained research assistants (average 18 observers each summer) recorded all food and beverage items brought to SDC by children and staff on an observation form developed from existing direct observation tools for the child-care centers and elementary schools [17, 18] and modified for the SDC settings. All foods and beverages were assessed to determine the impact of the HLC on children’s and staffs’ choices related to healthy eating. Categories of foods and beverages are displayed in Table I. Primary outcomes of interest were the proportion of children and staff bringing FVW to SDC. Inter-observer reliability between two trained research staffers of categories was estimated using weighted kappa (κw) and percent agreement. Percent agreement ranged from 77% to 100% (median 94%) and κw ranged from 0.22 to 1.00 (median 0.66) across all food and beverage categories. For the primary outcomes of FVW, percent agreement ranged from 94% to 97% and κw ranged from 0.71 to 0.93 indicating a high level of inter-observer reliability. Low κw or percent agreement was due to the limited occurrence (<5% of observations) of specific food and beverages observed (e.g. meat sandwiches on brown bread and milk). For all outcome measures, both children and staff were unaware of the days they were monitored.
Table I.
Percentage of children and staff that brought foods and drinks to the SDC for snacks and lunch at baseline (summer 2011) and during the HLC (summers 2012–13)
| Children (total of 3308 child observations across 98 days) |
Staff (total of 398 staff observations across 98 days) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change 2011–2013 |
Change 2011–2013 |
||||||||||||
| Category | 2011 | 2012 | 2013 | Δ | (95% CI) | P < 0.01 | 2011 | 2012 | 2013 | Δ | (95% CI) | P < 0.01 | |
| Beverages | |||||||||||||
| Soda/Pop | 3.4 | 1.5 | 0.9 | −2.5 | (−4.0, −1.0) | * | 10.0 | 3.6 | 0.0 | −10.0 | (−14.5, −5.5) | * | |
| Water (HLC target) | 41.9 | 61.3 | 49.4 | 7.5 | (−4.0, 19.0) | 63.5 | 58.1 | 57.7 | −5.8 | (−18.8, 7.2) | |||
| Juice 100% | 3.4 | 4.6 | 7.3 | 3.9 | (1.1, 6.7) | * | 1.6 | 3.3 | 1.1 | −0.5 | (−2.5, 1.5) | ||
| Juice other | 45.9 | 33.8 | 31.6 | −14.3 | (−21.7, −6.9) | * | 14 | 7.5 | 2.5 | −11.5 | (−18.6, −4.4) | * | |
| Milk | 0.7 | 0.8 | 1.5 | 0.8 | (0.0, 1.6) | 0.0 | 0.0 | 0.4 | 0.4 | (−0.5, 1.3) | |||
| Sports D | 13.6 | 11.3 | 12.7 | −0.9 | (−5.1, 3.3) | 15.8 | 13.5 | 3.6 | −12.2 | (−19.9, −4.5) | * | ||
| Energy D | 0.3 | 1.2 | 0.0 | −0.3 | (−0.6, 0.0) | 0.0 | 0.0 | 0.0 | 0.0 | ||||
| Fruits and vegetables | |||||||||||||
| Vegetable (HLC target) | 2.2 | 16.5 | 13.5 | 11.3 | (5.8, 16.8) | * | 8.6 | 21.5 | 10.4 | 1.8 | (−5.7, 9.3) | ||
| Fruit fresh (HLC target) | 28.2 | 43.8 | 44.3 | 16.1 | (10.5, 21.7) | * | 29.8 | 47.4 | 35.1 | 5.3 | (−13.9, 24.5) | ||
| Fruit dried | 2.8 | 3.3 | 4.2 | 1.4 | (−1.0, 3.8) | 5.2 | 0.0 | 2.2 | −3.0 | (−8.6, 2.6) | |||
| Fruit cup | 9.3 | 10.0 | 10.7 | 1.4 | (−1.5, 4.3) | 4.2 | 6.4 | 2.5 | −1.7 | (−5.9, 2.5) | |||
| Apple sauce | 8.1 | 9.2 | 11.1 | 3.0 | (−0.2, 6.2) | 4.8 | 2.5 | 2.7 | −2.1 | (−7.9, 3.7) | |||
| Sugar-based foods | |||||||||||||
| Fruit candy | 15.6 | 17.0 | 14.5 | −1.1 | (−5.5, 3.3) | 4.3 | 2.2 | 0.7 | −3.6 | (−7.4,0.2) | |||
| Cereal | 1.8 | 4.3 | 3.1 | 1.3 | (−0.4, 3.0) | 3.4 | 0.6 | 0.4 | −3.0 | (−5.7, −0.3) | * | ||
| Granola/cereal bar | 12.0 | 15.9 | 19.2 | 7.2 | (1.8, 12.6) | * | 21.8 | 25.5 | 6.0 | −15.8 | (−25.1, −6.5) | * | |
| Candy bar | 5.9 | 3.6 | 3.6 | −2.3 | (−5.2, 0.6) | 2.0 | 1.3 | 0.4 | −1.6 | (−3.8, 0.6) | |||
| Cookie | 23.5 | 22.9 | 23.9 | 0.4 | (−5.5, 6.3) | 10.5 | 7.9 | 1.3 | −9.2 | (−15.5, −2.9) | * | ||
| Pastries | 15.1 | 10.6 | 11.7 | −3.4 | (−7.6, 0.8) | 10.3 | 9.2 | 0.7 | −9.6 | (−15.5, −3.7) | * | ||
| Other dessert | 9.6 | 8.8 | 8.4 | −1.2 | (−4.8, 2.4) | 5.9 | 1.4 | 3.5 | −2.4 | (−7.9, 3.1) | |||
| Salty grains | |||||||||||||
| Cracker | 24.4 | 30.4 | 31.3 | 6.9 | (0.5,13.3) | * | 12.4 | 27.4 | 10.7 | −1.7 | (0.0,−3.4) | ||
| Popcorn | 3.0 | 2.2 | 1.2 | −1.8 | (−3.5, 0.1) | 4.3 | 1.7 | 0.2 | −4.1 | (−7.1, −1.1) | * | ||
| Chips | 52.5 | 42.0 | 38.0 | −14.5 | (−22.1, −6.9) | * | 48.0 | 17.5 | 9.6 | −38.4 | (−51.8, −25.0) | * | |
| Dips and dairy | |||||||||||||
| Dips | 3.5 | 6.6 | 5.8 | 2.3 | (−0.8, 5.4) | 2.4 | 13.5 | 3.6 | 1.2 | (0.0, 2.4) | |||
| Cheese | 5.3 | 9.3 | 8.6 | 3.3 | (0.1, 6.5) | * | 2.1 | 4.1 | 1.6 | −0.5 | (−3.5, 2.5) | ||
| Yogurt | 5.8 | 9.8 | 12.0 | 6.2 | (3.3, 9.1) | * | 2.6 | 8.7 | 4.1 | 1.5 | (−3.7, 6.7) | ||
| Pre-packaged foods | |||||||||||||
| Fast food | 7.2 | 3.2 | 1.8 | −5.4 | (−9.6, −1.2) | * | 9.0 | 7.9 | 5.9 | −3.1 | (−6.2, 0.0) | ||
| LunchableTM | 19.5 | 22.8 | 14.9 | −4.6 | (−6.0, −3.2) | * | 4.1 | 4.9 | 5.6 | 1.5 | (−6.0, 9.0) | ||
| Sandwiches and other | |||||||||||||
| Brown bread with meat | 5.4 | – | 5.8 | 0.4 | (−1.9, 2.7) | 0.1 | 10.4 | 6.0 | 5.9 | (0.0, 11.8) | |||
| White bread with meat | 18.3 | 15.9 | 16.3 | −2.0 | (−6.7, 2.7) | 17.1 | 6.3 | 7.1 | −10.0 | (−20.2, 0.2) | |||
| Brown bread non-meat | 6.8 | 8.1 | 4.9 | −1.9 | (−4.2, 0.4) | 5.7 | 3.5 | 2.5 | −3.2 | (−7.5, 1.1) | |||
| White bread non-meat | 17.7 | 15.9 | 14.0 | −3.7 | (−7.4, 0.0) | 3.0 | 5.9 | 0.9 | −2.1 | (−4.2, 0.0) | |||
| Meat sandwich | – | – | – | – | 9.3 | 8.1 | 5.8 | −3.5 | (−8.5, 1.5) | ||||
| Non-meat sandwich | – | – | – | – | 11.6 | 2.6 | 2.3 | −9.3 | (−13.6, −5.0) | * | |||
| Nuts | – | – | – | – | 0.6 | – | 3.7 | 3.1 | (−0.3, 6.5) | ||||
| Coffee | – | – | – | – | 0.6 | 0.0 | 0.4 | −0.2 | (−1.6, 1.2) | ||||
| Other (pasta, eggs) |
14.5 |
14.2 |
17.3 |
2.8 |
(−0.5, 6.1) |
14.1 |
27.5 |
16.6 |
2.5 |
(−4.6, 9.6) |
|||
* indicates statistical significance at P < 0.01.
Child consumption of fruits, vegetables or water
The consumption of FVW was observed during summer 2013, solely, to determine whether children actually ate/drank the items promoted by the HLC. During lunch and the afternoon snack, five children at each food occasion were observed by trained research staff for the presence of a fruit, vegetable and/or water, and whether they consumed one or more of the three items. The children were selected by randomly identifying five children sitting together during lunch or afternoon snack. The group of children had to have a mix of gender (i.e. boys and girls). Observers recorded the presence of fruits, vegetables and/or water, only, and their consumption. Minimum consumption level was defined as taking at least one bite or drink of the item. This definition was used since we were unable to determine the amount of the items children brought with them to the SDC, thereby precluding the ability to measure the amount consumed or wasted. Only fruits, vegetables and/or water were observed since children could have any number of items for food/beverage that day (see Table I for a complete list of items) and these items were the primary target of the HLC. Inter-observer reliability between two trained research staffers for presence and consumption ranged from 95% to 100% agreement with a κw ranging from 0.94 to 1.00. Children were unaware of the days they were monitored for consumption.
Staff role modeling behaviors
Staff healthy eating promotion behaviors were collected via the System for Observation of Staff Promotion of Activity and Nutrition (SOSPAN). This instrument utilizes momentary time sampling to record instances of staff promotion behaviors consistent with HEPA standards adopted by the SDC organization. SOSPAN has been validated and found reliable [19] in the SDC setting. The staff healthy eating promotion behaviors collected in this study include staff verbal promotion of healthy eating, staff healthy eating education, staff eating inappropriate foods and drinking beverages other than water. Data were collected during each snack and lunch on observation days. Behaviors were coded as either present or not present on each observation day. Inter-observer reliability between two trained research staffers for presence or absence of a staff healthy eating promotion behavior ranged from 94.1% to 100% with a κw ranging from 0.84 to 1.00.
Observer training
In May of each study year, prior to the start of SDC, observers received a 2-hour classroom training session to become familiarized with data collection protocol and operational definitions, and completed classroom-based observations of foods and beverages via photographs taken of actual child and staff foods/beverages brought to SDC, and staff behaviors via videos. Additionally, at the beginning of SDC (early June), the observers took part in eight field-based training sessions in SDCs to ensure accurate collection of all study-related outcomes.
Statistical analysis
Snack category percentages were calculated separately for children and staff for baseline and for each intervention summer. Changes in the daily percentage of foods and beverages brought by children and staff and staff behaviors across the three summers were made using mixed-effects repeated measures regression models, accounting for days nested within SDCs. All foods and beverages brought to the SDCs were expressed as the percentage of children or staff observed at the day level, hence, there was no tracking of individual children or staff across time. For the measure of consumption during lunch or the second afternoon snack, the presence of a fruit, vegetable and/or water was transformed into a percentage and consumption was transformed into a percentage observed each day with the denominator being the number of children with a given item (i.e. presence). Staff behaviors were expressed as a percentage of days that a behavior occurred during schedule snack or lunch. Logistic regression models were also estimated to evaluate the odds of observing a staff behavior at post-assessment compared with baseline. Data were analyzed using Stata (v.12.0; College Station, TX, USA). Additionally, changes in the percentage of children and staff bringing FVW across each of the four SDCs, separately, were evaluated. To account for the multiple comparisons, the Type I error rate was controlled by evaluating significance at P < 0.01.
Results
Across the three summers, a total of 3,308 child observations and 389 staff observations of foods and beverages were collected, representing a total of 98 days (∼33 days per summer or 24 days per SDC) included in the analyses. The types of foods and beverages brought to the SDC by children and staff for each year are presented in Table I. For the primary targets of the HLC, only children’s fruit (+16.1%) and vegetable (+11.3%) increased by summer 2013 when compared with baseline. Decreases in non-target foods and beverages were observed. For children, this included a decrease in soda/pop (−2.5%), non-100% juice (−14.3%), chips (−14.5%) and fast food (−5.4%). For staff, no increases were observed for fruits, vegetables or water. However, significant declines in non-targeted foods and beverages were observed—this includes soda/pop (−10%), non-100% juice (−11.5%), sports drinks (−12.2%), chips (−38.4%), and cookies and pastries (−9.2% to −9.6%) were observed. A total of 560 children were observed for consumption. Approximately 36%, 28% and 41% had water, vegetable and/or a fruit present in the lunch/snack box, respectively. Of these, 55%, 59% and 80% were observed drinking and/or eating the item, respectively. Of the 532 parent contacts across summer 2012 and 2013, 69% of parents each summer were aware of the HLC. Staff surveys indicated they were informed/trained on the HLC and that the majority (>75%) of staff reported wanting to be good role models and were actively involved in the HLC. Seventy percent of staff felt children were interested in the HLC; however, common explanations given for the lack of interest by children were that they were not motivated, or that some age groups (e.g. K and first) were too young to understand and be interested in the challenge.
Changes in staff behaviors are presented in Table II. Staff verbally promoting healthy eating and educating children about healthy eating increased across the three measurement periods from 0.0% of days to 87.1% and 80.6% of days, respectively. Staff consuming inappropriate foods and drinks initially decreased from 2011 to 2012 but increased to 74.2% and 64.5% of days at 2013, an 18.2% and 32.5% increase, respectively, from baseline to final post-assessment. Even with overall decreases in staff bringing inappropriate drinks (see Table I), staff were 2.2 times more likely to be observed drinking inappropriate foods in front of children at final post-assessment when compared with baseline.
Table II.
Increases and decreases of staff healthy eating promotion behaviors from baseline to post-assessment
| Percent of days observed during scheduled snack time |
||||||
|---|---|---|---|---|---|---|
| Summer 2011 | Summer 2012 | Summer 2013 | Δ from baseline to final assessment | Odds post- interventioa | 95% CI | |
| Healthy Eating Promoting Staff Behaviors | ||||||
| Staff verbally promoting healthy eatingb | 0.0 | 50.0 | 87.1 | 87.1 | – | – |
| Staff verbally educating children about healthy eatingb | 0.0 | 34.0 | 80.6 | 80.6 | – | – |
| Healthy Eating Discouraging Staff Behaviors | ||||||
| Staff eating inappropriate foods | 56.0 | 47.7 | 74.2 | 18.2 | 1.6 | (0.9, 2.6) |
| Staff drinking other than water | 32.0 | 25.0 | 64.5 | 32.5 | 2.2 | (1.2, 3.9) |
aOdds ratios derived from multilevel mixed-effects logit regression models. bNo analyses performed due to zero occurrences observed at baseline. Bolded numbers are statistically significant changes at P < 0.05.
Discussion
This study demonstrated that theory-based parent information materials, coupled with a weekly incentive program, can lead to significant and sizeable changes in the percentage of children that bring fruits and/or vegetables for snack or lunch to SDCs. Importantly, decreases in the percentage of children and staff bringing unhealthy foods and beverages, such as soda/pop and chips, were observed even though these were not targeted by the HLC. Thus, while additional refinement of the HLC is necessary, this study showed that it can help SDCs meet the Healthy Eating Standards.
The findings are consistent with the BCT where focusing on positive behaviors, like awarding children for bringing fruit, can lead to the substitution of the more healthful item in placement of less healthful items (e.g. apple instead of chips) [20, 21]. In this study, more children were observed with fruits and vegetables during the intervention summers, and conversely, fewer children with chips, fast food, soda/pop and non-100% juice. The HLC, therefore, can assist SDCs in limiting the less healthful foods and beverages without specifically singling them out. This is important where regulation of what types of foods and beverages can be brought into the SDC is perhaps not feasible, since parents may backlash against such restrictions (as suggested by the SDC leaders). Staff were also successful at creating a healthy eating environment by increasing the number of days that they promoted healthy eating and delivered healthy eating education. However, staff eating and drinking inappropriate foods and drinks in front of the children initially decreased but increased at the final post-assessment. This highlights the importance of continued reinforcement of standards and accountability of staff.
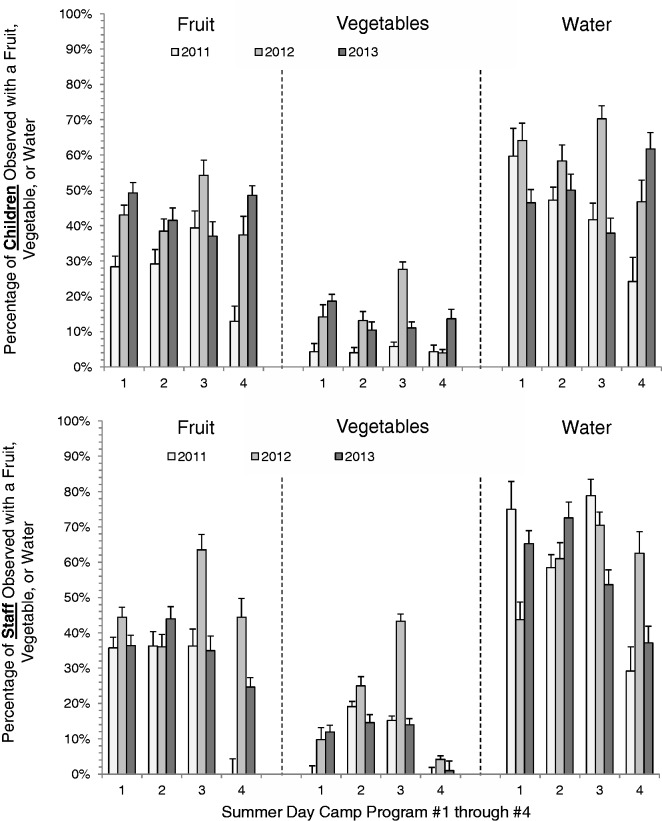
There were greater increases in the percentage of children and staff observed with FVW during the first intervention summer (2012), compared with the last intervention summer (2013). Implementation of the HLC was consistent across the two replications, with ∼69% of the parents during both summers reporting they knew about the HLC. However, based on field notes, the number of staff in summer 2013 was not fully invested in the HLC. This may be due to changes at the SDC leader position, with four new SDC leaders responsible for daily operations during summer 2013 compared with summer 2012. Also, there were inconsistencies across locations, with some SDCs exhibiting substantial increases from summer 2011 to 2013 in children and/or staff observed with a fruit, vegetable and/or water, compared with SDCs where decreases were observed from summer 2012 to 2013 (see Fig. 1). This speaks to the variability that new SDC leaders introduce when delivering the HLC and that future efforts need to take into account turnover at the SDC leader position and devise strategies to minimize its impact.
Fig. 1.
Percentage of children and staff bringing FVW during baseline (summer 2011) and intervention summers (2012–13) for each of the four SDCs, separately.
The strengths of this study include a large sample of children and staff, direct observation of foods and beverages brought to the SDC, direct observation of FVW consumption, theoretically grounded intervention and support of the theoretical premises, and the multiple replications of the intervention across two summers. Limitations include no control group, the delivery of the intervention within only four SDCs, and the potential lack of generalizability of the findings outside these four sites. Additionally, we were unable to fully quantify consumption based on the amount of items brought to the SDCs since children brought all their food and beverage items together and could eat/drink them at any time throughout the day. The design of the study and nature of SDC attendance did not allow for the tracking of kids across the three summers. Thus, the improvements observed could be the result of other factors such as secular changes in society, differences in children enrolled across summers or other unaccounted for variables external to the setting that are associated with an increase in fruits and vegetables and a decline in other less healthful foods (e.g. chips). Finally, in addition to new SDC leadership across the summers, staff employed at the SDCs changed each year. This is an unavoidable scenario in SDCs and potentially dilutes the effectiveness of the HLC by diminishing the implementation—each summer staff need to become familiar with delivering the HLC. Despite this, the HLC still resulted in positive, significant and sizable changes in both staff and child foods and beverages.
In conclusion, the HLC represents a scalable strategy SDCs can use to influence the types of foods and beverages both children and staff bring to SDCs. Future studies should incorporate additional healthy eating strategies to compliment the HLC. These may include partnering with local food sellers to provide discounts, sales or coupons on healthy foods items, sending home pictures of the top healthy lunch boxes to families, providing different rewards and including additional items in the HLC that children can receive points for, such as whole grains.
Funding
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number R21HL106020. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement
None declared.
References
- 1.Carrel AL, Clark RR, Peterson S, et al. School-based fitness changes are lost during the summer vacation. Arch Pediatr Adolesc Med. 2007;161:561–4. doi: 10.1001/archpedi.161.6.561. [DOI] [PubMed] [Google Scholar]
- 2.Gutin B, Yin Z, Johnson M, et al. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: The Medical College of Georgia Fitkid Project. Int J Pediatr Obes. 2008;3(Suppl. 1):3–9. doi: 10.1080/17477160801896457. [DOI] [PubMed] [Google Scholar]
- 3.von Hippel PT, Powell B, Downey DB, et al. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007;97:696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gillis L, McDowell M, Bar-Or O. Relationship between summer vacation weight gain and lack of success in a pediatric weight control program. Eat Behav. 2005;6:137–43. doi: 10.1016/j.eatbeh.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Baranowski T, O'Connor T, Johnston C, et al. School year versus summer differences in child weight gain: a narrative review. Child Obes. 2013;10:18–24. doi: 10.1089/chi.2013.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.America After 3 PM. Special Report on Summer: Missed Opportunities, Unmet Demand. Washington, DC: Afterschool Alliance; 2010. [Google Scholar]
- 7.American Camp Association. 2011 Camp Emerging Issues Survey. Martinsville, IN: 2011. Available at: www.acacamps.org/research/improve/emerging-issues. Accessed: 10 April 2014. [Google Scholar]
- 8.Wiecha JL, Gannett L, Hall G, et al. National Afterschool Association Standards for Healthy Eating and Physical Activity in Out-of-School Time Programs. Wellesley, MA: 2011. Available at: www.niost.org/pdf/host/Healthy_Eating_and_Physical_Activity_Standards.pdf. Accessed: 10 April 2014. [Google Scholar]
- 9.American Camp Association. Camp Trends Fact Sheet. 2009. Available at: www.acacamps.org/media/aca-facts-trends. Accessed: 10 April 2014. [Google Scholar]
- 10.National Afterschool Alliance. America After 3 PM Special Report on Summer. : Missed Opportunities, Unmet Demand. May 2010. Available at: www.afterschoolalliance.org/documents/Special_Report_on_Summer_052510.pdf. Accessed: 10 April 2014. [Google Scholar]
- 11.Bickel WK, Vuchinich RE. Reframing Health Behavior Change with Behavioral Economics. New Jersey: Lawrence Erlbaum Associates, Inc.; 2000. [Google Scholar]
- 12.Locke EA, Latham GP. New directions in goal-setting theory. Curr Direct Psychol Sci. 2006;15:265–8. [Google Scholar]
- 13.Spring B, Schneider K, McFadden HG, et al. Make Better Choices (MBC): study design of a randomized controlled trial testing optimal technology-supported change in multiple diet and physical activity risk behaviors. BMC Public Health. 2010;10:56. doi: 10.1186/1471-2458-10-586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spring K, Schneider K, McFadden HG, et al. Multiple behavior changes in diet and physical activity. Arch Intern Med. 2012;172:789–96. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Caruana A, Vassallo R. Children’s perception of their influence over purchases: the role of parental commuincation patterns. J Consum Mark. 2003;20:55–66. [Google Scholar]
- 16.Turner JJ, Kelly J, McKenna K. Food for thought: parents’ perspectives of child influence. Br Food J. 2006;108:181–91. [Google Scholar]
- 17.Ball SC, Benjamin SE, Ward DS. Development and reliability of an observation method to assess food intake of young children in child care. J Am Diet Assoc. 2007;107:656–61. doi: 10.1016/j.jada.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Economos CD, Sacheck JM, Kwan Ho Chui K, et al. School-based behavioral assessment tools are reliable and valid for measurement of fruit and vegetable intake, physical activity, and television viewing in young children. J Am Diet Assoc. 2008;108:695–701. doi: 10.1016/j.jada.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 19.Weaver R, Beets M, Webster C, et al. System for observing staff promotion of activity and nutrition (SOSPAN) J Phys Activity Health. 2014;11:173–85. doi: 10.1123/jpah.2012-0007. [DOI] [PubMed] [Google Scholar]
- 20.Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. J Public Health. 2012;34:I3–I10. doi: 10.1093/pubmed/fdr111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spring B, Schneider K, McFadden G, et al. Multiple behavior changes in diet and activity a randomized controlled trial using mobile technology. Arch Intern Med. 2012;172:789–96. doi: 10.1001/archinternmed.2012.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]