Abstract
Objective To determine if a school based educational programme aimed at reducing consumption of carbonated drinks can prevent excessive weight gain in children.
Design Cluster randomised controlled trial.
Setting Six primary schools in southwest England.
Participants 644 children aged 7-11 years.
Intervention Focused educational programme on nutrition over one school year.
Main outcome measures Drink consumption and number of overweight and obese children.
Results Consumption of carbonated drinks over three days decreased by 0.6 glasses (average glass size 250 ml) in the intervention group but increased by 0.2 glasses in the control group (mean difference 0.7, 95% confidence interval 0.1 to 1.3). At 12 months the percentage of overweight and obese children increased in the control group by 7.5%, compared with a decrease in the intervention group of 0.2% (mean difference 7.7%, 2.2% to 13.1%).
Conclusion A targeted, school based education programme produced a modest reduction in the number of carbonated drinks consumed, which was associated with a reduction in the number of overweight and obese children.
Introduction
Obesity in children has reached epidemic proportions.1 Ultimately energy imbalance is the reason for excessive weight gain, whether the main cause is genetic, endocrinal, or idiopathic.2 A contributory factor seems to be the consumption of carbonated drinks sweetened with sugar.3 These have a high glycaemic index and are energy dense. Children who drink one regular carbonated drink a day have an average 10% more total energy intake than non-consumers.4 In the United Kingdom more than 70% of adolescents consume carbonated drinks on a regular basis.5
Although school or family based programmes that promote physical activity, modification of dietary intake, and reduction of sedentary behaviours may help reduce obesity in children, few have been effective.6 Recently the United Kingdom based active programme prompting lifestyle in schools (APPLES) reported the effects of multiple interventions on obesity in children.7 The programme included teacher training, modification of school meals, action plans within the curriculum, changes to the tuck shop, physical education, and playground activities. Despite these initiatives there was only a modest increase in consumption of healthy foods such as vegetables without any change in obesity rates. In contrast, there is a paucity of studies on single factors considered to be important in obesity in children. We aimed to determine if a school based educational programme for reducing consumption of carbonated drinks could prevent excessive weight gain in children.
Participants and methods
The Christchurch obesity prevention project in schools (CHOPPS) took place between August 2001 and October 2002 over one school year. The project was based in six junior schools in children aged 7 to 11 years.
Outcome measures
Anthropometric measurements were taken at intervals of six months. Height (without shoes) was measured by one investigator (JJ) to the nearest 0.1 cm with the Portable Leister height measure (Seca, Marsden, United Kingdom). Weight (in light clothing) was measured to the nearest 0.1 kg on medical scales (Seca 770, Marsden). Waist circumference was measured according to published centile charts.8 We converted body mass index (weight (kg)/(height (m)2)) to standard deviation scores (or z scores) and to centile values using the British 1990 growth reference disc (Child Growth Foundation, London).9
The children completed diaries at baseline and at the end of the trial on drinks consumed over three days. Records were made over two weekdays and one weekend day. Collecting dietary data in this way has been shown to provide comprehensive results.10
Intervention
One investigator (JJ) delivered the programme to all classes. The main objective was to discourage the consumption of “fizzy” drinks (sweetened and unsweetened) with positive affirmation of a balanced healthy diet. We thought the children would respond best to a simple, uncomplicated message so they were told that by decreasing sugar consumption they would improve overall wellbeing and that by reducing the consumption of diet carbonated drinks they would benefit dental health. A one hour session was assigned for each class each term. Teachers assisted in the sessions and were encouraged to reiterate the message in lessons. The initial session focused on the balance of good health and promotion of drinking water. The children tasted fruit to learn about the sweetness of natural products. In addition, each class was given a tooth immersed in a sweetened carbonated cola to assess its effect on dentition. The second and third sessions comprised a music competition; each class was given a copy of a song (Ditch the Fizz) and challenged to produce a song or a rap with a healthy message. The final session involved presentations of art and a classroom quiz based on a popular television game show. The children were also encouraged to access further information through the project's website (www.b-dec.com).
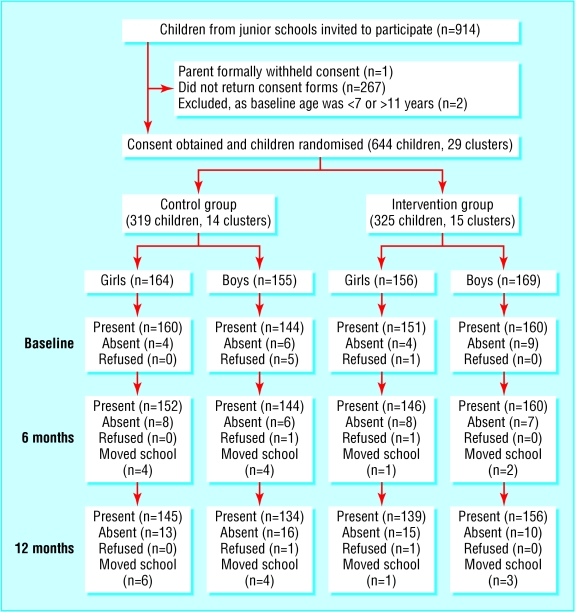
Fig 1.
Trial profile for anthropometric measurements
Statistical methods
We undertook a cluster, randomised controlled trial.11 Clusters were randomised according to a random number table, with blinding to schools or classes. Sample size was estimated based on data from a pilot study conducted in the same geographical area.12 In the pilot, 54% (n = 149) of children gave consent, of whom 71% (n = 108) completed drink diaries. From this we predicted that we needed an average of 12 children in each class. The standard deviation of carbonated drink consumption in the pilot was 0.6 glasses (average glass size 250 ml) a day, therefore a study of this sample size (31 clusters with an average of 12 children) would have 90% power to detect average reductions each day of 0.9, 0.7, and 0.6 glasses over three days using intracluster correlations of 0.1, 0.05, 0.01, and 0.001. Data were analysed using SPSS (version 11) with a 5% significance level. Data for interval scaled measurements for each cluster were derived by averaging all individual measurements for the children in the cluster, and dichotomous data were derived by calculating the proportion in the cluster. These were our summary measures, with clusters as the unit of analysis. All measures were normally distributed. We used the independent sample t test to establish significance between intervention and control clusters and the paired t test to establish the significance of changes within clusters. Intracluster correlation coefficients and 95% confidence intervals were calculated by using Searle's method, with adjustment for variable cluster size.13
Results
The figure outlines the study design. Each of 29 classes (two of the 31 clusters were excluded because they were mixed age classes) was considered as a cluster. Fifteen were randomised to the intervention group and 14 to the control group. At the time of consent, parents and children were unaware of randomisation group. The average class size was 22 (SD 5) children (table 1). In total, 644 of 914 (70.5%) parents and children (320 girls) gave written consent. The average age at baseline was 8.7 (SD 0.9) years (range 7.0 to 10.9 years). Consent was withdrawn for six children (five boys) over the school year. Both groups were similar at baseline for distributions of age, sex, consumption of sweetened carbonated drinks, and percentage overweight or obese (table 2).14 Body mass index was measured in 602 (93.5%) children at six months and 574 (89.1%) at 12 months.
Table 1.
Cluster properties
| School | No of clusters | Average No of children in clusters (No of boys) |
|---|---|---|
| A | 4 | 20 (9) |
| B | 6 | 26 (13) |
| C | 6 | 25 (14) |
| D | 7 | 16 (9) |
| E | 3 | 28 (13) |
| F | 3 | 20 (9) |
| Total | 29 | 22 (11) |
Table 2.
Age, prevalence of overweight and obese children, and mean number of glasses of carbonated drinks consumed daily at baseline
|
Girls
|
Boys
|
|||
|---|---|---|---|---|
| Characteristic | Control group (n=164) | Study group (n=156) | Control group (n=155) | Study group (n=169) |
| Mean (SD) age (years) | 8.7 (0.9) | 8.7 (1.0) | 8.6 (0.9) | 8.7 (0.8) |
| No (%) overweight* | (20) 13 | (19) 13 | (18) 13 | (21) 13 |
| No (%) obese* | (12) 8 | (10) 7 | (10) 7 | (11) 7 |
| Mean (SD) consumption of carbonated drinks; No of glasses in three days† | 1.7 (2.0);(n=5) | 2.2 (2.6);(n=77) | 1.8 (2.0);(n=89) | 1.6 (2.0);(n=91) |
| — | ||||
Defined according to 1990 British body mass index centile charts.14
Average glass size 250 ml.
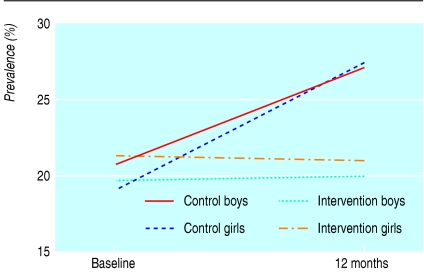
Table 3 shows the body mass indices, z scores (SDS), and percentage of children above the 91% centile at baseline and 12 months and change in anthropometric measurements over 12 months. The intracluster correlation coefficient for body mass index was 0.01 (95% confidence interval -0.01 to 0.06). After 12 months there was no significant change in the difference in body mass index (mean difference 0.13, -0.08 to 0.34) or z score (0.04, -0.04 to 0.12). At 12 months the mean percentage of overweight and obese children increased in the control clusters by 7.5%, compared with a decrease in the intervention group of 0.2% (mean difference 7.7%, 2.2% to 13.1%; fig 2). Assessing and comparing prevalence between studies is influenced by the methods used to classify overweight children (table 4).
Table 3.
Body mass indices, z scores (standard deviation scores), and mean percentages >91st centile at baseline and 12 months
| Characteristic | Control clusters (n=14) | Intervention clusters (n=15) | Mean difference (95% CI) |
|---|---|---|---|
| Baseline*: | |||
| Mean (SD) body mass index | 17.6 (0.7) | 17.4 (0.6) | 0.0 (−0.5 to 0.5) |
| Mean (SDS) z score† | 0.47 (0.2) | 0.50 (0.23) | −0.03 (−0.2 to 0.13) |
| Mean percentage >91 st centile (z score >1.34) | 19.4 (8.4) | 20.3 (6.3) | −0.9 (−6.6 to 4.8) |
| 12 months*: | |||
| Mean (SD) body mass index | 18.3 (0.8) | 17.9 (0.7) | 0.4 (−0.2 to 1.0) |
| Mean (SDS) z score | 0.60 (0.19) | 0.48 (0.23) | 0.12 (−0.04 to 0.28) |
| Mean percentage >91 st centile (z score >1.34) | 26.9 (12.3) | 20.1 (6.7) | 6.8 (−0.7 to 14.3) |
| Change over 12 months‡: | |||
| Mean (SD) body mass index | 0.8 (0.3) | 0.7 (0.2) | 0.1 (−0.1 to 0.3) |
| Mean z score | 0.08 (0.13) | 0.04 (0.07) | 0.04 (−0.04 to 0.12) |
| Mean percentage >91 st centile | 7.5 (8.0) | −0.2 (6.3) | 7.7 (2.2 to 13.1) |
Based on maximum number of children in each cluster.
Age and sex specific body mass index converted to standard deviation score using revised 1990 reference standards.
Based on children with data at baseline and 12 months.
Fig 2.
Mean change in prevalence of overweight and obese children from baseline to follow up at 12 months according to clusters
Table 4.
Prevalence of overweight and obese children (individual analysis). Values are numbers (percentages)
|
Body mass index
|
|||
|---|---|---|---|
| Characteristic | International Obesity Task Force cut off points15 | 1990 British centile charts14 | British waist circumference centile charts12 |
| Overweight boys | |||
| Baseline: | |||
| Control | 33 (18.8) | 28 (19.6) | 28 (20.3) |
| Intervention | 34 (20.1) | 32 (19.2) | 34 (21.5) |
| Follow up: | |||
| Control | 39 (22.2) | 33 (25.6) | 33 (25.0) |
| Intervention | 31 (18.3) | 31 (19.9) | 35 (22.6) |
| Overweight girls | |||
| Baseline: | |||
| Control | 46 (28.0) | 32 (20.1) | 38 (24.4) |
| Intervention | 43 (27.6) | 29 (19.2) | 33 (22.1) |
| Follow up: | |||
| Control | 50 (29.6) | 37 (28.3) | 52 (36.9) |
| Intervention | 39 (23.1) | 29 (20.9) | 40 (29.6) |
| Obese boys | |||
| Baseline: | |||
| Control | 3 (1.7) | 10 (7.0) | 14 (9.9) |
| Intervention | 7 (4.1) | 11 (6.9) | 15 (9.5) |
| Follow up: | |||
| Control | 3 (1.7) | 12 (9.0) | 14 (10.4) |
| Intervention | 6 (3.5) | 11 (7.1) | 13 (8.4) |
| Obese girls | |||
| Baseline: | |||
| Control | 12 (7.3) | 12 (7.5) | 17 (10.7) |
| Intervention | 9 (5.7) | 10 (6.6) | 15 (9.9) |
| Follow up: | |||
| Control | 11 (6.3) | 13 (9.0) | 27 (19.0) |
| Intervention | 8 (4.7) | 9 (6.5) | 16 (11.5) |
Overall, 55.0% (338 of 615) of the children returned the first drink diary and 56.0% (321 of 574) returned the second; 36% (235) returned both. Body mass indices between those children who returned the diaries and those who did not were similar (17.3 (2.3) v 17.5 (2.4), respectively, P = 0.3 using the t test) Overall, 19.0% of the children who did or did not return diaries at baseline were overweight. Baseline consumption of carbonated drinks was similar between children who did or did not return diaries at 12 months (1.8 v 1.9 glasses, -0.7 to 0.3 glasses).
The intracluster correlation for consumption of carbonated drinks was -0.009 (-0.03 to 0.05), suggesting independence between members of each cluster (table 5).13 At 12 months, consumption decreased in the intervention group compared with the control group (mean difference 0.7, 0.1 to 1.3). Water intake increased in both groups, but there was no difference between intervention and control clusters.
Table 5.
Changes in consumption of drinks over 12 months in control clusters (n=14) and intervention clusters (n=15)*. Values are means (SDs) unless stated otherwise
| Type of drink | Baseline | 12 months | Mean change (95% CI) | Difference in consumption (95% CI)† | P value‡ |
|---|---|---|---|---|---|
| Total carbonated drinks: | |||||
| Control clusters
|
1.6 (0.6)
|
1.8 (0.6)
|
0.2 (−0.2 to 0.5)
|
0.7 (0.1 to 1.3) | 0.4
|
| Intervention clusters | 1.9 (0.5) | 1.3 (0.6) | −0.6 (−1.0 to −0.1) | 0.02 | |
| Carbonated drinks with sugar: | |||||
| Control clusters
|
1.1 (0.6)
|
1.2 (0.5)
|
0.0 (−0.3 to 0.4)
|
0.1 (−0.4 to 0.5) | 0.9
|
| Intervention clusters | 1.2 (0.3) | 0.9 (0.6) | −0.3 (−0.6 to 0.1) | 0.2 | |
| Diet carbonated drinks: | |||||
| Control clusters
|
0.4 (0.3)
|
0.6 (0.3)
|
0.1 (−0.1,0.4)
|
0.6 (0.2 to 1.1) | 0.3
|
| Intervention clusters | 0.7 (0.3) | 0.4 (0.2) | −0.3 (−0.6 to −0.1) | 0.7 | |
| Carbonated drinks with caffeine: | |||||
| Control clusters
|
0.7 (0.4)
|
0.6 (0.5)
|
−0.1 (−0.3 to 0.1)
|
−0.0 (−0.4 to 0.3) | 0.4
|
| Intervention clusters | 0.8 (0.3) | 0.6 (0.3) | −0.2 (−0.4 to 0.1) | 0.2 | |
| Water: | |||||
| Control clusters
|
2.9 (0.3)
|
5.1 (2.0)
|
2.2 (0.9 to 3.5)
|
0.3 (−1.3 to 1.9) | 0.003
|
| Intervention clusters | 3.1 (1.1) | 4.3 (2.0) | 1.1 (0.2 to 2) | 0.02 |
Cluster sizes are based on maximum number of children within each cluster.
Units are number of glasses over three days (cluster is unit of analysis). All available data have been used in analysis.
Based on children with data at baseline and 12 months.
Two tailed test.
Discussion
A school based educational programme aimed at reducing the consumption of carbonated drinks to prevent excessive weight gain in children aged 7-11 year olds was effective. Our findings are important, especially as a recent Cochrane review has highlighted the lack of good quality evidence on the effectiveness of interventions in this area on which to base national strategies or to inform clinical practice.10
At the end of our 12 month study both the intervention group and the control group showed a significant increase in consumption of water, in part related to the promotion of drinking water during school to “improve concentration.” Alternatives to diet or sweetened, carbonated drinks are thought to be important in promoting dental health.16 In accordance with local dental guidelines, the children were encouraged not to drink carbonated drinks but to switch to water or to fruit juice diluted 1:3 with water.
Limitations of study
Some limitations to our study may have occurred due to contamination, as randomisation was according to classes and not schools; transfer of knowledge may have taken place outside the classroom, although this would have been minimised by the cluster randomisation design.17 Certain schools did change, encouraging consumption of water. This was seen in both the intervention group and the control group. We had two fewer clusters than anticipated owing to mixed year groups. The low return rate of drink diaries at baseline and completion may have resulted in a response bias; although the proportion of children who were overweight was similar in those who did or did not return the diaries. A further limitation was the use of the diaries over only three days. The validity of self collected dietary data can be questioned owing to a tendency for under-reporting of energy intake, particularly in those who are overweight or obese.10
Currently there is a plethora of guidelines on weight management in children, and obesity prevention is likely to be important within the United Kingdom based National Service Framework for children. Most studies on obesity prevention in children have been multifaceted.18 However, only one school based US study has shown benefit for reducing obesity rates, although this was limited to girls and probably a consequence of watching less television.19 A similar, intensive and multifaceted approach was used in the UK based active programme prompting lifestyle in schools study.7 In that study, children's consumption of vegetables increased but there was no change in prevalence of obesity. Prevention programmes based in the home environment have had beneficial results, but this approach is often difficult to implement across whole populations and historically has mainly focused on people who are already overweight or obese.18 Our intervention was simple, involved no teacher training, and could be easily implemented by a health educator working in several schools.
Small changes in energy intake and output seem to have a major impact on obesity risk. Theoretically, daily consumption of one can of a sweetened carbonated drink (0.50 MJ) over a 10 year period in a constant environment can add 50 kg of weight.20 Conversely, reducing daily intake by a nominal amount of energy or by increasing energy output (the “energy gap”) may help to prevent weight gain. Using data from national surveys, Hill and coworkers suggested that altering the energy gap by 0.42 MJ/day—that is, avoiding one can of sugar sweetened carbonated drink—would prevent excessive weight gain in most adult Americans.21 To have a similar preventive effect in children the energy gap may have to be more than 0.84 MJ/day.22
Recently the World Health Organization recommended that free sugars should account for no more than 10% of daily energy intake.16 This has not been universally accepted, particularly from within the food industry.23 Reducing easy access to energy dense foods may help to limit the opportunities for overeating.24
The term “toxic environment” has been used to describe the myriad factors increasing a child's risk of becoming overweight or obese.20 Although our targeted approach was modestly beneficial, other external influences on children's eating habits and leisure activities need to be debated widely in society. For most people, obesity still remains preventable.
What is already known on this topic
Obesity in children is a major public health problem
Although the cause is multifactorial it has been linked to the consumption of sugar sweetened drinks
Previous school based interventions have been relatively ineffective in preventing obesity
What this study adds
A school based education programme to discourage children from drinking carbonated drinks reduced the number of overweight or obese children in a school year
Schools can have an important role in obesity prevention in children
Amendment
The Results section of the abstract has been amended to read “Consumption of carbonated drinks over three days decreased by 0.6 glasses (average glass size 250 ml) in the intervention group” [not “decreased by 0.6 glasses... a day”]. Figure 2 has been changed because an incorrect version of the figure was included in the original version; data used for the new version of figure 2 do not change the conclusions of the paper.
We thank the headmasters, teachers, parents, and children at the participating schools, William Askew for writing and producing Ditch the Fizz, Julia Knott for help with data entry, Ruth Angel for discussion and advice, and the staff of the Bournemouth Diabetes and Endocrine Centre for help with anthropometric measurements.
Contributors: DK and JJ developed the original idea. JJ delivered the education programme, took the anthropometric measurements, and analysed the data. All authors contributed to writing the manuscript. PT provided statistical and methodological advice. DK directed the project; he will act as guarantor for the paper. DC obtained financial support.
Funding: This project was funded from unrestricted educational grants from GlaxoSmithKline, Aventis, and Pfizer and from internal resources within Bournemouth Diabetes and Endocrine Centre. The external funding bodies had no input into protocol development, data collection, or analyses or interpretation. JJ received a research scholarship from the Florence Nightingale Foundation.
Competing interests: DK and DC each had a child attending one of the schools involved in the Christchurch obesity prevention project in schools.
Ethical approval: This study was approved by the East Dorset research and ethics committee.
References
- 1.Matayka K. Managing obesity in children. Obes Pract 2002;4(2): 2-6. [Google Scholar]
- 2.Goran MI. Metabolic precursors and effects of obesity in children: a decade of progress, 1990-1999. Am J Clin Nutr 2001;73: 158-71. [DOI] [PubMed] [Google Scholar]
- 3.Ludwig DS, Peterson KE, Gortmaker SL. Relation between consumption of sugar-sweetened drinks and childhood obesity: a prospective, observational analysis. Lancet 2001;357: 505-8. [DOI] [PubMed] [Google Scholar]
- 4.Harnack L, Stang J, Story M. Soft drink consumption among US children and adolescents: nutritional consequences. J Am Diet Assoc 1999;99: 436-41. [DOI] [PubMed] [Google Scholar]
- 5.Gregory J, Lowe S. National diet and nutrition survey: young people aged 4 to 18 years. London: Stationery Office, 2000.
- 6.Atkinson RL, Nitzke SA. School based programmes on obesity. BMJ 2001;323: 1018-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Evaluation of implementation and effect of primary school based intervention to reduce risk factors for obesity. BMJ 2001;323: 1027-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Child Growth Foundation. Boys/girls waist circumference centile charts. Harlow: Harlow Printing, 2002.
- 9.Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr 1990;44: 45-60. [PubMed] [Google Scholar]
- 10.Campbell K, Waters E, O'Meara S, Summerbell C. Interventions for preventing obesity in children. Cochrane library, Issue 1. Oxford: Update Software, 2001.
- 11.Donnar A, Klar N. Design and analysis of cluster randomisation trials in health research. London: Arnold, 2000: 6-10.
- 12.James J, Thomas P, Kerr D. Childhood obesity: a big problem for small people. Diabetes Primary Care 2002;4(3): 75-9. [Google Scholar]
- 13.Ukoumunne OC. A comparison of confidence interval methods for the intraclass correlation coefficient in cluster randomised trials. Stat Med 2002;21: 3757-74. [DOI] [PubMed] [Google Scholar]
- 14.Cole TJ, Freeman JV, Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child 1995;73: 25-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole TJ, Bellizi MC, Flegal K, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000;320: 1240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization technical report series. Diet nutrition and the prevention of chronic diseases. Geneva: WHO, 2003: 916. [PubMed]
- 17.Torgerson DJ. Contamination in trials: is cluster randomisation the answer? BMJ 2001;322: 355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.University of York: NHS Centre for Reviews and Dissemination. Effective health care: the prevention and treatment of childhood obesity. London: Royal Society of Medicine, 2002;7(6).
- 19.Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Sujata D, Fox MK, et al. Reducing obesity via a school-based interdisciplinary intervention among youth. Arch Pediatr Adolesc 1999;153: 409-18. [DOI] [PubMed] [Google Scholar]
- 20.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet 2002;360: 473-82. [DOI] [PubMed] [Google Scholar]
- 21.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science 2003;299: 853-7. [DOI] [PubMed] [Google Scholar]
- 22.Butte NF, Ellis KJ. Science 2003;301: 598. [DOI] [PubMed] [Google Scholar]
- 23.Kapp C. Brundtland meets food and drink leaders but declines Coke cocktail. Lancet 2003;361: 1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science 1998;280: 1371-4. [DOI] [PubMed] [Google Scholar]