Abstract
Erosive pustular dermatosis of the scalp (EPDS) is a rare inflammatory disease with unknown etiology that usually occurs in the elderly. It is characterized by multiple sterile pustules, chronic crusted erosions, cicatricial alopecia, and skin atrophy. It typically develops in aged or sun-damaged skin and is most often accompanied by a history of local trauma. Histopathologically, non-specialized change manifests as atrophic epidermis and chronic inflammation. Although this disease mainly occurs in elderly white women, we here report a case of EPDS in a 35-year-old man, following hair transplantation as a local trauma, that was successfully treated with topical steroid.
Keywords: Erosive pustular dermatosis, hair transplantation, scalp
INTRODUCTION
Less than 150 cases have been reported since its first description by Pye et al. in 1979.[1] Erosive pustular dermatosis (EPD) is a rare condition characterized by pustules, erosions, and crusted lesions that heal with scarring alopecia.[1] The development of EPD has been observed previously in some specific conditions such as long-standing solar damage.[2] It is often preceded by trauma to the skin.[3]
Its association with autoimmune diseases has also been described. However, the pathogenesis of EPD remains unclear.[4] Cultures are generally negative, and laboratory and histopathological evaluations are not diagnostic.
CASE REPORT
A 35-year-old man, otherwise healthy, developed erosive crusted plaques on his scalp 9 months after hair transplantation for treatment of long-standing, male-type, androgenetic alopecia. Also, he suffered from mild burning sensation without other symptom such as pain, pruritus, and malodoration, and he did not use any medication such as topical minoxidil before development of this lesion. Despite treatment with topical and systemic antibiotics, the lesions enlarged gradually. He was referred to us for evaluation of the eruption. On physical examination, a large ulcerative plaque covered with crusts was seen on the parietal part of his scalp [Figure 1]. The remainder of the skin examination was essentially normal, with no features of a blistering disorder or psoriasis. There was no evidence of lymphadenopathy in head and neck on examination. Bacterial and fungal culture evaluations were negative. Routine laboratory blood tests were normal except for elevated values of markers of inflammation (erythrocyte sedimentation rate, C-reactive protein). Autoantibodies (antinuclear antibodies, rheumatoid factor, thyroglobulin, and microsomal antibodies) were negative. No abnormal finding was seen on serum immunoglobulin levels, anti-desmoglein 1 and 3, and anti-BP180 antibodies. No evidence of internal malignancy or infectious focus was revealed by various systemic examinations including chest X-ray, abdominal sonogram, and computed tomography.
Figure 1.

Clinical appearance of the scalp: Diffuse crusting associated with multiple pustular, exudative, and erosive lesions
After referral to us, a skin biopsy was done from the lesional area; we diagnosed the patient's eruption as EPD of the scalp. The patient was treated with topical clobetasol propionate lotion, twice daily, which resulted in significant pustular lesion improvement and re-epithelization within a week [Figure 2].
Figure 2.

After 1 week of the treatment with topical steroid
Pathological findings
A Histopathological examination of a 3-mm punch biopsy showed a dense, mainly perifollicular, dermal infiltrate of neutrophils and lymphocytes. There was no evidence of malignancy or vasculitis [Figure 3]. Direct Immunofluorescence findings were negative, ruling out the possibility of autoimmune blistering disease. Special staining for fungi was negative.
Figure 3.
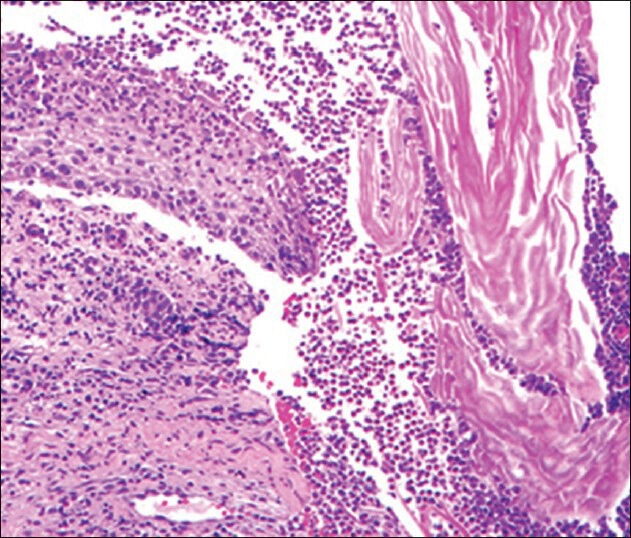
Dense infiltrate of neutrophils and lymphocytes in reticular dermis and around hair follicles
DISCUSSION
EPD of the scalp is an uncommon condition that occurs mainly in the elderly.[5] It tends to affect elderly white women and often has a preceding history of trauma to the skin, including sun-damage, skin grafting, laser, cryotherapy, and X-ray therapy.[6,7,8] First described in 1979, it is characterized by sterile pustules, chronic crusted erosions, cicatricial alopecia, and skin atrophy.[3] Although the pathogenesis is not well-known, predisposing factors such as recent or past local trauma and surgical procedures have been reported.[9,10] It is generally believed that local trauma such as incidental trauma,[9] skin graft for actinic keratoses,[8] or actinic damaged skin,[9] acts as a triggering factor.[5] Moreover, autoimmune disorders such as rheumatoid arthritis[4] have been described in association with EPDS. Therefore, it has been suggested that physical trauma to the skin might cause auto-antibody production acting against skin structures that results in a secondary inflammatory reaction.[4,11] The fact that EPDS responds to topical anti-inflammatory agents supports this hypothesis.[12] In our patient, we took into consideration the possibility that the tissue damage caused by hair transplantation might have induced subsequent EPDS. Usually skin swabs and scrapings are negative for bacteria and fungi. If microorganisms are found, this is probably the sign of a secondary colonization rather than that of a primary infection.[7,8] Histopathologically, EPDS is non-specific, showing atrophic epidermis and chronic inflammation consisting of lymphocytes, neutrophils, plasma cells, and occasional foreign body giant cells.[13] Erosive pustular dermatosis of the scalp is a diagnosis of exclusion,[14] based on histopathological and microbiological examination,[13] with a wide list of differential diagnoses including bacterial or fungal infection, pemphigus, squamous cell carcinoma and dermatitis artefacta, folliculitis decalvans, pyoderma gangrenosum, and cicatricial pemphigoid.[9,13] The nonspecific histopathological pattern, the evolution leading to scarring alopecia, and the resistance to antibiotics, with response to steroids, favor such a diagnosis.[5]
Several drugs have been tried to treat this disease, normally with partial improvement. Potent topical steroids have been widely used in EPDS[15] and, often, there is a good response to potent topical corticosteroids, but typically with a relapse when treatment is stopped. The following treatment regimens have been reported to be effective: Oral isotretinoin, zinc sulphate, nimesulide, topical tacrolimus, or calcipotriol.[7,16,17] Curiously, a single case treated with photodynamic therapy has also been described.[18] Topical application of corticosteroid may suppress the keratinocyte production of this neutrophil attractant, thereby exerting therapeutic effect.[19] Our patient was treated successfully with topical steroid plus oral zinc sulphate. We controlled the patient's condition for 6 months after his wound had healed; the result was that no relapse occurred.
LIMITATIONS
Our experience and success with topical steroid for EPDS is observational and not the result of a randomized, controlled trial.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pye PJ, Peachey RDG, Burton JL. Erosive pustular dermatosis of the scalp. Br J Dermatol. 1979;100:559–66. doi: 10.1111/j.1365-2133.1979.tb05581.x. [DOI] [PubMed] [Google Scholar]
- 2.Trueb RM, Krasovec M. Erosive pustular dermatosis of the scalp following radiation therapy for solar keratosis. Br J Dermatol. 1999;141:763–5. doi: 10.1046/j.1365-2133.1999.03138.x. [DOI] [PubMed] [Google Scholar]
- 3.Petersen BO, Bygum A. Erosive pustular dermatosis of the scalp: A case treated successfully with isotretinoin. Acta Derm Venereol. 2008;88:300–1. doi: 10.2340/00015555-0416. [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto T, Furuse Y. Erosive pustular dermatosis of the scalp in association with rheumatoid arthritis. Int J Dermatol. 1995;34:148. doi: 10.1111/j.1365-4362.1995.tb03605.x. [DOI] [PubMed] [Google Scholar]
- 5.Guarneri C, Vaccaro M. Erosive pustular dermatosis of the scalp following topical methylaminolaevulinate photodynamic therapy. J Am Acad Dermatol. 2009;60:521–2. doi: 10.1016/j.jaad.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Rongioletti F, Delmonte S, Rossi ME, Strani GF, Rebora A. Erosive pustular dermatosis of the scalp following cryotherapy and topical tretinoin for actinic keratoses. Clin Exp Dermatol. 1999;24:499–500. doi: 10.1046/j.1365-2230.1999.00546.x. [DOI] [PubMed] [Google Scholar]
- 7.Mastroianni A, Cota C, Ardigo M, Minutilli E, Berardesca E. Erosive pustular dermatosis of the scalp: A case report and review of the literature. Dermatology. 2005;211:273–6. doi: 10.1159/000087023. [DOI] [PubMed] [Google Scholar]
- 8.Ena P, Lissia M, Doneddu GME, Campus GV. Erosivepustular dermatosis of the scalp in skin grafts: Report of three cases. Dermatology. 1997;194:80–4. doi: 10.1159/000246066. [DOI] [PubMed] [Google Scholar]
- 9.Grattan CE, Peachey RD, Boon A. Evidence for a role of local trauma in the pathogenesis of erosive pustular dermatosis of the scalp. Clin Exp Dermatol. 1988;13:7–10. doi: 10.1111/j.1365-2230.1988.tb00639.x. [DOI] [PubMed] [Google Scholar]
- 10.Layton AM, Cunliffe WJ. A case of erosive pustular dermatosis of the scalp following surgery and a literature review. Br J Dermatol. 1995;132:472–3. doi: 10.1111/j.1365-2133.1995.tb08687.x. [DOI] [PubMed] [Google Scholar]
- 11.Hashimoto N, Ishibashi Y. Pustular dermatosis of the scalp associated with autoimmune diseases. J Dermatol. 1989;16:383–7. doi: 10.1111/j.1346-8138.1989.tb01285.x. [DOI] [PubMed] [Google Scholar]
- 12.Kim KR, Lee JY, Kim MK, Yoon TY. Erosive pustular dermatosis of the scalp following herpes zoster: Successful treatment with topical tacrolimus. Ann Dermatol. 2010;22:232–4. doi: 10.5021/ad.2010.22.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burton JL, Peachey RD, Pye RJ. Erosive pustular dermatosis of the scalp-a definition. Br J Dermatol. 1988;119:411. doi: 10.1111/j.1365-2133.1988.tb03242.x. [DOI] [PubMed] [Google Scholar]
- 14.Darwich E, Munoz-santos C, Mascaro JM., Jr Erosive pustular dermatosis of the scalp responding to acitretin. Arch Dermatol. 2011;147:252–3. doi: 10.1001/archdermatol.2010.442. [DOI] [PubMed] [Google Scholar]
- 15.Cenkowski MJ, Silver S. Topical tacrolimus in the treatment of erosive pustular dermatosis of the scalp. J Cutan Med Surg. 2007;11:222–5. doi: 10.2310/7750.2007.00027. [DOI] [PubMed] [Google Scholar]
- 16.Caputo R, Veraldi S. Erosive pustular dermatosis of the scalp. J Am Acad Dermatol. 1993;28:96–8. doi: 10.1016/0190-9622(93)70018-o. [DOI] [PubMed] [Google Scholar]
- 17.Boffa MJ. Erosive pustular dermatosis of the scalp successfully treated with calcipotriol cream. Br J Dermatol. 2003;148:593–5. doi: 10.1046/j.1365-2133.2003.05209_2.x. [DOI] [PubMed] [Google Scholar]
- 18.Meyer T, Lo’ pez-Navarro N, Herrera-Acosta E, Jose A, Herrera E. Erosive pustular dermatosis of the scalp: A successful treatment with photodynamic therapy. Photodermatol Photoimmunol Photomed. 2010;26:44–5. doi: 10.1111/j.1600-0781.2009.00478.x. [DOI] [PubMed] [Google Scholar]
- 19.Sawada Y, Bito T, Kawakami C, Shimauchi T, Nakamura M, Tokura Y. Erosive pustular dermatosis of the scalp and leg associated with myasthenia gravis: A possible pathogenetic role for neutrophil-stimulating cytokines and chemokines. Acta Derm Venereol. 2010;90:652–3. doi: 10.2340/00015555-0971. [DOI] [PubMed] [Google Scholar]


