Abstract
INTRODUCTION:
The prevalence of sleepy driving and sleep-related accidents (SRA) varies widely, and no data exist regarding the prevalence of sleepy driving in Saudi Arabia. Therefore, this study was designed to determine the prevalence and predictors of sleepy driving, near-misses, and SRA among drivers in Saudi Arabia.
MATERIALS AND METHODS:
A questionnaire was developed to assess sleep and driving in detail based on previously published data regarding sleepy driving. The questionnaire included 50 questions addressing socio-demographics, the Epworth Sleepiness Scale (ESS), driving items, and the Berlin Questionnaire. In total, 1,219 male drivers in public places were interviewed face-to-face.
RESULTS:
The included drivers had a mean age of 32.4 ± 11.7 years and displayed a mean ESS score of 7.2 ± 3.8. Among these drivers, 33.1% reported at least one near-miss accident caused by sleepiness. Among those who had actual accidents, 11.6% were attributed to sleepiness. In the past six months, drivers reported the following: 25.2% reported falling asleep at least once during, driving and 20.8% had to stop driving at least once because of severe sleepiness. Young age, feeling very sleepy during driving, and having at least one near-miss accident caused by sleepiness in the past six months were the only predictors of accidents.
CONCLUSION:
Sleepy driving is prevalent among male drivers in Saudi Arabia. Near-miss accidents caused by sleepiness are an important risk factor for car accidents and should be considered as a strong warning signal of future accidents.
Keywords: Accidents, drowsiness, near-miss accidents, sleepiness, sleepy driving
Motor vehicle accidents (MVAs) are a leading cause of mortality and morbidity worldwide and are expected to be the fourth leading cause of death in 2030.[1,2] MVAs cause a huge impact on human and economic resources. Nearly 1.3 million people die per year worldwide, whereas another 20-50 million sustain non-fatal injuries that account for significant disability.[1] Saudi Arabia has one of the highest MVA rates worldwide. In 2011, 544,179 MVAs occurred, resulting in 39,000 injuries and 7,135 deaths, a rate of 20 deaths per day.[3] More than 30% of the hospital beds in Saudi Arabia are occupied by those injured in MVAs.[4]
Universal data suggest that sleepy driving is prevalent and a major cause of MVAs.[5,6,7,8] Although it is difficult to estimate the number of fatal crashes that involve drowsy drivers, some modeling studies have estimated that 15-33% of fatal accidents may involve drowsy drivers.[9] Drowsiness results in several types of neurological dysfunction, such as reduced reaction time, decreased attention, and impaired decision-making skills.[9] Previous studies have identified several predictors of sleep-related accidents (SRA), including being young,[8,10,11,12] male,[8,13] unmarried,[8,10,11] and a professional driver.[8,11,12] It is worth noting that approximately 30% of the Saudi population is in the young age group (between 15-29 years old).[14] Additionally, sleep disorders, particularly sleep-disordered breathing, increase the risk of SRA.[6,10,15] Recent studies indicate that one out of three middle-aged Saudi men is at high risk for obstructive sleep apnea (OSA).[16] It has been estimated that SRAs account for 2.6-33% of MVAs in the U.S.A (8), the U.K. (6), Australia (6), Norway (7), Thailand (9), and the UAE (21). However, no data exist regarding the prevalence of sleepy driving or SRA in Saudi Arabia. We hypothesize that sleepy driving is prevalent among drivers in Saudi Arabia, thus increasing the risk of MVAs. The goal of this study was to determine the prevalence of sleepy driving, near-miss accidents, and SRA in three provinces in Saudi Arabia. Additionally, we aimed to explore the factors contributing to sleepy driving, together with the most effective countermeasures.
Materials and Methods
Study subjects
In this cross-sectional study, a face-to-face interview was performed with drivers in the waiting areas of bus stations, train stations, and hospitals. Truck and long-haul drivers were not included in this study. In total, 1500 drivers were asked to participate in the study. Among those, 1,219 drivers accepted to participate (81.3%). Recruitment occurred from September 2011 to July 2012 in three provinces of Saudi Arabia (Central region [66.0%], Western region [25.0%], and Eastern region [8.9%]).
Inclusion criteria included drivers who are ≥18 years old. Participation was voluntary and anonymous. The study was approved by the Institutional Review Board at the College of Medicine of King Saud University.
Questionnaire
The questionnaire used was obtained from previously published studies.[8,17] It contained 50 questions and took approximately 10 minutes to complete. The questionnaires were completed by trained medical students who interviewed the drivers. For near-miss driving accidents and driving accidents, the following definitions were adopted:[8] a near-miss driving accident was defined as an event that had limited impact and did not cause any damage or injury; a driving accident was defined as an event where physical injury or material damage occurred.
The following questions were included:
A set of eleven questions covering information regarding socio-demographics.
Daytime sleepiness was assessed using the Epworth Sleepiness Scale (ESS), which is a validated eight-item questionnaire designed to explore the subject's likelihood of falling asleep in common settings.[17] The questionnaire asks the subject to rate the probability of falling asleep on a scale of increasing probability from 0 to 3 for eight different situations that most people experience during their daily life. The score ranges from 0 to 24, and a score of ≥10 indicates increased daytime sleepiness.
Two questions evaluating work times and duration.
Ten questions evaluating sleep pattern and use of medication.
Five questions exploring driving habits.
Three questions assessing the presence, time, and location of sleepy driving in the past six months.
Two questions evaluating actually falling asleep behind the wheel and stopping the car because of sleepiness.
Three questions exploring the occurrence of sleepy driving accidents, near-miss driving accidents, and any another types of driving accidents.
Five more questions evaluating the cause of sleepy driving, the most frequently used countermeasures, and the most effective countermeasures according to the drivers.
The Berlin Questionnaire (BQ) was used to screen for OSA. BQ is a validated questionnaire that stratifies subjects into high-risk and low-risk categories according to their responses.[18]
Statistical analysis
The data are summarized as the mean values and standard deviations (SD) in both the text and tables. Student's t-test was performed to compare the mean values of continuous data. If the normality test failed, the Mann–Whitney U-test was used. For categorical data, the chi-square test was used. The results were considered to be statistically significant if P < 0.05. Variables with a significant P value were evaluated further using a multivariate logistic regression model. Statistical Package for the Social Sciences (SPSS), IBM version 19 (SPSS Inc., Chicago, IL, USA) software was used for data analysis and management.
Results
Sample characteristics
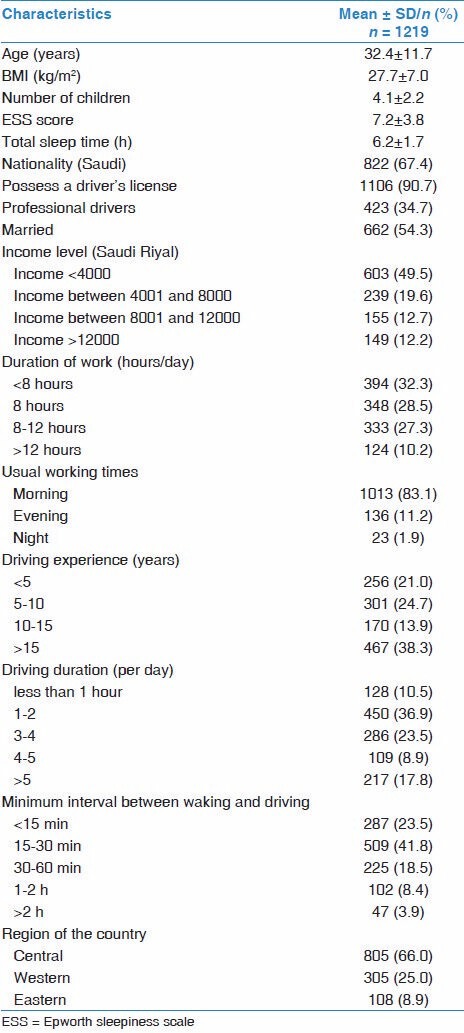
Table 1 presents the demographics and general characteristics of the sample (n = 1,219). The sample was exclusively composed of men, as women do not drive in Saudi Arabia. The group had a mean age of 32.4 ± 11.7 years and exhibited a body mass index of 27.7 ± 7.0 kg/m2. Saudis constituted 67.4% of the subjects. Professional drivers comprised 34.7% of the sample. The mean total sleep time of the drivers was 6.2 ± 1.7 h/day. Surprisingly, 9.3% of the surveyed drivers did not possess a driver's license. We found no difference in the rate of accidents between drivers with and without a driver's license. All participants denied taking alcohol, illicit drugs, or sedatives. Alcohol is illegal in Saudi Arabia and that might have influenced their response.
Table 1.
General and demographic characteristics of the participants
Sleepiness of drivers
The ESS score of the participants was 7.2 ± 3.8. The prevalence of sleepiness (ESS score ≥10) was 19.4%. Of the surveyed subjects, 64.1% felt very sleepy while driving at least once during the past six months, and approximately one-fifth (20.8%) of the drivers stopped driving because of sleepiness at least once in the past six months. Additionally, approximately one-quarter (25.2%) of the participants experienced falling asleep at the wheel at least once while driving in the past six months [Table 2].
Table 2.
Sleepiness, near-miss accidents and actual accidents
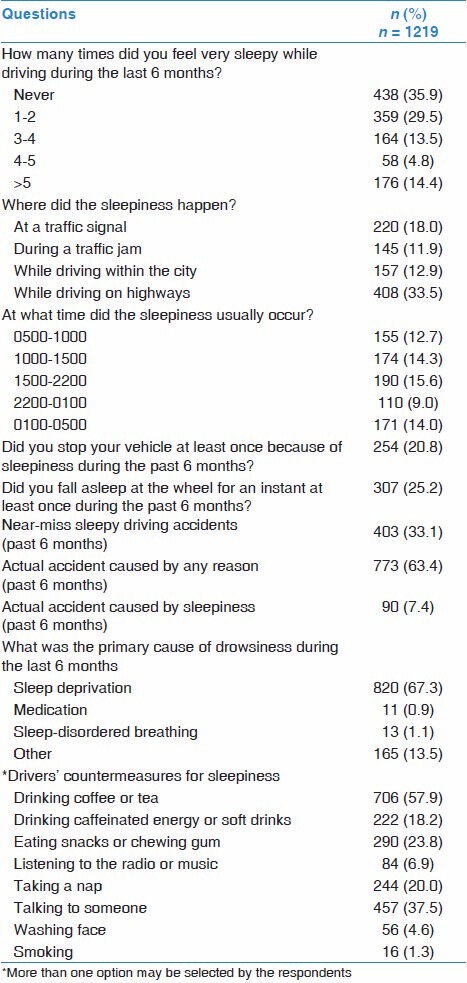
Near-miss accidents and accidents
During the past six months, 63.4% (n = 773) reported being in at least one accident [Table 1]. Of these accidents, 11.6% (n = 90) were caused by sleepiness. Moreover, 33.1% reported at least one near-miss accident caused by sleepiness during the past six months. Most of the participants (67.3%) considered sleep deprivation to be the primary cause of sleepy driving. Accidents were related to age and were more likely to occur among young drivers. The frequency of accidents in the age groups 18-30 years, 31-50 years, and >50 years were 59.7%, 30.9%, and 9.4%, respectively.
The most commonly used countermeasure to fight sleepiness was drinking coffee/tea (57.9%), followed by getting involved in a conversation (37.5%) [Table 2].
Table 3 provides a comparison between drivers who were in accidents and those who were not. Those who were in accidents were younger (31.5 ± 11.6 vs. 34 ± 11.9 years [P = 0.001]), more likely to feel very sleepy while driving (72.3% vs. 55.6% [P < 0.001]), more likely to fall asleep at least once while driving in the past six months (32.1% vs. 20.6% [P < 0.001]), and more likely to have experienced at least one near-miss accident caused by sleepiness during the past six months (40.7% vs. 21.7% [P < 0.001]).
Table 3.
Comparison between participants who experienced at least one actual accident during driving and those who did not
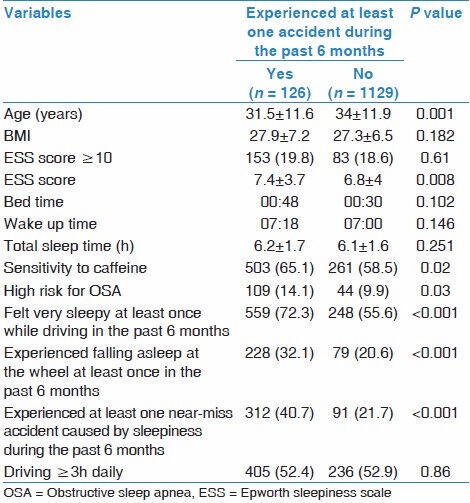
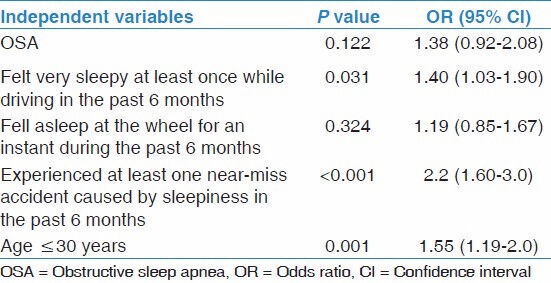
Table 4 presents the multivariate regression analysis performed to predict driving accidents. Younger age (≤30 years) (1.55; C.I: 1.19-2.0), feeling very sleepy during driving (1.40; C.I: 1.03-1.9), and experiencing at least one near-miss accident caused by sleepiness in the past six months (2.2; C.I: 1.60-3.0) were the only predictors of accidents.
Table 4.
Multivariate logistic regression analysis to predict automobile accidents
Discussion
This study is the first to address sleepiness and MVAs among drivers in Saudi Arabia (a country with one of the highest MVA rates). Sleepy driving, sleep-related near-miss accidents, and accidents are prevalent among drivers in Saudi Arabia.
Our data reveal that approximately one-fifth (20.8%) of the drivers in the sample stopped driving because of sleepiness at least once in the past six months, and approximately one-fourth (25.2%) of the participants experienced falling asleep at the wheel at least once while driving in the past six months. Our results are comparable to the results of Sagaspe et al. who demonstrated that approximately one-third of French drivers experienced at least one episode of severe sleepiness at the wheel over a one-year period.[8] In a sample of US drivers, who responded to a telephone survey, 41% admitted to having “fallen asleep or nodded off” at the wheel.[19] In the current study, we found that 19.4% of the drivers possessed an ESS score of ≥10. However, we found no association between pathological ESS scores and driving accidents. Our results concur with those of Sagaspe et al. in French drivers, in which no association was detected between pathological ESS and actual accidents.[8] In contrast, Powell et al. reported an association between ESS scores and accidents.[11] However, Powell et al. reported data over three-year period, increasing the statistical power of their data, whereas we utilized a six-month period and Sagaspe et al. utilized one-year period.[8,11] ESS is a measure of chronic sleepiness rather than acute sleepiness. In a population-based control study that included drivers involved in accidents (n = 571), Connor et al. found that acute sleepiness among automobile drivers significantly increased the risk of an injury-causing accident.[20] However, there was no increase in the risk associated with measures of chronic sleepiness.[20]
A high proportion of accidents were sleep-related. Among drivers who were in accidents in the past six months, 11.6% of the accidents were sleep-related. A national survey in the US estimated that 7.0% of all crashes in which a passenger vehicle was towed, 13.1% of crashes that resulted in a person being admitted to a hospital, and 16.5% of fatal crashes involved a drowsy driver.[19] Near-miss accidents caused by sleepiness were reported by approximately one-third of the surveyed drivers in the past six months. Our study identified near-miss accidents caused by sleepiness as a predictor of actual driving accidents. A near-miss accident by a sleepy driver has been reported to predict a higher accident risk in previous studies. In a cross-sectional internet-linked survey, Powell et al. reported that near-miss sleep-related accidents are strong predictors of actual driving accidents.[11] The risk of having an accident increased from 23.2% among those with no near-misses to 44.5% among those with four or more near-miss accidents over a three-year period.[11] Although the ESS score was significantly higher among those with accidents and was statistically significant (7.4 ± 3.7 vs. 6.8 ± 4 [P < 0.008]), the clinical significance of this difference (less than 1) is less obvious. Studies have shown that ESS does not correlate with objectively measured sleepiness among drivers.[21,22] Sadeghniiat-Haghighi et al. reported poor correlation between the ESS score and sleep latency in the maintenance of wakefulness test (MWT).[22] There was no difference in the ESS score of patients with normal and abnormal MWT 93.24 ± 2.4 vs. 4.08 ± 3).[22] It is possible that drivers underestimate or deny sleepiness to avoid suspending their driving license. Moreover, some drivers who had accidents due to sleepiness may not be sleepy on most of the days but experienced sleepiness on the day of the accident due to sleep deprivation the night before.
The majority of sleepy drivers (67.3%) attributed sleepiness to sleep deprivation. Leechawengwongs et al., reported that sleep deprivation was the primary cause of drowsiness driving among Thai bus and truck drivers.[23] In the U.S.A., it has been estimated that 56,000 accidents per year are related to sleep deprivation.[24] Dawson and Reid reported that wakefulness for 17 hours reduces cognitive and psychomotor performance to a level comparable to the performance impairment detected among those with a blood alcohol concentration (BAC) of 0.05%.[25] Another study demonstrated that the effects of 17-19 hours of wakefulness on performance were equivalent to or worse than the effects of a BAC of 0.05%.[26] Response speeds were decreased by up to 50% in some tests, and accuracy measures were lower among individuals experiencing sleep deprivation than among individuals who consumed alcohol.[26]
Increased risk of MVAs has been linked to younger age and sleep disorders.[6] We found that the prevalence of accidents was higher in the younger age group. In a counterbalanced design, Filtness et al., assessed the effect of sleep restriction for the preceding five hours on prolonged (two hours) afternoon simulated driving in 20 younger (mean age = 23 years) and 19 older (mean age = 67 years) healthy drivers.[27] Following normal sleep, there were no differences between the two groups. However, after sleep restriction, young drivers exhibited significantly more sleepiness-related lane deviations and greater low-frequency EEG power (4-11 Hz), indicative of sleepiness.[27] Several factors have been proposed for this association between young age and accidents, including a higher propensity to consume alcohol or other illicit drugs.[8,28] However, another likely factor is sleep deprivation. Young age is typically associated with sleep deprivation.[29] In the present study, the prevalence of a high risk for OSA was higher among drivers who were in accidents. In a systematic review, Ellen et al. reported that noncommercial drivers with OSA displayed a significantly increased risk of involvement in MVAs (two- to three-fold greater accident rate).[30] Successful treatment of OSA improved the drivers' performance.[30] This study found no difference in total sleep time between those who experienced at least one MVA in the past six months and those who did not; however, in this study, we did not assess bedtime, wake-up time and sleep duration objectively. It is possible that the data reported by the participants were affected by recall bias. In addition, those with sleepiness may have sleep disorders such as sleep apnea, which may explain the excessive sleepiness. Future studies should aim to assess sleep pattern objectively using portable devices like actigraphy.
Considering that sleepiness is an important cause of MVAs, it becomes important to explore the countermeasures used to prevent sleepiness. This topic has not been well-investigated in the literature. The majority of the drivers in our study (57.9%) consumed tea or coffee, followed by engaging in a conversation (37.5%). In a study in Sweden among people in the national register of vehicle owners, Anund et al., reported the following countermeasures against sleepiness among drivers: Stopping to take a walk (54%), turning on the radio or stereo (52%), opening a window (47%), drinking coffee (45%), and asking passengers to engage in a conversation (35%).[31] Previous studies have indicated that some countermeasures may be effective for reducing sleepiness and accidents. In a matched-control study among drivers on major highways in a rural Washington county, the accident risk was lower among drivers who used highway rest stops, drank coffee within two hours or listened to the radio while driving.[32] Horne and Reyner examined the effects of a <15-minute nap, 150 mg of caffeine in coffee, or a coffee placebo in a randomized study of 10 sleepy subjects who were evaluated using an automobile simulator.[33] They demonstrated that consuming caffeine and taking a nap significantly reduced driving impairments, subjective sleepiness and electroencephalographic (EEG) indications of drowsiness.[33] In another study, Sagaspe et al., tested the effects of a cup of coffee (200 mg of caffeine), a placebo (decaffeinated coffee, 15 mg of caffeine), or a 30-minute nap on nocturnal driving in young and middle-aged participants who drove 125 highway miles between 18:00 and 19:30 hours and between 02:00 and 03:30 hours after coffee, placebo, or a nap. The study showed that coffee significantly improves performance in young and middle-aged participants; however, napping is more effective in younger participants than in older participants.[34]
There are no official data regarding sleepy driving from the General Department of Traffic in Saudi Arabia. In addition, there are no Saudi traffic laws with respect to sleep-related accidents or driving with a sleep disorder. Several European countries, in addition to Canada, Australia, and several U.S.A. states, possess specific traffic laws that prohibit patients with sleep disorders, such as OSA and narcolepsy, from driving or obtaining a driver's license until the disorder is medically treated.[6,35] To reduce the number of accidents caused by sleepiness and sleep disorders in Saudi Arabia, traffic regulations must be implemented to reduce the risk of sleepy driving. Regulations should hold sleepy drivers accountable for the risks that they take and the damage that they cause.[36] In addition, a national campaign is required to increase drivers' awareness regarding the risk of sleepy driving. It is clear that the public's understanding of the risk of sleepy driving lags far behind the knowledge available to sleep specialists.[36] Drivers should realize the importance of getting adequate sleep before driving and using effective countermeasures for sleepiness. Individuals who complain of sleepy driving despite obtaining adequate sleep should seek medical attention.
Our study possesses some inherent limitations that must be addressed. No data were collected regarding material damage or injury. Self-reported data always suffer from recall bias. However, our data are consistent with previous studies.[8,20] In fact, we suggest that the prevalence of sleepy driving may be underestimated, as drivers may feel embarrassed to admit falling asleep and being in sleep-related accidents. Truck drivers are considered as a group at a high risk of sleepy driving. However, this study did not include that group of drivers. Future studies should examine sleepy driving among truck drivers. Moreover, the design of this study does not allow the assessment of fatal accidents secondary to sleepy driving. In addition, future studies should use objective measures to assess sleepiness as previous studies showed inconsistency between subjective and objective measures of daytime sleepiness. Finally, although some information about sleep pattern was gathered, detailed information about sleep hygiene was not collected.
In summary, sleepy driving is prevalent among male drivers in Saudi Arabia. Near-miss accidents caused by sleepiness are an important risk factor for car accidents and should be considered as a strong warning signal of future accidents. A national campaign to increase awareness regarding the risks of sleepy driving to prevent sleepy driving and promote effective countermeasures is required. Future studies should assess the health utilization and cost of sleep driving.
Acknowledgements
This study was supported by a grant from the National Plan for Science and Technology program by the King Saud University Project in Saudi Arabia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.World Health Organization (WHO) Global Plan for the Decade of Action for Road Safety 2011 2020. Geneva: WHO; [Lasted accessed on 2014 January 5]. Available from: http://www.who.int/roadsafety/decade_of_action/plan/english.pdf . [Google Scholar]
- 2.World Health Organization. The global burden of disease, update. [Lasted accessed on 2014 January 3]. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf .
- 3.Ageli MM, Zaidan AM. Road traffic accidents in saudi arabia: An ardl approach and multivariate granger causality. Int J Econ Finance. 2013;5:26–31. [Google Scholar]
- 4.More than one million traffic accident expected In 1442 AH. 2012. [Last cited on 2013 Jun 25]. Available from: http://www.kacst.edu.sa/en/about/media/news/Pages/news4061230-5507.aspx .
- 5.Nabi H, Guéguen A, Chiron M, Lafont S, Zins M, Lagarde E. Awareness of driving while sleepy and road traffic accidents: Prospective study in GAZEL cohort. BMJ. 2006;333:75. doi: 10.1136/bmj.38863.638194.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.de Mello MT, Narciso FV, Tufik S, Paiva T, Spence DW, Bahammam AS, et al. Sleep disorders as a cause of motor vehicle collisions. Int J Prev Med. 2013;4:246–57. [PMC free article] [PubMed] [Google Scholar]
- 7.Phillips RO, Sagberg F. Road accidents caused by sleepy drivers: Update of a Norwegian survey. Accid Anal Prev. 2013;50:138–46. doi: 10.1016/j.aap.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Sagaspe P, Taillard J, Bayon V, Lagarde E, Moore N, Boussuge J, et al. Sleepiness, near-misses and driving accidents among a representative population of French drivers. J Sleep Res. 2010;19:578–84. doi: 10.1111/j.1365-2869.2009.00818.x. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC). Drowsy driving - 19 states and the District of Columbia, 2009-2010. MMWR Morb Mortal Wkly Rep. 2013;61:1033–7. [PubMed] [Google Scholar]
- 10.Philip P, Sagaspe P, Lagarde E, Leger D, Ohayon MM, Bioulac B, et al. Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Med. 2010;11:973–9. doi: 10.1016/j.sleep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 11.Powell NB, Schechtman KB, Riley RW, Guilleminault C, Chiang RP, Weaver EM. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30:331–42. doi: 10.1093/sleep/30.3.331. [DOI] [PubMed] [Google Scholar]
- 12.Asaoka S, Abe T, Komada Y, Inoue Y. The factors associated with preferences for napping and drinking coffee as countermeasures for sleepiness at the wheel among Japanese drivers. Sleep Med. 2012;13:354–61. doi: 10.1016/j.sleep.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Abe T, Komada Y, Inoue Y. Short sleep duration, snoring and subjective sleep insufficiency are independent factors associated with both falling asleep and feeling sleepiness while driving. Intern Med. 2012;51:3253–60. doi: 10.2169/internalmedicine.51.7518. [DOI] [PubMed] [Google Scholar]
- 14.Ministry of Economy and Planning, Central Department of Statistics and Information. 2009-2010. [Last accessed 2013 December 28]. Available from: http://www.cdsi.gov.sa/english/
- 15.Howard ME, Desai AV, Grunstein RR, Hukins C, Armstrong JG, Joffe D, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–21. doi: 10.1164/rccm.200312-1782OC. [DOI] [PubMed] [Google Scholar]
- 16.BaHammam AS, Alrajeh MS, Al-Jahdali HH, BinSaeed AA. Prevalence of symptoms and risk of sleep apnea in middle-aged Saudi males in primary care. Saudi Med J. 2008;29:423–6. [PubMed] [Google Scholar]
- 17.Johns MW. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 18.Netzer NC, Hoegel JJ, Loube D, Netzer CM, Hay B, Alvarez-Sala R, et al. Sleep in Primary Care International Study Group. Prevalence of symptoms and risk of sleep apnea in primary care. Chest. 2003;124:1406–14. doi: 10.1378/chest.124.4.1406. [DOI] [PubMed] [Google Scholar]
- 19.Tefft B. The prevalence and impact of drowsy driving. Asleep at the Wheel: The Prevalence and Impact of Drowsy Driving. AAA Foundation for Traffic Safety. 2010. [Accessed on 2013 November 6]. Available from: https://www.aaafoundation.org/sites/default/files/2010DrowsyDrivingReport_1.pdf .
- 20.Connor J, Norton R, Ameratunga S, Robinson E, Civil I, Dunn R, et al. Driver sleepiness and risk of serious injury to car occupants: Population based case control study. BMJ. 2002;324:1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yamamoto K, Kobayashi F, Hori R, Arita A, Sasanabe R, Shiomi T. Association between pupillometric sleepiness measures and sleep latency derived by MSLT in clinically sleepy patients. Environ Health Prev Med. 2013;18:361–7. doi: 10.1007/s12199-013-0331-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sadeghniiat-Haghighi K, Moller HJ, Saraei M, Aminian O, Khajeh-Mehrizi A. The epworth sleepiness scale for screening of the drowsy driving: Comparison with the maintenance of wakefulness test in an Iranian sample of commercial drivers. Acta Medica Iran. 2014;52:125–9. [PubMed] [Google Scholar]
- 23.Leechawengwongs M, Leechawengwongs E, Sukying C, Udomsubpayakul U. Role of drowsy driving in traffic accidents: A questionnaire survey of Thai commercial bus/truck drivers. J Med Assoc Thai. 2006;89:1845–50. [PubMed] [Google Scholar]
- 24.National Highway Traffic Safety Administration. An Analysis of the Significant Decline in Motor Vehicle Traffic Fatalities in 2008. [Last accessed on 2013 Dec 10];Ann Emerg Med. 2011 58:377–8. doi: 10.1016/j.annemergmed.2011.08.008. Available from: http://www-nrd.nhtsa.dot.gov/Pubs/811346.pdf . [DOI] [PubMed] [Google Scholar]
- 25.Dawson D, Reid K. Fatigue, alcohol and performance impairment. Nature. 1997;388:235. doi: 10.1038/40775. [DOI] [PubMed] [Google Scholar]
- 26.Williamson AM, Feyer AM. Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med. 2000;57:649–55. doi: 10.1136/oem.57.10.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Filtness AJ, Reyner LA, Horne JA. Driver sleepiness-comparisons between young and older men during a monotonous afternoon simulated drive. Biol Psychol. 2012;89:580–3. doi: 10.1016/j.biopsycho.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 28.Calafat A, Blay N, Juan M, Adrover D, Bellis MA, Hughes K, et al. Traffic risk behaviors at nightlife: Drinking, taking drugs, driving, and use of public transport by young people. Traffic Inj Prev. 2009;10:162–9. doi: 10.1080/15389580802597054. [DOI] [PubMed] [Google Scholar]
- 29.Bonnet MH, Arand DL. We are chronically sleep deprived. Sleep. 1995;18:908–11. doi: 10.1093/sleep/18.10.908. [DOI] [PubMed] [Google Scholar]
- 30.Ellen RL, Marshall SC, Palayew M, Molnar FJ, Wilson KG, Man-Son-Hing M. Systematic review of motor vehicle crash risk in persons with sleep apnea. J Clin Sleep Med. 2006;2:193–200. [PubMed] [Google Scholar]
- 31.Anund A, Kecklund G, Peters B, Akerstedt T. Driver sleepiness and individual differences in preferences for countermeasures. J Sleep Res. 2008;17:16–22. doi: 10.1111/j.1365-2869.2008.00633.x. [DOI] [PubMed] [Google Scholar]
- 32.Cummings P, Koepsell TD, Moffat JM, Rivara FP. Drowsiness, counter-measures to drowsiness, and the risk of a motor vehicle crash. Inj Prev. 2001;7:194–9. doi: 10.1136/ip.7.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horne JA, Reyner LA. Counteracting driver sleepiness: Effects of napping, caffeine, and placebo. Psychophysiology. 1996;33:306–9. doi: 10.1111/j.1469-8986.1996.tb00428.x. [DOI] [PubMed] [Google Scholar]
- 34.Sagaspe P, Taillard J, Chaumet G, Moore N, Bioulac B, Philip P. Aging and nocturnal driving: Better with coffee or a nap. A randomized study? Sleep. 2007;30:1808–13. doi: 10.1093/sleep/30.12.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krieger J. Sleep apnoea and driving: How can this be dealt with? Eur Respir Rev. 2007;16:189–95. [Google Scholar]
- 36.Powell NB, Chau JK. Sleepy driving. Sleep Med Clin. 2011;6:117–24. [Google Scholar]


