Short abstract
The UK government is considering establishing a national primary angioplasty service for patients with acute myocardial infarction. David Smith and Kevin Channer debate whether moving away from first line thrombolysis is appropriate or practical
There seems little doubt that acute ST elevation myocardial infarction is the result of coronary arterial occlusion and that myocardial necrosis can be limited by early restoration of normal antegrade blood flow. The relation between normal coronary artery blood flow and mortality after myocardial infarction is well documented. A meta-analysis of angiographic infarct trials showed normal flow was associated with a mortality of 3.7% compared with 6.6% (P = 0.0001) in patients with impaired flow and 9.2% (P = 0.0003) in patients with occluded or nearly occluded infarct related arteries.1 This relation extends to microvascular reperfusion so that mortality after myocardial infarction can be reduced to less than 1% if normal epicardial blood flow and myocardial perfusion are restored.2 The mortality benefits of restoring normal flow have been shown to extend up to 12 years.3 Early restoration of normal myocardial blood flow must therefore be the therapeutic goal of the management of acute myocardial infarction.
Angioplasty is more widely applicable
For the past 20 years there have been two methods for restoring blood flow. Thrombolysis (the current first line treatment) is pharmacological, can be applied to only 60-80% of the presenting population, fails to make a definitive diagnosis, and leaves the treatment goal unconfirmed. Coronary angioplasty, on the other hand, is mechanical, can be applied to any patient, is guided by an accurate definitive diagnosis, and results in certainty about the therapeutic end point. Primary angioplasty carries no risk of inappropriate treatment and a low risk of serious complications whereas thrombolysis can be used inappropriately in up to 10% of presenting patients and has an appreciable risk of producing disabling stroke.
All trials comparing the two treatments support primary angioplasty as the better management. None of the trials show thrombolysis is superior, despite the favourable bias of restricting the studies to patients suitable for thrombolysis. Nevertheless, only a tiny proportion of patients with ST elevation myocardial infarction in Britain get primary angioplasty.
Let us consider the use of thrombolysis in 100 patients presenting with ST elevation myocardial infarction. About 25% of patients are ineligible because of late presentation, bleeding history, hypertension, etc, and some have treatment stopped prematurely because of reactions such as hypotension and allergy. Of the 75 patients who receive treatment 24 (32%) can expect to have normal coronary flow restored if streptokinase is used or 40.5 (54%) if alteplase is used.4 Of these, about 10% would have had spontaneous reperfusion and will have therefore received thrombolysis unnecessarily. On this basis between a quarter (streptokinase) and a half (alteplase) of patients presenting achieve the therapeutic goal without undue risk.
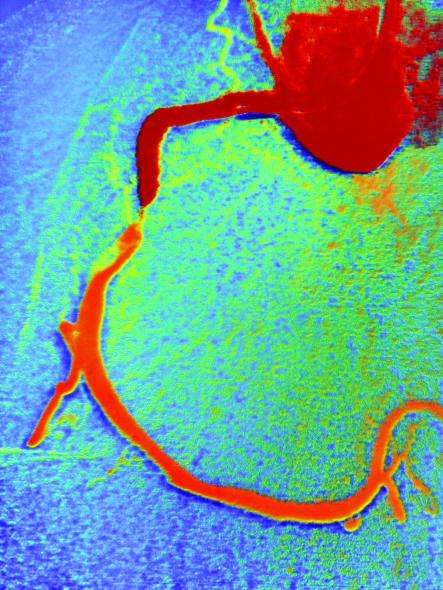
Figure 1.
Coloured angiogram showing blocked right coronary artery
Credit: SIMON FRASER/SPL
If primary angioplasty is used for the 100 patients, no patient is exempt and the diagnostic angiogram can usually identify the infarct related artery and assess the state of coronary perfusion. Treatment can then be given to those patients who have not reperfused spontaneously, and normal epicardial blood flow is likely to result in 90-97% of attempted angioplasties.5 With this approach, the therapeutic goal is achieved and documented in more than 90% of patients with no unnecessary risk.
More effective and efficient
Twenty three randomised trials have compared primary angioplasty with thrombolysis. A meta-analysis of these trials concludes that primary angioplasty has a highly significant benefit over thrombolysis for mortality, non-fatal reinfarction, and haemorrhagic stroke.6 None of these 23 trials suggests a trend in favour of thrombolysis, although only one trial individually shows a mortality benefit in favour of primary angioplasty.7 A similar meta-analysis of trials of thrombolysis versus control8 showed only an 18% risk reduction in mortality and, somewhat perversely, an increase risk of death in the first 24 hours.
The current strategy for management with thrombolytic drugs relies on electrocardiography as the prime diagnostic tool. It is used initially to diagnose ST elevation myocardial infarction, and resolution of the ST changes is used as a surrogate for reperfusion. Patients then wait for 3-7 days for a non-invasive test such as an exercise test or a myocardial perfusion scan to identify those at high risk; high risk patients are then either kept in hospital for angiography with a view to revascularisation or referred to another hospital where this can take place. This occupies a considerable number of bed days. If a strategy of primary angioplasty were used the angiographic diagnosis and the definitive treatment would be completed within the time taken for a streptokinase infusion to run through. Further non-invasive tests would not be required, and in many cases the patient could be discharged within 72 hours.9
Goal oriented treatment
The management suggested in the National Service Framework for Coronary Heart Disease is procedurally oriented and not goal oriented.10 The procedure is the administration of a fibrinolytic drugs, and performance is audited through the myocardial infarction national audit project (MINAP) returns, which record the percentage of patients receiving the drug within certain time limits. No mention is made of the therapeutic goal. It seems more appropriate to have a goal oriented guideline such as “80% of patients presenting with ST elevation myocardial infarction should have normal coronary flow restored in the infarct related artery within 90 minutes of presentation.” Primary angioplasty fulfils this role admirably. Not only does diagnostic angiography ensure appropriate and better guided treatment, but the therapeutic goal is easily audited and patients can be informed more accurately of their diagnosis and prognosis.
Primary angioplasty is not widely available in the United Kingdom, but it could be. On site cardiac surgery is not a requirement, and primary angioplasty can be performed safely and effectively in a district general hospital.11 Many more cardiac catheter laboratories and interventional cardiologists with the appropriate skills would be needed. However, much could be achieved by reordering clinical priorities. Angioplasty is of greater benefit in patients with ST elevation myocardial infarction than in those with non-ST elevation myocardial infarction; such patients, in turn, receive greater benefit from angioplasty than those with chronic stable angina. It seems more appropriate to apply the relatively limited resources where the benefit is greatest pending the development of more facilities.—David Smith
Contributors and sources: DS has been interested in primary angioplasty since 1987 and has pressed for the development of the service since 1995. In 1996, with John Dean, he performed a three month pilot of a 24 hour, 7 day a week primary angioplasty service in Exeter.
Competing interests: None declared.
References
- 1.Fath-Ordoubadi F, Huehns T, Al-Mohammad A, Beatt KJ. Significance of the thrombolysis in myocardial infarction scoring system in assessing infarct-related artery reperfusion and mortality rates after acute myocardial infarction. Am Heart J 1997;134: 62-8. [DOI] [PubMed] [Google Scholar]
- 2.Gibson CM, Cannon CP, Murphy SA, Ryan KA, Mesley R, Marble SJ, et al. Relationship of TIMI myocardial perfusion grade to mortality after administration of thrombolytic drugs. Circulation 2000;101: 125-30. [DOI] [PubMed] [Google Scholar]
- 3.French JK, Hyde TA, Patel H, Amos DJ, McLaughlin SC, Webber BJ, et al. Survival 12 years after randomization to streptokinase: the influence of thrombolysis in myocardial infarction flow at three to four weeks. J Am Coll Cardiol 1999;34: 62-9. [DOI] [PubMed] [Google Scholar]
- 4.GUSTO Angiographic Investigators. The effects of tissue plasminogen activator, streptokinase, or both on coronary-artery patency, ventricular function and survival after acute myocardial infarction. N Engl J Med 1993;329: 1615-22. [DOI] [PubMed] [Google Scholar]
- 5.Grines CL, Browne KF, Marco J, Primary Angioplasty in Myocardial Infarction Study Group (PAMI). A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. N Engl J Med 1993;328: 673-9. [DOI] [PubMed] [Google Scholar]
- 6.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 2003;361: 13-20. [DOI] [PubMed] [Google Scholar]
- 7.Garcia E, Elizaga J, Perez-Castellano N, Serrano JA, Soriano J, Abeytua M, et al. Primary angioplasty versus systemic thrombolysis in anterior myocardial infarction. J Am Coll Cardiol 1999;33: 605-11. [DOI] [PubMed] [Google Scholar]
- 8.Fibrinolytic Therapy Trialists' (FTT) Collaborative Group. Indications for fibrinolytic therapy in suspected acute myocardial infarction: collaborative overview of early mortality and major morbidity results from all randomised trials of more than 1000 patients. Lancet 1994;343: 311-22. [PubMed] [Google Scholar]
- 9.Grines CL, Marsalese DL, Brodie B, Griffin J, Donohue B, Costantini CR, et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. J Am Coll Cardiol 1998;31: 967-72. [DOI] [PubMed] [Google Scholar]
- 10.Department of Health. National service framework for coronary heart disease. London: DoH, 2000. www.nelh.nhs.uk/nsf/chd/nsf/main/mainreport.htm (accessed 26 Apr 2004).
- 11.Smith LDR, Dean JW. Primary angioplasty in the district general hospital. Interim analysis of the Exeter primary angioplasty pilot study. Heart 1997;77(suppl 1): 46.9038694 [Google Scholar]