Abstract
Introduction
While overall survival for most common cancers in Australia is improving, the rural–urban differential has been widening, with significant excess deaths due to lung, colorectal, breast and prostate cancer in regional Australia. Internationally a major focus on understanding variations in cancer outcomes has been later presentation to healthcare and later diagnosis. Approaches to reducing time to diagnosis of symptomatic cancer include public symptom awareness campaigns and interventions in primary care to improve early cancer detection. This paper reports the protocol of a factorial cluster-randomised trial of community and general practice (GP) level interventions to reduce the time to diagnosis of cancer in rural Western Australia (WA).
Methods and analysis
The community intervention is a symptom awareness campaign tailored for rural Australians delivered through a community engagement model. The GP intervention includes a resource card with symptom risk assessment charts and local referral pathways implemented through multiple academic detailing visits and case studies. Participants are eligible if recently diagnosed with breast, colorectal, lung or prostate cancer who reside in specific regions of rural WA with a planned sample size of 1350. The primary outcome is the Total Diagnostic Interval, defined as the duration from first symptom (or date of cancer screening test) to cancer diagnosis. Secondary outcomes include cancer stage, healthcare utilisation, disease-free status, survival at 2 and 5 years and cost-effectiveness.
Ethics and dissemination
Ethics approval has been granted by the University of Western Australia and from all relevant hospital recruitment sites in WA.
Results
Results of this trial will be reported in peer-reviewed publications and in conference presentations.
Trial registration number
Australian New Zealand Clinical Trials Registry (ANZCTR). ACTRN12610000872033.
Keywords: MEDICAL EDUCATION & TRAINING, PRIMARY CARE, PUBLIC HEALTH
Strengths and limitations of this study.
This is the first large scale randomised controlled trial to test the implementation of cancer risk tools based on the Hamilton CAPER studies. It is also novel in that it will measure the effect of separate and combined community and general practice interventions on time to cancer diagnosis.
Longer term follow-up will assess the impact on survival.
The community control area was matched as closely as possible within the constraints of the population distribution in different regions of Western Australia.
Background
Rural Australians are more likely to die within 5 years of a cancer diagnosis than people from metropolitan areas.1 While overall survival for most common cancers in Australia is improving, the rural–urban differential has been widening, with significant excess deaths due to lung, colorectal, breast and prostate cancer in regional Australia.2 Similar disparities in cancer outcomes across certain patient groups have been described worldwide.3 As part of the International Cancer Benchmarking Partnership, a major focus on understanding variations in cancer outcomes has been later presentation to healthcare and later diagnosis.4
Previous studies have shown that patients living in rural Australia are less likely to receive curative or reconstructive surgery, radiotherapy or anticancer drug treatment.5–8 Policy initiatives have focused, therefore, on reducing disparities in access to treatment.9 Access to treatment is an important determinant of outcome, but later presentation and stage at diagnosis have also been observed in rural patients with cancer.10 11 International research suggests that the time taken to appraise symptoms and seek help (so-called ‘patient delay’) and management in primary care are also key determinants of cancer outcomes.12 Time to diagnosis is associated with poorer survival for several common cancers.13 14
One of the approaches to reducing later presentation to healthcare has been community symptom awareness campaigns. These have formed a major component of the UK National Awareness and Early Diagnosis Initiative (NAEDI) as part of the policy to improve cancer outcomes.15 A systematic review of cancer symptom awareness campaigns published in 2009 found insufficient evidence about their effect on presentation to healthcare.16 Since then further studies have begun to show potential effects on presentation and cancer diagnoses.17
A second approach has aimed at improving early recognition of patients in primary care with symptoms suggestive of cancer. A major challenge for general practitioners (GPs) is that the symptoms of many cancers are common in the community and overlap with prevalent benign conditions. GPs need to assess the risk, or diagnostic probability, of an underlying cancer and determine whether further investigation is justified. Until recently, there was little epidemiological evidence demonstrating how well symptoms predict risk of an underlying cancer from primary care populations.18 Analysis of data in case–control studies using large UK general practice databases, notably the CAPER (Cancer Prediction in Exeter) studies19–22 and QCancer research,23 24 has led to significant advances in our understanding of the epidemiology of cancer symptoms in primary care.
The CAPER studies have quantified the risk of individual and paired symptoms, signs and primary care investigations for a number of cancers including colorectal, lung and prostate. These have been evaluated as risk assessment tools (RATs) in paper versions25 and are currently undergoing evaluation as computerised decision support tools embedded in the electronic medical records of English general practices.26 Various interventions including audit and feedback, educational visits, guidelines and decision support have been tested in general practice to improve cancer diagnosis.27 None of the 22 trials included in a systematic review of interventions to support cancer diagnosis in primary care examined effects on diagnostic delay, although audit and feedback was shown to improve clinical management.28
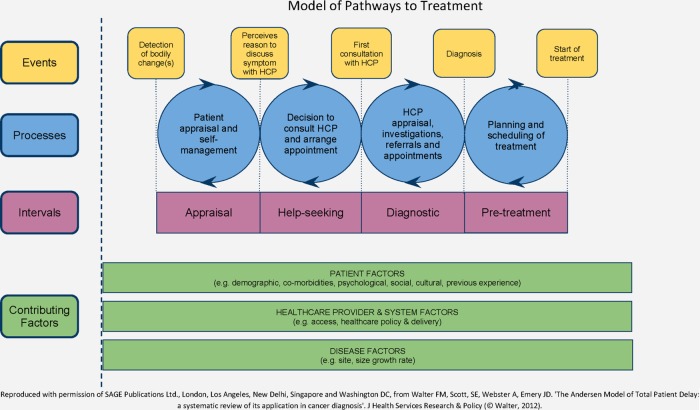
Conducting research in the field of ‘diagnostic delay’ in cancer has many methodological challenges. The Aarhus statement discusses these and provides consensus guidelines on appropriate definitions and the conduct and reporting of such research.29 One recommendation is the application of theoretical models such as The Model of Pathways to Treatment30 31 (figure 1). This model proposes four key intervals:
The Appraisal Interval: The nature of a person's symptoms is one of the most important factors determining the duration of the Appraisal Interval. Misattribution of symptoms either to a previous benign or concurrent condition or non-recognition of the seriousness of symptoms contribute to longer Appraisal Intervals.
The Help-Seeking Interval: Various factors may contribute to this interval including patient factors such as competing events (eg, holidays), and emotional ones such as fear. This includes fear of the consultation and examination, or of the diagnosis and treatment. Access to primary care and sanctioning help-seeking by family or friends, so that patients do not perceive themselves as wasting the doctor's time, are also important factors.32
The Diagnostic Interval: Depending on the healthcare setting this may involve a series of healthcare visits, referrals and investigations and often represents a complex process. System factors including the role of primary care as a gatekeeper and access to investigations and specialist care are key factors determining this interval.
The Pre-Treatment Interval: The time from formal cancer diagnosis to initiation of treatment is also strongly influenced by several healthcare system factors such as access to staging investigations and specialised treatments.
Figure 1.
Model of pathways to treatment.
Our research on rural cancer outcomes is applying the well-established Medical Research Council (MRC) methodological framework for the design and evaluation of complex interventions.33 34 Our initial exploratory mixed-methods study aimed to explore the context of rural cancer diagnosis in WA and inform the development of our complex intervention. In summary, in-depth interviews with 66 people recently diagnosed with breast, lung, prostate or colorectal cancer from regional WA found longer duration of symptom appraisal for colorectal cancer compared with other cancers. Participants defined core characteristics of rural Australians as optimism, stoicism and machismo. These features, as well as poorer access to healthcare, contributed to later presentation of cancer.18 In addition, there were significant overall differences between cancers in terms of time from presentation in general practice to referral, from GP referral to specialist appointment, and from specialist appointment to cancer diagnosis. These differences were due to the nature of presenting symptoms, access to diagnostic tests and multiple visits to specialists. Breast cancer was diagnosed more quickly because its symptoms are more specific and well recognised by the community, and due to better access to diagnostic tests and specialist one-stop clinics.35
These findings contributed to the development of the interventions and design of the Improving Rural Cancer Outcomes (IRCO) Trial: a factorial cluster-randomised controlled trial of community-based and general practice-based interventions which aims to reduce the time to diagnosis in rural patients presenting with prostate, breast, colorectal or lung cancer in Western Australia.
Methods and trial design
Design and setting
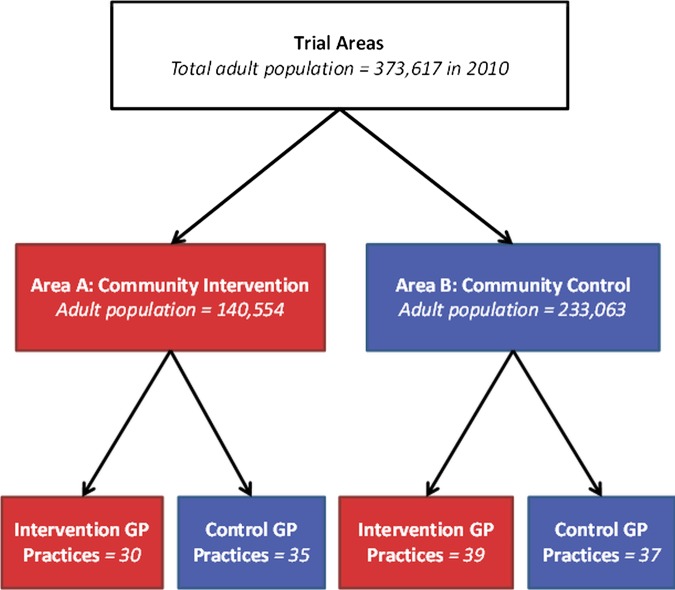
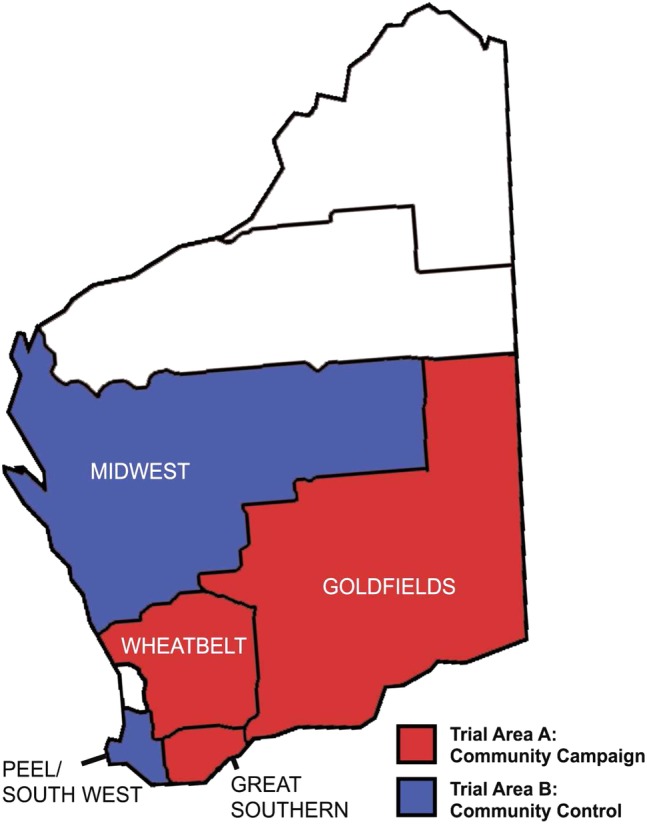
This 2×2 factorial cluster randomised controlled trial is set in Western Australia, the largest Australian state geographically, with a population of 2.29 million (approximately 10% of the Australian population). Two-thirds of the WA population live in metropolitan Perth and the remainder are widely geographically dispersed. Two Trial Areas were matched for population size, demographics including age and Aboriginality, and similar cancer incidence, based on the most recent available data (from 2006) when the trial was planned (figure 2 presents more recent data on population size from 2010). Trial Area A comprises the Wheatbelt (155 256km²), Goldfields (770 488 km²) and Great Southern (39 007 km²) regions, and Trial Area B includes the Peel/South West (29 646 km²) and MidWest (470 000 km²) regions.36
Figure 2.
Map of Western Australia depicting the regional boundaries of Trial Area A, receiving the community intervention, and Trial Area B, acting as the community control.
Randomisation
Trial Area A has been allocated to receive the community symptom awareness campaign intervention and Trial Area B acts as the community campaign control region. In both Trial Areas general practices have been randomised to receive the education intervention or control, stratified by practice size (≤1 GP; 2 to 4 GPs; 5+ GPs). GPs who worked at more than one practice have been identified, and their practices have been treated as one practice for the purpose of randomisation to avoid contamination (figure 3).
Figure 3.
The 2×2 factorial cluster randomised controlled trial design.37
Practices have been randomly assigned to intervention or control arm using a cluster version of Zelen's method of postrandomised consent: intervention practices have been invited to receive the educational package while control practices receive no information about the trial.37 This enables non-intervention practices to act as true controls by minimising the Hawthorne effect in a situation where placebo and double blind experimental conditions are impossible to achieve. The Hawthorne effect occurs when the researchers’ procedures and communications act as interventions in themselves that change behaviours, such as if the control cluster were to adopt the practices or policies promoted to the intervention cluster. This would destroy the trial's ability to identify a benefit of the intervention, if one exists. Furthermore, it allows a pragmatic delivery of the intervention and measure of its uptake in routine practice. Intervention practices which decline the invitation to receive the educational package will be analysed on an intention-to-treat basis. Randomisation has been performed by the trial statistician. As the number of working GPs in a given practice varies, the randomisation has taken into account practice size. Each practice has been categorised into: one GP in the practice, 2–4 GPs or five or more GPs. A random sample proportional to the size of the practice has been used employing ‘samplepps’ macro in Stata.
Patient recruitment and inclusion criteria
From 1 March 2012, 4 months after the interventions started, all patients meeting the following criteria are being invited to contribute their data for the trial:
Adults aged over 18 years;
Diagnosed with breast, lung, colorectal or prostate cancer between 1 January 2012 and the recruitment end date of 31 March 2014; and
Resident of Trial Areas A or B at the time of diagnosis.
Recruitment strategy
Eligible participants are identified via:
The WA Cancer Registry (WACR): A letter and participant information sheet is mailed from the WACR directly to newly diagnosed patients with cancer. After 3 weeks non responders are followed up by the research team via phone or mail.
Cancer Council Western Australia's (CCWA) residential lodges: We approach eligible patients while staying at CCWA charitable accommodation during their cancer treatment in Perth. A large proportion of rural patients with cancer, especially those receiving radiotherapy or chemotherapy, reside in one of the lodges for several weeks during their treatment. Eligible patients receive the same participant information sheet as part of their Lodge Welcome Pack by the lodge receptionists and are followed up by the research team.
Participants are invited to sign a consent form, which includes agreement to access their medical records, and return it with their completed SYMPTOM questionnaire.
Study interventions
The Trial includes interventions at two levels: a community symptom awareness campaign (‘the community intervention’); and a GP educational package incorporating symptom risk assessment charts and referral guidance which is implemented through multiple academic detailing visits and case studies (‘the GP intervention’). Both interventions are being delivered between 1 November 2011 and 31 December 2013.
The community intervention
We modified existing resources developed for The Cancer Research UK ‘Spot Cancer Early’ and the UK National Health Service ‘3 week cough’ campaigns to incorporate the findings of our exploratory mixed-methods study,18 35 and to make them relevant to a rural Australian community.
Materials have been further modified following three community forums held in the major towns of the campaign target regions. Feedback was obtained about the campaign logo, design, choice of images, locally acceptable language, and contact details. The campaign is named the Find Cancer Early campaign and the materials explicitly use the Cancer Council WA branding, recognising the strong community support and credibility of this organisation. Community members wanted the campaign to focus on the positives associated with early detection and the use of simple, non-medical terms when describing symptoms. A campaign message development meeting was then held between the project team, social marketing experts and health professionals to develop a framework for the campaign and message hierarchy.
The target of the campaign is men and women over the age of 40; it aims to raise awareness of the symptoms of bowel, lung, prostate and breast cancer and to help people overcome the barriers to seeking medical help. The primary campaign item is a plain-language symptom checklist (figure 4). Other materials include: newspaper adverts based on campaign materials; radio adverts for each of the four cancers; tumour-specific postcards featuring regional images and quotations about relevant symptoms (figure 4); generic postcards providing strategies to overcome barriers to seeking help (figure 4); a DVD outlining tumour specific symptoms featuring health professionals and regional community members; an Indigenous version of the symptom checklist; a website; and posters and banners.
Figure 4.
Examples of Find Cancer Early resources—General Symptom Checklist, Prostate postcard and Tell your doctor postcard.
Five project officers, with a combined full time equivalent of 3, are delivering the campaign across the three regions of WA in Trial Area A. They use a community engagement approach building partnerships to deliver and disseminate the campaign messages with presentations, displays and campaign resource distribution. Paid advertising and articles in regional newspapers and radio supplement this dissemination strategy. Television is not being used to avoid contamination in the control area.
The GP intervention
A GP education resource card, ‘The Rural Cancer Initiative: a Guide for General Practitioners’, has been developed with input from rural GPs and health professional advisors. The novel aspect of this intervention is the implementation of the CAPER risk assessment charts for colorectal,21 lung20 and prostate22 cancer. The resource card contains the clinical implications of these risk charts including diagnostic assessment. In addition the resource card summarises the National Breast and Ovarian Cancer Centre guidelines for investigating new breast symptoms38 and local referral guidelines and hospital contacts, including recommendations about access to cancer multidisciplinary teams.39
The GP resource card is being implemented through a series of four academic detailing practice visits, supplemented by a series of question-and-answer case studies for completion between visits designed to reinforce key messages.40 The practice visits present specific components of the resource card and facilitate discussion within the practice around recently diagnosed patients with cancer. GPs are eligible for Royal Australian College of General Practitioners and Australian College of Rural and Remote Medicine professional development points on completion of the case studies and attendance at practice visits.
Outcomes and measures
Primary outcome
The primary outcome is the Total Diagnostic Interval (TDI), defined as the time from first symptom to diagnosis. We will report our time intervals according to the principles outlined in the ‘Aarhus Statement’ on the conduct and reporting of research on cancer diagnosis,29 and will use the Model of Pathways to Treatment as our theoretical framework.30,31 The date of first symptom is defined as ‘the time-point when first bodily change(s) and/or symptom(s) is noticed’. For screen-detected cases we use the date of attendance for the screening test as the initial date in the patient pathway. Date of diagnosis is based on pathological diagnosis as reported to the WA Cancer Registry. We will divide the Total Diagnostic Interval further to include time from first presentation in general practice to referral (GP Interval), date of referral to first attendance at specialist (Specialist Access Interval), and time from first attendance at the specialist to date of diagnosis (Specialist Interval).41 The GP Interval includes the time taken to order and respond to investigations available directly in primary care. For patient-reported dates we will apply published mid-point rules to estimate the actual date where uncertainty exists.12 Where necessary, a clinical consensus group will review the data to confirm the date of first symptom and first presentation to healthcare.
Measurement tools
The following instruments will be used to obtain information about symptoms and key dates to calculate the Total Diagnostic Interval:
SYMPTOM Questionnaire: This self-administered questionnaire was developed from the C-SIM42 measure and has been applied in the UK SYMPTOM study.43 It includes items specific to each tumour site to capture details of symptoms, their date of onset and time taken to seek help.
GP record audit tool: This tumour-specific proforma is mailed to the participant's GP to obtain key information on: the date, type and duration of presenting symptoms within the last 12 months, referral information including referral date, and date of first appointment with specialist.
Date of cancer diagnosis is obtained from the WA Cancer Registry.
Secondary outcomes
Process measures of intervention delivery
Campaign Dose: Process evaluation is conducted in each intervention town to collect data on the amount of media exposure achieved, number of campaign resources distributed, number of partnerships established, and number of presentations, events and other activities carried out by campaign staff to promote the campaign messages. Information is collected via monthly reports by the campaign project officers.
Media Exposure: Media exposure is measured by number and square centimetre coverage of paid press advertisements and unpaid press articles. The value of unpaid media is estimated by calculating the square centimetre space and calculating the cost to purchase that space.
GP Monitoring: The campaign project officers document number of visits conducted, GP attendance at each visit, and number of case studies completed.
Costs of intervention delivery: Cost data of delivering the interventions are being collected prospectively (see Health Economic Evaluation below).
Impact measures of intervention
Campaign awareness is being measured at 18 months into the campaign intervention by a computer-assisted telephone interview survey. The survey is being conducted on a random sample of adults above 40 years old from the campaign regions and control regions stratified by sex and age, and regions within Trial Area A. Questions measure exposure to the campaign, including unprompted and prompted awareness of campaign elements (ie, radio, print and campaign brand and logos). Respondents reporting any exposure to the campaign are asked additional questions about comprehension and perceived effectiveness.
Measures of clinical outcomes
We will use the WA data sets44 to provide linked hospital morbidity and administrative, cancer diagnostic and mortality data in order to examine trends across time on clinical outcomes at the level of the community and individual. We will obtain these data in three tranches:
Cohort of patients diagnosed in 2002–2010 to provide a baseline understanding of the patterns of care and survival;
Cohort of patients diagnosed in 2011–2013 with all linked data after at least 2 years of follow-up to evaluate short-term clinical effects of the interventions on cancer stage, healthcare utilisation and disease free status;
Cohort of patients diagnosed in 2011–2013 with all linked data after at least 5 years of follow-up to evaluate medium-term clinical effects and survival.
Analysis
The cluster randomised design provides protection against contamination across trial groups when trial patients are managed within the same setting.45 The primary analysis will compare the Total Diagnostic Intervals and its subcomponents between trial groups. Simple analyses such as t tests or more complex regression analyses will be undertaken. Time data are invariably skewed and bounded by the absence of negative times. We will apply a log transformation prior to conducting general linear modelling to compare intervals accounting for exposure to the community and GP interventions within the model, accounting for clustering effects at the practice level. Where appropriate, comparisons of arithmetic or geometric means will be performed. The aim of statistical modelling is to identify the main factors that explain variation in the outcome for example, patient and practice characteristics. The primary aim is to adjust for the effect of covariates before the effect of the intervention is tested as well as ‘intervention × phase’ interaction with premeasurements and postmeasurements comparison. We will conduct a series of sensitivity analyses to account for:
Symptoms reported with a duration of greater than 2 years which will be excluded from the primary analysis.
Vague first symptoms such as fatigue and ‘feeling different’.
Using cancer registry, hospital morbidity and death data we will compare patterns of hospitalisation and treatment, pseudostaging at diagnosis using established methods where full staging data are not available,44 46–49 disease-free intervals and survival in people diagnosed with breast, lung, colorectal or prostate cancer resident in Trial Area A with those in Area B and those resident elsewhere in non-metropolitan and metropolitan WA. The comparisons will relate to patients diagnosed with one of the four target cancers in the 6 years prior to the interventions (2005–2010) and during the 2 years of intervention (late 2011—late 2013). This will enable the effects of the community-level intervention to be evaluated as a spatial contrast. The same analyses will be conducted after 5 years of follow-up. These analyses will entail all patients with cancer in WA during the specific time periods to assess the effects of the community intervention. In addition, we will conduct analyses of all participants who have given their consent to measure the effects of exposure to the GP intervention and combined effect of community and GP interventions on clinical outcomes at 2 and 5 years.
All analyses will be conducted by trial statisticians blinded to participant allocation.
Health economic evaluation
A health economic evaluation from a health system perspective will be undertaken to determine whether the resources committed to the trial between the four intervention arms represent a worthwhile investment in terms of the measured outcomes. This will include a cost-analysis of each intervention and a cost-effectiveness analysis which will compare costs with related outcomes. Cost components include: campaign intervention costs (eg, staffing, travel, campaign resources, media, events, in-kind support); GP intervention costs (eg, staffing, travel, education programme, resources); additional staff costs; non-intended costs of non-cancer diagnoses (hospital utilisation); in-kind personnel contributions from project partners. Resource units and cost per unit will be applied to calculate total cost.
Outcome data will be matched to cost data. In the first instance, cost per change in TDI will be calculated for each of the four arms of the trial. Longer term cost-effectiveness will also be calculated to estimate net cost per life year gained for each intervention. The TDI will provide a surrogate outcome for longer term outcomes using modelling techniques. Once longer term follow-up data are available, cost-effectiveness ratios will be calculated.
Sample size
The original sample size required for 80% power and α=0.05 to detect a halving of long-delay risk of 30% to 15% was 840 participants. This sample size calculation accounted for the design effects from hierarchical correlations and an intra-class correlation coefficient of 0.09 based on similar trial designs.50
Recruitment was planned to continue until 4 months after completion of intervention delivery to allow inclusion of a cohort of newly diagnosed patients with cancer who were exposed to the interventions (ie, 31 March 2014). We have achieved approximately a 50% accrual rate into the trial which was much higher than our original estimates. Our final estimated recruitment is 1359 participants. Based on the distributions of TDIs from our previous research, 18 35 this sample will provide 80% power to detect a 10% difference in TDI between intervention groups for all four cancers combined, and a 20% difference in TDI for breast, colorectal and prostate cancer separately, but not lung cancer as this would require a sample of 2600 participants.
Supplementary Material
Acknowledgments
The authors thank the following for their contributions to this trial: Find Cancer Early Project Officers (Lisa Barr, Pam Foulkes-Taylor, Libby Foster, Karen Hansen, Amanda Harding, Kerryn Keating, Tracey Price, Jo Woodall), Cancer Council WA staff and associated staff, Cancer Council WA Lodges, participants, GPs and Hospital specialists, Cancer Research UK, AH Crawford Treatment Society, Department of Health WA, WA Cancer and Palliative Care Network, WA Country Health Service, National Health and Medical Research Council, Cancer and Palliative Care Research and Evaluation Unit, Val Lishman Health Research Foundation, WA Cancer Registry Staff, WA Data Linkage Branch, Pat Booth, Rhonda Coleman, Hooi Ee, Dickon Hayne, Laura Keith, Andrew Kirke, Mike Mears, Leanne Monterosso, Violet Platt, Iain Steve Pratt, David Preen, Babu Simon, Craig Sinclair, Hayley Staples, Simon Towler, Clare Willix. Protocol V.3. 27 June 2014.
Footnotes
Contributors: JDE, CDJH, CS, KA, AKN, FMW and MB conceptualised and designed the study. All authors assisted with the development of the protocol, study design and refinement of study materials. All authors will contribute to implementation of the protocol and acquisition of data. JDE, VG and CDJH led the writing of the protocol. All authors have been involved in drafting and critical evaluation of the manuscript. All authors have read and approved the final version.
Funding: The project is funded by a National Health Medical Research Council (NHMRC) Partnership Grant (Grant ID 572765) and the AH Crawford Society. The project is a partnership with Cancer Council Western Australia, the WA Cancer and Palliative Care Network, and the Department of Health Western Australia. The funding source has no role in the design of this study, the interpretation of data or decision to submit results.
Dissemination: This is the first randomised controlled trial to test the individual and combined effects of a community awareness campaign and GP intervention on time to cancer diagnosis. We plan to publish the main trial outcomes in a single paper and anticipate publishing additional papers exploring the data in more detail and relating to the implementation of this complex intervention. We will present the findings at national and international conferences from late 2014.
Competing interests: None.
Ethics approval: The trial obtained primary ethics approval from The University of Western Australia's Human Research Ethics Committee (HREC) (RA/4/1/4527). Additional approval was gained through the Department of Health of Western Australia's ethics committee, as well as reciprocal approvals with relevant metropolitan and regional hospitals. There is no formal Data Monitoring Committee for this trial as it was felt unnecessary for this type of intervention. Data management procedures are reported in the HREC submission.
Provenance and peer review: Not commissioned; peer reviewed for ethical and funding approval prior to submission.
References
- 1.Underhill CR, Goldstein D, Grogan PB. Inequity in rural cancer survival in Australia is not an insurmountable problem. Med J Aust 2006;185:479–80 [DOI] [PubMed] [Google Scholar]
- 2.Cancer in Australia 2010: an overview. Canberra: Australian Institute of Health and Welfare, 2010 [Google Scholar]
- 3.Coleman MP, Forman D, Bryant H, et al. Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet 2011;377:127–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler J, Foot C, Bomb M, et al. The International Cancer Benchmarking Partnership: an international collaboration to inform cancer policy in Australia, Canada, Denmark, Norway, Sweden and the United Kingdom. Health Policy 2013;112:148–55 [DOI] [PubMed] [Google Scholar]
- 5.Hall SE, Holman CD, Wisniewski ZS, et al. Prostate cancer: socio-economic, geographical and private-health insurance effects on care and survival. BJU Int 2005;95:51–8 [DOI] [PubMed] [Google Scholar]
- 6.Baade PD, Youlden DR, Coory MD, et al. Urban-rural differences in prostate cancer outcomes in Australia: what has changed? Med J Aust 2011;194:293–6 [DOI] [PubMed] [Google Scholar]
- 7.Coory MD, Baade PD. Urban-rural differences in prostate cancer mortality, radical prostatectomy and prostate-specific antigen testing in Australia. Med J Aust 2005;182:112–15 [DOI] [PubMed] [Google Scholar]
- 8.Mitchell KJ, Fritschi L, Reid A, et al. Rural-urban differences in the presentation, management and survival of breast cancer in Western Australia. Breast 2006;15:769–76 [DOI] [PubMed] [Google Scholar]
- 9.Delivering Regional Cancer Centres. Department of Health and Ageing, 2010 [Google Scholar]
- 10.Jong KE, Vale PJ, Armstrong BK. Rural inequalities in cancer care and outcome. Med J Aust 2005;182:13–14 [DOI] [PubMed] [Google Scholar]
- 11.Baade PD, Dasgupta P, Aitken J, et al. Geographic remoteness and risk of advanced colorectal cancer at diagnosis in Queensland: a multilevel study. Br J Cancer 2011;105:1039–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer 2005;92:1959–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richards MA, Westcombe AM, Love SB, et al. Influence of delay on survival in patients with breast cancer: a systematic review. Lancet 1999;353:1119–26 [DOI] [PubMed] [Google Scholar]
- 14.Torring ML, Frydenberg M, Hansen RP, et al. Time to diagnosis and mortality in colorectal cancer: a cohort study in primary care. Br J Cancer 2011;104:934–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cancer Research UK. About the national awareness and early diagnosis initiative UK. Cancer Research UK, 2010. [cited 2014]. [Google Scholar]
- 16.Austoker J, Bankhead C, Forbes LJ, et al. Interventions to promote cancer awareness and early presentation: systematic review. Br J Cancer 2009;101(Suppl 2):S31–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Athey VL, Suckling RJ, Tod AM, et al. Early diagnosis of lung cancer: evaluation of a community-based social marketing intervention. Thorax 2012;67:412–17 [DOI] [PubMed] [Google Scholar]
- 18.Emery JD, Walter FM, Gray V, et al. Diagnosing cancer in the bush: a mixed-methods study of symptom appraisal and help-seeking behaviour in people with cancer from rural Western Australia. Fam Pract 2013;30:294–301 [DOI] [PubMed] [Google Scholar]
- 19.Hamilton W. The CAPER studies: five case-control studies aimed at identifying and quantifying the risk of cancer in symptomatic primary care patients. Br J Cancer 2009;101(S2):S80–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamilton W, Peters TJ, Round A, et al. What are the clinical features of lung cancer before the diagnosis is made? A population based case-control study. Thorax 2005;60:1059–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton W, Round A, Sharp D, et al. Clinical features of colorectal cancer before diagnosis: a population-based case-control study. Br J Cancer 2005;93:399–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamilton W, Sharp DJ, Peters TJ, et al. Clinical features of prostate cancer before diagnosis: a population-based, case-control study. Br J Gen Pract 2006;56:756–62 [PMC free article] [PubMed] [Google Scholar]
- 23.Hippisley-Cox J, Coupland C. Symptoms and risk factors to identify women with suspected cancer in primary care: derivation and validation of an algorithm. Br J Gen Pract 2013;63:e11–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hippisley-Cox J, Coupland C. Symptoms and risk factors to identify men with suspected cancer in primary care: derivation and validation of an algorithm. Br J Gen Pract 2013;63:e1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khan NF. Implementation of a diagnostic tool for symptomatic colorectal cancer in primary care: a feasibility study. Prim Health Care Res Dev 2009;10:54–64 [Google Scholar]
- 26.Hamilton W, Green T, Martins T, et al. Evaluation of risk assessment tools for suspected cancer in general practice: a cohort study. Br J Gen Pract 2013;63:e30–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mansell G, Shapley M, Jordan JL, et al. Interventions to reduce primary care delay in cancer referral: a systematic review. Br J Gen Pract 2011;61:e821–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cockburn J, Pit S, Zorbas H, et al. Investigating breast symptoms in primary care: enhancing concordance with current best advice. Cancer Detect Prev 2001;25:407–13 [PubMed] [Google Scholar]
- 29.Weller D, Vedsted P, Rubin G, et al. The Aarhus statement: improving design and reporting of studies on early cancer diagnosis. Br J Cancer 2012;106:1262–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walter F, Webster A, Scott S, et al. The Andersen Model of Total Patient Delay: a systematic review of its application in cancer diagnosis. J Health Serv Res Policy 2012;17:110–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scott SE, Walter FM, Webster A, et al. The model of pathways to treatment: conceptualization and integration with existing theory. Br J Health Psychol 2013;18:45–65 [DOI] [PubMed] [Google Scholar]
- 32.Smith LK, Pope C, Botha JL. Patients’ help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet 2005;366:825–31 [DOI] [PubMed] [Google Scholar]
- 33.Campbell NC, Murray E, Darbyshire J, et al. Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Emery JD, Walter FM, Gray V, et al. Diagnosing cancer in the bush: a mixed methods study of GP and specialist diagnostic intervals in rural Western Australia. Fam Pract 2013;30:541–50 [DOI] [PubMed] [Google Scholar]
- 36.WA Country Health Service. Regional Profiles. http://www.wacountry.health.wa.gov.au/index.php?id=506 WA Country Health Service, 2011 [Google Scholar]
- 37.Adamson J, Cockayne S, Puffer S, et al. Review of randomised trials using the post-randomised consent (Zelen's) design. Contemp Clin Trials 2006;27:305–19 [DOI] [PubMed] [Google Scholar]
- 38.National Breast and Ovarian Cancer Centre. The investigation of a new breast symptom: a guide for general practitioners. Australia: National Breast and Ovarian Cancer Centre, 2006 [Google Scholar]
- 39.Department of Health WA. Model of care for cancer. Perth: WA Cancer and Palliative Care Network, 2008 [Google Scholar]
- 40.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 2004;8:iii–iv, 1–72 [DOI] [PubMed] [Google Scholar]
- 41.Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. Br J Cancer 2009;101(Suppl 2):S5–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neal RD, Nafees S, Pasterfield D, et al. Patient-reported measurement of time to diagnosis in cancer: development of the Cancer Symptom Interval Measure (C-SIM) and randomised controlled trial of method of delivery. BMC Health Serv Res 2014;14:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Discovery Programme. The Symptom Study. Discovery Programme, 2014. http://discovery-programme.org/symptom_study.php [Google Scholar]
- 44.Department of Health WA. Data linkage WA. Western Australia: Department of Health, 2014. http://www.datalinkage-wa.org.au/ [Google Scholar]
- 45.Campbell MK, Mollison J, Steen N, et al. Analysis of cluster randomized trials in primary care: a practical approach. Fam Pract 2000;17:192–6 [DOI] [PubMed] [Google Scholar]
- 46.Yuen E, Louis D, Cisbani L, et al. Using administrative data to identify and stage breast cancer cases: implications for assessingquality of care. Tunmori 2011;97:428–35 [DOI] [PubMed] [Google Scholar]
- 47.Cooper GS, Yuan Z, Stange KC, et al. The utility of Medicare claims data for measuring cancer stage. Med Care 1999;37:706–11 [DOI] [PubMed] [Google Scholar]
- 48.Thompson B, Lumley J, Coory M. Hospital morbidity data for determining spread of disease at diagnosis for colorectal cancer: a validation study. Asia Pac J Clin Oncol 2012;8:e17–22 [DOI] [PubMed] [Google Scholar]
- 49.Thompson B, Watson M, Bowman R, et al. Hospital-activity data inaccurate for determining spread-of-disease at diagnosis for non-small cell lung cancer. Aust N Z J Public Health 2012;36:212–17 [DOI] [PubMed] [Google Scholar]
- 50.Campbell MK, Thomson S, Ramsay CR, et al. Sample size calculator for cluster randomized trials. Comput Biol Med 2004;34:113–25 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.