Abstract
Background
Multi-channel surface functional electrical stimulation (FES) for walking has been used to improve voluntary walking and balance in individuals with spinal cord injury (SCI).
Objective
To investigate short- and long-term benefits of 16 weeks of thrice-weekly FES-assisted walking program, while ambulating on a body weight support treadmill and harness system, versus a non-FES exercise program, on improvements in gait and balance in individuals with chronic incomplete traumatic SCI, in a randomized controlled trial design.
Methods
Individuals with traumatic and chronic (≥18 months) motor incomplete SCI (level C2 to T12, American Spinal Cord Injury Association Impairment Scale C or D) were recruited from an outpatient SCI rehabilitation hospital, and randomized to FES-assisted walking therapy (intervention group) or aerobic and resistance training program (control group). Outcomes were assessed at baseline, and after 4, 6, and 12 months. Gait, balance, spasticity, and functional measures were collected.
Results
Spinal cord independence measure (SCIM) mobility sub-score improved over time in the intervention group compared with the control group (baseline/12 months: 17.27/21.33 vs. 19.09/17.36, respectively). On all other outcome measures the intervention and control groups had similar improvements. Irrespective of group allocation walking speed, endurance, and balance during ambulation all improved upon completion of therapy, and majority of participants retained these gains at long-term follow-ups.
Conclusions
Task-oriented training improves walking ability in individuals with incomplete SCI, even in the chronic stage. Further randomized controlled trials, involving a large number of participants are needed, to verify if FES-assisted treadmill training is superior to aerobic and strength training.
Keywords: Functional electrical stimulation, Therapy, Physiotherapy, Spinal cord injury, Chronic, Incomplete, Walking, Balance
Introduction
In Canada, there are currently about 86 000 individuals living with spinal cord injury (SCI), with approximately 3400 new cases occurring each year.1 Given the significant impact sustaining an SCI holds to both the individual and to society, there is a need for the development of technologies that can aid in restoring independence in daily living in individuals with SCI. Not surprisingly, the recovery of walking ability has been identified as a top priority by people with SCI in order to regain maximum independence.2
The rate and degree of recovery following SCI varies, but some clear patterns do emerge across impairment groups. According to the Guidelines for Conduct of Clinical Trials for SCI, developed by the International Campaign for Cures of Spinal Cord Injury Paralysis panel, individuals with American Spinal Cord Injury Association Impairment Scale (AIS) C and D have a greater potential to achieve a high level of functional recovery, including ambulation, compared to individuals with AIS A and B.3 Regardless of impairment, the largest amount of recovery occurs within the first 6 months following injury and the rate of recovery plateaus at 12 to 18 months post-injury.3,4. However, there is evidence5–8 for the effectiveness of different therapeutic modalities for improving gait in persons with chronic incomplete SCI beyond the 12–18-month mark. For instance, Body Weight Support Treadmill Training (BWSTT) has been shown in several studies to improve gait in this patient population.5 Harkema et al. found improvements in balance and walking speed in 196 individuals with incomplete SCI who were between 32 days to more than 25 years post-SCI.5 As such, there is a need to further explore which types of therapeutic modalities can be applied to maximize function post-SCI, even for those people who are many years post-injury.
Functional electrical stimulation (FES)-assisted walking has been found to be a promising method for improving walking function in individuals with SCI.6,7 FES uses short electrical pulses to generate muscle contractions. If the muscle contractions are properly timed and coordinated one can generate walking function in otherwise paralysed individuals such as patients with SCI. Although many FES systems have been developed to function as permanent orthoses (i.e. the user would have to wear the system all the time in order to walk8), recent advances in FES therapy have shown that individuals with incomplete SCI have the capacity to improve voluntary walking function following short-term intensive FES therapy.9–13 In other words, one can use FES therapy as a means to deliver restorative locomotion therapy to enhance spinal and supraspinal neuroplasticity, instead of using it as a pure compensatory walking aid as was done in the past.6,7 Although the majority of FES therapies for walking have been delivered to individuals with SCI who have drop foot,10–13 our team and others have demonstrated that multichannel FES systems (eight channels and more), which activate the lower limb muscles in the proper walking-like sequence, can be used in persons with chronic incomplete SCI who have much more profound walking impairment and not only a drop foot, to help them improve or restore voluntary walking function.8,9 Specifically, we have demonstrated in a pilot study that a multichannel FES system that produces coordinated muscle activations in the lower limbs, which mimics the natural gait cycle, has the capacity to enhance voluntary over ground walking in SCI population9,11. Therefore, the specific intent of this study was to apply a multichannel FES system in a larger chronic incomplete SCI patient population as a restorative locomotion therapy, and to examine its capacity to improve voluntary over ground walking in this patient population.
To the best of our knowledge, no Phase II randomized controlled trials have been carried out to-date to test the efficacy of a multichannel short-term FES intervention for improving walking in individuals with chronic incomplete SCI. Therefore, the purpose of this study was to investigate whether a thrice weekly FES-assisted walking program was better than a non-FES exercise program for improving gait and balance in individuals with chronic incomplete traumatic SCI.
Methods
Subject selection
The design was a parallel group randomized controlled trial (http://www.clinicaltrials.gov – NCT00201968) conducted at Lyndhurst Centre, Toronto Rehabilitation Institute, University Health Network. The study was approved by the Research Ethics Board of the Toronto Rehabilitation Institute, and we certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed. Recruitment for the study commenced in March 2005, and the last subject completed follow-up in December 2010. The inclusion criteria were individuals who sustained a traumatic incomplete spinal cord lesion between C2 and T12 that was motor incomplete (grade C or D on the AIS neurological impairment scale) and who were at least 18 months post-injury at the time of recruitment. Furthermore, participants were expected either not to walk at all at the baseline, or if they were walking independently that they had to use an assistive device to walk (e.g. a walker) or they had to have walking speed ≤0.5 m/s, which precluded them from being community walkers.14 Participants were excluded if they had any contraindications for FES, such as cardiac pacemakers, skin lesions or rash at potential electrode sites, or denervation of targeted muscles. Muscle denervation was confirmed when the muscle did not produce a single twitch or a contraction after it was exposed to high intensity electrical stimulation (e.g. pulse amplitude ≥ 60 mA, frequency = 40 Hz and pulse duration = 300 μs). Participants were also excluded if they had grade 4 pressure ulcers anywhere on the lower extremities, grade 2 or 3 pressure ulcers at locations where FES or the harness was applied, or if they suffered from any of the following cardiovascular conditions: (1) uncontrolled hypertension; (2) symptoms of orthostatic hypotension upon standing for 15 minutes; or (3) susceptibility to autonomic dysreflexia, requiring medication. Medical clearance was required from the participant's family physician prior to recruitment in the study.
Randomization
Upon completion of baseline assessments, participants were randomly assigned to the intervention or control group in a 1:1 allocation ratio. The randomization sequence was generated using randperm.m function in Matlab (TheMathWorks, USA). Envelopes were prepared by a research assistant not involved in enrolling participants; each envelope contained a unique reference number. Each participant selected an unmarked, sealed envelope from a box. This reference number corresponded to another sealed envelope in a separate location that pointed to group allocation for that participant.
Intervention and control group protocols
Due to the nature of the treatment, it was not possible to blind the subjects (i.e. no placebo group). The patient's physician was blind to group allocation unless a serious adverse event occurred. The control group and the intervention group received the same volume of therapy, which was 45 minutes per session, 3 days per week, for 16 weeks (48 sessions in total). A physically active control protocol was selected so that any intervention effects were attributed to the FES walking protocol rather than an improved fitness level. Adherence was determined by counting the number of sessions completed. Subjects who missed sessions were permitted to make them up.
Control group
Individuals assigned to the control group participated in an individually tailored exercise program consisting of 20–25 minutes of resistance training (using hand weights, cables, and Uppertone training system (GPK Inc., USA)) and 20–25 minutes of aerobic training (arm cycling, leg cycling, and walking in parallel bars or on treadmill), supervised by trained kinesiologists. Two to three sets of a resistance training exercise were performed at 12–15 repetition maximum resistance for all major muscle groups that were capable of voluntary activity. Both the resistance and repetitions were progressively increased according to tolerance. During the therapy we monitored participants' blood pressure and heart rate, and we ensured that the aerobic exercise was performed at a moderate pace (3–5 on the Modified Borg Rating of Perceived Exertion Scale). By doing this we ensured that the progression in training did not increase the participant's exertion rate over the course of therapy. The supervised control group activities ensured that any differences between groups in the outcome measures were attributed to the FES walking intervention and were not a result of an increased level of physical activity. The control group had an opportunity to exercise on the treadmill in case if they were able to walk unassisted.
Intervention group
Individuals assigned to the intervention group (FES group) received FES stimulation while ambulating on body weight support treadmill and harness system (Loko70, Woodway, USA). FES was delivered using two non-invasive, 4 channel electric stimulators Compex Motion (Compex SA, Switzerland) that uses surface self-adhesive stimulation electrodes.15 The electrodes were placed on the subject's skin corresponding to the muscles targeted with FES. Stimulus signals were balanced, biphasic, and pulse-width modulated with constant current regulation. Pulse amplitudes from 8 to 125 mA were used (subject and muscle dependent), and pulse-widths from 0 to 300 µs were used to modulate the stimulation intensity depending on the gait phase. Pulse frequency of 40 Hz was used. Note: pulse amplitudes were selected such that they would generate contractions required to produce desired functional movements. Because we used a current regulated stimulator, the stimulation intensities did not change frequently from one session to the next. However, as the patient involved in the therapy gained muscle strength, the pulse amplitudes used to generate desired movements were typically gently reduced with time. These adjustments were individualized and no general pattern was observed.
The key muscles targeted by the FES were bilateral quadriceps, hamstrings, dorsiflexors, and plantarflexors in a physiological sequence that they are activated during ambulation in able-bodied individuals.9 The stimulator provided open-loop stimulation sequences triggered by a pushbutton, which was pressed by two physiotherapists to initiate each step. In the early stages of therapy, each therapist controlled one leg, independently. Which means that when the leg needed to go into push-off phase of the gait, the therapist would press the pushbutton and the push-off phase and all subsequent phases of the gait would be performed automatically by the FES system (i.e., open-loop control strategy). As the participant progressed with the therapy he/she was allowed to control the gait using the two push buttons, each being pressed by one hand, where each hand controlled the corresponding ipsilateral leg.
Walking exercises were performed on a body-weight support treadmill Loko 70, specifically designed for BWSTT. This apparatus includes an overhead harness that attached to cables and pulleys such that a constant upward force could be applied to the subject while walking as well as for the subject's safety. Minimal amount of body-weight support was used to facilitate walking. This amount differed between participants and from session to session. Walking exercises were performed at a speed decided by the attending physiotherapist to realize subject's natural walking. When we say natural walk we want to suggest a progression in gait at a locomotion speed that the study participant could tolerate with ease, and during which lower and upper limb movements were properly coordinated and the limbs moved in a manner as close as possible to the one observed in able-bodied individuals. We took special care that the movements of the trunk were also within the envelope of what natural gait would look like. We actively prevented events in which the participant was having jerky movements and was bouncing from one side of the treadmill to the other. Naturally, the first therapy sessions were not the easiest in this regard, and frequently we needed up to three therapists to assist with the training. However, after the initial 3 to 5 training sessions the gait of the participant fully stabilized and the participant's gait sequence looked very similar to the natural gait.
As suggested earlier, the gait speed was adjusted to meet patients individual therapy needs. This was done by adjusting the temporal aspects of the FES protocol. The push-off phase of the gait is short and intensive, and for the most part it has similar temporal properties for the walking speeds that we use during the FES therapy. The main difference was in the force exerted during the push-off phase, which was regulated by adjusting stimulation intensity. What differed between patients was the duration of the swing phase. On the first day of therapy we would provide the patient with the “swing phase duration” that we thought was appropriate for the early phase of rehabilitation for that individual, based on their actual (if the patient was able to walk on his/her own) or targeted walking speed. After each session the therapist would indicate if we need to speed up or slow down the walking cycle, and by how much. If a change was required, a temporal aspect of the swing phase was adjusted in the protocol. With our FES system this was very easy to do and this change took less than 5 minutes to carry out. The change would allow for a shorter or longer swing phase, as advised by the therapist. During the next treatment session we would examine how the patent walked, and we would either adopt this newly adjusted protocol, or we would need to adjust it one more time until the proper gait speed was achieved. This process typically did not require more than two iterations. It very seldom happened that we needed to adjust the gait speed within a session. When this was required, the engineering team was ready and available to make that change fast.
During the therapy, when needed, manual assistance was applied to the participant's lower extremities and lower back to facilitate walking and ensure that movements were carried out in a physiological way. Within a session, 4–5-minute bouts of walking were repeated as many times as possible with resting intervals in between.
Outcome measures
The original purpose of this study was to examine how the FES-assisted walking program would enable the reduction of secondary health complications in chronic incomplete individuals with SCI. Therefore, the primary outcomes were to investigate the between group differences in outcomes related to secondary health complications such as (i) spasticity, (ii) muscle atrophy, (iii) bone loss, and (iv) to determine whether the hypothesized reduction in secondary health complications resulted in improvement in participants' satisfaction with life and societal participation. Hence, the sample size calculations for the study were determined taking into consideration only the primary outcome measures, as explained in the section “Statistical Analysis”. The findings regarding bone loss and satisfaction with life and societal participation are reported elsewhere.16,17 The current report outlines the effects of the intervention on subjects' function, gait, balance, and spasticity.
Outcome measures were performed at baseline, and 4 months (i.e. upon completion of the treatment sessions), 6 months, and 12 months post-baseline, unless otherwise stated. All measures were performed when the participants were not using the FES system. In other words, only function that the participant could generate voluntary was assessed. Data were collected by blinded assessors. The tests administered were:
Gait measures
-
1.
6-Minute walk test: Participants were asked to walk at a comfortable pace for as long as they could up to a maximum of 6 minutes using their preferred assistive device (e.g. 2-wheel walker and cane) but with no manual assistance.18,19 The distances walked at 2, 4, and 6 minutes were assessed.
-
2.
10-Meter walk test: The time for walking 10 meters was recorded to evaluate the participant's maximum walking speed.19 The participants walked at their fastest walking speed between two pre-defined lines that were drawn on the floor 10 meters apart. The participants were allowed to use any assistive device that they routinely used during ambulation; however, no manual assistance was provided during the test.
-
3.
An assistive device score (ADS): ADS was obtained using an ordinal rating based on the usage of upper extremity devices and lower extremity orthoses.19,20
-
4.
Walking mobility scale (WMS): In order to determine the extent to which participants were walking at home and in the community, they were rated using the subjective and self-reported WMS.21
Balance and mobility measure
-
1.
Timed up-and-go test (TUG): The TUG was a test used to assess patients' dynamic balance during a functional task. In the TUG, the subject began from a sitting position, walked a 3-meter distance, turned around, walked back, and then sat down. The participants were timed from the point when his/her back stopped being in contact with the backrest of the chair to the time when they completed the walk and sat back down and his/her back was again resting on the backrest of the chair.21
Functional measures
-
1.
Spinal cord independence measure (SCIM): The SCIM is a disability scale that has been specifically developed to evaluate the functional outcomes of patients with traumatic and non-traumatic SCI.22 The SCIM assesses function in the three core areas: (1) self-care, which includes feeding, bathing, dressing, and grooming, and is scored between a range of 0–20; (2) respiration and sphincter management are scored between a range of 0–40; and finally (3) mobility, also scored between a range of 0–40. The SCIM was assessed only at baseline and at 12 months after baseline.
-
2.
Functional independence measure (FIM) locomotor score: A FIM locomotor score was recorded to provide a measure of the amount of physical assistance and independence in walking based on a 7-point ordinal scale.23
Spasticity measures
-
1.
Modified Ashworth scale (MAS): MAS is the most commonly used subjective scale for clinical assessment of spasticity, and primarily measures movement-provoked spastic muscle resistance (increased muscle tone), which has been employed in a number of studies examining spasticity in various populations that include stroke patients, persons with traumatic brain injuries, multiple sclerosis, and SCI.24 The scale requires that the examiner move the patient's limb through its full range of movement and to rate the amount of resistance felt according to an ordinal 6-point scale (grades 0, 1, 1+, 2, 3, 4). Grade 0 represents a normal response. The muscles tested were hip adductors, knee flexors, knee extensors, ankle dorsiflexors, and plantar flexors.
-
2.
Pendulum test: The pendulum test is an objective quantitative biomechanical measurement in which the knee is released from full extension and the leg allowed to swing until motion ceases. The data are collected by an electrogoniometer.25 The goniogram pattern of the pendulum test reflects the oscillations of knee flexion and extension accompanying the drop. Three trials were executed.
Statistical analysis
The trial reporting was done in accordance with the CONSORT criteria, and subject flow through the study was depicted using a CONSORT flow diagram (Fig. 1) (http://www.consortstatement.org/). Mean and standard deviation (SD) and count, percent were used to summarize participant characteristics and study outcome measures. Note: the original objective of this study was to examine how the FES-assisted walking program could be used to help reduce secondary health complications in chronic incomplete individuals with SCI. Consequently the primary outcomes in this study were between group differences in assessments related to secondary health complications such as: i) spasticity; ii) muscle atrophy; iii) bone loss; and iv) to determine if the hypothesized reduction in secondary health complications resulted in improvement in participants' satisfaction with life and societal participation. Therefore, for the purpose of this study the sample size was determined using the outcome that was expected to demonstrate the smallest effect size for the registered trial, namely tibia cortical bone mineral density (BMD; not reported here). In a report on FES-assisted cycling, Eser et al.26 reported a standard deviation of 0.03–0.06 g/cm3 for the tibial cortical BMD in participants with SCI (determined by computed tomographic scan). These values translated to relative changes of 0.6–0.8% per month. We considered 0.6% per month a clinically significant difference in BMD change. Therefore, n = 13 for a significance level of 5%. Assuming a 20% drop out rate, a total of 17 participants per group was the targeted recruitment number, i.e. 34 individuals in total.
Figure 1 .
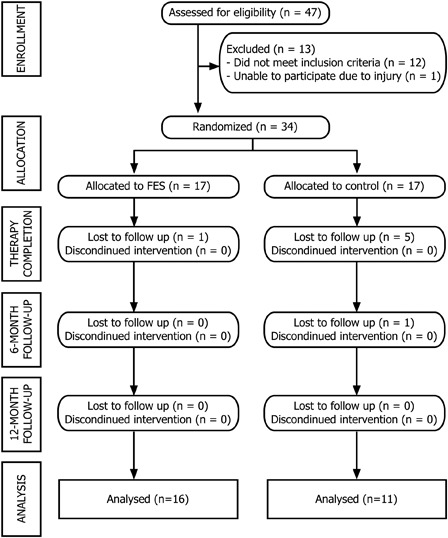
Consort diagram.
The comparison between the groups (control group and intervention group) and among time course (baseline, 4-, 6-, and 12-month) were performed using two-way repeated measures analysis of variance for each outcome measure (SPSS, IBM, USA). The comparisons were performed with the participants who completed all assessments in the study (see Consort diagram in Fig. 1 for details). A Bonferroni post hoc test was carried out where applicable. An α of 0.05 (two-tailed) was used for all tests unless indicated otherwise. The data are presented as mean (standard deviation) in the following sections and the tables.
Results
Thirty-four individuals with motor incomplete, traumatic, and chronic SCI, who passed the screening assessment and provided informed consent, were recruited in the study (Fig. 1). Upon completion of the study, we had 27 subjects who completed the training and attended all follow-up assessments and were included in analyses. Of the seven individuals that dropped out of the study, two dropouts were secondary to medical issues not related to the study, one was lost to follow-up secondary to leaving the country, one dropped out because of randomization to control group, and three participants dropped out for unknown reasons. Of the 27 participants who completed the study, 16 were in the intervention group (FES group) and 11 in the control group (conventional exercise group). Details of the participant demographics are listed in Table 1. On average participants in the study received 44.1 sessions during the training period (in the intervention group the average number of sessions was 43.5 and in the control group the average number of sessions was 44.5). Study-related adverse events have been reported previously.16
Table 1 .
Participant demographics, mean and standard deviations*
| Variable | Treatment | Control | Total |
|---|---|---|---|
| Age (years) | 56.59 (14.00) | 54.06 (16.45) | 55.32 (15.10) |
| Sex (M in %) | 82.35% (14) | 70.59% (12) | 76.5% (26) |
| Height (cm) | 174.25 (7.89) | 173.64 (9.20) | 173.95 (8.44) |
| Weight (kg) | 81.31 (13.05) | 90.74 (38.99) | 86.02 (26.03) |
| BMI | 26.74 (3.88) | 30.45 (14.35) | 28.60 (10.52) |
| Duration Injury (years) | 8.75 (9.74) | 10.32 (11.13) | 9.53 (10.33) |
| Para AIS C–D | 17.65% (3) | 29.41% (5) | 23.5% (8) |
| Tetra AIS C–D | 82.35% (14) | 70.59% (12) | 76.5% (26) |
| ASI motor score: UEMS | 38.29 (7.44) | 37.47 (13.83) | 37.88 (10.95) |
| ASI motor score: LEMS | 30.41 (8.19) | 27.94 (9.76) | 29.18 (8.96) |
| ASI motor score: TMS | 68.71 (11.32) | 65.47 (17.61) | 67.09 (14.67) |
| Ambulatory participants at baseline | 8 out of 11 | 13 out of 16 | 21 out of 27 |
| Etiology of SCI: MVA | 29.41% (5) | 23.53% (4) | 26.47% (9) |
| Etiology of SCI: Fall | 47.06% (8) | 41.18% (7) | 44.12% (15) |
| Etiology of SCI: GSW | 0% (0) | 5.88% (1) | 2.94% (1) |
| Etiology of SCI: Sports | 5.88% (1) | 23.53% (4) | 14.71% (5) |
| Etiology of SCI: Other | 17.65% (3) | 5.88% (1) | 11.76% (4) |
*The values are shown in mean (standard deviation).
BMI, body mass index; SCI, spinal cord injury.
Functional measures
SCIM
Table 2 shows the group means for SCIM. The SCIM data were available at both baseline and 12-month follow-up for 26 participants (one participant's SCIM data in the intervention group were not available for the baseline). The total SCIM scores showed a significant change over time (F(1, 24) = 4.75, P = 0.039). The main effect of the groups (F(1, 24) = 0.254, P = 0.619) and the time-group interaction (F(1, 24) = 2.681, P = 0.115) were not significant. In other words, there was no statistically significant difference in total SCIM scores between the groups, while both groups experienced increase in total SCIM scores at 12-month follow-up compared with baseline.
Table 2 .
Mean scores of Intervention (FES) and Control (CON) Groups on gait measures, functional measures, and balance measures. The values are shown as: mean (standard deviation)
| n - analyzed | Baseline |
4-month |
6-month |
12-month |
|||||
|---|---|---|---|---|---|---|---|---|---|
| FES/CON | FES | CON | FES | CON | FES | CON | FES | CON | |
| Gait measures | |||||||||
| 6-min walking test | |||||||||
| 2-min walk distance [m] | FES = 11 CON = 7 |
57.1 (43.2) |
27.4 (29.1) |
68.2 (46.2) |
43.5 (15.0) |
66.6 (50.0) |
45.8 (27.2) |
67.2 (46.2) |
42.9 (20.7) |
| 4-min walk distance [m] | FES = 11 CON = 7 |
115.3 (79.6) |
52.9 (56.5) |
134.1 (85.1) |
83.1 (27.5) |
135.2 (91.5) |
89.3 (53.4) |
138.1 (82.1) |
86.6 (45.6) |
| 6-min walk distance [m] | FES = 9 CON = 7 |
187.9 (123.4) |
79.4 (83.9) |
217.1 (134.4) |
130.9 (46.0) |
219.3 (146.2) |
132.3 (79.1) |
232.5 (138.9) |
126.4 (63.8) |
| 10-m walking test | |||||||||
| 10-m walk time [sec] | FES = 14 CON = 7 |
42.8 (46.2) |
49.1 (41.7) |
35.2 (49.8) |
28.7 (8.3) |
33.8 (39.8) |
30.9 (12.7) |
42.2 (67.7) |
35.1 (18.8) |
| WMS | FES = 16 CON = 11 |
2.6 (1.4) |
2 (1.2) |
2.7 (1.5) |
2.6 (1.4) |
2.9 (1.4) |
2.7 (1.7) |
2.8 (1.4) |
3.4 (3.2) |
| ADM | FES = 16 CON = 11 |
9.2 (2.6) |
6.3 (4.0) |
9.3 (3.0) |
6.9 (3.4) |
9.0 (2.8) |
6.6 (2.7) |
8.9 (2.8) |
7.2 (3.0) |
| Balance and mobility measure | |||||||||
| TUG [sec] | FES = 10 CON = 6 |
43.6 (25.5) |
61.6 (36.2) |
33.0 (15.7) |
49.5 (21.9) |
33.2 (16.7) |
43.2 (15.3) |
32.2 (19.1) |
51.3 (19.6) |
| Functional measures | |||||||||
| SCIM | FES = 15 CON = 11 |
57.7 (17.8) |
63.9 (18.9) |
– | – | – | – | 64.1 (19.2) |
64.8 (13.4) |
| SCIM mobility sub-score | FES = 15 CON = 11 |
17.27 (7.25) |
19.09 (7.08) |
– | – | – | – | 21.33 (7.62) |
17.36 (5.46) |
| FIM locomotor score | FES = 16 CON = 11 |
4.70 (1.82) |
4.18 (2.14) |
5.19 (1.80) |
4.82 (1.66) |
5.00 (1.86) |
4.81 (1.78) |
5.19 (1.83) |
5.09 (2.98) |
FES, functional electrical stimulation; WMS, walking mobility scale; TUG, timed up-and-go test; SCIM, spinal cord independence measure; FIM, functional independence measure.
SCIM mobility sub-score
There was no significant main effect for time (F(1, 24) = 1.747, P = 0.199) and no difference between the groups (F(1, 24) = 0.166, P = 0.687) on the SCIM mobility sub-score (Fig. 2 and Table 2). However, the interaction was significant (F(1, 24) = 10.716, P = 0.003). The mean score at baseline for the intervention group was 17.27 (SD = 7.25) and 19.09 (SD = 7.08) for the control group. The scores at 12 months post-intervention were 21.33 (SD = 7.62) for the intervention group and 17.36 (SD = 5.46) for the control group. When the interaction was examined, it was determined that the SCIM mobility sub-scores improved over time for the intervention group (P < 0.01) but not for the control group.
Figure 2 .
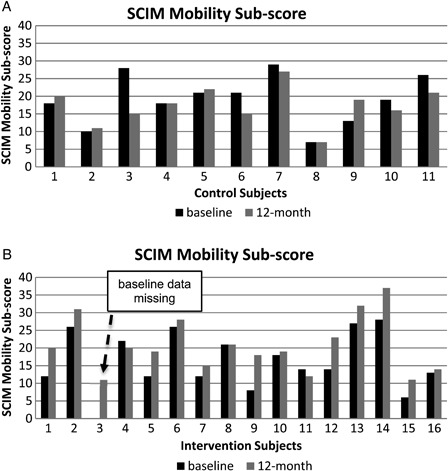
Individual subject results on the SCIM Mobility Sub-score assessment: a) Control Group results and b) Intervention Group results.
FIM locomotor score
We did not perform any statistical tests for this measure as no changes were seen in the FIM locomotor scores over the course of the study (Table 2).
Gait measures
6-Minute walking test
There was a wide variability in the baseline walking ability of the participants recruited, ranging from participants being unable to take any steps on over ground walking with or without an assistive device to participants being able to cover 413.9 m on a 6-minute walk test (intervention subject 2). Figure 3 shows the individual data for 2-minute walking distance. Of the 34 participants who were recruited and randomized, at baseline, 18 were able to complete a 2-minute walk at least at two time-points, 18 were able to complete a 4-minute walk, and 16 participants were able to complete a 6-minute walk. Irrespective of group allocation almost all participants showed an increase over time in the distance covered on the 2-minute (F(3, 48) = 7.09, P < 0.001), 4-minute (F(3, 48) = 6.33, P = 0.001), and 6-minute (F(3, 42) = 5.80, P = 0.002) walk distances (Fig. 3 and Table 2). However, there was no statistically significant difference between the two groups on any of the above three measures (F(1, 16) = 1.79, P = 0.199; F(1, 16) = 2.40, P = 0.141; F(1, 14) = 3.18, P = 0.096; for the 2-, 4-, and 6-minute walking distances, respectively). Furthermore, there was no significant interaction for any of these measures for any of the time points (F(3, 48) = 0.525, P = 0.667; F(3, 48) = 0.410, P = 0.746; F(3, 42) = 0.431, P = 0.732; for the 2-, 4-, and 6-minute walking distances, respectively).
Figure 3 .

Individual subjects results during 2-min Walk Tests: a) Control Group results and b) Intervention Group results. “Unable to walk” suggests that the participant was unable to perform the tests on all four assessment occasions.
10-Meter walking test
Of the 34 participants, 21 were able to complete the 10-meter walk test at baseline (intervention group – 14 and control group – 7). Figure 4 shows the individual data for 10-meter walking time, and its group result is shown in Table 2. A wide range of walking speeds were seen in our sample ranging from participants being unable to ambulate over ground (intervention subjects 3 and 15 and control subjects 2, 4, and 10) to a maximum walking speed of 1.66 m/s (intervention subject 11). The 10-meter walk test showed no significant change over time (F(1.27, 24.0) = 3.07, P = 0.084) and there was no difference between the groups (F(1, 19) = 0.048, P = 0.829). The interaction was also not significant (F(1.27, 24.0) = 1.78, P = 0.195).
Figure 4 .
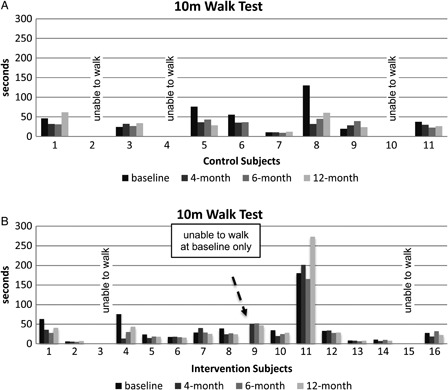
Individual subjects results during 10m Walk Tests: a) Control Group results and b) Intervention Group results. ”Unable to walk” suggests that the participant was unable to perform the tests on all four assessment occasions.
WMS and ADM
We did not perform any statistical tests for these measures. No changes were seen in the use of assistive devices (walking aids) for the participants over the course of the study, except for two participants (Table 2). One participant in intervention group went from using a cane at baseline to no walking aid at discharge and follow-up assessments. The second participant from the intervention group went from using a walker at baseline to no walking aids at discharge. However, this individual was using a walker when they returned for follow-up assessments at 6 months and the same individual used a cane when they returned for follow-up assessments at 12 months.
Balance and mobility measure
TUG
Sixteen participants were able to perform the TUG at baseline (intervention group – 10 and control group – 6). The average time taken to complete the test by the entire cohort was 51.3 seconds indicating that most of the participants recruited to the study were at risk for falling.27
The TUG test showed significant change over time (F(1.56, 21.9) = 5.55, P = 0.016) and there was no difference between the groups (F(1, 14) = 2.48, P = 0.138). The interaction was also not significant (F(1.56, 21.9) = 0.579, P = 0.528). In other words, there was no statistically significant difference in TUG scores between the groups, while both groups experienced increase in TUG scores at 4-, 6-, and 12-month follow-up assessments compared with baseline. Only two of the participants in the intervention group were able to complete the test in less than 14 seconds, which is considered the cut-off for increased risk of falls.27 It is worth noting that three participants in the intervention group including the two participants who were able to complete the test in less than 14 seconds were able to complete the TUG in less than 14 seconds at 12-month follow-up.
Spasticity measures
MAS
The MAS test for most of the muscles around the hip, knee, and ankle, except the right quadriceps and the left dorsiflexors, showed no statistically significant change over time or between groups. The time group interaction was also not significant. The right quadriceps showed a significant change overtime; however, this change was in an unexpected direction, i.e. spasticity in the right quadriceps worsened in both control group (0.58(1.17) and 0.92(1.24) at baseline and 4-month, respectively) and intervention group (0.13(0.34) and 0.44(0.81) at baseline and 4-month, respectively) (F(1, 26) = 5.272, P = 0.015). There was no significant main effect for group (F(1,26) = 2.15, P = 0.155), and no significant time-by-group interaction (F(1,26) = 0.005, P = 0.942).
Pendulum test
There was no statistically significant difference over time or between groups for the right or left leg (see Table 3). The time-by-group interaction was also not significant for either leg.
Table 3 .
Summarized results of the statistical analysis for the pendulum test*
| Time component of the pendulum test | ||||
|---|---|---|---|---|
| Limb | Source | df | F | P (1 – tailed) |
| Right leg | Group | (1, 13) | 0.067 | 0.400, NS |
| Time | (3, 39) | 1.802 | 0.082, NS | |
| Group × time | (3, 39) | 0.274 | 0.422, NS | |
| Left leg | Group | (1, 18) | 0.064 | 0.402, NS |
| Time | (3, 54) | 1.029 | 0.186, NS | |
| Group × time | (3, 54) | 1.224 | 0.154, NS | |
| Velocity component of the pendulum test | ||||
| Right leg | Group | (1, 13) | 0.001 | 0.490, NS |
| Time | (3, 39) | 0.047 | 0.493, NS | |
| Group × time | (3, 39) | 0.631 | 0.300, NS | |
| Left leg | Group | (1, 18) | 0.012 | 0.457, NS |
| Time | (3, 54) | 1.146 | 0.170, NS | |
| Group × time | (3, 54) | 1.768 | 0.082, NS | |
*None of the results were statistically significant.
Discussion
In this study, we found that based on the SCIM mobility sub-score the FES-assisted walking training was superior to a conventional exercise program, which included aerobic and resistance exercises. The SCIM mobility sub-score was the only outcome in this study that was significantly better after the FES-assisted walking intervention compared witn a conventional exercise program. On all other outcome measures, FES-assisted walking training was not superior to a conventional exercise program.
Of note, within group comparisons for two groups suggested that both interventions were efficacious. Both intervention group (FES group) and control group (conventional exercise group) improved significantly from the time they were assessed at baseline compared with assessments taken at 4-, 6-, and 12-month time intervals on the following measures: (i) 2-minute walking distances, (ii) 4-minute walking distances, (iii) 6-minute walking distances, and (iv) TUG. As such, both the intervention group and control group demonstrated improved functional abilities as a result of their respective therapies. The improvements in both intervention and control groups following 40 sessions of respective therapies were clinically meaningful and statistically significant, and they persisted over time. This essentially means that either of these two therapeutic interventions was able to improve walking ability in individuals with chronic traumatic incomplete SCI, but that FES-assisted walking may not be superior to a tailored exercise program that also targets walking.
To the best of our knowledge, this study was the first randomized control trial that has systematically attempted to look at the benefits of using a multichannel FES system to activate the lower limb muscles in close-to-physiological activation sequences.9,11 We chose an active comparator primarily to reduce attrition, but we were also interested in understanding if it was the FES-assisted walking, or just participating in therapeutic exercise, that could improve walking. To that end, we allowed participants in the group receiving conventional exercise to participate in lower extremity strengthening and, depending on individual ability, over-ground walking training. One of the key findings of our study is that the individuals with chronic traumatic incomplete SCI have the potential to improve function even years after injury. These results further support findings published by the NeuroRecovery Network27,28 and Field-Fote's team,29 which suggest that individuals with chronic incomplete SCI can improve gait if they are involved in a structured and task oriented rehabilitation program. This finding re-emphasizes the need for rehabilitation in chronic traumatic incomplete SCI population, and it also demands a change in attitude that 12–18 months following SCI, patients are not expected to improve any longer. This study and other recent studies in this patient population12,13,21,28,30–38 clearly demonstrate that individuals with chronic traumatic incomplete SCI have a capacity to improve walking and grasping function years following the injury.
Rehabilitation interventions for improving gait in individuals with incomplete SCI include BWSTT training, robotic devices and FES, and it is unclear whether one is superior to another. There is conflicting evidence regarding the benefits of BWSTT training and robot-assisted treadmill training for improving walking ability in SCI population, and presumably that is one of the reasons that these therapies have not been adopted widely in clinical practice.30,31,39 In a review by Wessels et al.,40 the authors concluded that over ground training is actually better than BWSTT training, i.e. individuals with subacute incomplete SCI who trained over ground reached higher levels of independent walking compared with individuals trained on BWSTT. The authors also indicated a need for more randomized controlled trials to clarify the effectiveness of BWSTT on walking ability, activities of daily living and quality of life for subgroups of persons with an incomplete SCI. In a recent study done by Schwartz et al.,39 the authors evaluated the benefits of Lokomat robotic training over conventional physiotherapy in subacute incomplete SCI, and found that all participants improved their walking ability measured by the Functional Ambulation Category and Walking Index of Spinal Cord Injury, irrespective of their group allocation. Therefore, our study adds to a growing body of evidence that suggests that walking training can improve with task-specific practice, but the optimal method remains elusive.
As noted, the FES therapy applied in this randomized clinical trial was different from most widely used FES intervention for walking in SCI population, which is better known as the drop foot stimulation.11 The drop foot stimulator is an FES system used to stimulate the peroneal nerve. Pending which stimulation method and which branch of the peroneal nerve is stimulated one can elicit either the spinal withdrawal reflex or a contraction of the tibialis muscle. The tibialis muscle contraction generates foot dorsiflexion that very effectively compensates for drop foot. On the other hand, the activation of the spinal withdrawal reflex essentially produces a “feeling of stepping on a sharp object” and in response to that sensation the leg moves away from the “sharp object”. By fine tuning the stimulation that is used to activate the spinal withdrawal reflex one can generate a leg movement that looks less abrupt and is sufficiently prolonged to appear like a walking sequence.15 A distinction has to be made that this is not a proper gait sequence. To date, there is no solid evidence to show that the foot dorsiflexion stimulation + BWSTT training or spinal withdrawal reflex + BWSTT training are superior to over ground walking or BWSTT training alone or robotic training.21,29,41,42 Probably the reasons for that finding is the fact that the spinal withdrawal reflex stimulation does not activate the lower limb muscles in the temporarily correct manner, as walking and the spinal withdrawal reflex have different muscle activation patterns and they engage different spinal circuits.9,11 Also, the drop foot is fairly infrequent and relatively minor problem in the SCI population, making it more challenging to demonstrate the benefits of foot dorsiflexion stimulation compared to other therapeutic interventions. Nevertheless, there is emerging evidence that the drop foot stimulation that produces only dorsiflexion, if it is used as a short term therapy, is capable of inducing lasting neurolastic changes in the motorcortex10.
This is why we anticipated that our multichannel FES intervention, which activates the multitude of limb muscles in the close-to-physiological activation sequences, would be superior as a neurorehabilitation intervention for improving voluntary walking function compared with conventional aerobic and resistance exercises. However, contrary to our hypothesis, FES-assisted walking was not superior to conventional exercise. The only exception was SCIM mobility sub-score, which was significantly higher after the FES-assisted walking intervention as compared with a conventional exercise program. However, this was the only assessment that showed a difference between the two groups. We have previously shown that individuals with chronic traumatic incomplete SCI can improve upper limb function with FES training, but that the benefits are more profound in the subacute (<6 months) stage.32–35 Therefore, future research might consider evaluating the efficacy of multichannel FES-assisted walking therapy in individuals with SCI who are subacute (<6 months post-SCI).
Limitations
Our study has several limitations that should be acknowledged. Our study may not have been adequately powered to detect small but clinically meaningful differences. Further, many participants could not complete all measures at all time points, resulting in missing data. Future research may need to choose a measure that is responsive to change across a wider range of gait abilities, or make the ability to complete the primary outcome an inclusion criterion. Our sample had a very wide range of functional abilities ranging from participants being wheelchair bound to participants who were community ambulators. There is evidence suggesting that individuals with SCI who have slower walking speed and limited ambulatory distance have a greater potential to improve, compared with those with increased gait abilities.20,29 We propose that future research include individuals with at least grade 2 manual muscle testing scores in key lower extremity muscles. Another limitation of this study is that we did not compare FES therapy to usual care, i.e. no intervention. Although we did not directly compare FES-assisted walking intervention to no intervention, the fact that subjects who took part in the study were individuals with chronic (≥18 months) SCI who were neurologically stable at the time they joined the study, suggests that FES-assisted walking intervention is better than no intervention. On the other hand, we believe that we were able to retain a large proportion of our sample at 12-month follow-up because we had an active comparator.
Conclusion
FES therapy for walking resulted in improved voluntary walking function in individuals with traumatic and chronic (≥18 months) motor incomplete SCI (level C2 to T12, AIS C or D), but it was not superior to an equal dose (45 minutes per session, with 3 sessions per week for 16 weeks) of aerobic and resistance training. The FES-assisted walking training was only superior to a conventional exercise program with respect to SCIM mobility sub-score, which was significantly higher after the FES-assisted walking intervention compared to a conventional exercise program. We speculate that the heterogeneity of the patient population that took part in the study, as well as the small sample size, resulted in the findings that are for the most part inconclusive. We believe that a study that will be performed with a larger sample size and with a much more homogenous population will be able to provide more conclusive results with respect to efficacy of the FES-assisted walking intervention. On the other hand, we can conclude that even in the chronic stage a structured and task oriented training may improve the walking function of individuals with chronic incomplete SCI.
Disclaimer statements
Contributors NK, KM, BCC, LMG, SLH, KR and MRP contributed in designing the study, and writing and analyzing data. NK, KM, LMG, SLH, KR helped with data acquisition and patient management. BCC and MRP helped to secure funding for the study and to manage the study.
Funding None.
Conflicts of interest None.
Ethics approval http://www.clinicaltrials.gov – NCT00201968.
Acknowledgements
This project was supported by the Ontario Neurotrauma Foundation [2004-SCI-SC-04] and by the Toronto Rehabilitation Institute – University Health Network.
References
- 1.Rick Hansen Institute and Urban Futures Dec 2010 The Incidence and Prevalence of Spinal Cord Injury in Canada Overview and estimates based on current evidence. Available at: http://fecst.inesss.qc.ca/fr/archives/nouvelle/article/the-incidence-and-prevalence-of-spinal-cord-injury-in-canada-overview-and-estimates-based-on-curren-1.html Accessed September 5, 2014.
- 2.Ditunno PL, Patrick M, Stineman M, Ditunno JF. Who wants to walk? Preferences for recovery after SCI: a longitudinal and cross-sectional study. Spinal Cord. 2008; 46(7):500–6 [DOI] [PubMed] [Google Scholar]
- 3.Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007;45(3):190–205 [DOI] [PubMed] [Google Scholar]
- 4.Curt A, van Hedel HJA, Klaus D, Dietz V. Recovery from a spinal cord injury: Significance of compensation, neural plasticity, and repair. J Neurotrauma 2008;25(6):677–85 [DOI] [PubMed] [Google Scholar]
- 5.Harkema SJ, Schmidt-Read M, Lorenz D, Edgerton VR, Behrman AL. Balance and ambulation improvements in individuals with chronic incomplete spinal cord injury using locomotor training-based rehabilitation. Arch Phys Med Rehabil 2012;93(9):1508–17 [DOI] [PubMed] [Google Scholar]
- 6.Masani K, Popovic MR. Chapter 46 – functional electrical stimulation: applications in rehabilitation and neurorehabilitation. In: Kramme R, Hoffmann KP, Pozos RS, (eds.) Springer handbook of medical technology. Springer; 2011. pp. 877–96 [Google Scholar]
- 7.Popovic MR, Thrasher TA. Neuroprostheses In: Wnek GE, Bowlin GL, (eds.) Encyclopedia of biomaterials and biomedical engineering. Marcel Dekker, Inc; 2004. Vol. 2, p. 1056–65 [Google Scholar]
- 8.Brissot R, Gallien P, Le Bot MP, Beaubras A, Laisné D, Beillot J, et al. Clinical experience with functional electrical stimulation-assisted gait with Parastep in spinal cord-injured patients. Spine (Phila Pa 1976) 2000;25(4):501–8 [DOI] [PubMed] [Google Scholar]
- 9.Thrasher TA, Flett HM, Popovic MR. Gait training regimen for incomplete spinal cord injury using functional electrical stimulation. Spinal Cord 2006;44(6):357–61 [DOI] [PubMed] [Google Scholar]
- 10.Stein RB, Everaert DG, Thompson AK, Chong SL, Whittaker M, Robertson J, et al. Long-term therapeutic and orthotic effects of a foot drop stimulator on walking performance in progressive and nonprogressive neurological disorders. Neurorehabil Neural Repair 2010;24(2):152–67 [DOI] [PubMed] [Google Scholar]
- 11.Thrasher TA, Popovic MR. Functional electrical stimulation for walking: function, exercise and rehabilitation. Ann Readapt Med Phys 2008;51(6):452–60 [DOI] [PubMed] [Google Scholar]
- 12.Field-Fote EC Combined use of body weight support, functional electric stimulation, and treadmill training to improve walking ability in individuals with chronic incomplete spinal cord injury. Arch Phys Med Rehabil 2001;82(6):818–24 [DOI] [PubMed] [Google Scholar]
- 13.Ladouceur M, Barbeau H. Functional electrical stimulation-assisted walking for persons with incomplete spinal injuries: longitudinal changes in maximal overground walking speed. Scandinavian J Rehabil Med 2000;32(1):28–36 [DOI] [PubMed] [Google Scholar]
- 14.Andrews AW, Chinworth SA, Bourassa M, Garvin M, Benton D, Tanner S. Update on distance and velocity requirements for community ambulation. J Geriatric Phys Ther 2010;33(3):128–34 [PubMed] [Google Scholar]
- 15.Popovic MR, Keller T. Modular transcutaneous functional electrical stimulation system. Med Eng Phys 2005;27(1):81–92 [DOI] [PubMed] [Google Scholar]
- 16.Giangregorio L, Craven BC, Richards K, Kapadia N, Hitzig SL, Masani K, et al. A randomized trial of functional electrical stimulation for walking in incomplete spinal cord injury: effects on body composition. J Spinal Cord Med 2012;35(5):351–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hitzig SL, Craven BC, Panjwani A, Kapadia N, Giangregorio LM, Richards K, et al. A randomized trial of functional electrical stimulation therapy for walking in incomplete spinal cord injury: effects on quality of life and community participation. Top Spinal Cord Inj Rehabil 2013;19(4):245–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guyatt GH, Sullivan MJ, Thompson PJ. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985;132(8):919–23 [PMC free article] [PubMed] [Google Scholar]
- 19.Van Hedel HJ, Wirz M, Dietz V. Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil 2005;86(2):190–6 [DOI] [PubMed] [Google Scholar]
- 20.Leahy TE Impact of a limited trial of walking training using body weight support and a treadmill on the gait characteristics of an individual with chronic, incomplete spinal cord injury. Physiother Theory Pract 2010;26(7):483–9 [DOI] [PubMed] [Google Scholar]
- 21.Field-Fote EC, Roach KE. Influence of a locomotor training approach on walking speed and distance in people with chronic spinal cord injury: a randomized clinical trial. Phys Ther 2011;91(1):48–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Itzkovich M, Tamir A, Philo O, Steinberg F, Ronen J, Spasser R, et al. Reliability of the Catz-Itzkovich spinal cord independence measure assessment by interview and comparison with observation. Am J Phys Med Rehabil 2003;82(4):267–72 [DOI] [PubMed] [Google Scholar]
- 23.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. In: Eisenberg MG, Grzesiak RC, (eds.) Advances in clinical rehabilitation. New York: Springer Publishing Company; 1987 [PubMed] [Google Scholar]
- 24.Sköld C, Harms-Ringdahl K, Hulting C, Levi R, Seiger A. Simultaneous Ashworth measurements and electromyographic recordings in tetraplegic patients. Arch Phys Med Rehabil 1998;79(8):959–65 [DOI] [PubMed] [Google Scholar]
- 25.Jamshidi M, Smith AW. Clinical measurement of spasticity using the pendulum test: comparison of electrogoniometric and videotape analyses. Arch Phys Med Rehabil 1996;77(11):1129–32 [DOI] [PubMed] [Google Scholar]
- 26.Eser P, de Bruin ED, Telley I, Lechner HE, Knecht H, Stussi E. Effect of electrical stimulation-induced cycling on bone mineral density in spinal cord-injured patients. Eur J Clin Invest 2003;33(5):412–9 [DOI] [PubMed] [Google Scholar]
- 27.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys Ther 2000;80:896–903 [PubMed] [Google Scholar]
- 28.Harkema SJ, Schmidt-Read M, Lorenz DJ, Edgerton VR, Behrman AL. Balance and ambulation improvements in individuals with chronic incomplete spinal cord injury using locomotor training-based rehabilitation. Arch Phys Med Rehabil 2012;93(9):1508–17 [DOI] [PubMed] [Google Scholar]
- 29.Field-Fote EC, Lindley SD, Sherman AL. Locomotor training approaches for individuals with spinal cord injury: a preliminary report of walking-related outcomes. J Neurol Phys Ther 2005;29(3):127–37 [DOI] [PubMed] [Google Scholar]
- 30.Alexeeva N, Sames C, Jacobs PL, Hobday L, Distasio MM, Mitchell SA, et al. Comparison of training methods to improve walking in persons with chronic spinal cord injury: a randomized clinical trial. J Spinal Cord Med 2011;34(4):362–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lucareli PR, Lima MO, Lima FP, de Almeida JG, Brech GC, D'Andréa Greve JM. Gait analysis following treadmill training with body weight support versus conventional physical therapy: a prospective randomized controlled single blind study. Spinal Cord 2011;49(9):1001–7 [DOI] [PubMed] [Google Scholar]
- 32.Kapadia N, Zivanovic V, Popovic MR. Restoring voluntary grasping function in individuals with incomplete chronic spinal cord injury: pilot study. Top Spinal Cord Inj Rehabil 2013;19(4):279–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Popovic MR, Kapadia N, Zivanovic V, Furlan JC, Craven BC, McGillivray C. Functional electrical stimulation therapy of voluntary grasping versus only conventional rehabilitation for patients with subacute incomplete tetraplegia: a randomized clinical trial. Neurorehabil Neural Repair 2011;25(5):433–42 [DOI] [PubMed] [Google Scholar]
- 34.Kapadia N, Popovic MR. Toronto Rehabilitation Institute's function electrical stimulation therapy for grasping in SCI: an overview. Top Spinal Cord Inj Rehabil 2011;17(1):70–6 [Google Scholar]
- 35.Popovic MR, Thrasher TA, Adams ME, Takes V, Zivanovic V, Tonack MI. Functional electrical therapy: retraining grasping in spinal cord injury. Spinal Cord 2006;44(3):143–51 [DOI] [PubMed] [Google Scholar]
- 36.Forrest GF, Lorenz DJ, Hutchinson K, Vanhiel LR, Basso DM, Datta S, et al. Ambulation and balance outcomes measure different aspects of recovery in individuals with chronic, incomplete spinal cord injury. Arch Phys Med Rehabil 2012;93(9):1553–64 [DOI] [PubMed] [Google Scholar]
- 37.Yang JF, Musselman KE, Livingstone D, Brunton K, Hendricks G, et al. Repetitive mass practice or focused precise practice for retraining walking after incomplete spinal cord injury? A pilot randomized clinical trial. http://pubget.com/journal/1545-9683/neurorehabilitation-and-neural-repairNeurorehabil Neural Repair 2014;28(4):314–24 [DOI] [PubMed] [Google Scholar]
- 38.Labruyère R, van Hedel HJA. Strength training versus robot-assisted gait training after incomplete spinal cord injury: a randomized pilot study in patients depending on walking assistance. J NeuroEng Rehabil 2014;11(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schwartz I, Sajina A, Neeb M, Fisher I, Katz-Luerer M, Meiner Z. Locomotor training using a robotic device in patients with subacute spinal cord injury. Spinal Cord 2011;49(10):1062–7 [DOI] [PubMed] [Google Scholar]
- 40.Wessels M, Lucas C, Eriks I, de Groot S. Body weight-supported gait training for restoration of walking in people with an incomplete spinal cord injury: a systematic review. J Rehabil Med 2010;42(6):513–9 [DOI] [PubMed] [Google Scholar]
- 41.Field-Fote EC, Fluet GG, Schafer SD, Schneider EM, Smith R, Downey PA, et al. The Spinal Cord Injury Functional Ambulation Inventory (SCI-FAI). Journal of Rehabilitation Medicine 2001;33:177–81 [DOI] [PubMed] [Google Scholar]
- 42.Postans NJ, Hasler JP, Granat MH, Maxwell DJ. Functional electric stimulation to augment partial weight-bearing supported treadmill training for patients with acute incomplete spinal cord injury: a pilot study. Arch Phys Med Rehabil 2004;85(4):604–10 [DOI] [PubMed] [Google Scholar]


